Abstract
Background
Correctional and detention facilities are disproportionately affected by COVID-19 due to shared space, contact between staff and detained persons, and movement within facilities. On March 18, 2020, Cook County Jail, one of the United States’ largest, identified its first suspected case of COVID-19 in a detained person.
Methods
This analysis includes SARS-CoV-2 cases confirmed by molecular detection among detained persons and Cook County Sheriff's Office staff. We examined occurrence of symptomatic cases in each building and proportions of asymptomatic detained persons testing positive, and timing of interventions including social distancing, mask use, and expanded testing and show outbreak trajectory in the jail compared to case counts in Chicago.
Results
During March 1-April 30, 907 symptomatic and asymptomatic cases of SARS-CoV-2 infection were detected among detained persons (n = 628) and staff (n = 279). Among asymptomatic detained persons in quarantine, 23.6% tested positive. Programmatic activity and visitation stopped March 9, cells were converted into single occupancy beginning March 26, and universal masking was implemented for staff (April 2) and detained persons (April 13). Cases at the jail declined while cases in Chicago increased.
Discussion/Conclusions
Aggressive intervention strategies coupled with widespread diagnostic testing of detained and staff populations can limit introduction and mitigate transmission of SARS-CoV-2 infection in correctional and detention facilities.
Keywords: COVID, Epidemiology, Respiratory disease, Infection control, Correction institutions
Background
In correctional and detention facilities, shared physical space and interaction of detained persons and staff facilitate introduction and spread of viruses like SARS-CoV-21. Large COVID-19 outbreaks have been reported in congregate settings2 , 3, including correctional and detention facilities4. Multiple interventions, including physical distancing and reducing introductions from the community via new detained persons, staff, and visitors, are likely needed to effectively interrupt SARS-CoV-2 transmission, but can be difficult to implement5 , 6. Many individuals incarcerated or detained in U.S. state and federal facilities are at elevated risk for severe COVID-19: they are more likely than the general population to be immunocompromised7 and approximately 50% have pre-existing medical conditions8.
Cook County Jail (CCJ) is one of the largest in the United States. On March 18, 2020, a person detained at CCJ reported influenza-like illness, including shortness of breath and fever, but tested negative for influenza. Cermak Health Services (CHS) medical staff suspected COVID-19, isolated the patient, and notified the Chicago Department of Public Health (CDPH). Although the patient did not meet COVID-19 testing criteria (no international travel or known exposure), CHS submitted diagnostic specimens to the Centers for Disease Control and Prevention (CDC). On March 28, a specimen tested positive for SARS-CoV-2 by real-time reverse transcriptase polymerase chain reaction (rRT-PCR).
We describe the subsequent outbreak of COVID-19 among detained persons1 and staff at CCJ and interventions to reduce transmission. CHS, the Cook County Sheriff's Office (CCSO), Cook County Health (CCH), CDPH, and CDC partnered to investigate, identify, and interrupt transmission.
Methods
Study population and facility-level interventions
In 2019, approximately 59,000 people were admitted into custody at CCJ; the average daily number of detained persons was 5,800. During March 1-April 30, 2020, the population of detained persons declined from 5,579 to 4,054; average daily census was 4,884. The Cook County justice system implemented measures such as releasing individuals to electronic monitoring to reduce the number of detained individuals. On March 1, CCSO had 2,370 sworn (trained correctional officers and command staff) personnel assigned to CCJ, representing the majority of people who work at CCJ. During the outbreak, 270 sworn personnel were added to secure an expansion in CCJ's geographic footprint (reopening of formerly closed cell-occupancy and dormitory-style living units to increase physical distancing).
CCJ houses detained persons in nine divisions in 13 buildings. Divisions are further divided into units; units are either open dormitories housing 40‒48 individuals on average (though one dormitory can house >600 detained persons at full capacity), or double-occupancy cells with shared common spaces. Participation in programmatic activities (eg, work assignments, school) and medical needs of individuals vary by division. Prior to March 1, 2020, CCJ utilized seven divisions; during March 1–April 30, two additional divisions were opened to achieve social distancing through single-cell occupancy in cell-based units and an alternating bunk model in dorm-based units.
Detection and infection control interventions
Case definition
COVID-19 cases were defined as SARS-CoV-2 infection by molecular detection in persons with an epidemiologic link to CCJ during March 1-April 30, 2020.
