The study performed a comparison of short-term results after high intensity electromagnetic treatment and electrostimulation for improvement of urinary incontinence.
Key Words: pelvic floor, ultrasonography, urinary incontinence
Abstract
Objectives
Pelvic floor muscles (PFMs) weakening and urinary incontinence (UI) represent health issues that have a negative impact on daily life. This study compares the immediate efficiency of high-intensity focused electromagnetic (HIFEM) therapy and electrostimulation for the treatment of weakened PFMs, accompanied by the UI.
Methods
Ninety-five parous women were considered for the study. Symptomatic patients received either HIFEM or electrostimulation treatment. Treated patients completed 10 therapies scheduled 2 to 3 times per week (HIFEM) or every other day (electrostimulation). Patients underwent examination by 3-dimensional transperienal ultrasound at the baseline and posttreatments. Levator-urethra gap, anteroposterior diameter, laterolateral diameter of levator hiatus, and hiatal area were measured. In addition, Pelvic Floor Disability Index 20 questionnaire and subjective evaluation of patient’s intimate health were assessed.
Results
Enrolled patients were divided into group I (n = 50, HIFEM), group II (n = 25, electrostimulation), and group III (n = 20, control) according the indication and treatment modality. Three-dimensional ultrasounds showed positive changes in dynamics of the pelvic floor posttreatment (decreased anteroposterior diameter, laterolateral diameter, and hiatal area). However, the significant (P < 0.05) changes of pelvic floor integrity were observed only in group I. In addition, group I achieved greater level of improvement in Pelvic Floor Disability Index 20 questionnaire compared with group II (52% and 18% respectively; P < 0.001). Substantially fewer patients in group I reported urine leakage after treatments.
Conclusions
Posttreatment results suggest that HIFEM technology is suitable for treatment of PFMs weakening and showed to be more effective when compared with electrostimulation in short-term. Therefore, we recommend HIFEM as treatment option for weakened PFMs and UI.
The pelvic floor is highly complex, consisting of skeletal and striated muscles. It plays an important role in the maintenance of continence mechanism. For its proper functioning, strong and well-conditioned pelvic floor muscles (PFMs) are required,1 ensuring the pelvic viscera’s integrity.2 Weakening of the PFMs may promote a wide range of health issues, such as pelvic organ prolapse or bladder dysfunction manifested as urinary incontinence (UI). Symptoms associated with UI directly affect the patient’s quality of life.3
Between 4% and 8% of the human population suffer from UI as implied by the data released by Global Forum of Incontinence.4 Prevalence of UI tends to increase with age5 and can be triggered by risk factors such as surgical intervention or childbirth (especially vaginal delivery).6,7 These may have a negative impact on the pelvic floor muscle’s activity and morphology.8 The deconditioning of PFMs accompanied with UI often influences the patient’s mental and physical health. Fortunately, there are both surgical and nonsurgical methods of treatment available for such conditions. However, the nonsurgical approach should be always recommended as first-line therapy.9
Pelvic floor muscles can be treated with either monotherapy or combination therapy, which includes a combination of available treatment modalities to enhance treatment outcomes.10–12 In general, nonsurgical approaches for the correction of pelvic muscle dysfunction include biofeedback therapy,12 Kegel exercises (and its modifications),13 magnetic stimulation,14,15 and a wide range of electrostimulation methods.16 Lately, a novel noninvasive technology utilizing the high-intensity focused electromagnetic (HIFEM) field was introduced for treating PFMs.17,18 The HIFEM field depolarizes membranes of peripheral motoneurons and initiates muscle contraction.19 High repetition rate of stimulation ensures that pelvic muscles reach nonvoluntary contractions of great intensities, referred to as “supramaximal” contractions. Although the effectiveness of HIFEM therapy was described earlier,17,18 comparative assessment with other treatment modalities is still lacking.
The changes of the function of PFMs with regards to the UI are often assessed by the subjective standardized questionnaires, in particular with Pelvic Floor Impact Questionnaire or Pelvic Floor Disability Index (PFDI).20 These are designed to allow patients comprehensively describe their perception of their pelvic area. This serves as a powerful tool for the practitioners when used in combination with some objective evaluation (magnetic resonance, ultrasound imaging, or electromyography).21,22 Especially, the 3-dimensional (3D) transperineal ultrasonography of the pelvic floor has become widely used due to its ability to promptly assess essential parameters of pelvic floor integrity.23,24
The goal of this pilot study is to investigate and compare the immediate efficiency of HIFEM technology and electrical stimulation, for the treatment of weakened PFMs accompanied by UI.
