Abstract
Influenza is a global challenge, and future pandemics of influenza are inevitable. One of the lessons learned from past pandemics is that all pandemic influenza viruses characterized to date possess viral genes originating from avian influenza viruses (AIVs). During the past decades, a wide range of AIVs have overcome the species barrier and infected humans with different clinical manifestations ranging from mild illness to severe disease and even death. Understanding the mechanisms of infection in the context of clinical outcomes, the mechanism of interspecies transmission, and the molecular determinants that confer interspecies transmission is important for pandemic preparedness. Here, we summarize the epidemiology, virology, and pathogenicity of human infections with AIVs to further our understanding of interspecies transmission.
Influenza A viruses are classified into different subtypes based on the major antigenic surface glycoproteins hemagglutinin (HA) and neuraminidase (NA). To date, 16 HA and 9 NA subtypes have been identified in aquatic birds. Aquatic birds are considered the natural reservoir in which avian influenza viruses (AIVs) typically cause asymptomatic infections with high viral replication rates. Some subtypes of AIVs can cause severe disease in poultry, especially in chickens. Based on their virulence in chickens, AIVs are therefore divided into high-pathogenicity AIVs (HPAIVs) and low-pathogenicity AIV (LPAIVs) (see fao.org/avianflu/en/index.html). All HPAIVs are of the H5 or H7 subtypes. LPAIVs of the H5 and H7 subtypes can evolve in poultry to become HPAIVs, causing severe disease and high mortality. In 1878, Perroncito was the first to report a serious outbreak of chicken disease in Italy, which was known as fowl plague, and was confirmed as an AIV of the H7N7 subtype in 1955 (Alexander and Brown 2009). Since then, a substantial number of poultry outbreaks caused by HPAI H5 and H7 subtype viruses have been reported worldwide, posing a great challenge for the poultry industry.
AIVs have occasionally caused human infections with clinical manifestations ranging from mild illness to severe disease and even death. Although no sustained human-to-human transmission has occurred, human infections with AIVs remain a cause for great concern for at least two reasons: First, viruses of the H5 and H7 subtypes may cause severe human disease with high case fatality rates (CFRs) (40%–60%), and second, recent studies indicate that HPAI H5 viruses require only a few amino acid mutations to become airborne transmissible among ferrets, highlighting the potential pandemic risk caused by AIVs (Herfst et al. 2012; Imai et al. 2012).
EPIDEMIOLOGY OF HUMAN INFECTIONS WITH AIVs
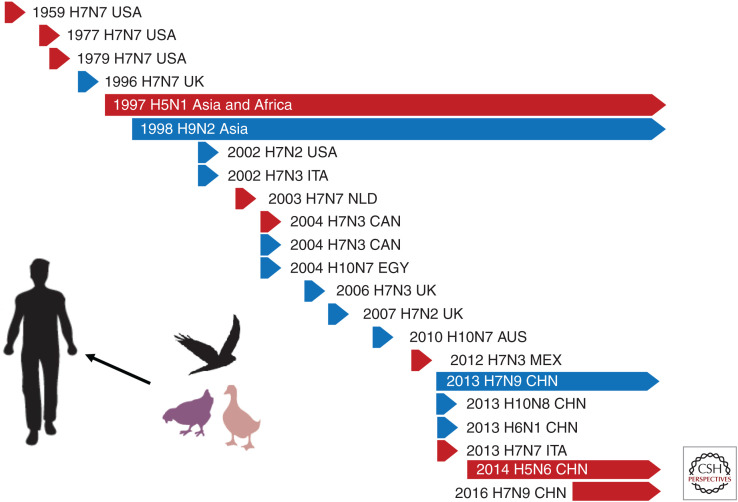
Because of the species barrier, AIVs rarely infect humans. In recent decades, both HPAIVs and LPAIVs have caused sporadic human infections, which are typically transmitted directly from poultry to humans. HPAIVs (H5N1, H5N6, H7N7, H7N3, and H7N9) and LPAIVs (H7N2, H7N3, H9N2, H7N9, H6N1, H10N7, and H10N8) have all caused human infections (Fig. 1). However, none of these avian viruses has transmitted efficiently among humans.
Figure 1.
The history of human infections with avian influenza viruses (AIVs). Arrows in red and blue indicate human infections with high-pathogenicity AIVs (HPAIVs) and low-pathogenicity AIVs (LPAIVs), respectively. The length of the arrows represents the time frame during which human cases were reported. (USA) United States of America, (UK) United Kingdom, (ITA) Italy, (NLD) the Netherlands, (CAN) Canada, (EGY) Egypt, (AUS) Australia, (MEX) Mexico, (CHN) China.
Human Infections with HPAI H5 Viruses
In 1997, the first laboratory-confirmed human infection with an HPAI H5N1 virus was documented in a 3-yr-old boy with acute pneumonia and respiratory distress syndrome in the Hong Kong Special Administrative Region (SAR) of China (Fig. 1). This fatal case showed that a purely AIV can cause respiratory disease and death in humans (Claas et al. 1998; Subbarao et al. 1998; Bender et al. 1999). Seventeen patients were subsequently diagnosed, including six fatal cases in Hong Kong. In 2003, human infections with HPAI H5N1 viruses reemerged in Asia (Peiris et al. 2004). Since then, as of September 2019, 861 cases of laboratory-confirmed human infections with highly pathogenic H5N1 AIVs have been reported in 17 countries, including 455 deaths (see who.int/influenza/human_animal_interface/2019_09_27_tableH5N1.pdf). Egypt has reported 359 human cases, and China, Indonesia, Vietnam, and Cambodia each have reported more than 50 human cases. Most of the HPAI H5N1 human cases (∼75%) have occurred in young adults and children (<30 yr of age) (Qin et al. 2015).
In April 2014, the first human infection with an HPAI H5N6 virus (which possessed an HA of the same lineage as HPAI H5N1 viruses) was reported in the Sichuan Province of China (Pan et al. 2016). As of September 2019, 24 HPAI H5N6 human cases have been reported in China, 16 of which were fatal. No HPAI H5N6 human cases have been reported outside China, although poultry outbreaks caused by HPAI H5N6 viruses have been reported in other countries such as Vietnam.
Human Infections with H7 Subtype AIVs
The first influenza A virus isolate was the fowl plague virus (FPV) isolated from chickens in 1902 (Alexander and Brown 2009). In 1955, it was recognized as an influenza A virus through an antigenicity study of the viral nucleoprotein (NP). This virus is now recognized as an H7N7 subtype influenza virus (A/chicken/Brescia/1902 [H7N7]) (Alexander and Brown 2009).
In 2003, an HPAI H7N7 influenza virus outbreak resulted in the death of tens of millions of poultry in the Netherlands. During this outbreak, 89 poultry workers were infected; most of them presented with conjunctivitis, except one veterinarian who died of severe pneumonia (van Kolfschooten 2003; Fouchier et al. 2004). Two H7N3 human cases were reported in Canada in 2004 (Tweed et al. 2004), caused by HPAI H7N3 and LPAI H7N3 viruses, respectively (Figs. 1 and 2) (Hirst et al. 2004).
Figure 2.
Areas with confirmed human cases of avian influenza virus (AIV) infection since 2000. The affected countries are colored in red. Labels indicate cases other than H5N1; imported cases are shown in blue. The map was created with mapchart.net.
In the spring of 2013, the first human infection with an LPAI H7N9 virus was reported in the Yangtze River Delta region of China (Gao et al. 2013b). The virus was not pathogenic to poultry, but most of the laboratory-confirmed human infections resulted in severe illness, and even death (Gao et al. 2013b; Zhang et al. 2013b). Before the vaccination of poultry was implemented in mainland China, five waves of H7N9 outbreaks occurred (Zhu et al. 2018). During the fifth wave in 2016–2017, the LPAI H7N9 virus evolved into an HPAI H7N9 virus, which caused high mortality among chickens, and also infected humans (Deng et al. 2017; Ke et al. 2017; Yang and Liu 2017; Zhang et al. 2017a). As of September 2019, a total of 1568 laboratory-confirmed H7N9 human cases have been reported, with a CFR of ∼39% (Wang et al. 2017) (see chinaivdc.cn/cnic/en/). All human H7N9 cases originated in China; two human H7N9 cases reported in Malaysia and Canada were traced back to travelers from China.
In January 2018, one human infection with an H7N4 subtype AIV was identified in the Jiangsu Province of China (Tong et al. 2018). This was the first human infection with an H7N4 virus. Since then, no additional H7N4 human cases have been reported (Figs. 1 and 2).
Human Infections with H9N2 Subtype AIVs
The first reported human infections with H9N2 AIVs occurred in Guangdong province in southern China in 1998, including two cases in Shaoguan city and three cases in Shantou city (Guo et al. 1999). The following year, two human infections with H9N2 AIVs were reported in Hong Kong (Peiris et al. 1999). As of September 2019, a total of 35 human infections with H9N2 AIVs have been reported in China, including one fatal case in an individual with underlying disease. Human infections with H9N2 AIVs have also been reported in other countries, including Pakistan, Bangladesh, and Egypt (Figs. 1 and 2). The reported number of human infections with H9N2 AIVs may be an underestimate because of the mild symptoms caused by H9N2 AIVs in humans. Serological studies indicate that additional human infections with H9N2 AIVs have occurred (Lu et al. 2008; Woo and Park 2008; Pawar et al. 2012; Shinde et al. 2012; Zhou et al. 2014; Li et al. 2017).
