Abstract
Background
In December 2019, a novel coronavirus disease (COVID-19) emerged in Wuhan, China, with an incredible contagion rate. However, the vertical transmission of COVID-19 is uncertain.
Objectives
This is a systematic review of published studies concerning pregnant women with confirmed COVID-19 and their neonates.
Search strategy
We carried out a systematic search in multiple databases, including PubMed, Web of Science, Google Scholar, Scopus, and WHO COVID-19 database using the following keywords: (Coronavirus) OR (novel coronavirus) OR (COVID-19) OR (COVID19) OR (COVID 19) OR (SARS-CoV2) OR (2019-nCoV)) and ((pregnancy) OR (pregnant) OR (vertical transmission) OR (neonate) OR (newborn) OR (placenta) OR (fetus) OR (Fetal)). The search took place in April 2020.
Selection criteria
Original articles published in English were eligible if they included pregnant patients infected with COVID-19 and their newborns.
Data collection and analyses
The outcomes of interest consisted of clinical manifestations of COVID-19 in pregnant patients with COVID-19 and also the effect of COVID-19 on neonatal and pregnancy outcomes.
Main results
37 articles involving 364 pregnant women with COVID-19 and 302 neonates were included. The vast majority of pregnant patients were in their third trimester of pregnancy, and only 45 cases were in the first or second trimester (12.4%). Most mothers described mild to moderate manifestations of COVID-19. Of 364 pregnant women, 25 were asymptomatic at the time of admission. The most common symptoms were fever (62.4%) and cough (45.3%). Two maternal deaths occurred. Some pregnant patients (12.1%) had a negative SARS‐CoV‐2 test but displayed clinical manifestations and abnormalities in computed tomography (CT) scan related to COVID‐19. Twenty‐two (6.0%) pregnant patients developed severe pneumonia. Two maternal deaths occurred from severe pneumonia and multiple organ dysfunction. Studies included a total of 302 neonates from mothers with COVID‐19. Of the studies that provided data on the timing of birth, there were 65 (23.6%) preterm neonates. One baby was born dead from a mother who also died from COVID-19. Of the babies born alive from mothers with COVID‐19, five newborns faced critical conditions, and two later died. A total of 219 neonates underwent nasopharyngeal specimen collection for SARS‐CoV‐2, of which 11 tested positive (5%). Seventeen studies examined samples of the placenta, breast milk, umbilical cord, and amniotic fluid, and all tested negative except one amniotic fluid sample.
Conclusions
A systematic review of published studies confirm that the course of COVID-19 in pregnant women resembles that of other populations. However, there is not sufficient evidence to establish an idea that COVID-19 would not complicate pregnancy.
Keywords: COVID-19, Immunity, Neonates, Pregnancy, SARS-CoV2, Vertical transmission
Background
The World Health Organization (WHO) announced the novel coronavirus disease (COVID-19) as a Pandemic on March 7, 2020, when the number of confirmed cases just exceeded 100,000 [1]. As of April 21, 2020, COVID-19 has reached all over the world, with about 180,000 deaths of a total of more than 2 million confirmed cases. Moreover, it seems there is an underestimation in the mortality rate of this infectious disease. Studies estimate the real mortality rate to be about 6% in China, rising to about 15% in other countries [2]. Therefore, COVID-19 is, in general, a life-threatening condition.
COVID-19 can affect multiple organs and systems [3–11], although it mainly involves the respiratory system, where its involvement can cause a wide range of symptoms from a common cold to severe respiratory distress [12–15]. In particular, the disease is more severe and deadly in older age groups and people who have pre-existing comorbidity. The immunopathogenesis of the disease is not clear [16–21]. However, as for other infectious conditions, immune dysregulation might increase the risk of severe illness and death from COVID-19 [21–27].
Pregnancy is a particular condition that can have significant effects on the biological systems of a woman’s body. Notably, pregnant women acquire changes so that their immune system will be able to tolerate pregnancy. These changes mostly place the maternal immune system under a down-regulated condition. As a result, pregnant women are generally considered vulnerable to infectious diseases.
Whereas its transmission mainly occurs through human-to-human contact, the novel coronavirus has shown its potential to transmit via multiple transmission routes [28] and affect both children and adults [13, 29]. It, however, remained unclear whether or not this potentially fatal virus can vertically be transmitted and what are the possible effects of the disease on the pregnancy outcomes.
Methods
The present systematic review was developed according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [14]. Before the study begins, the authors developed the study protocol that is available on request.
Literature search
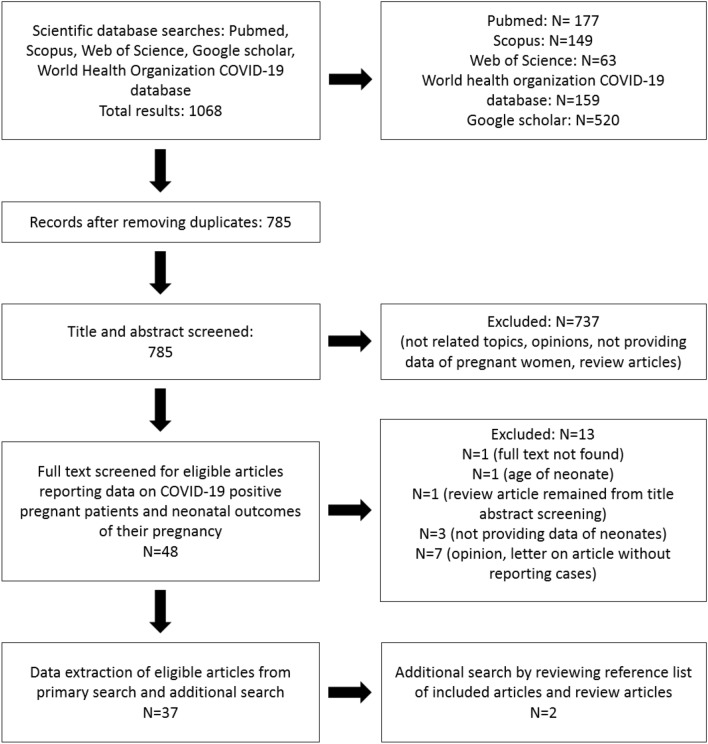
We carried out a systematic search in multiple databases, including PubMed, Web of Science, Google Scholar, Scopus, and WHO COVID-19 database using the following keywords: (Coronavirus) OR (novel coronavirus) OR (COVID-19) OR (COVID19) OR (COVID 19) OR (SARS-CoV2) OR (2019-nCoV)) and ((pregnancy) OR (pregnant) OR (vertical transmission) OR (neonate) OR (newborn) OR (placenta) OR (fetus) OR (Fetal)). The search took place in April 2020 (Fig. 1).
Fig. 1.
PRISMA flowchart of the literature search
Selection criteria
We sought studies that investigated the potential effect of COVID-19 on pregnancy and neonatal health. Original articles published in English were eligible if they included pregnant patients infected with COVID-19 and their newborns. The outcomes of interest consisted of clinical manifestations of COVID-19 in pregnant patients with COVID-19 and also, the effect of COVID-19 on neonatal and pregnancy outcomes.
Data extraction
For pregnant women infected with COVID-19, we extracted the following data: article title, author, study type, country, number of pregnant women with COVID-19, clinical manifestations of disease in pregnant women, the trimester of pregnancy, diagnostic technique, potential complications related to COVID-19, delivery, and the maternal outcome(s) of COVID-19. For neonates born from mothers with COVID-19, data on the article title, author, study type, country, number of neonates, neonatal maturity, clinical presentation, neonatal complications, a diagnostic test for COVID-19, Apgar score, and neonatal outcome were extracted. Finally, for pregnancy outcomes, we collected data on the article title, author, study type, country, placental test for viral nucleic acid, and pregnancy complications.
Results
Literature search
The systematic search yielded a total of 1068 search results, of which 785 discrete records remained for screening after removing duplicates. During title and abstract screening, we selected 48 articles for detailed review. In the detailed review process, we excluded thirteen articles with the following reasons for exclusion: seven articles not provided data on pregnant patients or neonatal outcomes [28, 30–35], three studies lacked data on neonates or vertical transmission [36–38], one study reported a 17-day neonate who had exposure to parents complaining of fever and cough [39], one study was not original research [40], and the full-text was not available for one article [41]. Also, we carried out an additional search through reviewing reference lists of 35 included articles from systematic search and related review articles and found two additional articles [42, 43]. Finally, a total number of 37 studies, including case reports and case series, were eligible to be included in this systematic review [42–76]. Tables 1, 2, 3 provide an overview of the characteristics of the included studies. Below is a narrative synthesis of studies that included pregnant women with confirmed COVID-19 and their neonates.
Table 1.
