Stroke is considered as the third most common cause of death and the single most common cause of disability worldwide.1 Headache often accompanies stroke with a prevalence varying between 7% and 65% depending on different data sources.2 In 1664, Thomas Willis described the autopsy finding of a patient who reported a right-sided headache and was found to have asymptomatic ipsilateral carotid artery occlusion. He also found dilatation of the left carotid and vertebral arteries up to 3 times the normal size.3 Since then, numerous papers were published regarding headache caused by different cerebrovascular lesions and the relationship between migraine and stroke.2 In this report, we present a case of a man who developed a new headache occurring for the first time with close temporal relation to vertebrobasilar insufficiency. In addition, a convulsive motor phenomenon is described in this case report which was difficult to differentiate from epileptogenic seizures. The case was challenging due to several difficulties including the delay in diagnosis, timing of neuroimaging, and the subsequent development of ischemic pontine stroke with no thrombolysis offered.
A 73-year-old male who was previously healthy until the day of presentation to the Emergency Department when he complained of sudden severe left temporal and retro-orbital headache that lasted minutes followed by dysarthria, facial asymmetry, and dense right hemiplegia. His weakness lasted only 20 minutes with full recovery. He was admitted to the hospital and was started on dual antiplatelet therapy including aspirin 81 mg daily and clopidogrel 75 mg daily. He was diagnosed as a case of transient ischemic attack. An extensive workup was carried out including electrocardiogram, echocardiography, computed tomography (CT) scan of the head, Doppler carotid, and all results came back unremarkable. On the third day following admission, he had 3 more similar attacks with each lasting 30 to 60 minutes. Interestingly, he developed brief intermittent right leg jerky movement that was described as a recurrent clonic movement of the right leg with each attack of transient ischemic attack with resolution once the symptoms disappear. The right leg jerky movement was not associated with loss of consciousness and not responding to 2 anti-epileptic medications (Levetiracetam and Lamotrigine). Routine electroencephalogram failed to show any abnormality. Both CT perfusion and magnetic resonance imaging (MRI) of the brain with diffusion were done which were absolutely normal. On the fifth day of admission, he developed another similar attack with persistence of dysarthria and hemiplegia. Neuroimaging was not repeated due to a refusal of the neuroradiologist to perform any further studies given the numerous normal previous examinations. Two days later and after a lengthy discussion, MRI of the brain was repeated, which demonstrated an acute infarction of the left medial aspect of the pons (Figure 1A). Magnetic resonance angiography of cerebral vasculatures demonstrated irregularity involving the left vertebral artery and basilar artery with mild luminal stenosis suggestive of atherosclerosis (Figure 1B). His past medical history was only remarkable for hypertension with no history of migraine, dyslipidemia, cardiac disease, trauma, and neck pain. Family and social history were all unremarkable. Clinically, the patient had right facial asymmetry, dysarthria, and dense hemiplegia. Upper extremities showed a power of 0/5 and the lower extremities showed a power of 3/5. He had right Babinski sign, and the rest of the examination was unremarkable. Thrombolysis was not offered to the patient, and he was transferred to a rehabilitation center for further management including physiotherapy and occupational therapy. The patient was seen in the clinic 6 months following discharge with remarkable improvement in his motor functions and speech.
Figure 1.
