Abstract
The move towards universal health coverage is premised on having well-functioning health systems, which can assure provision of the essential health and related services people need. Efforts to define ways to assess functionality of health systems have however varied, with many not translating into concrete policy action and influence on system development. We present an approach to provide countries with information on the functionality of their systems in a manner that will facilitate movement towards universal health coverage. We conceptualise functionality of a health system as being a construct of four capacities: access to, quality of, demand for essential services and its resilience to external shocks. We test and confirm the validity of these capacities as appropriate measures of system functionality. We thus provide results for functionality of the 47 countries of the WHO African Region based on this. The functionality of health systems ranges from 34.4 to 75.8 on a 0–100 scale. Access to essential services represents the lowest capacity in most countries of the region, specifically due to poor physical access to services. Funding levels from public and out-of-pocket sources represent the strongest predictors of system functionality, compared with other sources. By focusing on the assessment on the capacities that define system functionality, each country has concrete information on where it needs to focus, in order to improve the functionality of its health system to enable it respond to current needs including achieving universal health coverage, while responding to shocks from challenges such as the 2019 coronavirus disease. This systematic and replicable approach for assessing health system functionality can provide the guidance needed for investing in country health systems to attain universal health coverage goals.
Keywords: health systems, health systems evaluation
Key questions.
What is already known?
Health system functionality is crucial for attainment of universal health coverage and other health-related goals.
There have been multiple efforts to assess health system functionality, which have not provided the expected guidance towards appropriate investment in the system.
Health systems are more complex than building blocks, with various inter-relations and soft elements influencing the outputs from health system investments.
What are the new findings?
Health system functionality can be viewed from the status of four capacities: access to essential services, quality of care, demand for essential services and resilience of the health system.
Health systems have a wide range of functionality within the region, which is not explained solely by income level, country size or population.
Access to essential services remains the rate-limiting capacity for system functionality in most countries of the region, due to low levels of physical access to services.
Public financing provides the biggest improvement in health system functioning compared with external and out-of-pocket financing. Out-of-pocket expenditure is negatively correlated with system functionality.
Key questions.
What do the new findings imply?
Decision makers can make investments targeted at specific capacities of the health system based on their functionality scores.
The poor performance of the capacity on access to essential services is of regional concern and must therefore not be neglected in health systems development efforts.
Introduction
The health systems resilience supplement in the BMJ Global Health 2019 explored different perspectives on how to build and sustain resilient health systems in the context of multiple sector needs.1 Since then, the health landscape has evolved, as a result of the COVID-19 pandemic, but also the increasing country demand for initiatives and measurement approaches for performance of health systems, in the context of the primary healthcare revitalisation agenda. Drawing from available evidence, this article concludes the supplement by proposing an approach for measuring the functionality of health systems needed to address current health needs and facilitate movement towards health goals, specifically universal health coverage (UHC).
Understanding health systems has been central to the health agenda over the past 20 years. The 2000 WHO World Health Report initiated conceptual work around describing health systems, proposing health system boundaries and cross-country comparisons.2 Lessons from this process led to the elaboration of the health systems building blocks in 2007 as a means to define and characterise health systems, together with their linkages to health goals and objectives.3 This approach has been used to assess health systems, though this has largely been in high-income countries,4–7 with fewer such initiatives in the developing world.8–11 Additionally, the uptake and use of results from these assessments by decision makers and their impact on system development has been limited.12 13
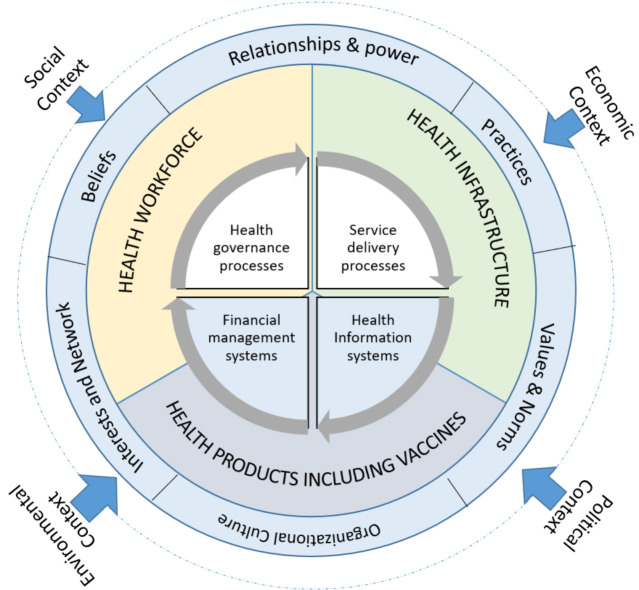
The building blocks conceptualisation however only tells part of the story of what a health system entails. As a result, further conceptual exploration has continued, specifically on how to incorporate the observed complexities of the health system, their structure and how they produce results.14 15 Sheikh et al16 proposed a conceptualisation that incorporates the role of software elements and the context in which a system operates, as important in describing what a health system entails. This conceptualisation highlights the need to focus on three sets of elements in a health system: the hardware: corresponding to the tangible (staff, infrastructure and medicines) and intangible systems and processes; the discreet elements: software corresponding to the intangible inter-related elements such as relationships, values and cultures; and the context: corresponding to the environment within which the system operates at a given place and time. The COVID-19 pandemic has, among other things, highlighted the importance of the contextual environment as an influence on health system functionality. Inhibitive social, environmental, economic and political environments have been shown to hinder the availability, functioning or use of the health system hardware and to influence the expression of the software. Figure 1 illustrates these different elements important in understanding a health system.
Figure 1.
Scope and relationships of health system elements.
An effective understanding of the functioning of a health system entails appreciation of the nature, depth and interactions among these complex and dynamic elements over time. The complex and adaptive characteristics of these elements and their interactions makes such an assessment complex and multifaceted. There are multiple correct ways to mix, match and interact the elements of a system to produce the desired outcomes. For instance, improving effective pentavalent vaccination coverage can be achieved by investing in different combinations of better staffing, expansion of infrastructure, expansion of service delivery processes, better management of vaccine logistics, among others. Singling out one intervention from these options will usually not lead to the desired result, as its effects may be undone by gaps in other elements. Multivariate analyses that explore different ways to invest in the system would thus be more appropriate. Despite the large data requirements for such an exercise, such an analysis will lead to multiple appropriate ways of mixing the elements to produce desired outcomes.
The difficulty of determining system functionality in a useful manner should not diminish its importance for decision making.17 In this paper, we present an approach for understanding the functionality of health systems that provide actionable information to decision makers.
Conceptual approach
Our conceptualisation of functionality focuses on how well a given health system is designed to deliver on expected results for the population. Instead of determining the state and interactions of the different elements constructing the system, we instead focus on understanding the capacities that a functional system needs to exhibit, irrespective of the investments and their interactions. By determining and monitoring these capacities, a decision maker is able to identify the appropriate mix and inter-relations of the system elements that will be optimal for improving functionality.
