Abstract
Background
Results of cervical cytology screening showing atypical squamous cells of undetermined significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL) indicate risk for high-grade cervical intraepithelial neoplasia (CIN 2 or 3). In a community-based randomized trial we compared the test performance of human papillomavirus (HPV) DNA testing with that of 6-month repeat Papanicolaou (Pap) test in detecting histologically confirmed CIN 2 or 3.
Methods
We randomly assigned 212 women aged 16-50 years with ASCUS or LSIL on cervical cytology screening to undergo either immediate HPV DNA testing or a repeat Pap test in 6 months. Cervical swabs for the HPV DNA testing and the Pap smears were obtained by their familiy physicians. We tested the swabs for oncogenic HPV using the Hybrid Capture II assay (Digene Corp., Beltsville, Md.). Community-based pathologists examined the Pap smears. All women were referred for colposcopy by their family physicians. Two gynecological pathologists assessed the histology findings. We calculated test performance in women who completed the trial using CIN 2 or 3 as the reference standard.
Results
A total of 159 women completed the study. Compared with HPV DNA testing, which detected 87.5% (7/8) of the cases of CIN 2 or 3, repeat Pap smear showing high-grade intraepithelial neoplasia (HSIL) detected 11.1% (1/9) of cases (p = 0.004), and repeat Pap smear showing ASCUS, LSIL or HSIL detected 55.6% (5/9) (p = 0.16). Corresponding specificities were 50.6%, 95.2% (p = 0.002) and 55.6% (p = 0.61). Loss to follow-up was 17.1% in the HPV test group and 32.7% in the repeat Pap group (p = 0.009). Given the 7 cases of CIN 2 or 3 detected by HPV testing and the 5 cases detected by the repeat Pap smear, the incremental cost of HPV testing was calculated to be $3003 per additional case of CIN identified.
Interpretation
HPV DNA testing was more costly but was associated with significantly less loss to follow-up. It may detect more cases of CIN 2 or 3 in women with low-grade cytologic abnormalities.
Atypical squamous cells of undetermined significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL) are detected in 5%-10% of women undergoing cervical cytology screening.1,2 Their management is controversial.1,2,3,4,5 About 30% of these women have low-grade cervical intraepithelial neoplasia (CIN 1);6,7,8,9 although many of these lesions will spontaneously regress,6 about 15%, and perhaps up to 40%, will progress to CIN 2 or 3.7,8,9,10,11,12
Only colposcopy-directed biopsy can definitively identify women with CIN 2 or 3. However, colposcopy services are costly3 and may be overwhelmed if all women with ASCUS or LSIL are referred for examination. Alternatively, the Papanicolaou (Pap) smear may be repeated in 6 months to see whether the low-grade finding persists or high-grade dysplasia is evident. However, a repeat smear may not be sufficiently sensitive for disease detection,13 and delayed testing may result in increased patient anxiety14 and loss to follow-up.11,12
Oncogenic types of human papillomavirus (HPV) are present in over 90% of women with cervical cancer15 and high-grade CIN.16 HPV testing may be useful in identifying high-grade CIN in women with ASCUS or LSIL on cervical cytology screening.8,9,10
There are no randomized trials comparing immediate HPV DNA testing with delayed repeat Pap test for disease detection. Nonrandomized trials have enrolled women from gynecology and colposcopy clinics; referral bias, including high prevalence rates of CIN 2 or 3, prevents generalizing results to settings with lower prevalence rates, such as family practices. We report a randomized clinical trial in which we enrolled women from community-based primary care practices and compared the performance of HPV DNA testing with a repeat Pap test at 6 months in detecting histologically confirmed CIN 2 or 3 in women with low-grade abnormalities on screening Pap test.
Methods
From November 1995 to October 1998 we invited consecutive women aged 16-50 years who had ASCUS or LSIL on cervical cytology screening to participate in the study. They were recruited from 52 community-based family practices and 1 university student health clinic in Ontario. We excluded patients for the following reasons: their family physician felt they would probably not comply with follow-up; they were pregnant; they had no cervix; they had previous diagnosis of high-grade CIN, atypical glandular cells of undetermined significance, glandular dysplasia or cervical cancer; they had previous destructive cervical treatment; they were currently followed with colposcopy; they had vaginal or vulvar neoplasia; they were immunosuppressed; or they currently required uterine body or adnexal surgery. For women who were eligible but declined to participate, we recorded their age, practice site and screening Pap smear findings; we did not record reasons why the women refused to participate. The Research Ethics Board of the Hamilton Health Sciences Corporation, Hamilton, Ont., approved the study design.