Quarantine, medical isolation, and testing of detained persons
Any detained person reporting symptoms consistent with COVID-19 was medically isolated in a single-occupancy cell, assessed by medical staff, and tested for SARS-CoV-2 via rRT-PCR performed at Illinois Department of Public Health, QUEST diagnostics (Secaucus, New Jersey), or Stroger Hospital using the m2000 system (Abbott Laboratories, Illinois, USA). In the event a detained person on a unit tested positive or ≥2 suspected cases were detected, they were removed from the unit, and the remaining individuals on the unit were quarantined in place for ≥14 days. Individuals on quarantined units remained on the unit, had meals delivered, medical care provided on the unit, and staff were kept as consistent as possible. Quarantined persons were assessed daily for symptoms; if any became symptomatic, they were medically isolated, and quarantine was extended an additional 14 days for the remainder of the unit. Additionally, once a unit was placed on quarantine, all individuals on that unit were tested. Any individuals found to be positive were removed from the unit and the quarantine was extended 14 days. All individuals on the unit were again tested at Day 10-14, prior to removing the unit from quarantine.
Initially, due to resource constraints, only asymptomatic individuals at high-risk for developing severe disease were tested. As resources became available, all detained persons entering the jail, and all those in quarantine were also tested. Testing was offered to asymptomatic detained persons in units placed under quarantine from March 25 onward. Beginning April 20, testing of newly detained persons was performed with the ID NOW COVID-19 assay (Abbott).
Screening and testing of staff
CCSO employees working on the CCJ campus were provided with a list of testing locations, but testing was optional. Staffs were required to report symptoms, positive test results, or COVID-19 clinical diagnoses to CCSO; affected individuals were provided paid time off. Staff cases were cross-referenced with Illinois’ National Electronic Disease Surveillance System (I-NEDSS) to validate laboratory results.
Data analyses
Epidemiologic curves by division were constructed using date of medical isolation as a proxy for date of symptom onset for detained persons, and by self-reported symptom onset date for staff. First positive specimen collection date was used if medical isolation date was not available. The overall attack rate (AR) among detained persons at CCJ was calculated using the average census population during the study period (N = 4,884) as the denominator; ARs by division are not reported due to fluctuations in daily census and variations in where asymptomatic testing was performed. Age, underlying conditions, temperature closest to specimen collection, and fatal outcome are described for all detained persons testing positive. Descriptive statistics and P values were calculated for each variable to assess association with symptomatic infection. Summaries of categorical variables are expressed as proportions and compared using Pearson χ2 for independence, Fisher's exact test, or Cochran-Armitage test as appropriate. The continuous age variable is expressed as median (interquartile range [IQR]) and compared using Wilcoxon rank sum test. Two-sided statistical tests were considered significant at a P < .05.
Data for all persons residing in the state of Illinois meeting the case definition for confirmed SARS-CoV-2 infection were extracted from I-NEDSS and included using the specimen collection date. We compared trends in case counts among detained persons, staff, and residents of Chicago during the study period by creating logarithmic-scale graphs of new and total cases; weekly averages were calculated to account for testing variation by day. All analyses were done using SAS v9.4 (Cary, North Carolina).
This study was reviewed by CDC, CDPH, CCH, and CCSO institutional review boards or the equivalent entity, and deemed not to be research involving human subjects and public health response.
Results
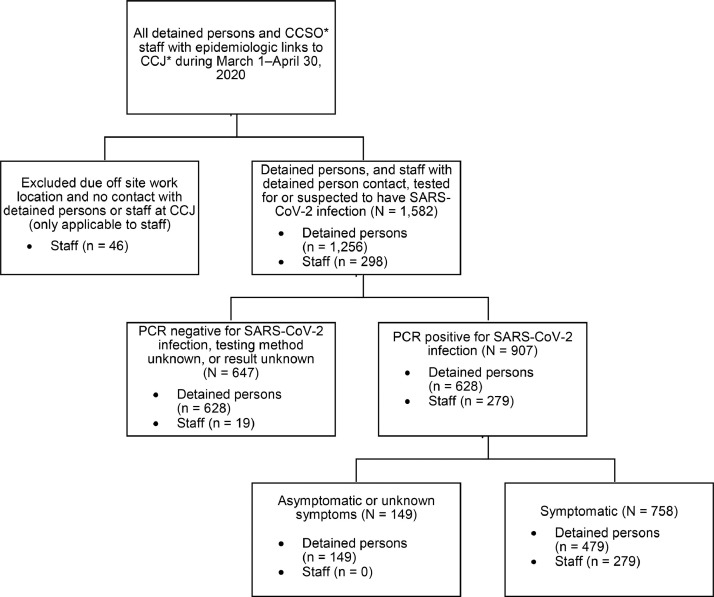
During March 1-April 30, 2020, 907 COVID-9 cases were identified among detained persons and staff epidemiologically linked to CCJ (Fig 1 ). Of 1,256 detained persons tested for SARS-CoV-2 during this period, 628 (50.0%) were positive, among whom 479 (76.3%) were symptomatic at the time of specimen collection and 149 (23.7%) were identified through asymptomatic testing. The overall AR was 12.9% (Table 1 ); median time at CCJ was 250 days (IQR 98-541), and 598 (95.2%) had been detained for >14 days at the time of their positive test.
