Abstract
Background: More than 300 million smokers make China the largest cigarette consumer globally, which is a huge economic burden. Smoking cessation (SC) clinics can offer counseling and follow-up services. The operational experience of SC clinics in China needs to be summarized and improved based on research evidence.
Purpose: The objectives of this study were to describe quit rates among attendees of SC clinics in Hunan and assess predictors of successful SC.
Methods: The participants in this study were smokers who visited the SC clinic of Hunan Cancer Hospital from February 1, 2015 to September 30, 2018. Individuals who received individual counseling and assessment from the SC clinic staff and were willing to quit smoking were eligible for inclusion. Those with critical illness or cancer were excluded. Application of smoking cessation clinic registration form (unified by Chinese Center for Disease Control and Prevention) was used to assess participants at the consultation. Follow-ups and counseling were performed over telephone at 1 week, 1 month, and 3 months after the initial cessation consultation or in times of need. Successful SC was checked for at 3 months after the start of SC.
Results: A total of 328 smokers (mean age 45.67 ± 12.38 years) had participated. The abstinence rate at 3 months was 28.4%. Binary regression analysis revealed significant independent predictors to be the total numbers of SC follow up sessions, previous SC attempts, and participants' decision on when to quit smoking (The relative to quit immediately group, quit within 30 days, quit after 30 days, and undecided quit were less likely to succeed in quitting. while quit within seven days had no statistical significance.
Conclusion: SC clinics can achieve a desirably high quit rate. Participant's previous attempts at quitting, three or more follow-ups, and the decision to quit immediately or within seven days were factors helpful in predicting the success of SC.
Keywords: smoking cessation, smoking cessation clinic, quitting predictor, smoker characteristic, smoking, abstinence rates, smoking quit rate, multivariate binary regression
Introduction
Smoking is the leading preventable cause of death worldwide (1). Smoking rates in China remain high; in the past 30 years, some progress in cigarette control has been made in China, with the smoking rate among men dropping from 61% in 1984 to 50.5% in 2018 (2, 3). However, it is still higher than the world average (36.1%) and European average (39.0%) (4). Studies have shown that smoking cigarettes can lead to a variety of malignant tumors, especially lung cancer (5–7). In addition, 10% of cardiovascular deaths can be attributed to smoking (8). Smoking 20 cigarettes daily was found to increase the risk of coronary heart disease by 127% in men and 295% in women. Even one cigarette per day increased the risk of coronary heart disease by 74% in men and 119% in women (9).
Quitting smoking plays a key role in greatly reversing preexisting damage and restoring health (10). People who quit smoking are less likely to have diseases than persistent smokers (11). Studies have shown that smoking cessation (SC) reduces the morbidity and mortality of smokers at any age (12). Smokers who give up smoking before the age of 40 can reduce their risk of mortality from smoking-related diseases by 90% compared to that of persistent smokers (13). For cancer patients, cigarette cessation can improve their prognosis, reduce the risk of a second primary tumor in the future, and increase their lifespan (14). Moreover, SC improves quality of life and longevity while rapidly reducing the risk of heart diseases (15).
Despite extensive smoking control efforts in China, cigarette smoking remains a challenging social and public issue. It has been reported that, without proper guidance and planning, approximately one-third of current Chinese male smokers will die from smoking-related diseases by 2030 (16). More than 40% of smokers attempt to quit every year, and only 3–5% succeed without help from a health care provider (17). However, with cessation aid provided by medical staff, the cessation rate increased (18), and brief advice was shown to increase quitting rates by 1–3% (19). There is evidence that cessation advice and counseling can increase successful quitting rates by ~3% (20). Huang et al. (21) reported that people who quit smoking were assessed over the phone interview and asked to report their quit status.
The WHO recommends offering cessation services as a part of primary health care (22). These services mainly include SC clinics, quit lines, pharmacotherapy, and health professionals who provide brief advice to smokers on quitting smoking as they avail health services (23). SC clinics where physicians and other health care providers give brief, professional advice are necessary to help smokers quit and decrease the health burden of tobacco smoking (24).
Furthermore, it is important for SC professionals to guide cessation based on evidence of predictor success. Predictors of successful SC include factors such as number of previous SC attempts, reasons to quit, setting a SC date, health status, and influence of family members. According to a study in Guangzhou, China, smokers who were confident and took the initiative to quit were more likely to succeed, with a prevalence quit rate of 24% after 6 month and 7 days (25). Jampakla et al. (26) studied 2,000 individuals who quit smoking at the SC clinics in Thailand, showed that age, cigarette consumption, and self-assessed addiction were the factors that reduced relapse. See et al. (27) reported a 27.6% abstinence rate after 6 months among inpatients who quit smoking; Of them, those who had adopted the cold turkey method and faced social pressure were more likely to succeed. Another study revealed that tobacco users with a relatively high socioeconomic status were more likely to have tried to quit (28). Hagimoto et al. (29) reported that the more nicotine dependent a smoker is, the less likely they are to succeed in quitting. A study of women quitting smoking in Saudi Arabia found that the most common reason for quitting was concern for their health, while the least likely reason was the fear that smoking affected their mood (30). Some studies showed that individualized consultation by medical staff improved the SC rates, and that consultation intensity had a strong dose-response relationship with the success rate of smoking cessation; consultation frequency of four or more was the most beneficial (1). A meta-analysis indicated that a brief tobacco intervention was also effective (31). Hence, we can infer that regular follow-up counseling may have a significant positive influence on SC.
SC clinics have been set up in hospitals in major cities in China since 2008. Alongside their effectiveness in improving SC rates, there is also evidence supporting their cost-effectiveness (1). SC clinic operation and experience of clinic attendees need to be summarized to make continuous improvement. In this study, we aimed to describe smoking behavior and determine smoking quit rates among people attending SC clinics. We also aimed to study predictors of successful SC.
Methods
Study Setting and Participants
This study was carried out in the SC clinic of Hunan Cancer Hospital (a tertiary cancer teaching hospital), which was set up in 2015. The clinic offers free quit-smoking service on two of the weekday afternoons (Tuesdays and Fridays) and a SC hotline during working hours. Individuals who were willing to quit smoking from February 1, 2015 to September 30, 2018 were included in the study. They came to the clinic by themselves or were referred by doctors. Some participants were also recruited from the communities; clinic nurses visited communities once a month to offer advice to residents about quitting smoking, as well as to recruit participants who wanted to quit smoking. Participants with critical illness such as cancer were excluded. This study was approved by the Ethics Committee of Hunan Cancer Hospital (KYJJ-094). Oral informed consents were obtained from all participants.
Sample Size Calculation
In this study, the sample size formula required to estimate the population rate is: . It is known that the smoking cessation rate of patients receiving smoking cessation intervention in smoking cessation clinic of six hospitals in Chengdu is 9.7% at 3 months (32), α = 0.05, U0.05/2 = 1.96, δ = 0.05, and the sample size is calculated to be at least 135 cases. Considering the 20% loss of follow-up rate, the estimated sample number should be at least 162 cases. Based on the above literature evidence, the team was only able to select the 3-month smoking cessation rate as the calculation criterion which is relatively low. Before 2013, China's smoking cessation clinics have not been carried out on a large scale. In recent years, the Chinese government has vigorously promoted tobacco control propaganda to improve public health literacy, which is conducive to increasing the smoking cessation rate. Combined with the smoking cessation rate in research of Aung et al. (33), the sample size of this study should be increased predictably.