Family physicians obtained written informed consent from eligible women. At enrolment each woman completed a self-administered questionnaire on sociodemographic characteristics, reproductive history and sexual behaviour. We then randomly assigned the women to undergo either immediate HPV DNA testing or a repeat Pap test in 6 months. We performed randomization centrally, using a computer-generated random numbers table in blocks of 4, after stratification for ASCUS and LSIL.
For the women in the HPV DNA testing group, immediately after randomization their family physician obtained material from the cervical os and transformation zone with a dacron swab and then placed the swab in transport tubes containing appropriate medium. The physicians referred all of the women for colposcopy; the physicians and the patients were blinded to the HPV test results. The specimens were tested at the McMaster University Regional Virology and Chlamydiology Laboratory using the Hybrid Capture II assay (Digene Corp., Beltsville, Md.). This assay is semi- automated and can detect 13 of the most common oncogenic types of HPV.17
Family physicians asked women assigned to the repeat Pap smear group to return in 6 months, at which time the physician obtained a cervical smear using a modified Ayre spatula with elongated tip. Some physicians also used a cervical brush, if that was their usual practice. Physicians referred all patients for colposcopy, regardless of the cytology results. Participating community laboratories processed the repeat Pap smears, and the laboratory pathologists classified them according to the Bethesda system.1
Colposcopic examinations were performed at the Henderson General Hospital, Hamilton, Ont. Colposcopists took directed biopsy specimens of any areas that appeared abnormal and performed an endocervical curettage if a lesion extended into the endocervical canal, or if the repeat Pap smear showed HSIL or cancer and there was no corresponding colposcopic lesion. If the colposcopist saw no abnormality, or if the criteria for endocervical curettage were not met, the colposcopist did not take any specimens for histological examination. The colposcopists were blinded to the HPV test results. The colposcopic examination was the reference standard for comparing the performance of the HPV test and the repeat Pap smear (sensitivity, specificity and predictive values), and was the designated exit from the study. If the patient did not present for colposcopy, we asked her family physician to remind her to attend.
At study closure we attempted to follow up women who did not present for exit colposcopy. We randomly selected 25% of these women and asked their family physicians whether these women had any subsequent testing or colposcopic examination.
HPV test specimens were stored at 4∘C and shipped to the laboratory at room temperature within 2 weeks of collection. The laboratory, blinded to patient identity and clinical information, performed the Hybrid Capture II assay according to the manufacturer's protocol. DNA from the cervical material was denatured and hybridized with a cocktail of 13 RNA probes to oncogenic HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. Hybrids were captured with alkaline-phosphatase-conjugated antibodies specific to HPV DNA:RNA hybrids. A dioxetane-based chemiluminescent substrate was added, and the resultant relative light units (RLUs) were measured in a luminometer. We designated specimens with RLUs equal to or above the mean RLUs of triplicate positive control specimens containing 1 pg/mL HPV DNA (5000 copies of HPV genome) as positive.
Community-based pathologists read the screening Pap smears for all women and the repeat Pap smears for those assigned to that group. We based study entry and calculation of Pap smear test indices on these pathologists' opinions. We did not submit the smears for consensus review, because this study was designed to mimic usual practice and to obtain generalizable results.
The Department of Pathology at the Henderson General Hospital processed the tissue specimens from the coloposcopy clinic, serially sectioning biopsies at 3 deeper levels. Two expert gynecologic pathologists, blinded to the HPV or repeat Pap test results, independently reviewed all specimens (kappa statistic for CIN 2 or 3 was 0.722). They used CIN terminology; changes consistent with HPV were classified as CIN 1 if no higher degree of dysplasia was present. If a case had multiple biopsies performed, including endocervical curettage, pathologists recorded the most severe diagnosis. For any disagreements in diagnosis the pathologists reviewed findings together and reached a final consensus.
We designated the cervix as normal if exit colposcopy showed no lesion and the colposcopists submitted no specimens for histologic examination, or if tissue was taken for histological examination but showed no CIN or cancer.
We performed an economic evaluation as previously described.18 We calculated costs and procedures associated with colposcopy only for women who had a positive HPV test result or abnormalities on the repeat Pap smear.