From a logical perspective, these capacities are viewed as the outputs of the investments made, at the input and process level, and can define attainment of desired outcomes. Though they already exist in literature, they have not been categorised as outputs. Originally, when the health system building blocks were introduced, three intermediate goals of a system were suggested: access to care including community engagement, quality of care, and coverage of services.18 We however view the goal of increased coverage as an outcome, arising from having access and quality capacities. Thus, when individuals, households and communities feel the need for and have access to quality services, then they will use these services, leading to increased coverage.19 Indeed, access and quality have been recognised as key capacities of a well-performing health system by many in academic discourse and policy spheres—access being concerned with the system’s capacity to overcome barriers to services, while quality of care is the process with which care is provided. In addition to these two capacities, the level of effective demand for essential services by a population is another potential capacity. The ongoing discourse on Primary Health Care (PHC) revitalisation demonstrates this, as it requires systems to put the needs and demands of people at the centre of their focus-shifting away from politically determined priorities.20–22 We therefore have identified three capacities important for determining the functionality of a health system: access to, quality of and demand for essential services. However, the capacity to sustain provision of these essential services is advocated for as an additional core capacity of a health system.23 24 The constant shocks health systems are subject to has brought the issue of service continuity to the fore.25 For example, 96 infectious disease outbreaks were documented in the region in 2018 alone,26 and the 2014 Ebola virus disease outbreak in West Africa and the COVID-19 pandemic have all highlighted the devastating effects of shocks on health systems’ ability to deliver essential services.27 The capacity to be resilient to external shocks, ensuring populations have access to quality services they have demanded, is therefore important for optimal functionality of any system.
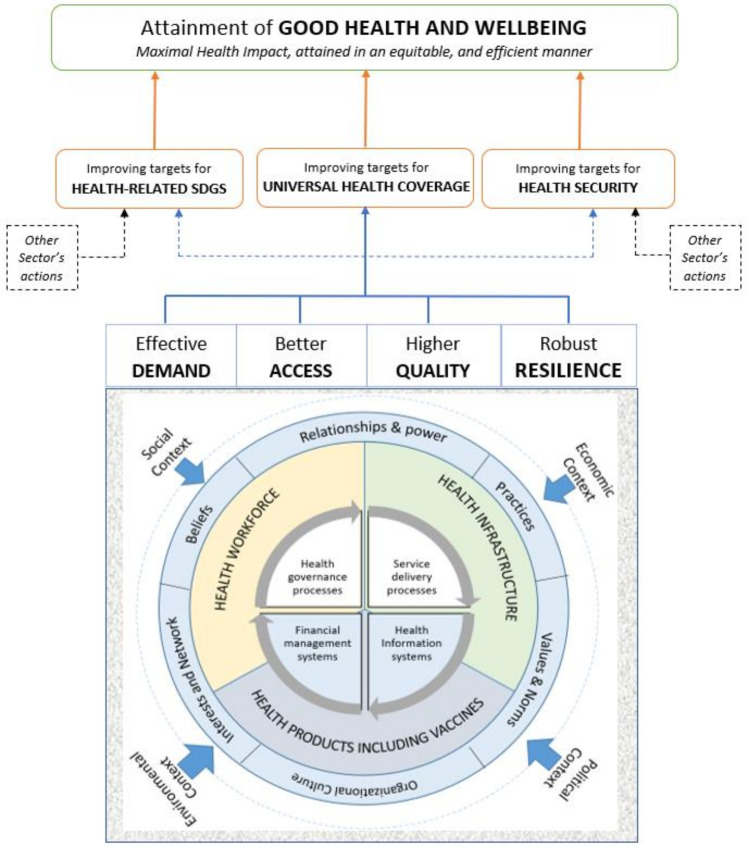
We therefore use, as a working definition, these four capacities as the basis of a functional health system that can deliver on its health outcomes. Irrespective of the unique way health systems are structured in a given country, they should aim to improve these four capacities, in order to place them on a path to achieving desired outcomes.28 A functional health system in this context is conceptualised as one that maximises the attainment of UHC in a country, but also contributes to better coverage of other health-related targets and health security. The functional health system contributes, together with interventions from other sectors, to the desired coverage of health-related Sustainable Development Goal (SDG) targets and health security. Subsequently, the realisation of desired coverage for UHC, health security and other health-related outcomes will place countries on the path to good health and well-being in an effective, efficient and equitable manner. These linkages are illustrated in figure 2.
Figure 2.
Conceptual approach linking system functionality with outcomes and impact.
This study aims to derive a value for each of the four capacities in each country of the WHO African Region as a reflection of its status. This would provide guidance on which capacities a decision maker needs to focus on—the lower the value, the higher the need to focus on it. For instance, a value showing low access to essential services compared with resilience points decision makers to the need to prioritise efforts for improving access. We opted to construct an index value for each capacity of health system functionality. This approach is widespread in global development, including in emergency preparedness and response,29 health security30 and essential health service coverage.19 It provides a practical way to demonstrate how the capacities of functionality compare to each other in a country and across peer countries.
We recognise the complex set of issues hidden behind each of the four capacities that would require a wide range of indicators to unpack. As such, we deconstruct each capacity into vital signs, representing a group of subcapacities that, taken together, constitute the overall capacities. Use of vital signs allows a more targeted group of indicators to be selected and monitored and also provides more granular information on where a country needs to focus within each capacity. The proposed vital signs are those used in the WHO Africa Regional Framework for health systems development towards attainment of UHC, following a 2-year (2016–2018) process of expert consultations involving the 47 countries of the region.31 32 Access to essential services comprises three vital signs: physical access, financial access and sociocultural access; quality of care comprises three vital signs: user experiences, patient safety and effectiveness of care. Demand for essential services comprises two vital signs: individual healthy actions and health-seeking behaviours. Finally, resilience comprises two vital signs: specific resilience (emergency preparedness and response capacity), and the non-specific resilience (inherent capacity of the health system); these are defined in more detail in a separate publication.33 34 The index for each capacity is computed based on the scores for the vital signs that constitute it.
We present the approach to test these capacities, as measures of system functionality, and the emerging results for the 47 countries of the WHO African Region.
Methods
Deriving the scores for each vital sign
Vital signs were constructed from indicators that relate to it. Multiple indicators were used for each vital sign to reduce the influence of a single indicator and ensure the score and resulting capacity index reflects the multiple actions that are needed to improve it. Given challenges in data availability across multiple indicators across 47 countries, proxy indicators were used, which were selected based on the following criteria: (1) it is thematically related to the vital sign; (2) there is country-level data for the indicator; and (3) the data are publicly available from a reputable source. The proxy indicators represent the closest data that exist, related to a specific vital sign and are shown in table 1.
Table 1.
