Abstract
Background
Coping strategies play a key role in modulating the physical and psychological burden on caregivers of stroke patients. The present study aimed to determine the relationship between the severity of burden of care and coping strategies amongst a sample of Iranian caregivers of older stroke patients. It also aimed to examine the differences of coping strategies used by male and female caregivers.
Methods
A total of 110 caregivers of older patients who previously had a stroke participated in this descriptive and cross-sectional study. The Zarit Burden Interview and Lazarus coping strategies questionnaires were used for data collection. Questionnaires were completed by the caregivers, who were selected using convenience sampling. The collected data were analyzed using Pearson's correlations and independent t-tests.
Results
The mean age of participants was 32.09 ± 8.70 years. The majority of the caregivers sampled reported mild to moderate (n = 74, 67.3%) burden. The most commonly used coping strategies reported were positive reappraisal and seeking social support. Results of the independent t-test showed that male caregivers used the positive reappraisal strategy (t(110) = 2.76; p = 0.007) and accepting responsibility (t(110) = 2.26; p = 0.026) significantly more than female caregivers. Pearson’s correlations showed a significant positive correlation between caregiver burden and emotional-focused strategies, including escaping (r = 0.245, p = 0.010) and distancing (r = 0.204, p = 0.032).
Conclusions
Caregivers with higher burden of care used more negative coping strategies, such as escape-avoidance and distancing. In order to encourage caregivers to utilize effective coping skills, appropriate programs should be designed and implemented to support caregivers. Use of effective coping skills to reduce the level of personal burden can improve caregiver physical health and psychological well-being.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-021-00556-z.
Keywords: Aged, Stroke, Caregiver, Burden of care, Coping strategies
Background
The world’s older population is projected to continue to grow at an unprecedented rate due to improvement in life expectancy and health care techniques [1]. Aging is a period of life in which older people are exposed to potential threats such as chronic conditions, loneliness, isolation, lack of social support, and a decline in independence [2, 3]. Additionally, both physical and psychological (e.g., dementia) chronic diseases tend to become more common with age [3]. Aging is a well-known risk factor for the increase of multiple chronic diseases, including cardiovascular disease, stroke, cancer, osteoarthritis, and dementia [4]. Approximately 80% of older adults have at least one chronic disease; the cost and duration of treatment for these diseases is 20–30 times higher than acute illnesses [2].
One of the major health problems among older adults is stroke, which is the third leading cause of death in the world after cardiovascular diseases and cancer [5, 6]. Stroke is one of the most severe neurological disorders which results from a decrease in cerebral blood flow in certain parts of the brain due to vascular injuries [7]. It is one of the most debilitating neurological conditions that cause chronic and severe disabilities [8, 9]. Stroke patients are very often dependent on their families for their physical and emotional needs after discharge from the hospital [10]. Given that patients often need long-term care, the role of home caregivers is critically important [11].
Essential caregiving for stroke survivors plays an important role in the recovery process, and in preventing additional strokes and improving patients’ overall health [12]. Informal, or home caregivers are critical for long-term care and are often composed of family members, friends, and relatives [13]. Informal caregivers are defined as individuals who provide some type of unpaid, ongoing assistance with activities of daily living or instrumental activities of daily living for individuals with a chronic illness or disability [14]. Oftentimes, one individual serves as the primary caregiver and is assigned to be primarily responsible for most of the physical care and supervision [15]. Caregiving is a difficult task, particularly for untrained primary caregivers who are taking care of an individual with serious, chronic health problems [16]. Unsurprisingly, caregiver stress is common and is caused by the ongoing emotional and physical strain of caregiving [17].