We estimated that a sample size of 110 participants per study group would be needed to detect a difference of 15% in the sensitivities of immediate HPV DNA testing and repeat Pap smear showing HSIL in identifying histologically confirmed CIN 2, CIN 3 or carcinoma in tissue obtained at colposcopy (probability of type I error [α] set at 0.05 [two-tailed] and type II error [β] set at 0.20). We assumed the sensitivity of repeat Pap smear with HSIL to be 75%10,19,20 and loss to follow-up to be 10%. We used the χ2 test or Fisher's exact test, when appropriate, to compare categorical variables and the Student's t-test for continuous variables. We analyzed test indices and calculated their exact 95% confidence intervals (CIs), and we analyzed patient characteristics and calculated kappa statistic. All p values are two-tailed. We included all women who underwent exit colposcopy in our analyses. We designated any missing HPV or repeat Pap test results from these women as negative.
Results
A total of 212 women agreed to participate in the study (Fig. 1). Table 1 shows their baseline characteristics. Among the 159 women who completed the trial, characteristics were similar between the 2 groups except that there were fewer women who ever smoked in the HPV test group than in the repeat Pap smear group (47.4% [36/76] v. 69.1% [47/68], p = 0.008). There was no significant association between ever smoking and prevalence of CIN 2 or 3 in the 2 groups at exit (data not shown).
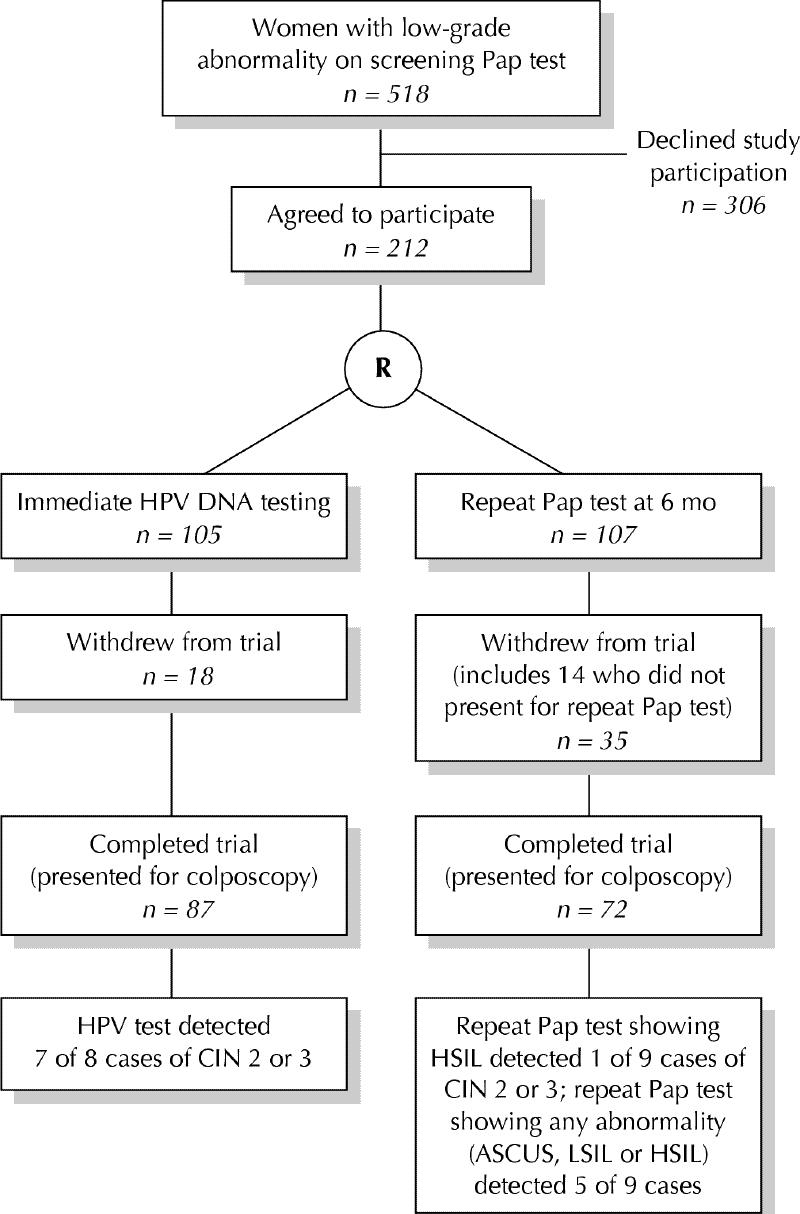
Fig. 1: Profile of trial. R = randomization, HSIL = high-grade squamous intraepithelial lesion, ASCUS = atypical squamous cells of undetermined significance, LSIL = low-grade squamous intraepithelial lesion.