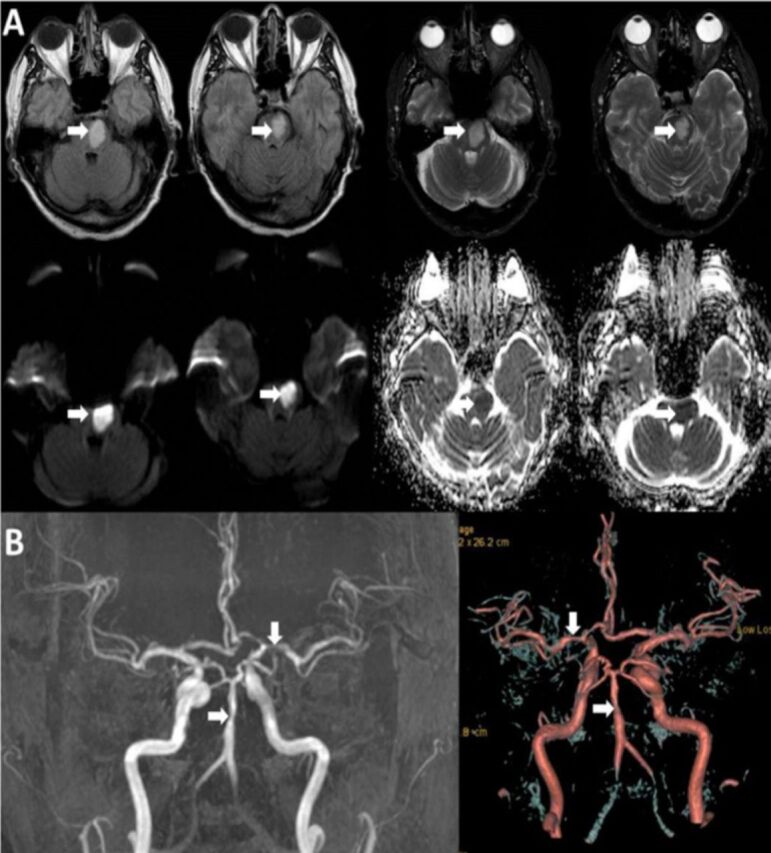
Neuroimaging studies of our patient with A) MRI of the brain showing acute infarction at the left aspect of the pons/lower midbrain with high signal intensity on FLAIR and T2-weighted images and restriction of diffusion with minimal mass effect and, B) MRA showing multiple segments with irregularity and narrowing at the basilar artery and left M-1 segment.
Headache attributed to ischemic stroke is described as “a new headache developing simultaneously with or in close temporal relationship to signs or other evidence of ischemic stroke associated with neuroimaging confirmation of ischemic infarction”. When a new headache occurs for the first time in close temporal relation to symptoms and signs suggestive of a vascular disorder, it should be considered and coded as a secondary headache disorder until proven otherwise. This is also true if the headache has the clinical characteristics of primary headache disorders such as migraine or cluster headache. Factors that support adding the diagnosis of a secondary headache disorder (vascular) include a close temporal relation to the vascular disorder, marked worsening of the pre-existing headache, good evidence that the vascular disorder can aggravate the headache, and improvement of the headache after the acute phase of the vascular disorder.2 In our patient, the headache was new with a close temporal relation with the signs and symptoms of stroke including dysarthria and hemiplegia. Unfortunately, frequently performed neuroimaging including CT and MRI were unremarkable, which made the treating team diagnose him as a primary headache disorder, mainly hemiplegic migraine. For this reason, he was not offered thrombolytic therapy despite labeling him in our rounds as the gentleman with “Willis Headache”.
The headache of ischemic cerebrovascular disease is usually unilateral, focal, of mild to moderate severity, and likely to be abrupt or gradual in onset. In 1940, Ray and Wolff observed that stimulation of a single vessel in the meninges and at the base of the brain resulted in an ipsilateral headache, which is in accordance with several recent and extensive studies. In 1962, Williams and Wilson3 reported that 21-53% of patients with vertebrobasilar insufficiency developed occipital headache that was either lateralized or nonlateralized. It was described as throbbing or bursting in nature that is frequently accentuated by stooping and straining. Rarely, headache was localized to occipitofrontal or frontal distributions (lateralized or nonlateralized) and was described as band-like. Several studies reported that anterior circulation stroke (carotid) usually give rise to frontal headache and that posterior circulation strokes cause occipital headache.2
The capsular and pontine warning syndromes are defined as a subset of crescendo transient ischemic attacks and characterized by repetitive episodes of motor dysfunction due to ischemia in the region of internal capsule and pons, respectively. Since its first description by Donnan et al4 in the 1980s, several reports were published regarding this vascular entity. Upon reviewing the literature, none of these reports described headache as part of the symptoms of this syndrome.
