Abstract
Objective
To determine whether trophectoderm (TE) grade or inner cell mass (ICM) grade have predictive value after euploid frozen embryo transfer (euFET) among recurrent pregnancy loss (RPL) patients.
Design
Retrospective cohort study.
Setting
Single fertility center.
Patient(s)
Women with ≥2 prior pregnancy losses with ≥1 euploid embryo for transfer undergoing preimplantation genetic testing for aneuploidy.
Intervention(s)
Intracytoplasmic sperm injection, TE biopsy, blastocyst grading and vitrification, and single euFET, with first transfer outcome recorded.
Main Outcome Measure(s)
Live birth and clinical miscarriage rates.
Result(s)
The study included 660 euFET cycles. In a binomial logistic regression analysis accounting for age, body mass index, antimüllerian hormone level, and day of blastocyst biopsy, or ICM grade C was not significantly associated with odds of live birth, miscarriage, or biochemical pregnancy loss. TE grade C was significantly associated with odds of live birth and was not associated with odds of miscarriage or biochemical pregnancy loss. Blastocyst grade CC had significantly lower live birth rate compared with all other blastocyst grades.
Conclusion(s)
Embryo grade CC and TE grade C are associated with decreased odds of live birth after euFET in RPL patients. Embryo grade is not associated with odds of clinical miscarriage in this cohort of RPL patients, suggesting that additional embryonic or uterine factors may influence the risk of pregnancy loss.
Key Words: Embryo grade, euploid transfer, miscarriage, PGT-A, recurrent pregnancy loss
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/users/16110-fertility-and-sterility/posts/xfre-d-20-00090
Management of patients with recurrent pregnancy loss (RPL) continues to be a challenge for clinicians. The role of aneuploidy in miscarriage is well documented, with over 50% of pregnancy losses attributed to fetal chromosomal abnormalities and even higher aneuploidy rates reported among older patients (1, 2). Due to the prevalence of aneuploidy in first-trimester losses and in the RPL population, preimplantation genetic testing for aneuploidy (PGT-A) has been used as a method for reducing miscarriage by selecting only euploid embryos for transfer (3, 4). Causes of euploid miscarriage, particularly in the setting of RPL, remain a topic of great interest to both physicians and patients. In the absence of an explanation, patients often seek unproven testing and treatments.
The current literature on the prognostic value of blastocyst assessment applies to the general infertile population. Blastocyst morphological grading was first described by Gardner et al. (5). Since then, studies have teased apart the relative contribution of trophectoderm (TE) and inner cell mass (ICM) grade on an embryo’s potential to implant and result in a live birth. After transfer of untested blastocysts, TE grade has been shown to be a superior predictor of live birth in fresh cycles (6, 7) and a superior predictor of live birth and miscarriage in frozen cycles (8). Embryo morphology, however, is not consistently correlated with euploidy.
Both ICM and TE grades have been reported by Capalbo et al. (9) to be unrelated to implantation outcomes after frozen euploid embryo transfer (euFET), but only 13 embryos were included in the poor-quality blastocyst group. Conflicting results have subsequently been published using the same classification scheme but with a larger comparison group of 106 poor-quality euploid embryos. In the latter study, Irani et al. (10) reported an approximately twofold higher pregnancy rate and 25-fold lower miscarriage rate among excellent-quality euploid blastocysts compared with poor-quality euploid blastocysts and that ICM morphology is a better predictor of pregnancy outcomes than TE morphology (10). A large study by Zhao et al. (11) showed similar predictive value of TE and ICM grades in pregnancy outcomes after euFET. Our study examined whether TE grade or ICM grade retained their established predictive values after euFET in a cohort of RPL patients.