Table 1
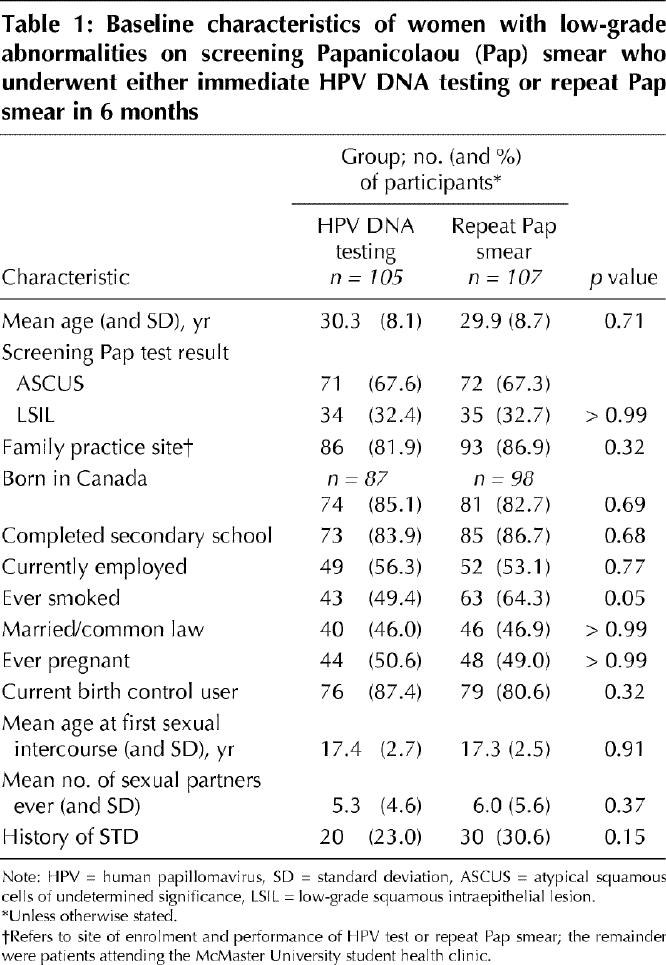
Women who declined entry into the study were similar to the enrolled patients in mean age (p = 0.26), proportion screened in family practice office (p = 0.29) and proportion with screening Pap smear showing ASCUS (p = 0.63).
Cervical swab specimens were obtained from all 105 women assigned to the HPV DNA test group. A swab from 1 woman did not have sufficient material for testing; this woman was included in subsequent analyses and her HPV test result was designated as negative. In total, 54.3% (57/105) of the women were positive for oncogenic HPV.
Of the 107 women assigned to the repeat Pap smear group, 14 (13.1%) did not return for the test. Of those who did present, the specimen from 1 woman was not received by the laboratory and could not be traced, and 2 women presented after the 6 months and were referred immediately for colposcopy without a repeat Pap smear. These 3 women were included in subsequent analyses and their Pap test results were designated as negative. The Pap test results were normal or showed benign cellular changes in 54.8% (51/93), ASCUS or LSIL in 39.8% (37/93) and HSIL in 5.4% (5/93).
Thirty-five (32.7%) of the women in the repeat Pap test group failed to present for colposcopy, which was almost twice the proportion in the HPV test group (17.1% [18/105], p = 0.009). Women who did not present for colposcopy were significantly younger than those who did (mean age 26.6 years [standard deviation (SD) 6.3] v. 31.3 years [SD 8.7], p < 0.001) and less likely to have been born in Canada (56.6% v. 86.8%, p = 0.05). There were no significant differences in other baseline characteristics (data not shown). In the random sample of 25% (n = 14) of the women who withdrew, 1 woman underwent colposcopy elsewhere (no dysplasia detected) and 1 women had a Pap smear that showed ASCUS.
In the HPV test group 46 (52.9%) of the 87 women who presented for colposcopy were HPV positive. Of the 72 women in the repeat Pap test group who presented for colposcopy, 39 (54.2%) had normal results or benign cellular changes, 29 (40.2%) had ASCUS or LSIL, and 4 (5.6%) had HSIL.