Fig 1.
Criteria for inclusion in description of a COVID-19 outbreak in one of the largest jails in the United States—Cook County, IL, March 1–April 30, 2020
Abbreviations: CCSO, Cook County Sheriff's Office; CCJ, Cook County Jail; PCR, polymerase chain reaction assay; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
The average detained person census during the study period was 4,884; the average number of staff on site daily was approximately 1,500. Among 1,256 detained persons and 289 staff with detained person contact epidemiologically linked to CCJ, 479 symptomatic detained persons, 149 asymptomatic detained persons, and 279 symptomatic staff were PCR-positive for SARS-CoV-2 and included in analyses. Self-reported positive SARS-CoV-2 test results by staff were confirmed using the Illinois National Notifiable Disease Surveillance System.
Table 1.
Housing characteristics and COVID cases in one of the largest jails in the United States by housing division—Cook County, IL, March 1–April 30, 2020
| Division name | Type of housing | Date of first case and type | Outbreak duration (days) | Cases among staff* | Cases among detained persons† | Maximum capacity | Division characteristics |
|---|---|---|---|---|---|---|---|
| Intake/release | No housing | March 12, 2020 Staff |
47 | 33 | 20 | N/A | N/A |
| Division 6 | Single cell double cell |
March 13, 2020 Staff |
48 | 25 | 81 | 992 | Engage heavily in activities, work assignments, school, and contact with community members through programming activities. |
| Division 2 (Dorm 4) |
Dormitory | March 16, 2020 Staff |
27 | 10 | 17 | 684 | High turnover. |
| Cermak | Dormitory single cell double cell |
March 17, 2020 Staff |
36 | 9 | 19 | 136 | Delivery of health services, on-site medical personnel. |
| Division 9 | Single cell double cell |
March 21, 2020 Staff |
40 | 18 | 39 | 1,066 | Low turnover. |
| Division 11 | Single cell Double cell |
March 21, 2020 Staff |
37 | 14 | 115 | 1,536 | Heavy engagement in activities and programs. |
| Division 2 (Dorm 2) |
Dormitory | March 24, 2020 Staff |
36 | 12 | 28 | 464 | High turnover. |
| Division 5 | Single cell Double cell |
March 24, 2020 Both |
36 | 25 | 46 | 992 | Expanded to aid social distancing. |
| Division 8 (Residential Treatment Unit) | Dormitory single cell double cell |
March 25, 2020 Detained person |
34 | 42 | 220 | 979 | Houses detained persons with medical comorbidities, including those who use CPAP. |
| Division 2 (Dorm 1) |
Dormitory | March 27, 2020 Staff |
19 | 5 | 0 | 384 | High turnover. |
| Division 10 | Single cell Double cell |
April 1, 2020 Both |
23 | 2 | 15 | 768 | Persons with medical and mental health needs; heavy engagement in activities and educational programs. |
| Division 4 | Single cell | April 6, 2020 Staff |
24 | 3 | 14 | 704 | Opened during physical expansion. |
| Division 2 (Dorm 3) |
Dormitory | April 7, 2020 Detained person |
18 | 3 | 9 | 428 | High turnover; detained persons engage heavily in activities, work assignments, school, and contact with community members. |
Characteristics for all buildings housing detained persons during the study period, plus the site of intake and release, are displayed in the table in order of ascending capacity.
202 staff with work assignments in detained person intake, release, and housing divisions are included in the table; the remaining 77 staff have functional assignments with detained person transportation and movement (31), central kitchen (13), external operations (9), emergency response team (6), laundry (6), offsite (6), mental health treatment center (3), division 16 (1), electronic monitoring (1), or sanitation (1).
All cases among detained persons (asymptomatic and symptomatic) are included and correspond to the housing division in which they were located at the time of symptom onset or specimen collection.