Caregiver burden can be defined as the strain that is experienced by a person who cares for a chronically ill, disabled, or older family member [18]. The burden of care is used to describe the side effects of care that are extremely problematic for the patients and their families [19]. It is a multidimensional response to physical, psychological, emotional, social, and financial stressors associated with the caregiving experience [20, 21]. Caregivers are hidden patients who, as a result of their involvement with caregiving responsibilities, may not be able or eager to seek care for their own health needs [22]. Caregiver burden and strain have been associated with increased health-risk behaviors (such as smoking) and higher rates of drug use [23]. Caregiver mental health can be even more at risk when caregivers perceive that the patient's care needs exceed their caregiving capabilities [10]. Most studies of family caregivers of stroke survivors have reported that caregiving had negative impacts on the caregivers’ health and well-being [24, 25]. Due to the abrupt onset of disability and the chronic nature of stroke recovery, caring for a stroke survivor has been found to have a negative impact on the physical, mental, and psychological health of caregivers [26, 27]. Primary caregivers of stroke patients tend to report more somatic and depressive symptoms, sleep disorders, stress and social isolation than general population [28].
Support is needed to enable informal caregivers to continue in their role as long as possible, without compromising their physical or mental health. Effective and adaptive coping strategies may play a protective role in reducing the caregiver's distress [29]. According to Lazarus and Folkman et al. [30], coping is a process that addresses how people respond and act both when experiencing stress and when the level of exposure to stress rises. Coping strategies are the cognitive and behavioral efforts of individuals to interpret and overcome problems and challenges [31, 32]. It has been proposed that females and males use different coping strategies to deal with stressors [33]. Previous studies about gender differences in the use of coping strategies showed that differences in preferred coping strategies existed [34–36].
Coping strategies have been conceptualized in a variety of ways in the literature, however more broadly, they have been considered to fall into two main categories: problem-focused and emotion-focused [37]. Problem-focused coping strategies aim to change the situation and take control of the source of stress. They involve evaluating the source of stress and actively considering and implementing potential solutions to reduce the aversive effects of the stressor [38, 39]. On the other hand, emotion-based coping involves emotional response to stressors. Emotion-focused coping strategies can also entail enlisting emotional support from others [40].
Eight ways of coping are identified based on the ways of coping (WOC) Questionnaire by the Folkman and Lazarus. These include: Confrontive Coping and Planful Problem-Solving classified under problem-focused coping, and Distancing, Self-Controlling, Accepting Responsibility, Positive Reappraisals, and Escape-Avoidance considered to be emotion-focused coping. The coping strategy of Seeking Social Support functions as both problem and emotion-focused coping.
Confrontive coping refers to the aggressive effort to modify stressful situations while planful problem solving involves analytic approach to providing solutions to problems [41]. Detaching oneself from stressful situations is described as distancing and this strategy may be common for caregivers who do not feel they have the coping resources to face a particular scenario they find confronting [30]. Distancing relates to denial, distracting, or detaching [42]. This may be seen when a family member is diagnosed with a stroke where a caregiver may turn to distractions to avoid acknowledging the problem.
Self-controlling is the individual’s effort to manage their own emotions and actions. Accepting responsibility involves acknowledging one’s contribution to the problem and doing the right thing [43, 44]. For caregivers this can be considered an adaptive and useful coping strategy. Accepting the situation and acknowledging they are in control of how they can respond and cope to it can be an important part of managing news of a stroke. This may assist with managing negative psychological sequalae that may result to death-related depression or anxiety as well as preparatory grief and loss [45–48].
Another coping strategy that is focused on positively interpreting situations is positive reappraisal, wherein thinking about stressful event may be re-framed to be considered as benign, valuable, or beneficial [43, 44]. It is often associated with personal growth and some religious dimensions [32]. For caregivers, positive appraisal may involve considering stroke as unavoidable or inevitable. They may consider the situation as fortunate in that it did not result in death. Unlike hope and optimism [49–53], reappraisal-type strategies are often used in cognitive behaviour therapy [54] and could be seen as a productive and rational coping strategy.
Escape-avoidance is described as the thoughts and behavioral efforts to escape stressful situations or problems [47]. This may involve actively avoiding the problem or withdrawing from others or the situation causing stress. It can also involve wishful thinking. Escape-avoidance and distancing can have negative implications on a person being cared for [42]. A caregiver who withdraws support and care can either physically or psychology, place people with a chronic disease or injury at great risk.