Characteristics of pregnant women with COVID-19 included in the systematic review
| Article title | Author | Study type | Country | Number of patients | Clinical features of the disease in pregnant patients | The onset of disease presentation (= N) |
Diagnosing technique | Complications due to viral infection | Delivery | The maternal outcome(s) of disease in pregnant patients |
|---|---|---|---|---|---|---|---|---|---|---|
| Pregnant women with new coronavirus infection: a clinical characteristics and placental pathological analysis of three cases | Chen et al. | Case study | China | 3 | Fever (= 3) | Third trimester (= 3) |
2 cases: positive nucleic acid test through throat swab, 1 case: clinical confirmation |
None | Cesarean section (= 3) | 2 patients cured and discharged; one underwent isolation treatment |
| Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia | Zhu et al. | Case study | China | 9 |
Fever (= 7) Cough (= 4) Cholecystitis (= 1) Diarrhea (= 1) |
Third trimester* | Chest CT scan and throat swab nucleic acid testing** | None |
Cesarean section (= 7) Vaginal delivery (= 2) |
Cured and discharged |
| Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records | Chen et al. | Case study | China | 9 |
Fever (= 7) Cough (= 4) Myalgia (= 3) Sore throat (= 2) Malaise (= 2) |
Third trimester | CT scan of lung and throat swab nucleic acid testing | None | Cesarean section (= 9) | Cured and discharged |
| Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province | Zhang et al. | Case–control | China |
16 (45 Controls) |
15 moderate case and 1 severe case of pneumonia | Third trimester | Clinical diagnosis and throat swab nucleic acid detection | Severe case (= 1) | Cesarean section (= 16) | Cured and discharged |
| Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy | Liu et al. | Case Study | China | 13 |
Fever (= 10) Dyspnea (= 3) Fatigue (= 2) Cough (= 2) Sore throat (= 1) No symptoms (= 1) |
Third trimester (= 11), Less than 28 weeks GA (= 2) |
Clinical symptoms and throat swab nucleic acid detection | Severe pneumonia and intubation (= 1) |
Cesarean section (= 10) Still pregnant (= 3) |
Cured and discharged One case still in the hospital |
| Lack of vertical transmission of severe acute respiratory syndrome Coronavirus 2, China | Li et al. | Case Report | China | 1 | Cough and temperature of 37.2 °C | Third trimester | Clinical symptoms and throat swab nucleic acid detection | None | Cesarean section | Cured and discharged |
| A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery | Wang et al. | Case Report | China | 1 | Fever | Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section | Cured and discharged |
| A case report of neonatal COVID-19 infection in China | Wang et al. | Case report | China | 1 | Fever | Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section | Cured and discharged |
| Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? | Fan et al. | Case report | China | 2 |
Fever (= 2) Nasal congestion (= 2) Chill (= 1) Sore throat (= 1) Abdominal rush (= 1) |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section (= 2) |
One case still in the hospital One case cured and discharged |
| Clinical analysis of pregnant women with 2019 Novel Coronavirus Pneumonia | Chen et al. | Case series | China | 5 |
Fever (= 5) Coryza (= 1) Sputum (= 1) Cough (= 1) |
Third trimester (= 5) |
Clinical symptoms and Chest CT scan and SARS-CoV-2 quantitative RT-PCR |
None |
Cesarean section (= 2) Vaginal delivery (= 3) |
No death was reported |
| Possible vertical transmission of SARS-CoV-2 From an infected mother to her newborn | Dong et al. | Case report | China | 1 | Fever and Nasal congestion | Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section | Cured and discharged |
| Lung ultrasound and computed tomographic findings in a pregnant woman with COVID-19 | Kalafat et al. | Case report | Turkey | 1 | Cough and shortness of breath | Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Severe pneumonia and intubation | Cesarean section | Still in hospital |
| Coronavirus disease 2019 (COVID-19) during pregnancy: a case series | Liu et al. | Case series | China | 3 |
Fever (= 2) Cough (= 1) |
Third trimester (= 3) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None |
Cesarean section (= 2) Vaginal delivery (= 1) |
No death was reported |
| Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case–control study | Li et al. | Case–control | China | 16 | Fever (= 12) | Third trimester (= 16) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None |
Cesarean section (= 14) Vaginal delivery (= 2) |
No death was reported Cured and discharged (= 8) |
| A pregnant woman with COVID-19 in Central America | Zambrano et al. | Case report |
The United States, USA |
1 | Fever, headache, myalgia, and cough | Third trimester | Clinical symptoms and throat swab nucleic acid detection | None | Vaginal delivery | No death was reported |
|
Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis |
Liu et al. | Cross-sectional | China | 15 |
Fever (= 13) Cough (= 9) Fatigue (= 4) Muscle ache (= 3) Dyspnea (= 1) Sore throat (= 1) Diarrhea (= 1) No clinical symptoms (= 1) Post-partum fever (= 1) |
Third trimester (= 13) Second trimester (= 2) |
Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None |
Cesarean section (= 10) Vaginal delivery (= 1) Still pregnant (= 4) |
All patients survived |
| Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-center, descriptive study | Yu et al. | Retrospective study | China | 7 |
Fever (= 6) Cough (= 1) Dyspnea (= 1) Diarrhea (= 1) |
Third trimester (= 7) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None |
Cesarean section (= 7) |
Cured and discharged (= 7) |
|
Neonatal early-onset Infection with SARS CoV-2 in 33 neonates born to mothers With COVID-19 in Wuhan, China |
Zeng et al. | Cohort study | China | 33 |
Fever on admission (= 8) Cough (= 10) Post-partum fever (= 5) |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None |
Cesarean section (= 26) Vaginal delivery (7) |
No death was reported |
| Mortality of a pregnant patient diagnosed with COVID-19: a case report with clinical, radiological, and histopathological findings | Karami et al. | Case report | Iran | 1 |
Fever Myalgia Cough |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Multiple organ dysfunction and death | Vaginal delivery | Not survived |
| Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report | Peng et al. | Case report | China | 1 |
Fever Fatigue Shortness of breath |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported | Cesarean section | Survived |
| Severe COVID-19 during pregnancy and possible vertical transmission | Alzamora et al. | Case report |
The United States, USA |
1 |
Fever (low grade) Shortness of breath Malaise |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Severe pneumonia and intubation | Cesarean section | No death was reported |
| Preterm delivery in a pregnant woman with critical COVID-19 pneumonia and vertical transmission | Zamanian et al. | Case report | Iran | 1 |
Fever Myalgia Nausea Cough Dyspnea Anorexia |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Severe pneumonia and intubation | Cesarean section | Not survived |
| Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19 | Xiong et al. | Case report | China | 1 |
Fever Cough Shivering |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported | Vaginal delivery | Healthy and discharged |
| Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women | Khan et al. | Case series | China | 17 |
Cough (= 6) Fever (= 3) Diarrhea (= 3) Nasal congestion (= 2) shortness of breath (= 2) Sputum production (= 1) |
Third trimester (= 17) | Clinical symptoms and Chest CT scan and/or throat swab nucleic acid detection | Not reported | Cesarean section (= 17) | No case of death was reported |
| Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to- neonatal intrapartum transmission of COVID-19 during natural birth | Khan et al. | Case report | China | 3 |
Fever (= 2) Cough (= 3) Chest tightness (= 1) |
Third trimester (= 3) | Clinical symptoms throat swab nucleic acid detection | Not reported | Vaginal delivery (= 3) | No case of death was reported |
| Clinical characteristics of 19 neonates born to mothers with COVID-19 | Liu et al. | Retrospective study | China | 19 |
Fever (= 11) Cough (= 5) Diarrhea (= 2) |
Third trimester (19) |
Clinical diagnosis (= 9) Laboratory confirmed (= 10) |
Not reported |
Cesarean section (= 18) Vaginal delivery (= 1) |
No case of death was reported |
| COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals | Breslin et al. | Cohort study |
The United States, USA |
43 |
No symptoms (= 14) Fever (= 14) Cough (= 19) Myalgias or fatigue (= 11) Dyspnea (= 7) Chest pain (= 5) Headache (= 8) |
Third trimester (43) | Clinical symptoms and throat swab nucleic acid detection |
Severe case (= 4) Intubation and ICU admission (= 2) |
Cesarean section (= 8) Vaginal delivery (= 10) Discharge for continuing pregnancy (= 25) |
No case of death was reported |
| Clinical features and outcomes of pregnant women suspected of Coronavirus Disease 2019 | Yang et al. | Case–control | China | 13 (42 controls) |
Prenatal fever (= 2) Postpartum Fever (= 8) Cough (= 2) |
Third trimester | Clinical symptoms and Chest CT scan and/or throat swab nucleic acid detection | Not reported |
Cesarean section (= 9) Vaginal delivery (= 4) |
No case of death was reported |
| Asymptomatic COVID-19 in pregnant woman with typical chest CT manifestation: a case report | Renbin et al. | Case report | China | 1 | Asymptomatic | Third trimester | Chest CT scan and throat swab nucleic acid detection | Not reported | Cesarean section | No case of death was reported |
| Chest CT Findings in a Pregnant patient with 2019 Novel Coronavirus Disease | Liao et al. | Case report | China | 1 |
Fatigue Cough |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported | Cesarean section | No case of death was reported |
| Infants born to mothers with a new Coronavirus (COVID-19) | Chen et al. | Case report | China | 4 |
Fever (= 3) Cough (= 2) Headache (= 2) |
Third trimester (= 4) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported |
Cesarean section (= 3) Vaginal delivery (= 1) |
No case of death was reported |
| Anesthetic management for emergent cesarean delivery in a parturient with recent diagnosis of Coronavirus Disease 2019 (COVID-19): a case report | Song et al. | Case report | China | 1 |
Fever Cough Myalgia |
Third trimester | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported | Cesarean section | No case of death was reported |
| Clinical characteristics and risk assessment of newborns born to mothers with COVID-19 | Yang et al. | Case series | China | 7 |
Fever (= 5) Cough (= 1) Diarrhea (= 1) Abdominal pain (= 1) |
Third trimester (= 7) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Not reported | Cesarean section (= 7) | No case of death was reported |
| COVID-19 in pregnancy: early lessons | Breslin et al. | Case series |
The United States, USA |
7 |
Fever (= 2) Cough (= 3) Myalgia (= 3) Headache (= 2) Asymptomatic (= 2) |
Third trimester (= 7) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | Intubation and ICU admission (= 2) |
Cesarean Section (= 2) No report of other 5 patients |
No case of death was reported |
| Antibodies in infants born to mothers with COVID-19 Pneumonia | Zeng et al. | Case study | China | 6 |
Mild clinical presentations (= 6) |
Third trimester (= 6) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section (= 6) | No case of death was reported |
| Novel Coronavirus infection in newborn babies under 28 days in China | Zhang et al. | Case series | China | 4 |
Fever (= 3) Cough (= 2) A decrease in appetite (= 1) Oil intolerance (= 1) |
Third trimester (= 4) | Clinical symptoms and Chest CT scan and throat swab nucleic acid detection | None | Cesarean section (= 4) | No case of death was reported |
| Clinical characteristics of pregnant women with Covid-19 in Wuhan, China | Chen et al. | Retrospective study | China | 118 |
Fever (= 84) Cough (= 82) Chest tightness (= 20) Fatigue (= 19) Dyspnea (= 8) Diarrhea (= 8) Headache (= 7) Asymptomatic (= 6) |
Third trimester (= 75) First or second trimester (= 43) |
84 women confirmed with Nucleic acid testing and 34 others diagnosed with CT scan | 9 severe case and 1 need of mechanical ventilation |
Cesarean section (= 63) Vaginal delivery (= 5) Spontaneous abortion (= 3) Ectopic pregnancy (= 2) Induced abortion (= 4) Still pregnant (= 41) |
No case of death was reported |
| Summary | Total number of cases: 386 |
Fever (= 227/364) Cough (= 165/364) Asymptomatic (25/364) Fatigue (= 26/364) Dyspnea (= 21/364) Chest tightness (21/364) Headache (= 20/364) Diarrhea (= 17/364) Myalgia (= 13/364) Sore throat (5/364) Malaise (= 3/364) |
Third trimester (= 341) Second trimester (= 45) |
Clinical + CT scan + oropharyngeal swab NAT |
Severe pneumonia (= 22) Number of death (= 2) |
Cesarean section (= 257) Vaginal delivery (= 42), Continuing pregnancy (= 73) Spontaneous abortion (= 3) Ectopic pregnancy (= 2) Induced abortion (= 4) |
Number of death: 2 |
NAT Nucleic Acid testing, CT computed tomography
*4 cases before delivery, 2 cases on the day of delivery, 3 cases after delivery
**Mother of twins, with typical clinical and chest CT finding of nCoV-2019 pneumonia confirmed as a nCoV-2019 after rule out of other causes although NAT was negative
***3 patients cured and discharged to continue the pregnancy, 9 patients gave birth and then cured and discharged, 1 patient with severe pneumonia intubated
Table 2.