Human Infections with AIVs of Other Subtypes
In May 2013, the only human infection with an H6N1 virus was reported in Taiwan province, China (Wei et al. 2013). From November 2013 to February 2014, three human infections with H10N8 viruses were reported in Jiangxi province, China, two of which were fatal (Chen et al. 2014); since then, no other human infections with H10N8 viruses have been reported. Mild human infections with H10N7 AIVs have been reported previously in Egypt and Australia (Figs. 1 and 2) (Organization PAH 2004; Arzey et al. 2012). Serological evidence suggests that AIVs of the H4, H6, and H11 subtypes may also have caused human infections (Shortridge 1992; Peiris et al. 2007).
Comparative Epidemiology of Human Infections with H7N9 and H5N1 AIVs
Humans are generally not susceptible to AIV infections, mainly because of the differences in the receptor-binding specificity between human and AIVs. As a consequence, AIVs do not easily cross the species barrier to infect humans. However, as described earlier, AIVs occasionally infect humans. A major source of human infections with AIVs are live poultry markets, where people may be exposed to infected birds, to AIVs in the environment, or both (Wan et al. 2011; Han et al. 2013; Shi et al. 2013b). Limited human-to-human transmission of AIVs may have occurred (Olsen et al. 2005), including vertical transmission (Shu et al. 2006).
Most of the (fatal) human infections with AIVs have been caused by viruses of the H7N9 and H5N1 subtypes. Human H7N9 infections have mainly affected the elderly of >60-yr of age, whereas human H5N1 infections primarily have occurred in young adults. The sex ratio of human infections with H5N1 virus is balanced, but H7N9 AIVs have infected more males than females (with a ratio of 2:1). The CFR of human infections with H7N9 influenza viruses is ∼39%, whereas that of human infections with H5N1 influenza viruses is ∼60% (Cowling et al. 2013b; To et al. 2013; Qin et al. 2015).
VIROLOGICAL CHARACTERISTICS OF HUMAN INFECTIONS WITH AIVs
Typically, all eight viral RNA segments of AIVs that infect humans are derived from AIVs, and there has been no natural reassortment with influenza viruses prevalent in human or pig populations.
Receptor-Binding Profiles of AIVs That Cause Human Infections
Transmission of AIVs to humans is rare, in part because of host range restrictions that limit influenza virus transmissions between avian species and mammals. The host species restriction and cell and tissue tropism of influenza viruses are determined by several factors, including differences in receptor distribution between avian and mammalian cells and differences in the receptor-binding specificities of human and AIVs. The HA proteins of AIVs typically have a binding preference for sialic acid (SA) residues with an α-2,3-Gal terminating sequence found primarily on the surfaces of epithelial cells in the intestinal tract of ducks. In the human respiratory tract, α-2,6 SA receptors are predominantly expressed on ciliated cells in the upper respiratory tract (URT), whereas α-2,3 SA receptors are mainly present on nonciliated cells of the lower respiratory tract (LRT) and on type II pneumocytes (Fig. 3) (Connor et al. 1994; Shinya et al. 2006; Chandrasekaran et al. 2008). Accordingly, although AIVs can infect humans without a change in receptor-binding specificity, mutations that confer binding to α-2,6 SA receptors are likely critical to confer sustained human-to-human transmission. Replication of HPAI H5N1 viruses (which bind to α-2,3 SA receptors) in humans is mainly confined to the LRT, which may have limited the number of virus particles expelled through breathing and/or coughing.
Figure 3.
Airway tract tissue tropism illustration and the receptor-binding profiles of seasonal influenza viruses, avian H5N1 viruses, and influenza A(H7N9) viruses.
Like all subtypes of AIVs, AIVs of the H7 subtype can be subdivided into two genetic lineages according to the geographic origin of the viruses: the North American lineage and the Eurasian lineage, with viruses from both lineages having infected humans (Fig. 1). Most Eurasian H7 subtype viruses resemble HPAI H5N1 viruses in their preferential binding to α-2,3 SA receptors. However, the H7N9 viruses that emerged in 2013 can bind to both SA α-2,3-Gal and SA α-2,6-Gal receptors (Fig. 3) (Shi et al. 2013a; Tharakaraman et al. 2013; Watanabe et al. 2013; Xiong et al. 2013; Zhou et al. 2013). This dual receptor-binding profile may lead to more frequent human infections with H7N9 viruses, as compared with human infections with AIVs of other subtypes.
Key Mammalian-Adapting Molecular Markers of AIVs That Cause Human Infections
One of the most common amino acid substitutions associated with converting LPAI strains from avian- to mammalian-receptor specificity is the HA Q226L substitution (H3 numbering). For example, LPAI H9N2 isolates from birds can acquire a Q226L substitution that increases the viruses’ receptor-binding affinity for mammalian cells and may facilitate the infection of mammalian hosts (Wan et al. 2008). With regard to human isolates of H7N9 viruses, A/Shanghai/1/2013 (encoding HA Q226) and A/Anhui/1/2013 (encoding HA L226) bind preferentially to avian α-2,3-Gal receptor analogs or to both α-2,3-Gal and α-2,6-Gal receptors, respectively (Yamada et al. 2006; Nidom et al. 2010; Yang et al. 2010; Srinivasan et al. 2013). The Q226L mutation has not been commonly observed in the HA of HPAI H5N1 field isolates. The HA G186V substitution (H3 numbering) is associated with the dual receptor-binding specificity of both HPAI and LPAI influenza H7N9 viruses (Shi et al. 2013a; Zhou et al. 2013; Zhu et al. 2017).
Although receptor-binding specificity is an important factor in the interspecies transmission of influenza viruses, additional factors are involved in the mammalian adaptation of AIVs. In 2012, Herfst and colleagues (Herfst et al. 2012) showed that introduction of the HA Q226L/G228S and PB2 E627K mutations into an H5N1 virus did not confer virus transmission via respiratory droplets among ferrets. However, respiratory transmission among ferrets occurred after the virus had been passaged 10 times in ferrets (Herfst et al. 2012), resulting in three additional mutations (PB1 H99Y, HA H110Y, and HA T160A) that might be essential for the viral respiratory droplet transmissibility in ferrets (Linster et al. 2014). In the study by Imai et al. (2012), the artificially introduced substitutions HA N224K/Q226L (which confer binding to α-2,6-Gal receptors) and the additional HA N158D/T318I mutations (which emerged during two passages in ferrets) were required to generate an airborne-transmissible H5 virus (with the remaining seven segments from the human A/ California/04/2009 H1N1 virus) in ferrets. Mutations at either position 158 or 160 resulted in loss of the N-glycosylation site at 158–160 of HA, which has been shown to affect the receptor-binding profiles and the virulence of HPAI H5 viruses (Herfst et al. 2012; Imai et al. 2012). Moreover, H1N1 virus genes encoding the acidic polymerase (PA) and nonstructural (NS1) proteins rendered the H5N1 virus transmissible by respiratory droplets between guinea pigs (Zhang et al. 2013c). Other H1N1 genes, including those that encode the NP, NA, and the matrix (M1) protein, as well as mutations in H5 HA that improve affinity for human-like airway receptors, could enhance the mammal-to-mammal transmission (Zhang et al. 2013c). These reports have established that mutant and/or reassortant H5N1 AIVs can transmit among mammals. Analyses of field viruses indicate that some circulating viruses already contain some of the mutations identified in these H5 transmission studies (Russell et al. 2012). Enhanced surveillance should be performed to closely monitor these mutations in zoonotic influenza viruses.
Besides HA-receptor binding, key factors for viral fitness in mammals include substitutions in the viral polymerase proteins, including PB2-E627K (Table 1) (Hatta et al. 2001). Avian influenza virus isolates exclusively contain glutamic acid at position 627 in PB2, whereas it is frequently mutated to lysine in human-derived isolates (Fonville et al. 2013; Manz et al. 2013). The PB2-E627K mutation is required for the airborne transmissibility of HPAI H5N1 viruses in ferrets and high viral replication in mice (Hatta et al. 2001; Herfst et al. 2012; Imai et al. 2012). However, avian H5N1 and H7N9 viruses that retained the avian-like glutamic acid at position 627 of PB2 have frequently caused fatal human infections (Zhu et al. 2015), indicating that PB2-E627K is not always strictly necessary for avian viruses to infect mammals.
Table 1.
Molecular markers associated with increased transmissibility in animal models of AIVs
| Function | Gene | Position and AA | Reference(s) |
|---|---|---|---|
| Enhanced binding to human-type receptor | H5 | Loss of glycosylation site at 158–160 | Herfst et al. 2012; Imai et al. 2012 |
| 186K | Chutinimitkul et al. 2010; Yamada et al. 2006 | ||
| 190D | Chen et al. 2012; Stevens et al. 2006 | ||
| 196R/H | Chen et al. 2012; Watanabe et al. 2011; Yamada et al. 2006 | ||
| 222E/Q | Guo et al. 2017; Manz et al. 2010 | ||
| 224K | Imai et al. 2012 | ||
| 226L | Harvey et al. 2004; Herfst et al. 2012; Imai et al. 2012; Stevens et al. 2006; Chutinimitkul et al. 2010 | ||
| 227N/R | Chen et al. 2012; Chutinimitkul et al. 2010; Gambaryan et al. 2006; Guo et al. 2017; Shinya et al. 2010 | ||
| 228S | Chutinimitkul et al. 2010; Harvey et al. 2004; Herfst et al. 2012; Stevens et al. 2006; Wang et al. 2010 | ||
| H6 | 225D | de Vries et al. 2017b | |
| 226L | Qu et al. 2017 | ||
| H7 | Gain of glycosylation site at 133 | Srinivasan et al. 2013 | |
| 186V | Xiong et al. 2013; Yang et al. 2010; Shi et al. 2013a; Tharakaraman et al. 2013 | ||
| 193T | de Vries et al. 2017a | ||
| 224K | de Vries et al. 2017a | ||
| 226L/I | Shi et al. 2013a; Srinivasan et al. 2013; Tharakaraman et al. 2013; Xiong et al. 2013 | ||
| 228S | Srinivasan et al. 2013; Tharakaraman et al. 2013 | ||
| H9 | 226L | Wan et al. 2008 | |
| Increased polymerase activity in mammalian host | PB2 | Q591K | Chan et al. 2016; Mok et al. 2014 |
| E627K | Herfst et al. 2014; Mok et al. 2014; Zhu et al. 2015 | ||
| D701N | Mok et al. 2014; Zhu et al. 2015 |
EMERGENCE, EVOLUTION, AND DISSEMINATION OF AIVs THAT CAUSE HUMAN INFECTIONS
LPAI H7N9 Viruses
The influenza A(H7N9) viruses have caused five epidemic waves in humans in China. Since their emergence, studies have been conducted to learn about the viruses’ origin and evolution. Most likely, the HA of these viruses originated from a duck influenza virus; the NA was related to N9 viruses detected in migratory birds, and the six internal genes were from avian influenza H9N2 viruses (Gao et al. 2013b; Liu et al. 2013).