MATERIALS AND METHODS
Inclusion Criteria and Ethical Principles
Between the 2018 and early 2019, 95 postpartum women in reproductive age referred to the Hospital Lapino (MD Medical Group) were considered for the study. The present study is a retrospective analysis of all the short-term data, which were gathered during their pretreatment and posttreatment examination.
The inclusion criteria were age 18 to 45 years and history of vaginal childbirth (not earlier than 6 months ago). The exclusion criteria included the following: pelvic organ prolapse; pregnancy at the time of therapy initiation (urinary pregnancy test was done in both groups at the baseline); the presence of metal implants in the area of lumbosacral spine, pelvis, or hip joints or intrauterine device, which includes any metal components, cardiac pacemaker, or other inner electronic devices; and general contraindications for physiotherapy. All the patients signed a voluntary informed consent.
Treatment Protocol
Patients who showed PFMs weakness and continence issues received either therapy with the BTL EMSELLA (BTL Industries Inc, Boston, MA) or BioBravo (MTR+ Vertriebs GmbH, Germany) device. BTL EMSELLA uses HIFEM technology for PFM strengthening and reduction of UI. The device is consisted of a power generator and a circular coil mounted in the seat of the chair. During the treatment, the patient is fully clothed and seated on the center of the chair while the alternating magnetic fields with intensities of up to 2.5 T have been penetrating the pelvic area. In total, 10 HIFEM treatments (for 28 minutes each) with frequency 2 to 3 sessions per week were delivered to match the electrostimulation protocol.
BioBravo portable low-frequency stimulator is used for self-administered PFMs stimulation to treat urinary/fecal incontinence symptoms (approved by European Union conformity mark, not Food and Drug Administration cleared or approved). Patients performed a course of 10 procedures at home (every other day or, at least, 3 times a week) with BioBravo device, after they passed preliminary training. Time of each BioBravo session was set to 28 minutes to mirror the duration of Emsella’s treatment.
Evaluation of Study Outcomes
Various methods for documentation of treatment outcomes were used. The first (baseline) visit consisted of medical anamnesis, gynecological examination, and 3D transperineal ultrasound of the pelvic floor area by Voluson E10 device (RIC6-12-D transducer). During the examination, patients were placed in the dorsal lithotomy position with both hips symmetrically flexed, legs abducted, and knees flexed. The transducer was located on the perineum between the mons pubis and the anal margin. In particular, measured biometric indices of pelvic floor integrity included anteroposterior diameter (LH-AD) and laterolateral diameter (LH-LD) of levator hiatus and hiatal area (HA). In addition, levator-urethra gap (LUG) was studied before the first treatment (pelvic prolapse detection due to the levator ani avulsion). The ultrasound examination was repeated after the prescribed course of treatments.
Treated women were also asked to complete PFDI-20 standardized questionnaire to assess the degree of PFM functioning and continence issues. These patients also evaluated their intimate health on bimodal basis (yes/no), according to following questions: Q1 — Are you experiencing vaginal laxity during intimacy? Q2 — Are you experiencing changes of vaginal topography? Q3 — Does the water or air enter the vagina during swimming and exercise? Q4 — Are you experiencing stress UI symptoms (eg, involuntary urine leakage during physical activity, when coughing or sneezing or before you can visit the toilet)? After the successful completion of all treatments, the patients reevaluated their continence and PFM functioning.
Safety and comfort of the patients were monitored (any possible adverse effects or adverse events, for example, pain, muscle fatigue, or bruising induced by therapies). Patients who performed treatments at home were instructed to record any inconveniences caused by electrotherapy.
There was a large number of patients to provide sufficient sample for statistical analysis, further verified by G-power 3.1.9.2 software.25 Gathered results were statistically analyzed using Statistica version 6 software (StatSoft Inc, Tulsa, OK) using the paired t test and 2-way analysis of variance followed by least significant difference post hoc test. Level of significance α was set to 5%. Assumption of normality was tested by Kolmogorov-Smirnov and Lilliefors tests.