Characteristics of neonates born from pregnant women with COVID-19 included in the systematic review
| Article title | Author | Study type | Country | Number of neonates | Neonatal maturity (= N) |
Neonatal clinical presentations (= N) |
Neonatal complications | Neonate test for nCoV-2019 | Apgar score | Neonatal outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Result | Diagnostic method | ||||||||||
| Pregnant women with new coronavirus infection: clinical characteristics and placental pathological analysis of three cases | Chen et al. | Case study | China | 3 |
Mature infants (= 2) Premature with LBW (= 1) |
No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | Not reported | Healthy and discharged |
| Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia | Zhu et al. | Case study | China |
10 (2 twins) |
4 full terms, 6 premature (2 SGA AND 1 LGA) |
Respiratory distress (= 6), GI tract symptoms (= 4), Fever (= 2) Increased heart rate (= 1) Vomiting (= 1) |
Death (= 1)** DIC (= 1)** |
Negative | Neonatal throat swab nucleic acid testing |
5th min Apgar score: 10 (= 6) 9 (= 2) 8 (= 2) |
Cured (= 5) In hospital (= 4) Died (= 1) |
| Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records | Chen et al. | Case study | China | 9 | Full-term babies (= 5), birth at 36th week of gestational age (= 4*) | No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | All babies with 5th min Apgar score of 9 to 10 | None of the neonates needed special treatment |
| Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province | Zhang et al. | Case–control | China | 10 |
Full-term babies (= 9) Premature babies (= 1) |
3 neonate developed bacterial pneumonia | No complications were reported | Negative | Neonatal throat swab nucleic acid testing and imaging study | Not reported | None of the neonates needed special treatment. No neonatal death |
| Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy | Liu et al. | Case Study | China | 10 | Full-term babies (= 4), Premature babies (= 6) |
9 neonates survived with no remarkable clinical problem, 1 died due to ARDS and MODS |
1 neonate died due to MODS | Negative | Neonatal throat swab nucleic acid testing | 1st min Apgar score: 10 for all nine alive babies | 1 dead neonate because of MODS |
| Lack of Vertical transmission of severe acute respiratory syndrome Coronavirus 2, China | Li et al. | Case Report | China | 1 | Premature baby in 35th week of GA | No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | Not reported | Healthy and discharged |
| A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery | Wang et al. | Case report | China | 1 | Premature baby in 30th week of GA | No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 10 | Healthy and discharged |
| A case report of neonatal COVID-19 infection in China | Wang et al. | Case report | China | 1 | Full-term baby | COVID-19 Pneumonia | No complications were reported | Positive | Neonatal throat swab nucleic acid testing (36th-hour birth) | 5th min Apgar score: 9 | Healthy and discharged |
| Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? | Fan et al. | Case report | China | 2 |
Full-term neonate (= 1) 36th week and 5 days of GA (= 1) |
Mild neonatal pneumonia and lymphopenia (= 1) Low-grade Fever and diffuse haziness of lungs without patchy consolidation which cured with antibiotic |
No complications were reported | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 10 | Healthy and discharged |
| Clinical analysis of pregnant women with 2019 Novel Coronavirus pneumonia | Chen et al. | Case series | China | 5 | Full-term neonate (= 5) | Fetal tachycardia (= 1) | No complications were reported | Negative | Neonatal throat swab nucleic acid testing |
5th min Apgar score: 10 (= 5) |
Healthy |
| Possible vertical transmission of SARS-CoV-2 From an infected mother to her newborn | Dong et al. | Case report | China | 1 | 34 weeks and 5 days | Elevated IgM antibody*** | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 10 | Healthy and discharged |
|
Lung ultrasound and computed tomographic findings in a pregnant woman with COVID-19 |
Kalafat et al. | Case report | Turkey | 1 | 35 weeks and 3 days | No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 9 | Healthy |
| Title: Coronavirus disease 2019 (COVID-19) during pregnancy: a case series | Liu et al. | Case series | China | 3 | Full-term neonates (= 3) | Chorioamnionitis and meconium aspiration syndrome (= 1) | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 9 (= 3) | Survived (= 3) |
| Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case–control study | Li et al. | Case–control | China | 17 |
Full-term (= 13) Premature (= 4) LBW (= 3) |
Intrauterine fetal distress (= 2) | No complications were reported | Negative |
Neonatal throat swab nucleic acid testing (= 3)**** |
5th min Apgar score: 10 (= 17) |
No death was reported |
| A pregnant woman with COVID-19 in Central America | Zambrano et al. | Case report |
United States, USA |
1 | 32 weeks of GA | No remarkable clinical problem was reported | No complications were reported | Negative | Neonatal throat swab nucleic acid testing | Not reported | No death was reported |
|
Pregnancy and Perinatal outcomes of women with Coronavirus Disease (COVID-19) Pneumonia: A Preliminary Analysis |
Liu et al. | Cross-sectional | China | 11 |
Full-term (= 8) Preterm delivery (= 3) |
No remarkable clinical problem was reported | No complications were reported | Negative | Not reported***** | 5th min Apgar score: 9 | No death was reported |
| Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-center, descriptive study | Yu et al. | Retrospective study | China | 7 |
Full-term (= 7) |
Mild shortness of breath (= 1) | Mild pulmonary infection in a neonate with positive COVID-19 test |
Negative (= 2) Positive (= 1)****** |
Neonatal throat swab nucleic acid testing |
5th min Apgar score: 9 -10 (= 7) |
No death was reported |
| Neonatal early-onset infection with SARS CoV-2 in 33 neonates born to mothers With COVID-19 in Wuhan, China | Zeng et al. | Cohort study | China | 33 |
Full-term (= 29) Preterm (= 4) |
Fever (= 2; both with positive COVID-19) Shortness of breath (= 4; 3 with negative COVID-19 and one positive) Cyanosis (= 3; 2 with negative COVID-19 and one with positive) Feeding intolerance (= 3; 2 with negative COVID-19 and one with positive) |
Asphyxia (= 2; one neonate with negative COVID-19 infection and one neonate with positive COVID-19 infection) Pneumonia (3; all 3 with positive COVID-19) Respiratory distress syndrome (4; 3 with negative COVID-19 and one positive) Requiring mechanical ventilation: 1 baby with COVID-19 positive |
Negative (= 30) Positive (= 3) |
Neonatal throat swab nucleic acid testing | Not reported******* | No death was reported |
| Mortality of a pregnant patient diagnosed with COVID-19: a case report with clinical, radiological, and histopathological findings | Karami et al. | Case report | Iran | 1 | Stillbirth | – | – | Not reported | Not reported | Apgar score:0 | Fetal death |
| Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report | Peng et al. | Case report | China | 1 | Preterm | Mild respiratory distress | None | Negative | Neonatal throat and anal and swab and sputum and serum nucleic acid testing | 5th min Apgar score: 10 | Survived |
| Severe COVID-19 during pregnancy and possible vertical transmission | Alzamora et al. | Case report | The United States, USA | 1 | Preterm |
Mild respiratory distress And sporadic cough |
Intubation because of mother’s sedation | Positive |
Neonatal throat swab nucleic acid testing (16 h after delivery) |
5th min Apgar score: 8 | No death was reported |
| Preterm delivery in a pregnant woman with critical COVID-19 pneumonia and vertical transmission | Zamanian et al. | Case report | Iran | 1 | Preterm | Fever | None | Positive | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 9 | Survived |
| Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19 | Xiong et al. | Case report | China | 1 | Full-term | No remarkable clinical problem was reported | None | Negative | Neonatal throat and anal swab nucleic acid testing | 5th min Apgar score: 10 | Healthy and discharged |
| Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women | Khan et al. | Case series | China | 17 |
Full-term (= 14) Preterm (= 3) |
Neonatal pneumonia (= 5) 2 case of COVID-19 which one of them developed pneumonia |
No serious complications were reported |
Negative (= 15) Positive (= 2) |
Neonatal throat and anal swab nucleic acid testing | 5th min Apgar score: 9–10 | No case of death was reported |
| Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to- neonatal intrapartum transmission of COVID-19 during natural birth | Khan et al. | Case report | China | 3 |
Full-term (= 2) Preterm (= 1) |
No remarkable clinical problem was reported | None | Negative (= 3) | Neonatal throat and anal swab nucleic acid testing | 5th min Apgar score: 9–10 | No case of death was reported |
| Clinical characteristics of 19 neonates born to mothers with COVID-19 | Liu et al. | Retrospective study | China | 19 |
Full-term (= 17) Preterm (= 2) |
No remarkable clinical problem was reported | None | Negative (= 19) | Neonatal throat and anal swab nucleic acid testing | 5th min Apgar score: 9 | No case of death was reported |
| COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals | Breslin et al. | Cohort study |
The United States, USA |
18 |
Full-term (= 17) Premature (= 1) |
Respiratory distress (= 1) One patient with congenital disease |
None | Negative (= 18; including one intermediate result which considers as negative because of low detection) | Neonatal throat and anal swab nucleic acid testing | 5th min Apgar score: 9–10 | All healthy and discharged |
| Clinical features and outcomes of pregnant women suspected of Coronavirus Disease 2019 | Yang et al. | Case–control | China | 20******** | Mean ± SD GA: 38.2 ± 2.3 | Fever (= 1 from COVID-19 positive mother) | None | Negative | Neonatal throat and anal swab nucleic acid testing | Not reported | No case of death was reported |
| Asymptomatic COVID-19 in a pregnant woman with typical chest CT manifestation: a case report | Renbin et al. | Case report | China | 1 | Full-term | No remarkable clinical problem was reported | None | Negative | Neonatal throat swab nucleic acid testing | Not reported | Healthy and discharged |
| Chest CT findings in a pregnant patient with 2019 Novel Coronavirus Disease | Liao et al. | Case report | China | 1 | Preterm | No remarkable clinical problem was reported | None | Negative | Neonatal throat and anal swab nucleic acid testing | Not reported | No case of death was reported |
| Infants born to mothers with a new Coronavirus (COVID-19) | Chen et al. | Case report | China | 4 | Full-term (= 4) | No remarkable clinical problem was reported | None |
Negative (= 4) |
Neonatal throat and anal swab nucleic acid testing | Not reported | No case of death was reported |
| Anesthetic management for emergent cesarean delivery in a parturient with recent diagnosis of Coronavirus Disease 2019 (COVID-19): a case report | Song et al. | Case report | China | 1 | Preterm | No remarkable clinical problem was reported | None | Negative | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 9 | Healthy and discharged |
| Clinical characteristics and risk assessment of newborns born to mothers with COVID-19 | Yang et al. | Case series | China | 7 |
Full-term (= 3) Preterm (= 4) |
Mild respiratory distress syndrome (= 2) Vomiting and hypoglycemia (= 1) |
None |
Negative (performed for 6 neonates) |
Neonatal throat swab nucleic acid testing | 5th min Apgar score: 9–10 | No case of death was reported |
| COVID-19 in pregnancy: early lessons | Breslin et al. | Case series |