Materials and methods
Patient selection
Patients with RPL having PGT-A performed with at least one euploid embryo for transfer from 2012–2018 were included in the study. We defined RPL as two or more prior pregnancy losses, inclusive of biochemical conceptions but independent of other infertility diagnoses. All patients had a complete RPL workup as recommended by the American Society for Reproductive Medicine (ASRM), including bloodwork for parental karyotypes and to detect the presence of antiphospholipid antibody syndrome (APLA) including anticardiolipin antibody, lupus anticoagulant, and β2-glycoprotein, as well as a uterine cavity evaluation. Patients were also routinely screened for hypothyroidism and hyperprolactinemia with serum thyroid-stimulating hormone and prolactin, respectively. Patients who were known to be translocation carriers (either maternal or paternal) were excluded. Patients with the APLA syndrome were offered low-dose aspirin and prophylactic heparin. Patients with uterine cavity anomalies, including a uterine septum, intramural fibroids, or uterine polyps, underwent hysteroscopy and transection of the uterine septum, myomectomy, or polypectomy, respectively, before embryo transfer.
Clinical protocols
Controlled ovarian hyperstimulation was performed according to standard protocols per physician discretion. The stimulation protocols included microdose flare, Lupron down-regulation, gonadotropin-releasing hormone antagonist, and natural cycle. After transvaginal oocyte retrieval, all oocytes were fertilized with intracytoplasmic sperm injection, and all blastocysts underwent TE biopsy on day 5, 6, or 7 of embryo development once full expansion had been achieved. All embryos were vitrified after TE biopsy. Embryos were graded at the time of cryopreservation using the Gardner grading scale. We implemented PGT-A using next-generation sequencing (NGS), quantitative reverse-transcription polymerase chain reaction (qRT-PCR), or array comparative genomic hybridization platforms. All patients underwent frozen transfer of a single euploid blastocyst.
The endometrial lining was prepared using modified natural cycle or medicated cycle protocols per physician discretion. For natural cycles, patients used vaginal progesterone suppositories for luteal support until 8 weeks’ gestational age. For medicated cycles, the endometrium was primed with oral estradiol, estrogen patches, or intramuscular estrogen valerate, and luteal support was provided through intramuscular progesterone in oil until 8 weeks’ gestational age, at which time support was transitioned to vaginal suppositories until 10 weeks.
Blastocyst transfer took place on the sixth day after human chorionic gonadotropin (hCG) administration in modified natural cycles, and on day 6 of progesterone supplementation in programmed cycles. Embryo transfers were performed with transabdominal ultrasound guidance after confirmation of embryo survival after warming. The serum progesterone level was measured 2 days after transfer, and the serum hCG level was obtained 9 days after transfer. Transvaginal ultrasound to monitor for the presence of a gestational sac was performed during the fifth week of gestation, with subsequent pregnancy ultrasounds to monitor the fetal heart rate and appropriate growth between 6 to 8 weeks’ gestation. The outcome of the first euFET was recorded.
Outcome variables
The main outcome measured was live birth, defined as birth of a neonate at or beyond 24 weeks’ gestation. The secondary outcome was clinical miscarriage, defined as loss of pregnancy after visualization of a gestational sac on ultrasound. Additional outcomes measured included implantation (defined as β-hCG >5 mIU/mL), clinical pregnancy (defined as β-hCG >5 mIU/mL and a visualized gestational sac), and biochemical pregnancy loss (defined as loss of pregnancy after conception, β-hCG level >5 mIU/mL, and before visualization of a gestational sac on transvaginal ultrasound). Implantation, clinical pregnancy, and live birth were calculated per embryo transfer. Biochemical pregnancy loss rate was calculated per implantation. Clinical miscarriage rate was calculated per clinical pregnancy.