RESULTS
All 95 patients were recruited. In total, 75 women reported PFMs weakness and incontinence issues. Symptomatic patients were divided into 2 groups. Group I (n = 50, mean ± SD age of 31.1 ± 5.4 years) received therapy with the EMSELLA device. Group II (n = 25, mean ± SD age of 32.0 ± 7.7 years) was treated with BioBravo stimulator. The remaining patients marked as a group III (n = 20, mean age of 27.2 ± 4.3 years) were classified as healthy participants and were used only as control for 3D ultrasound measurements.
Each patient from groups I and II finished the prescribed course of treatments. No adverse events or pain were reported. None of the patients experienced prolapse of pelvic floor, which can be seen in Table 1. Thickness of LUG on both sides of the pelvis did not exceed the cutoff value of 25 mm as stated in literature,26 and thus, both treated groups met the inclusion criteria. The minor differences in LUG thickness within the groups were insignificant.
TABLE 1.
Examination of LUG Thickness for Determination of Levator Ani Avulsion as Sign of Pelvic Organ Prolapse
| Levator Avulsion | LUG Right Side, Mean (SD), mm | LUG Left Side, Mean (SD), mm |
|---|---|---|
| Group I | 20.94 (3.22) | 21.76 (3.14) |
| Group II | 20.96 (2.49) | 21.48 (2.68) |
| Group III | 20.70 (2.68) | 20.85 (2.94) |
Data are expressed as mean with SD.
3D Ultrasounds of Pelvic Floor
The rest of the parameters obtained by 3D ultrasounds are documented in Table 2. Before the treatment, significantly higher values were documented in all studied indices against the control group. After the last therapy, the initially high values of LH-AD, LH-LD, and HA were significantly reduced only in group I (P < 0.05), approaching the averages of group III. Results of group II showed similar yet insignificant trend (P > 0.05). Such difference indicates the significant effect only in patients treated by HIFEM technology.
TABLE 2.
Three-dimensional Ultrasound Examination of Intervention (I and II) and Control (III) Groups
| PFM Integrity | LH-AD, Mean (SD), mm | LH-LD, Mean (SD), mm | HA, Mean (SD), cm2 | |||
|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | |
| Group I | 51.10 (6.80)† | 47.98 (6.25)* | 41.44 (6.43)† | 38.40 (6.03)* | 14.47 (1.72)† | 13.09 (1.78)* |
| Group II | 52.52 (5.75)† | 51.36 (5.36)† | 46.60 (6.70)† | 45.56 (6.41)† | 14.77 (1.82)† | 14.69 (1.79)† |
| Group III | 46.60 (2.30) | N/A | 35.40 (2.50) | N/A | 11.59 (0.35) | N/A |
Data are expressed as mean with SD. Group III was measured only at the baseline as a reference, therefore values after treatment are not available.
*Statistically significant differences against baseline (P < 0.05).
†Statistically significant differences against control.
N/A, not available.
The examples of 3D ultrasounds obtained before and after HIFEM treatments are visualized on the Figure 1. There is visible improvement in LH-AD and HA parameters. Thickness of LHAD was decreased by 2.6 mm, which is comparable with mean difference of whole group I (−3.12 mm on average). In addition, HA showed more profound reduction of 1.83 cm2 that exceeds the group I average difference (−1.38 cm2) of almost 0.5 cm2.
FIGURE 1.