The United States, USA |
2 | Full-term (= 2) | No remarkable clinical problem was reported | None |
Negative (performed for one neonate) |
Neonatal throat swab nucleic acid testing | Not reported | No case of death was reported |
|
Antibodies in Infants Born to mothers with COVID-19 Pneumonia |
Zeng et al. | Case study | China | 6 | Not reported | No remarkable clinical problem was reported********* | None | Negative (= 6) | Neonatal throat and serum swab nucleic acid testing | Not reported | No case of death was reported |
| Novel Coronavirus infection in newborn babies under 28 days in China | Zhang et al. | Case series | China | 2 | Full-term (= 2) | Shortness of breath (= 1) | None | Positive | Neonatal throat swab nucleic acid testing | Not reported | No case of death was reported |
| Clinical characteristics of pregnant women with Covid-19 in Wuhan, China | Chen et al. | Retrospective study | China |
70 (2 set of twins) |
Full-term (= 56) Preterm (14) |
No remarkable clinical problem was reported | None | Negativeϕ | Neonatal throat swab nucleic acid testing | 5th min Apgar score: 8-9ϕ | No case of death was reported |
| Total results | Total number of neonates: 302 |
Full-term (= 210/276) Premature (= 65/276) stillbirth (= 1) |
DIC (= 2) MODS (= 1) |
Negatives (= 208) And positive (= 11) |
Survived (= 299) died (= 3) |
||||||
MODS Multiple organ dysfunction syndrome, ARDS Acute respiratory distress syndrome, DIC Disseminated intravascular coagulation, GA gestational age, SGA Small for gestational age, LGA Large for gestational age, LBW low birth weight, C-Section Cesarean section
We considered GA < 37 weeks as preterm delivery
*One complicated with pre-eclampsia, one with history of 2 stillbirth, one with history of 2 previous c-sections and irregular contractures, and one with premature rupture of membranes
**One neonate in which first symptom was increased heart rate developed refractory shock and gastric bleeding which lead to death, another neonate with shortness of breath and moaning and later with DIC that cured
***SARS-CoV-2 IgG level: 140.32 AU/mL and IgM level: 45.83 AU/mL 2 h after birth and also 16 days after birth repeated test revealed IgG level of 69.94 AU/mL and IgM level of 11.75 AU/mL
****The specimens collected from three neonates whom delivered by cesarean section
*****The study claimed that no COVID-19 infection was represented in neonates but did not clarified by which method -clinical or nucleic acid testing-
******Specimens collected from three neonates and positive sample was collected 36 h after birth
*******Except one of infected neonates with confirmed COVID-19 infection born with need of resuscitation and Apgar score of 3, 4, 5 in 1, 5 and 10 min
********The total number of neonates were 57 and 20 neonates tested for COVID-19 but study did not clarify how many neonates belong to the case group
*********2 neonates had elevated serum IgM levels
ϕNasopharyngeal swab was taken from 8 neonates
ϕϕApgar score was measured for 66 neonates
Table 3.
A summary of studies on pregnancy outcomes in pregnant women with COVID-19 included in the systematic review
| Article title | Author | Study type | Country | Placental test for nCoV-2019 nucleic acid | Pregnancy complications | Further information | |
|---|---|---|---|---|---|---|---|
| Result | Method | ||||||
| Pregnant women with new coronavirus infection: clinical characteristics and placental pathological analysis of three cases | Chen et al. | Case study | China | Negative | RT-PCR | Not reported |
Umbilical cord and fetal membranes were tested and went negative |
| Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia | Zhu et al. | Case study | China | Not reported | Not reported |
Premature rupture of membranes (= 3), One polyhydramnios, One oligohydramnios |
No further samples were examined |
| Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records | Chen et al. | Case study | China | Not reported | Not reported |
Premature rupture of Membranes (= 2), Fetal distress (= 2) |
All amniotic fluid, cord blood, breastmilk samples from six patients were negative (3 cases has unsuccessful sample collection) |
| Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province | Zhang et al. | Case–control | China | Not reported | Not reported |
Pre-eclampsia (= 1), PROM (= 3), Fetal distress (= 1), Premature birth (= 3), Asphyxia (= 1) |
No further samples were examined |
| Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy | Liu et al. | Case study | China | Not reported | Not reported |
Fetal distress (= 3), PROM (= 1), Stillbirth (= 1) |
No further samples were examined |
| Lack of vertical transmission of severe acute respiratory syndrome Coronavirus 2, China | Li et al. | Case report | China | Negative | RT-PCR | Not reported | Serum, urine, feces, amniotic fluid, umbilical cord blood and placenta, and breast milk samples were negative |
| A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery | Wang et al. | Case report | China | Negative | RT-PCR | Not reported | Amniotic fluid and cord blood were negative |
| A case report of neonatal COVID-19 infection in China | Wang et al. | Case report | China | Negative | RT-PCR | Not reported | Cord blood and mother's breast milk were negative |
| Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? | Fan et al. | Case report | China | Negative | RT-PCR | Not reported | Umbilical cord blood, amniotic fluid, vaginal swabs, and mother’s breast milk were negative |
| Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia | Chen et al. | Case series | China | Not reported | Not reported |
Pre-eclampsia (= 1) Gestational diabetes (= 2) |
Not reported |
| Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn | Dong et al. | Case report | China | Not reported | Not reported | Not reported | Mother’s vaginal discharge and breastmilk were negative for COVID-19 PCR test result |
| Lung ultrasound and computed tomographic findings in a pregnant woman with COVID-19 | Kalafat et al. | Case report | Turkey | Negative | RT-PCR | Not reported | Breast milk and cord blood were negative |
| Coronavirus disease 2019 (COVID-19) during pregnancy: a case series | Liu et al. | Case series | China | Negative | RT-PCR | Gestational hypertension | Breast milk, cord blood, amniotic fluid, neonatal serum, and mothers’ vaginal mucosa were negative |
| Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case–control study | Li et al. | Case–control | China | Not reported | Not reported |
gestational diabetes mellitus (= 3) PROM (= 1) gestational hypertension (= 3), hypothyroidism (= 2), pre-eclampsia (= 1) Sinus tachycardia (= 1) Fetal distress (= 2) |
Not reported |
| A pregnant woman with COVID-19 in Central America | Zambrano et al. | Case report |
United States, USA |
Not reported | Not reported |
gestational hypertension and hypothyroidism |
Neonate’s blood sample was negative |
| Pregnancy and perinatal outcomes of women with Coronavirus Disease (COVID-19) pneumonia: a preliminary analysis | Liu et al. | Cross-sectional | China | Not reported | Not reported | Placenta previa (= 1) | Not reported |
| Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-center, descriptive study | Yu et al. | Retrospective study | China | Not reported | Not reported |
Uterine scarring (= 3) Hypothyroidism (= 1) |
Not reported |
|
Neonatal Early-Onset Infection with SARS CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China |
Zeng et al. | Cohort study | China | Not reported | Not reported | PROM (= 3) | Not reported |
| Mortality of a pregnant patient diagnosed with COVID-19: A case report with clinical, radiological, and histopathological findings | Karami et al. | Case report | Iran | Not reported | Not reported | Not reported | Not reported |
| Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report | Peng et al. | Case report | China | Negative | RT-PCR | Not reported | Amniotic fluid, vaginal mucosa, cord blood, and breast milk were all negative |
| Severe COVID-19 during pregnancy and possible vertical transmission | Alzamora et al. | Case report |
The United States, USA |
Not reported | Not reported | Diabetes mellitus | Not reported |
| Preterm delivery in a pregnant woman with critical COVID-19 pneumonia and vertical transmission | Zamanian et al. | Case report | Iran | Not reported | Not reported | Not reported | Cord blood was negative, but Amniotic fluid was positive |
| Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19 | Xiong et al. | Case report | China | Negative | RT-PCR | Not reported | Amniotic fluid was negative |
| Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women | Khan et al. | Case series | China | Not reported | Not reported | 5 women with other complications | Not reported |
| Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to- neonatal intrapartum transmission of COVID-19 during natural birth | Khan et al. | Case report | China | Not reported | Not reported | Not reported | The cord blood sample was negative |
| Clinical characteristics of 19 neonates born to mothers with COVID-19 | Liu et al. | Retrospective study | China | Not reported | Not reported | Not reported | Breast milk sample, amniotic fluid, and cord blood were negative |
| COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals | Breslin et al. | Cohort study |
The United States, USA |
Not reported | Not reported | PROM | Not reported |
| Clinical features and outcomes of pregnant women suspected of Coronavirus Disease 2019 | Yang et al. | Case–control | China | Not reported | Not reported | Not reported | Not reported |
| Asymptomatic COVID-19 in a pregnant woman with typical chest CT manifestation: a case report | Renbin et al. | Case report | China | Not reported | Not reported | Not reported | Not reported |
| Chest CT findings in a pregnant patient with 2019 Novel Coronavirus Disease | Liao et al. | Case report | China | Negative | RT-PCR | Not reported | Amniotic fluid and cord blood were negative |
| Infants born to mothers with a new Coronavirus (COVID-19) | Chen et al. | Case report | China | Not reported | Not reported | Placenta (= 1) | Not reported |
| Anesthetic management for emergent cesarean delivery in a parturient with recent diagnosis of Coronavirus Disease 2019 (COVID-19): a case report | Song et al. | Case report | China | Not reported | Not reported | Not reported | Not reported |
| Clinical characteristics and risk assessment of newborns born to mothers with COVID-19 | Yang et al. | Case series | China | Not reported | Not reported | Not reported | Cord blood and amniotic fluid were negative |
| COVID-19 in pregnancy: early lessons | Breslin et al. | Case series |
The United States, USA |
Not reported | Not reported | Type 2 diabetes mellitus (= 2) | Not reported |
| Antibodies in infants born to mothers with COVID-19 pneumonia | Zeng et al. | Case study | China | Not reported | Not reported | Not reported | Not reported |
| Novel Coronavirus infection in newborn babies under 28 Days in China | Zhang et al. | Case series | China | Not reported | Not reported | Not reported | Not reported |
| Clinical characteristics of pregnant women with Covid-19 in Wuhan, China | Chen et al. | Retrospective study | China | Not reported | Not reported | Not reported | Breast milk of three mothers were negative for the virus |
| Total results | All samples examined were negative | RT-PCR | |||||
RT-PCR Reverse transcription-polymerase chain reaction, PROM Premature rupture of membranes
Clinical presentation of COVID-2019 in pregnant women
Of 37 studies, two provided no data on clinical symptoms of pregnant patients [43, 44]. A total of 364 pregnant women was, thus, included in the data synthesis of clinical manifestations of COVID-19 in pregnant women.