Proxy indicators by capacity and vital sign for monitoring overall health system functionality
| Capacities | Vital signs | Proxy indicators |
| Access to essential services | Physical access | Number of medical (general and specialist) personnel (per 1000 population). |
| Number of nursing personnel (including midwives (per 1000 population)). | ||
| Number of public health facilities (per square kilometre). | ||
| Number of hospital beds (per 1000 population). | ||
| Financial access | Domestic general government health expenditure (% of current health expenditure). | |
| Domestic general government health expenditure (% of general government expenditure). | ||
| Out-of-pocket expenditure per capita, Purchasing Power Parity (PPP) (current international $). | ||
| Out-of-pocket expenditure (% of current health expenditure). | ||
| Incidence of catastrophic expenditure (%): at 10% of household total consumption or income. | ||
| Sociocultural access | Secondary school completion rate, female (% of relevant age group). | |
| Primary school completion rate, female (% of relevant age group). | ||
| Women’s labour force participation. | ||
| Intimate partner violence against women (%). | ||
| Quality of care in service provision | Individual healthy actions | Antenatal coverage (% receiving 4+ visits). |
| Community health workers density (per 1000 population). | ||
| Total alcohol consumption per capita (litres of pure alcohol), 15+ years of age. | ||
| Smoking prevalence, total (ages 15+ years). | ||
| Health-seeking behaviours | Antenatal Care (ANC) 1– 4 drop out. | |
| Diptheria, Pertusis, Tetanus (DP) containing vaccine, dose 1– 3 drop out. | ||
| DTP3-Measles Containing Vaccine (MCV) drop out. | ||
| Demand for family planning satisfied by modern methods. | ||
| Care seeking behaviour for child pneumonia. | ||
| Effective demand for essential services | User experiences | General service readiness (%). |
| Satisfaction with basic health services (%). | ||
| Patient safety | Standard precautions for infection prevention and control (%). | |
| Stillbirth rate (per 1000 total births). | ||
| Effectiveness of care | Tuberculosis treatment success rate (% of new cases). | |
| Mortality from Cardio Vascular Disease (CVD), cancer, diabetes or Chronic Respiratory Disease (CRD) between exact ages 30 and 70 years (%). | ||
| Suicide mortality rate (per 100 000 population). | ||
| Resilience to disruptive shock events | Specific resilience | Capacity for preparedness. |
| Capacity for detection. | ||
| Capacity for response. | ||
| Non-specific resilience | Awareness of system capacities and risks. | |
| Diversity of services and capacities. | ||
| Self-regulatory capacity for rapid decision making. | ||
| Local resource mobilisation capacity. | ||
| Transformation capacity. |
Data sources
For the indicators identified, a preference was given to data sources that provide primary data, including household surveys and facility assessments. Beyond these, indicator data were obtained from publicly available sources, including the WHO Health Observatory, the United Nations Sustainable Development Goals database and the World Bank World Development Indicators. The only vital sign with no data from these sources was on non-specific resilience, which was derived from health facility resilience assessments conducted during routine disease surveillance activities among countries in the region.33 The data used in this study represent the latest data values available for each country between 2010 and 2018 and are shared in online supplemental appendix S2. In instances where data points were absent for some countries, we implemented Multivariate Imputation by Chained Equations (MICE) using R software to impute for the missing data; the methodology works under the assumption that given the variables we used in the imputation procedure, the missing data are missing at random. This implies that the probability that a value is missing depends only on observed values and not on unobserved values.
bmjgh-2020-004618supp001.pdf (1.2MB, pdf)
We used a regression equation with the relationship that overall performance is explained by 34 proxy indicators. Based on this relationship, the missing variables were imputed using the predictive mean matching, a procedure implemented within the MICE package in R software.
Calculating the index
For each vital sign, a score was derived from the values of the proxy indicators in a stepwise manner. This involved: (1) normalisation of all the indicator values to a range of 0–100 to make them comparable; (2) centralisation of the indicator values for each vital sign into a score; (3) centralisation of the score values for each vital sign in a capacity to derive a capacity index; and (4) centralisation of the four capacity index values to derive the overall functionality index.
Normalisation of the indicators was done using the formula:
where Minimum and Maximum are the lowest and highest reported values, respectively.
This standardisation made the indicators comparable, with each country’s value ranging from 0 to 100, representing the worst and best country values for the indicator.
The score for each vital sign was derived as the arithmetic mean of the indicators constituting it. Similarly, the index for each capacity was derived as the arithmetic mean for each of the vital signs constituting it, with the overall system functionality index being the arithmetic mean of the four capacities constituting it. Finally, the regional values for each of the capacities and the overall index were calculated as the geometric mean of all country scores. We applied the same weighting at each stage to emphasise the importance of each indicator, vital sign and capacity, respectively. A differential weighting denotes an implicit ranking of importance, which is contrary to the assumption that they are all crucial for overall system functionality.
Construct validity
We make several structural and conceptual assumptions, whose validity we tested to improve confidence in the approach. Specifically, we explored whether: (1) the four capacities are appropriate predictors of desired health outcomes on their own; (2) the applied proxy indicators are appropriate predictors for the vital signs for each capacity; and (3) the emerging results are associated with predictors of functionality, such as efficiency, equity and/or effectiveness. We calculated Spearman’s rank correlation coefficients (rho) between the computed index and certain key indicators to test face validity. Correlations were interpreted in a standard manner as defined in literature: <0.35 low, 0.36–0.67 moderate and 0.68–1.0 as high.35 We explore both the magnitude and the relative strengths of correlations in ascertaining face validity, as well as our conceptual approach and methods. See online supplemental appendix S3 for details.
In ascertaining how appropriate the four capacities are in predicting desired health outcomes, we compared the emerging results with the UHC service coverage index, minus its service capacity and access component. This is constructed from multiple service coverage outcomes, providing an appropriate comparator for system functionality. We opted to focus our analysis of UHC solely on elements of service coverage, rather than financial risk protection, given the ongoing debate on the measurement challenges associated with current thresholds used in the calculation of the official SDG indicator on financial protection as a component of UHC.36–38 We removed the service capacity and access component as it is conceptually meant to measure the health system functionality component and thus may introduce predictable collinearity. We calculated values for spearman’s rho between the emerging functionality scores and the UHC index, postulating that a strong correlation would confer face validity of the emerging index as a good predictor of UHC attainment. We anticipate a reduced correlation between the emerging functionality index and health security/other health-related outcomes, as these require investments from other sectors whose magnitude varies in different countries and contexts.
Looking at the correlation between the emerging results and the impact level, we postulate that there is a strong significant correlation between a functioning health system and better impact based on improved health outcomes and systems efficiency. We postulate that the emerging correlation, while strong, should be weaker than that with the UHC service coverage index (minus service capacity and access component). We calculated values of Spearman’s rho between the emerging functionality index and maternal mortality ratio (MMR), under-5 (U5) mortality rate and neonatal mortality rate. We also examined its relationship with independently derived efficiency levels of health sectors.39 To advance this efficiency analysis, we also examined the relationship between the functionality index and funding by source. This was to better understand which funding sources are most effective at improving health system functionality for attainment of universal health coverage. We calculated Spearman’s rank correlation coefficients between the system functionality index and public, private, out-of-pocket and external sources of funding.
Sensitivity analysis
The emergent values are dependent on the decision of indicators, representativeness of data used, methodology for imputation of missing data points, index construction process (arithmetic vs geometric mean) and the methodology for standardisation of constituent indicators. Sensitivity analyses tests the robustness of the decisions relating to these variables.
We recalculated the index using the arithmetic mean for regional values, as opposed to the geometric mean. We also assessed the effect of switching the data normalisation methodology to using a standardised minimum value of zero as compared with using the least value as the zero value based on the formula:
In order to explore the appropriateness of the proxy indicators used to measure the respective vital signs and capacities, we drew on the work of Hogan et al40 to assess the sensitivity of the index to each indicator by assessing the impact on the value by dropping one indicator at a time. If a given indicator is not appropriate, its removal would lead to a significant change in the values of the vital sign and the overall index value for that capacity.
Finally, to test the robustness of the index to alternate weighting schemes, we recomputed the index with an adjusted weighting scheme, applying weights generated through principal component analysis (PCA). The emergent index was then correlated with the original index that defaults to equal weighting across all indicators. In carrying out the PCA, we selected the first four components, as they cumulatively explained 50% of the variation. We then generated the indicator loadings (eigenvectors) for each of the selected four components. The weights for each indicator were calculated based on the square of the loading, multiplied by the normalised value of the indicator (see online supplemental appendix S3).