Statistical analysis
The baseline parameters of the patients were compared using t tests or single factor analysis of variance. Chi-square analysis was performed to compare the proportion of assisted reproduction outcomes within each morphologic grade. We modeled the association between TE grade or ICM grade (A, B, or C, with A as reference) and pregnancy outcome (live birth, clinical miscarriage, or biochemical pregnancy loss) after euFET using logistic regression. The model was adjusted for age (continuous), body mass index (BMI; categorical subdivided as BMI ≥25 kg/m2 or BMI <25 kg/m2), antimüllerian hormone level (AMH; categorical subdivided as AMH <1 ng/mL or ≥1 ng/mL), and day of blastocyst biopsy (day 5, 6, or 7). We included AMH level as a covariate in our analysis because it has been shown to be a predictor of live-birth rate in RPL patients overall (12); also RPL patients with AMH <1 ng/mL have a higher percentage of aneuploid blastocysts (13). Statistical analysis was performed using SPSS software version 25 (IBM, Inc.). P<.05 was considered statistically significant. This study was exempt from institutional review board approval because it was a retrospective analysis of deidentified data.
Results
We included 660 euFET cycles in the analysis. The average patient age was 36.7 ± 3.4 years, average BMI was 25.7 ± 5.6 kg/m2, and patients had on average 3.5 ± 1.5 prior pregnancies, 0.5 ± 0.8 term deliveries, and 2.6 ± 1.1 prior pregnancy losses. The average AMH level was 3.4 ± 3.8 ng/mL and average FSH level was 7.5 ± 2.8 IU/mL before stimulation start. Patients with TE grade C (average age 38.3 years) were statistically significantly older than the patients with TE grade B (average age 37.2 years; P=.02) and patients with TE grade A (average age 36.5 years, P<.05). Patients with TE grade C had an average AMH level (3.4 ± 3.8 ng/mL) similar to the patients with TE grade B (average AMH, P=.95) and patients with TE grade A (average AMH 3.9 ± 4.5 ng/mL; P=.10). Patients with TE grades A, B, and C had a similar BMI (P=.80). Patients with ICM grade C (average age 37.5 years) were statistically significantly older than patients with ICM grade A (average age 36.0 years; P=.01) and similar in age to patients with ICM grade B (average age 37.0 years; P=.43). Patients with ICM grade A, B, and C had similar BMI (P=.55). Patients with embryo grade CC were on average 37.0 ± 4.3 years of age with AMH 2.7 ± 2.4 ng/mL. Compared with the overall cohort, these patients did not differ in terms of age (P=.69) or AMH level (P=.52).
For controlled ovarian hyperstimulation, 82% of cycles used an antagonist protocol, 11% of cycles used a microdose flare protocol, 6% used a long Lupron protocol, and 1% used a natural cycle. For PGT-A, 54% were performed using a qRT-PCR platform, 45% used NGS, and a microarray platform was used for 1% of cycles. On average per oocyte retrieval, 15.5 ± 9.8 oocytes were retrieved, 5.4 ± 3.8 blastocysts were biopsied for PGT-A, and 3.6 ± 2.9 embryos were euploid. Patients with TE grade C had on average per oocyte retrieval 11.1 ± 7.8 oocytes retrieved, 2.6 ± 1.7 embryos biopsied, and 1.4 ± 0.9 euploid embryos.
Compared with patients with TE grades A and B, patients with TE grade C had fewer oocytes retrieved (P<.01), fewer embryos biopsied (P<.01) and fewer euploid embryos (P<.01). Patients with embryo grade CC had on average per oocyte retrieval 11.0 ± 5.8 oocytes retrieved, 2.4 ± 1.6 embryos biopsied, and 1.5 ± 1.0 euploid embryos. Compared with the overall cohort, patients with embryo grade CC did not differ in terms of number of oocytes retrieved (P=.06) but had statistically significantly fewer embryos biopsied (P≤.01) and fewer number of euploid embryos (P≤.01).
The endometrial lining was prepared before transfer by use of a medicated cycle for 78% of transfers and a natural cycle protocol for the remaining cycles (22%). The average endometrial thickness before embryo transfer was 9.4 ± 2.1 mm. The overall live-birth rate per euFET was 62% (n = 408).