Seeking social support is a commonly used adaptive coping strategy which refers to sharing feelings and thoughts, or seeking care, resources, or emotional support from others [55, 56]. Caregivers may seek social support from family or friends, or elicit information from professionals which can be a form of social support as well [57]. Social support and intergenerational contact has been found to be essential for health outcomes in older adults, ageing, and ageism [58].
Despite the high prevalence rates of stroke in Iran [59] and caregiving responsibilities of family members [60] as well as the reported negative impacts of caregiving on caregiver health status, psychological problems, and the quality of life of caregivers [61], only few studies have examined the coping strategies adopted by caregivers of stroke patients in Iran. Therefore, the aim of this study was to determine the relationships between caregiving burden and coping strategies used by a group of caregivers of older patients with a history of having a stroke to better understand this area of healthcare.
We aimed to answer the following questions:
What is the level of care burden in caregivers of older patients with a stroke?
What are the most common coping strategies used by caregivers of older patients with a stroke?
What kind of relationship is there between care burden and coping strategies in caregivers of older patients with a stroke?
Do coping strategies used differ based on the gender of the caregiver?
Methods
This cross-sectional and correlational study was conducted on 110 caregivers of older patients with a history of stroke. The convenience sampling method was used for selecting the representative sample. To identify the caregivers, medical files of stroke patients hospitalized in the Valiasr hospital in the six-month period before the start of the study were extracted and reviewed. Contact information for the caregivers of stroke patients was extracted from the files, and they were then called for the initial screening. Valiasr hospital is the only hospital in Zanjan, Iran that admits stroke patients.
Inclusion criteria for primary caregivers included a willingness to participate, aged 18 years old or over, being able to communicate, having at least a primary level education, being the principal caregiver for a minimum of 1 month, not being paid for the care provided, and having a family relationship with the older patient. Caregivers who were caring for multiple patients were not considered for inclusion in this study. Older patients who were included in the study are 60 years old and above, have been diagnosed with stroke, and have a family caregiver. Those who met the inclusion criteria based on their report were invited to come to the rehabilitation centers or clinic of neurology, depending on the region where they resided. At the time of the phone call, an explanation about the study purpose and procedures were provided to the potential participants.
It was determined that 100 participants were needed to find a correlation coefficient (r = 0.25) between care burden and coping strategies, extracted from a similar study by Alnazly et al. [34], at an alpha level of 0.05, and 90% power. By considering a 10% nonresponsive rate, a sample size of 110 caregivers was finalized for this study.
Data collection was carried out from December 2017 to May 2018. The questionnaires were completed by the primary caregivers of the older patients.
Instruments
Zarit Burden Interview (ZBI), Lazarus coping strategies questionnaires, and demographic checklists were used to gather the data.
The ZBI questionnaire was used to measure caregiving burden. It is the most widely used instrument to assess perceived caregiving burden in clinical and research settings [62], which measures the physical, emotional-psychological, social, and economic impacts of caregiving. This questionnaire is consists of 22 items and is scored on a five-point Likert scale where 0 = “never” and 4 = “nearly always.” The total ZBI score ranges from 0 to 88 points. Higher scores indicate greater burden [63]. The ZBI is a validated instrument for Iranian populations. Navidian et al. [64] have culturally adjusted this scale; its congruent validity was confirmed with a positive correlation with the Hamilton anxiety scale (r = 0.89) and Beck depression inventory (r = 0.67).
The Lazarus coping strategies questionnaire [30] consists of 66 questions about coping with a stressful situation. Responses are given on a 4-point Likert scale, ranging from 0 = “does not apply and/or not used” to 3 = “used a great deal.” It measures 8 subscales consisting of confrontive coping (6 questions), distancing (6 questions), self-controlling (7 questions), seeking social support (6 questions), accepting responsibility (4 questions), escape-avoidance (8 questions), problem-solving (6 questions), and positive reappraisal (7 questions). The remaining questions are distractor items. Higher scores in each subscale indicate greater use of that particular coping strategy [65]. The Lazarus coping strategies questionnaire was validated in Iranian students [66]. Internal consistency of this questionnaire is high (Cronbach's alpha = 0.85) as confirmed by Ramzi et al. [67].