Patient and pubic involvement statement
Neither patients nor the public were directly involved in the design of the study as it was primarily analytical. The research question and measures were not informed by patients’ or public’s experiences, as this study was largely analytical and based on publicly available data.
Results
Construct validity
The computed functionality index has a strong correlation with the UHC service coverage index minus service capacity and access component (r=0·7844, p<0.001) by country (figure 3).
Figure 3.
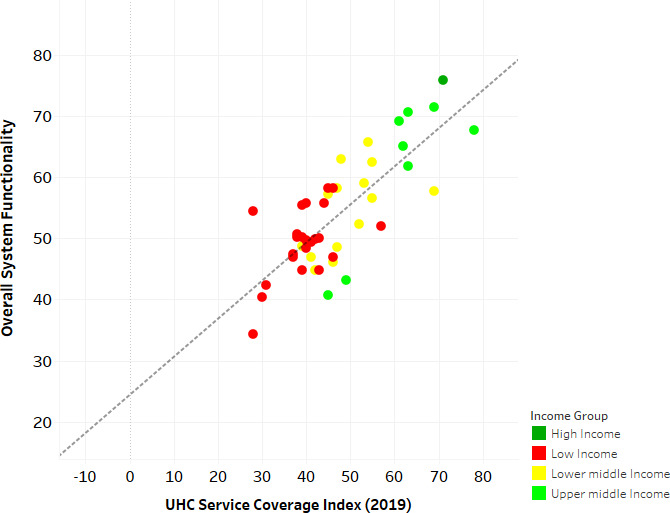
Functionality index correlation with UHC service coverage index (minus service capacity and access component) by country. UHC, universal health coverage.
The emerging functionality index can therefore be considered a valid predictor of the desired health service outcomes countries are aspiring to achieve.
Looking at the value of each of the four capacities in constructing the functionality index, the overall functionality index correlation with the UHC index dropped to r=0.7056 when we removed resilience capacity (functionality due to access, demand and quality capacities); r=0.6439 when we removed access capacity (functionality due to resilience, demand and quality capacities); r=0.6256 when we removed quality capacity (functionality due to access, resilience and demand capacities) and r=0.6641 when we removed demand capacity (functionality due to access, quality and resilience capacities). Each of these correlations remained strong but weaker than the correlation of the original index (constituted by the four capacities); this validated their importance as a consolidated set of capacities.
The correlation between the emerging functionality index and health security is low (r=0.282, p>0.15)- in line with our expectations; the influence of other sector actions is significant and varied enough to make the correlation low. Health system functionality is not the sole predictor of health security as we postulated in our conceptual approach.
The absolute Spearman’s rho values for the correlation of the functionality index with MMR, U5 mortality and neonatal mortality rate were 0.595, 0.709 and 0.675, respectively, all with p<0.001, further pointing towards strong face validity of the computed index. The strength of the correlation is lower than that of the UHC service coverage index (r=0.7844, p<0.001) as hypothesised, thus also validating the relationship highlighted in the conceptual approach.
Looking at the correlation of the index with measures of system efficiency, there was also a strong positive correlation between the overall system functionality index and health system technical efficiency scores for UHC (r=0.6908, p<0.001).
Furthermore, we find a moderate correlation between total current health expenditure per capita and overall system functionality (r=0.484, p<0.001). We explored the reasons for this moderate correlation with funding, despite high correlation with efficiency, by disaggregating the different funding sources and exploring correlations between each source of funds and the system functionality index. A statistically significant correlation is found with public and out-of-pocket funding sources: positive with public funding (r=0.604, p<0.001) and negative with out-of-pocket expenditure (r=−0.503, p<0.001). No correlation or statistical significance was found with other sources of health funds (external funding r=−0.166, p=0.113; domestic private health expenditure r=0.181, p=0.197; voluntary health insurance r=0.340, p=0.029).
Index values by country and component of functionality
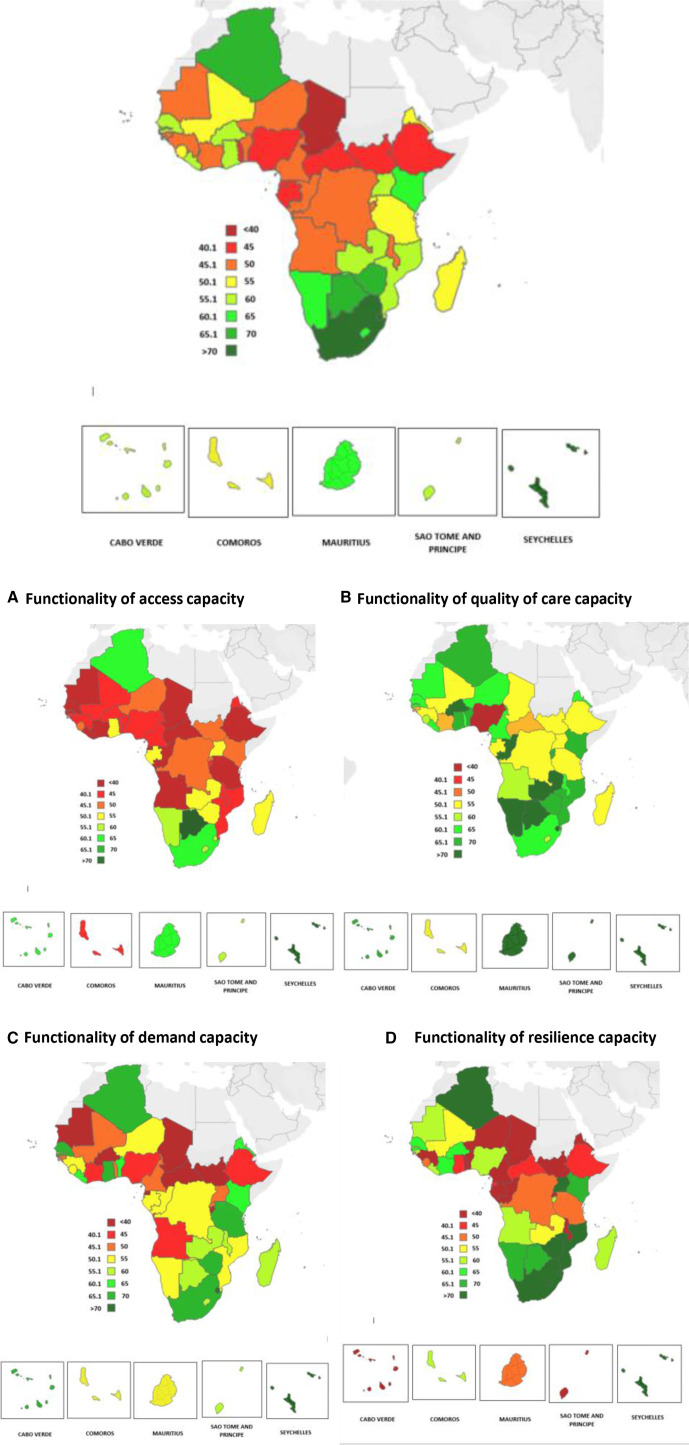
On confirming the validity of the construct and data, we now present the emerging findings by country. Figure 4 illustrates the relative functionality of health systems in the African Region overall and for each capacity.
Figure 4.
Relative functionality of health systems across countries of the WHO African Region. (A) Functionality of access capacity, (B) functionality of quality of care capacity, (C) functionality of demand capacity and (D) functionality of resilience capacity.