The clinical outcomes stratified by ICM and TE grade are shown in Table 1. There were 217 ICM grade A euFETs, 405 ICM grade B euFETs, and 38 ICM grade C euFETs. The live birth, clinical miscarriage, and biochemical pregnancy loss rates were similar for ICM grades A, B, and C (P=.08, P=.38, and P=.45, respectively, chi-square analysis). In a logistic regression analysis accounting for age, BMI, AMH, and day of blastocyst biopsy, ICM grade B was not statistically significantly associated with odds of live birth (adjusted odds ratio [aOR] 0.80; 95% confidence interval [CI] 0.56–1.14; P=.21), miscarriage (aOR 1.53; 95% CI 0.85–2.77; P=.16), or biochemical pregnancy loss (aOR 0.87; 95% CI 0.47–1.62; P=.66) (Table 2). Also ICM grade C was not statistically significantly associated with odds of live birth (aOR 0.50; 95% CI 0.24–1.02; P=.057), miscarriage (aOR 1.67; 95% CI 0.56–5.00; P=.36), or biochemical pregnancy loss (aOR 1.58; 95% CI 0.53–4.75; P=.42).
Table 1.
Comparison of outcomes after euploid frozen embryo transfer stratified by inner cell mass and trophectoderm blastocyst grades.
| Grade | euFET (n) | Implantationa | P valueb | Clinical pregnancyc | P valueb | Live birthd | P valueb | Clinical miscarriagee | P valueb | Biochemical pregnancy lossf | P valueb |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICM | |||||||||||
| A | 217 | 185 (85) | .24 | 164 (76) | .26 | 145 (67) | .08 | 18 (11) | .38 | 19 (10) | .45 |
| B | 405 | 327 (81) | 293 (72) | 244 (60) | 47 (16) | 31 (9) | |||||
| C | 38 | 29 (81) | 24 (63) | 19 (50) | 5 (21) | 5 (17) | |||||
| TE | |||||||||||
| A | 312 | 259 (83) | .38 | 232 (74) | .09 | 203 (65) | .01 | 28 (12) | .25 | 24 (9) | .37 |
| B | 277 | 228 (82) | 205 (75) | 172 (62) | 31 (15) | 22 (10) | |||||
| C | 71 | 54 (76) | 44 (62) | 33 (46) | 11 (25) | 9 (17) |
Note: Values are number (percentage) unless specified otherwise. euFET = euploid frozen embryo transfer; ICM = inner cell mass; TE = trophectoderm.
Implantation was defined as β-human chorionic gonadotropin level > 5 mIU/mL.
Chi-square analysis.
Clinical pregnancy was defined as a visualized gestational sac.
Live birth was defined as delivery of a neonate at or beyond 24 weeks.
Clinical miscarriage rate was calculated per clinical pregnancy.
Biochemical pregnancy loss was defined as loss of pregnancy after conception and before visualization of a gestational sac on transvaginal ultrasound. Biochemical pregnancy loss rate was calculated per implantation.
Table 2.
Association between inner cell mass or trophectoderm grade and pregnancy outcome after euploid frozen embryo transfer.
| Outcome | Crude OR (95% CI) | P value | Adjusted OR (95% CI)a | P value |
|---|---|---|---|---|
| ICM grade Bb | ||||
| Live birth | 0.75 (0.53–1.06) | .10 | 0.80 (0.56–1.14) | .21 |
| Clinical miscarriage | 1.12 (0.42–3.02) | .82 | 1.53 (0.85–2.77) | .16 |
| Biochemical pregnancy loss | 0.87 (0.48–1.57) | .64 | 0.87 (0.47–1.62) | .66 |
| TE grade Bb | ||||
| Live birth | 0.86 (0.62–1.21) | .38 | 0.90 (0.63–1.27) | .53 |
| Clinical miscarriage | 1.33 (0.78–2.27) | .30 | 1.37 (0.79–2.39) | .27 |
| Biochemical pregnancy loss | 1.04 (0.57–1.90) | .90 | 1.08 (0.58–2.00) | .82 |
| ICM grade Cb | ||||
| Live birth | 0.45 (0.22–0.90) | .02 | 0.50 (0.24–1.02) | .057 |
| Clinical miscarriage | 1.68 (0.58–4.82) | .34 | 1.67 (0.56–5.00) | .36 |
| Biochemical pregnancy loss | 1.58 (0.55–4.52) | .40 | 1.58 (0.53–4.75) | .42 |
| TE grade Cb | ||||
| Live birth | 0.47 (0.28–0.79) | .004 | 0.49 (0.28–0.86) | .01 |
| Clinical miscarriage | 1.86 (0.88–3.94) | .11 | 2.00 (0.89–4.47) | .09 |
| Biochemical pregnancy loss | 1.74 (0.77–3.93) | .18 | 1.85 (0.77–4.44) | .17 |
Note: AMH = antimüllerian hormone; BMI = body mass index; CI = confidence interval; ICM = inner cell mass; OR = odds ratio; TE = trophectoderm.