Since the first detection of the novel H7N9 viruses in 2013, the six internal genes have frequently reassorted with those of H9N2 viruses cocirculating in poultry (Wu et al. 2013; Zhang et al. 2013a; Cui et al. 2014; Lam et al. 2015; Wang et al. 2016). From wave III onward, the evolution of the NP gene changed in that it was most frequently derived from cocirculating H7N9 viruses rather than from H9N2 viruses (Zhu et al. 2018). Dynamic reassortment events generated multiple genotypes. Most of these genotypes were transient, although some gradually became dominant. One of the genotypes, ZJ11-like viruses, emerged in the late phase of wave III, slightly increased in frequency late in wave IV, and substantially increased in frequency from the beginning of wave V. The ZJ11 genotype viruses accounted for most of the human infections in wave V (Zhu et al. 2018). Overall, the H7N9 viruses have evolved rapidly since their emergence.
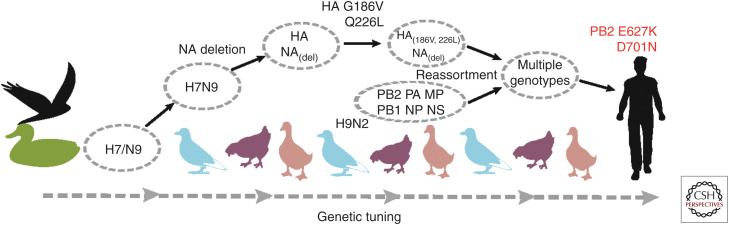
A “genetic tuning” mechanism was proposed to explain the possible process of interspecies transmission of avian H7N9 viruses (Fig. 4) (Wang et al. 2014a; Zhu and Shu 2015). Through this process, H7N9 viruses may have first acquired mutations that facilitate replication in poultry before acquiring mutations that facilitate replication in mammals.
Figure 4.
Proposed “genetic tuning” mechanism for influenza A(H7N9) viruses. (Created from data in Wang et al. 2014a and Zhu and Shu 2015.)
HPAI H7N9 Viruses
Currently, the LPAI H7N9 viruses have evolved into two regionally distinct lineages—the Yangtze Delta lineage and the Pearl Delta lineage—based on the sequences of their HA and NA genes (Wang et al. 2016). Although HPAI H7N9 viruses were first isolated in the Pearl Delta region, they have exclusively belonged into the Yangtze Delta lineage (Ke et al. 2017; Yang et al. 2017). HPAI H7N9 viruses arose from the LPAI H7N9 progenitors. The acquisition of multiple basic amino acids at the HA cleavage site (a hallmark of HPAI, discussed in more detail later) occurred in late May 2016 in the Pearl Delta region. Different motifs of basic amino acids at the HA cleavage site have been detected in HPAI H7N9 viruses in poultry (Shi et al. 2017). In contrast, HPAI H7N9 viruses isolated from humans bear only two types of amino acid insertions (Yang et al. 2017).
Dynamic reassortment of the internal genes of LPAI H7N9 and H9N2 viruses has been broadly reported (Wu et al. 2013; Zhang et al. 2013a; Cui et al. 2014; Lam et al. 2015; Wang et al. 2016). Similar to LPAI H7N9 viruses, HPAI H7N9 viruses also reassorted with LPAI H7N9 or H9N2 viruses in poultry (Yang et al. 2017). Several genotypes emerged that differed in their internal genes. One of these genotypes (Genotype II [Yang et al. 2017]) may have a fitness advantage over the others, because this genotype was the only one to spread from Guangdong province to other regions.
HPAI H5N6 Viruses
HPAI H5N6 viruses are currently circulating in poultry throughout China and South East Asia and occasionally infect humans in China. The HA gene of H5N6 viruses originated from the clade 2.3.4 HPAI H5N1 viruses that emerged in chickens in China in 2005. In 2007, the HPAI H5 viruses evolved into clade 2.3.4.4. From 2009 to 2012, the clade 2.3.4.4. H5 viruses reassorted with waterfowl viruses of different NA subtypes, including N2, N6, and N8, generating HPAI H5N2/N6/N8 viruses (Yang et al. 2016). Phylogenetic and the “time to most recent common ancestor” (tMRCA) analyses suggested that two independent reassortment pathways generated two subclades of H5N6 viruses between 2011 and 2013. In the first pathway, H5N2 viruses with a clade 2.3.4.4 HA gene may have reassorted with an H6N6 virus between mid-2011 and mid-2012 to acquire the N6 NA gene; then, further reassortment might have occurred involving the acquisition of the six internal genes of poultry clade 2.3.2.1c H5N1 viruses, generating so-called “Reassortant A” viruses. In the second pathway, reassortment likely occurred among an H5N8 virus with a clade 2.3.4.4 HA gene, an H6N6 virus with an NA gene containing a deletion in the stalk region, and poultry clade 2.3.2.1c H5N1 viruses, which provided the internal genes; the resulting H5N6 virus was designated “Reassortant B.” Since 2015, consecutive reassortment events of “Reassortant B” H5N6 viruses with the six internal genes from chicken H9N2 viruses have resulted in so-called “Reassortant C” H5N6 viruses (Yang et al. 2016).
All three reassortant viruses have caused human infections. The virus isolated from the first reported H5N6 human case in Sichuan Province in 2014 was a “Reassortant A” virus. Viruses from human cases in Guangdong Province in late 2014 had the gene cassette of “Reassortant B,” and human isolates from Yunnan and Guangdong provinces since 2015 have belonged to “Reassortant C.” Since then, HPAI H5N6 viruses have continued to evolve. In 2016, two H5N6 viruses were isolated from two patients in China. The internal gene cassettes of these two strains differ from those reported previously, representing two novel genotypes of H5N6 viruses (Zhang et al. 2017b). Another novel influenza H5N6 virus with a unique internal gene cassette was isolated from a patient in Jiangsu province in China in 2018 (unpubl. data). Most likely, novel genotypes of H5N6 viruses will continue to emerge.
CLINICAL FEATURES OF HUMAN INFECTIONS WITH AIVs
Clinical Manifestations
AIVs generally do not cause clinical symptoms in their natural reservoir, but poultry (such as chickens) infected with HPAIVs usually present with severe syndromes and high mortality. The clinical presentation of human infections with AIVs varies from mild respiratory symptoms and conjunctivitis to acute pneumonia and even death. Most humans infected with highly pathogenic H5 AIVs develop a severe illness with a high case fatality rate (Yuen et al. 1998; Uyeki 2009; Shinya et al. 2011). Before 2013, conjunctivitis was the main manifestation of human infections with viruses of the H7 subtype, with the exception of a fatal human infection with an HPAI H7 virus (Koopmans et al. 2004). Respiratory conditions, including pneumonia and respiratory distress syndrome, are the main manifestations of human infections with the novel H7N9 AIVs (Gao et al. 2013a; Lu et al. 2013; Yu et al. 2013a,b). Although the novel H10N8 viruses are of the low-pathogenicity type, they can cause serious illness or death (Chen et al. 2014). Symptoms of human infection with H9N2 viruses are generally mild, mainly manifested as respiratory symptoms such as fever.
Viral Factors That Contribute to Severe Clinical Symptoms in Infected People
Pathogenesis is the result of complex interactions between the virus and host, with many factors from both the virus and the host involved in this interplay. Besides the HA-mediated receptor-binding specificity discussed above, key to viral pathogenicity is the presence of a multibasic HA cleavage site (MBCSs). HPAIV generally encode a MBCS at the HA cleavage site (Bosch et al. 1981; Webster and Rott 1987), whereas HAs from mammalian viruses or LPAIV usually encode only a single basic residue at their cleavage site (Garten and Klenk 1999; Klenk and Garten 1994). The presence of the polybasic residues allows the HA to be cleaved by enzymes that are expressed in a wide range of tissues, whereas the cleavage site that contains a single basic residue can only be cleaved by enzymes in the respiratory tract or intestinal tract. Because HA cleavage is required for viral infectivity, the polybasic cleavage site broadens the tissue range of the virus and is strongly associated with systemic spread and increased infectivity and virulence in birds and mammals (Hatta et al. 2001; Tanaka et al. 2003; Suguitan et al. 2012). HPAI H5N1 viruses with an MBCS cause severe infections in humans. Some H7N9 viruses also have acquired an MBCS to become highly pathogenic in chickens. HPAI H7N9 viruses with an MBCS showed increased disease severity in the ferret model compared with an LPAI H7N9 virus (Imai et al. 2017). However, LPAI H7N9 viruses that lack an MBCS still cause severe disease in most human cases (Gao et al. 2013a,b). Thus, the MBCS is a key virulence factor for AIVs in avian species, but not a key determinant for the severity of AIV infections in humans.