Demographic characteristics for caregivers included age, gender, marital status, educational level, financial status, job, and history of chronic illnesses. Demographic characteristics for the older patients included age, gender, marital status, and level of education.
Ethical considerations
All stages of the study were based on the Provisions of the Declaration of Helsinki of 1975. After giving information about the purpose and procedure of the study and prior to completing the questionnaires, written informed consent forms were signed by all the caregivers. The study was approved by the Ethics Committee of Qazvin University of Medical Sciences, Qazvin, Iran (IR.QUMS.REC. 1396.371).
Statistical analysis
All statistical analyses were conducted using the Statistical Package for Social Science version 19 (SPSS IBM V.19, New York). Descriptive statistics were used to report the characteristics of the caregivers and the severity of burden of care. Continuous variables were presented as mean and standard deviations and categorical data were reported using frequencies and percentages.
Pearson’s correlations were used to examine the association between caregiver burden and coping strategies. Differences in the mean scores of coping strategies scales for gender were analyzed using independent t-tests. The statistical significance level was set at p < 0.05.
Results
A total of 110 caregivers with mean age of 32.09 ± 8.80 years participated in this descriptive and cross-sectional study. Caregivers were predominately women (n = 77, 70.0%), married (n = 75, 68.2%), unemployed (n = 76, 79.1%), and had children (n = 67, 60.9%). Nearly half of the sample had a diploma or academic education (n = 56, 50.9%) and had a self-reported middle‑range income (n = 60, 54.5%). Nearly 90% of the caregivers reported not having any chronic diseases.
The mean age of care recipients was 69.91 ± 10.50 years old. More than half were female (n = 57, 51.8%), the majority were married (n = 82, 74.5%), and illiterate (n = 82, 74.5%; see Table 1).
Table 1.
Sociodemographic characteristics of caregivers of older patients with stroke
| Demographic characteristics | n | % |
|---|---|---|
| Sex | ||
| Female | 77 | 70.0 |
| Male | 33 | 30.0 |
| Marital status | ||
| Married | 75 | 68.2 |
| Single | 35 | 31.8 |
| Job | ||
| Unemployed | 76 | 79.1 |
| Retired | 4 | 3.6 |
| Employed | 30 | 27.3 |
| Children | ||
| 0 | 43 | 39.1 |
| 1 | 29 | 26.4 |
| ≥ 2 | 38 | 34.5 |
| Education level | ||
| Illiterate | 6 | 5.5 |
| Under diploma | 48 | 43.6 |
| Diploma or higher | 56 | 50.9 |
| Financial status | ||
| Low | 33 | 30.0 |
| Middle | 60 | 54.5 |
| High | 17 | 15.5 |
| History of chronic illnesses | ||
| Yes | 12 | 10.9 |
| No | 98 | 89.1 |
The mean of caregiving burden was 32.80 ± 11.97. The majority of the caregivers suffered from mild (n = 58, 52.7%) to moderate (n = 51, 46.4%) burden and just one caregiver (0.9%) was under severe burden. The results showed that the most common coping strategies used were positive reappraisal (15.16 ± 5.18) and seeking social support (8.58 ± 2.90), and the least were direct confronting (6.58 ± 2.70) and escape-avoidance (14.37 ± 4.98). The greatest caregiver burden was physical burden (15.49 ± 5.06) and the least was social burden (4.68 ± 3.56) (see Table 2).
Table 2.