Adjusted for age (continuous), overweight (categorical, BMI ≥25 kg/m2 or BMI <25 kg/m2), AMH (categorical, <1 ng/mL or ≥1 ng/mL), and day of blastocyst biopsy (5, 6, or 7).
Logistic regression model, ICM or TE grade A used as reference.
There were 312 TE grade A euFETs, 277 TE grade B euFETs, and 71 TE grade C euFETs. The live-birth rates for TE grades A, B, and C differed statistically significantly by chi-square analysis (P=.01) whereas the clinical miscarriage and biochemical pregnancy loss rates were similar (P=.25 and P=.37, respectively, chi-square analysis). In a logistic regression analysis accounting for age, BMI, AMH, and day of blastocyst biopsy, TE grade B was not associated with odds of live birth (aOR 0.90; 95% CI 0.63–1.27; P=.53), miscarriage (aOR 1.37; 95% CI 0.79–2.39; P=.27), or biochemical pregnancy loss (aOR 1.08; 95% CI 0.58–2.00; P=.82). Trophectoderm grade C was statistically significantly associated with odds of live birth (aOR 0.49; 95% CI 0.28–0.86; P=.01) and was not associated with odds of miscarriage (aOR 2.00; 95% CI 0.89–4.47; P=.09) or biochemical pregnancy loss (aOR 1.85; 95% CI, 0.77–4.44; P=.17).
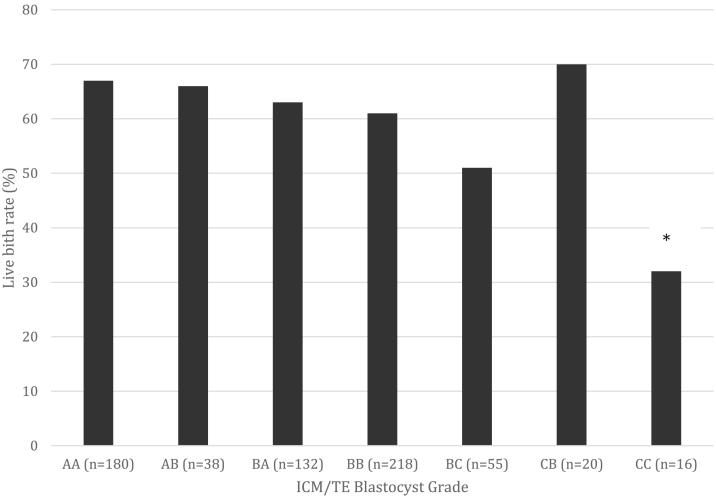
Live-birth outcomes for embryos with combined ICM and TE grades AA, AB, BA, BB, BC, CA, CB, and CC are shown in Figure 1. Sixteen blastocysts were grade CC, with an implantation rate of 69% (n = 11), clinical pregnancy rate of 50% (n = 8), live-birth rate of 31% (n = 5), clinical miscarriage rate of 38% (n = 3), and biochemical loss rate of 27% (n = 3). Blastocyst grade CC had a statistically significantly lower live-birth rate compared with all other blastocyst grades: AA, AB, BA, BB, BC, and CB (P<.05, chi-square analysis).
Figure 1.