Definition and Evaluation of Indicators
Participants were assessed by the SC clinic doctors or nurses and provided with individual counseling at the time of their initial visit or consultation. The first assessment included collecting information on participants' demographic data, nicotine dependence, and willingness to quit smoking. Smoking cessation reasons and motivation are assessed (Table 2). The questionnaire used was designed by the Chinese CDC (34).
Demographic Information and General Condition
Demographic information of participants included gender, age, occupation, and education level. Participants general condition (well, fair, poor) was assessed by the doctors or nurses of SC clinic.
Nicotine Dependence and Smoking Status
Nicotine dependence was assessed according to the Fagerstrom Test for Nicotine Dependence (FTND) (35). Its scores were categorized as the following: 0 as no dependency, 1–3 as low dependency, 4–6 as moderate dependency, and 7–10 as severe dependency. Information about daily cigarette consumption and smoking duration were also collected.
CO Level Test
Smokers are given CO tests when they consulted with the SC clinic nurses or doctors. Exhalatory carbon monoxide test value (ppm): 0–6 for non-smoking; 7–10 are light smoking; 11–20 were moderate smoking; 21–72 are heavy smoking (36).
Operational Definitions
Smokers
According to WHO (35), smokers are defined as those who smoke continuously or accumulatively for 6 months or more in their lifetime. Regular smokers are defined as smokers who smoke ≥ 1 cigarette per day for more than half a year (37).
A former smoker is one who had smoked one cigarette per day for at least 6 months and had quit at the time of the survey (38).
Attempts to Quit Smoking
It includes any attempt by a smoker to quit smoking within the past 12 months (39).
Assessment of Smoking Cessation
After the initial consultation, standardized telephone follow-up assessments were conducted by the same group of trained investigators at 1 week, 1 month, and 3 months. The abstinence time was calculated as beginning from the day the individual stopped smoking to the day of the assessment. Smokers who did not go to the SC clinic in person were assessed by telephonic interview (21). Rather than directly asking whether they had quit smoking, they were asked how many cigarettes they smoked per day. Those who answered that they no longer smoked were considered successful quitters.
Success in Smoking Cessation
This was decided based on the self-report of smokers who have maintained their smoking cessation status from the beginning of treatment until the end (34).
Assistance in Quitting
Face-to-Face Consultation
Trained nurses and doctors provided face-to-face SC counseling for 20–30 min during the first consultation of the participants.
Behavioral Support
Detailed counseling and a brief advice (19, 40) was given to participants during consulting and telephonic interview, respectively. The 5As/5Rs, given by Prochaska and Goldstein (41), were also applied to SC. The “5As” refers to ask, advice, appraise, assistance, and arrangement. The “5Rs” are measures that enhance the motivation to quit smoking; they include relevancy, risk, reward, road block, and repeat.
Follow Up Guidelines
At least three follow-up sessions took place over the telephone, at 1 week, 1 month, and 3 months, after the initial visit by clinic nurses to the community. Follow-ups were provided according to the individual's needs. With every follow up, behavioral support and health education were given to the participant. Additionally, the staff also filled out the standard evaluation form at the three follow-ups. According to the results of these three assessments, the help required by the participants was determined: (1) for those who had successfully adhered to the goal of SC, medical staff provided guidance for successfully dealing with withdrawal symptoms and encouraged participants to continue cessation in order to increase their confidence and prevent relapse; (2) for smokers who had not yet quit, medical staff tried to understand the resistance to SC and emphasized the harm of smoking and benefits of SC; and (3) participants who relapsed after quitting were encouraged to use medication or given advice about another attempt.
Lost to Follow-Up
Those whose telephone numbers were wrong and who never answered were counted as lost participants at the first follow up. Those whose telephone numbers could be rung but who did not answer after seven or more times were considered to have failed in SC.
Medication Therapy
SC medication therapy is advised for people who want to quit smoking (23). SC doctors prescribed the medication for those who were willing to quit if the participants agreed.
Statistical Analysis
Data were entered and analyzed using SPSS version 18.0 (SPSS, Chicago, IL, USA). Descriptive statistics were calculated for demographic information and smoking status. We performed univariate analyses with chi-square tests between the SC success group and the SC failed group. A binary regression analysis was used to identify the factors predicting 3 months of cessation. Odds ratios (ORs) and 95% confidence intervals (CIs) were evaluated in multivariable analysis. A P-value < 0.05 denoted statistical significance.
Results
Overall SC Rate and the Participant Baseline Characteristics
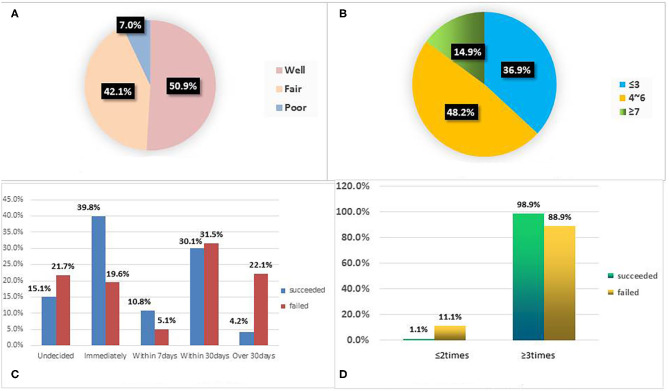
A total of 335 participants were enrolled in this study. Seven participants with incomplete data were excluded, and the final sample included 328 participants. We were unable to contact 12 participants among them; the lost to follow-up rate was 3.67% (12/328). The overall SC rate at 3 months was 28.4% (93/328). There were 97.6% male participants (320/328) and only 2.4% (8/328) female participants. The mean age of the participants was 45.67 ± 12.38 years. The youngest and oldest participants were 18 and 80 years old, respectively. In terms of education, 8.2, 31.7, 27.2, and 32.9% of the participants had primary school or less, junior high school, senior high school, and college education or above, respectively. The most common occupation was enterprise/business/service personnel (39.6%), followed by farmers (24.1%). In terms of health assessment, 50.9% (167/328) participants' general condition was well, while 7.0% (23/328) were in poor condition (Figure 1A). Univariate analysis showed that there was no significant difference in gender, age, education level, occupation, duration of smoking habit, daily cigarette consumption, nicotine dependence score, CO test, and SC aids between the SC success group and the SC failed group (P > 0.05). However, the total number of SC follow up sessions (P = 0.003), the number of previous SC attempts (P = 0.002), health assessment (P = 0.031), and date of SC (P < 0.001) were significantly different between the two groups (Table 1).
Figure 1.
(A) Health assessment represents the proportion of the subjective assessment of physical condition grade of 328 patients; (B) Fagerstrom score represents the proportion of Fagerstrom Test for Nicotine dependence among 328 patients. (C) Date of SC represents the proportional distribution characteristics of the expected start time of smoking cessation between the successful and unsuccessful smoking cessation groups; (D) Follow ups represents the proportional distribution characteristics of the number of follow-up visits between the successful group and the failed group. SC, smoking cessation.
Table 1.
