Abstract
Objectives:
To descriptively assess Epilepsy Monitoring Units (EMUs) and the provided services in Saudi Arabia and compare them based on the geographic region.
Methods:
In this cross-sectional study, an electronic questionnaire was emailed to all directors of EMUs in Saudi Arabia from July 2013 to January 2016, with constant updates being made by all respondents throughout the period of data collection.
Results:
All EMU directors participated. There were 11 EMUs in KSA operating in 8 hospitals; 8 (54.5%) EMUs in Riyadh, 2 (18.2%) in Dammam, 2 (18.2%) in Makkah and 1 (9.1%) in Jeddah. Five (54.5%) EMUs were shared for adults and pediatrics, 3 (27.3%) were devoted to adult patients, and 3 (27.3%) to pediatric patients. The average waiting time was 11 weeks (range: 2-52 weeks). The mean percentage of patients coming from an outside region was 30.6%. The average length of stay was 7 days. Less than 100 patients were monitored annually in 54.5% of the EMUs. Seven EMUs (63.6%) admitted less than 100 patients for seizure characterization. Intracranial monitoring was available in all EMUs. Most EMUs (54.5%) admitted less than 100 patients for pre-surgical workup while 36.4% admitted 100-199, and 9.1% admitted more than 300 patients per year. Epilepsy surgeries were performed for less than 50 patients annually in 81.8% of the hospitals.
Conclusion:
There are 11 EMUs in Saudi Arabia fully equipped to serve epileptic patients. However, they are underutilized considering the number of admitted patient and the number of epilepsy surgeries per year. Also, they are unequally distributed throughout the kingdom.
Epilepsy is a common neurological disorder in the Kingdom of Saudi Arabia (KSA) affecting 6.54 per 1,000 Saudis.1 It affects patients of different age groups, and is known to negatively influence patients’ quality of life.2,3 Epilepsy represents a burden to the community and economy, which can be aggravated if the disorder is not properly managed.4-6 Multiple studies have been conducted over the world investigating the services provided to epileptic patients.7-9 Such services include the Epilepsy Monitoring Units (EMUs), which provide Long-term video-electroencephalography monitoring (LTM).10 The LTM is an important investigational tool used for improving accuracy of the diagnosis of different spells, for seizure classification, and for completing pre-surgical workup in patients with drug resistant epilepsy.11 Numerous reports from various countries have discussed the characteristics of their EMUs;10,12-16 however, similar studies have not been conducted in Saudi Arabia, which has a population of approximately 32.3 million, despite the presence of EMUs in several regions of the country. Thus, our objectives are to descriptively assess the EMUs and the provided services in Saudi Arabia and to perform a region based comparison.
Methods
In this cross-sectional study, an electronic questionnaire was designed to collect the following information regarding EMUs: the region, unit type (adult, pediatrics, or shared), percentage of patients admitted from outside regions, waiting time, average stay time, and the number of adult and pediatric epileptologists, neurologists, neurosurgeons, epilepsy neurosurgeons, neuropsychologists, and technicians, and the number of beds. The survey also included questions about the date of establishment and number of cases monitored per year, along with questions about the available diagnostic modalities and the workup performed for the admitted patients in the EMU. The questions on diagnostic modalities included the availability and number of cases monitored using electroencephalograms (EEG), magnetic resonance imaging (MRI), functional MRI (fMRI), positron emission tomography (PET), single-photon emission computed tomography (SPECT), magnetoencephalography (MEG) and intracranial monitoring (ICM). Additionally, questions related to epilepsy surgery and stimulation treatment for intractable epilepsy were added.
The study was approved by the Institutional review board (IRB) of King Saud University. After the IRB approval, a list of all the tertiary hospitals and EMUs in Saudi Arabia was obtained through officials in the Saudi Ministry of Health and the Saudi Epilepsy Society. The inclusion criteria involved all hospitals with EMUs in Saudi Arabia. Other tertiary hospitals without EMUs were excluded from the study. The questionnaire was emailed to the directors of all the EMUs in Saudi Arabia from July 2013 to January 2016 with constant updates being made by all the respondents through the period.
Statistical analysis
The data was entered in an excel spreadsheet then converted into a IBM Statistical Package for the Social Sciences (SPSS) dataset. The frequencies and percentages for all variables were obtained, and the means and ranges of all numeric variables were calculated using for Windows, Version 21.0. (Armonk, NY: IBM Corp.). The files were split by the region and unit type and then analyzed for comparison purposes.