Overall system functionality is particularly low in the central African group of countries. The capacities relating to access to essential services and resilience of health systems appear to have the lowest functionality.
The actual values by country, together with values for the specific vital signs under each capacity, are shown in table 2. The functionality does not appear related to income level, country size, nor population. The most functional health systems are for Seychelles, South Africa, Eswatini, Botswana and Algeria, respectively, while those with the least functional are for Gabon, South Sudan, Equatorial Guinea, Central African Republic and Chad. Using Algeria as an example, overall system functionality is high compared with other countries of the region (67.7), which is contributed to by all the four capacities, though access to essential services is the lowest performing capacity (62.3), primarily due to low financial access vital sign (55.2 value).
Table 2.
Health System Functionality Index values overall by capacity and vital sign for each country of the WHO African Region
| Country | Health system functionality (range of 0–100) | ||||||||||
| Index | Access | Quality | Demand | Resilience | |||||||
| Physical | Financial | Socio-cultural | User experiences | Safety | Care effective-ness | Healthy actions | Health seeking | Non-specific resilience | Specific Resilience (IHR core capacity) | ||
| Algeria | 67.7 | 62.3 | 68.6 | 68.7 | 71.4 | ||||||
| 62.7 | 55.2 | 68.8 | 39.3 | 70.7 | 95.8 | 69.5 | 67.8 | 54.7 | 88.0 | ||
| Angola | 48.8 | 36.3 | 55.9 | 44.6 | 58.3 | ||||||
| 16.1 | 54.9 | 37.8 | 53.7 | 46.7 | 67.2 | 45.6 | 43.7 | 22.6 | 94.0 | ||
| Benin | 48.3 | 41.4 | 68.3 | 60.4 | 23.2 | ||||||
| 12.0 | 49.5 | 62.6 | 71.9 | 60.9 | 72.3 | 73.3 | 47.5 | 13.4 | 33.0 | ||
| Botswana | 69.2 | 71.6 | 77.9 | 58.0 | 69.3 | ||||||
| 64.6 | 69.4 | 80.7 | 83.3 | 82.9 | 67.5 | 46.7 | 69.4 | 69.7 | 69.0 | ||
| Burkina Faso | 57.2 | 44.4 | 75.0 | 39.6 | 70.0 | ||||||
| 13.2 | 59.8 | 60.2 | 79.7 | 78.5 | 66.7 | 31.7 | 47.5 | 100.0 | 40.0 | ||
| Burundi | 49.8 | 43.3 | 65.9 | 30.2 | 59.9 | ||||||
| 15.1 | 58.2 | 56.5 | 72.7 | 55.4 | 69.5 | 11.2 | 49.2 | 47.7 | 72.0 | ||
| Cabo Verde | 57.7 | 62.7 | 65.4 | 65.7 | 37.0 | ||||||
| 45.6 | 63.0 | 79.5 | 36.4 | 85.6 | 74.2 | 46.1 | 85.3 | 26.9 | 47.0 | ||
| Cameroon | 46.1 | 41.7 | 63.5 | 46.2 | 33.0 | ||||||
| 30.3 | 39.0 | 55.9 | 58.1 | 69.8 | 62.5 | 46.0 | 46.3 | 40.0 | 26.0 | ||
| Central African Republic | 40.4 | 37.2 | 47.9 | 35.0 | 41.8 | ||||||
| 24.1 | 50.8 | 36.5 | 53.7 | 25.4 | 64.4 | 42.9 | 27.0 | 38.6 | 45.0 | ||
| Chad | 34.4 | 32.2 | 51.9 | 29.2 | 24.3 | ||||||
| 11.0 | 46.1 | 39.6 | 56.3 | 40.5 | 58.8 | 32.0 | 26.3 | 25.7 | 23.0 | ||
| Comoros | 52.4 | 44.1 | 54.6 | 54.1 | 56.8 | ||||||
| 32.1 | 40.4 | 60.0 | 53.7 | 37.1 | 73.0 | 63.6 | 44.6 | 44.5 | 69.0 | ||
| Congo, Dem. Rep | 49.4 | 46.6 | 52.3 | 52.4 | 46.6 | ||||||
| 42.8 | 52.2 | 44.7 | 36.7 | 39.4 | 80.8 | 60.4 | 44.3 | 33.2 | 60.0 | ||
| Congo, Rep | 48.8 | 39.2 | 72.2 | 50.5 | 33.2 | ||||||
| 11.6 | 51.6 | 54.3 | 53.7 | 83.2 | 79.5 | 41.1 | 60.0 | 6.3 | 60.0 | ||
| Cote d'Ivoire | 48.6 | 40.0 | 49.5 | 40.8 | 63.9 | ||||||
| 19.7 | 49.9 | 50.4 | 57.3 | 48.5 | 42.8 | 36.2 | 45.5 | 75.9 | 52.0 | ||
| Equatorial Guinea | 40.7 | 24.1 | 63.5 | 30.6 | 44.6 | ||||||
| 26.9 | 13.7 | 31.6 | 53.7 | 79.9 | 56.8 | 31.4 | 29.8 | 34.3 | 55.0 | ||
| Eritrea | 50.2 | 40.6 | 61.3 | 63.9 | 35.2 | ||||||
| 25.2 | 39.6 | 57.1 | 53.7 | 61.1 | 69.1 | 78.1 | 49.7 | 30.3 | 40.0 | ||
| Eswatini | 70.6 | 56.9 | 71.8 | 71.9 | 81.7 | ||||||
| 43.5 | 66.4 | 60.8 | 80.5 | 84.8 | 50.1 | 70.5 | 73.3 | 63.5 | 100.0 | ||
| Ethiopia | 44.8 | 38.2 | 52.6 | 44.9 | 43.4 | ||||||
| 15.1 | 55.1 | 44.5 | 53.3 | 23.8 | 80.8 | 47.1 | 42.6 | 46.8 | 40.0 | ||
| Gabon | 43.2 | 53.4 | 53.4 | 50.7 | 15.4 | ||||||
| 54.1 | 62.8 | 43.4 | 6.7 | 86.5 | 67.0 | 46.7 | 54.8 | 5.8 | 25.0 | ||
| Gambia | 55.7 | 43.8 | 62.0 | 57.6 | 59.7 | ||||||
| 9.0 | 58.2 | 64.1 | 53.7 | 56.9 | 75.3 | 53.1 | 62.1 | 56.3 | 63.0 | ||
| Ghana | 58.2 | 54.6 | 69.3 | 68.6 | 40.2 | ||||||
| 27.9 | 57.1 | 78.9 | 70.9 | 60.5 | 76.5 | 69.0 | 68.1 | 44.4 | 36.0 | ||
| Guinea | 46.9 | 42.2 | 53.6 | 52.8 | 39.1 | ||||||
| 29.2 | 47.1 | 50.1 | 23.9 | 65.3 | 71.8 | 52.1 | 53.5 | 70.2 | 8.0 | ||
| Guinea-Bissau | 49.6 | 42.4 | 49.4 | 49.6 | 57.1 | ||||||
| 15.2 | 59.0 | 53.1 | 53.7 | 18.6 | 75.9 | 58.5 | 40.8 | 71.2 | 43.0 | ||
| Kenya | 62.5 | 48.0 | 69.1 | 63.7 | 69.1 | ||||||