Clinical characteristic of participants between success group and failure group in SC for 3 months.
| Variables | Total (n = 328) | Abstinence succeeded (n = 93) | Abstinence failed (n = 235) | χ2 | P |
|---|---|---|---|---|---|
| Gender | 0.034a | 0.854 | |||
| Male | 320 (97.6) | 90 (28.1) | 230 (71.9) | ||
| Female | 8 (2.4) | 3 (37.5) | 5 (62.5) | ||
| Age (y) | A:45.67 ± 12.38 | 1.797 | 0.407 | ||
| 18–40 | 110 (33.6) | 32 (29.1) | 78 (70.9) | ||
| 41–59 | 167 (50.9) | 43 (25.7) | 124 (74.3) | ||
| ≥60 | 51 (15.5) | 18 (35.3) | 33 (64.7) | ||
| Education Level | 1.943 | 0.584 | |||
| Primary school or less | 27 (8.2) | 5 (18.5) | 22 (81.5) | ||
| Middle school | 104 (31.7) | 28 (26.9) | 76 (73.1) | ||
| High school | 89 (27.2) | 26 (29.2) | 63 (70.8) | ||
| College school or above | 108 (32.9) | 34 (31.5) | 74 (68.5) | ||
| Occupation | 5.660 | 0.462 | |||
| Teachers | 7 (2.1) | 2 (28.6) | 5 (71.4) | ||
| Medical staff | 21 (6.4) | 8 (38.1) | 13 (61.9) | ||
| Government/institution staff | 27 (8.2) | 9 (33.3) | 18 (66.7) | ||
| Retired/unemployed | 31 (9.5) | 13 (41.9) | 18 (58.1) | ||
| The others | 33 (10.1) | 9 (27.3) | 24 (72.7) | ||
| Farmers | 79 (24.1) | 18 (22.8) | 61 (77.2) | ||
| Enterprise/business/service personnel | 130 (39.6) | 34 (26.2) | 96 (73.8) | ||
| Health Assessment | 6.936 | 0.031 | |||
| Well | 167 (50.9) | 45 (26.9) | 122 (73.1) | ||
| Fair | 138 (42.1) | 36 (26.1) | 102 (73.9) | ||
| Poor | 23 (7.0) | 12 (52.2) | 11 (47.8) | ||
| Duration of smoking (y) | A: 22.81 ± 12.32 | 1.377 | 0.711 | ||
| ≤10 | 73 (22.3) | 23 (31.5) | 50 (68.5) | ||
| 11–20 | 94 (28.7) | 24 (25.5) | 70 (74.5) | ||
| 21–30 | 90 (27.4) | 28 (31.1) | 62 (68.9) | ||
| ≥31 | 71 (21.6) | 18 (25.4) | 53 (74.6) | ||
| Daily cigarettes consumption | A: 21.85 ± 11.36 | 2.587 | 0.460 | ||
| ≤10 | 61 (18.6) | 22 (36.1) | 39 (63.9) | ||
| 11–20 | 175 (53.4) | 48 (27.4) | 127 (72.6) | ||
| 21–30 | 52 (15.9) | 14 (26.9) | 38 (73.1) | ||
| ≥31 | 40 (12.1) | 9 (22.5) | 31 (77.5) | ||
| SC attempts previously | 9.282 | 0.002 | |||
| Yes | 212 (64.6) | 72 (34.0) | 140 (66.0) | ||
| No | 116 (35.4) | 21 (18.1) | 95 (81.9) | ||
| Fagerstrom score | A: 4.27 ± 2.12 | 2.128 | 0.345 | ||
| ≤3 | 121 (36.9) | 40 (33.1) | 81 (66.9) | ||
| 4–6 | 158 (48.2) | 41 (25.9) | 117 (74.1) | ||
| ≥7 | 49 (14.9) | 12 (24.5) | 37 (75.5) | ||
| CO test results | 0.881 | 0.644 | |||
| 0–5 | 37 (22.1) | 8 (21.6) | 29 (78.4) | ||
| 6–10 | 25 (15.0) | 8 (32.0) | 17 (68.0) | ||
| 11–72 | 105 (62.9) | 29 (27.6) | 76 (72.4) | ||
| Date of SC | 20.512 | 0.000 | |||
| Undecided | 65 (19.8) | 14 (21.5) | 51 (78.5) | ||
| Immediately | 83 (25.3) | 37 (44.6) | 46 (55.4) | ||
| Within 7 days | 22 (6.7) | 10 (45.5) | 12 (54.5) | ||
| Within 30 days | 102 (31.1) | 28 (27.5) | 74 (72.5) | ||
| Over 30 days | 56 (17.1) | 4 (7.1) | 52 (92.9) | ||
| Follow up | A:2.81 ± 0.66 | 8.800 | 0.003 | ||
| ≤2 | 27 (8.2) | 1 (3.7) | 26 (96.3) | ||
| ≥3 | 301 (91.8) | 92 (30.6) | 209 (69.4) | ||
| SC adds | 0.131* | ||||
| BS | 316 (96.4) | 87 (27.5) | 229 (72.5) | ||
| BS and Medication | 6 (1.8) | 4 (66.7) | 2 (33.3) | ||
| BS and EC | 6 (1.8) | 2 (33.3) | 4 (66.7) |
A, mean ± standard deviation,
continuous correction Value; SC, smoking cessation; BS, behavior support; EC, electronic cigarettes.
Monte Carlo P.
Participants' Smoking Behavior Prior to Consultation
Among the current smokers, the average duration of smoking was 22.81 ± 12.32 years, and the average consumption per day was 21.85 ± 11.36 cigarettes. A significant proportion of smokers (77.7%) had smoked for more than 10 years, with the longest smoking period being 60 years. Over 80% participants smoked 10 cigarettes or more per day, with the highest proportion of participants smoking 11–20 cigarettes per day (53.4%).
A total of 64.6% participants (212/328) had previously made quitting attempts. The SC success group had a higher rate of previous attempts than the SC failed group (77.4 and 59.6%, respectively) (Table 1).
Nicotine Dependence Score and CO Tests Results
FTND assessment results showed an average nicotine dependence score of 4.27 ± 2.12 (Figure 1B). CO tests were performed using a gas detector on 167 participants who were willing to accept the procedure. Results showed that heavy smokers and light smokers accounted for 80.7% (105/130) and 19.3% (25/130) of the participants who received the CO test, respectively (Table 1).
The Quitting Date and the Methods Used to Assist in Quitting Smoking
In relation to the quitting dates of the 328 participants, 25.3% (83/328) quit immediately, 6.7% (22/328) quit within seven days, 31.1% (102/328) quit within 30 days, 17.1% (56/328) decided to quit after 30 days, and 19.8% (65/328) did not decide when to quit (Figure 1C).
Every participant received at least one counseling session. In the SC success group, 98.9% (92/93) participants received three or more follow-ups. For the SC failure group, this figure was 88.9% (209/235). The mean follow-up frequency was 2.81 ± 0.66 (Figure 1D). During the 3-month SC follow-up, 96.4% (316/328) of the participants received only behavioral support interventions, 1.8% (6/328) received pharmacotherapy and behavioral support interventions, and 1.8% (6/328) chose e-cigarette as a means of self-assisted SC in addition to behavioral support interventions (Table 1).
Reasons and Motivations for Quitting Smoking
The top four reasons and motivations for quitting smoking were the following: (1) awareness of the hazards of smoking and wanting to return to a healthy life, (2) belief that smoking was causing a gradual decline in one's health, (3) family demands, and (4) knowing someone who was sick from smoking. They accounted for 74.4% (224/328), 24.4% (80/328), 19.5% (64/328), and 15.9% (52/328), respectively. Other reasons and motivations to quit smoking were that their friends disliked them for smoking, they could afford to quit, and that they could not smoke in places that were non-smoking for fear of causing trouble among other reasons. There was no statistically significant difference in the analysis of smoking cessation reasons and motivation between the SC successful group and the SC failure group (P > 0.05) (Table 2).