Of 364 pregnant women, 25 were asymptomatic at the time of admission. The most common symptoms were fever (62.4%) and cough (45.3%). The other common symptoms included myalgia, diarrhea, dyspnea, headache, and chest tightness. There were two women with specific presentations: one with Cholecystitis [50] and another with oil intolerance [67].
For nearly all pregnant women, the diagnosis was made based on a combination of clinical symptoms, nucleic acid testing for the novel coronavirus, and computed tomography (CT). As for the general population, some pregnant patients (n = 44) had a negative SARS-CoV-2 test but displayed clinical manifestations and abnormalities in CT scan related to COVID-19 [50, 53, 55].
Twenty-two (6.0%) pregnant patients developed severe pneumonia. Among them, 10 cases (2.8%) required mechanical ventilation and therefore were admitted to the intensive care unit (ICU) [42, 44, 53, 58, 60, 63, 65, 73, 74]. Two of these ten patients died from severe pneumonia and multiple organ dysfunction [65, 73].
The vast majority of patients were in their third trimester of pregnancy, and only 45 cases were in the first or second trimester (12.4%). Of the total number of 299 births, there were 257 (86%) cesarean sections, and 42 (14%) vaginally completed. Zhang L et al. and Breslin et al. reported obstetric reasons such as premature rupture of membrane, fetal distress, and other indications for the Cesarean section [44, 60]. Chen et al. reported that 38 of 63 cases who underwent cesarean sections claimed to have a fear of COVID-19 [53]. There were three cases of spontaneous abortions, two ectopic pregnancy, and four induced abortions. Pregnant women seeking induced abortion were most afraid of COVID-19 and its potential effects on pregnancy outcomes [53].
Neonatal outcomes
Thirty-seven studies included a total of 302 neonates from mothers with COVID-19. Two studies have not indicated the timing of birth [43, 57]. Of the studies that provided data, there were 210 full-term and 65 preterm neonates.
Karami et al. reported the death of a mother from COVID-19 and also her fetus [65]. The dead baby was born with an Apgar score of 0, did not respond to resuscitation, and was not considered for COVID-19 diagnostic tests. Of the babies born alive from mothers with COVID-19, five newborns faced critical conditions. One of them presented with a fast heart rate developed gastric bleeding and refractory shock later and died. The second complicated case was a premature newborn born from a mother, who had a diagnosis of severe COVID-19 pneumonia [50]. This neonate showed shortness of breath at presentation and developed disseminated intravascular coagulation (DIC). This case could be cured. The third neonate died due to the multiple organ dysfunction syndrome and could not survive [58]. The nasopharyngeal samples of these three babies were all negative for SARS-CoV-2 RNA detection. The fourth one suffered from pneumonia and needed intubation at birth. Sixteen hours after birth, the neonate tested positive for SARS-CoV-2 RNA with throat swab nucleic acid testing [74]. This neonate was later extubated and discharged without any complications. The fifth one was a premature baby with the gestational age of 31 weeks and 2 days. This neonate had an Apgar score of 3, 4, and 4 at the first, fifth, and tenth minute after delivery and required resuscitation [66]. This neonate was later confirmed as a definite case of COVID-19 and developed DIC. Vital signs were successfully stabilized on the day of 14. This neonate had close contact with the mother after delivery.
Except for the babies mentioned above, most babies born alive had a 5-min Apgar score of 8 and 9 (Table 2). A total of 219 neonates underwent nasopharyngeal specimen collection for SARS-CoV-2 nucleic acid testing. Of them, 11 tested positive, and two of which were described above. A study by Wang S et al. reported a neonate with a positive throat specimen for COVID-19 [48]. This neonate had early close contact with COVID-19 positive mother, and the specimen was collected 36 h after birth, while the placental and cord blood specimens taken at birth were negative. Yu N et al. collected nasopharyngeal swab from three neonates, of which one was positive for COVID-19 [56]. This specimen was collected 36 h after birth, and that no nucleic acid testing was performed for the placenta, cord blood, or other pregnancy products.
In a cohort study of 33 neonates, there were two neonates with a positive test [66]. Both neonates survived. None of the placenta, cord blood, and other pregnancy products were tested for COVID-19 in this study. Zamanian et al. reported another newborn with a positive test who had fever without any further complications. By the end of the study, the neonate was healthy and stable [73]. Also, the other four COVID-19 positive neonates did not develop any complications and survived [46]. Seventeen studies reported the collection of the amniotic fluid, cord blood, placenta, and breast milk samples, and all tested negative except one amniotic fluid sample. Zamanyan et al. reported a pregnant woman with COVID-19 infection and her positive newborn. Nucleic acid testing was done on the cord blood and amniotic fluid samples [73]. Whereas no viral RNA was detected in the cord blood, the amniotic fluid was positive for viral RNA.
Pregnancy outcomes
In a case–control study by Zhang et al., there was no difference between 16 pregnant women with COVID-19 and 45 pregnant women without COVID-19 in terms of pregnancy complications, including eclampsia, fetal distress, and premature rupture of membrane (Table 3) [44].
Discussion
This systematic review included 386 pregnant women with COVID-19. There were 257 cesarean sections and 42 vaginal delivery. This relatively higher rate of cesarean sections would reflect the existence of indications for a cesarean section as well as the role of fear of vertical transmission. Most women represented common symptoms, and two deaths occurred (death rate of 0.5%). While COVID-19 has, to date, caused a total number of 163,097 deaths out of 2.4 million confirmed cases, corresponding to the mortality rate of about 7% [77]. Therefore, compared to the general population, pregnant women have not shown a more aggressive form of COVID-19.
Among the total number of 302 neonates from mothers with COVID-19, there were nasopharyngeal specimens collected from 219 neonates, of which 11 tested positives for SARS-CoV-2. One study reported a positive SARS-CoV-2 for amniotic fluid samples [73]. Interestingly, two studies reported high IgM levels in neonates who tested negative for SARS-CoV2 [43, 69]. Because there is no possibility of IgM transfer through the placenta, this laboratory data can be suggestive of vertical transmission of COVID-19. More studies are required to investigate the potential of COVID-19 to be transmitted via the vaginal route and the possible association between maternal infection with COVID-19 and long-term child health.
Nearly all mothers were healthy women without underlying severe diseases such as diabetes mellitus, cardiovascular disease, and autoimmune diseases. Therefore, further research is necessary to evaluate whether or not ethnicity/race, maternal comorbidities, and pregnancy stage would influence the course of COVID-19 in pregnancy and how this, in turn, would affect delivery complications.
Finally, one crucial issue which remained unresolved is the psychosocial effects of the COVID-19 outbreak on mental health during pregnancy. Pregnant women frequently report psychosocial stress, depression, and panic disorder. In particular, there is a direct correlation between the level of antenatal psychosocial stress and the risk of poor pregnancy outcomes in the manner that the higher the antenatal psychosocial stress, the greater the risk of poor pregnancy outcomes. Therefore, pregnancy might be complicated during the COVID-19 outbreak, even if women do not get infected by the virus.
In this study, from 386 parturient women with COVID-19, 257 out of 299 patients gave birth by cesarean section, which means the cesarean section rate among these patients was about to 86%, which is very high. In a national cohort study reported by Knight et al., the cesarean rate in pregnant women with COVID-19 in the United Kingdom was about 59% [78]. In Germany, the CRONOS register website established to gather comprehensive data on mothers with COVID-19 who give birth around this country reports cesarean rate as about 37.5% by the last of January 2021 [79]. These national reports come from two highly developed countries equipped with the best available strategies to control the COVID-19 and related stress. It may positively impact pregnant women’s psychological status when choosing delivery method. Another possible reason for the difference in results is the method of data gathering. This study is a systematic review including studies pertinent to different countries. At the time of systematic search by the last of April 2020, many studies reporting pregnant women with COVID-19 were case reports, case series, or studies with a low sample size. Still, the two mentioned studied were at a grander scale, which may effectuate the result. On the other hand, in our study, there is no patient from England or Germany, and most of the patients are from China. Although the CRONOS register is a large-scale registry, it lacks clinically important details, such as signs, symptoms, and history, about every individual registered in this program.
Since December 2019, COVID-19 has been a resident of the world. Early efforts ranged from the development of diagnostic assays [80–83] and specific therapeutics [84–102] to optimizing health monitoring [103, 104]. Despite this effort, in addition to our knowledge and experience from the recent outbreaks [105], it mainly relied on non-pharmacological interventions to control the pandemic, e.g., quarantine and social isolation [106, 107]. Such a condition triggers stress [108]. The stress was, in particular, of high level at the time when the outbreak was initiated. Growing knowledge about different aspects of the disease, namely about the origin and pathogenesis of disease varying dependent on the immunogenetic background and the presence of comorbidities [4, 109–120], could protect against the stress and related damage, which is potentially critical in pregnant women and their neonates. Our review included studies conducted in the first six months of the pandemic when there was a high degree of stress and fear. This explains why the cesarean rate we calculated is relatively high, and also one can simply predict its reduction over time.
A major limitation is the lack of data in developing countries. Perinatal care is a crucial issue in less developed countries, while pregnant women in these countries may not have feasible access to health care facilities. Besides, insufficient perinatal care leads to a high rate of perinatal adverse events [122] while worsening during the pandemic. It is, therefore, important to gather enough data on pregnant women and their neonates in these countries. However, when this study was carried out, the data on less developed countries were too scarce, which may be because of lack of diagnostic facilities in these countries, insufficient referring, or reporting system. So further investigations are necessary to discover the impact of COVID-19 on perinatal events in developing countries.
Conclusion
The present systematic review suggests that clinical features and prognosis of pregnant women with COVID-19 may not be worse than the general population as well as some previous studies [121]. Still, this result should not lead to pregnant women ignore their suspect signs and symptoms to present themselves to medical care centers. It is crucial to provide optimum health care for pregnant women during the COVID-19 pandemic and follow their health status, especially respiratory signs and symptoms. The current evidence suggests that clinical features, diagnosis, and prognosis of COVID-19 in pregnant women are not different from those of the disease reported in society. Despite the high rate of contagion of COVID-19, vertical transmission of the novel coronavirus may remain a missing piece of the puzzle due to a lack of sufficient evidence. International collaboration remains a fundamental component of any future attempt to solve the puzzle [123–127].