Substitutions in the ribonucleoprotein (RNP) complex (which comprises the polymerase subunits PB2, PB1, and PA and NP) are frequently linked to increased replication and virulence of viruses. PB2 is a major host range determinant of influenza viruses. One of the most critical substitutions is PB2-E627K, which, as already mentioned, contributes to human infections with AIVs. The PB2 E627K mutation is strongly linked to increased virulence in mice of HPAIV H5N1 (Hatta et al. 2001; Maines et al. 2005; Chen et al. 2007), HPAIV H7N7 (Munster et al. 2007), LPAIV H7N9 (Mok et al. 2014; Zhu et al. 2015), and the 1918 H1N1 virus (Qi et al. 2012).
Most influenza H7N9 viruses isolated from chickens cause no clinical symptoms in mice and are nonlethal in ferrets (Zhang et al. 2013b; Shi et al. 2017). LPAI or HPAI H7N9 viruses isolated from patients cause mild to severe disease or are lethal in these mammal models, respectively (Richard et al. 2013; Watanabe et al. 2013; Zhu et al. 2013; Imai et al. 2017). Of note, an HPAI H7N9 virus was shown to be more pathogenic in mice and ferrets than an LPAI H7N9 virus (Imai et al. 2017). In addition, H7N9 viruses isolated from humans are generally more transmissible in ferrets than those isolated from avian species (Zhang et al. 2013b; Zhu et al. 2013; Imai et al. 2017; Shi et al. 2017). This may be due to mammalian-adapting mutations, including PB2 E627K. Studies have shown that after replication in mice and ferrets, LPAI or HPAI H7N9 viruses isolated from avian species acquired mammalian-adapting mutations such as PB2 E627K or PB2 D701N (Zhu et al. 2015; Shi et al. 2017). However, no such mutations occurred when the virus replicated in chickens. When HPAI H7N9 viruses of avian origin acquired mammalian-adapting mutations, they became lethal in mice and ferrets and highly transmissible among ferrets (Shi et al. 2017).
Some mutations in PB1 (such as PB1 473V and 598P) and NP (such as NP 357K) have also been found to increase the pathogenicity of AIVs in mammals (Xu et al. 2012; Zhu et al. 2019). Other genes, including those encoding NS1 and the nuclear export protein (NEP), also encode molecular markers associated with pathogenicity. NS1 is critical for natural infection because it inhibits the host innate immune response (Donelan et al. 2003; Hale et al. 2008) through species-specific interactions with multiple host proteins (Rajsbaum et al. 2012). Mutations in NS1 have been frequently observed during mouse adaptation of AIVs (Dankar et al. 2011; Zhang et al. 2011). When crossing the species barrier, HPAIV H5N1 could acquire the adaptive substitution M16I in NEP to escape restricted viral genome replication in human cells (Mänz et al. 2012; Reuther et al. 2014).
Host Factors That Contribute to Severe Clinical Symptoms in Infected People
Several studies have explored the host factors that contribute to the severe clinical symptoms caused by AIV infections, including cytokine storms, preexisting immunity, age biases in exposure to infected poultry (Cowling et al. 2013a; Rivers et al. 2013), and host genes. However, none of these studies can fully explain the patterns of severe disease and mortality. A recent study revealed that childhood HA imprinting could provide profound, lifelong protection against severe infection and death caused by H5N1 and H7N9 viruses (Gostic et al. 2016). This study highlighted the contribution of antigenic imprinting to the severity of clinical symptoms. Nevertheless, we still have a long way to go before we fully understand the complex interplay between the pathogen and the host.
The Cytokine Storm
One hallmark of human HPAI H5 infections is a rapid and robust cytokine response, often referred to as a “cytokine storm” or hypercytokinemia. This buildup of cytokines causes an inflammatory environment at the site of infection, leading to immune cell infiltration (de Jong et al. 2006; Zhou et al. 2013; Wang et al. 2014b; Guo et al. 2015). Following infection with HPAI H5N1 viruses in animal models, including chickens, ferrets, and rhesus macaques, increased expression of specific pro-inflammatory cytokines, particularly interleukin (IL)-6 and IL-8, was observed, suggesting that IL-6 and IL-8 may be key regulators leading to worsened pathology of viruses. Upon human infections with H5N1 viruses, a similarly robust cytokine response occurs with the up-regulation of IL-6, IL-10, and tumor necrosis factor (TNF)-α. The levels of IP-10, MIG, MCP-1, IL-6, IL-8, and IFN-α in sera from H7N9 virus-infected patients were significantly higher than those of healthy people (Zhou et al. 2013). Therefore, the “cytokine storm” caused by disorder of the natural immune response may be an important contributor to severe infections. Infections of chickens with the recently emerged HPAI H5N6 viruses (which have caused several human fatalities), results in a very distinct immune response relative to other H5N6 strains by inducing much higher levels of IL-6, IL-8, and other pro-inflammatory mediators such as TNF-α (Gao et al. 2017).
Tissue Tropism
Unlike seasonal influenza virus infections, which are often confined to the respiratory system, H5N1 AIV infection can cause viremia (Likos et al. 2007). H5N1 viruses can be detected and isolated in the plasma of the patients, and the virus can spread to all organs and tissues including the brain (Chutinimitkul et al. 2006; Likos et al. 2007; Gao et al. 2010). Additionally, viruses can also be detected in human fecal specimens (Gao et al. 2010). Limited studies have shown that systemic spread of the virus may exacerbate disease progression, with megatrophils potentially playing an important role (Gao et al. 2010; Schrauwen et al. 2012). Similar to HPAI H5N1 viruses, LPAI H7N9 viruses can infect type II alveolar epithelial cells and replicate in them effectively, which may further damage lung function (van Riel et al. 2013; Zhou et al. 2013). Compared with LPAI H7N9 viruses, which mainly replicate in respiratory tissues, HPAI H7N9 viruses can spread systemically in infected ferrets (Zhu et al. 2015; Imai et al. 2017; Shi et al. 2017). These latter viruses could infect and replicate efficiently in brain tissue, thus causing the death of the ferrets.
Host Genes
Interferon-induced transmembrane protein 3 (IFITM3) genetic variants influence the severity of clinical symptoms. The effects of genetic variation in the IFITM3 gene on influenza disease were first identified during the 2009 H1N1 pandemic (Everitt et al. 2012; Zhang et al. 2013d). This genetic variation was also associated with severe disease in some H7N9 patients (Wang et al. 2014b; Lee et al. 2017; Pan et al. 2017). Among H7N9 patients, the IFITM3 C/C genotype was associated with more severe clinical symptoms than the C/T and T/T genotypes (Wang et al., 2014b). Other host factors, including TMPRSS2, LGALS1, and CD55, were also reported to be associated with poor outcomes of H7N9 infections (Table 2) (Chen et al. 2015; Cheng et al. 2015; Lee et al. 2017).
Table 2.
Host genes associated with severe outcomes of H7N9 infections in humans
| Host gene | SNP | Animal studies | Reference(s) |
|---|---|---|---|
| IFITM 3 | rs12252/rs34481144 | + | Wang et al. 2014b; Lee et al. 2017; Pan et al. 2017 |
| TMRPSS2 | rs2070788/rs383510 | + | Cheng et al. 2015 |
| LGALS1 | rs4820294/rs2899292 haplotype GG | + | Chen et al. 2015 |
| CD55 | rs2564978 | − | Lee et al. 2017 |
(SNP) Single-nucleotide polymorphism, (+) validated in mouse models, (−) not validated in mouse models.
CONCLUDING REMARKS
Influenza is an acute respiratory disease caused by influenza viruses. It can cause serious public health concerns such as epidemics, zoonotic infections, and pandemics. Influenza pandemics are unpredictable but recurring events that can have profound consequences on human health and economic well-being worldwide. Risk assessment tools and pandemic preparedness plans are essential to help mitigate the impact of a pandemic. Recently, the United States Center for Disease Control and the World Health Organization have developed different risk assessment tools that can be used to assess the pandemic risk of influenza viruses with pandemic potential. Since 1997, AIVs of the H5 subtype have been considered zoonotic viruses with pandemic potential; fortunately, no such event has occurred to date. However, we cannot exclude the possibility of AIVs causing pandemics in future. These viruses may acquire the ability to transmit efficiently among humans, through mutations, reassortments, or both. Under the “One Health” approach, the global surveillance system for zoonotic influenza viruses should be further expanded in animals and humans, and epidemiologic investigations as well as virologic and pathogenesis research should be reinforced to provide essential scientific evidence for the risk assessment and early warning of a potential pandemic. Universal influenza vaccines and novel antiviral drugs may provide better protection against future pandemics.
ACKNOWLEDGMENTS
This study was supported by the National Nature Science Foundation of China (81961128002), the National Key Research and Development Program of China (2016YFD0500208), and the National Mega-projects for Infectious Diseases (2017ZX10104001002002).
This article has been made freely available online courtesy of TAUNS Laboratories.