Among staff, 279 cases of SARS-CoV-2 were identified through self-report to CCSO and verified in I-NEDSS, all of whom reported symptoms. Data on staff who tested negative were not available.
Symptomatic cases among detained persons and staff are included in epidemic curves (Fig. 2 and 3 ) and asymptomatic cases among detained persons, including percent testing positive, are displayed by date and division (Supplemental Figure 1).
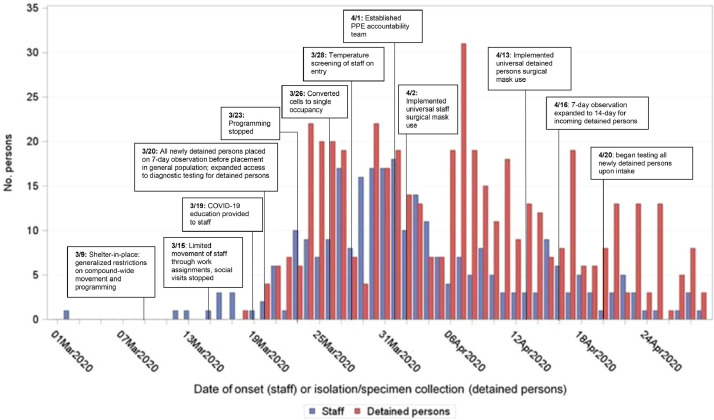
Fig 2.
Number of symptomatic cases of COVID-19 by date of symptom onset among staff and detained persons with timeline of interventions in one of the largest jails in the United States—Cook County, IL, March 1-April 30, 2020 (n = 628).
When constructing the epidemiologic curve, the date of medical isolation as a proxy for the date of symptom onset was used for detained persons, and self-reported symptom onset date was used for staff. Screening for influenza-like illness among incoming detained persons occurs on an annual basis, beginning October 1 of each year; in 2019 it was put in place and then expanded on January 21, 2020 to include symptoms of COVID-19 consistent with CDC guidelines. Screening of asymptomatic detained persons (not displayed in epidemic curve) began on March 3, 2020 among high-risk individuals in the Residential Treatment Unit; testing of all incoming detained persons upon intake began on April 20, 2020.
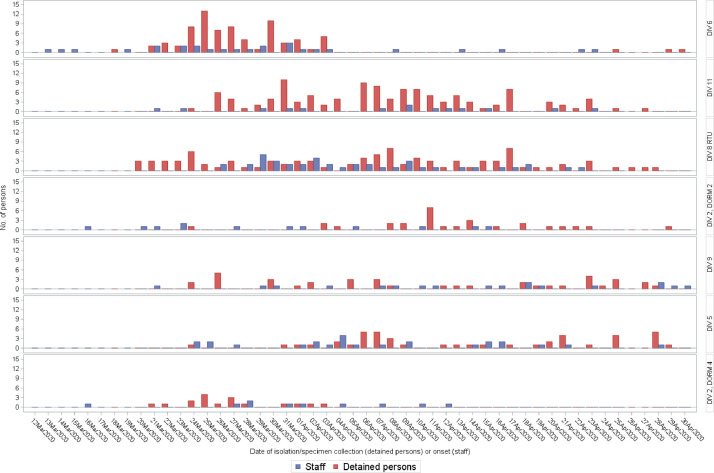
Fig 3.
Number of symptomatic cases of COVID-19 by date of symptom onset among detained persons and staff by housing division in one of the largest jails in the United States—Cook County, IL, March 1–April 30, 2020
Epidemic curves for seven buildings representing six housing divisions (Division 6, Division 11, Division 8 [Residential Treatment Unit], Division 2 Dorm 2, Division 9, Division 5, and Division 2 Dorm 4) with COVID-19 cases among staff and symptomatic detained persons are shown. Building names are labeled on the right hand side of each respective curve. Buildings are those with high case counts compared to remaining buildings not shown (Divisions 10 and 4, Division 2 Dorms 1 and 3, Cermak, and intake/release).
Symptomatic cases
Beginning January 21, 2020, screening of newly detained persons was expanded to include COVID-19 symptoms (cough, shortness of breath, fever) per CDC guidelines5. The earliest reported date of symptom onset in a person later testing positive for SARS-CoV-2—a staff member in the transportation unit (Fig 2)—was March 2. In the week following identification of the first case in a detained person (March 18), 101 additional symptomatic cases (65 in detained persons, 36 in staff) were identified. Symptom onset among all cases peaked March 30, with 39 symptomatic cases (22 in detained persons, 17 in staff). Symptomatic cases among detained persons peaked on April 7 (n = 31).