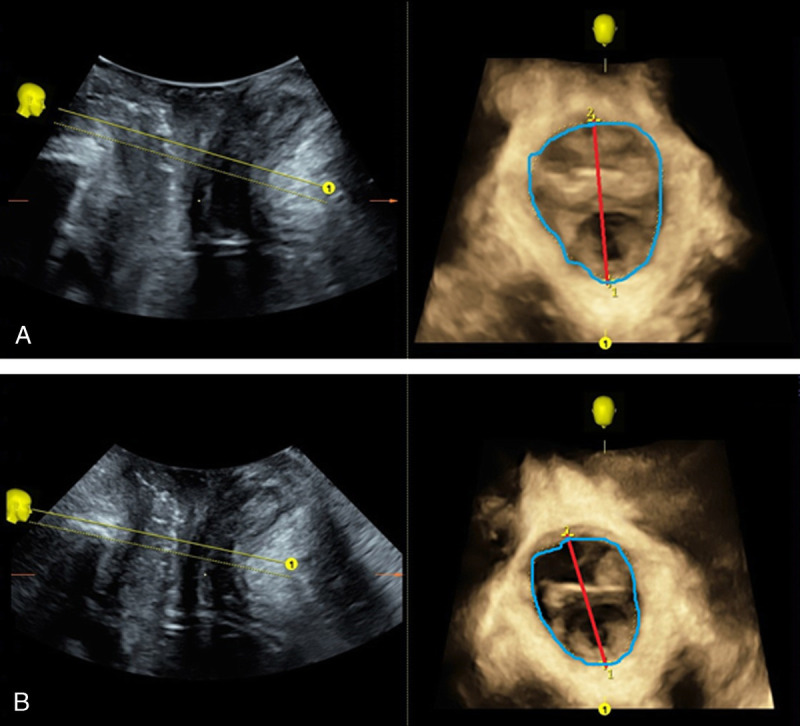
A 39-year-old patient, 1 childbirth. Visualization of ultrasound measurements (Voluson E10, equipped with RIC6-12-D transducer) before (A) and after (B) HIFEM treatments. Midsagittal plane on the left, axial rendered volume on the right. Red line indicates LH-AD dimensions. Area of HA is bordered by blue line. Direction of view in 3D is indicated by yellow lines and 1 mark.
PFDI-20 Standardized Questionnaire
No difference in the baseline PFDI-20 score was found. Although the baseline score was slightly higher in group II, this tendency showed to be insignificant (P = 0.45). The more profound change has been achieved by group I. After the HIFEM treatments, patients improved by 31.45 points (52%, P < 0.001). On the contrary, group II showed lesser yet significant mean difference of 11.70 points (18%, P < 0.001). The comparison of results obtained after the last treatments revealed also significant difference between the group I and II mean scores (P < 0.001; Table 3).
TABLE 3.
Mean Scores of the Standardized PFDI-20 Questionnaire Including the 95% CIs
| PFDI-20 | Baseline Score (CI) | After Tx Score (CI) | P |
|---|---|---|---|
| Group I | 60.22 (50.62–69.82) | 28.77 (20.74–36.81) | <0.001 |
| Group II | 66.21 (54.08–78.34) | 54.51 (43.92–65.11) | <0.001 |
| P value | 0.45 | <0.001 |
Data were gathered at baseline and after treatments (After Tx).
CI, confidence interval;Tx, treatment.
Patient’s Self-Evaluation
Results of the patient’s subjective bimodal evaluation are summarized in Table 4. The percentages describe a portion of patients who answered questions Q1 to Q4 positively (yes). After the treatments, the percentage of answers regressed in both groups; however, group I showed substantially greater differences in comparison with group II. On average, the subjective assessment revealed that patient self-reported 2 times greater results after HIFEM treatment. Especially remarkable improvement was observed in questions Q1 (laxity) and Q4 (incontinence). In group I, the differences reached up to 30% (Q1) and 44% (Q4), respectively, whereas group II reported much lower change of 16%.
TABLE 4.
Subjective Examination of Patient’s Intimate Health Obtained at the Baseline and After Treatments (After Tx)
| Question | Group I | Group II | ||||
|---|---|---|---|---|---|---|
| Baseline | After Tx | Difference | Baseline | After Tx | Difference | |
| Q1 | 48% | 18% | −30% | 44% | 28% | −16% |
| Q2 | 36% | 12% | −24% | 36% | 24% | −12% |
| Q3 | 34% | 16% | −18% | 48% | 36% | −12% |
| Q4 | 74% | 30% | −44% | 72% | 56% | −16% |
The percentages express the portion of patients who answered yes.
Tx, treatment.
Sample Size and Verification of Power
Using G-power software, we calculated the minimal sample size to reveal statistical significance in gathered data as 16 patients for both 2-tailed t test (α = 0.05; power, 0.95; effect size, 1) and analysis of variance (α = 0.05; power, 0.95; 3 groups; effect size, 1). In addition, the power of conduced statistical analysis was verified post hoc and showed to be equal to 0.99.