Results
All EMUs directors participated. There were 11 EMUs in Saudi Arabia operating in 8 hospitals; 8 (54.5%) EMUs in Riyadh, 2 (18.2%) in Dammam, 2 (18.2%) in Makkah and 1 (9.1%) Jeddah. Five (54.5%) EMUs were shared for adults and pediatric, 3 (27.3%) were devoted only for adult patients, and 3 (27.3%) were devoted only for pediatrics. The number of in-patient beds allocated to neurology departments in all hospitals was 161, with a mean of 20 beds per hospital (range: 13-30). The total number adult EMU beds was 31, with a mean of 3.88 beds per hospital (range: 2 -7). The total number of pediatric EMU beds was 12, with a mean of 1.5 beds per hospital (range: 1–3). Table 1 shows manpower in the 8 hospitals with EMUs.
Table 1.
Descriptive analysis of manpower in the 8 hospitals with epilepsy monitoring units in Saudi Arabia.
| Staff | Minimum number in a hospital | Maximum number in a hospital | Total number in all hospitals |
|---|---|---|---|
| Adult Epileptologists | 1 | 4 | 16 |
| Pediatric Epileptologists | 0 | 4 | 11 |
| Adult Neurologists | 4 | 13 | 55 |
| Pediatric Neurologists | 0 | 7 | 23 |
| Adult Neurosurgeons | 2 | 6 | 33 |
| Pediatric Neurosurgeons | 0 | 3 | 10 |
| Adult Epilepsy Neurosurgeons | 1 | 2 | 9 |
| Pediatric Epilepsy Neurosurgeons | 0 | 1 | 4 |
| Technicians | 1 | 5 | 25 |
The average waiting time in the 11 EMUs was 11 weeks (range: 2–52). The mean percentage of patients coming from an outside region was 30.6% (range: 5-80%). The average length of EMU stay was 7 days (range: 4-14 days).
Patients admitted to EMUs for seizure characterization were less than 100 in 7 (63.6%), 100-199 in 2 (18.2%), 200-299 in 1 (9.1%), and more than 300 in 1 (9.1%). Patients admitted to EMUs for pre-surgical evaluation were less than 100 in 6 (54.5%), 100-199 in 4 (36.4%), and more than 300 in 1 (9.1%).
Table 2 shows the available diagnostic utilities (outpatient EEG, inpatient EEG, ambulatory EEG, MRI, fMRI, SPECT, PET and MEG) for all the EMUs and how many times per year they were utilized. Intracranial monitoring (ICM) was available in all EMUs. All but one EMU provided ICM for less than 50 patients annually. Only one EMU provided ICM for 50-99 patients annually.
Table 2.
Availability and utilization of diagnostic modalities in the 8 hospitals with epilepsy monitoring units.
| Diagnostic modality | Availability in hospitals | The ranges of cases investigated per year | The number of EMUs |
|---|---|---|---|
| Outpatient EEG | 100% | 500-799 | 2 |
| 800-1000 | 1 | ||
| More than 1000 | 5 | ||
| Inpatient EEG | 100% | 100-299 | 2 |
| 300-499 | 2 | ||
| 500-799 | 3 | ||
| More than 1000 | 1 | ||
| Ambulatory EEG | 87.5% | Less than 100 | 3 |
| 100-199 | 3 | ||
| 200-300 | 1 | ||
| MRI | 100% | 100-199 | 2 |
| 200-300 | 2 | ||
| More than 300 | 4 | ||
| Functional MRI | 50% | Less than 50 | 4 |
| SPECT | 87.5% | 1-49 | 5 |
| 50-99 | 1 | ||
| More than 200 | 1 | ||
| PET | 75% | 1-49 | 3 |
| 50-99 | 1 | ||
| 100-200 | 1 | ||
| More than 200 | 1 | ||
| MEG | 12.5% | 50-99 | 1 |
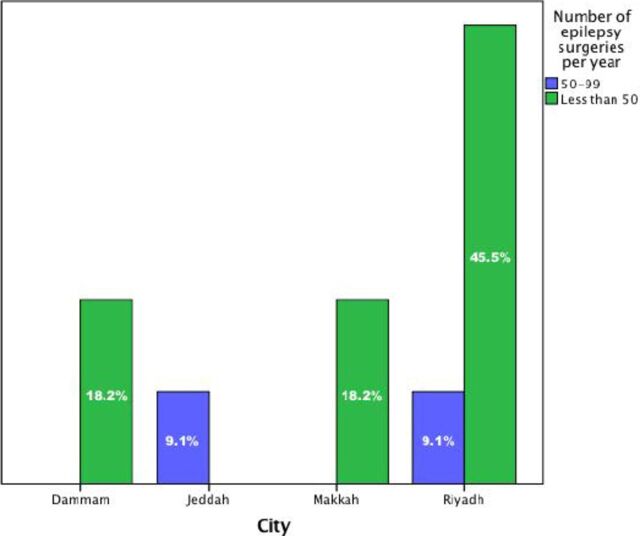
The performed epilepsy surgeries per year were less than 50 in 81.8% of the hospitals, and 50-99 in the remaining hospitals. Figure 1 shows the variation between cities based on the number of epilepsy surgeries per year. Surgeries for lesional epilepsy were performed for 10-49 patients in 63.6% of the hospitals, while less than 10 patients had such surgeries performed in 36.4% of the hospitals. Non-lesional epilepsy surgeries were performed for less than 50 patients in 54.5% of the hospitals, while the remaining hospitals did not provide such surgeries.