Interventions
Early interventions included enhanced cleaning and disinfection, eliminating aerosol-generating procedures (eg, continuous positive airway pressure devices [CPAP]) in common areas (beginning March 20), provision of hand hygiene supplies and education, and training staff on personal protective equipment (PPE) use. PPE was provided to all staff.
CCJ began “sheltering in place” March 9, placing generalized restrictions on compound-wide movement and reducing programmatic activity. On March 15, social visitation was suspended, and as of March 20, all newly detained persons were cohorted in small groups (10-30 individuals) under 7-day observation (extended to 14-day on April 16) to monitor symptoms before entering the general population. All programmatic activity was suspended on March 23.
CDPH conducted an on-site assessment on March 25 and provided guidance consistent with interventions already implemented by CHS/CCH. These included symptom screening (later supplemented by COVID-19 testing) at intake, social distancing, immediate medical isolation of symptomatic individuals, and ≥14-day quarantine of all detained persons on a unit where a case had been identified. Social distancing included spacing beds 6 feet apart in a head-to-foot layout in dormitories and reducing all cells to single occupancy beginning March 26 and completed by April 21; this required expansion of the geographic footprint. CDPH expanded infection control guidance for staff, including recommendations for PPE use based on task and cohorting by duty location (Fig 2).
Beginning March 28, all staffs were screened for fever (99.4°F/38°C) and COVID-19 symptoms upon entry into CCJ.5 Presence of fever or symptoms required staff to abstain from work for 14 days. A PPE accountability team was assembled April 1, and staff were required to use surgical masks beginning April 2. Universal surgical mask use by detained persons during waking hours began April 13. On April 20, all newly detained persons were tested on intake using ID NOW in addition to undergoing 14-day quarantine (Fig 2).
Division characteristics and epidemic curves
All nine housing divisions experienced cases despite variation in housing type, capacity, security, and programmatic involvement (Table 1). Epidemic curves for certain divisions demonstrated a traditional bell-shape; others experienced sporadic cases (Fig 3). In 9 of 13 buildings, staff cases arose first, with a median 3 days between the first case in a staff member and a detained person.
Division 6 had the highest level of programmatic activity and was the first to experience symptomatic cases among both detained persons and staff, including 75 among detained persons (16% of all symptomatic cases) and 25 among staff (9% of all staff cases). At the start of the outbreak, detained persons were housed in double cells and had programming involving movement outside of their unit until March 19 (Fig 2).
The Residential Treatment Unit (RTU) housed more individuals with medical needs and at increased risk for COVID-19 due to medical complications than other divisions. RTU had the most symptomatic cases overall (137), including 42 among staff (15% of all staff cases) and 95 among symptomatic detained persons (20% of all symptomatic cases) (Fig 3).
Asymptomatic cases among detained persons
In total, 631 asymptomatic detained persons were tested for SARS-CoV-2; 149 (23.6%) were positive, with percent positive ranging from 8% (2/25, Division 5) to 50% (125/249, RTU; Supplemental Figure 1). The unit with the highest percent positive was a dormitory with 37 individuals in the RTU, which housed individuals with comorbidities, including some who used CPAP until use in common areas was stopped. Of the 275 asymptomatic persons tested upon entry into the jail (newly detained persons), 12 (4.8%) were positive. The 149 cases identified through asymptomatic testing represented 23.7% of all cases among detained persons at CCJ.
Symptomatic infection
All detained persons testing positive (628) were included, and compared based on whether they reported symptoms (479) or were asymptomatic (149). The median age of all detained persons testing positive was 35 years (IQR 27-48). Obesity (BMI ≥30 kg/m2), hypertension, and asthma or COPD were the most common underlying conditions. Among those with hypertension and diabetes, persons more often reported being symptomatic (62% vs 39%, and 62% vs 38%, respectively (P-values: <.01 for both). Additionally, of all persons testing positive, 109 (17%) had a temperature ≥37.7°C, and 72 (11%) had a temperature ≥38°C. Most (95%) with a temperature ≥37.7°C also had other symptoms (Table 2 ).
Table 2.