Comparison of live birth rate per patient after euploid frozen embryo transfer stratified by combined inner cell mass (ICM)/ trophectoderm (TE) blastocyst grades. Results not shown in graph: one grade CA embryo was transferred, resulting in implantation and subsequent miscarriage. ∗P<.05, chi-square analysis.
Discussion
In this cohort of RPL patients, we report that TE grade C and blastocyst grade CC are associated with a statistically significant decrease in odds of live birth after euFET. After the transfer of untested blastocysts in general infertile cohorts, TE grade has been shown to be a superior predictor of live birth in fresh cycles (6, 7) and a superior predictor of live birth and miscarriage in frozen cycles (8).To our knowledge, ours is the first report on the association of embryo grade and outcomes in RPL patients undergoing euFET, and our data support the previous reports that blastocyst morphology is associated with live-birth outcome after euFET (10, 11).
In any patient population, myriad factors influence reproductive outcomes. Among RPL patients in whom additional factors may impact outcomes, it is notable that blastocyst morphology retains its predictive value for live birth. The association, if any, between embryo grade and pregnancy loss is particularly interesting in the RPL patient population. Irani et al. (10) reported a striking trend among euFET cycles in a general infertile cohort, with a 25% miscarriage rate after frozen transfer of poor-quality euploid blastocysts (n = 51) compared with no miscarriages after frozen transfer of excellent-quality euploid blastocysts (n = 32) and a 6% miscarriage rate after frozen transfer of good-quality euploid blastocysts (n = 50). Patients with RPL are at higher risk of euploid miscarriage (14), and the varying contributions of embryonic and uterine factors are unknown.
In our study, when comparing outcomes for embryos with ICM or TE grade C compared with higher grades, there was a trend toward higher risk of miscarriage with poorer embryo grade, but the differences were not statistically significant. This finding is likely multifactorial, due in part to the small size of the subgroups, but also may suggest that there is additional variability in reproductive efficiency among RPL patients that is not captured by euploidy or blastocyst morphology. The parameters that affect outcomes in a general infertile population may be less predictive among RPL patients, in whom uterine factors that are not accounted for or embryo factors that are yet to be understood may play an important role in miscarriage. This information can be used as an aid to counsel RPL patients on risk of miscarriage after euploid transfer.
The strengths of this study include a relatively large sample size for studying an RPL population and use of single blastocyst euploid frozen transfer for all patients to minimize confounding due to number of embryos transferred and the effect of freeze/thaw cycles on the TE or ICM. A limitation of the study, as previously noted in the literature, is the intra- and interobserver variability in embryo grading (15, 16). Our results, however, are from a single center with regular proficiency and consistency checks. Because our outcome was limited to a single-embryo transfer, we were not able to identify overall egg or sperm quality. Furthermore, our analysis was limited to patients reaching transfer of at least a CC grade or higher quality euploid embryo, which may not be reflective of outcomes in poorer prognosis cycles. In addition, our findings may not be applicable to an unscreened population of embryos because morphologic assessment was only performed on the embryos designated as being of sufficient quality to merit cryopreservation.
Although all RPL patients underwent a complete evaluation per ASRM guidelines, and all patients with translocations were excluded, the granular data on the number of patients who received treatment for APLA or correction of uterine anomalies was not available and may present unmeasured confounding. As this study focused exclusively on patients with RPL, our findings cannot be used to differentiate the prognostic value of the embryos from other subgroups of patients. Our findings are, however, supported by prior studies in a general infertile population (10, 11).
Different PGT-A platforms were used for this study, which introduces heterogeneity and potential for unmeasured confounding of study results. However, qRT-PCR, NGS, and array comparative genomic hybridization have been validated for use through large, prospective randomized clinical studies (17, 18, 19). In addition, many studies examining PGT-A are similarly limited by heterogeneity of testing methodology such that ASRM does not endorse one testing platform in particular (20). Also, although day-7 blastocysts have been associated with lower pregnancy and live-birth rates and could bias study results (21, 22, 23, 24), of the 660 cycles included in this study, only four (0.6%) performed TE biopsy on day 7.
