Abstract
Background
Skull fractures are commonly seen after both accidental and nonaccidental head injuries in young children. A history of recent trauma may be lacking in either an accidental or nonaccidental head injury event. Furthermore, skull fractures do not offer an indication of the stage of healing on radiologic studies because they do not heal with callus formation as seen with long bone fractures. Thus, a better understanding on the timing of skull fracture resolution may provide guidance on the medical evaluation for accidental or nonaccidental head injury.
Objective
The aim of the study was to determine the time required for radiographic skull fracture resolution in children younger than 24 months.
Methods
This was a retrospective observational analysis of children younger than 24 months referred with skull fractures between January 2008 and December 2012. Analysis included children with accidental head injuries with a known time interval since injury and a negative skeletal survey who underwent serial radiographic studies. Complete healing of a skull fracture was defined as resolution of fracture lucency by radiograph.
Results
Of the 26 children who met inclusion criteria, 11 (42.3%) demonstrated resolution of skull fracture(s) on follow-up imaging. Fracture resolution on radiologic studies ranged from 2 to 18 weeks. Twelve fractures in 10 children demonstrated fracture resolution at 10 or more weeks after injury.
Conclusions
Healing or resolution of a skull fracture can take months in children younger than 24 months. With the high variability in skull fracture presentation and large window to fracture resolution, unexplained or multiple skull fractures in children younger than 24 months may be the result of a single or multiple events of head trauma.
Key Words: child abuse, skeletal survey, skull fracture, fracture healing
Epidemiologic studies on child maltreatment have shown that children younger than 2 years have high rates of both nonaccidental head trauma1 and serious physical abuse.2 The rate of nonaccidental head trauma in infants is more than twice the rate of young children between the ages of 1 and 3 years.1,2 However, in a study using a US database of hospitalized children, almost all cases of skull fracture were attributable to accidental falls, especially in infants younger than 12 months.3 Infants are more likely to have skull fractures than toddlers after falls regardless of fall height.4,5 Although skull fractures are more commonly identified after accidental falls than nonaccidental head trauma,6 the linear parietal skull fracture is the most common fracture type identified in both types of trauma in children younger than 2 years.7,8 In the clinical setting, a skull fracture may be identified in a young child who presents when scalp swelling is observed by a caregiver without a reported history of head trauma. Likewise, a young child may have more than 1 skull fracture identified. In these scenarios, the diagnostic dilemma may lie in how to interpret the skull fracture(s) in the context of the child's age and development without a clear timeline of injury and whether to initiate an age-appropriate evaluation for nonaccidental trauma.
A comprehensive medical history and physical examination are important in the determination of accidental versus nonaccidental head trauma. This history includes the mechanism of injury (details of the injury event), the child's developmental abilities, and whether the injury event was witnessed. Although most childhood fractures occur from a reported fall,9,10 a fall is also the most common history of injury provided in cases of nonaccidental head trauma.11,12 Identification of other injuries such as scalp swelling, abrasions, bruises, and oral trauma add to the understanding of the mechanism and timing of injury. When scalp swelling is noted on initial examination and/or radiologic studies with an injury, it can aid in the assessment of the timing of the injury.13 However, approximately 10% of children with skull fractures have no clinically appreciable or radiographic evidence of scalp or facial soft tissue swelling at the time of presentation.4,14 The presence or absence of signs of skeletal healing on radiographic study may be useful in the assessment of injury timing. Although there are studies on the radiologic healing of long bone fractures in children15–20 and clavicular birth injuries,21 there are no published studies on the healing of skull fractures. Furthermore, the mechanism of healing differs between long bones and bones of the calvarium, thus studies of long bone healing do not translate to skull fractures.22 Our objective was to determine the time to radiologic fracture resolution in children younger than 24 months presenting with skull fracture(s).
METHODS
This was a retrospective, single-center study conducted at a tertiary pediatric hospital with a multidisciplinary child abuse program that included subspecialty trained child abuse physicians, social workers, pediatric radiology, and neuroradiology. The study was approved by the hospital's institutional review board. Data were extracted from the child abuse program database on cases of children younger than 24 months with skull fractures who were evaluated between January 1, 2008, and December 31, 2012. These children were referred to the child abuse program either because the skull fracture occurred in an infant younger than 12 months or because the referring emergency department (ED) physician had a concern for child abuse or neglect. As part of the consultation for head injury, the child abuse program completed safety education and psychosocial assessments as well as comprehensive consultations by child abuse physicians if indicated. Inclusion criteria were as follows: (1) younger than 24 months, (2) identified skull fracture(s), (3) caregiver provided a history of recent head trauma, (4) known time of injury, (5) no additional fractures on skeletal survey, and (6) completion of follow-up skull radiographs.