Characteristics of detained persons testing positive with SARS-CoV-2 — Cook County, IL, 2020
| All positive (N = 628) |
Symptomatic (N = 479) |
Asymptomatic (N = 149) |
P-value | |||
|---|---|---|---|---|---|---|
| Age at first positive test (years), median (IQR) | 35 (27-48) | 34 (27-47) | 40 (28-52) | .01 | ||
| 18-34 | 288 | 232 | 80.6 | 56 | 19.4 | <.01 |
| 35-54 | 226 | 170 | 75.2 | 56 | 24.8 | |
| ≥55 | 91 | 61 | 67.0 | 30 | 33.0 | |
| Underlying conditions, n (%) | ||||||
| HIV | 15 | 10 | 66.7 | 5 | 33.3 | .4 |
| Asthma, COPD | 146 | 104 | 71.2 | 42 | 28.8 | .1 |
| Cirrhosis | 9 | 5 | 55.6 | 4 | 44.4 | .1 |
| Diabetes | 98 | 61 | 62.2 | 37 | 37.8 | <.01 |
| Hypertension | 187 | 115 | 61.5 | 72 | 38.5 | <.01 |
| Obese | 233 | 171 | 73.4 | 62 | 26.6 | .2 |
| Clinical presentation and outcome, n (%) | ||||||
| Temperature (Celsius) | ||||||
| ≥37.7° | 109 | 104 | 95.4 | 5 | 4.6 | <.01 |
| ≥38° | 72 | 71 | 98.6 | 1 | 1.4 | <.01 |
| Died | 5 | 4 | 80.0 | 1 | 20.0 | 1.0 |
COPD, chronic obstructive pulmonary disease.
Temperature reflects measurement closest to date of positive specimen collection.
Obesity defined as Body Mass Index ≥30 kg/m2.
Mortality
Seven detained persons and two staff died (case-fatality rate for both = 1.1%). Of fatal cases among detained persons, ages ranged from 42 to 64 years; all were male and had multiple comorbidities, most commonly hypertension, hyperlipidemia, and obesity10.
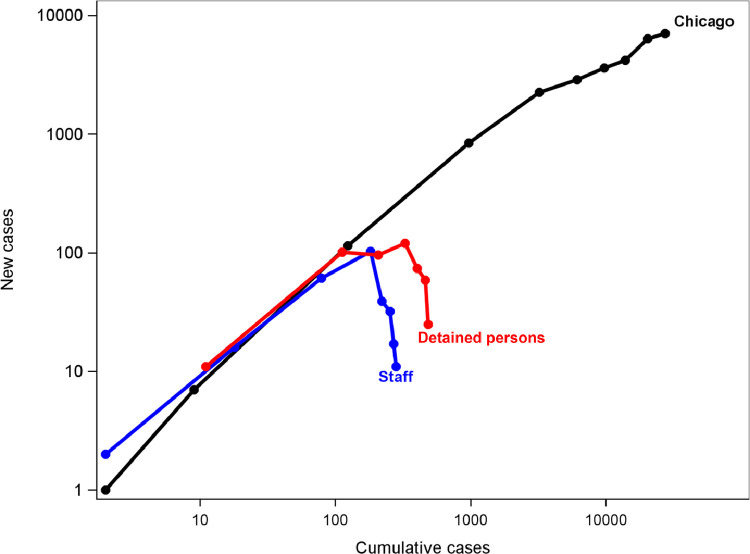
Outbreak trajectory
Early in the outbreak, increases in cases among staff and detained persons paralleled that in Chicago, Illinois. After implementation of interventions, cases declined in detained persons and staff, even as cases increased dramatically in Chicago (Fig 4 ). Weekly averages demonstrated a decline in cases among detained persons a week after staff cases began declining.
Fig 4.
Ratio of new to cumulative cases among detained persons and staff in Cook County Jail compared to Chicago—IL, March 1-April 30, 2020.
Ratios of new cases to cumulative cases were calculated for each week of the study period among detained persons, staff, and residents of Chicago and plotted on a logarithmic scale to show outbreak trajectories. For staff, all symptomatic persons with validated molecular test results from the Illinois National Notifiable Disease Surveillance System (I-NEDSS) were included using date of onset as the referent time point; all asymptomatic and symptomatic detained persons testing PCR-positive were included using date of symptom onset or specimen collection as the referent time point. Data for all persons residing in the state of Illinois meeting the case definition for confirmed SARS-CoV-2 infection were extracted from the I-NEDSS system and included using the date of specimen collection.