Footnotes
Editors: Gabriele Neumann and Yoshihiro Kawaoka
Additional Perspectives on Influenza: The Cutting Edge available at www.perspectivesinmedicine.org
REFERENCES
- Alexander DJ, Brown IH. 2009. History of highly pathogenic avian influenza. Rev Sci Tech 28: 19–38. 10.20506/rst.28.1.1856 [DOI] [PubMed] [Google Scholar]
- Arzey GG, Kirkland PD, Arzey KE, Frost M, Maywood P, Conaty S, Hurt AC, Deng YM, Iannello P, Barr I, et al. 2012. Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg Infect Dis 18: 814–816. 10.3201/eid1805.111852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender C, Hall H, Huang J, Klimov A, Cox N, Hay A, Gregory V, Cameron K, Lim W, Subbarao K. 1999. Characterization of the surface proteins of influenza A (H5N1) viruses isolated from humans in 1997–1998. Virology 254: 115–123. 10.1006/viro.1998.9529 [DOI] [PubMed] [Google Scholar]
- Bosch FX, Garten W, Klenk HD, Rott R. 1981. Proteolytic cleavage of influenza virus hemagglutinins: primary structure of the connecting peptide between HA1 and HA2 determines proteolytic cleavability and pathogenicity of avian influenza viruses. Virology 113: 725–735. 10.1016/0042-6822(81)90201-4 [DOI] [PubMed] [Google Scholar]
- Chan LL, Bui CT, Mok CK, Ng MM, Nicholls JM, Peiris JS, Chan MC, Chan RW. 2016. Evaluation of the human adaptation of influenza A/H7N9 virus in PB2 protein using human and swine respiratory tract explant cultures. Sci Rep 6: 35401. 10.1038/srep35401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekaran A, Srinivasan A, Raman R, Viswanathan K, Raguram S, Tumpey TM, Sasisekharan V, Sasisekharan R. 2008. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat Biotechnol 26: 107–113. 10.1038/nbt1375 [DOI] [PubMed] [Google Scholar]
- Chen H, Bright RA, Subbarao K, Smith C, Cox NJ, Katz JM, Matsuoka Y. 2007. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Res 128: 159–163. 10.1016/j.virusres.2007.04.017 [DOI] [PubMed] [Google Scholar]
- Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. 2012. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology 422: 105–113. 10.1016/j.virol.2011.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Yuan H, Gao R, Zhang J, Wang D, Xiong Y, Fan G, Yang F, Li X, Zhou J, et al. 2014. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: descriptive study. Lancet 383: 714–721. 10.1016/S0140-6736(14)60111-2 [DOI] [PubMed] [Google Scholar]
- Chen Y, Zhou J, Cheng Z, Yang S, Chu H, Fan Y, Li C, Wong BH, Zheng S, Zhu Y, et al. 2015. Functional variants regulating LGALS1 (Galectin 1) expression affect human susceptibility to influenza A(H7N9). Sci Rep 5: 8517. 10.1038/srep08517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Z, Zhou J, To KK, Chu H, Li C, Wang D, Yang D, Zheng S, Hao K, Bosse Y, et al. 2015. Identification of TMPRSS2 as a susceptibility gene for severe 2009 pandemic A(H1N1) influenza and A(H7N9) influenza. J Infect Dis 212: 1214–1221. 10.1093/infdis/jiv246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chutinimitkul S, Bhattarakosol P, Srisuratanon S, Eiamudomkan A, Kongsomboon K, Damrongwatanapokin S, Chaisingh A, Suwannakarn K, Chieochansin T, Theamboonlers A, et al. 2006. H5N1 influenza A virus and infected human plasma. Emerg Infect Dis 12: 1041–1043. 10.3201/eid1206.060227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chutinimitkul S, van Riel D, Munster VJ, van den Brand JM, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA, de Wit E. 2010. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J Virol 84: 6825–6833. 10.1128/JVI.02737-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claas EC, Osterhaus AD, van Beek R, De Jong JC, Rimmelzwaan GF, Senne DA, Krauss S, Shortridge KF, Webster RG. 1998. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351: 472–477. 10.1016/S0140-6736(97)11212-0 [DOI] [PubMed] [Google Scholar]
- Connor RJ, Kawaoka Y, Webster RG, Paulson JC. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205: 17–23. 10.1006/viro.1994.1615 [DOI] [PubMed] [Google Scholar]
- Cowling BJ, Freeman G, Wong JY, Wu P, Liao Q, Lau EH, Wu JT, Fielding R, Leung GM. 2013a. Preliminary inferences on the age-specific seriousness of human disease caused by avian influenza A(H7N9) infections in China, March to April 2013. Euro Surveill 18: 20475. [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Jin L, Lau EH, Liao Q, Wu P, Jiang H, Tsang TK, Zheng J, Fang VJ, Chang Z, et al. 2013b. Comparative epidemiology of human infections with avian influenza A H7N9 and H5N1 viruses in China: a population-based study of laboratory-confirmed cases. Lancet 382: 129–137. 10.1016/S0140-6736(13)61171-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui L, Liu D, Shi W, Pan J, Qi X, Li X, Guo X, Zhou M, Li W, Li J, et al. 2014. Dynamic reassortments and genetic heterogeneity of the human-infecting influenza A (H7N9) virus. Nat Commun 5: 3142. 10.1038/ncomms4142 [DOI] [PubMed] [Google Scholar]
- Dankar SK, Wang S, Ping J, Forbes NE, Keleta L, Li Y, Brown EG. 2011. Influenza A virus NS1 gene mutations F103L and M106I increase replication and virulence. Virol J 8: 13. 10.1186/1743-422X-8-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, et al. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med 12: 1203–1207. 10.1038/nm1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y, Li C, Han J, Wen Y, Wang J, Hong W, Li X, Liu Z, Ye Q, Li J, et al. 2017. Phylogenetic and genetic characterization of a 2017 clinical isolate of H7N9 virus in Guangzhou, China during the fifth epidemic wave. Sci China Life Sci 60: 1331–1339. 10.1007/s11427-017-9152-1 [DOI] [PubMed] [Google Scholar]
- de Vries RP, Peng W, Grant OC, Thompson AJ, Zhu X, Bouwman KM, de la Pena ATT, van Breemen MJ, Ambepitiya Wickramasinghe IN, de Haan CAM, et al. 2017a. Three mutations switch H7N9 influenza to human-type receptor specificity. PLoS Pathog 13: e1006390. 10.1371/journal.ppat.1006390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries RP, Tzarum N, Peng W, Thompson AJ, Ambepitiya Wickramasinghe IN, de la Pena ATT, van Breemen MJ, Bouwman KM, Zhu X, McBride R, et al. 2017b. A single mutation in Taiwanese H6N1 influenza hemagglutinin switches binding to human-type receptors. EMBO Mol Med 9: 1314–1325. 10.15252/emmm.201707726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelan NR, Basler CF, García-Sastre A. 2003. A recombinant influenza A virus expressing an RNA-binding-defective NS1 protein induces high levels of β interferon and is attenuated in mice. J Virol 77: 13257–13266. 10.1128/JVI.77.24.13257-13266.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt AR, Clare S, Pertel T, John SP, Wash RS, Smith SE, Chin CR, Feeley EM, Sims JS, Adams DJ, et al. 2012. IFITM3 restricts the morbidity and mortality associated with influenza. Nature 484: 519–523. 10.1038/nature10921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonville JM, Burke DF, Lewis NS, Katzelnick LC, Russell CA. 2013. Quantifying the fitness advantage of polymerase substitutions in Influenza A/H7N9 viruses during adaptation to humans. PLoS ONE 8: e76047. 10.1371/journal.pone.0076047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, Kuiken T, Rimmelzwaan GF, Schutten M, Van Doornum GJ, et al. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci 101: 1356–1361. 10.1073/pnas.0308352100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344: 432–438. 10.1016/j.virol.2005.08.035 [DOI] [PubMed] [Google Scholar]
- Gao R, Dong L, Dong J, Wen L, Zhang Y, Yu H, Feng Z, Chen M, Tan Y, Mo Z, et al. 2010. A systematic molecular pathology study of a laboratory confirmed H5N1 human case. PLoS ONE 5: e13315. 10.1371/journal.pone.0013315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao HN, Lu HZ, Cao B, Du B, Shang H, Gan JH, Lu SH, Yang YD, Fang Q, Shen YZ, et al. 2013a. Clinical findings in 111 cases of influenza A (H7N9) virus infection. N Engl J Med 368: 2277–2285. 10.1056/NEJMoa1305584 [DOI] [PubMed] [Google Scholar]
- Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, et al. 2013b. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 368: 1888–1897. 10.1056/NEJMoa1304459 [DOI] [PubMed] [Google Scholar]
- Gao S, Kang Y, Yuan R, Ma H, Xiang B, Wang Z, Dai X, Wang F, Xiao J, Liao M, et al. 2017. Immune responses of chickens infected with wild bird-origin H5N6 avian influenza virus. Front Microbiol 8: 1081. 10.3389/fmicb.2017.01081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garten W, Klenk HD. 1999. Understanding influenza virus pathogenicity. Trends Microbiol 7: 99–100. 10.1016/S0966-842X(99)01460-2 [DOI] [PubMed] [Google Scholar]
- Gostic KM, Ambrose M, Worobey M, Lloyd-Smith JO. 2016. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science 354: 722–726. 10.1126/science.aag1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Li J, Cheng X. 1999. [Discovery of men infected by avian influenza A (H9N2) virus]. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 13: 105–108. [PubMed] [Google Scholar]