Author contributions
MM: Conceptualized the study, conducted database search, search results screening, detailed review, and prepared the initial draft. AS: Prepared the final draft. NR: Supervised the project and critically appraised the manuscript. All authors have read and approved the manuscript.
Declarations
Conflict of interest
The authors declare that they have co conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hanaei S, Rezaei N. COVID-19: developing from an outbreak to a pandemic. Arch Med Res. 2020;51(6):582–584. doi: 10.1016/j.arcmed.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20(7):773. doi: 10.1016/S1473-3099(20)30195-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hessami A, Shamshirian A, Heydari K, Pourali F, Alizadeh-Navaei R, Moosazadeh M, Abrotan S, Shojaie L, Sedighi S, Shamshirian D, Rezaei N. Cardiovascular diseases burden in COVID-19: systematic review and meta-analysis. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jabalameli N, Rajabi F, Firooz A, Rezaei N. The overlap between genetic susceptibility to COVID-19 and skin diseases. Immunol Invest. 2021 doi: 10.1080/08820139.2021.1876086. [DOI] [PubMed] [Google Scholar]
- 5.Jahanshahlu L, Rezaei N. Central nervous system involvement in COVID-19. Arch Med Res. 2020;51(7):721–722. doi: 10.1016/j.arcmed.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nejadghaderi SA, Heidari A, Shakerian N, Saghazadeh A, Rezaei N. Cardiovascular system is at higher risk of affecting by COVID-19. Acta Biomed. 2020;91(3):e2020018. doi: 10.23750/abm.v91i3.9718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saleki K, Banazadeh M, Saghazadeh A, Rezaei N. The involvement of the central nervous system in patients with COVID-19. Rev Neurosci. 2020;31(4):453–456. doi: 10.1515/revneuro-2020-0026. [DOI] [PubMed] [Google Scholar]
- 8.Vakhshoori M, Heidarpour M, Shafie D, Taheri M, Rezaei N, Sarrafzadegan N. Acute cardiac injury in COVID-19: a systematic review and meta-analysis. Arch Iran Med. 2020;23(11):801–812. doi: 10.34172/aim.2020.107. [DOI] [PubMed] [Google Scholar]
- 9.Yazdanpanah N, Saghazadeh A, Rezaei N. Anosmia: a missing link in the neuroimmunology of coronavirus disease 2019 (COVID-19) Rev Neurosci. 2020;31(7):691–701. doi: 10.1515/revneuro-2020-0039. [DOI] [PubMed] [Google Scholar]
- 10.Heidarpour M, Vakhshoori M, Abbasi S, Shafie D, Rezaei N. Adrenal insufficiency in coronavirus disease 2019: a case report. J Med Case Rep. 2020;14(1):134. doi: 10.1186/s13256-020-02461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goudarzi S, Dehghani Firouzabadi F, Dehghani Firouzabadi M, Rezaei N. Cutaneous lesions and COVID-19: cystic painful lesion in a case with positive SARS-CoV-2. Dermatol Ther. 2020;33(6):e14266. doi: 10.1111/dth.14266. [DOI] [PubMed] [Google Scholar]
- 12.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aleebrahim-Dehkordi E, Soveyzi F, Deravi N, Rabbani Z, Saghazadeh A, Rezaei N. Human Coronaviruses SARS-CoV, MERS-CoV, and SARS-CoV-2 in children. J Pediatr Nurs. 2021;56:70–79. doi: 10.1016/j.pedn.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lotfi M, Rezaei N. SARS-CoV-2: a comprehensive review from pathogenicity of the virus to clinical consequences. J Med Virol. 2020;92(10):1864–1874. doi: 10.1002/jmv.26123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rokni M, Hamblin MR, Rezaei N. Cytokines and COVID-19: friends or foes? Hum Vaccin Immunother. 2020;16(10):2363–2365. doi: 10.1080/21645515.2020.1799669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: friend or foe? Life Sci. 2020;256:117900. doi: 10.1016/j.lfs.2020.117900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahanchian H, Moazzen N, Joghatayi SH, Saeidinia A, Khoshkhui M, Aelami MH, Rezaei N, Haghi NSM. Death due to COVID-19 in an infant with combined immunodeficiencies. Endocr Metab Immune Disord Drug Targets. 2020 doi: 10.2174/1871530320666201021142313. [DOI] [PubMed] [Google Scholar]
- 19.Babaha F, Rezaei N. Primary immunodeficiency diseases in COVID-19 pandemic: a predisposing or protective factor? Am J Med Sci. 2020;360(6):740–741. doi: 10.1016/j.amjms.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bahrami A, Vafapour M, Moazzami B, Rezaei N. Hyperinflammatory shock related to COVID-19 in a patient presenting with multisystem inflammatory syndrome in children: first case from Iran. J Paediatr Child Health. 2020 doi: 10.1111/jpc.15048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delavari S, Abolhassani H, Abolnezhadian F, Babaha F, Iranparast S, Ahanchian H, Moazzen N, Nabavi M, Arshi S, Fallahpour M, Bemanian MH, Shokri S, Momen T, Sadeghi-Shabestari M, Molatefi R, Shirkani A, Vosughimotlagh A, Safarirad M, Sharifzadeh M, Pashangzadeh S, Salami F, Shirmast P, Rezaei A, Moeini Shad T, Mohraz M, Rezaei N, Hammarström L, Yazdani R, Aghamohamamdi A. Impact of SARS-CoV-2 pandemic on patients with primary immunodeficiency. J Clin Immunol. 2021;41(2):345–355. doi: 10.1007/s10875-020-00928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khosroshahi LM, Rezaei N. Dysregulation of the immune response in COVID-19. Cell Biol Int. 2020 doi: 10.1002/cbin.11517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saghazadeh A, Rezaei N. Immune-epidemiological parameters of the novel coronavirus - a perspective. Expert Rev Clin Immunol. 2020;16(5):465–470. doi: 10.1080/1744666x.2020.1750954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torabi-Rahvar M, Rezaei N. Storm at the time of Corona: a glimpse at the current understanding and therapeutic opportunities of the SARS-CoV-2 cytokine storm. Curr Pharm Des. 2020 doi: 10.2174/1381612826666201125102649. [DOI] [PubMed] [Google Scholar]
- 25.Mojtabavi H, Saghazadeh A, Rezaei N. Interleukin-6 and severe COVID-19: a systematic review and meta-analysis. Eur Cytokine Netw. 2020;31(2):44–49. doi: 10.1684/ecn.2020.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarzaeim M, Rezaei N. Kawasaki disease and multisystem inflammatory syndrome in children with COVID-19. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00558-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nasab MG, Saghazadeh A, Rezaei N. SARS-CoV-2-A tough opponent for the immune system. Arch Med Res. 2020;51(6):589–592. doi: 10.1016/j.arcmed.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang H, Wang C, Poon LC. Novel coronavirus infection and pregnancy. Ultrasound Obstet Gynecol. 2020;55(4):435–437. doi: 10.1002/uog.22006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rezaei N. COVID-19 affects healthy pediatricians more than pediatric patients. Infect Control Hosp Epidemiol. 2020;41(9):1106–1107. doi: 10.1017/ice.2020.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Favre G, Pomar L, Musso D, Baud D. 2019-nCoV epidemic: what about pregnancies? Lancet. 2020;395(10224):e40. doi: 10.1016/S0140-6736(20)30311-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashokka B, Loh M-H, Tan CH, Su LL, Young BE, Lye DC, Biswas A, Illanes E, S, Choolani M, Care of the pregnant woman with COVID-19 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am J Obstet Gynecol. 2020;223(1):66. doi: 10.1016/j.ajog.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dashraath P, Jing Lin Jeslyn W, Mei Xian Karen L, Li Min L, Sarah L, Biswas A, Arjandas Choolani M, Mattar C, Lin SL. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;41:7. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayor S. Covid-19: Nine in 10 pregnant women with infection when admitted for delivery are asymptomatic, small study finds. BMJ. 2020;369:m1485. doi: 10.1136/bmj.m1485. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) Coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020 doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Omer S, Ali S, Babar ZUD. Preventive measures and management of COVID-19 in pregnancy. Drugs Ther Perspect. 2020 doi: 10.1007/s40267-020-00725-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu X, Sun R, Chen J, Xie Y, Zhang S, Wang X. Radiological findings and clinical characteristics of pregnant women with COVID-19 pneumonia. Int J Gynaecol Obstet. 2020 doi: 10.1002/ijgo.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wen R, Sun P, Xing Q-S. A patient with SARS-CoV-2 infection during pregnancy in Qingdao, China. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vlachodimitropoulou Koumoutsea E, Vivanti AJ, Shehata N, Benachi A, Le Gouez A, Desconclois C, Whittle W, Snelgrove J, Malinowski KA. COVID19 and acute coagulopathy in pregnancy. J Thromb Haemost. 2020 doi: 10.1111/jth.14856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeng LK, Tao XW, Yuan WH, Wang J, Liu X, Liu ZS. First case of neonate infected with novel coronavirus pneumonia in China. Zhonghua Er Ke Za Zhi. 2020;58:E009. doi: 10.3760/cma.j.issn.0578-1310.2020.0009. [DOI] [PubMed] [Google Scholar]
- 40.Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 41.Lei D, Wang C, Li C, Fang C, Yang W, Chen B, Wei M, Xu X, Yang H, Wang S, Fan C. Clinical characteristics of COVID-19 in pregnancy: analysis of nine cases. Chin J Perinat Med. 2020;23(3):159–165. [Google Scholar]
- 42.Breslin N, Baptiste C, Miller R, Fuchs K, Goffman D, Gyamfi-Bannerman C, D’Alton M. COVID-19 in pregnancy: early lessons. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajogmf.2020.100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, Long X. Antibodies in infants born to mothers With COVID-19 Pneumonia. JAMA. 2020 doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang L, Jiang Y, Wei M, Cheng BH, Zhou XC, Li J, Tian JH, Dong L, Hu RH. Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province. Zhonghua Fu Chan Ke Za Zhi. 2020;55:E009. doi: 10.3760/cma.j.cn112141-20200218-00111. [DOI] [PubMed] [Google Scholar]
- 45.Song L, Xiao W, Ling K, Yao S, Chen X (2020) Anesthetic management for emergent cesarean delivery in a parturient with recent diagnosis of Coronavirus Disease 2019 (COVID-19): a case report. Transl Perioper Pain Med. 10.31480/2330-4871/118