Each node represents 1 week of the study period; the highest number of total cases were identified in the jail the week of April 5th and fell thereafter. The initial doubling times for Chicago, staff, and detained persons were 2.22, 2.15, and 2.1 days, respectively, represented by the increasing slope prior to peak for each population.
Discussion
Less than 2 months after the first COVID-19 case was identified in CCJ, almost 1,000 detained persons and staff had been infected with SARS-CoV-2. This represents an AR of nearly 13% among detained persons and occurred despite early adoption of containment and mitigation practices. This constitutes one of the largest outbreaks of COVID-19 in a congregate setting described to date, illustrating the difficulties of controlling spread in correctional and detention facilities. Estimates of influenza spread in enclosed populations have found similar ARs (13%)9; experience suggests viral respiratory pathogens like COVID-19 can cause sizeable epidemics in large jails despite implementation of public health interventions10. Expanding CCJ's footprint to facilitate physical distancing, limiting movement, and implementing expanded testing were complex and resource-intensive interventions, but effectively slowed spread relative to the surrounding community even as cases there surged. Implementing expanded diagnostic testing at key points, such as intake, helped limit new introductions of the virus.
Investigations into outbreaks of respiratory viruses in other correctional and detention facilities have identified visitors11 and persons transferred between facilities12 as possible sources. Restriction of movement within the jail was likely one of the most critical and timely interventions in gaining control of this outbreak; the division with the highest level of movement and most contact with individuals entering from the community experienced the earliest peak. Implementation and enforcement of social distancing of ≥6 feet, surgical mask use, increased access to soap and alcohol-based hand sanitizer, and enhanced cleaning and disinfection practices also likely reduce extent of spread. Later expansion of diagnostic testing, including at intake and of asymptomatic individuals, allowed for medical isolation of cases and reduction in spread. Enhanced measures including PPE accountability, including CCSO establishing a PPE Accountability Team who performed walking rounds on the compound to assess PPE compliance among CCSO staff, were likely also effective.
Our data suggest the important role that community-dwelling staff played in COVID-19 introductions into CCJ as cases among staff often preceded cases in detained persons. We also show the effectiveness of employee interventions despite inclusion of <100% of personnel, as vendor and contractors could not be reliably included, nor the same policies enforced; however, temperature and symptoms screening upon entry to CCJ was universal. Implementation of universal screening for symptoms and temperature checks is important, but ensuring access to testing and compliance with illness reporting are vital, as are flexible and non-punitive leave policies to allow sick employees to stay home.
As with other outbreaks in correctional and detention facilities13, close cooperation between onsite medical service providers, correctional staff, and local and federal public health officials were critical to successful containment of SARS-CoV-2. Efforts to facilitate social distancing and medical isolation through expanding CCJ's footprint likely reduced transmission14. Physical distancing to the degree accomplished at CCJ may not be feasible in all facilities, but use of quarantine and cohort housing may be possible even in smaller, more restricted facilities.
Of all persons testing positive, the majority (76%) reported symptoms. Whereas asthma or COPD, diabetes, hypertension, and obesity were all common in this population, only those with diabetes and hypertension were found to be significantly associated with being symptomatic when testing positive. A substantial portion (24%) of persons testing positive were asymptomatic, similar to other congregate settings such as homeless shelters15. The role of these individuals in SARS-CoV-2 transmission is not well understood16. Widespread testing facilitates rapid identification, early medical isolation, and reduction in potential for spread, though and early widespread testing can prevent further cases17. Newly detained persons are exposed to the community prior to entering the jail, making expanded testing and cohorting at intake essential to limiting transmission.
This investigation has several limitations. First, testing capacity was limited early in the outbreak, potentially underestimating the number of cases; comprehensively employed mitigation methods reduced transmission even in the absence of full testing capacity. Also, since temperature ≥37.7°C prompted testing, results may be biased toward a higher proportion of persons testing positive also exceeding the temperature of 37.7°C. Our case definition required a positive PCR result; this may have excluded staff who were diagnosed clinically, or who had only serology performed. Further, while CCSO staff represented the largest group of staff members entering CCJ, other staff (eg, healthcare staff) had a wide range of employers with no centralized listing and were not included in the study. Lastly, because interventions were often implemented simultaneously, it was difficult to ascertain relative effectiveness; and this manuscript focuses on a specific period of time, but does not assess whether the interventions were effective long-term. Additionally, we do not comment on interventions put in place in Chicago at the time, and so we cannot attribute causality to the CCJ interventions and difference in cases in the community.