Figure 1.
The number of performed epilepsy surgeries in the 4 cities with epilepsy monitoring units.
Eight (72.7%) EMUs located in Riyadh, Jeddah and Dammam provide vagal nerve stimulation (VNS) as a treatment modality for intractable epilepsy. The VNS was performed for 352 patients annually with a mean of 44 (range: 12-70) per EMU. Deep brain stimulation was not utilized by any of the participating hospitals at the time of the study.
Neuropsychologists were available at 81.8% of the EMUs. The total number of neuropsychologists was 14 with an average of 1.56 (range: 1-3) per EMU. Nine (81.8%) EMUs had psychologists to treat patients with pseudoseizures, while the remainder had psychiatrists to manage such cases. Table 3 demonstrates allocation of EMUs and their resources in the 4 cities.
Table 3.
Demonstrates the differences between the cities with epilepsy monitoring units (EMU).
| Comparison Variables | EMU Cities | |||
|---|---|---|---|---|
| Dammam | Jeddah | Makkah | Riyadh | |
| Establishment year of first EMU | 2010 | 2002 | 2010 | 1998 |
| Number of shared EMUs | 0 | 1 | 2 | 2 |
| Number of adult EMUs | 1 | 0 | 0 | 2 |
| Number of pediatric EMUs | 1 | 0 | 0 | 2 |
| Average percentage of patients from outside regions | 40% | 30% | 12.5% | 40% |
| Average waiting time (weeks) | 10 | 12 | 2 | 14.7 |
| Number of adult epileptologists | 1 | 2 | 3 | 10 |
| Number of pediatric epileptologists | 1 | 1 | 0 | 9 |
| Number of adult epilepsy neurosurgeons | 1 | 1 | 2 | 5 |
| Number of pediatric epilepsy neurosurgeons | 1 | 0 | 0 | 3 |
| Technicians | 3 | 3 | 4 | 15 |
| Number of adult EMU beds | 2 | 2 | 9 | 18 |
| Number of pediatric EMU beds | 2 | 2 | 1 | 7 |
| Patient’s average stay in EMU (days) | 5.5 | 5 | 5 | 8.2 |
EMU - Epilepsy monitoring units
Discussion
We performed this study to characterize the EMUs in Saudi Arabia. It is evident that there are many fully equipped EMUs in the country. However, these EMUs are underutilized considering the number of admitted patients and the number of epilepsy surgeries performed per year. A possible reason for such underutilization is the lack of supportive services beyond physicians, such as limited number of EMU technicians, as we noted that there were only 3 EMU technicians in Damam and 1 technician in another EMU unit in western region.
The distribution of EMUs among the provinces of the country represents a significant barrier to care provision as 30% of all patients had to travel from a different city. In Riyadh, where most of the EMUs (54.5%) are located, 80% of patients were from other regions. Located in Riyadh are 6 EMUs with 18 beds for adult patients and 7 for pediatric patients serving an approximate population of 7 million. On the other hand, there are no EMUs in the Asir region which has a population of around 2 million.17 There are 2 main healthcare sectors in Saudi Arabia. The first belongs to the government and the other is the private sector. In this regard, it is important to mention that all the EMUs are governmental facilities. Thus, access to EMU services is generally limited to Saudi Nationals.