| 16.7 | 58.5 | 68.7 | 70.9 | 43.5 | 92.8 | 61.3 | 66.0 | 58.2 | 80.0 | ||
| Lesotho | 63.0 | 56.1 | 57.3 | 55.6 | 82.8 | ||||||
| 35.4 | 66.8 | 66.1 | 60.1 | 70.1 | 41.7 | 44.1 | 67.1 | 65.6 | 100.0 | ||
| Liberia | 55.4 | 39.0 | 64.4 | 62.3 | 55.8 | ||||||
| 37.0 | 37.9 | 42.0 | 53.7 | 63.2 | 76.2 | 52.9 | 71.7 | 31.6 | 80.0 | ||
| Madagascar | 54.5 | 51.0 | 51.7 | 57.4 | 58.0 | ||||||
| 28.7 | 65.0 | 59.1 | 6.7 | 74.0 | 74.6 | 65.0 | 49.7 | 62.9 | 53.0 | ||
| Malawi | 47.0 | 44.8 | 64.6 | 56.6 | 22.0 | ||||||
| 13.6 | 62.2 | 58.6 | 44.3 | 63.2 | 86.4 | 45.9 | 67.4 | 36.0 | 8.0 | ||
| Mali | 50.6 | 44.5 | 54.5 | 49.7 | 53.7 | ||||||
| 33.5 | 55.7 | 44.5 | 66.4 | 31.1 | 66.1 | 46.3 | 53.1 | 67.4 | 40.0 | ||
| Mauritania | 47.0 | 37.3 | 60.9 | 31.8 | 58.0 | ||||||
| 20.7 | 49.3 | 41.8 | 54.3 | 52.7 | 75.9 | 19.6 | 44.0 | 76.0 | 40.0 | ||
| Mauritius | 61.8 | 64.2 | 81.9 | 54.4 | 46.6 | ||||||
| 63.0 | 50.2 | 79.6 | 75.0 | 100.0 | 70.8 | 33.7 | 75.1 | 22.1 | 71.0 | ||
| Mozambique | 58.2 | 42.6 | 67.3 | 52.7 | 70.2 | ||||||
| 7.1 | 69.6 | 51.2 | 45.9 | 71.3 | 84.6 | 43.0 | 62.4 | 54.4 | 86.0 | ||
| Namibia | 65.0 | 56.3 | 80.2 | 55.1 | 68.5 | ||||||
| 35.1 | 69.4 | 64.4 | 76.7 | 94.6 | 69.2 | 36.8 | 73.3 | 46.9 | 90.0 | ||
| Niger | 47.4 | 45.9 | 61.7 | 54.0 | 28.0 | ||||||
| 36.8 | 48.5 | 52.3 | 65.5 | 42.3 | 77.4 | 66.8 | 41.1 | 41.1 | 15.0 | ||
| Nigeria | 44.8 | 41.1 | 39.7 | 42.4 | 56.0 | ||||||
| 32.8 | 34.7 | 56.0 | 43.6 | 9.0 | 66.5 | 37.4 | 47.5 | 62.1 | 50.0 | ||
| Rwanda | 52.0 | 48.7 | 70.1 | 49.7 | 39.4 | ||||||
| 15.6 | 65.8 | 64.6 | 53.7 | 76.6 | 79.8 | 39.2 | 60.1 | 53.9 | 25.0 | ||
| Sao Tome and Principe | 56.6 | 59.2 | 72.1 | 60.0 | 35.0 | ||||||
| 52.7 | 61.1 | 63.7 | 53.7 | 79.6 | 82.9 | 49.3 | 70.7 | 30.1 | 40.0 | ||
| Senegal | 57.3 | 38.1 | 62.1 | 65.5 | 63.5 | ||||||
| 13.3 | 52.2 | 48.8 | 50.0 | 55.1 | 81.2 | 71.7 | 59.3 | 75.1 | 52.0 | ||
| Seychelles | 75.8 | 83.4 | 84.7 | 65.2 | 69.8 | ||||||
| 71.8 | 78.6 | 99.8 | 98.0 | 100.0 | 56.0 | 44.6 | 85.8 | 39.6 | 100.0 | ||
| Sierra Leone | 50.2 | 46.1 | 57.9 | 50.9 | 45.8 | ||||||
| 35.4 | 44.3 | 58.5 | 50.3 | 68.7 | 54.8 | 35.9 | 66.0 | 31.7 | 60.0 | ||
| South Africa | 71.5 | 62.0 | 60.4 | 69.8 | 93.8 | ||||||
| 47.7 | 67.3 | 71.0 | 51.3 | 76.3 | 53.5 | 50.1 | 89.4 | 87.6 | 100.0 | ||
| South Sudan | 42.4 | 46.8 | 51.6 | 32.4 | 38.8 | ||||||
| 17.3 | 84.3 | 39.0 | 36.7 | 38.2 | 79.9 | 2.6 | 62.2 | 37.6 | 40.0 | ||
| Togo | 44.8 | 40.3 | 62.3 | 48.6 | 27.8 | ||||||
| 6.3 | 36.2 | 57.5 | 40.6 | 56.0 | 63.7 | 70.3 | 62.8 | 31.6 | 24.0 | ||
| Uganda | 58.3 | 54.3 | 54.5 | 45.1 | 79.2 | ||||||
| 29.9 | 47.7 | 43.4 | 50.9 | 73.8 | 62.3 | 36.9 | 60.3 | 76.3 | 82.0 | ||
| United Republic of Tanzania | 50.1 | 33.3 | 53.4 | 66.6 | 47.0 | ||||||
| 35.8 | 62.1 | 65.0 | 44.0 | 34.7 | 84.7 | 38.7 | 51.5 | 63.9 | 30.0 | ||
| Zambia | 59.0 | 51.8 | 72.6 | 59.2 | 52.6 | ||||||
| 35.7 | 65.2 | 54.5 | 67.3 | 67.9 | 82.5 | 46.2 | 72.2 | 55.2 | 50.0 | ||
| Zimbabwe | 65.8 | 55.1 | 69.1 | 66.3 | 72.6 | ||||||
| 24.0 | 64.0 | 77.1 | 65.0 | 74.4 | 68.0 | 60.4 | 72.2 | 78.3 | 67.0 | ||
| Regional average | 52.9 | 46.3 | 61.6 | 51.4 | 48.4 | ||||||
| 25.2 | 53.4 | 55.8 | 50.5 | 56.2 | 69.8 | 46.4 | 55.6 | 43.1 | 47.6 | ||
Red text denotes the lowest capacity for a given country. Green represent the countries with the highest overall functionality.
IHR, International Health Regulations.
Looking at the vital signs, insufficient physical access, low user experiences, low household health-seeking behaviours and low general resilience are the rate limiting vital signs across the capacities for access, quality, demand and resilience of systems, respectively. Physical access is exceptionally low, making this a key area of regional concern. Populations are just not able to reach the facilities able to provide them with the essential services they need.
Emphasis needs to be placed on capacities and their vital signs with lowest values. While the sector needs to invest in actions across all the capacities, as none of them are fully functional, higher priority should be placed on activities that will improve the capacities with lower values. Interpretation is therefore more powerful at a country level.
Sensitivity analysis
The sensitivity tests indicated that the index is largely robust and stable across various computational approaches.
Substituting the arithmetic mean for the geometric mean, the rank correlation between the values for overall system functionality across both calculations was strong (r=0.9904, p<0.001).