- 46.Khan S, Jun L, Nawsherwan SR, Li Y, Han G, Xue M, Nabi G, Liu J. Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women. Clin Microbiol Infect. 2020 doi: 10.1016/j.cmi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li Y, Zhao R, Zheng S, Chen X, Wang J, Sheng X, Zhou J, Cai H, Fang Q, Yu F, Fan J, Xu K, Chen Y, Sheng J. Lack of vertical transmission of severe acute respiratory syndrome Coronavirus 2, China. Emerg Infect Dis. 2020 doi: 10.3201/eid2606.200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liao X, Yang H, Kong J, Yang H. Chest CT findings in a pregnant patient with 2019 Novel Coronavirus. Balkan Med J. 2020;37(4):226–228. doi: 10.4274/balkanmedj.galenos.2020.2020.3.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9(1):51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen S, Liao E, Shao Y. Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia. J Med Virol. 2020 doi: 10.1002/jmv.25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/s0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen L, Li Q, Zheng D, Jiang H, Wei Y, Zou L, Feng L, Xiong G, Sun G, Wang H, Zhao Y, Qiao J. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020 doi: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang P, Wang X, Liu P, Wei C, He B, Zheng J, Zhao D. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J Clin Virol. 2020;127:104356. doi: 10.1016/j.jcv.2020.104356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu W, Wang J, Li W, Zhou Z, Liu S, Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front Med. 2020 doi: 10.1007/s11684-020-0772-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, Liu Y, Xiao J, Liu H, Deng D, Chen S, Zeng W, Feng L, Wu J. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. 2020;20(5):559–564. doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sun G, Tang F, Peng M, Gao Y, Peng J, Xie H, Zhao Y, Jin Z. Clinical Features and outcomes of pregnant women suspected of Coronavirus Disease 2019. J Infect. 2020;88(1):e40–e44. doi: 10.1016/j.jinf.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect. 2020 doi: 10.1016/j.jinf.2020.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu W, Wang Q, Zhang Q, Chen L, Chen J, Zhang B, Lu Y, Wang S, Xia L, Huang L, Wang K, Liang L, Zhang Y, Turtle L, Lissauer D, Lan K, Feng L, Yu H, Liu Y, Sun Z (2020) Coronavirus disease 2019 (COVID-19) during pregnancy: a case series. https://www.preprints.org/manuscript/202002.0373/v1
- 60.Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, Ring L, Landau R, Purisch S, Friedman AM, Fuchs K, Sutton D, Andrikopoulou M, Rupley D, Sheen JJ, Aubey J, Zork N, Moroz L, Mourad M, Wapner R, Simpson LL, D'Alton ME, Goffman D. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khan S, Peng L, Siddique R, Nabi G, Nawsherwan u, Xue M, Liu J, Han G, Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infect Control Hospital Epidemiol. 2020 doi: 10.1017/ice.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen D, Xu W, Lei Z, Huang Z, Liu J, Gao Z, Peng L. Recurrence of positive SARS-CoV-2 RNA in COVID-19: a case report. Int J Infect Dis. 2020;93:297–299. doi: 10.1016/j.ijid.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kalafat E, Yaprak E, Cinar G, Varli B, Ozisik S, Uzun C, Azap A, Koc A. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound in Obstetrics Gynecology. 2020;55(6):835–837. doi: 10.1002/uog.22034. [DOI] [PubMed] [Google Scholar]
- 64.Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, Yue L, Li Q, Sun G, Chen L, Yang L. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Karami P, Naghavi M, Feyzi A, Aghamohammadi M, Novin MS, Mobaien A, Qorbanisani M, Karami A, Norooznezhad AH. Mortality of a pregnant patient diagnosed with COVID-19: a case report with clinical, radiological, and histopathological findings. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, Zhou W. Neonatal early-onset infection With SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang ZJ, Yu XJ, Fu T, Liu Y, Jiang Y, Yang BX, Bi Y. Novel Coronavirus infection in newborn babies under 28 days in China. Eur Respir J. 2020 doi: 10.1183/13993003.00697-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, Bao Y, Sun Y, Huang J, Guo Y, Yu Y, Wang S. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dong L, Tian J, He S, Zhu C, Wang J, Liu C, Yang J. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020 doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, Zheng C. Pregnancy and Perinatal outcomes of women with Coronavirus Disease (COVID-19) Pneumonia: a preliminary analysis. Am J Roentgenol. 2020 doi: 10.2214/AJR.20.23072. [DOI] [PubMed] [Google Scholar]
- 71.Zambrano LI, Fuentes-Barahona IC, Bejarano-Torres DA, Bustillo C, Gonzales G, Vallecillo-Chinchilla G, Sanchez-Martinez FE, Valle-Reconco JA, Sierra M, Bonilla-Aldana DK, Cardona-Ospina JA, Rodriguez-Morales AJ. A pregnant woman with COVID-19 in Central America. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen S, Huang B, Luo DJ, Li X, Yang F, Zhao Y, Nie X, Huang BX. Pregnant women with new coronavirus infection: a clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi. 2020;49:E005. doi: 10.3760/cma.j.cn112151-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 73.Zamaniyan M, Ebadi A, Aghajanpoor Mir S, Rahmani Z, Haghshenas M, Azizi S. Preterm delivery in pregnant woman with critical COVID-19 pneumonia and vertical transmission. Prenat Diagn. 2020 doi: 10.1002/pd.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020 doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peng Z, Wang J, Mo Y, Duan W, Xiang G, Yi M, Bao L, Shi Y. Unlikely SARS-CoV-2 vertical transmission from mother to child: A case report. J Infect Public Health. 2020 doi: 10.1016/j.jiph.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xiong X, Wei H, Zhang Z, Chang J, Ma X, Gao X, Chen Q, Pang Q. Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.25857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.(WHO) WHO (2020) WHO COVID-19 Dashboard. https://covid19.who.int. Accessed 21 Apr 2020
- 78.Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, O'Brien P, Quigley M, Brocklehurst P, Kurinczuk JJ. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.CRONOS Register. https://www.dgpm-online.org/index.php?id=60
- 80.Basiri A, Heidari A, Nadi MF, Fallahy MTP, Nezamabadi SS, Sedighi M, Saghazadeh A, Rezaei N. Microfluidic devices for detection of RNA viruses. Rev Med Virol. 2021;31(1):1–11. doi: 10.1002/rmv.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rabiee N, Rabiee M, Bagherzadeh M, Rezaei N. COVID-19 and picotechnology: Potential opportunities. Med Hypotheses. 2020;144:109917. doi: 10.1016/j.mehy.2020.109917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tantuoyir MM, Rezaei N. Serological tests for COVID-19: potential opportunities. Cell Biol Int. 2020 doi: 10.1002/cbin.11516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jabbari P, Rezaei N. With risk of reinfection, is COVID-19 here to stay? Disaster Med Public Health Prep. 2020;14(4):e33. doi: 10.1017/dmp.2020.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Basiri A, Pazhouhnia Z, Beheshtizadeh N, Hoseinpour M, Saghazadeh A, Rezaei N. Regenerative medicine in COVID-19 treatment: real opportunities and range of promises. Stem Cell Rev Rep. 2020 doi: 10.1007/s12015-020-09994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jahanshahlu L, Rezaei N. Monoclonal antibody as a potential anti-COVID-19. Biomed Pharmacother. 2020;129:110337. doi: 10.1016/j.biopha.2020.110337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lotfi M, Rezaei N. CRISPR/Cas13: a potential therapeutic option of COVID-19. Biomed Pharmacother. 2020;131:110738. doi: 10.1016/j.biopha.2020.110738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mansourabadi AH, Sadeghalvad M, Mohammadi-Motlagh HR, Rezaei N. The immune system as a target for therapy of SARS-CoV-2: a systematic review of the current immunotherapies for COVID-19. Life Sci. 2020;258:118185. doi: 10.1016/j.lfs.2020.118185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mohamed K, Yazdanpanah N, Saghazadeh A, Rezaei N. Computational drug discovery and repurposing for the treatment of COVID-19: a systematic review. Bioorg Chem. 2021;106:104490. doi: 10.1016/j.bioorg.2020.104490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Moradian N, Gouravani M, Salehi MA, Heidari A, Shafeghat M, Hamblin MR, Rezaei N. Cytokine release syndrome: inhibition of pro-inflammatory cytokines as a solution for reducing COVID-19 mortality. Eur Cytokine Netw. 2020;31(3):81–93. doi: 10.1684/ecn.2020.0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Palit P, Chattopadhyay D, Thomas S, Kundu A, Kim HS, Rezaei N. Phytopharmaceuticals mediated Furin and TMPRSS2 receptor blocking: can it be a potential therapeutic option for Covid-19? Phytomedicine. 2020 doi: 10.1016/j.phymed.2020.153396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Peymani P, Dehesh T, Aligolighasemabadi F, Sadeghdoust M, Kotfis K, Ahmadi M, Mehrbod P, Iranpour P, Dastghaib S, Nasimian A, Ravandi A, Kidane B, Ahmed N, Sharma P, Shojaei S, Bagheri Lankarani K, Madej A, Rezaei N, Madrakian T, Los MJ, Labouta HI, Mokarram P, Ghavami S. Statins in patients with COVID-19: a retrospective cohort study in Iranian COVID-19 patients. Transl Med Commun. 2021;6(1):3. doi: 10.1186/s41231-021-00082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pourahmad R, Moazzami B, Rezaei N. Efficacy of plasmapheresis and immunoglobulin replacement therapy (IVIG) on patients with COVID-19. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Saghazadeh A, Rezaei N. Towards treatment planning of COVID-19: rationale and hypothesis for the use of multiple immunosuppressive agents: anti-antibodies, immunoglobulins, and corticosteroids. Int Immunopharmacol. 2020;84:106560. doi: 10.1016/j.intimp.2020.106560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Seyedpour S, Khodaei B, Loghman AH, Seyedpour N, Kisomi MF, Balibegloo M, Nezamabadi SS, Gholami B, Saghazadeh A, Rezaei N. Targeted therapy strategies against SARS-CoV-2 cell entry mechanisms: a systematic review of in vitro and in vivo studies. J Cell Physiol. 2020 doi: 10.1002/jcp.30032. [DOI] [PubMed] [Google Scholar]