Of the 159 women who underwent colposcopy 121 (76.1%) had no cervical abnormality, based either on a normal colposcopic impression or on histologic findings; 21 (13.2%) had CIN 1, and 17 (10.7%) had CIN 2 or 3. None of the women had invasive carcinoma. Overall, 10.1% (11/109) of the women with ASCUS and 12.0% (6/50) of those with LSIL on the screening Pap smear had histologically confirmed CIN 2 or 3.
HPV DNA testing detected 87.5% of the cases of histologically confirmed CIN 2 or 3 (95% CI 47.4%-99.7%). Repeat Pap smear showing HSIL detected significantly fewer of these cases than HPV DNA testing (11%; 95% CI 0.3%-48.3%) (p = 0.004). If repeat Pap smear showed ASCUS, LSIL or HSIL, it detected 55.6% of the cases of histologically confirmed CIN 2 or 3 (95% CI 21.1%-86.3%) (Table 2); although the sensitivity of the repeat Pap smear showing ASCUS, LSIL or HSIL was not significantly different from that of the HPV DNA testing, there was a trend (p = 0.16) favouring the sensitivity of the latter test. The specificity of the repeat Pap smear showing ASCUS, LSIL or HSIL, and its positive and negative predictive values, did not differ significantly from those of HPV DNA testing. Results were similar for comparisons of test indices among women with repeat Pap smears showing ASCUS and LSIL (data not shown).
Table 2
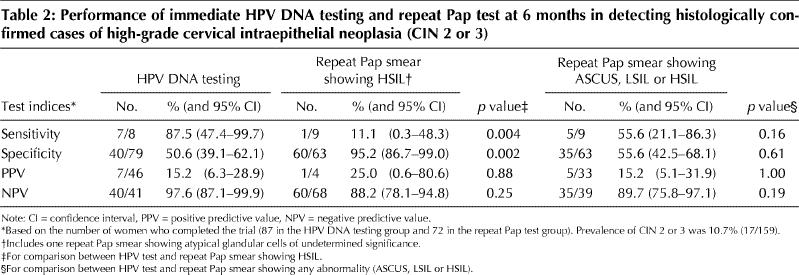
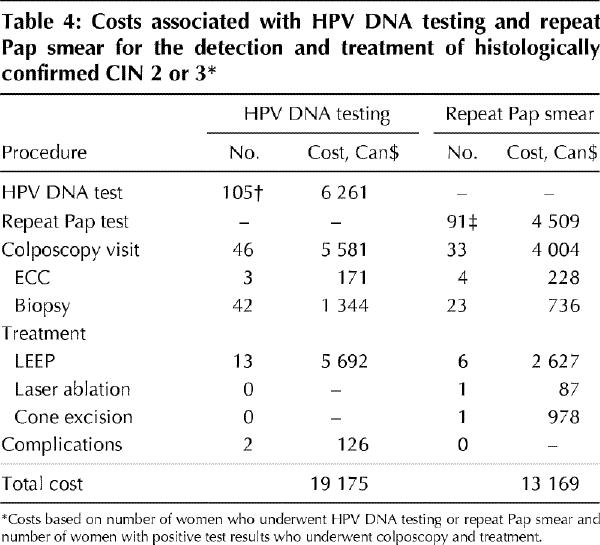
Table 3 shows the costs of the procedures, and Table 4 shows the number of procedures and costs accrued by each study group. Given the poor performance of the repeat Pap smear with HSIL in detecting CIN 2 or 3, practitioners may not be willing to accept this strategy into clinical practice, and so we did not feel that it would be useful to determine the cost of this strategy. The literature advocates referral for colposcopy if low-grade abnormalities are present on repeat Pap smear,3 and so we based the figures in Table 4 on the referral of patients whose repeat smear showed ASCUS, LSIL or HSIL. Given the point estimates of 5 cases of CIN 2 or 3 detected by repeat Pap smear and 7 detected by HPV DNA testing, the incremental cost of HPV DNA testing was calculated to be $3003 per additional case of CIN 2 or 3 detected ([$19 175 - $13 169] ÷ [7 - 5]).