Radiologic imaging at the time of ED presentation was at the discretion of the ED physician with all children initially imaged by head computed tomography (CT) with 3-dimensional (3D) reconstruction. Other radiologic studies ordered at the time of initial presentation included skull radiographs (before head CT) and skeletal surveys (after identification of a skull fracture) in some children. The need for additional follow-up imaging was determined clinically, for example, to evaluate for leptomeningeal cyst formation as recommended by neurosurgery. Follow-up imaging included 2 view skull radiographs (frontal and lateral) offered at 2 to 3 weeks (in conjunction with a follow-up skeletal survey) and several months after initial injury. Follow-up skeletal surveys still included skull radiographs as the timing of this study overlapped the American College of Radiology recommendation for elimination of skull radiographs from the follow-up skeletal survey.23 Follow-up skeletal surveys were recommended but not required in infants younger than 1 year with isolated skull fractures at the time of this study. Accidental head injury was defined as a child presenting with a history of witnessed accidental injury (such as a fall) occurring in the absence of additional concerning injuries such as nonscalp cutaneous trauma (bruising), oral trauma, or skeletal injury.
Data that were extracted included the child's age in months, sex, ethnicity (Hispanic or non-Hispanic), race, maternal age, instrumentation used, and mode of delivery (as rarely skull fractures can occur with instrumented deliveries24,25 and the length of time for a birth skull fracture to heal is unpublished), date of presentation to the ED and consultation with child abuse physician, fall history, fall height, floor surface, location of skull fracture (calvarial), type of fracture (simple vs complex), associated soft tissue swelling on clinical examination and radiography, type of radiologic study completed, and radiologic findings on follow-up skull radiographs. A simple skull fracture was defined as single and linear, whereas complex fractures were defined as being multiple, bilateral, diastatic, depressed, or stellate.26 The presence or absence and resolution of skull fractures were based on the official reading of pediatric radiologists. Complete healing of the skull fracture was defined as resolution of the fracture lucency by skull radiograph. Fracture length and width during follow-up imaging were not measured. A child abuse physician reviewed all imaging with the pediatric radiologists at the time of the initial consultation and follow-up. Timing of radiographically demonstrated fracture resolution was determined in weeks. The time interval between initial injury and the fracture resolution on skull radiograph was rounded to the nearest week. Descriptive statistics were used in analysis.
RESULTS
After reviewing data on 106 children evaluated by the child abuse program between January 1, 2008, and December 31, 2012, 26 children were eligible for inclusion in the study. Figure 1 shows the study subject flow chart. The median age of the children was 7 months with a range of 0 to 18 months. The study population was 80.8% Hispanic, consistent with the population of the region, and 46.2% of the children were male. Most children (69.2%) were born by vaginal delivery without instrumentation (Table 1). A child abuse physician evaluated 50% of the children within 24 hours and 69.2% within 48 hours of injury. The remainder were seen more than 48 hours after injury as the discovery of scalp swelling was noted days after the occurrence of a fall. Per inclusion criteria, all children had a skeletal survey on presentation. All children were scheduled for a complete follow-up skeletal survey at 2 weeks. However, 9 children (34.6%) did not complete a follow-up skeletal survey at 2 weeks (eg, cancellations, no-shows, rescheduling, caregiver preference to limit imaging to skull views) but did return later for follow-up skull imaging.
FIGURE 1.