Table 2.
Univariate analysis of smoking cessation reasons and motivation of participants.
| Variables | Total (n = 328) | Succeeded (n =93) | Failed (n = 235) | χ2 | P |
|---|---|---|---|---|---|
| Knowing the hazards of smoking | |||||
| No | 84 (25.6) | 29 (34.5) | 55 (65.5) | 2.116 | 0.146 |
| Yes | 224 (74.4) | 64 (26.2) | 180 (73.8) | ||
| Decline in health | 2.301 | 0.129 | |||
| No | 248 (75.6) | 65 (26.2) | 183 (73.8) | ||
| Yes | 80 (24.4) | 28 (35.0) | 52 (65.0) | ||
| Knowing somebody sick because of smoking | 0.847 | 0.357 | |||
| No | 276 (84.1) | 81 (29.3) | 195 (70.7) | ||
| Yes | 52 (15.9) | 12 (23.1) | 40 (76.9) | ||
| Family asks to quit smoking | 3.274 | 0.070 | |||
| No | 264 (80.5) | 69 (26.1) | 195 (73.9) | ||
| Yes | 64 (19.5) | 24 (37.5) | 40 (62.5) | ||
| People around me hate me smoking | 0.007 | 0.931 | |||
| No | 290 (88.4) | 82 (28.3) | 208 (71.7) | ||
| Yes | 38 (11.6) | 11 (28.9) | 27 (71.1) | ||
| Have ability to quit smoking myself | 0.000 | 1a | |||
| No | 313 (95.4) | 89 (28.4) | 224 (71.6) | ||
| Yes | 15 (4.6) | 4 (26.7) | 11 (73.3) | ||
| Avoid the hassles caused in non-smoking places | 0.000 | 1a | |||
| No | 316 (96.3) | 90 (28.5) | 226 (71.5) | ||
| Yes | 12 (3.7) | 3 (25.0) | 9 (75.0) | ||
| Take part in sports | 0.195⋆ | ||||
| No | 325 (99.1) | 91 (28.0) | 234 (72.0) | ||
| Yes | 3 (0.9) | 2 (66.7) | 1 (33.3) | ||
| Avoid conflicts with family | 0.021 | 0.885a | |||
| No | 313 (95.4) | 88 (28.1) | 225 (71.9) | ||
| Yes | 15 (4.6) | 5 (33.3) | 10 (66.7) | ||
| Avoid trouble at school/workplace | 0.000 | 1a | |||
| No | 320 (97.6) | 91 (28.4) | 229 (71.6) | ||
| Yes | 8 (2.4) | 2 (25.0) | 6 (75.0) | ||
| Improve grooming and eliminate bad odors | 0.513 | 0.474a | |||
| No | 316 (96.3) | 88 (27.8) | 228 (72.2) | ||
| Yes | 12 (3.7) | 5 (41.7) | 7 (58.3) | ||
| Increase appetite/weight | 0.000 | 1a | |||
| No | 321 (97.9) | 91 (28.3) | 230 (71.7) | ||
| Yes | 7 (2.1) | 2 (28.6) | 5 (71.4) | ||
| The Others | 0.533 | 0.465a | |||
| No | 322 (98.2) | 90 (28.0) | 232 (72.0) | ||
| Yes | 6 (1.8) | 3 (50.0) | 3 (50.0) | ||
| Number of reasons and motivations for quitting | 0.833* | ||||
| 0 | 16 (4.9) | 3 (18.8) | 13 (81.2) | ||
| 1 | 205 (62.5) | 60 (29.3) | 145 (70.7) | ||
| 2 | 51 (15.5) | 15 (29.4) | 36 (70.6) | ||
| ≥3 | 56 (17.1) | 15 (26.8) | 41 (73.2) |
Continuity correction,
The monte carlo P-Value,
Fisher P-Value.
The Predictor Factors of SC
The factors with statistical significance in univariate analysis were included in binary logistic regression to assess the predictors of successful SC at 3 months. We found that previous SC attempts, date of SC, and follow-ups were independent predictors of a 3-month success in SC. The results showed that smokers who had three or more follow-ups were more likely to quit smoking than those who had no more than two follow-ups (OR = 13.266, 95% CI: 1.725–101.991, P = 0.013). Compared with those who had never tried to quit before, participants who had made previous attempts at quitting were more than twice as likely to quit (OR = 2.070, 95% CI: 1.155–3.709, P = 0.015). Those who chose to quit smoking within 30 days (OR = 0.430, 95%CI: 0.229–0.810, P = 0.009), after 30 days (OR = 0.103, 95%CI: 0.034–0.317, P < 0.001), and those who did not decide when to quit smoking (OR = 0.370, 95%CI: 0.173–0.788, P = 0.010) were less likely to quit smoking than those who quit immediately (Table 3).
Table 3.
Smoking cessation predictive factors multivariate binary logistic regression analysis.
| Variable | β | SE | Waldχ2 | P | Estimated odds ratio | 95% confidence interval |
|---|---|---|---|---|---|---|
| Previous SC attempts | ||||||
| No | 1 | |||||
| Yes | 0.727 | 0.298 | 5.975 | 0.015 | 2.070 | 1.155–3.709 |
| Date of SC | ||||||
| Date of SC (Immediately) | 1 | |||||
| Date of SC (Within 7 days) | 0.028 | 0.503 | 0.003 | 0.956 | 1.028 | 0.384–2.757 |
| Date of SC (Within 30 days) | −0.843 | 0.323 | 6.823 | 0.009 | 0.430 | 0.229–0.810 |
| Date of SC (After 30 days) | −2.270 | 0.572 | 15.747 | 0.000 | 0.103 | 0.034–0.317 |
| Date of SC (Undecided) | −0.995 | 0.386 | 6.647 | 0.010 | 0.370 | 0.173–0.788 |
| Follow ups | ||||||
| ≤2 | 1 | |||||
| ≥3 | 2.585 | 1.041 | 6.171 | 0.013 | 13.266 | 1.725–101.991 |
Discussion
Characteristics of SC Participants
Most participants of this study were male (97.6%), which is similar to the participant characteristics of other studies (42–44). Gender differences may be related to the low smoking rate among women in Chinese (2.1%) (2). Similar low smoking rates among women have been observed in other countries. Vietnam's demographic surveillance system showed that men and women have a smoking rate of 34.7 and 0.9%, respectively (45). In a cross-sectional study in rural Andhra Pradesh, India, the smoking rate among men was significantly higher (50.3%) than among women (4.8%), but the SC rate among women (45.5%) was significantly higher than that among men (18.8%) (46). Giovino et al. 's (42) analysis of data from 14 low and middle-income countries showed that men in Global Adult Tobacco Survey (GATS) countries have a smoking rate of 48.6% and women 11.3%.
In this study, univariate analysis showed no statistically significant difference between age bracket and success rate of SC. Some studies have suggested that age is a factor in the success of quitting, while others have found the opposite (21, 47–49). Further research is needed to determine the role of age as a factor in SC success.
The attendance rate of smokers at our SC clinics was lower than that in the study by Hamadeh et al. (50) in Bahrain, which was attended by more than 100 patients monthly. Patients' attendance in consulting a health professional is dependent on their willingness to quit smoking as well as their access to SC resources. One of the main reasons for the low attendance rate of smokers in this study can be that Hunan is a large province, and it is not convenient for participants from all over the province to come to the hospital. To strengthen interventions for SC, future studies are advised to use mobile phones or other electronic devices, which are convenient for interaction and reinforcement for both the professional and the smokers (51, 52).