Table 3
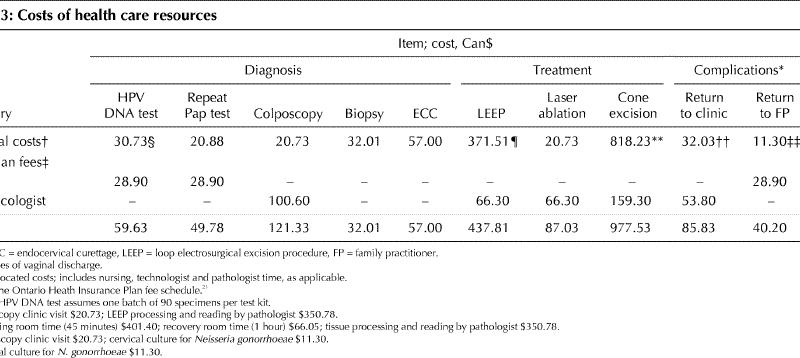
Table 4
Interpretation
This is the first randomized controlled trial to compare the performance of cervical HPV DNA testing and delayed repeat Pap test in detecting high-grade cervical cancer precursors in women whose screening Pap smear showed low-grade abnormalities (ASCUS or LSIL). It is a pragmatic management trial, with women recruited from, and managed in, primary care practices. Consequently, the results of this trial are more generalizable to a primary care setting than those obtained in a colposcopy referral population.
Our study showed that immediate testing for oncogenic HPV detected significantly more histologically confirmed cases of CIN 2 or 3 than did repeat Pap smear showing HSIL performed at 6 months. Our results also suggested that more cases of CIN 2 or 3 are identified if women are referred for colposcopy on the basis of positive immediate HPV testing than if referral is dependent on finding ASCUS, LSIL or HSIL on the delayed repeat Pap smear. This difference did not reach statistical significance; however, this may have been due to inadequate power associated with loss to follow-up and the size of the sample. The data also suggested that the possible improved sensitivity of immediate HPV DNA testing compared with repeat Pap smear showing ASCUS, LSIL or HSIL was not associated with a substantial reduction in specificity.
Among the 159 women who completed the trial, the proportion who ever smoked was higher in the repeat Pap smear group than in the HPV testing group. However, since we found no association in our data between ever smoking and the prevalence of CIN 2 or 3 at exit colposcopy, it is unlikely that the distribution of this baseline characteristic affected test performance.
It may be argued that our test comparisons are not fair because the Pap test results were based, not on central review, but on reports by community pathologists. As well, we did not instruct family physicians to use a cervical brush in addition to the Ayre spatula every time they obtained the repeat Pap smear. This methodology was used purposely because the study was designed to reflect actual community practice.
Only one previous study,8 which was not randomized, compared HPV testing by Hybrid Capture II assay and repeat Pap test in women with low-grade abnormalities on screening Pap smear. Women who had undergone routine cervical cytology screening in gynecology clinics and whose Pap test results showed ASCUS were recruited, and their immediate HPV test results were compared with Pap test results obtained at colposcopy clinic 2-3 months later. This study suggested that HPV testing was able to detect more cases of CIN 2 or 3 than the repeat Pap test showing ASCUS, LSIL or HSIL.
We performed our cost-effectiveness analysis assuming that HPV testing detects more cases of CIN 2 or 3 than repeat Pap test. Based on local Ontario practices and costs, HPV testing was more costly than delayed Pap test. Whether the cost of HPV testing of $3003 per additional case of CIN 2 or 3 detected is an acceptable expenditure depends on the weighing of opportunity costs.22,23 In addition, the cost of HPV testing may be higher or lower than our estimate, depending on local conditions in different provinces and territories.
We did not evaluate the cost of missing cases of CIN 2 or 3. The proportion of undetected cases that progress to invasive cervical cancer is unclear, with estimates ranging from 10% to 40%.24 We also do not know what proportion of cases of CIN 2 or 3 may be detected on future investigations, including Pap smear. However, if sufficient numbers of cases of invasive cancer are prevented through improved detection of high-grade CIN, then more costly tests may become affordable because of money saved from invasive cancer management.