Means and standard deviations of the subscales of burden and coping strategies
| Variable | Subscales | Mean ± SD | Mean/number of items |
|---|---|---|---|
| Burden care | Physical | 15.49 ± 5.06 | 1.70 |
| Emotional | 9.83 ± 4.60 | 1.40 | |
| Economic | 2.79 ± 2.20 | 1.39 | |
| Social | 4.68 ± 3.56 | 1.17 | |
| Total | 32.79 ± 15.42 | 19.59 | |
| Coping strategies | Positive reappraisal | 15.16 ± 5.18 | 1.51 |
| Seeking social support | 8.58 ± 2.90 | 1.43 | |
| Problem-solving | 12.45 ± 4.28 | 1.38 | |
| Self-controlling | 12.28 ± 4.13 | 1.36 | |
| Accepting responsibility | 7.90 ± 2.94 | 1.31 | |
| Distancing | 8.15 ± 3.14 | 1.16 | |
| Confronting | 6.85 ± 2.70 | 1.14 | |
| Escape-avoidance | 14.37 ± 4.98 | 1.10 | |
| Total | 85.75 ± 19.25 | 10.39 |
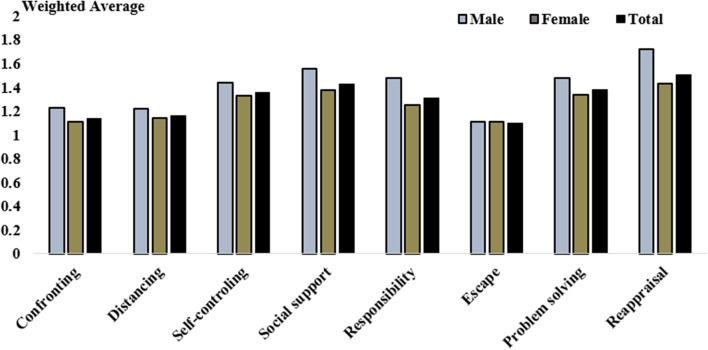
Figure 1 shows the average range of coping strategies used amongst caregivers of older patients with a history of stroke based on gender. Results of the independent t-test showed that male caregivers used the positive reappraisal strategy (t(108) = 2.76; p = 0.007) and accepting responsibility (t(108) = 2.26; p = 0.026) significantly more than female caregivers.
Fig. 1.
Weighted average of subscales of coping strategies among caregivers of elderly patients with stroke
The information displayed in Table 3 shows that the burden of care was significantly and positively correlated with use of the escape-avoidance coping strategy (r = 0.245, p = 0.010) and distancing coping strategy (r = 0.204, p = 0.032).
Table 3.
Associations between caregiving burden and coping strategies and its subscales
| Reappraisal | Problem solving | Escape | Responsibility | Social support | Self-controlling | Distancing | Confronting | Coping strategy (total) | |
|---|---|---|---|---|---|---|---|---|---|
| Caregiving burden | |||||||||
| r | 0.183 | 0.078 | 0.245 | 0.156 | 0.165 | 0.052 | 0.204 | 0.102 | 0.238 |
| p values | 0.055 | 0.420 | 0.010 | 0.103 | 0.085 | 0.586 | 0.032 | 0.291 | 0.012 |
Bold indicates statistically significant associations (p < 0.05)
Discussion
Coping strategies are common ways for dealing with demands and in situations that are perceived as threatening [68]. Therefore, the present study aimed to determine the associations between caregiving burden and use of coping strategies among caregivers of older patients with a history of stroke. It also sought to determine the differences in coping strategies used by male and female caregivers.
The present study findings revealed that the care burden reported by the majority of caregivers of stroke survivors was mild to moderate. The findings are partially supported by Kumar et al. [16] who reported that 63% of caregivers of patients with stroke suffered from mild to moderate care burden. However, Rawat et al. [69] reported that more than half (56.67%) of stroke caregivers felt exhausted (high/extreme burden). The reason for these different results in the care burden of caregivers of stroke patients may be related to the degree of dependence of the patients for the daily living activities. In this regard, Baumann et al. [70] found that a decrease in patients’ ability to perform daily activities was significantly associated with an increase in the care burden of caregivers of stroke patients.