The Relationship Between Reasons, Motivation, and Success in Quitting Smoking
In this study, the main reasons and motivations for the patients to quit smoking included recognizing smoking as a health hazard, knowing someone sick from smoking, family demands, and believing that smoking led to a gradual decline in their health status. The following literature also proves the result of this study, Wang et al. (53) suggested that the direct or indirect health issues experienced by smokers were the main motivation for quitting smoking, which was also an important reason for smokers to succeed in quitting smoking. A cohort study of adult smokers in six European Union countries showed that focus on individual health and paying close attention to related diseases caused by smoking were important reasons for quitting smoking. Factors such as affecting the health of non-smokers, health care professionals' advice, and the opposition of friends and family were considered important reasons to stop smoking, but were not successful predictors of SC (54). Thomas et al. (55) believed that health problems were one of the most common reasons for smokers to quit, and while the reasons to quit could not predict ultimate success in SC, it led the smoker to continue to try to quit. A study in Singapore (27) showed that smokers who cited social pressures from by family or friends as quitting motivation were more likely to quit (P < 0.001), and quitting due to social pressure as quitting motivation (OR = 1.35, 95%CI = 1.10–1.66, P = 0.005) remained an independent predictor of successful quitting. However, Klemperer et al. (56) conducted an intervention on motivation of people who were initially reluctant to quit smoking and found that the increase of motivation to quit could predict the smokers' attempts to quit smoking and their success in quitting. Pineiro et al. (57) found that smokers' motivation to quit can predict short- and long-term success in quitting, as well as the maintenance of this long-term success, which is consistent with reports from other studies (58, 59).
Success Rate of SC
Our study showed that the participants' 3-month SC rate was 28.4% (93/328). This is higher than usual; success rate of SC is generally <10% (17). This could be because SC rates vary depending on the method used. The SC clinic in this study offered both face-to-face counseling and follow-up through telephone. In China, the quit rate in the general population without any aids is <5% (2). The SC intervention in primary health care units in Thailand had a continuous smoking cessation rate of 25.62% at 6 months (33). A research in Mumbai, India, reported that the women's community SC program used health education, games, and follow-up counseling sessions to intervene once every 3 months, and the SC rate at 12 months was 33.5% (60). Another study conducted in India reported a rate of merely 2.6% (61). SC clinics may encourage tobacco control efforts and help decrease the health burden of smoking.
Predictors of SC
Binary logistic regression predictor analysis revealed that the starting date of SC, the number of previous quitting attempts, and the number of follow-up after the first consultation were independent predictors of smoking cessation success (P < 0.05). However, the duration of smoking, daily cigarettes consumption, Fagerstrom score, and exhaled CO value at first visit were not associated with successful smoking cessation in this study. Ma et al. (62) showed that lower nicotine dependence level, and counseling sessions received were significantly associated with success in quitting smoking (P < 0.01). Shie et al. (63) found that smokers with the higher intention to quit was more likely to quit smoking successfully (P < 0.001). Huang et al. analyzed smoking cessation rate in a hospital smoking cessation clinic in Taiwan, showed that the independent predictors of smoking cessation success were the average number of cigarettes smoked each day, nicotine dependence level, exhaled CO value at first visit, and number of clinic visits (P < 0.05) (21). However, a study on smoking cessation clinic of a hospital in inland China (Ningbo City) showed that the number of outpatient visits was the most important factor for success in smoking cessation, while the CO level exhaled at the first visit was not associated with success in smoking cessation (64). These results all confirm that the number of counseling sessions after starting smoking cessation is an independent predictor of success, with some variation in other predictors. These different findings arise and require further exploration.
Previous Attempts to Quit Smoking Enhance Quit Rate
Approximately 64.6% of current smokers in this study had attempted to quit smoking previously. The result also indicated that previous attempts to quit smoking were positive factors for SC success and a greater number of attempts to quit smoking increased the possibility of SC success, which is consistent with another study in China (65). Other studies reported that SC intentions and SC attempts were also important indicators for predicting future SC attempts and success rates (48, 66). A study of five smoking cessation clinics in Malaysia suggested that smokers who have tried to quit smoking for longer are more likely to quit (67). At the same time, related studies have shown that the duration of smoking cessation attempt is related to the success of quitting smoking (68, 69). A study exploring patterns and predictors of cessation success among adult smokers in Thailand showed that smokers who tried to quit for more than a week predicted short-term success in quitting (26). In a study of smokers' quitting behavior in six Chinese cities, a history of quitting for longer than 6 months was also an independent predictor of smoking cessation (69). A Bangladeshis study showed that both smokers who had tried to quit 6 months earlier (OR = 0.23, 95% CI:0.09–0.62) and those who had never tried to quit (OR = 0.75, 95% CI:0.34–1.66) were less likely to quit than those who had tried within the last 6 months (70). These results imply that the SC strategies are therefore needed to motivate and encourage smokers to become more ready to quit.
Behavioral Support and Follow-Up Are Important Factors for Successful SC
All participants in this study received 20–30 min face-to-face detailed counseling and 0–3 telephone follow-up sessions. Additionally, 1.8% of the participants received behavioral support interventions plus pharmacotherapy and 1.8% were using e-cigarettes alongside behavioral support interventions during SC procedure. Pharmacotherapy can increase the success rate of quitting smoking (23, 40). It is considered an important factor affecting SC success in another study (71), with the withdrawal rate reaching 44.0% at 9–12 weeks (72, 73). However, in our study, it was not a factor affecting SC. We found that the proportion of participants using SC products was 1.8%. Hence, the effectiveness of pharmacotherapy may be underestimated in our study.
A reason for fewer participants choosing pharmacotherapy as preferred intervention was likely because Chinese people are less interested in SC drugs (74). Furthermore, these medications are not covered by medical insurance in China and are often too expensive for smokers to afford. Although there is evidence that e-cigarettes may help smokers quit (75), the WHO has clearly stated that e-cigarettes are harmful, and they may lead to nicotine addiction in teenagers (76). The proportion of successful quitters receiving three or more follow-up sessions was significantly higher than that of unsuccessful quitters [98.9% (92/93) vs. 88.9% (206/235)], which is consistent with the findings of previous studies (77, 78). Two studies in Malaysia suggest that the clinic follow-up sessions was a strong predictor of successful cessation, attending more than one follow-up session increased the chance of success (79, 80). Rabius et al. (81) also found that five psychological interventions together with two telephone follow-up interventions had a 4.1% higher SC rate than only five psychological interventions. A rehabilitation center in Munich, Germany, reported that the SC rate reached with the first psychological intervention alone was 16.8%. With the addition of a follow-up SC intervention, the rate was 30.3% (82). Therefore, follow-up to help smokers quit smoking is very important.
Relation Between Setting the Quitting Date and SC Success
The time taken to quit smoking was also associated with success in quitting (P < 0.05); the shorter the time was set, the higher the likelihood of SC success. Compared to those who quit immediately, those who were undecided or decided to quit within 30 days or later have a lower success rate of quitting. Li et al. (69) investigated the quitting behavior of adult smokers in six Chinese cities, and the results showed that those who planned to quit smoking within 1 month were more than twice as likely to succeed as those who did not (OR = 2.46, 95% CI: 1.61–3.75), similar to the results of research in Southeast Asia (Malaysia and Thailand) (OR = 2.18, 95% CI: 1.46–3.27) (68). Quit-date goal setting is an important element of an effective brief SC intervention. The quit-date goal setting enhances quit attempts (83). Complete abstinence in the first week after the quit date was a strong predictor of long-term success (84). Health professionals should promptly alleviate the concerns of smokers and help them develop a quality quit-date and an immediate quit plan.