DISCUSSION
According to the documented results, we suggest that HIFEM therapy was more effective method for treatment of weakened pelvic floor than electrostimulation in short-term. Apparently, based on the evaluation by both subjective (questionnaires) and objective (3D transperineal ultrasound) methods, HIFEM therapy produces more profound improvement in PFMs and UI posttreatment.
Besides the magnetic resonance, one of the most reliable methods for examination of pelvic area is diagnostic ultrasound. Because of the complex manner of structures forming the pelvic floor, 2-dimensional image may not always provide proper visualization. Hence, the examination should be combined with 3D analysis.23 The use of such technology in routine practice may help to reveal pelvic floor muscles weakening even if the patient does not have any subjective complaints. Early diagnosis helps start timely treatment, as the 3D reconstruction of pelvic floor allows to obtain specific parameters of its integrity (LUG, LH-AD, LH-LD, and HA).
Recent research demonstrated that LUG is strongly associated with puborectalis avulsion, and the cutoff threshold for its diagnosis appears to be 25 to 27.5 mm.23,26 Our initial gynecological examination showed no levator avulsion, which would exclude patients from the study. Levator-urethra gap ranged from 20.70 to 21.76 mm (Table 1), and thus, no pelvic organ prolapse was diagnosed because measured values showed to be substantially lower than cut-off threshold.
The biometric indices of control group are comparable with the results reported in literature for nuliparous women at rest.27 It was found that LH-AD in healthy patients ranges from 45.2 to 48.4 mm, LH-LD from 32.8 to 37.5, and HA from 11.3 to 12.0 cm2, which corresponds to our observations in healthy parous women (group III). However, both treated groups at the baseline showed significantly higher LH-AD, LH-LD, and HA in comparison with the group III. As a result of the treatments, these indices decreased toward the control values. Nonetheless, significant changes of the pelvic floor anatomy were demonstrated only in patients treated by HIFEM technology (Table 2; Fig. 1).
The presented data showed an enhanced functioning of PFMs with reduction of UI severity and impact on the quality of life has been achieved (Tables 3 and 4). Differences in PFDI-20 mean scores were found to be highly statistically significant. Both treatment modalities proved to be effective in treating PFMs weakness accompanied with UI. However, our observations indicate significantly more profound efficiency of the HIFEM technology in comparison with the electrostimulation after a course of 10 treatment sessions. Based on the questionnaire data, it was proved (P < 0.001) that group I reached a higher level of improvement (2.68 times) after a series of 10 treatments. Patients treated by HIFEM technology showed mean difference in PFDI of over 50%. On the contrary, group II was only able to reach an average improvement of 18%.
The patient’s subjective bimodal assessment revealed greater results in group I, which reported reduced incontinence symptoms after the treatments, when compared with group II. In addition, those who received HIFEM therapy noticed a substantial reduction in vaginal laxity symptoms. Modest improvement of incontinence and laxity issues was seen in group II, probably attributed to the less recognizable improvement of PFM functioning. Conversely, the greater results observed in patients from group I correlate to their significant change in pelvic floor integrity and PFDI-20 score.
For PFM strengthening, the strong contractions with interposed rest periods should be involved to deliver sufficient load.28 If the muscles are properly stimulated, both endurance and strength are regained.29 Superior results after HIFEM therapy in our study may be explained by the deep penetration of high-intensity electromagnetic field into the pelvic area, resulting in uniform activation of PFMs. On the contrary, electrical devices may not be able to involve whole pelvic floor with sufficient intensity of the stimuli. Because of its superficial application, the electrostimulators lost the largest portion of emitted energy on the surface, and only its fraction reaches deep-lying tissues.30 Although some positive effects of electrostimulation on PFM strengthening was documented in the past, there is still not sufficient evidence to determine whether it is more effective than traditional exercise.20,31,32
In this study, the treated postpartum patient groups were consisted of relatively young women of average age 31.1 ± 5.4 years and 32.0 ± 7.7 years. However, we assume that our findings are applicable also in the older postmenopausal patients who would probably show symptoms of greater severity because of the estrogen deficiency. Samuels et al,33 for instance, was able to reach similar degree of immediate posttreatment improvement after the series of 6 HIFEM treatments in patient group aged 55.5 ± 12.8 years. Almost identically aged group (55.2 ± 12.8 years) was established also by Castro et al34 who described significant and continuous results of electrostimulation therapy.