The pathophysiological mechanisms behind the development of headache in association with acute ischemic stroke include hemorrhagic transformation, edema, and changes in the trigeminovascular system. The headache symptoms is more likely to occur in the posterior circulation strokes compared to strokes in other vascular territories. This could be due to the heavy innervation of the cerebral vasculature of meninges in the posterior circulation by nociceptive afferents. Another possible explanation includes vasodilation of arteries following emboli or thrombus formation in the base of the brain or occlusion of several arterial branches leading to change in the vascular perfusion. A further mechanism may be the release of vasoactive substances (e. g. serotonin and prostaglandin) from activated platelets.1,2 The trigeminal nerve has an important role in pain transmission and blood flow control. This is indicated by the circumscribed unilateral headache and pain referred to the cutaneous receptive field of the first trigeminal division. The pial nerve fibers are of trigeminal origin, and the perivascular nerve fibers contain vasoactive neuropeptides (e. g. calcitonin gene-related peptide and substance P), which on release into the vessel wall, increase blood flow and vascular permeability. The origin and distribution of the perivascular afferent fibers explain several unique features of vascular headache. For example, the predominantly ipsilateral distribution of trigeminal fibers explains the strictly ipsilateral distribution in many vascular headaches. In addition, the bilateral innervation of certain vessels (e. g. anterior cerebral artery) explains the bilateral or even contralateral location of the headache in diseases affecting these vessels. Moreover, the dual innervation of the superior cerebellar artery and the rostral basilar artery (i.e. from the upper cervical roots and the trigeminal fibers) provides an anatomical explanation for the coexistence of occipital and frontal headaches.1
In general, headache disorder has no specific diagnostic workup. However, if a red flag exists and an underlying secondary etiology is suspected, careful diagnostic evaluation is warranted. In cryptogenic strokes or strokes in young patients, further tests should be considered including anticardiolipin antibodies, antithrombin III, lupus anticoagulant, and protein C and S. Neuroimaging studies (CT, MRI, MRA, or CTA) are necessary to evaluate the possibility of aneurysm, subarachnoid hemorrhage, intracerebral hemorrhage, cerebral neoplasm, or ischemic infarct. Cerebrospinal fluid analysis may be considered to rule out subarachnoid hemorrhage, primary central nervous system angiitis, or central nervous system infection. Cardiac evaluation may exclude or confirm a cardiogenic or aortic source of cerebral embolism and should include electrocardiography, Holter monitor, and transesophageal echocardiography.2
There is no particular information available for the management of headache associated with an ischemic cerebrovascular disease. Headache can be treated with acetylsalicylic acid or acetaminophen (when hemorrhage is excluded). Triptans and dihydroergotamine are contraindicated. Beta-blockers or calcium-channel blockers may be used if antihypertensive treatment is indicated.2
Patients with brainstem strokes may develop involuntary convulsive-like movements that vary in nature, frequency, and trigger. This phenomenon was reported in few articles in the literature with all patients having normal electroencephalogram, preserved consciousness, and no effect of anti-epileptic medications. The mechanism behind the occurrence of such movements could be due to ischemia of the corticospinal tract bilaterally or disruption of the inhibitory projection of the cortex to the spine or brainstem.5
In conclusion, this paper reported a rare case of vertebrobasilar insufficiency associated with unilateral headache and convulsive-like movements. This case indicates that a frontal headache with dysarthria, hemiplegia, and convulsive-like movements are warning signs for posterior circulation stroke that should be taken seriously. Elderly patients presenting a new headache for the first time that is recurrent, not responding to treatment, or presenting with a clinical red flag should be fully investigated to rule out a vascular disorder, mainly stroke. Early identification of a stroke within the therapeutic window of thrombolytic therapy will lead to better outcomes and may be life-saving. We are reporting two new symptoms to be added to the list of symptoms of pontine warning syndrome.
References
- 1.Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30. doi: 10.3389/fneur.2014.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diener HC, Katsarava Z, Weimar C. Headache associated with ischemic cerebrovascular disease. Rev Neurol (Paris) 2008;164:819–824. doi: 10.1016/j.neurol.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Willis T. Thomas Willis: the anatomy of the brain and nerves. Montreal: McGill University Press; Cerebre anatome: cui accesit nervorum descripto et usus, reporduced in fascimile. In: Feindel W, editor. p. 1664. [Google Scholar]
- 4.Donnan GA, O’malley HM, Quang L, Hurley S, Bladin PF. The capsular warning syndrome: pathogenesis and clinical features. Neurology. 1993;43:957–962. doi: 10.1212/wnl.43.5.957. [DOI] [PubMed] [Google Scholar]
- 5.Saposnik G, Caplan LR. Convulsive-like movements in brainstem stroke. Arch Neurol. 2001;58:654–657. doi: 10.1001/archneur.58.4.654. [DOI] [PubMed] [Google Scholar]