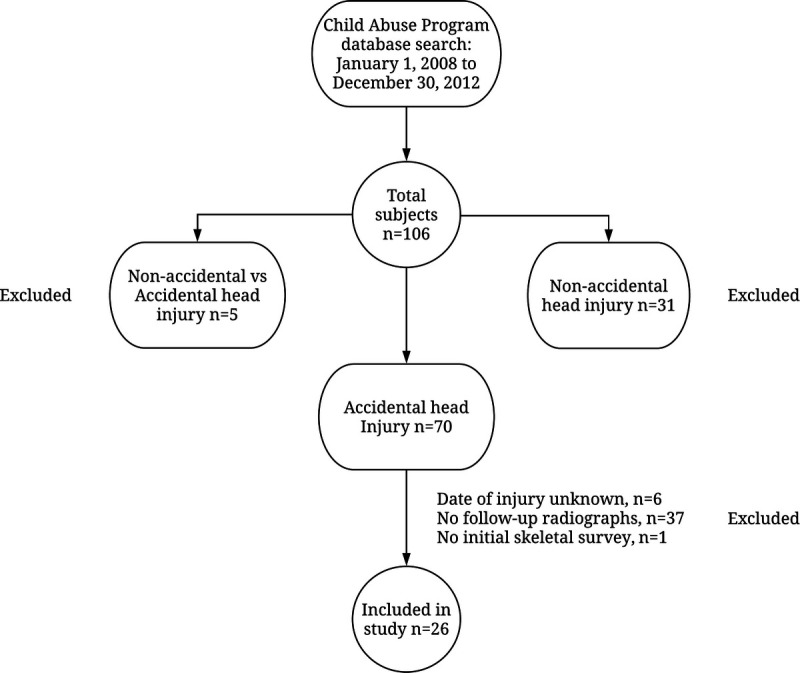
Flow chart of subject selection.
TABLE 1.
Population Demographics
| Subjects (N = 26), n (%) | |
|---|---|
| Sex | |
| Male | 12 (46.2) |
| Female | 14 (53.8) |
| Age, mo | |
| 0–3 | 8 (30.7) |
| 4–6 | 1 (3.8) |
| 7–9 | 7 (26.9) |
| 10–12 | 9 (34.6) |
| >12 | 1 (3.8) |
| Ethnicity | |
| Hispanic | 21 (80.8) |
| Non-Hispanic | 5 (19.2) |
| Race | |
| White | 19 (73.1) |
| Black | 1 (3.8) |
| Others | 4 (15.4) |
| No data | 2 (7.7) |
| Mode of delivery | |
| Vaginal | 17 (65.4) |
| Vaginal with instrumentation (forceps) | 1 (3.8) |
| C-section | 6 (23.1) |
| No data | 2 (7.7) |
| Fall heights | |
| Unknown | 7 (26.9) |
| <3 ft | 12 (46.2) |
| 3–6 ft | 7 (26.9) |
| Floor surface | |
| Tile/concrete | 10 (38.5) |
| Other surface flooring/concrete | 4 (15.4) |
| Carpet/concrete | 1 (3.8) |
| Tile | 2 (7.7) |
| Dirt | 1 (3.8) |
| Wood | 3 (11.5) |
| Concrete | 2 (7.7) |
| Unknown | 3 (11.5) |
An estimated fall height was available for 19 children (73.1%), 12 (46.2%) with an estimated fall height less than 3 feet and 7 (26.9%) between 3 and 6 feet. Most falls (17 children or 65.4%) occurred onto a surface involving concrete (uncovered or with an overlying surface such as linoleum). Simple and complex skull fractures were seen with both fall heights, but 60% of the complex skull fractures occurred between 3 and 6 feet (Table 2).
TABLE 2.
Comparison of Fall Heights to Type of Fracture and Surface
| <3 ft, n (%) | 3–6 ft, n (%) | Unknown Height, n (%) | |
|---|---|---|---|
| No. patients | 12 (46.2) | 7 (26.9) | 7 (26.9) |
| Simple fractures | 11 (42.3) | 4 (15.4) | 6 (23.1) |
| Complex fractures | 1 (3.8) | 3 (11.5) | 1 (3.8) |
| Concrete surface | 1 (3.8) | 0 | 1 (3.8) |
| Tile/concrete surface | 5 (19.2) | 2 (7.7) | 3 (15.4) |
| Carpet/concrete surface | 1 (3.8) | 0 | 0 |
| Other/concrete surface | 2 (7.7) | 2 (7.7) | 0 |
| Tile surface | 0 | 1 (3.8) | 1 (3.8) |
| Dirt surface | 0 | 1 (3.8) | 0 |
| Wood surface | 2 (7.7) | 1 (3.8) | 0 |
| Unknown surface | 1 (3.8) | 0 | 2 (7.7) |
N = 26.