Continuity of results after noninvasive pelvic floor stimulation is still being investigated in the literature. Based on the long-term observation of treatment outcomes after magnetic and electrical stimulation, it is assumed that beneficial effect of induced PFM strengthening may be sustained up to 1 year.14,35 However, after this period of time, the relapse may occur and maintenance session should be considered in some patients.
Although the presented data are based on the short-term observation of patient cohort, the discovered findings showed to be sufficient to identify contrast in efficacy between the HIFEM technology and electrostimulation. Future research should verify the persistence of herein published results and further tendencies in patient’s PFMs and UI management as well as retreatment period. Treatment groups of at least 16 patients should be established when the great effect of intervention is observed. Otherwise, the higher number of patients might be required.
It was demonstrated that HIFEM technology was able to significantly improve biometric indices of pelvic floor integrity and UI symptoms. Therefore, we recommend HIFEM for a widespread uses in practice as the treatment of weakened pelvic muscles and continence issues.
Footnotes
This article published online ahead of print on December 19, 2019.
The authors have declared they have no conflicts of interest.
Contributor Information
Dragana Zarkovic, Email: dragana.z@seznam.cz.
Evgeniia Astafeva, Email: dr_astafeva@mail.ru.
Ramina Soldatskaia, Email: doctor_ras@rambler.ru.
Mekan Orazov, Email: omekan@mail.ru.
Marina Belkovskaya, Email: usimar@rambler.ru.
Mark Kurtser, Email: m.kurtser@mcclinics.ru.
REFERENCES
- 1.Jundt K, Peschers U, Kentenich H. The investigation and treatment of female pelvic floor dysfunction. Dtsch Ärztebl Int 2015;112(33–34):564–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elneil S. Complex pelvic floor failure and associated problems. Best Pract Res Clin Gastroenterol 2009;23(4):555–573. [DOI] [PubMed] [Google Scholar]
- 3.Zargham M Alizadeh F Moayednia A, et al. The role of pelvic organs prolapse in the etiology of urinary incontinence in women. Adv Biomed Res 2013;2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Incontinence — Global Forum on Incontinence — GFI . Available at: http://www.gfiforum.com/incontinence. Accessed January 30, 2019.
- 5.Gomelsky A, Dmochowski RR. Urinary incontinence in the aging female: etiology, pathophysiology and treatment options. Aging Health 2011;7(1):79–88. [Google Scholar]
- 6.Wang X Shi JX Zhai GR, et al. Postpartum stress urinary incontinence and associated obstetric factors. Zhonghua Fu Chan Ke Za Zhi 2010;45(2):104–108. [PubMed] [Google Scholar]
- 7.Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol 2004;6(Suppl 3):S3–S9. [PMC free article] [PubMed] [Google Scholar]
- 8.Aoki Y Brown HW Brubaker L, et al. Urinary incontinence in women. Nat Rev Dis Primer 2017;3:17042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radzimińska A Strączyńska A Weber-Rajek M, et al. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: a systematic literature review. Clin Interv Aging 2018;13:957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siff LN Hill AJ Walters SJ, et al. The effect of commonly performed exercises on the levator hiatus area and the length and strength of pelvic floor muscles in postpartum women. Female Pelvic Med Reconstr Surg 2018. [DOI] [PubMed] [Google Scholar]
- 11.Yang S Sang W Feng J, et al. The effect of rehabilitation exercises combined with direct vagina low voltage low frequency electric stimulation on pelvic nerve electrophysiology and tissue function in primiparous women: a randomised controlled trial. J Clin Nurs 2017;26(23–24):4537–4547. [DOI] [PubMed] [Google Scholar]
- 12.Newman DK. Pelvic floor muscle rehabilitation using biofeedback. Urol Nurs 2014;34(4):193–202. [PubMed] [Google Scholar]
- 13.Kegel AH. Physiologic therapy for urinary stress incontinence. JAMA 1951;146(10):915. [DOI] [PubMed] [Google Scholar]