Limitations
Only the short-term abstinence rate (12 weeks) was reported in our study. The long-term abstinence rate (13–52 weeks) needs to be further evaluated. Moreover, SC success was evaluated by the researcher only according to participants' report that was obtained through telephonic interview; this might lead to biased results.
Conclusion
In conclusion, in this study, a SC clinic affected SC rate in clinical practice. Smokers receiving regular follow-up counseling for 3 months at the SC clinic exhibited an improved SC rate (28.4%) compared with that of other smokers. Participants who received regular SC counseling were more likely to quit smoking successfully than those who did not receive further counseling. Smokers who had previously tried to quit and who were in a poor physical condition were also more likely to quit. It is suggested that motivation enhancement, cognitive behavioral strategies, and persistent counseling be combined to improve the quit rate. Moreover, the results indicate the need to develop and strengthen SC outpatient services, not only in Hunan Province but also in other parts of China and other countries to obtain a significant decrease in smoking rates.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Hunan Cancer Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
YNH, JHX, and RZ wrote this article. XCC, JHC, WW, and YHZ supervised the whole study and critically revised the paper. LMZ, RZ, XHY, and OYC read and amended the final manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank R. H. Yu statistical experts of School of Xiangya Public Health, Central South University guided the data analysis in this study. We would like to thank Editage (www.editage.com) for English language editing.
Footnotes
Funding. This study was founded by the Changsha Science and Technology Bureau in China (Grant Number kq1901085). Hunan Provincial Bureau of Science and Technology (Grant Numbers: 2020ZK4065 and 2017WK2061).
References
- 1.Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence 2008 Update: Clinical Practice Guideline. U.S:Department of Health and Human Service; (2008). p. 29–30. [Google Scholar]
- 2.Global Adult Tobacco Survey (Gats) . Chinese Center for Disease Control and Prevention, Global Adult Tobacco Survey in China in 2018. (2019). Available online at: http://www.chinacdc.cn/jkzt/sthd_3844/slhd_4156/201908/t20190814_204616.html (accessed August 14, 2019).
- 3.Wang M, Luo X, Xu S, Liu W, Ding F, Zhang X, et al. Wang W Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. (2018) 7:35–45. 10.1016/S2213-2600(18)30432-6 [DOI] [PubMed] [Google Scholar]
- 4.WHO . World Health Statistics. Geneva: World Health Organization; (2015). p. 101–11. [Google Scholar]
- 5.Han W, Jian JM, Li JY, Zeng XJ, Zou XN, Wu YP, et al. Contributions of major smoking-related diseases to reduction in life expectancy associated with smoking in Chinese adults: a cross-sectional study. BMC Public Health. (2013) 13:1147. 10.1186/1471-2458-13-1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res. (2015) 4:327–38. 10.3978/j.issn.2218-6751.2015.08.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhi XY, Zou XN, Hu M, Jiang Y, Jia MM, Yang GH. Increased lung cancer mortality rates in the Chinese population from 1973-1975 to 2004-2005: an adverse health effect from exposure to smoking. Cancer. (2015) 121:3107–12. 10.1002/cncr.29603 [DOI] [PubMed] [Google Scholar]
- 8.Gellert C, Schöttker B, Müller H, Holleczek B, Brenner H. Impact of smoking and quitting on cardiovascular outcomes and risk advancement periods among older adults. Eur J Epidemiol. (2013) 28:649–58. 10.1007/s10654-013-9776-0 [DOI] [PubMed] [Google Scholar]
- 9.Hackshaw A, Morris JK, Boniface S, Tang JL, Milenković D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ. (2018) 360:j5855. 10.1136/bmj.j5855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. (2014) 34:509–15. 10.1161/ATVBAHA.113.300156 [DOI] [PubMed] [Google Scholar]
- 11.Hazlinda AH, Noorizan AA, Yahaya H, Hassan F. Does the duration of smoking cessation have an impact on hospital admission and health-related quality of life amongst COPD patients? Int J Chronic Obstruct Pulm Dis. (2014) 9:493–9. 10.2147/COPD.S56637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gellert C, Schottker B, Brenner H, Holleczek B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Int Med. (2012) 172:837–44. 10.1001/archinternmed.2012.1397 [DOI] [PubMed] [Google Scholar]
- 13.Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. New Engl J Med. (2013) 368:341–50. 10.1056/NEJMsa1211128 [DOI] [PubMed] [Google Scholar]
- 14.Toll BA, Brandon TH, Gritz ER, Warren GW, Herbst RS. Assessing tobacco use by cancer patients and facilitating cessation: an American Association for Cancer Research policy statement. Clin Cancer Res. (2013) 19:1941–8. 10.1158/1078-0432.CCR-13-0666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Life CAL. Quitting smoking: the benefits. Breathe. (2017) 13:263–5. 10.1183/20734735.ELF133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen ZM, Peto R, Zhou M, Sherman RL, Noone AM, Howlader N, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. (2015) 386:1447–56. 10.1016/S0140-6736(15)00340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hughes JR. Motivating and helping smokers to stop smoking. J Gen Intern Med. (2003) 18:1053–7. 10.1111/j.1525-1497.2003.20640.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheffer CE, Anders M, Brackman SL, Steinberg MB, Barone C. Tobacco intervention practices of primary care physicians treating lower socioeconomic status patients. Am J Med Sci. (2012) 343:388–96. 10.1097/MAJ.0b013e3182302749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochr Database Syst Rev. (2013) 2013:CD001008. 10.1002/14651858.CD000165.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.PHS Guideline Update Panel, Liaisons, and Staff (2008) . Treating tobacco use and dependence: 2008 update U.S. Public Health Service Clinical Practice Guideline executive summary. Respir Care. 53:1217–22. [PubMed] [Google Scholar]
- 21.Huang WH, Hsu HY, Chang BC, Chang FC. Factors correlated with success rate of outpatient smoking cessation services in Taiwan. Int J Environ Res Public Health. (2018) 15:1218. 10.3390/ijerph15061218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strengthening Health Systems for Treating Tobacco Dependence in Primary Care. Buildingcapacity for Tobacco Control: Training Package. Geneva: World Health Organization; (2013). Avilable online at: http://www.who.int/tobacco/publications/building_capacity/training_package/treatingtobaccodependence/en (accessed June 25, 2019). [Google Scholar]
- 23.Singh P, Kumar R. Assessment of the effectiveness of sustained release Bupropion and intensive physician advice in smoking cessation. Lung India Off Organ Indian Chest Soc. (2010) 27:11–8. 10.4103/0970-2113.59262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization . Tobacco Free Initiative (TFI). WHO Report on the Global Tobacco Epidemic, (2017). Available online at: http://www.who.int/tobacco/global_report/2015/en/ (accessed June 20, 2019).