There were 31 skull fractures that occurred in 26 children. Simple fractures were noted in 21 children (80.8%) whereas complex fractures occurred in 5 children (19.2%). Four (80%) of the 5 complex skull fractures were bilateral parietal fractures with 1 child having a complex fracture of the parietal and occipital bones. Of the simple fractures, 14 (66.7%) were found on the right side and 7 (33.3%) on the left. The parietal bone was affected in 22 fractures (71%), followed by the occipital bone with 4 fractures (12.9%), and the frontal bone with 1 fracture (3.2%). No temporal bone fractures were seen in our study. Two children (7.7%) did not have associated soft tissue swelling on clinical examination or radiography. Twenty-five children (96.1%) had initial neuroimaging, which included 3D head CT. Eleven children (42.3%) had intracranial bleeds on CT—10 extra-axial hemorrhages and 1 cortical hemorrhage. All intracranial hemorrhages were small, focal, and associated with the fracture area.
Of the 26 children with 31 skull fractures, skull fracture resolution occurred for 13 fractures (41.9%) from 11 children (42.3%) on follow-up imaging. The radiologic studies demonstrating fracture resolution ranged from 2 to 18 weeks, as 1 child demonstrated resolution of a frontal bone fracture on the initial 2-week follow-up skeletal survey. Ten children (38.5%) received only follow-up imaging at 2 to 3 weeks after injury with 9 of these children still demonstrating the presence of a fracture on imaging. Therefore, the follow-up imaging at 2 to 3 weeks demonstrated persistence of skull fracture(s) in 90% of these studies. The remaining 16 children (61.5%) with 20 fractures returned for additional imaging beyond the follow-up skeletal survey. Twelve fractures in 10 children demonstrated fracture resolution on follow-up imaging between 9 and 18 weeks after injury. One child with a bilateral skull fracture did not have resolution of one side of the fracture at a final imaging visit at 18 weeks. Eight fractures in the remaining 6 children did not demonstrate fracture resolution when imaged between 9 and 18 weeks after injury.
DISCUSSION
These results are particularly valuable because there are no published studies on the “healing” of skull fractures. Dating of skull fractures has been limited to the presence or absence of scalp swelling indicating a more recent injury, whereas the absence of scalp swelling is not helpful in timing. It is notable that there is high variability in the presentation of skull fractures with both simple and complex skull fractures (eg, bilateral skull fractures) occurring in falls of less than 3 feet in this study population. The small number of complex skull fractures in this series limits further analysis. However, in a case-control study of the biomechanical characteristics of falls in children, no association was seen between fall height and the presence of simple or complex skull fractures.5 Although it is difficult to date head injuries and fractures in children, determining a window of injury may be helpful in cases where the history is unclear, the history includes multiple falls or injury events, or when multiple fractures are present. This study provides some initial data to aid in that process. Although most children in this case series had scalp swelling at the time of presentation supporting a recent injury, soft tissue swelling was not present in all children. There were children without fracture resolution at follow-up visits between 9 and 18 weeks after injury. In those children that did demonstrate healing, fracture resolution largely occurred 10 or more weeks after injury. Therefore, a skull fracture that presents without soft tissue swelling may be a recent injury or may represent a prior head injury event. In addition, with the large window to fracture resolution, unexplained or multiple skull fractures in children younger than 24 months may be the result of a single or multiple events of head trauma.
This study used a child abuse program database for data extraction. Every child received a multidisciplinary evaluation by the child abuse program team including psychosocial assessment and additional medical evaluation including skeletal survey and neuroimaging with 3D head CT in all children. This study has limitations as the population included in this study is a subset of the pediatric population with skull fractures, which represents a risk for selection bias. These children were referred to the child abuse physician either because they were infants younger than 12 months and sustained a skull fracture, or the referring ED physician had a suspicion for nonaccidental head trauma in a child older than 12 months. This suspicion for nonaccidental trauma by the ED physician may have been based on the examination findings such as absence of scalp swelling, presence of additional bruises, presence of a complex skull fracture, or psychosocial risk factors such as prior involvement with child protective services. Despite the initial concern for nonaccidental head trauma in some referrals, all of the children in the study had a history of witnessed accidental injury (such as a fall) occurring in the absence of additional concerning injuries such as nonscalp cutaneous trauma or skeletal injury. The study population is small because not all children with skull fractures presenting to the ED were referred to the child abuse program for a multidisciplinary evaluation, and not all children who were referred were eligible as they did not complete follow-up imaging.