Finally, the results are limited by the relatively small number of poorer quality embryos. The lack of difference in clinical outcomes between various embryo grades may be due to limited statistical power. Larger scale, prospective analyses accounting for total cycle potential are warranted to confirm the reported findings.
Conclusion
Association between embryo grade and clinical outcomes had not been previously been reported in RPL patients. Embryo grade CC and TE grade C are associated with a statistically significant decrease in odds of live birth after euFET in RPL patients. Furthermore, embryo grade was not predictive of clinical miscarriage rate in this cohort of RPL patients, suggesting that additional embryonic or uterine factors may influence their risk of pregnancy loss.
Footnotes
G.M. has nothing to disclose. J.G.K. has nothing to disclose. J.D.K. has nothing to disclose. B.M.H. has nothing to disclose. S.A.N. has nothing to disclose. A.W.T. has nothing to disclose. E.K.O. has nothing to disclose. R.T.S. has nothing to disclose. R.B.L. has nothing to disclose.
References
- 1.Viaggi C.D., Cavani S., Malcarne M., Floriddia F., Zerega G., Baldo C. First trimester euploid miscarriages analyzed by array CGH. J Appl Genet. 2013;54:353–359. doi: 10.1007/s13353-013-0157-x. [DOI] [PubMed] [Google Scholar]
- 2.Marquard K., Westphal L.M., Milki A.A., Lathi R.B. Etiology of recurrent pregnancy loss in women over the age of 35 years. Fertil Steril. 2010;94:1473–1477. doi: 10.1016/j.fertnstert.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 3.Shahine L., Lathi R.B. Embryo selection with preimplantation chromosomal screening in patients with recurrent pregnancy loss. Semin Reprod Med. 2014;32:93–99. doi: 10.1055/s-0033-1363550. [DOI] [PubMed] [Google Scholar]
- 4.Murugappan G., Shahine L.K., Perfetto C.O., Hickok L.R., Lathi R.B. Intent to treat analysis of in vitro fertilization and preimplantation genetic screening versus expectant management in patients with recurrent pregnancy loss. Hum Reprod. 2016;31:1668–1674. doi: 10.1093/humrep/dew135. [DOI] [PubMed] [Google Scholar]
- 5.Gardner D.K., Lane M., Stevens J., Schlenker T., Schoolcraft W.B. Blastocyst score affects implantation and pregnancy outcome: toward a single blastocyst transfer. Fertil Steril. 2000;73:1155–1158. doi: 10.1016/s0015-0282(00)00518-5. [DOI] [PubMed] [Google Scholar]
- 6.Ahlstom A., Westin C., Reismer E., Wikland M., Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod. 2011;26:3289–3296. doi: 10.1093/humrep/der325. [DOI] [PubMed] [Google Scholar]
- 7.Hill M.J., Richter K.S., Heitmann D.O., Graham J.R., Tucker M.J., DeCherney A.H. Trophectoderm grade predicts outcomes of single blastocyst transfers. Fertil Steril. 2013;99:1283–1289. doi: 10.1016/j.fertnstert.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Honnma H., Baba T., Sasaki M., Hashiba Y., Ohno H., Fukunaga T. Trophectoderm morphology significantly affects the rates of ongoing pregnancy and miscarriage in frozen-thawed single-blastocyst transfer cycle in vitro fertilization. Fertil Steril. 2012;98:361–367. doi: 10.1016/j.fertnstert.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Capalbo A., Rienzi L., Cimadomo D., Maggiulli R., Elliott T., Wright G. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;29:1173–1181. doi: 10.1093/humrep/deu033. [DOI] [PubMed] [Google Scholar]