- Guo J, Huang F, Liu J, Chen Y, Wang W, Cao B, Zou Z, Liu S, Pan J, Bao C, et al. 2015. The serum profile of hypercytokinemia factors identified in H7N9-infected patients can predict fatal outcomes. Sci Rep 5: 10942. 10.1038/srep10942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, de Vries E, McBride R, Dekkers J, Peng W, Bouwman KM, Nycholat C, Verheije MH, Paulson JC, van Kuppeveld FJ, et al. 2017. Highly pathogenic influenza A(H5Nx) viruses with altered H5 receptor-binding specificity. Emerg Infect Dis 23: 220–231. 10.3201/eid2302.161072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale BG, Randall RE, Ortin J, Jackson D. 2008. The multifunctional NS1 protein of influenza A viruses. J Gen Virol 89: 2359–2376. 10.1099/vir.0.2008/004606-0 [DOI] [PubMed] [Google Scholar]
- Han J, Jin M, Zhang P, Liu J, Wang L, Wen D, Wu X, Liu G, Zou Y, Lv X, et al. 2013. Epidemiological link between exposure to poultry and all influenza A(H7N9) confirmed cases in Huzhou city, China, March to May 2013. Euro Surveill 18: 20481. [PubMed] [Google Scholar]
- Harvey R, Martin AC, Zambon M, Barclay WS. 2004. Restrictions to the adaptation of influenza a virus H5 hemagglutinin to the human host. J Virol 78: 502–507. 10.1128/JVI.78.1.502-507.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatta M, Gao P, Halfmann P, Kawaoka Y. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293: 1840–1842. 10.1126/science.1062882 [DOI] [PubMed] [Google Scholar]
- Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, et al. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336: 1534–1541. 10.1126/science.1213362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herfst S, Imai M, Kawaoka Y, Fouchier RA. 2014. Avian Influenza virus transmission to mammals. Curr Top Microbiol Immunol 385: 137–155. [DOI] [PubMed] [Google Scholar]
- Hirst M, Astell CR, Griffith M, Coughlin SM, Moksa M, Zeng T, Smailus DE, Holt RA, Jones S, Marra MA, et al. 2004. Novel avian influenza H7N3 strain outbreak, British Columbia. Emerg Infect Dis 10: 2192–2195. 10.3201/eid1012.040743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, et al. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486: 420–428. 10.1038/nature10831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Kiso M, Nakajima N, Yamayoshi S, Iwatsuki-Horimoto K, Hatta M, Yamada S, Ito M, Sakai-Tagawa Y, et al. 2017. A highly pathogenic avian H7N9 influenza virus isolated from a human is lethal in some ferrets infected via respiratory droplets. Cell Host Microbe 22: 615–626 e8. 10.1016/j.chom.2017.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ke C, Mok CKP, Zhu W, Zhou H, He J, Guan W, Wu J, Song W, Wang D, Liu J, et al. 2017. Human infection with highly pathogenic avian influenza A(H7N9) virus, China. Emerg Infect Dis 23: 1332–1340. 10.3201/eid2308.170600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klenk HD, Garten W. 1994. Host cell proteases controlling virus pathogenicity. Trends Microbiol 2: 39–43. 10.1016/0966-842X(94)90123-6 [DOI] [PubMed] [Google Scholar]
- Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, Meijer A, van Steenbergen J, Fouchier R, Osterhaus A, et al. 2004. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363: 587–593. 10.1016/S0140-6736(04)15589-X [DOI] [PubMed] [Google Scholar]
- Lam TT, Zhou B, Wang J, Chai Y, Shen Y, Chen X, Ma C, Hong W, Chen Y, Zhang Y, et al. 2015. Dissemination, divergence and establishment of H7N9 influenza viruses in China. Nature 522: 102–105. 10.1038/nature14348 [DOI] [PubMed] [Google Scholar]
- Lee N, Cao B, Ke C, Lu H, Hu Y, Tam CHT, Ma RCW, Guan D, Zhu Z, Li H, et al. 2017. IFITM3, TLR3, and CD55 gene SNPs and cumulative genetic risks for severe outcomes in Chinese patients with H7N9/H1N1pdm09 influenza. J Infect Dis 216: 97–104. 10.1093/infdis/jix235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Tian B, Jianfang Z, Yongkun C, Xiaodan L, Wenfei Z, Yan L, Jing T, Junfeng G, Tao C, et al. 2017. A comprehensive retrospective study of the seroprevalence of H9N2 avian influenza viruses in occupationally exposed populations in China. PLoS ONE 12: e0178328. 10.1371/journal.pone.0178328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Likos AM, Kelvin DJ, Cameron CM, Rowe T, Kuehnert MJ, Norris PJ, National Heart Lung Blood Institute Retrovirus Epidemiology Donor Study-II (REDS-II) 2007. Influenza viremia and the potential for blood-borne transmission. Transfusion 47: 1080–1088. 10.1111/j.1537-2995.2007.01264.x [DOI] [PubMed] [Google Scholar]
- Linster M, van Boheemen S, de Graaf M, Schrauwen EJA, Lexmond P, Mänz B, Bestebroer TM, Baumann J, van Riel D, Rimmelzwaan GF, et al. 2014. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell 157: 329–339. 10.1016/j.cell.2014.02.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Shi W, Shi Y, Wang D, Xiao H, Li W, Bi Y, Wu Y, Li X, Yan J, et al. 2013. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses. Lancet 381: 1926–1932. 10.1016/S0140-6736(13)60938-1 [DOI] [PubMed] [Google Scholar]
- Lu CY, Lu JH, Chen WQ, Jiang LF, Tan BY, Ling WH, Zheng BJ, Sui HY. 2008. Potential infections of H5N1 and H9N2 avian influenza do exist in Guangdong populations of China. Chin Med J (Engl) 121: 2050–2053. 10.1097/00029330-200810020-00020 [DOI] [PubMed] [Google Scholar]
- Lu S, Zheng Y, Li T, Hu Y, Liu X, Xi X, Chen Q, Wang Q, Cao Y, Wang Y, et al. 2013. Clinical findings for early human cases of influenza A(H7N9) virus infection, Shanghai, China. Emerg Infect Dis 19: 1142–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines TR, Lu XH, Erb SM, Edwards L, Guarner J, Greer PW, Nguyen DC, Szretter KJ, Chen LM, Thawatsupha P, et al. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol 79: 11788–11800. 10.1128/JVI.79.18.11788-11800.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manz B, Matrosovich M, Bovin N, Schwemmle M. 2010. A polymorphism in the hemagglutinin of the human isolate of a highly pathogenic H5N1 influenza virus determines organ tropism in mice. J Virol 84: 8316–8321. 10.1128/JVI.00850-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mänz B, Brunotte L, Reuther P, Schwemmle M. 2012. Adaptive mutations in NEP compensate for defective H5N1 RNA replication in cultured human cells. Nat Commun 3: 802. 10.1038/ncomms1804 [DOI] [PubMed] [Google Scholar]
- Manz B, Schwemmle M, Brunotte L. 2013. Adaptation of avian influenza A virus polymerase in mammals to overcome the host species barrier. J Virol 87: 7200–7209. 10.1128/JVI.00980-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok CK, Lee HH, Lestra M, Nicholls JM, Chan MC, Sia SF, Zhu H, Poon LL, Guan Y, Peiris JS. 2014. Amino acid substitutions in polymerase basic protein 2 gene contribute to the pathogenicity of the novel A/H7N9 influenza virus in mammalian hosts. J Virol 88: 3568–3576. 10.1128/JVI.02740-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster VJ, de Wit E, van Riel D, Beyer WE, Rimmelzwaan GF, Osterhaus AD, Kuiken T, Fouchier RA. 2007. The molecular basis of the pathogenicity of the Dutch highly pathogenic human influenza A H7N7 viruses. J Infect Dis 196: 258–265. 10.1086/518792 [DOI] [PubMed] [Google Scholar]
- Nidom CA, Takano R, Yamada S, Sakai-Tagawa Y, Daulay S, Aswadi D, Suzuki T, Suzuki Y, Shinya K, Iwatsuki-Horimoto K, et al. 2010. Influenza A (H5N1) viruses from pigs, Indonesia. Emerg Infect Dis 16: 1515–1523. 10.3201/eid1610.100508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen SJ, Ungchusak K, Sovann L, Uyeki TM, Dowell SF, Cox NJ, Aldis W, Chunsuttiwat S. 2005. Family clustering of avian influenza A (H5N1). Emerg Infect Dis 11: 1799–1801. 10.3201/eid1111.050646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization PAH. 2004. Avian influenza virus A (H10N7) circulating among humans in Egypt. https://www.paho.org/hq/index.php?option=com_docman&view=download&alias=8363-avian-influenza-virus-a-h10n7-circulating-among-humans-egypt-vol-2-no-18-7-may-2004-363&category_slug=see-influenza-reports-by-year-4302&Itemid=270&lang=en
- Pan M, Gao R, Lv Q, Huang S, Zhou Z, Yang L, Li X, Zhao X, Zou X, Tong W, et al. 2016. Human infection with a novel, highly pathogenic avian influenza A (H5N6) virus: virological and clinical findings. J Infect 72: 52–59. 10.1016/j.jinf.2015.06.009 [DOI] [PubMed] [Google Scholar]
- Pan Y, Yang P, Dong T, Zhang Y, Shi W, Peng X, Cui S, Zhang D, Lu G, Liu Y, et al. 2017. IFITM3 Rs12252-C variant increases potential risk for severe influenza virus infection in Chinese population. Front Cell Infect Microbiol 7: 294. 10.3389/fcimb.2017.00294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawar SD, Tandale BV, Raut CG, Parkhi SS, Barde TD, Gurav YK, Kode SS, Mishra AC. 2012. Avian influenza H9N2 seroprevalence among poultry workers in Pune, India, 2010. PLoS ONE 7: e36374. 10.1371/journal.pone.0036374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. 1999. Human infection with influenza H9N2. Lancet 354: 916–917. 10.1016/S0140-6736(99)03311-5 [DOI] [PubMed] [Google Scholar]
- Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, Ng TK, Chan KH, Lai ST, Lim WL, et al. 2004. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 363: 617–619. 10.1016/S0140-6736(04)15595-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris JS, de Jong MD, Guan Y. 2007. Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev 20: 243–267. 10.1128/CMR.00037-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi L, Davis AS, Jagger BW, Schwartzman LM, Dunham EJ, Kash JC, Taubenberger JK. 2012. Analysis by single-gene reassortment demonstrates that the 1918 influenza virus is functionally compatible with a low-pathogenicity avian influenza virus in mice. J Virol 86: 9211–9220. 10.1128/JVI.00887-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin Y, Horby PW, Tsang TK, Chen E, Gao L, Ou J, Nguyen TH, Duong TN, Gasimov V, Feng L, et al. 2015. Differences in the epidemiology of human cases of avian influenza A(H7N9) and A(H5N1) viruses infection. Clin Infect Dis 61: 563–571. 10.1093/cid/civ345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Z, Ma S, Kong H, Deng G, Shi J, Liu L, Suzuki Y, Chen H. 2017. Identification of a key amino acid in hemagglutinin that increases human-type receptor binding and transmission of an H6N2 avian influenza virus. Microbes Infect 19: 655–660. 10.1016/j.micinf.2017.09.008 [DOI] [PubMed] [Google Scholar]
- Rajsbaum R, Albrecht RA, Wang MK, Maharaj NP, Versteeg GA, Nistal-Villan E, García-Sastre A, Gack MU. 2012. Species-specific inhibition of RIG-I ubiquitination and IFN induction by the influenza A virus NS1 protein. PLoS Pathog 8: e1003059. 10.1371/journal.ppat.1003059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuther P, Giese S, Gotz V, Kilb N, Manz B, Brunotte L, Schwemmle M. 2014. Adaptive mutations in the nuclear export protein of human-derived H5N1 strains facilitate a polymerase activity-enhancing conformation. J Virol 88: 263–271. 10.1128/JVI.01495-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard M, Schrauwen EJ, de Graaf M, Bestebroer TM, Spronken MI, van Boheemen S, de Meulder D, Lexmond P, Linster M, Herfst S, et al. 2013. Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature 501: 560–563. 10.1038/nature12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivers C, Lum K, Lewis B, Eubank S. 2013. Estimating human cases of avian influenza A(H7N9) from poultry exposure. PLoS Curr 5. pii: ecurrents.outbreaks.264e737b489bef383fbcbaba260daf928. 10.1371/currents.outbreaks.264e737b489bef383fbcbaba60daf928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell CA, Fonville JM, Brown AE, Burke DF, Smith DL, James SL, Herfst S, van Boheemen S, Linster M, Schrauwen EJ, et al. 2012. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336: 1541–1547. 10.1126/science.1222526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrauwen EJ, Herfst S, Leijten LM, van Run P, Bestebroer TM, Linster M, Bodewes R, Kreijtz JH, Rimmelzwaan GF, Osterhaus AD, et al. 2012. The multibasic cleavage site in H5N1 virus is critical for systemic spread along the olfactory and hematogenous routes in ferrets. J Virol 86: 3975–3984. 10.1128/JVI.06828-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Zhang W, Wang F, Qi J, Wu Y, Song H, Gao F, Bi Y, Zhang Y, Fan Z, et al. 2013a. Structures and receptor binding of hemagglutinins from human-infecting H7N9 influenza viruses. Science 342: 243–247. 10.1126/science.1242917 [DOI] [PubMed] [Google Scholar]
- Shi J, Deng G, Liu P, Zhou J, Guan L, Li W, Li X, Guo J, Wang G, Fan J, et al. 2013b. Isolation and characterization of H7N9 viruses from live poultry markets—implication of the source of current H7N9 infection in humans. Chinese Sci Bull 58: 1857–1863. 10.1007/s11434-013-5873-4. [DOI] [Google Scholar]
- Shi J, Deng G, Kong H, Gu C, Ma S, Yin X, Zeng X, Cui P, Chen Y, Yang H, et al. 2017. H7N9 virulent mutants detected in chickens in China pose an increased threat to humans. Cell Res 27: 1409–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinde PV, Koratkar SS, Pawar SD, Kale SD, Rawankar AS, Mishra AC. 2012. Serologic evidence of avian influenza H9N2 and paramyxovirus type 1 infection in emus (Dromaius novaehollandiae) in India. Avian Dis 56: 257–260. 10.1637/9878-080511-Case.1 [DOI] [PubMed] [Google Scholar]
- Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440: 435–436. 10.1038/440435a [DOI] [PubMed] [Google Scholar]
- Shinya K, Makino A, Hatta M, Watanabe S, Kim JH, Kawaoka Y. 2010. A mutation in H5 haemagglutinin that conferred human receptor recognition is not maintained stably during duck passage. J Gen Virol 91: 1461–1463. 10.1099/vir.0.018572-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Makino A, Hatta M, Watanabe S, Kim JH, Hatta Y, Gao P, Ozawa M, Le QM, Kawaoka Y. 2011. Subclinical brain injury caused by H5N1 influenza virus infection. J Virol 85: 5202–5207. 10.1128/JVI.00239-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortridge KF. 1992. Pandemic influenza: a zoonosis? Semin Respir Infect 7: 11–25. [PubMed] [Google Scholar]
- Shu Y, Yu H, Li D. 2006. Lethal avian influenza A (H5N1) infection in a pregnant woman in Anhui Province, China. N Engl J Med 354: 1421–1422. 10.1056/NEJMc053524 [DOI] [PubMed] [Google Scholar]
- Srinivasan K, Raman R, Jayaraman A, Viswanathan K, Sasisekharan R. 2013. Quantitative description of glycan-receptor binding of influenza A virus H7 hemagglutinin. PLoS One 8: e49597. 10.1371/journal.pone.0049597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312: 404–410. 10.1126/science.1124513 [DOI] [PubMed] [Google Scholar]
- Subbarao K, Klimov A, Katz J, Regnery H, Lim W, Hall H, Perdue M, Swayne D, Bender C, Huang J, et al. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279: 393–396. 10.1126/science.279.5349.393 [DOI] [PubMed] [Google Scholar]
- Suguitan AL Jr, Matsuoka Y, Lau YF, Santos CP, Vogel L, Cheng LI, Orandle M, Subbarao K. 2012. The multibasic cleavage site of the hemagglutinin of highly pathogenic A/Vietnam/1203/2004 (H5N1) avian influenza virus acts as a virulence factor in a host-specific manner in mammals. J Virol 86: 2706–2714. 10.1128/JVI.05546-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka H, Park CH, Ninomiya A, Ozaki H, Takada A, Umemura T, Kida H. 2003. Neurotropism of the 1997 Hong Kong H5N1 influenza virus in mice. Vet Microbiol 95: 1–13. 10.1016/S0378-1135(03)00132-9 [DOI] [PubMed] [Google Scholar]
- Tharakaraman K, Jayaraman A, Raman R, Viswanathan K, Stebbins NW, Johnson D, Shriver Z, Sasisekharan V, Sasisekharan R. 2013. Glycan receptor binding of the influenza A virus H7N9 hemagglutinin. Cell 153: 1486–1493. 10.1016/j.cell.2013.05.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- To KK, Chan JF, Chen H, Li L, Yuen KY. 2013. The emergence of influenza A H7N9 in human beings 16 years after influenza A H5N1: a tale of two cities. Lancet Infect Dis 13: 809–821. 10.1016/S1473-3099(13)70167-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong XC, Weng SS, Xue F, Wu X, Xu TM, Zhang WH. 2018. First human infection by a novel avian influenza A(H7N4) virus. J Infect 77: 249–257. 10.1016/j.jinf.2018.06.002 [DOI] [PubMed] [Google Scholar]
- Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, Li Y, Katz J, Krajden M, Tellier R, et al. 2004. Human illness from avian influenza H7N3, British Columbia. Emerg Infect Dis 10: 2196–2199. 10.3201/eid1012.040961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uyeki TM. 2009. Human infection with highly pathogenic avian influenza A (H5N1) virus: review of clinical issues. Clin Infect Dis 49: 279–290. 10.1086/600035 [DOI] [PubMed] [Google Scholar]
- van Kolfschooten F. 2003. Dutch veterinarian becomes first victim of avian influenza. Lancet 361: 1444. 10.1016/S0140-6736(03)13156-X [DOI] [PubMed] [Google Scholar]
- van Riel D, Leijten LM, de Graaf M, Siegers JY, Short KR, Spronken MI, Schrauwen EJ, Fouchier RA, Osterhaus AD, Kuiken T. 2013. Novel avian-origin influenza A (H7N9) virus attaches to epithelium in both upper and lower respiratory tract of humans. Am J Pathol 183: 1137–1143. 10.1016/j.ajpath.2013.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan H, Sorrell EM, Song H, Hossain MJ, Ramirez-Nieto G, Monne I, Stevens J, Cattoli G, Capua I, Chen LM, et al. 2008. Replication and transmission of H9N2 influenza viruses in ferrets: evaluation of pandemic potential. PLoS ONE 3: e2923. 10.1371/journal.pone.0002923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan XF, Dong L, Lan Y, Long LP, Xu C, Zou S, Li Z, Wen L, Cai Z, Wang W, et al. 2011. Indications that live poultry markets are a major source of human H5N1 influenza virus infection in China. J Virol 85: 13432–13438. 10.1128/JVI.05266-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Lu B, Zhou H, Suguitan AL Jr, Cheng X, Subbarao K, Kemble G, Jin H. 2010. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J Virol 84: 6570–6577. 10.1128/JVI.00221-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Yang L, Gao R, Zhang X, Tan Y, Wu A, Zhu W, Zhou J, Zou S, Li X, et al. 2014a. Genetic tuning of the novel avian influenza A(H7N9) virus during interspecies transmission, China, 2013. Euro Surveill 19: 20836. 10.2807/1560-7917.ES2014.19.25.20836 [DOI] [PubMed] [Google Scholar]