The large number of women who failed to present for colposcopy is worrisome. Random sampling indicated that most of these women did not undergo subsequent colposcopy or Pap test. The high rate of noncompliance occurred despite the fact that most of the women (84.4%) were part of stable family practices, that we recruited women judged most likely to comply with management and that attempts were made to ensure attendance at the colposcopy clinic. Women who did not present for colposcopy were younger and were less likely to have been born in Canada than those who did present. A previous study in the United States suggested that acculturation, including the proportion of life lived in the United States, may affect adherence to follow-up among women with abnormal Pap test results.25 Factors associated with age and acculturation that influence compliance, and that may be modifiable, need to be elucidated. However, one potentially distinct and modifiable factor is waiting time for further investigations. Our study clearly showed that, if women had to wait 6 months for an additional investigation and subsequent colposcopy, default from colposcopy increased. Previous studies have also noted decreased compliance among women with abnormal screening Pap test results as management time was prolonged.11,12
In summary, relying on the detection of HSIL on repeat Pap smear to identify cases of CIN 2 or 3 may not represent optimal management for women with low-grade abnormalities on screening Pap smear. It has been recommended that colposcopy may be delayed for 2 years if repeat Pap smears show a low-grade abnormality or that it be delayed until a cervical smear shows HSIL.5 This management strategy may effectively detect cases of CIN 2 or 3 and may be safe;26 however, loss to follow-up may limit its success. Similarly, basing referral for colposcopy on finding any abnormality (ASCUS, LSIL or HSIL) on 6-month repeat Pap smear may be unsuccessful because of nonadherence to follow-up. Immediate HPV DNA testing offers the advantage of quicker triage, and our results suggest that it may be more sensitive for detecting CIN 2 or 3 than delayed repeat Pap smear showing ASCUS, LSIL or HSIL.
Terminology .
Cytology
ASCUS Atypical squamous cells of undetermined significance. Refers to cells on Pap smear having an appearance approaching, but not sufficient for, either a low- or high-grade squamous intraepithelial lesion. Most Pap smears with ASCUS represent reactive cervical changes.
LSIL Low-grade squamous intraepithelial lesion.
HSIL High-grade squamous intraepithelial lesion.
AGUS Atypical glandular cells of undetermined significance. Refers to cells having an appearance approaching, but uncertain for, glandular adenocarcinoma.
Histology
CIN Cervical intraepithelial neoplasia.
CIN 2 and 3 Considered high-grade intraepithelial neoplastic lesions because of their potential to progress to invasive cancer. In other terminology, CIN 2 corresponds to moderate squamous dysplasia and CIN 3 to severe squamous dysplasia and squamous carcinoma in situ.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Dr. Charles Goldsmith, Department of Clinical Epidemiology and Biostatistics, McMaster University, for his help with the statistical analyses, Marg Pauls and Linda Hardcastle for overall study management, Joan Randazzo for colposcopy clinic study management and Sylvia Chong for performing the HPV Hybrid Capture II assays. We also thank the many patients who participated in this study. We gratefully acknowledge the assistance of MDS Laboratories Ontario and Gamma-Dynacare Laboratories.
This research was supported by grant 95-32 from the Physicians' Services Incorporated Foundation. Hybrid Capture II assay kits and use of a luminometer were provided free of charge by Digene Corporation.
Reprint requests to: Dr. Alice Lytwyn, Department of Pathology, Sunnybrook & Women's College Health Sciences Centre, Women's College Campus, 76 Grenville St., Toronto ON M5S 1B2; fax 416 323-6116; alice.lytwyn@swchsc.on.ca
References
- 1.Kurman RJ, Solomon D. The Bethesda system for reporting cervical/vaginal cytologic diagnoses. New York: Springer-Verlag; 1994.