Use of an alternate methodology in normalising the indicators left the relative functionality values largely unchanged, with a strong rank correlation coefficient of r=0.971, p<0.001 between the two approaches.
Looking at the appropriateness of the proxy indicators, the rank correlation coefficient across all the indicator permutations for access to essential services was strong (highest: r=0.9964; lowest: r=0.8889, p<0.0001), and the median absolute difference in the regional value for the various index permutations as compared with the original index was 0.649 (IQR=4.2). For quality of care, the rank correlation coefficient across all the permutations was strong (highest: r=0.9606; lowest: r=0.7061), and the median absolute difference in the various index permutations as compared with the original index was 0.089 (IQR=2.1). For demand for essential services, the rank correlation coefficient across all the permutations was strong (highest: r=0.9845; lowest: r=0.8439), and the median absolute difference in the various index permutations as compared with the original index was 0.197 (IQR=2.1). Finally, for resilience, the rank correlation coefficient across all the permutations was strong (highest: r=0.9741; lowest: r=0.5955), and the median absolute difference in the various index permutations as compared with the original index was 0.028 (IQR=4.2).
Finally, the correlation coefficient between the index with a differential weighting scheme versus the index that applied equal weighting was r=0.844, which indicates a very strong correlation between both approaches and therefore suggests that the author’s choice of an equal or unequal scheme does not significantly change country rankings in the relative index. The choice to default to equal weighting is further justified, as no single weighting scheme can reflect every country’s priorities.
Discussion
Assessments of health system functionality have often employed complex approaches for comparing countries’ health systems against each other. These analyses have generated debate on their practicality and relevance for policy-making. The approach taken in this paper recognises these challenges and offers a different approach that aims at providing countries with guidance on where to strengthen their systems.
We use a systematic and easily replicable method, based on publicly available data, to provide country-specific information on where emphasis needs to be placed to develop systems. The conceptual approach, together with the methods, have been validated, strengthening confidence in the results. The four capacities used to construct functionality appear to be adequate and accurate at this, and the system functionality index is a stronger predictor of desired health service outcomes captured in the UHC index but not for other outcomes influenced significantly by actions in other sectors. This is especially important when we attempt to link health security with health systems status, as has been attempted during the COVID-19 pandemic and previously presumed to be a given. The state of health security in a country cannot be predicted just by the state of health systems. More effort is needed to improve the general resilience that needs to exist within a system, irrespective of the kinds of threats it faces for this to improve.
Looking at the emerging picture, the varied levels of functionality observed across the region reflects the complexity of systems and the need for country-specific determination of actions towards UHC. A broad one-size-fits-all approach will not be the best use of available resources. That the access to essential services capacity is quite low in most countries is of concern, despite the current emphasis placed on addressing financial barriers. It shows that the move towards UHC, even with good financial access, remains difficult when populations still have very low levels of physical access. This needs to be addressed in each country by focusing on the health system investment areas that will make the biggest difference in improving physical access. Alternative service delivery approaches, including use of digital health and other technological innovations, need to be explored to accelerate improvements in these.
The strong correlation with efficiency and effectiveness measures is useful, as it shows efforts to improve the capacities in countries will ultimately lead to good impact. Of equal interest is the finding that functionality correlates strongest with public funding, as compared with non-public sources of funding, a finding that shows the importance of governments’ investment in health with domestic resources. This also aligns with the current drive to increase public funding and reduce out-of-pocket funding in order to move towards UHC. The inconsistent contribution of external health expenditures, domestic private health expenditure and voluntary private health insurance reflect the different ways these sources are mobilised and used in countries.
Study limitations
While we have explored the face validity of the computed index, we recognise the process still has some limitations.
First, we limit the ascertainment of construct validity to predictability of UHC service coverage at the outcome level. While UHC is a common target across countries, it does not represent the full range of outcomes countries need to work towards. Better outcomes across other health-related sectors are also important but not reflected in the UHC index.
Second, the use of proxy indicators will always be inferior to having the actual indicators. We call for a more detailed appraisal of indicators and country-level data systems, particularly if a similar analysis is being carried out at the subnational level.
Third, we avoid prescribing areas of the health system where interventions are needed, recognising the fact that each country has unique ways they need to develop their system. However, it would be important to have a menu of possible health system interventions for each of the health system elements that would guide countries in terms of system investments that would have impacts on each of the given capacities.
Fourth, while the capacities identified are an appropriate measure of system functionality for UHC, absence of an equity correlation is a big gap. This could be incorporated in similar subnational assessments by analysing changes in functionality driven by equity stratifiers such as wealth quintiles, age, gender and geographic location. This would allow system development priorities arising from this analysis to incorporate equity considerations.
Finally, an element that may further strengthen this empirical analysis is to historically calculate the index for previous years to be able to observe how performance changes over time and how this variation is correlated with time variation in other indices. An objective for further research would be to correlate the index with exogenous policy changes over time to evaluate its influence on policy change at country level.
Conclusion
The paper offers a new approach for conceptualising system functionality and generating information on the functionality of health systems for UHC attainment. It provides a systematic but policy-relevant approach that countries can use to develop their systems. The focus was to have a practical, empirical approach that decision makers can use, based on available information, to determine how their systems are functioning and where their efforts for improvement are best placed. The disaggregation of the overall functionality index into four capacities, and their vital signs, gives more information on where effort needs to be placed. We move the discussion of system functionality away from a focus on standalone analyses of its constituent building blocks, to a focus on understanding the strengths and gaps in cross-cutting capacities that allow a decision maker to determine which elements in the system they can focus on to improve functionality. This has a key value proposition for countries, given that issues faced by their systems are cross-cutting, not mutually exclusive and context specific.
The outcomes of the paper are both the methodology and the results of its application. Countries can replicate this assessment at the subnational level to monitor the functionality of those systems for more targeted policy action.
Footnotes
Handling editor: Seye Abimbola
Twitter: @karamagih, @Hillarykipruto, @julienabyonga, @AminataSeydi1, @ZawairaFelly, @GerardSchmets, @WHOAFRO
Contributors: JWC and PT conceived the study; HCK, RT-O, HK and BD developed the methodology; HCK, RT-O, HK and AB-WS analysed the data and consolidated the paper; JN, FZ and GS reviewed the interpretations and conclusions.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data are available on request. All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study was derived from reputable public open access sources. Any additional information needed is available in the supplementary appendix and on request.