The study has other limitations such as the timing of follow-up radiographs was not standardized. Therefore, follow-up intervals varied between patients and were dependent on caregiver availability. A study designed with more frequent follow-up intervals may allow identification of the timing of fracture resolution more precisely as fractures may have resolved earlier than 10 weeks (between 3 and 9 weeks) or later than 18 weeks. Finally, initial fracture length or separation was not measured in this study and may also affect the timing of fracture resolution.
A final limitation of this study is that both physicians and caregivers may have expressed concern regarding radiation exposure reducing follow-up imaging. In general, the use of radiation in pediatric patients should be judicious. Radiation should not be an overriding concern in skeletal surveys given the overall estimated low cumulative dose of 0.2 mSv.27 Using the data provided by Berger et al,27 the individual effective dose of an AP skull radiograph is 0.005 mSv (55 kVp and 2 mAs), and the effective dose of a lateral skull radiograph is 0.008 mSv (60 kVp and 2.5 mAs). Thus, the cumulative dose of a 2-view skull is 0.013 mSv. In comparison, the yearly average absorbed dose from the American Nuclear Society is estimated at 6.2 mSv per person per year or a daily dose of 0.017 mSv.28 Although a future study with standardized imaging intervals and a larger number of subjects could provide more precise information on the resolution of skull fractures, it may also be difficult because of the concern for cumulative radiation exposure from repeated imaging. It may be feasible to design a study of fracture healing using ultrasonography as information continues to accrue on this technique for skull fracture identification in the pediatric population.29,30
CONCLUSIONS
Healing or radiographic resolution of a skull fracture in young children can take months. In this retrospective chart review, those skull fractures with follow-up imaging demonstrated radiographic resolution at or after 10 weeks. Emergency medicine physicians and multidisciplinary teams should be aware of the high variability in skull fracture presentation and the large window to skull fracture resolution when children younger than 24 months present with unexplained or multiple skull fractures.
Footnotes
Disclosure: N.S.H.'s institution has received payment for expert witness court testimony that has been provided in cases of suspected child abuse in which she has been subpoenaed to testify. N.S.H. and S.E. have provided paid expert testimony in cases of suspected child abuse. The other authors declare no conflict of interest.
Contributor Information
Sonja Eddleman, Email: sonja.eddleman@dchstx.org.
Khushbu Shukla, Email: dr_kshukla@yahoo.com.
Maria Veronica Narcise, Email: mhavienarcisemd@yahoo.com.
Laura J. Padhye, Email: laura.padhye@gmail.com.
Loralie J. Peterson, Email: pete6391@umn.edu.
Michael A. Murati, Email: mura0071@umn.edu.
Caroline L. S. George, Email: cgeorge@umn.edu.
REFERENCES
- 1.Niederkrotenthaler T Xu L Parks SE, et al. Descriptive factors of abusive head trauma in young children-United States, 2000-2009. Child Abuse Negl. 2013;37:446–455. [DOI] [PubMed] [Google Scholar]
- 2.Leventhal JM, Martin KD, Gaither JR. Using US data to estimate the incidence of serious physical abuse in children. Pediatrics. 2012;129:458–464. [DOI] [PubMed] [Google Scholar]
- 3.Leventhal JM, Martin KD, Asnes AG. Fractures and traumatic brain injuries: abuse versus accidents in a US database of hospitalized children. Pediatrics. 2010;126:e104–e115. [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim NG Wood J Margulies SS, et al. Influence of age and fall type on head injuries in infants and toddlers. Int J Dev Neurosci. 2012;30:201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes J Maguire S Jones M, et al. Biomechanical characteristics of head injuries from falls in children younger than 48 months. Arch Dis Child. 2016;101:310–315. [DOI] [PubMed] [Google Scholar]
- 6.Kemp AM Dunstan F Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008;337:a1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billmire ME, Myers PA. Serious head injury in infants: accident or abuse? Pediatrics. 1985;75:340–342. [PubMed] [Google Scholar]