- 2.CDC surveillance summary. Trends in cancer screening — United States, 1987 and 1992. MMWR 1995;45:57-61. [PubMed]
- 3.Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH. Interim guidelines for management of abnormal cervical cytology. JAMA 1994;271:1866-9. [PubMed]
- 4.Austoker J. Screening for cervical cancer. BMJ 1994;309:241-8. [DOI] [PMC free article] [PubMed]
- 5.Miller AB, Anderson G, Brisson J, Laidlaw J, Le Pitre N, Malcolmson P, et al. Report of a National Workshop on Screening for Cancer of the Cervix. CMAJ 1991;145(10):1301-25. [PMC free article] [PubMed]
- 6.Surjanen KJ. Spontaneous evolution of intraepithelial lesions according to the grade and type of the implicated human papillomavirus (HPV). Eur J Obstet Gynecol Reprod Biol 1996;65:45-53. [DOI] [PubMed]
- 7.Ferris DG, Wright TC, Litaker MS, Richart RM, Lorincz AT, Sun XW, et al. Triage of women with ASCUS and LSIL on Pap smear reports: management by repeat Pap smear, HPV DNA testing or colposcopy? J Fam Pract 1998;46:125-34. [PubMed]
- 8.Manos MM, Kinney WK, Hurley LB, Sherman ME, Shieh-Ngai J, Kurman RJ, et al. Identifying women with cervical neoplasia. Using human papillomavirus DNA testing for equivocal Papanicolaou results. JAMA 1999;218:1605-10. [DOI] [PubMed]
- 9.Wright TC, Sun WX, Koulos J. Comparison of management algorithms for the evaluation of women with low-grade cytologic abnormalities. Obstet Gynecol 1995;85:202-10. [DOI] [PubMed]
- 10.Cox JT, Lorincz AT, Schiffman MH, Sherman ME, Cullen A, Kurman RJ. Human papillomavirus testing by hybrid capture appears to be useful in triaging women with a cytologic diagnosis of atypical squamous cells of undetermined significance. Am J Obstet Gynecol 1995;172:946-54. [DOI] [PubMed]
- 11.Flannelly G, Anderson D, Kitchener HC, Mann EMF, Campbell M, Fisher P, et al. Management of women with mild and moderate cervical dyskaryosis. BMJ 1994;308:1399-403. [DOI] [PMC free article] [PubMed]
- 12.Cruickshank ME, Buchan S, Melvin WT, Kitchener HC. Human papillomavirus type 16 and 18 detection in the management of mild dyskaryosis. Br J Obstet Gynaecol 1999;106:969-76. [DOI] [PubMed]
- 13.Cruickshank ME, Kitchener HC. Towards optimal management of the mildly abnormal smear. Curr Opin Obstet Gynecol 1995;7:20-3. [PubMed]
- 14.Peters T, Somerset M, Baxter K, Wilkinson C. Anxiety among women with mild dyskaryosis: a randomized trial of an educational intervention. Br J Gen Pract 1999;49:348-52. [PMC free article] [PubMed]
- 15.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:12-9. [DOI] [PubMed]
- 16.Lungu O, Sun XW, Wright TC, Ferenczy A, Richart RM, Silverstein S. A polymerase chain reaction-enzyme-linked immunosorbent assay method for detecting human papillomavirus in cervical carcinoma and high grade cervical cancer precursors. Obstet Gynecol 1995;85:337-42. [DOI] [PubMed]
- 17.Peyton CL, Schiffman MH, Lorincz At, Hunt WC, Mielzynska I, Bratti C, et al. Comparison of PCR- and hybrid capture-based human papillomavirus detection systems using multiple cervical specimen collection strategies. J Clin Microbiol 1998;36:3248-54. [DOI] [PMC free article] [PubMed]
- 18.Lytywn A, Gafni A, Sellors JW, Goeree R, Randazzo J, Mahony JB, et al. Economic evaluation of hybrid capture human papillomavirus testing in women with low-grade Papanicolaou smear abnormalities. J Lower Genital Tract Dis 1998;2:213-20. [DOI] [PubMed]
- 19.Giles JA, Deery A, Crow J, Walker P. The accuracy of repeat cytology in women with mildly dyskaryotic smears. Br J Obstet Gynaecol 1988;96:1067-70. [DOI] [PubMed]
- 20.Slawson DC, Bennett JH, Herman JM. Follow-up Papanicolaou smear of cervical atypia: Are we missing significant disease? A HARNET Study. J Fam Pract 1993;36:289-93. [PubMed]
- 21.Ontario Ministry of Health. Schedule of benefits, physician services under the Health Insurance Act. Toronto: The Ministry; 1992.
- 22.Birch S, Gafni.A. Cost-effectiveness/utility analyses: Do current decision rules lead us to where we want to be? J Health Econ 1992;11:279-96. [DOI] [PubMed]
- 23.Birch S, Gafni A. Cost-effectiveness ratios: in a league of their own. Health Policy 1994;28:133-41. [DOI] [PubMed]
- 24.Mitchell MF, Tortolero-Luna G, Wright T, Sarkar A, Richards-Kortum R, Hong WK, et al. Cervical human papillomavirus infection and intraepithelial neoplasia: a review. J Natl Cancer Inst Monogr 1996;21:17-25. [PubMed]
- 25.Crane LA. Social support and adherence behavior among women with abnormal Pap smears. J Cancer Educ 1996;11:164-7. [DOI] [PubMed]
- 26.Jones MH, Jenkins D, Cuzick J, Wolfendale MR, Jones JJ, Balogun-Lynch C, et al. Mild cervical dyskaryosis: safety of cytological surveillance. Lancet 1992;339:1440-3. [DOI] [PubMed]