- 10.Irani M., Reichman D., Robles A., Melnick A., Davis O., Zaninovic N. Morphologic grading of euploid blastocysts influences implantation and ongoing pregnancy rates. Fertil Steril. 2017;107:664–670. doi: 10.1016/j.fertnstert.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Y.Y., Yu Y., Zhang X.W. Overall blastocyst quality, trophectoderm grade, and inner cell mass grade predict pregnancy outcome in euploid blastocyst transfer cycles. Chin Med J (Engl) 2018;131:1261–1267. doi: 10.4103/0366-6999.232808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murugappan G., Shahine L., Lathi R.B. Antimullerian hormone is a predictor of live birth in patients with recurrent pregnancy loss. Fertil Res Pract. 2019;5:2. doi: 10.1186/s40738-019-0054-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shahine L., Marshall L., Lamb J.D., Hickok L.R. Higher rates of aneuploidy in blastocysts and higher risk of no embryo transfer in recurrent pregnancy loss patients with diminished ovarian reserve undergoing in vitro fertilization. Fertil Steril. 2016;106:1124–1128. doi: 10.1016/j.fertnstert.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Ogasawara M., Aoki K., Okada S., Suzumori K. Embryonic karyotype of abortuses in relation to the number of previous miscarriages. Fertil Steril. 2000;73:300–304. doi: 10.1016/s0015-0282(99)00495-1. [DOI] [PubMed] [Google Scholar]
- 15.Filho E.S., Noble J.A., Poli M., Griffiths T., Emerson G., Wells D. A method for semi-automatic grading of human blastocyst microscopic images. Hum Reprod. 2012;27:2641–2648. doi: 10.1093/humrep/des219. [DOI] [PubMed] [Google Scholar]
- 16.Paternot G., Devroe J., Debrock S., d’Hooghe T.M., Spiessens C. Intra- and inter-observer analysis in the morphological assessment of early-stage embryos. Reprod Biol Endocrinol. 2009;7:105. doi: 10.1186/1477-7827-7-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Treff N.R., Tao X., Ferry K.M., Su J., Taylor D., Scott R.T., Jr. Development and validation of an accurate quantitative real-time polymerase chain reaction-based assay for human blastocyst comprehensive chromosomal aneuploidy screening. Fertil Steril. 2012;97:819–824. doi: 10.1016/j.fertnstert.2012.01.115. [DOI] [PubMed] [Google Scholar]
- 18.Treff N.R., Krisher R.L., Tao X., Garnsey H., Bohrer C., Silva E. Next generation sequencing-based comprehensive chromosome screening in mouse polar bodies, oocytes, and embryos. Biol Reprod. 2016;94:76. doi: 10.1095/biolreprod.115.135483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Capalbo A., Treff N.R., Cimadomo D., Tao X., Upham K., Ubaldi F.M. Comparison of array comparative genomic hybridization and quantitative realtime PCR-based aneuploidy screening of blastocyst biopsies. Eur J Hum Genet. 2015;23:901–906. doi: 10.1038/ejhg.2014.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Practice Committee of the American Society for Reproductive Medicine The use of preimplantation genetic testing for aneuploidy (PGT-A) Fertil Steril. 2018;109:429–436. doi: 10.1016/j.fertnstert.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 21.Hammond E.R., Cree L.M., Morbeck D.E. Should extended blastocyst culture include cay 7? Hum Reprod. 2019;3:991–997. doi: 10.1093/humrep/dey091. [DOI] [PubMed] [Google Scholar]
- 22.Whitney J.B., Balloch K., Anderson R.E., Nugent N., Schiewe M.C. Day 7 blastocyst euploidy supports routine implementation for cycles using preimplantation genetic testing. JBRA Assist Reprod. 2019;2:45d50. doi: 10.5935/1518-0557.20180089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su Y., Li J.J., Wang C., Haddad G., Wang W.H. Aneuploidy analysis in day 7 human blastocysts produced by in vitro fertilization. Reprod Biol Endocrinol. 2016;14:2. doi: 10.1186/s12958-016-0157-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitney J.B., Anderson R.E., Schiewe M.C. Day 7 blastocyst euploidy and implantation rates warrant implantation for all programs using preimplantation genetic screening (PGS) Fertil Steril. 2016;106:e146. [Google Scholar]