- 8.Meservy CJ Towbin R McLaurin RL, et al. Radiographic characteristics of skull fractures resulting from child abuse. AJR Am J Roentgenol. 1987;149:173–175. [DOI] [PubMed] [Google Scholar]
- 9.Duhaime AC Alario AJ Lewander WJ, et al. Head injury in very young children: mechanisms, injury types, and ophthalmologic findings in 100 hospitalized patients younger than 2 years of age. Pediatrics. 1992;90(2 pt 1):179–185. [PubMed] [Google Scholar]
- 10.Leventhal JM, Gaither JR. Incidence of serious injuries due to physical abuse in the United States: 1997 to 2009. Pediatrics. 2012;130:e847–e852. [DOI] [PubMed] [Google Scholar]
- 11.Adamsbaum C Grabar S Mejean N, et al. Abusive head trauma: judicial admissions highlight violent and repetitive shaking. Pediatrics. 2010;126:546–555. [DOI] [PubMed] [Google Scholar]
- 12.Chadwick DL Chin S Salerno C, et al. Deaths from falls in children: how far is fatal? J Trauma. 1991;31:1353–1355. [DOI] [PubMed] [Google Scholar]
- 13.Kleinman PK, Spevak MR. Soft tissue swelling and acute skull fractures. J Pediatr. 1992;121(5 pt 1):737–739. [DOI] [PubMed] [Google Scholar]
- 14.Metz JB Otjen JP Perez FA, et al. Fracture-associated bruising and soft tissue swelling in young children with skull fractures: how sensitive are they to fracture presence? Pediatr Emerg Care. 2020, Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 15.Halliday KE Broderick NJ Somers JM, et al. Dating fractures in infants. Clin Radiol. 2011;66:1049–1054. [DOI] [PubMed] [Google Scholar]
- 16.Islam O Soboleski D Symons S, et al. Development and duration of radiographic signs of bone healing in children. AJR Am J Roentgenol. 2000;175:75–78. [DOI] [PubMed] [Google Scholar]
- 17.Malone CA, Sauer NJ, Fenton TW. A radiographic assessment of pediatric fracture healing and time since injury. J Forensic Sci. 2011;56:1123–1130. [DOI] [PubMed] [Google Scholar]
- 18.Prosser I Lawson Z Evans A, et al. A timetable for the radiologic features of fracture healing in young children. AJR Am J Roentgenol. 2012;198:1014–1020. [DOI] [PubMed] [Google Scholar]
- 19.Yeo LI, Reed MH. Staging of healing of femoral fractures in children. Can Assoc Radiol J. 1994;45:16–19. [PubMed] [Google Scholar]
- 20.Shopfner CE. Periosteal bone growth in normal infants. A preliminary report. Am J Roentgenol Radium Ther Nucl Med. 1966;97:154–163. [DOI] [PubMed] [Google Scholar]
- 21.Walters MM Forbes PW Buonom C, et al. Healing patterns of clavicular birth injuries as a guide to fracture dating in cases of possible infant abuse. Pediatr Radiol. 2014;44:1224–1229. [DOI] [PubMed] [Google Scholar]
- 22.Marx RE. Bone and bone graft healing. Oral Maxillofac Surg Clin North Am. 2007;19:455–466, v. [DOI] [PubMed] [Google Scholar]
- 23.Meyer JS Gunderman R Coley BD, et al. ACR Appropriateness Criteria(®) on suspected physical abuse-child. J Am Coll Radiol. 2011;8:87–94. [DOI] [PubMed] [Google Scholar]
- 24.Hughes CA Harley EH Milmoe G, et al. Birth trauma in the head and neck. Arch Otolaryngol Head Neck Surg. 1999;125:193–199. [DOI] [PubMed] [Google Scholar]
- 25.Dupuis O Silveira R Dupont C, et al. Comparison of “instrument-associated” and “spontaneous” obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol. 2005;192:165–170. [DOI] [PubMed] [Google Scholar]
- 26.Kleinman PK. (ed). Diagnostic Imaging of Child Abuse. 3rd ed. Cambridge: Cambridge University Press; 2015. [Google Scholar]
- 27.Berger RP Panigrahy A Gottschalk S, et al. Effective radiation dose in a skeletal survey performed for suspected child abuse. J Pediatr. 2016;171:310–312. [DOI] [PubMed] [Google Scholar]
- 28.American Nuclear Society. Radiation Dose Calculator . Available at: http://www.ans.org/pi/resources/dosechart/msv.php. Accessed May 8, 2017.
- 29.Rabiner JE Friedman LM Khine H, et al. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics. 2013;131:e1757–e1764. [DOI] [PubMed] [Google Scholar]
- 30.Parri N Crosby BJ Mills L, et al. Point-of-care ultrasound for the diagnosis of skull fractures in children younger than two years of age. J Pediatr. 2018;196:230–236.e2. [DOI] [PubMed] [Google Scholar]