- 25.Zhu WH, Yang L, Jiang CQ, Deng LZ, Lam TH, Zhang JY, et al. Characteristics of smokers and predictors of quitting in a smoking cessation clinic in Guangzhou, China. J Public Health. (2010) 32:267–76. 10.1093/pubmed/fdp107 [DOI] [PubMed] [Google Scholar]
- 26.Jampaklay A, Borland R, Yong HH, Sirirassamee B, Fotuhi O, Fong GT. Predictors of successful quitting among Thai adult smokers: evidence from ITC-SEA (Thailand) survey. Int J Environm Res Public Health. (2015) 12:12095–109. 10.3390/ijerph121012095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.See JHJ, Yong TH, Poh SLK, Lum YC. Smoker motivations and predictors of smoking cessation: lessons from an inpatient smoking cessation programme. Singapore Med J. (2019) 60:583–9. 10.11622/smedj.2019148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aluckal E, Pulayath C, Chithra P, Balakrishna MS, Luke AM, Mathew S. Tobacco cessation behavior among smoking and smokeless form tobacco users in the indigenous population of Ernakulam, India. J Pharm Bioallied Sci. (2020) 12:S194–8. 10.4103/jpbs.JPBS_58_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hagimoto A, Nakamura M, Morita T, Masui S, Oshima A. Smoking cessation patterns and predictors of quitting smoking among the Japanese general population: a 1-year follow-up study. Addiction. (2010) 105:164–73. 10.1111/j.1360-0443.2009.02735.x [DOI] [PubMed] [Google Scholar]
- 30.Al-Nimr YM, Farhat G, Alwadey A. Factors affecting smoking initiation and cessation among Saudi women attending smoking cessation clinics. Sultan Qaboos Univ Med J. (2020) 20:95. 10.18295/squmj.2020.20.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wray JM, Funderburk JS, Acker JD, Wray LO, Maisto SA. A meta-analysis of brief tobacco interventions for use in integrated primary care. Nicotine Tobacco Res. (2018) 20:1418–26. 10.1093/ntr/ntx212 [DOI] [PubMed] [Google Scholar]
- 32.Zhang XY, Yang L, Tian HM, Qiu M, Liu X. Follow-up effect of smoking cessation clinics in Chengdu. J Preventive Med Info. (2013) 29:193–6. [Google Scholar]
- 33.Aung MN, Yuasa M, Moolphate S, Lorga T, Yokokawa H, Fukuda H, et al. Effectiveness of a new multi-component smoking cessation service package for patients with hypertension and diabetes in northern Thailand: a randomized controlled trial (ESCAPE study). Subst Abuse Treat Prev Policy. (2019) 14:10. 10.1186/s13011-019-0197-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guidelines for Smoking Cessation Clinics. Beijing: People's Medical Publishing House Co. Control Office of Chinese Center for Disease Control and Prevention; (2008). p. 60–89. [Google Scholar]
- 35.World Health Organization . Guidelines for Controlling and Monitoring the Tobacco Epidemic. Geneva: World Health Organization Library Cataloguing in Publication Data; (1998). [Google Scholar]
- 36.Wu L, He Y, Jiang B, Zuo F, Liu QH, Zhang L, et al. Predictors for successful quitting smoking among males carried out in a Smoking Cessation Clinic. Chin J Epidemiol. (2014) 35:792–6. 10.16168/j.cnki.issn.1002-9982.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 37.Yang GH. (1998). Epidemiological investigation of smoking behavior in China in 1996. China Cancer. 3–5. [Google Scholar]
- 38.West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Health Educ Authority Thorax. (2000) 55:987–99. 10.1136/thorax.55.12.987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chinese Center for Disease Control and Prevention . 2015 Chinese Adult Tobacco Survey Report. Beijing: People's Medical Publishing House. (2015). [Google Scholar]
- 40.Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochr Database Syst Rev. (2018) 5:CD000146. 10.1002/14651858.CD000146.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prochaska JO, Goldstein MG. Process of smoking cessation. Implications for clinicians. Clin Chest Med. (1991) 12:727–35. [PubMed] [Google Scholar]
- 42.Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, Bhala N, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. (2012) 380:668–79. 10.1016/S0140-6736(12)61085-X [DOI] [PubMed] [Google Scholar]
- 43.Liu S, Zhang M, Yang L, Wang L, Huang Z, Wang L, et al. Prevalence and patterns of tobacco smoking among Chinese adult men and women: findings of the 2010 national smoking survey. J Epidemiol Commun Health. (2017) 71:154–61. 10.1136/jech-2016-207805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhing DF. Findings From the First Round to the Fifth Round of the ITC China Survey Report. Beijing: China Textile Press; (2018). p. 22–23. [Google Scholar]
- 45.Thi Thanh Huong L, Khanh Long T, Xuan Son P, Thi Tuyet-Hanh T. Prevalence of Smoking and Associated Factors: evidence from the CHILILAB demographic surveillance system in Vietnam. Asia Pac J Public Health. (2017) 29:53S–61S. 10.1177/1010539517718333 [DOI] [PubMed] [Google Scholar]
- 46.Corsi DJ, Subramanian SV, Lear SA, Teo KK, Boyle MH, Raju PK, et al. Tobacco use, smoking quit rates, and socioeconomic patterning among men and women: a cross-sectional survey in rural Andhra Pradesh, India. Eur J Prev Cardiol. (2014) 21:1308–18. 10.1177/2047487313491356 [DOI] [PubMed] [Google Scholar]
- 47.Hakim S, Chowdhury M, Uddin MJ. Correlates of unsuccessful smoking cessation among adults in Bangladesh. Prev Med Rep. (2017) 8:122–8. 10.1016/j.pmedr.2017.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hyland A, Borland R, Li Q, Yong HH, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. (2006) 15:iii83–94. 10.1136/tc.2005.013516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.West R, Evins AE, Benowitz NL, Russ C, McRae T, Lawrence D, et al. Factors associated with the efficacy of smoking cessation treatments and predictors of smoking abstinence in EAGLES. Addiction. (2018) 113:1507–16. 10.1111/add.14208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamadeh RR, Ahmed J, Al-Kawari M, Bucheeri S. Quit tobacco clinics in Bahrain: smoking cessation rates and patient satisfaction. Tobacco Induced Dis. (2017) 5:7. 10.1186/s12971-017-0115-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Businelle MS, Ma P, Kendzor DE, Frank SG, Vidrine DJ, Wetter DW. An ecological momentary intervention for smoking cessation: evaluation of feasibility and effectiveness. J Med Int Res. (2016) 18:e321. 10.2196/jmir.6058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu HM, Su HM, Zou XM, Zhou ZY. Application of whole-process management based on Internet + in outpatient smoking cessation patients. Chin J Lung Dis. (2019) 12:657–659. [Google Scholar]
- 53.Wang J, Li C, Jia C, Liu Y, Liu J, Yan X, et al. Smoking, smoking cessation and tobacco control in rural China: a qualitative study in Shandong Province. BMC Public Health. (2014) 14:916. 10.1186/1471-2458-14-916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Girvalaki C, Filippidis FT, Kyriakos CN, Driezen P, Herbeć A, Mons U, et al. Perceptions, predictors of and motivation for quitting among smokers from six European countries from 2016 to 2018: findings from EUREST-PLUS ITC Europe surveys. Int J Environ Res Public Health. (2020) 17:6263. 10.3390/ijerph17176263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomas DP, Lyons L, Borland R. Predictors and reasons for starting and sustaining quit attempts in a national cohort of Aboriginal and Torres Strait Islander smokers. Drug Alcohol Rev. (2019) 38:244–53. 10.1111/dar.12917 [DOI] [PubMed] [Google Scholar]
