To the Editor:
We report a case of central retinal vein occlusion (CRVO) in the setting of symptomatic coronavirus disease 2019 (COVID-19) infection in an otherwise healthy adult male.
Case report
A 39-year-old male with no past medical or ocular history developed a fever in the Dominican Republic. The following day, the patient traveled back to the United States and tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by reverse transcriptase polymerase chain reaction (RT-PCR) assay. A week after the positive test, the patient developed decreased vision and floaters in the right eye and was referred for retinal exam 1 month later.
On initial presentation, visual acuity was 20/150 in the right eye (OD) and 20/30 in the left eye (OS). Pupils were equal, round, and reactive to light, and intraocular pressures were 16 mmHg OD and 17 mmHg OS. Slit lamp biomicroscopy of the anterior segment was normal except for nasal pterygia in both eyes. Dilated fundus examination OD revealed a hyperemic optic nerve head, macular thickening, tortuous vasculature, and diffusely scattered intraretinal hemorrhages (Fig. 1a). Fluorescein angiography OD showed tortuous vasculature and vessel wall staining without neovascularization, leakage, or areas of non-perfusion (Fig. 1b). Optical coherence tomography OD demonstrated cystoid macular edema (CME) (Fig. 2a). Fundus exam and ancillary testing OS were unremarkable.
Fig. 1.
a Color fundus photograph OD showing a hyperemic optic nerve head, macular thickening, vascular tortuosity, and diffuse intraretinal hemorrhages. b Late-phase fluorescein angiogram OD demonstrating vascular tortuosity and vessel wall staining without capillary non-perfusion
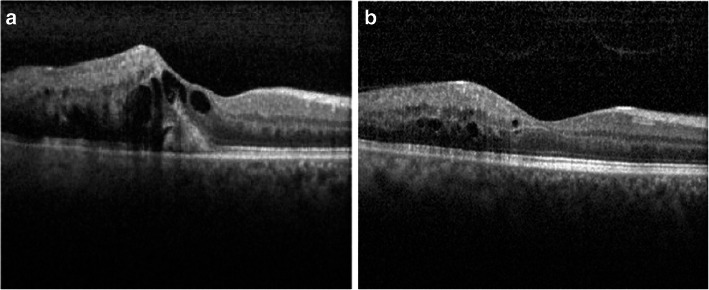
Fig. 2.
a Optical coherence tomography (OCT) OD showing CME on initial presentation. b OCT OD showing improvement of CME after intravitreal injection of bevacizumab
Diagnostic workup, including blood pressure, complete blood count, glucose level, QuantiFERON Gold, anti-Treponemal IgG and IgM antibodies, antinuclear antibodies, anti-double stranded DNA antibodies, angiotensin converting enzyme, rheumatoid factor, homocysteine, C-reactive protein, erythrocyte sedimentation rate, and thrombophilia panel, were unremarkable. The patient was treated with intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections of bevacizumab. After a series of injections, the macular edema decreased significantly and the patient’s visual acuity improved to 20/30 OD (Fig. 2b).
Discussion
COVID-19-associated coagulopathy has been documented and studied since the onset of the pandemic [1]. Autopsy findings of patients with severe COVID-19 infection have demonstrated a hallmark diffuse small vessel thrombosis thought to be caused by complement-mediated microvascular injury, with platelet-fibrin microthrombi regularly found in venules, arterioles, and capillaries [2]. In addition, affinity of SARS-CoV-2 for vascular endothelial cell angiotensin-converting enzyme-2 (ACE2) receptors has been shown to activate apoptotic pathway signaling and prothrombotic cascades [3].
Hypercoagulability is a major risk factor for CRVO, and it is imperative to rule out other causes of CRVO in an otherwise healthy patient. Our patient did not have any significant medical history and infectious, inflammatory, and hypercoagulable studies were negative. There have only been a small number of cases of COVID-19-associated CRVO in recent literature [4–6]. Our patient’s positive RT-PCR SARS-CoV-2 assay and subsequent visual symptoms support the possibility that the pro-thrombotic state created by COVID-19 contributed to the development of CRVO.
This case builds upon the existing literature that demonstrates the occurrence of CRVO in the setting of COVID-19. Patients with COVID-19 are at risk for vascular occlusive events, and early detection and treatment are paramount in restoring visual function.
Acknowledgements
Not applicable.
Abbreviations
- CRVO
Central retinal vein occlusion
- COVID-19
Coronavirus disease 2019
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- RT-PCR
Reverse transcriptase polymerase chain reaction
- OD
Right eye
- OS
Left eye
- Anti-VEGF
Anti-vascular endothelial growth factor
- ACE2
Angiotensin-converting enzyme-2
Authors’ contributions
AD and JL worked together to diagnose the patient, and JL provided treatment for the patient with regular follow-up. NR compiled the images and was primary author of the case report. All authors read and approved the final manuscript.
Funding
This research is supported by gifts from Lewis Henkind, as well as the Irving and Branna Sisenwein Endowment Fund to the Department of Ophthalmology, Montefiore Medical Center.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheth JU, Narayanan R, Goyal J, Goyal V. Retinal vein occlusion in COVID-19: a novel entity. Indian J Ophthalmol. 2020;68:2291–2293. doi: 10.4103/ijo.IJO_2380_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Invernizzi A, Pellegrini M, Messenio D, et al. Impending central retinal vein occlusion in a patient with coronavirus disease 2019 (COVID-19) Ocul Immunol Inflamm. 2019;28(8):1290–1292. doi: 10.1080/09273948.2020.1807023. [DOI] [PubMed] [Google Scholar]
- 6.Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central retinal vein occlusion in a young healthy COVID-19 patient: a case report. Am J Ophthalmol Case Rep. 2020;20:100992. doi: 10.1016/j.ajoc.2020.100992. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.