Abstract
Rationale: Health outcomes of people with coronavirus disease (COVID-19) range from no symptoms to severe illness and death. Asthma, a common chronic lung disease, has been considered likely to increase the severity of COVID-19, although data addressing this hypothesis have been scarce until very recently.
Objectives: To review the epidemiologic literature related to asthma’s potential role in COVID-19 severity.
Methods: Studies were identified through the PubMed (MEDLINE) and medRxiv (preprint) databases using the search terms “asthma,” “SARS-CoV-2” (severe acute respiratory syndrome coronavirus 2), and “COVID-19,” and by cross-referencing citations in identified studies that were available in print or online before December 22, 2020.
Measurements and Main Results: Asthma prevalence data were obtained from studies of people with COVID-19 and regional health statistics. We identified 150 studies worldwide that allowed us to compare the prevalence of asthma in patients with COVID-19 by region, disease severity, and mortality. The results of our analyses do not provide clear evidence of increased risk of COVID-19 diagnosis, hospitalization, severity, or mortality due to asthma.
Conclusions: These findings could provide some reassurance to people with asthma regarding its potential to increase their risk of severe morbidity from COVID-19.
Keywords: asthma, SARS-CoV-2, COVID-19, disease severity, mortality
At a Glance Commentary
Scientific Knowledge on the Subject
People with asthma are considered to be more vulnerable to becoming severely ill with coronavirus disease (COVID-19). However, many aspects of COVID-19 pathophysiology are under investigation, and the relationship between asthma and COVID-19 severity is unclear.
What This Study Adds to the Field
We used prevalence data from 150 studies conducted worldwide to assess whether asthma increases the risk of morbidity and severity of COVID-19. The results of our analyses do not provide clear evidence of increased risk of COVID-19 diagnosis, hospitalization, severity, or mortality due to asthma.
Coronavirus disease (COVID-19) emerged in Wuhan City, Hubei Province, China, as a pneumonia of unknown origin, and it was declared an international public health emergency in February of 2020 (1). Shortly thereafter, in March of 2020, the World Health Organization (WHO) declared that the situation had escalated to pandemic status. As of January 1, 2021, there have been over 83 million confirmed cases of COVID-19 worldwide and over 1.8 million deaths attributed to the pandemic (2). Health outcomes of individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of COVID-19, range from the lack of any symptoms to severe illness and death (3).
In addition to advanced age, suspected risk factors for developing severe illness due to SARS-CoV-2 infection include the presence of comorbidities, such as cardiovascular disease, obesity, certain malignancies, and diabetes (3). Asthma is a highly prevalent chronic inflammatory disease of the airways that afflicts over 330 million people worldwide (4). Because SARS-CoV-2 is primarily a respiratory virus, people with asthma are apprehensive that they may be at increased risk of acquiring COVID-19 and suffer poorer outcomes. Among younger patients hospitalized with COVID-19 in the United States, obesity, asthma, and diabetes were the most common comorbidities (5). The CDC and WHO have each stated that people with asthma are more vulnerable to becoming severely ill with COVID-19 (6, 7). These statements are consistent with the chronic inflammation and airways dysfunction characterizing asthma, and the increased frequency and severity of respiratory infections in patients with asthma, such as is the case with influenza (8). In fact, the human rhinovirus, the most common cause of the common cold, is a potent trigger of asthma exacerbations (9). However, many aspects of COVID-19 pathophysiology remain unclear, and emerging data from epidemiologic studies have not consistently supported an increased risk of COVID-19 severity in people with asthma. Given these uncertainties, we used prevalence data from studies conducted worldwide to assess whether susceptibility to COVID-19 diagnosis, hospitalization, or severity are altered in people with asthma.
Methods
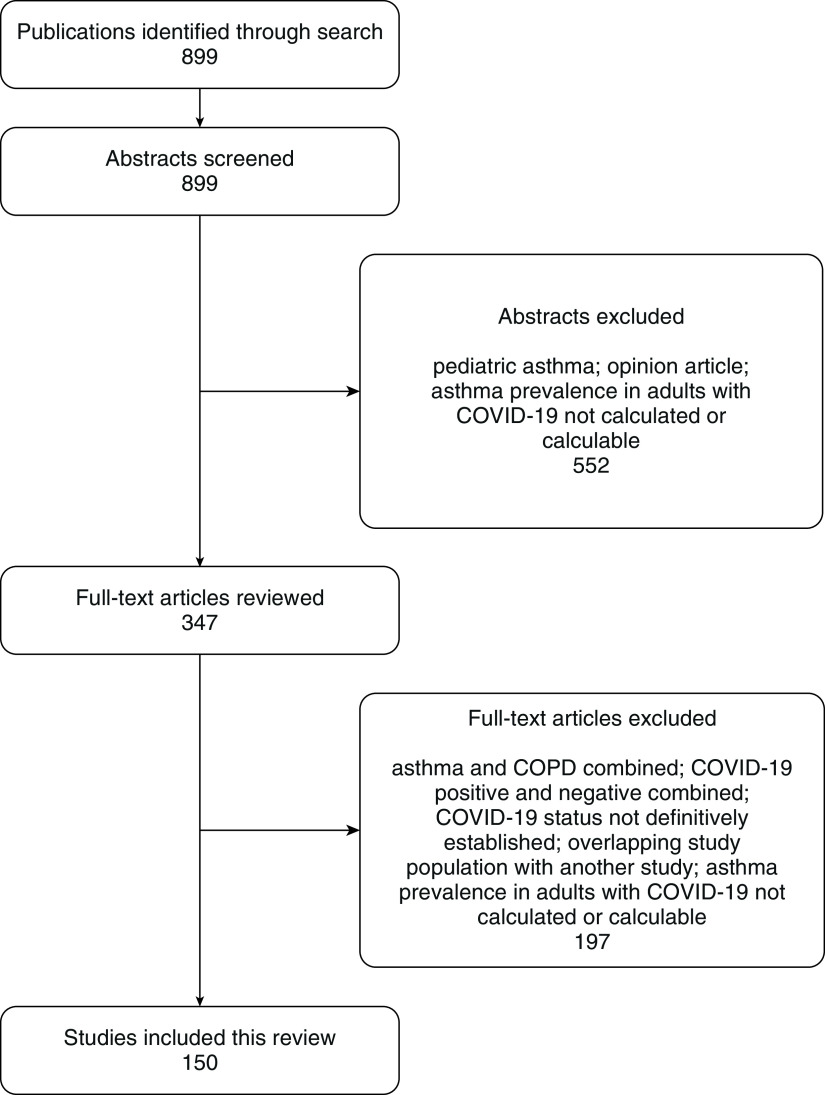
Studies included in this article were identified by searching the PubMed (MEDLINE) and medRxiv (preprint) databases, using the search terms “asthma,” “SARS-Cov-2,” and “COVID-19,” and by cross-referencing citations in identified studies that were available in print or online before December 22, 2020 (Figure 1). We did not consider studies that focused on pediatric cases, those that excluded patients without asthma, those that excluded symptomatic patients, those that examined asthma inseparably from chronic obstructive pulmonary disease (COPD), those that analyzed patients who were COVID-19 positive inseparably from individuals who were COVID-19 negative, or those with a study population that largely overlapped that of another published study. In this way, we identified 150 studies that examined the prevalence of asthma in approximately 1 million people with confirmed COVID-19 in more than 30 countries. Given the marked geographic variation in reported asthma prevalence, we performed analyses by region, and in some regions where a large number of studies were conducted (United States, New York City, Mexico, Europe, South Korea, and China), we sought estimates of asthma prevalence in general populations to interpret published data in their regional context.
Figure 1.
Literature acquisition flow diagram. COPD = chronic obstructive pulmonary disease; COVID-19 = coronavirus disease.
We calculated the overall prevalence of asthma in study populations, as well as the prevalence of asthma in people hospitalized and not hospitalized with COVID-19. Among hospitalized patients, we compared the prevalence of asthma according to categories of COVID-19 severity and mortality. The severity of COVID-19 was categorized in various ways in previous studies. When studies dichotomized hospitalized (still living) patients as having “severe” versus “not severe” COVID-19, we abstracted asthma prevalence data into those same categories in our analyses, even though the underlying criteria for such classification may have varied among those studies. Other studies dichotomized patients as requiring “ICU” versus “no ICU,” which was our primary measure of COVID-19 severity. Secondary measures of severity included requiring “invasive mechanical ventilation” versus “no invasive mechanical ventilation,” “critical” versus “not critical,” or having COVID-19 that “progressed” versus “stabilized.” We considered people in the first category to have “severe” COVID-19 and those in the second to have “not severe” disease.
Statistical Methods
A series of meta-analyses using the Freeman-Tukey transformation were performed to establish the pooled proportion of asthma in people with COVID-19 overall in the examined studies and according to hospitalization, COVID-19 severity, COVID-19 positivity, and mortality. The weighted final proportion was calculated for each meta-analysis. Cochran’s Q test was used to test for heterogeneity of effects across the reported results in the studies. Random-effects models were used for each meta-analysis. Forest plots were produced to provide a visual depiction of the meta-analysis findings.
A separate series of meta-analyses were conducted to produce the weighted pooled prevalence ratio (PR) of asthma for hospitalized versus nonhospitalized participants, those with severe COVID-19 versus nonsevere COVID-19, COVID-19–positive versus COVID-19–negative participants, and those who died versus survived, as defined above. The heterogeneity of the treatment effects in each model was accounted for using Mantel-Haenszel analyses to generate the pooled PR for the random-effects models. The meta-analyses associated with pooled prevalence and PR were performed using scistat.com (MedCalc Software).
Finally, a meta-analysis was performed to test for a pooled effect associated with adjusted odds ratios from studies in which confounding variables were taken into account when testing for associations between asthma and COVID-19 mortality. That analysis was performed using the “metan” function in Stata (StataCorp).
Results
Among the studies that were included in our analysis (Figure 1), we analyzed the prevalence of asthma in people with COVID-19 by geographic region, severity, and mortality.