Based on the results of this study, women compromised a large majority of caregivers. This is consistent with national [71, 72] and international [73–75] studies which have found that most caregivers are women. A possible explanation for this might be that women believe that caregiving is their role and responsibility, as caregiving of children and other family members is often undertaken by women. Furthermore, women are more emotional than men and are willing to sacrifice their social life for their family [72], and they request little assistance from others, even if social support is available [76]. The results of the present study did not find any differences between men and women in the burden of caregiving. Although other studies have not detected any significant relationship between gender and caregiver burden even across different types of burden [77, 78], some previous studies have reported that female caregivers experience more caregiver burden than their male counterparts [74, 79]. This discrepancy may be related to Iranian culture, where women believe that caregiving is their duty and is expected of them from family members and society.
The results showed that caregivers used more positive reappraisal and social support. Likewise, Alnazly [34] showed that caregivers of dialysis patients used more self-control and positive reappraisal. Ayuarno et al. [29] also found that caregivers of patients with Alzheimer’s disease were more likely to use emotion-focused strategies [80]. Similarly, García-Alberca et al. [81] reported that the use of emotion-focused or problem-solving coping strategies is significantly associated with the level of psychological distress in Alzheimer disease caregivers. Papastavrou et al. [82] also found that the type of coping strategy used among caregivers of cancer patients is related to the levels of care burden. Furthermore, coping strategies are typically related to the task/problem that the caregiver is facing [83].
The results of this study showed that male caregivers were more likely to use the strategies of positive reappraisal and accepting responsibility compared to female caregivers. Consistent with the results of this study, Hassan et al. [35] reported that male caregivers of patients with schizophrenia were more likely to use reappraisal coping strategies than their female counterparts. However, Alnazly [34] found that male caregivers of patients undergoing hemodialysis used distancing more than women caregivers. In addition, Suriyamoorthi et al. [36] showed that male caregivers of patients with bipolar disorder used self-distraction and substance use as coping strategies while females used religion and denial. These different results may be related to the type of care needed based on the differences in patients’ illnesses.
Based on the results of the present study, caregivers with higher care burden used more emotion-focused strategies such as escape-avoidance and distancing. The results of many previous studies are in line with this result. Kumar et al. [68] reported that caregivers of stroke patients under greater burden used emotion-focused coping strategies. Abbasi et al. [83] also showed that there was a direct and significant relationship between the use of emotion-focused coping skills and increasing care burden of the caregivers of cancer patients. As caregivers with high burden care did not adopt appropriate coping strategies and tended to employ emotion-focused coping [82, 84]. In other words, increasing the burden of care beyond the caregiver’s ability can result in reliance on less effective emotion-based strategies rather than more effective problem-focused coping strategies and consulting with others [85].
Limitations
The present study includes a few limitations. This study only focused on caregivers of older patients with a history of stroke. As the literature shows a variety of other coping strategies are used depending on the type of illness present, the findings cannot be extended to caregivers of all older patients. Second, since this study was conducted on Iranian caregivers, it may be difficult to extend the findings to other countries or cultures. Third, convenience sampling was used, which reduces generalizations to all caregivers of older patients with a history of stroke. Fourth, the limited sample size of the male caregivers (N = 33) may not have been sufficient to find other statistical differences across the subscales. Finally, the nature of the study and the type of analyses used limit the findings to associations and not causal influence.
Conclusion
Caregivers adopted varied types of coping strategies to overcome burden and the adoption of coping strategies was associated with the severity of burden in caregivers of stroke patients. The informal caregivers with higher burden of care used emotion-focused strategies which often do not help in reducing caregiver stress. As such, training programs that teach caregivers efficient coping strategies are needed in order to increase their use of effective and healthy coping strategies. Furthermore, psychosocial support should be provided by governmental and nongovernmental organizations to reduce the care burden of caregivers of older stroke patients.
Supplementary Information
Additional file 1: Caregivers burden and coping strategies. SA Motalebi, Sup. data.