The described interventions collectively proved effective in mitigation of the spread of SARS-CoV-2. However, it is important to acknowledge that increased isolation and use of single-celled environments, restricted visitation, and reduced programming may have negative impact outside the context of infection prevention. While not measured in this review, exacerbation of behavioral health issues should be considered.
Conclusion
SARS-CoV-2 can spread rapidly in correctional and detention facilities, causing significant morbidity and mortality. Effective response to the COVID-19 outbreak at CCJ demonstrates the need for dynamic and aggressive application of intervention strategies, but also shows how timely response can reduce case counts and prevent morbidity and mortality in correctional or detention facilities.
Acknowledgments
We would like to acknowledge the contributions of Cook County Sheriff Thomas J. Dart, Dr Andrew Defuniak, Dr Stamatia Richardson, Michael Miller, Brad Curry, Tarry Williams, and Linda Follenweider for their tireless efforts to implement these interventions. We would also like to acknowledge Jaqueline Tate, Kathryn Curran, Reena Doshi, Patrick Moonan, and the CDC field study team for their support. Mary Ann K. Hall, Sharon Saydah, and Louise K. Francoise Watkins contributed meaningfully to the review of this manuscript.
Footnotes
Conflicts of interest: The authors of this manuscript have all reviewed and approved of publication and declare no conflicts of interest.
Funding: Support was provided from standard operating budgets and no additional grants or external funding sources were provided.
Detained persons encompasses detained and incarcerated individuals; the majority of individuals were detained pre-trial, with a smaller portion post-sentencing.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.ajic.2021.03.020.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Kinner SA, Young JT, Snow K. Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health. 2020;5:e188–e189. doi: 10.1016/S2468-2667(20)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McMichael TM, Currie DW, Clark S. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kakimoto K, Kamiya H, Yamagishi T. Initial investigation of transmission of COVID-19 among crew members during quarantine of a cruise ship — Yokohama, Japan, February 2020. MMWR Morb Mortal Wkly Rep. 2020;69:312–313. doi: 10.15585/mmwr.mm6911e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallace M, Hagan L, Curran KG. COVID-19 in correctional and detention facilities — United States, February–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:587–590. doi: 10.15585/mmwr.mm6919e1. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Interim guidance on management of coronavirus disease 2019 (COVID-19) in correctional and detention facilities. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html. Accessed April 20, 2021.
- 6.Okano JT, Blower S. Preventing major outbreaks of COVID-19 in jails. The Lancet. 2020;395:1542–1543. doi: 10.1016/S0140-6736(20)31015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dolan K, Wirtz AL, Moazen B. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. The Lancet. 2016;388:1089–1102. doi: 10.1016/S0140-6736(16)30466-4. [DOI] [PubMed] [Google Scholar]
- 8.Maruschak LM, Sabol WJ, Potter RH. Pandemic influenza and jail facilities and populations. Am J Public Health. 2009;99(S2):S339–S344. doi: 10.2105/AJPH.2009.175174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finnie TJR, Copley VR, Hall IM. An analysis of influenza outbreaks in institutions and enclosed societies. Epidemiol Infect. 2014;142:107–113. doi: 10.1017/S0950268813000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montoya-Barthelemy AG, Lee CD, Cundiff DR. COVID-19 and the correctional environment: The american prison as a focal point for public health. Am J Prevent Med. 2020;58:888–891. doi: 10.1016/j.amepre.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Awofeso N, Fennell M, Waliuzzaman Z. Influenza outbreak in a correctional facility. Aust N Z J Public Health. 2001;25:443–446. [PubMed] [Google Scholar]
- 12.Stanley L.L. Influenza at San Quentin Prison, California. Public Health Reports. 1919;34:996–1008. [Google Scholar]
- 13.Chao W-C, Liu P-Y, Wu C-L. Control of an H1N1 outbreak in a correctional facility in central Taiwan. J Microbiol Immunol Infect. 2017;50:175–182. doi: 10.1016/j.jmii.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Akiyama MJ, Spaulding AC, Rich JD. Flattening the curve for incarcerated populations - Covid-19 in jails and prisons. N Engl J Med. 2020;382:2075–2077. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baggett TP, Keyes H, Sporn N. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020;323:2191–2192. doi: 10.1001/jama.2020.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arons MM, Hatfield KM, Reddy SC. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hatfield KM, Reddy SC, Forsberg K. Facility-wide testing for SARS-CoV-2 in nursing homes—seven U.S. jurisdictions, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1095–1099. doi: 10.15585/mmwr.mm6932e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.