Asthma Prevalence by Geographic Region
North American studies were conducted in the United States, Canada, and Mexico (see Table E1 in the online supplement). The pooled prevalence for asthma in 63 studies conducted in the United States (n = 351,728) (5, 10–71) was 11.0% (95% confidence interval [CI], 9.8–12.3%). In 19 studies conducted in the New York City region (n = 50,256) (10–28), the pooled prevalence for asthma was 8.7% (95 % CI, 7.3–10.2%). In five studies conducted in Mexico (n = 409,800) (72–76), the pooled prevalence was 2.9% (95 % CI, 2.8–3.1%). In 31 studies conducted in Europe (n = 203,978) (70, 77–106), the pooled prevalence was 7.6% (95 % CI, 6.0–9.4%). Asian studies were conducted primarily in China and South Korea. In 11 studies conducted in China (n = 4,050) (107–117), the pooled prevalence was 1.9% (95 % CI, 0.4–4.4%). In nine studies conducted in South Korea (n = 37,938) (70, 118–125), the pooled prevalence was 5.4% (95 % CI, 2.3–9.6%). Data regarding asthma prevalence in people with COVID-19 in Canada (126), Brazil (127–129), India (130, 131), Bangladesh (132, 133), the Philippines (134), Japan (135, 136), Africa (137–140), Iran (141, 142), Kuwait (143), Turkey (144–146), Israel (147–149), and Saudi Arabia (150) were relatively sparse, making them difficult to characterize by country, but they were generally within the range of the prevalences reported above.
Asthma Prevalence by Severity of COVID-19
Twenty-six studies provided data on the prevalence of asthma in people who were hospitalized with COVID-19 and those who were deemed well enough to be sent home with the disease (Tables 1 and E1 and E2 and Figure 2) (12, 20, 23, 27, 31, 32, 34, 35, 37, 39, 43, 50, 51, 53, 54, 56, 59, 73–75, 86, 89, 121, 147, 148, 151). The prevalence of asthma in these two groups was 10.0% (95% CI, 8.0–12.2%) and 9.5% (95% CI, 8.0–11.0%), respectively. The pooled PR for hospitalized individuals versus those not hospitalized was 1.06 (95% CI, 0.94–1.19; P = 0.37).
Table 1.
Summary of Asthma Prevalence Data by Measures of COVID-19 Severity
| Hospital Admission* |
COVID-19 Severity† |
COVID-19 Survival‡ |
||||
|---|---|---|---|---|---|---|
| Hospitalized | Not Hospitalized | Severe | Not Severe | Died | Survived | |
| Asthma prevalence, % | 10.0 (8.0–12.2) | 9.5 (8.0–11.0) | 9.9 (7.8–12.3) | 8.2 (7.0–10.0) | 7.1 (5.6–8.8) | 8.6 (7.0–10.3) |
| Pooled prevalence ratio | 1.06 (0.94–1.19); P = 0.37 | 1.18 (0.98–1.42); P = 0.07 | 0.89 (0.77–1.02); P = 0.09 | |||
Definition of abbreviation: COVID-19 = coronavirus disease.
Numbers in the parentheses are 95% confidence intervals.
Hospitalization: 26 studies, n = 385,737.
Severity (among patients who survived during the study period): 42 studies, n = 180,770.
Mortality: 43 studies, n = 311,732.
Figure 2.
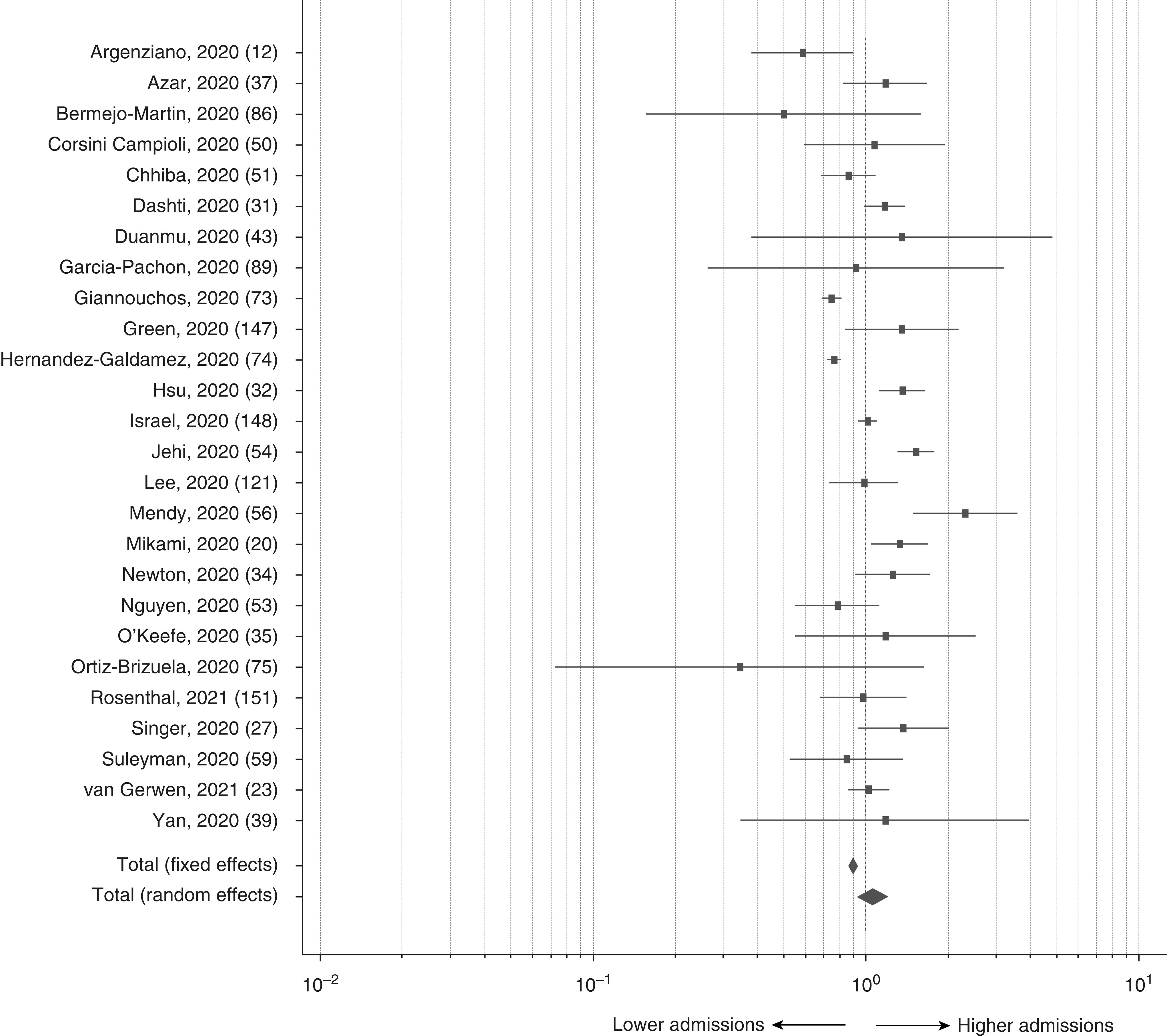
Prevalence ratios of asthma in hospitalized versus not hospitalized patients with COVID-19; pooled prevalence ratio = 1.06 (95% confidence interval, 0.94–1.19; P = 0.37). COVID-19 = coronavirus disease.
Forty-two studies provided data on asthma prevalence among living patients hospitalized with COVID-19 according to disease severity (Tables 1 and E1 and E2 and Figure 3) (11, 12, 16, 18, 19, 28, 31–34, 37, 41, 45, 48, 56, 59, 73–75, 86, 87, 98–100, 102–104, 110, 111, 113–115, 121, 130, 132, 135, 136, 142–144, 150, 151). The prevalence of asthma in patients with “severe” and “not severe” COVID-19 was 8.7% (95% CI, 6.9–10.7%) and 9.1% (95% CI, 7.8–10.5%), respectively. The pooled PR for asthma according to COVID-19 severity was 1.18 (95% CI, 0.98–1.42; P = 0.07).
Figure 3.
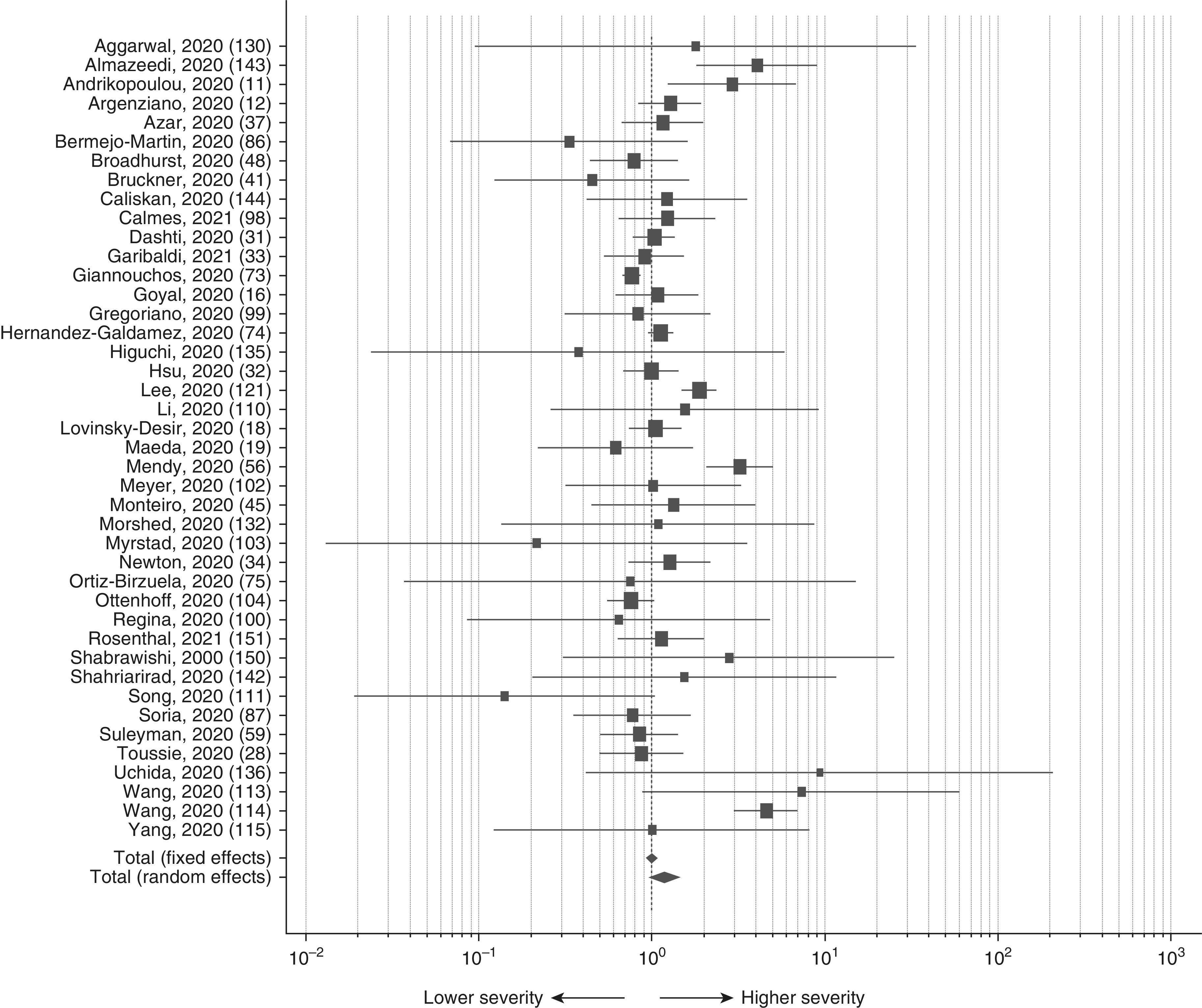
Prevalence ratios of asthma in “severe” versus “not severe” patients hospitalized with COVID-19; pooled prevalence ratio = 1.18 (95% confidence interval, 0.98–1.42; P = 0.07). COVID-19 = coronavirus disease.