- 95.Shojaeefar E, Malih N, Rezaei N. The possible double-edged sword effects of vitamin D on COVID-19: a hypothesis. Cell Biol Int. 2021;45(1):54–57. doi: 10.1002/cbin.11469. [DOI] [PubMed] [Google Scholar]
- 96.Zarandi PK, Zinatizadeh MR, Zinatizadeh M, Yousefi MH, Rezaei N. SARS-CoV-2: from the pathogenesis to potential anti-viral treatments. Biomed Pharmacother. 2021;137:111352. doi: 10.1016/j.biopha.2021.111352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fathi N, Rezaei N. Lymphopenia in COVID-19: therapeutic opportunities. Cell Biol Int. 2020;44(9):1792–1797. doi: 10.1002/cbin.11403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pezeshki PS, Rezaei N. Immune checkpoint inhibition in COVID-19: risks and benefits. Expert Opin Biol Ther. 2021 doi: 10.1080/14712598.2021.1887131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rezaei N. COVID-19 and medical biotechnology. Avicenna J Med Biotechnol. 2020;12(3):139. [PMC free article] [PubMed] [Google Scholar]
- 100.Sharifkashani S, Bafrani MA, Khaboushan AS, Pirzadeh M, Kheirandish A, Yavarpour Bali H, Hessami A, Saghazadeh A, Rezaei N. Angiotensin-converting enzyme 2 (ACE2) receptor and SARS-CoV-2: potential therapeutic targeting. Eur J Pharmacol. 2020;884:173455. doi: 10.1016/j.ejphar.2020.173455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Torabi S, Bahreini F, Rezaei N. The role of angiotensin-converting enzyme 2 in COVID-19 induced lung injury. Acta Biomed. 2020;91(4):e2020142. doi: 10.23750/abm.v91i4.10159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pashaei M, Rezaei N. Immunotherapy for SARS-CoV-2: potential opportunities. Expert Opin Biol Ther. 2020;20(10):1111–1116. doi: 10.1080/14712598.2020.1807933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020;126:104345. doi: 10.1016/j.jcv.2020.104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jabbari P, Taraghikhah N, Jabbari F, Ebrahimi S, Rezaei N. Adherence of the general public to self-protection guidelines during the COVID-19 pandemic. Disaster Med Public Health Prep. 2020 doi: 10.1017/dmp.2020.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jabbari P, Jabbari F, Ebrahimi S, Rezaei N. COVID-19: a chimera of two pandemics. Disaster Med Public Health Prep. 2020;14(3):e38–e39. doi: 10.1017/dmp.2020.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Samieefar N, Yari Boroujeni R, Jamee M, Lotfi M, Golabchi MR, Afshar A, Miri H, Khazeei Tabari MA, Darzi P, Abdullatif Khafaie M, Amirheidari B, Tamadon A, Rambod Rad N, Samimi N, Farjam M, Shiravi F, Farshidi N, Hedayati ChM, Doostkamel D, Alikhani R, Razmkhah M, Abdollahifard S, Nasiri Kalmarzi R, Kelishadi R, Khazaei H, Aghamohammadi A, Jafari Mousavi FS, Shamsizadeh M, Khojasteh A, Rezaei N. Country quarantine during COVID-19: critical or not? Disaster Med Public Health Prep. 2020 doi: 10.1017/dmp.2020.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hanaei S, Takian A, Majdzadeh R, Maboloc CR, Grossmann I, Gomes O, Milosevic M, Gupta M, Shamshirsaz AA, Harbi A, Burhan AM, Uddin LQ, Kulasinghe A, Lam CM, Ramakrishna S, Alavi A, Nouwen JL, Dorigo T, Schreiber M, Abraham A, Shelkovaya N, Krysztofiak W, Ebrahimi Warkiani M, Sellke F, Ogino S, Barba FJ, Brand S, Vasconcelos C, Salunke DB, Rezaei N. Emerging Standards and the hybrid model for organizing scientific events during and after the COVID-19 pandemic. Disaster Med Public Health Prep. 2020 doi: 10.1017/dmp.2020.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Salehi M, Amanat M, Mohammadi M, Salmanian M, Rezaei N, Saghazadeh A, Garakani A. The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: a systematic-review and meta-analysis. J Affect Disord. 2021;282:527–538. doi: 10.1016/j.jad.2020.12.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Darbeheshti F, Rezaei N. Genetic predisposition models to COVID-19 infection. Med Hypotheses. 2020;142:109818. doi: 10.1016/j.mehy.2020.109818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hassan SS, Ghosh S, Attrish D, Choudhury PP, Aljabali AAA, Uhal BD, Lundstrom K, Rezaei N, Uversky VN, Seyran M, Pizzol D, Adadi P, Soares A, El-Aziz TMA, Kandimalla R, Tambuwala MM, Azad GK, Sherchan SP, Baetas-da-Cruz W, Takayama K, Serrano-Aroca Á, Chauhan G, Palu G, Brufsky AM. Possible transmission flow of SARS-CoV-2 based on ACE2 features. Molecules. 2020 doi: 10.3390/molecules25245906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lundstrom K, Seyran M, Pizzol D, Adadi P, Mohamed Abd El-Aziz T, Hassan SS, Soares A, Kandimalla R, Tambuwala MM, Aljabali AAA, Kumar Azad G, Pal Choudhury P, Uversky VN, Sherchan SP, Uhal BD, Rezaei N, Brufsky AM. Viewpoint: origin of SARS-CoV-2. Viruses. 2020 doi: 10.3390/v12111203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Seyran M, Pizzol D, Adadi P, El-Aziz TMA, Hassan SS, Soares A, Kandimalla R, Lundstrom K, Tambuwala M, Aljabali AAA, Lal A, Azad GK, Choudhury PP, Uversky VN, Sherchan SP, Uhal BD, Rezaei N, Brufsky AM. Questions concerning the proximal origin of SARS-CoV-2. J Med Virol. 2020 doi: 10.1002/jmv.26478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yousefzadegan S, Rezaei N. Case report: death due to COVID-19 in three brothers. Am J Trop Med Hyg. 2020;102(6):1203–1204. doi: 10.4269/ajtmh.20-0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Khanmohammadi S, Rezaei N. Role of Toll-like receptors in the pathogenesis of COVID-19. J Med Virol. 2021 doi: 10.1002/jmv.26826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Razavi A, Hamblin MR, Rezaei N. COVID-19 in patients with cancer: risks and precautions. Am J Emerg Med. 2021 doi: 10.1016/j.ajem.2021.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Safdarian AR, Momenzadeh K, Kahe F, Farhangnia P, Rezaei N. Death due to COVID-19 in a patient with diabetes, epilepsy, and gout comorbidities. Clin Case Rep. 2020;9(1):461–464. doi: 10.1002/ccr3.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sadeghmousavi S, Rezaei N. COVID-19 and multiple sclerosis: predisposition and precautions in treatment. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Seyran M, Takayama K, Uversky VN, Lundstrom K, Palù G, Sherchan SP, Attrish D, Rezaei N, Aljabali AAA, Ghosh S, Pizzol D, Chauhan G, Adadi P, Mohamed Abd El-Aziz T, Soares AG, Kandimalla R, Tambuwala M, Hassan SS, Azad GK, Pal Choudhury P, Baetas-da-Cruz W, Serrano-Aroca Á, Brufsky AM, Uhal BD. The structural basis of accelerated host cell entry by SARS-CoV-2†. FEBS J. 2020 doi: 10.1111/febs.15651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jenab Y, Rezaei N, Hedayat B, Naderian M, Shirani S, Hosseini K. Occurrence of acute coronary syndrome, pulmonary thromboembolism, and cerebrovascular event in COVID-19. Clin Case Rep. 2020;8(12):2414–2417. doi: 10.1002/ccr3.3112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sahu KK, Siddiqui AD, Rezaei N, Cerny J. Challenges for management of immune thrombocytopenia during COVID-19 pandemic. J Med Virol. 2020;92(11):2277–2282. doi: 10.1002/jmv.26251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Figueiro-Filho EA, Yudin M, Farine D. COVID-19 during pregnancy: an overview of maternal characteristics, clinical symptoms, maternal and neonatal outcomes of 10,996 cases described in 15 countries. J Perinat Med. 2020;48(9):900–911. doi: 10.1515/jpm-2020-0364. [DOI] [PubMed] [Google Scholar]
- 122.Zupan J. Perinatal mortality in developing countries. N Engl J Med. 2005;352(20):2047–2048. doi: 10.1056/NEJMp058032. [DOI] [PubMed] [Google Scholar]
- 123.Mohamed K, Rezaei N, Rodríguez-Román E, Rahmani F, Zhang H, Ivanovska M, Makka SA, Joya M, Makuku R, Md Shahidul I, Nesrine R, Laila R, Goda R, Sunny OA, Mujtaba S, Zoghi S, Irtsyan S, Ling I, Orsolya C, Attig-Bahar F, Hazar Sayar E, Soloukey C, Giulia G. International efforts to save healthcare personnel during COVID-19. Acta Biomed. 2020;91(3):e2020044. doi: 10.23750/abm.v91i3.9891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mohamed K, Rodríguez-Román E, Rahmani F, Zhang H, Ivanovska M, Makka SA, Joya M, Makuku R, Islam MS, Radwan N, Rahmah L, Goda R, Abarikwu SO, Shaw M, Zoghi S, Irtsyan S, Ling I, Cseprekal O, Faten AB, Hazar Sayar E, Soloukey C, Grancini G, Rezaei N. Borderless collaboration is needed for COVID-19-A disease that knows no borders. Infect Control Hosp Epidemiol. 2020;41(10):1245–1246. doi: 10.1017/ice.2020.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Momtazmanesh S, Ochs HD, Uddin LQ, Perc M, Routes JM, Vieira DN, Al-Herz W, Baris S, Prando C, Rosivall L, Abdul Latiff AH, Ulrichs T, Roudenok V, Aldave Becerra JC, Salunke DB, Goudouris E, Condino-Neto A, Stashchak A, Kryvenko O, Stashchak M, Bondarenko A, Rezaei N. All together to Fight COVID-19. Am J Trop Med Hyg. 2020;102(6):1181–1183. doi: 10.4269/ajtmh.20-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Moradian N, Ochs HD, Sedikies C, Hamblin MR, Camargo CA, Jr, Martinez JA, Biamonte JD, Abdollahi M, Torres PJ, Nieto JJ, Ogino S, Seymour JF, Abraham A, Cauda V, Gupta S, Ramakrishna S, Sellke FW, Sorooshian A, Wallace Hayes A, Martinez-Urbistondo M, Gupta M, Azadbakht L, Esmaillzadeh A, Kelishadi R, Esteghamati A, Emam-Djomeh Z, Majdzadeh R, Palit P, Badali H, Rao I, Saboury AA, Jagan Mohan Rao L, Ahmadieh H, Montazeri A, Fadini GP, Pauly D, Thomas S, Moosavi-Movahed AA, Aghamohammadi A, Behmanesh M, Rahimi-Movaghar V, Ghavami S, Mehran R, Uddin LQ, Von Herrath M, Mobasher B, Rezaei N. The urgent need for integrated science to fight COVID-19 pandemic and beyond. J Transl Med. 2020;18(1):205. doi: 10.1186/s12967-020-02364-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mohamed K, Rezaei N. COVID-19 pandemic is not the time of trial and error. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]