- 14.Lim R Liong ML Leong WS, et al. Pulsed magnetic stimulation for stress urinary incontinence: 1-year followup results. J Urol 2017;197(5):1302–1308. [DOI] [PubMed] [Google Scholar]
- 15.Yokoyama T Fujita O Nishiguchi J, et al. Extracorporeal magnetic innervation treatment for urinary incontinence. Int J Urol 2004;11(8):602–606. [DOI] [PubMed] [Google Scholar]
- 16.Martellucci J, ed. Electrical Stimulation for Pelvic Floor Disorders New York, NY: Springer International Publishing; 2015. Available at: https://www.springer.com/gp/book/9783319069463. Accessed March 26, 2019. [Google Scholar]
- 17.Samuels J, Guerette NL. HIFEM technology the non-invasive treatment of urinary incontinence. Lasers Surg Med 2018;50(S29):S4–S56.29574789 [Google Scholar]
- 18.Alinsod R Vasilev V Yanev K, et al. HIFEM technology a new perspective in treatment of stress urinary incontinence. Lasers Surg Med 2018;50(S29):S4–S56.29574789 [Google Scholar]
- 19.Voorham-Van Der Zalm PJ Pelger RC Stiggelbout AM, et al. Effects of magnetic stimulation in the treatment of pelvic floor dysfunction. BJU Int 2006;97(5):1035–1038. [DOI] [PubMed] [Google Scholar]
- 20.Bø K Berghmans B Mørkved S, et al. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. Edinburgh, Scotland: Churchill Livingstone; 2015.
- 21.Zuchelo LTS Bezerra IMP Da Silva ATM, et al. Questionnaires to evaluate pelvic floor dysfunction in the postpartum period: a systematic review. Int J Womens Health 2018;10:409–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glazer HI, Romanzi L, Polaneczky M. Pelvic floor muscle surface electromyography. Reliability and clinical predictive validity. J Reprod Med 1999;44(9):779–782. [PubMed] [Google Scholar]
- 23.Yan Y Dou C Wang X, et al. Combination of tomographic ultrasound imaging and three-dimensional magnetic resonance imaging-based model to diagnose postpartum levator avulsion. Sci Rep 2017;7(1):11235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dietz HP. Pelvic floor ultrasound: a review. Am J Obstet Gynecol 2010;202(4):321–334. [DOI] [PubMed] [Google Scholar]
- 25.Faul F Erdfelder E Lang A-G, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 26.Dietz HP, Abbu A, Shek KL. The levator-urethra gap measurement: a more objective means of determining levator avulsion? Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 2008;32(7):941–945. [DOI] [PubMed] [Google Scholar]
- 27.Gaspari AL, Sileri P. Pelvic Floor Disorders: Surgical Approach. Milan, Italy: Springer-Verlag Mailand; 2014. [Google Scholar]
- 28.Nyland J, ed. Clinical Decisions in Therapeutic Exercise: Planning and Implementation. Upper Saddle River, NJ: Pearson Education; 2006. [Google Scholar]
- 29.Fowler CJ, Panicker JN, Emmanuel A. Pelvic Organ Dysfunction in Neurological Disease: Clinical Management and Rehabilitation. Cambridge, England: Cambridge University Press; 2010. [Google Scholar]
- 30.Prodanovic M Malešević J Filipovic M, et al. Numerical simulation of the energy distribution in biological tissues during electrical stimulation. Serbian J Electr Eng 2013;10:165–173. [Google Scholar]
- 31.Amaro JL Gameiro MO Kawano PR, et al. Intravaginal electrical stimulation: a randomized, double-blind study on the treatment of mixed urinary incontinence. Acta Obstet Gynecol Scand 2006;85(5):619–622. [DOI] [PubMed] [Google Scholar]
- 32.Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999;318(7182):487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Samuels JB Pezzella A Berenholz J, et al. Safety and efficacy of a non-invasive high-intensity focused electromagnetic field (HIFEM) device for treatment of urinary incontinence and enhancement of quality of life. Lasers Surg Med 2019;51(9):760–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Castro RA Arruda RM Zanetti MRD, et al. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics 2008;63(4):465–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fürst MC Mendonça RR Rodrigues AO, et al. Long-term results of a clinical trial comparing isolated vaginal stimulation with combined treatment for women with stress incontinence. Einstein (Sao Paulo) 2014;12(2):168–174. [DOI] [PMC free article] [PubMed] [Google Scholar]