- 56.Klemperer EM, Mermelstein R, Baker TB, Hughes JR, Fiore MC, Piper ME, et al. Predictors of smoking cessation attempts and success following motivation-phase interventions among people initially unwilling to quit smoking. Nicotine Tob Res. (2020) 22:1446–52. 10.1093/ntr/ntaa051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pineiro B, López-Durán A, Del Río EF, Martínez Ú, Brandon TH, Becoña E. Motivation to quit as a predictor of smoking cessation and abstinence maintenance among treated Spanish smokers. Addict Behav. (2016) 53:40–5. 10.1016/j.addbeh.2015.09.017 [DOI] [PubMed] [Google Scholar]
- 58.Im PK, McNeill A, Thompson ME, Fong GT, Xu S, Quah AC, et al. Individual and interpersonal triggers to quit smoking in China: a cross-sectional analysis. Tobacco Control. (2015) 24(Suppl. 4):iv40–7. 10.1136/tobaccocontrol-2014-052198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kasza KA, Hyland AJ, Borland R, McNeill A, Fong GT, Carpenter MJ, et al. Cross-country comparison of smokers' reasons for thinking about quitting over time: findings from the International Tobacco Control. (2017) 26:641–8. 10.1136/tobaccocontrol-2016-053299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mishra GA, Kulkarni SV, Majmudar PV, Gupta SD, Shastri SS. Community-based tobacco cessation program among women in Mumbai, India. Indian J Cancer. (2014) 51:S54–9. 10.4103/0019-509X.147474 [DOI] [PubMed] [Google Scholar]
- 61.Sarkar BK, West R, Arora M, Ahluwalia JS, Reddy KS, Shahab L. Effectiveness of a brief community outreach tobacco cessation intervention in India: a cluster-randomised controlled trial (the BABEX Trial). Thorax. (2017) 72:167–73. 10.1136/thoraxjnl-2016-208732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ma E, Chan T, Zhang O, Yang JS, Wang YY, Li YC, et al. Effectiveness of acupuncture for smoking cessation in a Chinese population. Asia Pac J Public Health. (2015) 27:NP2610–22. 10.1177/1010539513503867 [DOI] [PubMed] [Google Scholar]
- 63.Shie HG, Pan SW, Yu WK, Chen WC, Ho LI, Ko HK. Levels of exhaled carbon monoxide measured during an intervention program predict 1-year smoking cessation: a retrospective observational cohort study. NPJ Prim Care Respir Med. (2017) 27:59. 10.1038/s41533-017-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhu N, Lin S, Cao C, Xu N, Yu X, Chen X. Nomogram to predict successful smoking cessation in a Chinese outpatient population. Tob Induc Dis. (2020) 18:86. 10.18332/tid/127736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jia XR, Qi F, Li SP, Geng MY, Yi F. Survey on smoking cessation behaviors and analysis of tobacco control strategy in Qingdao city. Chin J Dis Control. (2017) (2017) 21:444–8. 10.16462/j.cnki.zhjbkz.2017.05.004 [DOI] [Google Scholar]
- 66.Andrew H, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. (2004) 6:S363–9. 10.1080/14622200412331320761 [DOI] [PubMed] [Google Scholar]
- 67.Wee LH, Shahab L, Bulgiba A, West R. Stop smoking clinics in malaysia: characteristics of attendees and predictors of success. Addict Behav. (2011) 36:400–3. 10.1016/j.addbeh.2010.11.011 [DOI] [PubMed] [Google Scholar]
- 68.Li L, Borland R, Yong HH, Fong GT, Bansal-Travers M, Quah AC, et al. Predictors of smoking cessation among adult smokers in Malaysia and Thailand: findings from the International Tobacco Control Southeast Asia Survey. Nicotine Tob Res. (2010) 1:S34–44. 10.1093/ntr/ntq030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li L, Feng G, Jiang Y, Yong HH, Borland R, Fong GT. Prospective predictors of quitting behaviours among adult smokers in six cities in China: findings from the International Tobacco Control (ITC) China Survey. Addiction. (2011) 106:1335–45. 10.1111/j.1360-0443.2011.03444.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abdullah AS, Driezen P, Quah AC, Nargis N, Fong GT. Predictors of smoking cessation behavior among Bangladeshi adults: findings from ITC Bangladesh survey. Tob Induc Dis. (2015) 13:23. 10.1186/s12971-015-0050-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.West R, Raw M, McNeill A, Stead L, Aveyard P, Bitton J, et al. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Addiction. (2015) 110:1388–403. 10.1111/add.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jorenby DE, Hays JT, Rigotti NA, Azoulay S, Watsky EJ, Williams KE. Efficacy of varenicline, an α4β2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. (2006) 296:56–63. 10.1001/jama.296.1.56 [DOI] [PubMed] [Google Scholar]
- 73.Zhou C, Wu L, Liu Q, An H, Jiang B, Zuo F. Evaluation of smoking cessation intervention in patients with chronic diseases in smoking cessation clinics. Medicine. (2017) 96:e7459. 10.1097/MD.0000000000007459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jiang Y, Elton-Marshall T, Fong GT, Li Q. Quitting smoking in China: findings from the ITC China Survey. Tob Control. (2010) 19:12–5. 10.1136/tc.2009.031179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Malas M, van der Tempel J, Schwartz R, Minichiello A, Lightfoot C, Noormohamed A, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res. (2016) 18:1926–36. 10.1093/ntr/ntw119 [DOI] [PubMed] [Google Scholar]
- 76.World Health Organization . WHO Report on the Global Tobacco Epidemic 2019: Offer Help to Quit Tobacco Use, Geneva: (2019). [Google Scholar]
- 77.Bacha ZA, Layoun N, Khayat G, Allit S. Factors associated with smoking cessation success in Lebanon. Pharm Pract. (2018) 16:111. 10.18549/PharmPract.2018.01.1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sim JY, Han NY, Cheong YS, Yoo SM, Park EW. Factors associated with success of smoking cessation at smoking-cessation clinic. Taehan Kanho Hakhoe Chi. (2002) 36:441–2. 10.1016/S0093-691X(02)01226-8 [DOI] [Google Scholar]
- 79.Ezzat W, Salehuddin A, Aljunid S, Zarihah Z. Patterns and predictors of smoking cessation among smokers attending smoking cessation clinics in Peninsular Malaysia. J Comm Health. (2008) 14:17–23. [Google Scholar]
- 80.Yasin SM, Retneswari M, Moy FM, Taib KM, Ismail N. Predictors of sustained six months quitting success: efforts of smoking cessation in low intensity smoke-free workplaces. Ann Acad Med Singap. (2013) 42:401–7. 10.12669/pjms.294.3797 [DOI] [PubMed] [Google Scholar]
- 81.Rabius V, Pike KJ, Hunter J, Wiatrek D, McAlister AL. Effects of frequency and duration in telephone counseling for smoking cessation. Tob Control. (2007) 16:i71–4. 10.1136/tc.2007.019950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Metz K, Floter S, Kroger C, Donath C, Piontek D, Gradl S. Telephone booster sessions for optimizing smoking cessation for patients in rehabilitation centers. Nicotine Tobacco Res. (2007) 9:853–63. 10.1080/14622200701485000 [DOI] [PubMed] [Google Scholar]
- 83.Brady RB, Nair US, Gerald JK, Yuan NP, Krupski LA, Thomson CA. Higher quality quit-date goal setting enhances quit attempts among quitline callers. Tob Prev Cessat. (2019) 5:20. 10.18332/tpc/109537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tonnesen P. Smoking cessation: nicotine replacement, gums and patches. Monaldi Arch Chest Dis. (1999) 54:489–94. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.