We examined the prevalence of asthma in 43 studies that provided data from patients who either died of COVID-19 or survived (Tables 1 and E1 and E2 and Figure 4) (13, 15, 18, 20, 21, 23, 25, 30–33, 37, 46, 53, 61, 67, 74, 77, 81, 82, 85, 88, 97, 98, 102, 105, 106, 118, 119, 121, 129, 133, 134, 141–146, 151–154). The prevalence of asthma in these two groups was 6.8% (95% CI, 5.7–8.0%) and 8.4% (95% CI, 7.2–9.8%), respectively. The pooled PR for asthma among patients who died of COVID-19 versus those who survived was 0.85 (95 % CI, 0.71–1.01; P = 0.07). The majority of these meta-analyses yielded statistically significant heterogeneity indices related to the pooled effects (Table E2).
Figure 4.
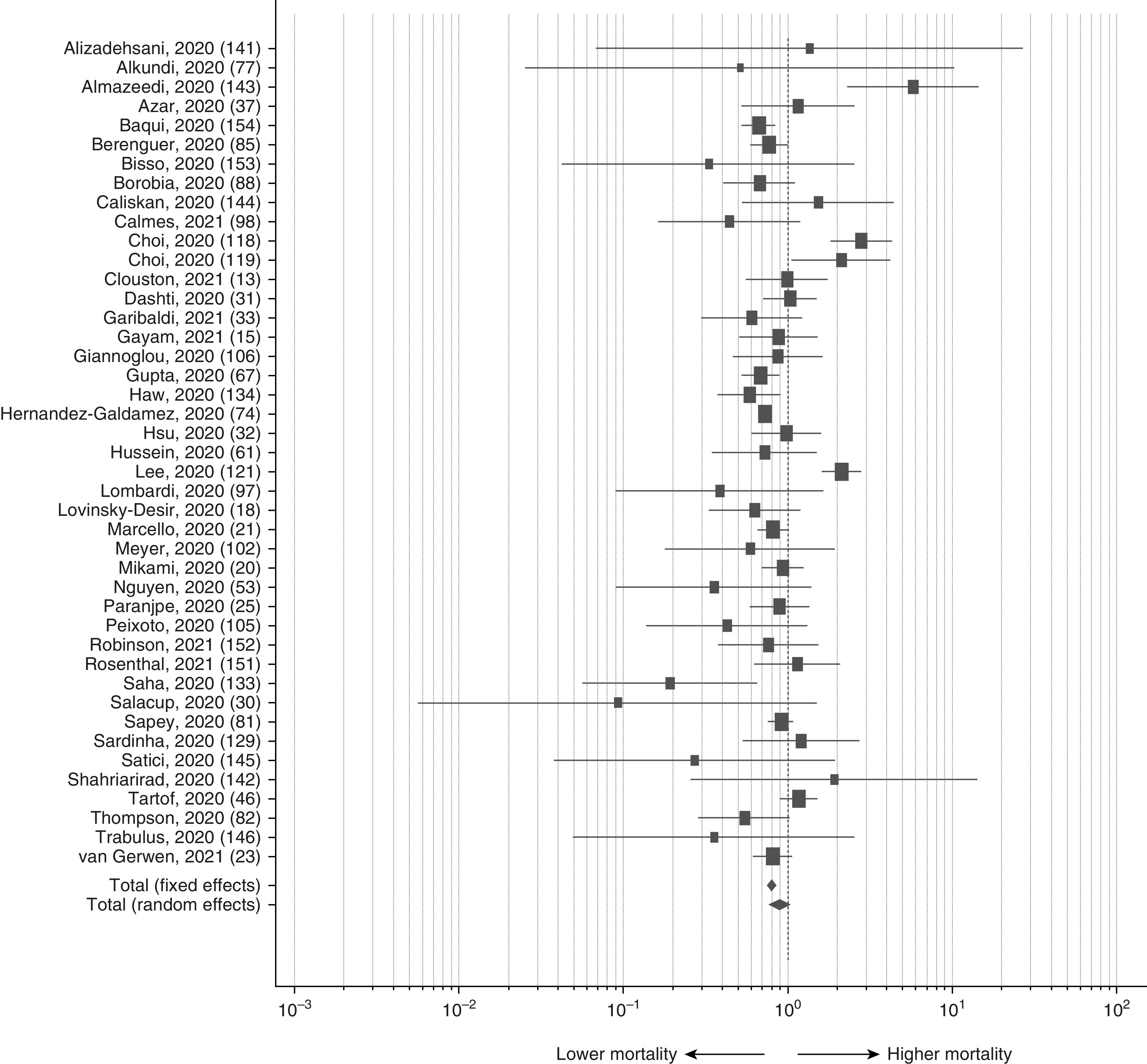
Prevalence ratios of asthma by survival status (“died” vs. “survived”) in patients hospitalized with COVID-19; pooled prevalence ratio = 0.89 (95% confidence interval, 0.77–1.02; P = 0.09). COVID-19 = coronavirus disease.
Studies That Adjusted Relative Measures of Association for Confounding Factors
Multivariable modeling was used in a subset of 24 studies of asthma and COVID-19 mortality (13, 17, 24, 29, 46, 58, 74, 76, 78, 82, 90, 98, 105, 118, 119, 124, 127, 143, 146, 152, 155–158), with adjustment for such factors as age, sex, ethnicity/race, education, and various comorbidities. These studies showed meta-odds ratio = 0.82 (95% CI, 0.79–0.85; P < 0.001), albeit with significant heterogeneity (I2 = 59.1%; 95% CI, 29.7–72.9) (Table E2).
Asthma Prevalence in People Testing Positive versus Negative for SARS-CoV-2
Seventeen studies compared asthma prevalence among people with suspected COVID-19 who subsequently tested positive for SARS-CoV-2 with those who tested negative (n = 1,828,284) (17, 21, 27, 37, 38, 47, 49, 55, 73, 79, 80, 125, 126, 128, 144, 147, 149). Asthma prevalence was significantly lower among people who tested positive (7.8%; 95 % CI, 5.1–11.1%) than among those who tested negative (10.2%; 95 % CI, 7.5–13.3%) (Table E2). One of these studies compared asthma prevalence among people who tested positive for SARS-CoV-2 with that among remaining members of their large cohort, who were not tested (79). In that study, asthma prevalence was higher in those who tested positive (13.2% vs. 11.5%). The pooled PR for asthma prevalence in these 17 studies was 0.74 (95% CI, 0.68–0.81; P < 0.001).
Discussion
The questions addressed in our analyses are among those that would seem most meaningful to people who have asthma in a time of high respiratory-related morbidity and mortality from a novel infectious disease of unclear etiology, one for which there is limited treatment. The public health significance of these questions is underscored by the high worldwide prevalence of asthma and the relatively rapid appearance in the literature of many studies addressing aspects of the association between asthma and COVID-19. However, the results and conclusions presented here should be viewed in light of the likelihood that the results of many additional relevant studies will be available in the near future.
Does Asthma Increase the Risk of Contracting Morbid COVID-19?
The prevalence of asthma in study populations diagnosed with COVID-19 can be compared with that among regional general populations, possibly suggesting whether patients with asthma are more likely than average to be negatively affected by SARS-CoV-2. In 63 U.S.-based studies, for example, the prevalence of asthma in people with COVID-19 was 11.0%, approximately 43% higher than the estimated 7.7% of adults with asthma in the general U.S. population, including adults over age 65 (159). This suggests the possibility that individuals with asthma may be more likely than individuals without asthma to be diagnosed with COVID-19 in the United States. In 19 studies conducted in the New York City region, however, the prevalence of asthma in patients with COVID-19 was 8.7%, which is approximately the same as the 8.8% estimated prevalence among adults in New York City (160). In 31 studies conducted in Europe, the prevalence of asthma in patients with COVID-19 was 7.6%, which is 7% lower than the estimated 8.2% prevalence among adults in Europe (161). Likewise, the pooled prevalence of asthma in studies of people with COVID-19 conducted in Mexico (2.9%), Korea (5.4%), and China (1.9%) is similar to, or lower than, estimates from general population surveys in those countries (162–164).
Comparisons of asthma prevalence in studies of people with morbid COVID-19 with that in general population surveys are problematic, with population estimates varying among samples and over time, and with generally no standardization for such factors as age, sex, race/ethnicity, and the methods by which asthma was diagnosed. At best, such comparisons using data from the studies we reviewed crudely suggest that there are no obvious trends toward higher asthma prevalence in study populations afflicted with COVID-19 compared with regional general populations.
In our review, 17 studies compared asthma prevalence among people with suspected COVID-19 who subsequently tested positive with those who tested negative. In those studies, investigators classified patients’ asthma status using standardized electronic health records within the same hospital or health system. The results do not support an increased risk of COVID-19 morbidity in people with asthma; rather, they suggest the possibility of a moderate decreased risk.