Based on our results, VNS has been implemented widely in Saudi Arabia unlike deep brain stimulation (DBS). The VNS has proven to be effective in managing epilepsy along with other disorders like depression.18-20 However, VNS is not the scope of this article as it has already been discussed thoroughly in the local and international literature.21-23 Rubboli et al13 had previously published a study about safety issues in 48 EMUs in 18 European countries. Similar data to that provided in the present study were found in their article. Despite the difference in terms of the response rates between our study (100%) and Rubboli et al13 (32%), comparisons were conducted and are shown in Table 4. The EMUs in Saudi Arabia are underutilized as only 1 of the 11 EMUs admitted more than 250 patients per year compared with 9 of the 48 EMUs in Europe, this is despite the long waiting lists in Saudi Arabia.13 Most of the European EMUs (74%) were shared for adult and pediatric patients, which may allow the provision of a higher quality of training for residents, fellows, technicians and nurses. The length of stay is long in Saudi EMUs, Spritzer et al14 conducted a study investigating the EMU services in Mayo Clinic and Bannar Good Samaritan Hospital; the mean length of stay at both sites was 4.5 and 3.3 days, respectively. This is shorter than that in our study, and might be related to the fact that the majority of patients who travel from distant regions to seek treatment in Saudi hospital might stay longer in hospitals because they are unable to complete outpatient management ahead of admission and additional time is usually required to arrange for return trips. Further comparisons could not be performed due to methodological differences.
Table 4.
Shows the differences between epilepsy monitoring units in KSA and those in 18 European countries.
| Comparison variables | EMUs in KSA n (%) | EMUs in Europe13 n (%) |
|---|---|---|
| Availability of intracranial monitoring | ||
| Yes | 11 (100) | 37 (77) |
| No | 0 (0) | 11 (23) |
| EMU type | ||
| Adult | 3 (27.3) | 6 (13) |
| Pediatric | 3 (27.3) | 6 (13) |
| Shared | 5 (45.4) | 36 (74) |
| Number of EMU beds | ||
| 1–2 | 5 (45.4) | 20 (43) |
| 3–4 | 2 (18.2) | 16 (34) |
| 5–6 | 2 (18.2) | 9 (19) |
| >6 | 2 (18.2) | 2 (4) |
| Average number of admissions per year | ||
| <50 | 3 (27.3) | 8 (17) |
| 50–150 | 5 (45.4) | 17 (36) |
| 150–250 | 2 (18.2) | 13 (28) |
| >250 | 1 (9.1) | 9 (19) |
A major limitation in this study is the long period of data collection, which was minimized by the constant update of information from the respondents. This study did not investigate the epilepsy services provided by hospitals with no EMUs as it has already been discussed previously.24
In conclusion, there are 11 EMUs in Saudi Arabia fully equipped to serve epileptic patients. They also appears to be a potential to service more patients per year at most centers. It seems that the unbalanced regional distribution of EMUs probably impedes timely patient assessments, and further development of EMUs at highly populated yet underserviced regions would improve overall epilepsy care throughout the Kingdom. Thus, further studies are needed to address the obstacles and suggest solutions.
Footnotes
References
- 1.Al Rajeh S, Awada A, Bademosi O, Ogunniyi A. The prevalence of epilepsy and other seizure disorders in an Arab population: a community-based study. Seizure. 2001;10:410–414. doi: 10.1053/seiz.2001.0602. [DOI] [PubMed] [Google Scholar]
- 2.Gao L, Xia L, Pan SQ, Xiong T, Li SC. Burden of epilepsy: a prevalence-based cost of illness study of direct, indirect and intangible costs for epilepsy. Epilepsy Res. 2015;110:146–156. doi: 10.1016/j.eplepsyres.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Gulpek D, Bolat E, Mete L, Arici S, Celebisoy M. Psychiatric comorbidity, quality of life and social support in epileptic patients. Nord J Psychiatry. 2011;65:373–380. doi: 10.3109/08039488.2011.565798. [DOI] [PubMed] [Google Scholar]
- 4.Riechmann J, Strzelczyk A, Reese JP, Boor R, Stephani U, Langner C, et al. Costs of epilepsy and cost-driving factors in children, adolescents, and their caregivers in Germany. Epilepsia. 2015;56:1388–1397. doi: 10.1111/epi.13089. [DOI] [PubMed] [Google Scholar]
- 5.Bolin K, Berggren F, Landtblom AM. Prevalence and cost of epilepsy in Sweden--a register-based approach. Acta Neurol Scand. 2015;131:37–44. doi: 10.1111/ane.12297. [DOI] [PubMed] [Google Scholar]