- Wang Z, Zhang A, Wan Y, Liu X, Qiu C, Xi X, Ren Y, Wang J, Dong Y, Bao M, et al. 2014b. Early hypercytokinemia is associated with interferon-induced transmembrane protein-3 dysfunction and predictive of fatal H7N9 infection. Proc Natl Acad Sci 111: 769–774. 10.1073/pnas.1321748111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Yang L, Zhu W, Zhang Y, Zou S, Bo H, Gao R, Dong J, Huang W, Guo J, et al. 2016. Two outbreak sources of influenza A (H7N9) viruses have been established in China. J Virol 90: 5561–5573. 10.1128/JVI.03173-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Jiang H, Wu P, Uyeki TM, Feng L, Lai S, Wang L, Huo X, Xu K, Chen E, et al. 2017. Epidemiology of avian influenza A H7N9 virus in human beings across five epidemics in mainland China, 2013–17: an epidemiological study of laboratory-confirmed case series. Lancet Infect Dis 17: 822–832. 10.1016/S1473-3099(17)30323-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe Y, Ibrahim MS, Ellakany HF, Kawashita N, Mizuike R, Hiramatsu H, Sriwilaijaroen N, Takagi T, Suzuki Y, Ikuta K. 2011. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog 7: e1002068. 10.1371/journal.ppat.1002068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, et al. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501: 551–555. 10.1038/nature12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster RG, Rott R. 1987. Influenza virus A pathogenicity: the pivotal role of hemagglutinin. Cell 50: 665–666. 10.1016/0092-8674(87)90321-7 [DOI] [PubMed] [Google Scholar]
- Wei SH, Yang JR, Wu HS, Chang MC, Lin JS, Lin CY, Liu YL, Lo YC, Yang CH, Chuang JH, et al. 2013. Human infection with avian influenza A H6N1 virus: an epidemiological analysis. Lancet Respir Med 1: 771–778. 10.1016/S2213-2600(13)70221-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo JT, Park BK. 2008. Seroprevalence of low pathogenic avian influenza (H9N2) and associated risk factors in the Gyeonggi-do of Korea during 2005–2006. J Vet Sci 9: 161–168. 10.4142/jvs.2008.9.2.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu A, Su C, Wang D, Peng Y, Liu M, Hua S, Li T, Gao GF, Tang H, Chen J, et al. 2013. Sequential reassortments underlie diverse influenza H7N9 genotypes in China. Cell Host Microbe 14: 446–452. 10.1016/j.chom.2013.09.001 [DOI] [PubMed] [Google Scholar]
- Xiong X, Martin SR, Haire LF, Wharton SA, Daniels RS, Bennett MS, McCauley JW, Collins PJ, Walker PA, Skehel JJ, et al. 2013. Receptor binding by an H7N9 influenza virus from humans. Nature 499: 496–499. 10.1038/nature12372 [DOI] [PubMed] [Google Scholar]
- Xu C, Hu WB, Xu K, He YX, Wang TY, Chen Z, Li TX, Liu JH, Buchy P, Sun B. 2012. Amino acids 473V and 598P of PB1 from an avian-origin influenza A virus contribute to polymerase activity, especially in mammalian cells. J Gen Virol 93: 531–540. 10.1099/vir.0.036434-0 [DOI] [PubMed] [Google Scholar]
- Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, Muramoto Y, Ito M, Kiso M, Horimoto T, et al. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444: 378–382. 10.1038/nature05264 [DOI] [PubMed] [Google Scholar]
- Yang JR, Liu MT. 2017. Human infection caused by an avian influenza A (H7N9) virus with a polybasic cleavage site in Taiwan, 2017. J Formos Med Assoc 116: 210–212. 10.1016/j.jfma.2017.02.011 [DOI] [PubMed] [Google Scholar]
- Yang H, Chen LM, Carney PJ, Donis RO, Stevens J. 2010. Structures of receptor complexes of a North American H7N2 influenza hemagglutinin with a loop deletion in the receptor binding site. PLoS Pathog 6: 1001081. 10.1371/journal.ppat.1001081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Zhu W, Li X, Bo H, Zhang Y, Zou S, Gao R, Dong J, Zhao X, Chen W, et al. 2016. Genesis and dissemination of highly pathogenic H5N6 avian influenza viruses. J Virol 91: e02199-02116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Zhu W, Li X, Chen M, Wu J, Yu P, Qi S, Huang Y, Shi W, Dong J, et al. 2017. Genesis and spread of newly emerged highly pathogenic H7N9 avian viruses in mainland China. J Virol 91: e01277-01217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H, Cowling BJ, Feng L, Lau EH, Liao Q, Tsang TK, Peng Z, Wu P, Liu F, Fang VJ, et al. 2013a. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet 382: 138–145. 10.1016/S0140-6736(13)61207-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Wang Z, Chen Y, Ding W, Jia H, Chan JF, To KK, Chen H, Yang Y, Liang W, et al. 2013b. Clinical, virological, and histopathological manifestations of fatal human infections by avian influenza A(H7N9) virus. Clin Infect Dis 57: 1449–1457. 10.1093/cid/cit541 [DOI] [PubMed] [Google Scholar]
- Yuen KY, Chan PK, Peiris M, Tsang DN, Que TL, Shortridge KF, Cheung PT, To WK, Ho ET, Sung R, et al. 1998. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351: 467–471. 10.1016/S0140-6736(98)01182-9 [DOI] [PubMed] [Google Scholar]
- Zhang Z, Hu S, Li Z, Wang X, Liu M, Guo Z, Li S, Xiao Y, Bi D, Jin H. 2011. Multiple amino acid substitutions involved in enhanced pathogenicity of LPAI H9N2 in mice. Infect Genet Evol 11: 1790–1797. 10.1016/j.meegid.2011.07.025 [DOI] [PubMed] [Google Scholar]
- Zhang L, Zhang Z, Weng Z. 2013a. Rapid reassortment of internal genes in avian influenza A(H7N9) virus. Clin Infect Dis 57: 1059–1061. 10.1093/cid/cit414 [DOI] [PubMed] [Google Scholar]
- Zhang Q, Shi J, Deng G, Guo J, Zeng X, He X, Kong H, Gu C, Li X, Liu J, et al. 2013b. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science 341: 410–414. 10.1126/science.1240532 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Zhang Q, Kong H, Jiang Y, Gao Y, Deng G, Shi J, Tian G, Liu L, Liu J, et al. 2013c. H5N1 hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science 340: 1459–1463. 10.1126/science.1229455 [DOI] [PubMed] [Google Scholar]
- Zhang YH, Zhao Y, Li N, Peng YC, Giannoulatou E, Jin RH, Yan HP, Wu H, Liu JH, Liu N, et al. 2013d. Interferon-induced transmembrane protein-3 genetic variant rs12252-C is associated with severe influenza in Chinese individuals. Nat Commun 4: 1418. 10.1038/ncomms2433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F, Bi Y, Wang J, Wong G, Shi W, Hu F, Yang Y, Yang L, Deng X, Jiang S, et al. 2017a. Human infections with recently-emerging highly pathogenic H7N9 avian influenza virus in China. J Infect 75: 71–75. 10.1016/j.jinf.2017.04.001 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Chen M, Huang Y, Zhu W, Yang L, Gao L, Li X, Bi F, Huang C, Kang N, et al. 2017b. Human infections with novel reassortant H5N6 avian influenza viruses in China. Emerg Microbes Infect 6: e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Wang D, Gao R, Zhao B, Song J, Qi X, Zhang Y, Shi Y, Yang L, Zhu W, et al. 2013. Biological features of novel avian influenza A (H7N9) virus. Nature 499: 500–503. 10.1038/nature12379 [DOI] [PubMed] [Google Scholar]
- Zhou P, Zhu W, Gu H, Fu X, Wang L, Zheng Y, He S, Ke C, Wang H, Yuan Z, et al. 2014. Avian influenza H9N2 seroprevalence among swine farm residents in China. J Med Virol 86: 597–600. 10.1002/jmv.23869 [DOI] [PubMed] [Google Scholar]
- Zhu W, Shu Y. 2015. Genetic tuning of avian influenza A (H7N9) virus promotes viral fitness within different species. Microbes Infect 17: 118–122. 10.1016/j.micinf.2014.11.010 [DOI] [PubMed] [Google Scholar]
- Zhu H, Wang D, Kelvin DJ, Li L, Zheng Z, Yoon SW, Wong SS, Farooqui A, Wang J, Banner D, et al. 2013. Infectivity, transmission, and pathology of human-isolated H7N9 influenza virus in ferrets and pigs. Science 341: 183–186. 10.1126/science.1239844 [DOI] [PubMed] [Google Scholar]
- Zhu W, Li L, Yan Z, Gan T, Li L, Chen R, Chen R, Zheng Z, Hong W, Wang J, et al. 2015. Dual E627 K and D701N mutations in the PB2 protein of A(H7N9) influenza virus increased its virulence in mammalian models. Sci Rep 5: 14170. 10.1038/srep14170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W, Zhou J, Li Z, Yang L, Li X, Huang W, Zou S, Chen W, Wei H, Tang J, et al. 2017. Biological characterisation of the emerged highly pathogenic avian influenza (HPAI) A(H7N9) viruses in humans, in mainland China, 2016 to 2017. Euro Surveill 22: 30533. 10.2807/1560-7917.ES.2017.22.19.30533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W, Dong J, Zhang Y, Yang L, Li X, Chen T, Zhao X, Wei H, Bo H, Zeng X, et al. 2018. A gene constellation in avian influenza A (H7N9) viruses may have facilitated the fifth wave outbreak in China. Cell Rep 23: 909–917. 10.1016/j.celrep.2018.03.081 [DOI] [PubMed] [Google Scholar]
- Zhu W, Feng Z, Chen Y, Yang L, Liu J, Li X, Liu S, Zhou L, Wei H, Gao R, et al. 2019. Mammalian-adaptive mutation NP-Q357K in Eurasian H1N1 swine influenza viruses determines the virulence phenotype in mice. Emerg Microbes Infect 8: 989–999. 10.1080/22221751.2019.1635873 [DOI] [PMC free article] [PubMed] [Google Scholar]