Does Asthma Increase the Severity of COVID-19?
Asthma prevalence was compared among people hospitalized with COVID-19 and ambulatory patients; among surviving hospitalized patients with “severe” and “nonsevere” COVID-19; and among those surviving and not surviving the disease. None of these comparisons showed strong or statistically significant differences. Unlike studies comparing asthma prevalence among study populations with that among local populations, these pooled PRs related to COVID-19 hospitalization, severity, and mortality were based on asthma prevalence assessed similarly among study participants with the same disease, COVID-19, underlying their visit to the same hospitals during the same time periods. Furthermore, our analysis of 24 studies that adjusted asthma’s association with mortality for factors such as age, sex, ethnicity/race, and education, does not suggest that an appreciable harmful effect of asthma on COVID-19 severity was masked by confounding. Of course, in the latter studies, there is still potential bias from confounding by other factors.
Several other studies relating asthma to COVID-19 severity have been conducted that were not included in our analyses. A case series of 1,827 adults with laboratory-confirmed COVID-19 in Boston, Massachusetts (data not included in our analyses because all participants had asthma), showed similar COVID-19 severity and mortality risks when compared with all patients with COVID-19 in the Mass General Brigham system during the same time period (165). Likewise, a cohort of patients with severe asthma and COVID-19 in Italy showed a hospitalization rate similar to that in the general Italian population (166). In Spain, a survey of the medical records of 71,192 patients with asthma showed 1.4% had been diagnosed with COVID-19 (167), considerably lower than the approximately 4% diagnosis in the Spanish population (168). Investigators at the CDC used data from the national Veterans Health Administration to compare asthma prevalence in 3,948 hospitalized patients with COVID-19 (March 1 to May 31, 2020) with that in 5,453 hospitalized patients with influenza (October 1, 2018, to February 1, 2020) (66). The prevalence of asthma in patients with COVID-19 (6.9%) was significantly lower than that in patients with influenza (10.5%). Similarly, the prevalence of asthma in patients hospitalized with COVID-19 (14.3%) was lower than that among patients hospitalized with influenza (27.3%) during the same time period in Finland, although the study was small and statistical significance for this difference was lacking (169). A multivariable analysis using data from electronic health records of over 17 million adults with suspected COVID-19 in London, England, in the National Health Service database, showed a hazard ratio of death for “asthma with no recent use of oral corticosteroids” of 0.99 (95% CI, 0.93–1.05), whereas the estimate for “asthma with recent use of oral corticosteroids” was 1.13 (95% CI, 1.01–1.26) (170). That study analyzed “suspected” cases of COVID-19 that were not necessarily diagnostically confirmed and therefore may include false positives. Although the possibility of effect modification by oral corticosteroid use is of interest, a recent systematic review (171), in agreement with recent mechanistic data (172), found that “there is no evidence to support the withdrawal of ICS [inhaled corticosteroids] in patients treated with these drugs, and to do so is likely to be harmful.” Overall, these data, together with those discussed above, do not support a clear increased risk of COVID-19 severity among most people with asthma.
Biological Mechanisms
The presumption that asthma increases the risk of COVID-19 severity and mortality is consistent with the chronic inflammatory infiltration and airways dysfunction characterizing asthma, and the increased frequency and severity of respiratory infections in patients with asthma, such as is the case with influenza (8). The biological mechanisms underlying any protection in people with asthma regarding severe COVID-19 are unknown at this time. It has been suggested that decreased ACE2 (angiotensin-converting enzyme 2) receptor expression may lower the risk of COVID-19 severity and mortality in patients with atopic asthma (173). It has also been suggested that T-helper 2 (Th2) immune response in patients with asthma may counter the inflammation induced by SARS-CoV-2 infection (174). Inhaled corticosteroids, such as budesonide (171) or ciclesonide (175, 176), used by patients with asthma, may reduce the risk of infection or of developing symptoms leading to diagnosis. Biological mechanisms are still speculative, but ciclesonide, for example, may inhibit the replication of SARS-CoV-2 genomic RNA by targeting the viral endonuclease NSP15 (176). The lack of known biological mechanisms notwithstanding, data from the studies included in our analyses do not clearly show an altered risk of COVID-19 morbidity among adults with asthma.
Limitations
Our study has several limitations. Asthma diagnosis criteria were often not specified, or otherwise varied from self-report to physician diagnosis to use of asthma medication, likely resulting in an unknown degree of misclassification. The type of asthma (atopic, nonatopic) was rarely specified, a limitation given patients with atopic asthma may be less susceptible to increased COVID-19 morbidity (52, 57, 125). The prevalence of asthma in people with COVID-19 also varied greatly across regions, and from sample to sample within regions. Without knowing the reasons for this variation, it is difficult to assess whether or to what extent biased estimates may have influenced our findings. It is possible that certain factors influenced diagnosis patterns, such as increased screening for COVID-19 among people with asthma (177). Certainly, the low estimates of asthma prevalence in the studies conducted in China compared with estimates from other countries and those in the local Chinese populations require explanation. We can speculate that patients with asthma in those study catchment areas tended to stay home due to fear of contracting COVID-19 (178). Lack of chronic airways disease awareness and lack of community spirometric testing are other possible reasons (179).
The majority of the meta-analyses that we performed yielded significant heterogeneity indices related to the pooled effects (Table E2), which may be indicative of the aforementioned biases. This heterogeneity may detract from the generalizability and interpretability of the pooled effects. Nonetheless, these findings may reflect the disparate epidemiological characteristics of COVID-19 in human populations around the world.
Finally, several of the studies included in our analyses were still in preprint (13, 21, 24, 31, 34, 35, 47, 49, 53, 56, 65, 70, 71, 76, 79, 80, 87, 91, 104–106, 115, 126–129, 132, 133, 138–140, 148, 149, 153, 167) and had yet to fully undergo the peer-review process. Whereas early access to study data may facilitate the timely dissemination of information to researchers, policymakers, and the public, the peer-review process helps to ensure the validity of study data and conclusions (180).
In conclusion, whereas patients with asthma are naturally apprehensive about the threat posed by COVID-19, in our review and analysis of the literature, we did not find clear evidence of increased risk of COVID-19 diagnosis, hospitalization, severity, or mortality due to asthma. However, additional studies are needed to clarify these associations, particularly studies with adequate sample size; clearly defined and consistently applied criteria for COVID-19 diagnosis and severity; clearly defined criteria for asthma diagnosis, including phenotype (atopic, nonatopic) and severity; and reliable, accurate data on asthma prevalence in people without COVID-19 who are otherwise comparable on such factors as age, sex, geographic region, and diagnostic methods. Nevertheless, our findings could provide some reassurance to people with asthma regarding its potential to increase their risk of severe consequences of COVID-19.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank Mr. David Peterson of the Preston Medical Library at the University of Tennessee Medical Center for his assistance in conducting the literature search for this article.
Footnotes
Author Contributions: Conception and design: P.D.T. and R.D. Analysis and interpretation: P.D.T., R.E.H., and R.D. Drafting the manuscript for important intellectual content: P.D.T., R.E.H., and R.D.
Data Availability: Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202008-3266OC on January 25, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.WHO COVID-19 Public Health Emergency of International Concern (PHEIC) global research and innovation forum Geneva, Switzerland: World Health Organization; 2020[accessed 2020 Oct 29]. Available from: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum [Google Scholar]
- 2.WHO WHO Coronavirus Disease (COVID-19) dashboard Geneva, Switzerland: World Health Organization;2020[updated 2021 Feb 2; accessed 2020 Oct 29]. Available from: https://covid19.who.int [Google Scholar]
- 3.Weill Cornell Medicine COVID-19: why is it mild for some, deadly for others? New York, New York: Weill Cornell Medicine; 2020[accessed 2020 Oct 29]. Available from: https://weillcornell.org/news/COVID-19-why-is-it-mild-for-some-deadly-for-others [Google Scholar]
- 4.Global Asthma Network The global asthma report Auckland, New Zealand: Global Asthma Network; 2018[accessed 2020 Oct 29]. Available from: http://www.globalasthmareport.org/Global%20Asthma%20Report%202018.pdf [Google Scholar]
- 5.Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Centers for Disease Control and Prevention Precautions regarding COVID-19 and asthma Atlanta, Georgia: Center for Disease Control and Prevention; 2020[updated 2021 Jan 20; accessed 2020 Oct 29]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html [Google Scholar]
- 7.World Health Organization Coronavirus disease (COVID-19) advice for the public Geneva Switzerland: World Health Organization; 2020[accessed 2020 Oct 29]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters [Google Scholar]
- 8.US Centers for Disease Control and Prevention Flu & people with asthma Atlanta, Georgia: Centers for Disease Control and Prevention; [updated 2021 Jan 28; accessed 2020 Oct 29]. Available from: https://www.cdc.gov/flu/highrisk/asthma.htm [Google Scholar]