Acknowledgements
We wish to thank the participants of this study without whom the study would not have been accomplished.
Abbreviations
- WOC
Ways of coping
- ZBI
Zarit Burden Interview
Authors' contributions
AK, SAM, JA and KAA conceived and designed the research method and helped to draft the manuscript. AK collected the data. MM performed the statistical analysis. AK, SAM, and KAA revised the manuscript. All authors read and approved the final manuscript.
Funding
This article was extracted from a self-financed master thesis in geriatric nursing.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [supplementary file:SPSS file].
Declarations
Ethics approval and consent to participate
The study was approved by the by the Ethics Committee of Qazvin University of Medical Sciences, Qazvin, Iran (IR.QUMS.REC. 1396.371). Prior to completing the questionnaires, written informed consent forms were signed by all the caregivers.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Peiman H, Yaghoubi M, Seyed Mohammadi A, Delpishe A. Prevalence of chronic diseases in the elderly in Ilam. Iran J Ageing. 2012;6(4):7–13. [Google Scholar]
- 2.Habibi A, Nemadi-Vosoughi M, Habibi S, Mohammadi M. Quality of life and prevalence of chronicillnesses among elderly people: a cross-sectional survey. J health. 2012;3(1):58–66. [Google Scholar]
- 3.Fassih-Ramandi Z, Soleimani MA, Allen K-A, Gorgulu O, Motalebi SA. Validity and reliability of the flourishing scale in a sample of older adults in Iran. Clin Interv Aging. 2020;15:673–681. doi: 10.2147/CIA.S251067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atella V, Piano Mortari A, Kopinska J, Belotti F, Lapi F, Cricelli C, et al. Trends in age-related disease burden and healthcare utilization. Aging Cell. 2019;18(1):e12861. doi: 10.1111/acel.12861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nikookar R, Ghaffari S, Akbari Kamrani AA, Sahaf R, Moghadam M, Ghadimi MR. Assessing the duration of unnecessary hospitalization and expenses in older individuals suffering from cerebral vascular accident in the chronic care unit. Iran J Ageing Salmand. 2015;10(2):180–187. [Google Scholar]
- 6.Ilali E, Taraghi Z, Yazdani J, Golmohammadi M, Savasari R, Mosavi JA. The relationship between praying and spiritual health among Iranian older people with cerebrovascular accidents. Iran J Ageing. 2016;11(3):424–431. [Google Scholar]
- 7.Tajvidi M, Dalvandi A, Sahaf R, Rahgozar M. Relationship between general health and demographic characteristics of family caregivers of stroke survivors. Iran J Ageing. 2018;12(4):494–505. [Google Scholar]
- 8.Johnson CO, Nguyen M, Roth GA, Nichols E, Alam T, Abate D, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439–458. doi: 10.1016/S1474-4422(19)30034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King RB, Hartke RJ, Lee J, Raad J. The stroke caregiver unmet resource needs scale: development and psychometric testing. J Neurosci Nurs. 2013;45(6):320–328. doi: 10.1097/JNN.0b013e3182a3ce40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahmani Anaraki H, Mahmoodi GR, Rouhi G, Asayesh H, Nasiri H, Rakhshani H. General health status of neurologic patients’ caregivers and the related factors. J Res Dev Nurs Midwif. 2013;9(2):49–55. [Google Scholar]
- 11.Kheirollahi N, Khatiban M, Oshvandi K, Alhani F, Faradmal J. The effect of family-centered empowerment intervention on perceived severity of threat in caregivers of patients with stroke: a semi experimental study. J Neurosci Nurs. 2014;22(3):74–82. [Google Scholar]