- 6.Begley CE, Durgin TL. The direct cost of epilepsy in the United States: A systematic review of estimates. Epilepsia. 2015;56:1376–1387. doi: 10.1111/epi.13084. [DOI] [PubMed] [Google Scholar]
- 7.Bennett L, Bergin M, Gooney M, Doherty CP, Synnott C, Wells JS. Epilepsy services in Ireland:'A survey of people with epilepsy in relation to satisfaction, preferences and information provision'. Epilepsy Res. 2015;113:11–18. doi: 10.1016/j.eplepsyres.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Iyer A, Appleton R. Transitional services for adolescents with epilepsy in the U.K.: a survey. Seizure. 2013;22:433–437. doi: 10.1016/j.seizure.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Reuber M, Torane P, Mack C. Do older adults have equitable access to specialist epilepsy services? Epilepsia. 2010;51:2341–2343. doi: 10.1111/j.1528-1167.2010.02661.x. [DOI] [PubMed] [Google Scholar]
- 10.Buelow JM, Privitera M, Levisohn P, Barkley GL. A description of current practice in epilepsy monitoring units. Epilepsy Behav. 2009;15:308–313. doi: 10.1016/j.yebeh.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Alving J, Beniczky S. Diagnostic usefulness and duration of the inpatient long-term video-EEG monitoring: findings in patients extensively investigated before the monitoring. Seizure. 2009;18:470–473. doi: 10.1016/j.seizure.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Wagner JL, Berg AT. Direct health care charges for new-onset pediatric epilepsy: How much does it cost? Neurology. 2015;85:486–487. doi: 10.1212/WNL.0000000000001819. [DOI] [PubMed] [Google Scholar]
- 13.Rubboli G, Beniczky S, Claus S, Canevini MP, Kahane P, Stefan H, et al. A European survey on current practices in epilepsy monitoring units and implications for patients'safety. Epilepsy Behav. 2015;44:179–184. doi: 10.1016/j.yebeh.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Spritzer SD, Pirotte BD, Agostini SD, Aniles E, Hentz JG, Noe KH, et al. The influence of staffing on diagnostic yield of EMU admissions: a comparison study between two institutions. Epilepsy Behav. 2014;41:264–267. doi: 10.1016/j.yebeh.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 15.Sauro KM, Macrodimitris S, Krassman C, Wiebe S, Pillay N, Federico P, et al. Quality indicators in an epilepsy monitoring unit. Epilepsy Behav. 2014;33:7–11. doi: 10.1016/j.yebeh.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Labiner DM, Bagic AI, Herman ST, Fountain NB, Walczak TS, Gumnit RJ, et al. Essential services, personnel, and facilities in specialized epilepsy centers--revised 2010 guidelines. Epilepsia. 2010;51:2322–2333. doi: 10.1111/j.1528-1167.2010.02648.x. [DOI] [PubMed] [Google Scholar]
- 17.Central Department of Statistics & Information Statistical Yearbook 47. Riyadh (KSA): General Authority for Statistics; 2011. Available from: https://www.stats.gov.sa/en/node . [Google Scholar]
- 18.Carosella CM, Greiner HM, Byars AW, Arthur TM, Leach JL, Turner M, et al. Vagus Nerve Stimulation for Electrographic Status Epilepticus in Slow-Wave Sleep. Pediatr Neurol. 2016;60:66–70. doi: 10.1016/j.pediatrneurol.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 19.Panebianco M, Zavanone C, Dupont S, Restivo DA, Pavone A. Vagus nerve stimulation therapy in partial epilepsy: a review. Acta Neurol Belg. 2016;116:241–248. doi: 10.1007/s13760-016-0616-3. [DOI] [PubMed] [Google Scholar]
- 20.Ansari S, Chaudhri K, Al Moutaery KA. Vagus nerve stimulation: indications and limitations. Acta Neurochir Suppl. 2007;97:281–286. doi: 10.1007/978-3-211-33081-4_31. [DOI] [PubMed] [Google Scholar]
- 21.Al-Said Y, Baeesa S, Khalid M, Abdeen M, Kayyali HR. Vagus nerve stimulation for refractory epilepsy: experience from Saudi Arabia. Ann Saudi Med. 2015;35:41–45. doi: 10.5144/0256-4947.2015.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Revesz D, Rydenhag B, Ben-Menachem E. Complications and safety of vagus nerve stimulation:25 years of experience at a single center. J Neurosurg Pediatr. 2016;18:97–104. doi: 10.3171/2016.1.PEDS15534. [DOI] [PubMed] [Google Scholar]
- 23.Cukiert A. Vagus Nerve Stimulation for Epilepsy: An Evidence-Based Approach. Prog Neurol Surg. 2015;29:39–52. doi: 10.1159/000434654. [DOI] [PubMed] [Google Scholar]
- 24.Alfayez SM, Aljafen BN. Epilepsy services in Saudi Arabia. Quantitative assessment and identification of challenges. Neurosciences (Riyadh) 2016;21:326–330. doi: 10.17712/nsj.2016.4.20160053. [DOI] [PMC free article] [PubMed] [Google Scholar]