- 9.Busse WW, Lemanske RF, Jr, Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376:826–834. doi: 10.1016/S0140-6736(10)61380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abrams MP, Wan EY, Waase MP, Morrow JP, Dizon JM, Yarmohammadi H, et al. Clinical and cardiac characteristics of COVID-19 mortalities in a diverse New York City Cohort. J Cardiovasc Electrophysiol. 2020;31:3086–3096. doi: 10.1111/jce.14772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andrikopoulou M, Madden N, Wen T, Aubey JJ, Aziz A, Baptiste CD, et al. Symptoms and critical illness among obstetric patients with coronavirus disease 2019 (COVID-19) infection. Obstet Gynecol. 2020;136:291–299. doi: 10.1097/AOG.0000000000003996. [DOI] [PubMed] [Google Scholar]
- 12.Argenziano MG, Bruce SL, Slater CL, Tiao JR, Baldwin MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. doi: 10.1136/bmj.m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clouston SAP, Luft BJ, Sun E.History of premorbid depression is a risk factor for COVID-related mortality: analysis of 1,387 COVID+ patients [preprint] medRxiv 2021[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.12.17.20248362v2. [Google Scholar]
- 14.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gayam V, Chobufo MD, Merghani MA, Lamichhane S, Garlapati PR, Adler MK. Clinical characteristics and predictors of mortality in African-Americans with COVID-19 from an inner-city community teaching hospital in New York. J Med Virol. 2021;93:812–819. doi: 10.1002/jmv.26306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lieberman-Cribbin W, Rapp J, Alpert N, Tuminello S, Taioli E. The impact of asthma on mortality in patients with COVID-19. Chest. 2020;158:2290–2291. doi: 10.1016/j.chest.2020.05.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lovinsky-Desir S, Desphpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146:1027–1034, e4. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maeda T, Obata R, Do DR, Kuno T.The association of interleukin-6 value, interleukin inhibitors, and outcomes of patients with COVID-19 in New York City J Med Virol[online ahead of print] 28 Jul 2020 [DOI] [PubMed]
- 20.Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, et al. Risk factors for mortality in patients with COVID-19 in New York City J Gen Intern Med[online ahead of print] 30 Jun 2020 [DOI] [PMC free article] [PubMed]
- 21.Marcello RK, Dolle J, Grami S, Adule R, Li Z, Tatem K, et al. Characteristics and outcomes of COVID-19 patients in New York City’s public hospital system [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.05.29.20086645v3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108:154262. doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Gerwen M, Alsen M, Little C, Barlow J, Genden E, Naymagon L, et al. Risk factors and outcomes of COVID-19 in New York City; a retrospective cohort study. J Med Virol. 2021;93:907–915. doi: 10.1002/jmv.26337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang AL, Zhong Z, Hurd YL.Comorbidity and sociodemographic determinants in COVID-19 mortality in an US urban healthcare system [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.11.20128926v1. [Google Scholar]
- 25.Paranjpe I, Russak AJ, De Freitas JK, Lala A, Miotto R, Vaid A, et al. Clinical characteristics of hospitalized COVID-19 patients in New York City [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.04.19.20062117v2. [Google Scholar]
- 26.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area JAMA 20203232052–2059.[Published erratum appears in JAMA 323:2098.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singer AJ, Morley EJ, Meyers K, Fernandes R, Rowe AL, Viccellio P, et al. Cohort of Four thousand four hundred four persons under investigation for COVID-19 in a New York hospital and predictors of ICU care and ventilation. Ann Emerg Med. 2020;76:394–404. doi: 10.1016/j.annemergmed.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, et al. Clinical and chest radiography features determine patient outcomes in young and middle-aged adults with COVID-19. Radiology. 2020;297:E197–E206. doi: 10.1148/radiol.2020201754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox T, Ruddiman K, Lo KB, Peterson E, DeJoy R, Salacup G, et al. The relationship between diabetes and clinical outcomes in COVID-19: a single-center retrospective analysis. Acta Diabetol. 2021;58:33–38. doi: 10.1007/s00592-020-01592-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salacup G, Lo KB, Gul F, Peterson E, De Joy R, Bhargav R, et al. Characteristics and clinical outcomes of COVID-19 patients in an underserved-inner city population: a single tertiary center cohort J Med Virol[online ahead of print] 3 Jul 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dashti HT, Bates D, Fiskio JM, Roche EC, Mora S, Demler O.Clinical characteristics and severity of COVID-19 disease in patients from Boston area hospitals [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.07.27.20163071v1. [Google Scholar]
- 32.Hsu HE, Ashe EM, Silverstein M, Hofman M, Lange SJ, Razzaghi H, et al. Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an urban safety-net medical center - Boston, Massachusetts, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:864–869. doi: 10.15585/mmwr.mm6927a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garibaldi BT, Fiksel J, Muschelli J, Robinson ML, Rouhizadeh M, Perin J, et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study Ann Intern Med 202117433–41.[Published erratum appears in Ann Intern Med 174:144.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newton S, Zollinger B, Freeman J, Moran S, Helfand A, Authelet K, et al. Factors associated with clinical severity in Emergency Department patients presenting with symptomatic SARS-CoV-2 infection [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.12.08.20246017v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Keefe JB, Tong EJ, Taylor TH, O’Keefe GDD, Tong DC.Initial experience in predicting the risk of hospitalization of 496 outpatients with COVID-19 using a telemedicine risk assessment tool medRxiv 2020[accessed 2020 Dec 29]. Available from: 10.1101/2020.07.21.20159384. [DOI] [Google Scholar]
- 36.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39:1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 38.Shah SJ, Barish PH, Prasad PA, Kistler A, Neff N, Kamm J, et al. Clinical features, diagnostics, and outcomes of patients presenting with acute respiratory illness: a retrospective cohort study of patients with and without COVID-19. EClinicalMedicine. 2020;27:100518. doi: 10.1016/j.eclinm.2020.100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yan CH, Faraji F, Prajapati DP, Ostrander BT, DeConde AS. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol. 2020;10:821–831. doi: 10.1002/alr.22592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. COVID-19 in critically ill patients in the Seattle region: case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruckner FS, McCulloch DJ, Atluri V, Blain M, McGuffin SA, Nalla AK, et al. Clinical features and outcomes of 105 hospitalized patients with COVID-19 in Seattle, Washington. Clin Infect Dis. 2020;71:2167–2173. doi: 10.1093/cid/ciaa632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lokken EM, Walker CL, Delaney S, Kachikis A, Kretzer NM, Erickson A, et al. Clinical characteristics of 46 pregnant women with a severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. 2020;223:911.e1–911.e14. doi: 10.1016/j.ajog.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duanmu Y, Brown IP, Gibb WR, Singh J, Matheson LW, Blomkalns AL, et al. Characteristics of emergency department patients with COVID-19 at a single site in Northern California: clinical observations and public health implications. Acad Emerg Med. 2020;27:505–509. doi: 10.1111/acem.14003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferguson J, Rosser JI, Quintero O, Scott J, Subramanian A, Gumma M, et al. Characteristics and outcomes of coronavirus disease patients under nonsurge conditions, Northern California, USA, March-April 2020. Emerg Infect Dis. 2020;26:1679–1685. doi: 10.3201/eid2608.201776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Monteiro AC, Suri R, Emeruwa IO, Stretch RJ, Cortes-Lopez RY, Sherman A, et al. Obesity and smoking as risk factors for invasive mechanical ventilation in COVID-19: a retrospective, observational cohort study. PLoS One. 2020;15:e0238552. doi: 10.1371/journal.pone.0238552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tartof SY, Qian L, Hong V, Wei R, Nadjafi RF, Fischer H, et al. Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization. Ann Intern Med. 2020;173:773–781. doi: 10.7326/M20-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dai CL, Kornilov SA, Roper RT, Cohen-Cline H, Jade K, Smith B, et al. Characteristics and factors associated with COVID-19 infection, hospitalization, and mortality across race and ethnicity [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.14.20212803v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Broadhurst R, Peterson R, Wisnivesky JP, Federman A, Zimmer SM, Sharma S, et al. Asthma in COVID-19 hospitalizations: an overestimated risk factor? Ann Am Thorac Soc. 2020;17:1645–1648. doi: 10.1513/AnnalsATS.202006-613RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barasa S, Kiage-Moyaka J, Cruz-Madrid K, Friedlander M.Smoking increases the risk of COVID-19 positivity, while never-smoking reduces the risk [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.11.30.20241380v1. [Google Scholar]
- 50.Corsini Campioli C, Cano Cevallos E, Assi M, Patel R, Binnicker MJ, O’Horo JC. Clinical predictors and timing of cessation of viral RNA shedding in patients with COVID-19. J Clin Virol. 2020;130:104577. doi: 10.1016/j.jcv.2020.104577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chhiba KD, Patel GB, Vu THT, Chen MM, Guo A, Kudlaty E, et al. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol. 2020;146:307–314, e4. doi: 10.1016/j.jaci.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mahdavinia M, Foster KJ, Jauregui E, Moore D, Adnan D, Andy-Nweye AB, et al. Asthma prolongs intubation in COVID-19. J Allergy Clin Immunol Pract. 2020;8:2388–2391. doi: 10.1016/j.jaip.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nguyen AB, Upadhyay GA, Chung B, Smith B, Besser SA, Johnson JA, et al. Outcomes and cardiovascular comorbidities in a predominantly African-American population with COVID-19 [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.28.20141929v1. [Google Scholar]
- 54.Jehi L, Ji X, Milinovich A, Erzurum S, Merlino A, Gordon S, et al. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLoS One. 2020;15:e0237419. doi: 10.1371/journal.pone.0237419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meyers KJ, Jones ME, Goetz IA, Botros FT, Knorr J, Manner DH, et al. A cross-sectional community-based observational study of asymptomatic SARS-CoV-2 prevalence in the greater Indianapolis area. J Med Virol. 2020;92:2874–2879. doi: 10.1002/jmv.26182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mendy A, Spewokin S, Wells AA, Morrow AL.Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 patients [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.25.20137323v2. [Google Scholar]