References
- 1.Tumusiime P, Nabyonga-Orem J, Karamagi H, et al. Resilient health systems for attaining universal health coverage. BMJ Glob Health 2019;4:e002006. 10.1136/bmjgh-2019-002006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . The world health report 2000: health systems: improving performance. Geneva: WHO; 2000. [Google Scholar]
- 3.World Health Organization . Everybody’s business: strengthening health systems to improve health outcomes : WHO’s frmaework for action. Geneva: WHO; 2007. [Google Scholar]
- 4.Schoen C, Davis K, How SKH, et al. U.S. health system performance: a national scorecard. Health Aff 2006;25:W457–75. 10.1377/hlthaff.25.w457 [DOI] [PubMed] [Google Scholar]
- 5.Lakhani A, Coles J, Eayres D, et al. Creative use of existing clinical and health outcomes data to assess NHS performance in England: Part 1--performance indicators closely linked to clinical care. BMJ 2005;330:1426–31. 10.1136/bmj.330.7505.1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tashobya C, Ssengooba F, Nabyonga-Orem J. Health systems performance assessment in low-income countries: learning from international experiences 2014;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.. Health system performance frameworks: aligning frameworks for sectors and organizations to health systems. Ottawa, Canada: Canadian Insitute for Health Information; 2015. [Google Scholar]
- 8.Kumah E, Ankomah SE, Fusheini A, et al. Frameworks for health systems performance assessment: how comprehensive is Ghana's holistic assessment tool? Glob Health Res Policy 2020;5:10. 10.1186/s41256-020-00139-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edward A, Kumar B, Kakar F, et al. Configuring balanced scorecards for measuring health system performance: evidence from 5 years' evaluation in Afghanistan. PLoS Med 2011;8:e1001066. 10.1371/journal.pmed.1001066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma A, Prinja S, Aggarwal AK. Measurement of health system performance at district level: a study protocol. J Public health Res;3. 10.4081/jphr.2017.917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Massyn N, Barron P, Day C. District health barometer. Health Systems Trust 2020. [Google Scholar]
- 12.Lynch T. A critique of health system performance measurement. Int J Health Serv 2015;45:743–61. 10.1177/0020731415585987 [DOI] [PubMed] [Google Scholar]
- 13.Fekri O, Macarayan ER, Klazinga N. Health system performance assessment in the who European region: which domains and indicators have been used by member states for its measurement? Copenhagen: WHO Regional Office for Europe, 2018. http://www.ncbi.nlm.nih.gov/books/NBK519096/ [PubMed] [Google Scholar]
- 14.de Savigny D, Adam T. Systems thinking: what it is and what it means for health systems. In: Systems thinking for health systems strengthening, 2009. [Google Scholar]
- 15.Peters DH. The application of systems thinking in health: why use systems thinking? Health Res Policy Sys 2014;12:51. 10.1186/1478-4505-12-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheikh K, Gilson L, Agyepong IA, et al. Building the field of health policy and systems research: framing the questions. PLoS Med 2011;8:e1001073. 10.1371/journal.pmed.1001073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clancy C. The performance of performance measurement: performance of performance measurement. Health Services Research 2007;42:1797–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization . Everybody’s business: strengthening health systems to improve health outcomes : WHO’s frmaework for action. Geneva: WHO; 2007. [Google Scholar]
- 19.World Health Organization . Primary health care on the road to universal health coverage monitoring report, 2019. Available: https://www.who.int/healthinfo/universal_health_coverage/report/uhc_report_2019.pdf?ua=1
- 20.Kraef C, Kallestrup P. After the Astana declaration: is comprehensive primary health care set for success this time? BMJ Glob Health 2019;4:e001871. 10.1136/bmjgh-2019-001871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magnussen L, Ehiri J, Jolly P. Comprehensive versus selective primary health care: lessons for global health policy. Health Aff 2004;23:167–76. 10.1377/hlthaff.23.3.167 [DOI] [PubMed] [Google Scholar]
- 22.Rifkin SB, Walt G. Why health improves: defining the issues concerning 'comprehensive primary health care' and 'selective primary health care'. Soc Sci Med 1986;23:559–66. 10.1016/0277-9536(86)90149-8 [DOI] [PubMed] [Google Scholar]
- 23.Barasa E, Mbau R, Gilson L. What is resilience and how can it be Nurtured? A systematic review of empirical literature on organizational resilience. Int J Health Policy Manag 2018;7:491–503. 10.15171/ijhpm.2018.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kruk ME, Myers M, Varpilah ST, et al. What is a resilient health system? Lessons from Ebola. The Lancet 2015;385:1910–2. 10.1016/S0140-6736(15)60755-3 [DOI] [PubMed] [Google Scholar]
- 25.Zolia Y, Musa E, Wesseh CS, et al. Setting the scene for Post-Ebola health system recovery and resilience in Liberia: lessons learned and the way forward. Health Systems and Policy Research 2017;04. 10.21767/2254-9137.100061 [DOI] [Google Scholar]
- 26.Mboussou F, Ndumbi P, Ngom R, et al. Infectious disease outbreaks in the African region: overview of events reported to the world Health organization in 2018. Epidemiol Infect 2019;147:e299. 10.1017/S0950268819001912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cabore JW, Karamagi HC, Kipruto H, et al. The potential effects of widespread community transmission of SARS-CoV-2 infection in the world Health organization African region: a predictive model. BMJ Glob Health 2020;5:e002647. 10.1136/bmjgh-2020-002647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Orgainzation Regional Office for Africa . Framework for health systems development towards universal health coverage in the context of the sustainable development goals in the African region. Available: https://www.afro.who.int/sites/default/files/2018-01/AFR-RC67-10%20Framework%20for%20health%20systems%20development-Rev%2023.09.17.pdf
- 29.Oppenheim B, Gallivan M, Madhav NK, et al. Assessing global preparedness for the next pandemic: development and application of an epidemic preparedness index. BMJ Glob Health 2019;4:e001157. 10.1136/bmjgh-2018-001157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Global Health Security Index . The Economict intelligence unit and Johns Hopkins Bloomberg school of public health, 2019. Available: https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf
- 31.WHO Regional Committee for Africa . Framework for health systems development towards universal health coverage in the context of the sustainable development goals, 2017. Available: https://www.afro.who.int/sites/default/files/2018-01/AFR-RC67-10%20Framework%20for%20health%20systems%20development-Rev%2023.09.17.pdf
- 32.Ibeneme S, Ongom M, Ukor N, et al. Realigning health systems strategies and approaches; what should African countries do to strengthen health systems for the sustainable development goals? Front Public Health 2020;8:372. 10.3389/fpubh.2020.00372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karamagi HC, Barasa E, Titi-Ofei R. On the resilience of health systems in the WHO African region for sustained provision of essential services health emergencies. BMJ Glob Health. [Google Scholar]
- 34.Tumusiime P, Karamagi H, Titi-Ofei R, et al. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the fifth health sector directors' policy and planning meeting for the WHO African region. BMC Proc 2020;14:16. 10.1186/s12919-020-00203-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taylor R. Interpretation of the correlation coefficient: a basic review. Journal of Diagnostic Medical Sonography 1990;6:35–9. 10.1177/875647939000600106 [DOI] [Google Scholar]
- 36.Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med 2014;11:e1001701. 10.1371/journal.pmed.1001701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsu J, Flores G, Evans D, et al. Measuring financial protection against catastrophic health expenditures: methodological challenges for global monitoring. Int J Equity Health 2018;17:69. 10.1186/s12939-018-0749-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grépin KA, Irwin BR, Sas Trakinsky B. On the measurement of financial protection: an assessment of the usefulness of the catastrophic health expenditure indicator to monitor progress towards universal health coverage. Health Syst Reform 2020;6:e1744988. 10.1080/23288604.2020.1744988 [DOI] [PubMed] [Google Scholar]
- 39.Jordi E, Pley C, Jowett M, et al. Assessing the efficiency of countries in making progress towards universal health coverage: a data envelopment analysis of 172 countries. BMJ Glob Health 2020;5:e002992. 10.1136/bmjgh-2020-002992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hogan DR, Stevens GA, Hosseinpoor AR, et al. Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. Lancet Glob Health 2018;6:e152–68. 10.1016/S2214-109X(17)30472-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-004618supp001.pdf (1.2MB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data are available on request. All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study was derived from reputable public open access sources. Any additional information needed is available in the supplementary appendix and on request.