- 57.Keswani A, Dhana K, Rosenthal JA, Moore D, Mahdavinia M. Atopy is predictive of a decreased need for hospitalization for coronavirus disease 2019. Ann Allergy Asthma Immunol. 2020;125:479–481. doi: 10.1016/j.anai.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arshad S, Kilgore P, Chaudhry ZS, Jacobsen G, Wang DD, Huitsing K, et al. Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19. Int J Infect Dis. 2020;97:396–403. doi: 10.1016/j.ijid.2020.06.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open. 2020;3:e2012270. doi: 10.1001/jamanetworkopen.2020.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gold JAW, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:545–550. doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hussein MH, Toraih EA, Attia AS, Burley N, Zhang AD, Roos J, et al. Asthma in COVID-19 patients: an extra chain fitting around the neck? Respir Med. 2020;175:106205. doi: 10.1016/j.rmed.2020.106205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with COVID-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Silver V, Chapple AG, Feibus AH, Beckford J, Halapin NA, Barua D, et al. Clinical characteristics and outcomes based on race of hospitalized patients with COVID-19 in a New Orleans cohort. Open Forum Infect Dis. 2020;7:ofaa339. doi: 10.1093/ofid/ofaa339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bajaj JS, Garcia-Tsao G, Biggins SW, Kamath PS, Wong F, McGeorge S, et al. Comparison of mortality risk in patients with cirrhosis and COVID-19 compared with patients with cirrhosis alone and COVID-19 alone: multicentre matched cohort Gut[online ahead of print] 13 Jul 2020 [DOI] [PMC free article] [PubMed]
- 65.Bramante CT, Ingraham NE, Murray TA, Marmor S, Hoversten S, Gronski J, et al. Observational study of metformin and risk of mortality in patients hospitalized with Covid-19 [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.19.20135095v2. [Google Scholar]
- 66.Cates J, Lucero-Obusan C, Dahl RM, Schirmer P, Garg S, Oda G, et al. Risk for in-hospital complications associated with COVID-19 and influenza - Veterans health administration, United States, October 1, 2018-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1528–1534. doi: 10.15585/mmwr.mm6942e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. STOP-COVID Investigators Factors associated with death in critically ill patients with coronavirus disease 2019 in the US JAMA Intern Med 20201801–12.[Published erratum appears in DOI: 10.1001/jamainternmed.2020.4568.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim L, Garg S, O’Halloran A, Whitaker M, Pham H, Anderson EJ, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the U.S. Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET) Clin Infect Dis[online ahead of print] 16 Jul 2020 [DOI] [PMC free article] [PubMed]
- 69.Ko JY, Danielson ML, Town M, Derado G, Greenlund KJ, Kirley PD, et al. Risk factors for COVID-19-associated hospitalization: COVID-19-associated hospitalization surveillance network and behavioral risk factor surveillance system Clin Infect Dis[online ahead of print] 18 Sep 2020 [DOI] [PMC free article] [PubMed]
- 70.Burn E, You SC, Sena AG, Kosta K, Abedtash H, Abrahao MTF, et al. Deep phenotyping of 34,128 patients hospitalised with COVID-19 and a comparison with 81,596 influenza patients in America, Europe and Asia: an international network study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.04.22.20074336v2. [Google Scholar]
- 71.Burn E, Sena AG, Prats-Uribe AP, Spotnitz M, DuVall S, Lynch KE, et al. Use of dialysis, tracheostomy, and extracorporeal membrane oxygenation among 240,392 patients hospitalized with COVID-19 in the United States [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.11.25.20229088v1. [Google Scholar]
- 72.Bello-Chavolla OY, Gonzalez-Diaz A, Antonio-Villa NE, Fermin-Martinez CA, Marquez-Salinas A, Vargas-Vasquez A, et al. Unequal impact of structural health determinants and comorbidity on COVID-19 severity and lethality in older Mexican adults: considerations beyond chronological aging J Gerontol A Biol Sci Med Sci[online ahead of print] 29 Jun 2020 [DOI] [PMC free article] [PubMed]
- 73.Giannouchos TV, Sussman RA, Mier JM, Poulas K, Farsalinos K.Characteristics and risk factors for COVID-19 diagnosis and adverse outcomes in Mexico: an analysis of 89,756 laboratory: confirmed COVID-19 cases Eur Respir J[online ahead of print] 30 Jul 2020 [DOI] [PMC free article] [PubMed]
- 74.Hernandez-Galdamez DR, Gonzalez-Block MA, Romo-Duenas DK, Lima-Morales R, Hernandez-Vincente IA, Lumbreras-Guzman M, et al. Increased risk of hospitalization and death in patients with COVID-19 and pre-existing noncommunicable diseases and modifiable risk factors in Mexico. Arch Med Res. 2020;51:683–689. doi: 10.1016/j.arcmed.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ortiz-Brizuela E, Villanueva-Reza M, González-Lara MF, Tamez-Torres KM, Román-Montes CM, Díaz-Mejía BA, et al. Clinical and epidemiological characteristics of patients diagnosed with COVID-19 in a tertiary care center in Mexico City: a prospective cohort study. Rev Invest Clin. 2020;72:165–177. doi: 10.24875/RIC.20000211. [DOI] [PubMed] [Google Scholar]
- 76.Solis P, Carreno H.COVID-19 fatality and comorbidity risk factors among diagnosed patients in Mexico [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.04.21.20074591v1. [Google Scholar]
- 77.Alkundi A, Mahmoud I, Musa A, Naveed S, Alshawwaf M. Clinical characteristics and outcomes of COVID-19 hospitalized patients with diabetes in the UK: a retrospective single centre study. Diabetes Res Clin Pract. 2020;165:108263. doi: 10.1016/j.diabres.2020.108263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cavallaro M, Moiz H, Keeling MJ, McCarthy ND.Contrasting factors associated with COVID-19-related ICU and death outcomes: interpretable multivariable analyses of the UK CHESS dataset [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.12.03.20242941v1. [Google Scholar]
- 79.Chudasama YV, Zaccardi F, Gillies CL, Razieh C, Yates T, Kloecker DE, et al. Patterns of multimorbidity and risk of severe SARS-CoV-2 infection: an observational study in the UK [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.21.20216721v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Goodacre S, Thomas B, Lee E, Sutton L, Loban A, Waterhouse S, et al. Characterisation of 22446 patients attending UK emergency departments with suspected COVID-19 infection: observational cohort study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.08.10.20171496v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sapey E, Gallier S, Mainey C, Nightingale P, McNulty D, Crothers H, et al. All clinicians and students at University Hospitals Birmingham NHS Foundation Trust. Ethnicity and risk of death in patients hospitalised for COVID-19 infection in the UK: an observational cohort study in an urban catchment area. BMJ Open Respir Res. 2020;7:e000644. doi: 10.1136/bmjresp-2020-000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thompson JV, Meghani NJ, Powell BM, Newell I, Craven R, Skilton C, et al. Patient characteristics and predictors of mortality in 470 adults admitted to a district general hospital in England with Covid-19. Epidemiol Infect. 2020;148:e285. doi: 10.1017/S0950268820002873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Docherty AB, Harrison EM, Green CA, Hardwick H, Pius R, Normal L, et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO clinical characterisation protocol. BMJ. 2020 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Butler MW, O’Reilly A, Dunican EM, Mallon P, Feeney ER, Keane MP, et al. Prevalence of comorbid asthma in COVID-19 patients. J Allergy Clin Immunol. 2020;146:334–335. doi: 10.1016/j.jaci.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Berenguer J, Ryan P, Rodríguez-Baño J, Jarrín I, Carratalà J, Pachón J, et al. COVID-19@Spain Study Group Fundación SEIMC-GESIDA Hospital General Universitario Gregorio Marañón Hospital Universitario La Paz Hospital Infanta Leonor Complejo Hospitalario Virgen de la Salud et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain Clin Microbiol Infect 2020261525–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bermejo-Martin JF, González-Rivera M, Almansa R, Micheloud D, Tedim AP, Domínguez-Gil M, et al. Viral RNA load in plasma is associated with critical illness and a dysregulated host response in COVID-19. Crit Care. 2020;24:691. doi: 10.1186/s13054-020-03398-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Soria ME, Corton M, Martinez-Gonzalez B, Lobo-Vega R, Vazquez-Sirvent L, Lopez-Rodriguez R, et al. High SARS-CoV-2 viral load is associated with a worse clinical outcome of COVID-19 disease [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.11.13.20229666v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Borobia AM, Carcas AJ, Arnalich F, Alvarez-Sala R, Montserrat J, Quintana M, et al. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J Clin Med. 2020;9:1733. doi: 10.3390/jcm9061733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Garcia-Pachon E, Zamora-Molina L, Soler-Sempere MJ, Baeza-Martinez C, Grau-Delgado J, Canto-Reig V, et al. Asthma prevalence in patients with SARS-CoV-2 infection detected by RT-PCR not requiring hospitalization. Respir Med. 2020;171:106084. doi: 10.1016/j.rmed.2020.106084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Poblador-Plou B, Carmona-Pírez J, Ioakeim-Skoufa I, Poncel-Falcó A, Bliek-Bueno K, Cano-Del Pozo M, et al. Baseline chronic comorbidity and mortality in laboratory-confirmed COVID-19 Cases: results from the PRECOVID study in Spain. Int J Environ Res Public Health. 2020;17:5171. doi: 10.3390/ijerph17145171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Prieto-Alhambra D, Ballo E, Coma E, Mora N, Aragon M, Prats-Uribe A, et al. Hospitalization and 30-day fatality in 121,263 COVID-19 outpatient cases [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.05.04.20090050v1. [Google Scholar]
- 92.San-Juan R, Barbero P, Fernández-Ruiz M, López-Medrano F, Lizasoáin M, Hernández-Jiménez P, et al. Incidence and clinical profiles of COVID-19 pneumonia in pregnant women: a single-centre cohort study from Spain. EClinicalMedicine. 2020;23:100407. doi: 10.1016/j.eclinm.2020.100407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Beurnier A, Jutant E-M, Jevnikar M, Boucly A, Pichon J, Preda M, et al. Characteristics and outcomes of asthmatic patients with COVID-19 pneumonia who require hospitalisation. Eur Respir J. 2020;56:2001875. doi: 10.1183/13993003.01875-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Grandbastien M, Piotin A, Godet J, Abessolo-Amougou I, Ederlé C, Enache I, et al. SARS-CoV-2 pneumonia in hospitalized asthmatic patients did not induce severe exacerbation. J Allergy Clin Immunol Pract. 2020;8:2600–2607. doi: 10.1016/j.jaip.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Barroso B, Valverde-Monge M, Canas JA, Bodrigo-Munoz JM, Gonzalez-Cano B, Villalobos-Vilda C, et al. Prevalence, characteristics and outcome of asthmatic patients with Type 2 diseases in hospitalized subjects with COVID-19 in Madrid, Spain. J Investig Allergol Clin Immunol. 2020;30:382–384. doi: 10.18176/jiaci.0627. [DOI] [PubMed] [Google Scholar]
- 96.Caminati M, Lombardi C, Micheletto C, Roca E, Bigni B, Furci F, et al. Asthmatic patients in COVID-19 outbreak: few cases despite many cases. J Allergy Clin Immunol. 2020;146:541–542. doi: 10.1016/j.jaci.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lombardi C, Roca E, Bigni B, Cottini M, Passalacqua G. Clinical course and outcomes of patients with asthma hospitalized for severe acute respiratory syndrome coronavirus pneumonia: a single-center, retrospective study. Ann Allergy Asthma Immunol. 2020;125:707–709. doi: 10.1016/j.anai.2020.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Calmes D, Graff S, Maes N, Frix AN, Thys M, Bonhomme O, et al. Asthma and COPD are not risk factors for ICU stay and death in case of SARS-CoV2 infection. J Allergy Clin Immunol Pract. 2021;9:160–169. doi: 10.1016/j.jaip.2020.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gregoriano C, Koch D, Haubitz S, Conen A, Fux CA, Mueller B, et al. Characteristics, predictors and outcomes among 99 patients hospitalised with COVID-19 in a tertiary care centre in Switzerland: an observational analysis. Swiss Med Wkly. 2020;150:w20316. doi: 10.4414/smw.2020.20316. [DOI] [PubMed] [Google Scholar]
- 100.Regina J, Papadimitriou-Olivgeris M, Burger R, Filippidis P, Tschopp J, Desgranges F, et al. Epidemiology, risk factors and clinical course of SARS-CoV-2 infected patients in a Swiss university hospital: an observational retrospective study. Plos One. 2020;15:e0240781. doi: 10.1371/journal.pone.0240781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Avdeev S, Moiseev S, Brovko M, Yavorovskiy A, Umbetova K, Akulkina L, et al. Low prevalence of bronchial asthma and chronic obstructive lung disease among intensive care unit patients with COVID-19. Allergy. 2020;75:2703–2704. doi: 10.1111/all.14420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Meyer CN. Transmission, start of symptom and morbidity among Danish COVID-19 patients admitted to hospital. Dan Med J. 2020;67:A05200325. [PubMed] [Google Scholar]
- 103.Myrstad M, Ihle-Hansen H, Tveita AA, Andersen EL, Nygård S, Tveit A, et al. National Early Warning Score 2 (NEWS2) on admission predicts severe disease and in-hospital mortality from Covid-19 - a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2020;28:66. doi: 10.1186/s13049-020-00764-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ottenhoff MC, Ramos LL, Potters W, Janssen MLF, Hubers D, Pina-Fuentes D, et al. Predicting mortality of individual COVID-19 patients: a multicenter Dutch cohort [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.10.20210591v1. [Google Scholar]
- 105.Peixoto VR, Vieira A, Aguiar P, Sousa P, Carvalho C, Thomas D, et al. COVID-19: determinants of hospitalization, ICU and death among 20,293 reported cases in Portugal [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.05.29.20115824v1. [Google Scholar]
- 106.Giannoglou D, Meimeti E, Provatopoulou X, Stathopoulos K, Roukas IK, Galanis P.Predictors of mortality in hospitalized COVID-19 patients in Athens, Greece [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.12.20211193v1. [Google Scholar]
- 107.Guan W-J, Liang W-H, Zhao Y, Liang H-R, Chen Z-S, Li Y-M, et al. China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Huang Y, Tu M, Wang S, Chen S, Zhou W, Chen D, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: a retrospective single center analysis. Travel Med Infect Dis. 2020;36:101606. doi: 10.1016/j.tmaid.2020.101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Song J, Zeng M, Wang H, Qin C, Hou HY, Sun Z-Y, et al. Distinct effects of asthma and COPD comorbidity on disease expression and outcome in patients with COVID-19 Allergy[online ahead of print] 27 Jul 2020 [DOI] [PubMed] [Google Scholar]
- 112.Shi W, Gao Z, Ding Y, Zhu T, Zhang W, Xu Y. Clinical characteristics of COVID-19 patients combined with allergy. Allergy. 2020;75:2405–2408. doi: 10.1111/all.14434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang W, Zhao Z, Liu X, Liu G, Xie D, Xu Z, et al. Clinical features and potential risk factors for discerning the critical cases and predicting the outcome of patients with COVID-19. J Clin Lab Anal. 2020;34:e23547. doi: 10.1002/jcla.23547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang J, Guo S, Zhang Y, Gao K, Zuo J, Tan N, et al. Clinical features and risk factors for severe inpatients with COVID-19: a retrospective study in China PLoS One2020;15e0244125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yang S, Ma L, Wang YL, Wang Q, Tong Q, Chen M, et al. Risk factors for critical-ill events of patients with COVID-19 in Wuhan, China: a retrospective cohort study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.14.20130765v1. [Google Scholar]
- 116.Wei XS, Wang XR, Zhang JC, Yang WB, Ma WL, Yang BH, et al. A cluster of health care workers with COVID-19 pneumonia caused by SARS-CoV-2. J Microbiol Immunol Infect. 2020;27:S1684–S1182. doi: 10.1016/j.jmii.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhang J-J, Dong X, Cao Y-Y, Yuan Y-D, Yang Y-B, Yan Y-Q, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 118.Choi YJ, Park JY, Lee HS, Suh J, Song JY, Byun MK, et al. Effect of asthma and asthma medication on the prognosis of patients with COVID-19 Eur Respir J[online ahead of print] 25 Sep 2020 [DOI] [PMC free article] [PubMed]
- 119.Choi HG, Wee JH, Kim SO, Kim JH, Kim HI, Park JY, et al. Association between asthma and clinical mortality/morbidity in COVID-19 patients using clinical epidemiologic data from Korean Disease Control and Prevention Allergy[online ahead of print] 28 Nov 2020
- 120.Lee S, Kim T, Lee E, Lee C, Kim H, Rhee H, et al. Clinical course and molecular viral shedding among asymptomatic and symptomatic patients with SARS-CoV-2 infection in a community treatment center in the Republic of Korea JAMA Intern Med[online ahead of print] 6 Aug 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lee SC, Son KJ, Han CH, Jung JY, Park SC. Impact of comorbid asthma on severity of coronavirus disease (COVID-19) Sci Rep. 2020;10:21805. doi: 10.1038/s41598-020-77791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kim DW, Byeon KH, Kim J, Cho KD, Lee N. The correlation of comorbidities on the mortality in patients with COVID-19: an observational study based on the Korean National Health Insurance Big Data. J Korean Med Sci. 2020;35:e243. doi: 10.3346/jkms.2020.35.e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kim ES, Chin BS, Kang CK, Kim NJ, Kang YM, Choi JP, et al. Korea National Committee for Clinical Management of COVID-19. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean Cohort Study on COVID-19. J Korean Med Sci. 2020;35:e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kim S, Jung CG, Lee JY, Kim G, Choi SW, Jin HJ, et al. Characterization of asthma and risk factors for delayed SARS-CoV-2 clearance in adult COVID-19 inpatients in Daegu Allergy[online ahead of print] 4 Oct 2020 [DOI] [PMC free article] [PubMed]
- 125.Yang JM, Koh HY, Moon SY, Yoo IK, Ha EK, You S, et al. Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol. 2020;146:790–798. doi: 10.1016/j.jaci.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sundaram ME, Calzavara A, Mishra S, Kustra R, Chan AK, Hamilton MA, et al. The individual and social determinants of COVID-19 in Ontario, Canada: a population-wide study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.11.09.20223792v1. [Google Scholar]
- 127.de Souza FSH, Hojo-Souza NS, de Oliveira Batista BD, da Silva CM, Guidoni DL.On the analysis of mortality risk factors for hospitalized covid-19 patients: a data-driven study using the major Brazilian database [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.09.24.20200766v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Porto LC, da Costa CH, Nunes AS, Bouzas I, Ferreira TC, Porto VM, et al. Clinical and laboratory characteristics in outpatient diagnosis of COVID-19 in healthcare professionals in Rio de Janeiro, Brazil [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.22.20217851v1. [DOI] [PubMed] [Google Scholar]
- 129.Sardinha DM, Lima KVB, da Silva Ferreira AL, Garcez JCD, Ueno TMRL, Rodrigues YC, et al. Clinical characteristics of severe acute respiratory syndrome by COVID-19 in indigenous of Brazil [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.11.20128926v1. [Google Scholar]
- 130.Aggarwal A, Shrivastava A, Kumar A, Ali A. Clinical and epidemiological features of SARS-CoV-2 patients in SARI ward of a tertiary care centre in New Delhi. J Assoc Physicians India. 2020;68:19–26. [PubMed] [Google Scholar]
- 131.Goel N, Spalgais S, Mrigpuri P, Khanna M, Menon B, Kumar R.Characteristics of COVID-19 at a non-COVID tertiary pulmonary care centre in Delhi, India Monaldi Arch Chest Dis 2020. 90:688–691. [DOI] [PubMed] [Google Scholar]
- 132.Morshed S, Mosabbir AA, Chowdhury P, Ashadulla SM, Hossain MS.Clinical manifestations of patients with coronavirus disease 2019 (COVID- 19) attending at hospitals in Bangladesh [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.07.30.20165100v2. [Google Scholar]
- 133.Saha A, Ahsan MM, Quader TU, Shohan MUS, Naher S, Dutta P, et al. Characteristics, management and outcomes of critically ill COVID-19 patients admitted to ICU in hospitals in Bangladesh: a retrospective study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.09.24.20201285v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Haw JNL, Uy J, Sy KTL, Abrigo MRM. Epidemiological profile and transmission dynamics of COVID-19 in the Philippines. Epidemiol Infect. 2020;148:e204. doi: 10.1017/S0950268820002137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Higuchi T, Nishida T, Iwahashi H, Morimura O, Otani Y, Okauchi Y, et al. Early clinical factors predicting the development of critical disease in Japanese patients with COVID-19: a single-center, retrospective, observational study J Med Virol[online ahead of print] 14 Oct 2020 [DOI] [PMC free article] [PubMed]
- 136.Uchida Y, Uemura H, Yamaba S, Hamada D, Tarumoto N, Maesaki S, et al. Significance of liver dysfunction associated with decreased hepatic CT attenuation values in Japanese patients with severe COVID-19. J Gastroenterol. 2020;55:1098–1106. doi: 10.1007/s00535-020-01717-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ashinyo ME, Duti V, Dubik SD, Amegah KE, Kutsoati S, Oduro-Mensah E, et al. Clinical characteristics, treatment regimen and duration of hospitalization among COVID-19 patients in Ghana: a retrospective cohort study. Pan Afr Med J. 2020;37:9. doi: 10.11604/pamj.supp.2020.37.1.25718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ombajo LA, Mutono N, Sudi P, Mutua M, Sood M, Loo AMA, et al. Epidemiological and clinical characteristics of COVID-19 patients in Kenya [preprint] medRxiv2020 [accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.11.09.20228106v1. [Google Scholar]
- 139.Otuonye NM, Olumade TJ, Ojetunde MM, Holdbrooke SA, Ayoola JB, Nyam IY, et al. Clinical and demographic characteristics of COVID-19 patients in Lagos, Nigeria: a descriptive study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.09.15.20195412v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Leulseged TW, Hassen IS, Maru EH, Zewde WC, Chamiso NW, Bayisa AB, et al. Characteristics and outcome profile of hospitalized African COVID-19 patients: the Ethiopian context [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.27.20220640v1. [Google Scholar]
- 141.Alizadehsani R, Sani ZA, Behjati M, Roshanzamir Z, Hussain S, Adedini N, et al. Risk factors prediction, clinical outcomes, and mortality in COVID-19 patients J Med Virol[online ahead of print] 28 Nov 2020 [DOI] [PMC free article] [PubMed]
- 142.Shahriarirad R, Khodamoradi Z, Erfani A, Hosseinpour H, Ranjbar K, Emami Y, et al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis. 2020;20:427. doi: 10.1186/s12879-020-05128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Almazeedi S, Al-Youha S, Jamal MH, Al-Haddad M, Al-Muhaini A, Al-Ghimlas F, et al. Characteristics, risk factors and outcomes among the first consecutive 1096 patients diagnosed with COVID-19 in Kuwait. EClinicalMedicine. 2020;24:100448. doi: 10.1016/j.eclinm.2020.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Caliskan T, Saylan B. Smoking and comorbidities are associated with COVID-19 severity and mortality in 565 patients treated in Turkey: a retrospective observational study. Rev Assoc Med Bras (1992) 2020;66:1679–1684. doi: 10.1590/1806-9282.66.12.1679. [DOI] [PubMed] [Google Scholar]
- 145.Satici C, Demirkol MA, Sargin Altunok E, Gursoy B, Alkan M, Kamat S, et al. Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. Int J Infect Dis. 2020;98:84–89. doi: 10.1016/j.ijid.2020.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Trabulus S, Karaca C, Balkan II, Dincer MT, Murt A, Ozcan SG, et al. Kidney function on admission predicts in-hospital mortality in COVID-19. PLoS One. 2020;15:e0238680. doi: 10.1371/journal.pone.0238680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Green I, Merzon E, Vinker S, Golan-Cohen A, Magen I.COVID-19 susceptibility in bronchial asthma J Allergy Clin Immunol Pract[online ahead of print] 24 Nov 2020 [DOI] [PMC free article] [PubMed]
- 148.Israel A, Schaffer AA, Cicurel A, Feldhamer I, Tal A, Cheng K, et al. Large population study identifies drugs associated with reduced COVID-19 severity [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.10.13.20211953v2. [Google Scholar]
- 149.Israel A, Feldhamer E, Lahad A, Levin-Zamir D, Lavie G.Smoking and the risk of COVID-19 in a large observational population study [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.06.01.20118877v2. [Google Scholar]
- 150.Shabrawishi M, Al-Gethamy MM, Naser AY, Ghazawi MA, Alsharif GF, Obaid EF, et al. Clinical, radiological and therapeutic characteristics of patients with COVID-19 in Saudi Arabia. PLoS One. 2020;15:e0237130. doi: 10.1371/journal.pone.0237130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rosenthal JA, Awan SF, Fintzi J, Keswani A, Ein D. Asthma is associated with increased risk of intubation but not hospitalization or death in coronavirus disease 2019. Ann Allergy Asthma Immunol. 2021;126:93–95. doi: 10.1016/j.anai.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Robinson LB, Fu X, Bassett IV, Triant VA, Foulkes AS, Zhang Y, et al. COVID-19 severity in hospitalized patients with asthma: a matched cohort study. J Allergy Clin Immunol Pract. 2021;9:497–500. doi: 10.1016/j.jaip.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bisso IC, Huespe I, Lockhart C, Masso A, Anaya JG, Hornos M, et al. Clinical characteristics of critically ill patients with COVID-19 [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.12.09.20246413v1. [Google Scholar]
- 154.Baqui P, Bica I, Marra V, Ercole A, van der Schaar M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Health. 2020;8:e1018–e1026. doi: 10.1016/S2214-109X(20)30285-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Atkins JL, Masoli JAH, Delgado J, Pilling LC, Kuo C-L, Kuchel GA, et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J Gerontol A Biol Sci Med Sci. 2020;75:2224–2230. doi: 10.1093/gerona/glaa183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Murillo-Zamora E, Hernandez-Suarez CM.Survival in adult inpatients with COVID-19 Public Health[online ahead of print] 10 Nov 2020 [DOI] [PMC free article] [PubMed]
- 157.Pujadas E, Chaudhry F, McBride R, Richter F, Zhao S, Wajnberg A.SARS-CoV-2 viral load predicts COVID-19 mortality Lancet Respir Med[online ahead of print] 8 Sep 2020 [DOI] [PMC free article] [PubMed]
- 158.Santos MM, Lucena EES, Lima KC, Brito AAC, Bay MB, Bonfada D. Survival and predictors of deaths of patients hospitalised due to COVID-19 from a retrospective and multicentre cohort study in Brazil. Epidemiol Infect. 2020;148:e198. doi: 10.1017/S0950268820002034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.US Centers for Disease Control and Prevention National Health Interview Survey data Atlanta, Georgia: Centers for Disease Control and Prevention; 2018[accessed 2020 Oct 29]. Available from: https://www.cdc.gov/asthma/nhis/2018/table4-1.htm [Google Scholar]
- 160.US Centers for Disease Control and Prevention Asthma in New York state Atlanta, Georgia: Centers for Disease Control and Prevention; 2018[accessed 2020 Oct 29]. Available from: https://www.cdc.gov/asthma/stateprofiles/Asthma_in_NYS.pdf [Google Scholar]
- 161.Selroos O, Kupczyk M, Kuna P, Łacwik P, Bousquet J, Brennan D, et al. National and regional asthma programmes in Europe. Eur Respir Rev. 2015;24:474–483. doi: 10.1183/16000617.00008114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Carrillo G, Mendez-Domínguez N, Datta-Banik R, Figueroa-Lopez F, Estrella-Chan B, Alvarez-Baeza A, et al. Asthma mortality and hospitalizations in Mexico from 2010 to 2018: retrospective epidemiologic profile. Int J Environ Res Public Health. 2020;17:5071. doi: 10.3390/ijerph17145071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, et al. China Pulmonary Health (CPH) Study Group. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. 2019;394:407–418. doi: 10.1016/S0140-6736(19)31147-X. [DOI] [PubMed] [Google Scholar]
- 164.Kim S, Kim J, Kim K, Kim Y, Park Y, Baek S, et al. Healthcare use and prescription patterns associated with adult asthma in Korea: analysis of the NHI claims database. Allergy. 2013;68:1435–1442. doi: 10.1111/all.12256. [DOI] [PubMed] [Google Scholar]
- 165.Wang L, Foer D, Bates DW, Boyce JA, Zhou L. Risk factors for hospitalization, intensive care, and mortality among patients with asthma and COVID-19. J Allergy Clin Immunol. 2020;146:808–812. doi: 10.1016/j.jaci.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Antonicelli L, Tontini C, Manzotti G, Ronchi L, Vaghi A, Bini F, et al. Severe asthma in adults does not significantly affect the outcome of COVID-19 disease: results from the Italian Severe Asthma Registry Allergy[online ahead of print] 14 Aug 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Izquierdo JL, Almonacid C, Gonzalez Y, Del Rio-Bermudez C, Ancochea J, Cardenas R, et al. The impact of covid-19 on patients with asthma [preprint] medRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.medrxiv.org/content/10.1101/2020.07.24.20161596v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.World Health Organization Global COVID-19: Spain Geneva, Switzerland: World Health Organization; 2020[updated 2021 Feb 2; accessed 2020 Oct 29]. Available from: ]https://covid19.who.int/region/euro/country/es [Google Scholar]
- 169.Auvinen R, Nohynek H, Syrjänen R, Ollgren J, Kerttula T, Mäntylä J, et al. Comparison of the clinical characteristics and outcomes of hospitalized adult COVID-19 and influenza patients - a prospective observational study. Infect Dis (Lond) 2021;53:111–121. doi: 10.1080/23744235.2020.1840623. [DOI] [PubMed] [Google Scholar]
- 170.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Halpin DMG, Singh D, Hadfield RM. Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective. Eur Respir J. 2020;55:2001009. doi: 10.1183/13993003.01009-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Maes T, Bracke K, Brusselle GG. COVID-19, asthma, and inhaled corticosteroids: another beneficial effect of inhaled corticosteroids? Am J Respir Crit Care Med. 2020;202:8–10. doi: 10.1164/rccm.202005-1651ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ma X, Wang L, Liu L, Yang C, Gai Z.Is asthma an exclusionary condition for SARS-CoV-2 infection in China? -the relationship between asthma and COVID-19 J Asthma[online ahead of print] 4 Aug 2020 [DOI] [PubMed] [Google Scholar]
- 174.Carli G, Cecchi L, Stebbing J, Parronchi P, Farsi A.Is asthma protective against COVID-19? Allergy[online ahead of print] 1 Jun 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Matsuyama S, Kawase M, Nao N, Shirato K, Ujike M, Kamitani W, et al. The inhaled corticosteroid ciclesonide blocks coronavirus RNA replication by targeting viral NSP15 [preprint] bioRxiv 2020[accessed 2020 Dec 29]. Available from: https://www.biorxiv.org/content/10.1101/2020.03.11.987016v1. [Google Scholar]
- 176.Kimura H, Kurusu H, Sada M, Kurai D, Murakami K, Kamitani W, et al. Molecular pharmacology of ciclesonide against SARS-CoV-2. J Allergy Clin Immunol. 2020;146:330–331. doi: 10.1016/j.jaci.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Szklo M, Jieto FJ. Epidemiology: beyond the basics. 4th ed. Burlington, MA: Jones & Bartlett Learning; 2019. Medical surveillance (or detection) bias; pp. 153–154. [Google Scholar]
- 178.Qin L, Zhang C, Yue J, Xie M. Reply. J Allergy Clin Immunol. 2020;146:335–336. doi: 10.1016/j.jaci.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Fang L, Gao P, Bao H, Tang X, Wang B, Feng Y, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. 2018;6:421–430. doi: 10.1016/S2213-2600(18)30103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Tennant JP. The state of the art in peer review. FEMS Microbiol Lett. 2018;365:fny204. doi: 10.1093/femsle/fny204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.