- 12.Aldehaim AY, Alotaibi FF, Uphold CR, Dang S. The impact of technology-based interventions on informal caregivers of stroke survivors: a systematic review. Telemed e-Health. 2016;22(3):223–231. doi: 10.1089/tmj.2015.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khatti Dizabadi F, Yazdani J, Eftekhar Ardebili H, Batebi A, Shojaezadeh D. The status of caregiving among informal caregivers of community-dwelling elderly. J Mazandaran Univ Med Sci. 2013;23(100):31–41. [Google Scholar]
- 14.Plöthner M, Schmidt K, De Jong L, Zeidler J, Damm K. Needs and preferences of informal caregivers regarding outpatient care for the elderly: a systematic literature review. BMC Geriatr. 2019;19(1):1–22. doi: 10.1186/s12877-019-1068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farhadi A, Foroughan M, Mohammadi F, Rassouli M, Sadegh Moghadam L, Nazari Sh, et al. Caregiving appraisal in family caregivers of older adults. Iran J Ageing Salmand. 2016;11(1):8–19. doi: 10.21859/sija-110108. [DOI] [Google Scholar]
- 16.Kumar R, Kaur S, Reddemma K. Burden and coping strategies in caregivers of stroke survivors. J Neurol Neurosci. 2015;1:1–5. [Google Scholar]
- 17.Penning MJ, Wu Z. Caregiver stress and mental health: impact of caregiving relationship and gender. Gerontologist. 2016;56(6):1102–1113. doi: 10.1093/geront/gnv038. [DOI] [PubMed] [Google Scholar]
- 18.Rohani H, Eslami AA, Jafari-Koshki T, Raei M, Abrishamkarzadeh H, Mirshahi R, et al. The factors affecting the burden of care of informal caregivers of the elderly in Tehran. J Kermanshah Univ Med Sci J Kermanshah Univ Med Sci. 2014;18(12):726–733. [Google Scholar]
- 19.Alizadeh M, Hoseini M, Shojaeizadeh D, Rahimi A, Arshinchi MHR. Assessing anxiety, depression and psychological wellbeing status of urban elderly under represent of Tehran metropolitan city Iran. J Ageing Salmand. 2012;7(3):66–73. [Google Scholar]
- 20.Haresabadi M, Bibak B, Hosein Zadeh E, Bayati M, Arki M, et al. Assessing burden of family caregivers of patients with schizophrenia Admitted in Imam Reza hospital-Bojnurd 2010. J N Khorasan Univ Med Sci. 2010;4(2):165–71. [Google Scholar]
- 21.Veenstra C. Management of cancer in the older patient. JAMA. 2012;307(19):2106–2107. doi: 10.1001/jama.2012.4814. [DOI] [Google Scholar]
- 22.Ghada M, Mourad Rania A, Zaki Rasmia A. Improving coping abilities among caregivers of patients with cerebrovascular stroke. J Educ Pract. 2014;5(36):8–19. [Google Scholar]
- 23.Reinhard SC, Given B, Petlick NH, Bemis A. Supporting family caregivers in providing care. Patient safety and quality: an evidence-based handbook for nurses: agency for Healthcare Research and Quality (US); 200. [PubMed]
- 24.Haley WE, Roth DL, Hovater M, Clay OJ. Long-term impact of stroke on family caregiver well-being: a population-based case-control study. Neurology. 2015;84(13):1323–1329. doi: 10.1212/WNL.0000000000001418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart DE. Stroke survivors’ behavioral and psychologic symptoms are associated with informal caregivers’ experiences of depression. Arch Phys Med Rehabil. 2006;87(2):177–183. doi: 10.1016/j.apmr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Costa TFd, Costa KNdFM, Martins KP, Fernandes MdGdM, Brito SdS. Burden over family caregivers of elderly people with stroke. Escola Anna Nery. 2015;19(2):5–35.
- 27.Bhattacharjee M, Vairale J, Gawali K, Dalal PM. Factors affecting burden on caregivers of stroke survivors: population-based study in Mumbai (India) Ann Indian Acad Neurol. 2012;15(2):113–119. doi: 10.4103/0972-2327.94994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu Y, Hu J, Efird JT, McCoy TP. Social support, coping strategies and health-related quality of life among primary caregivers of stroke survivors in China. J Clin Nurs. 2013;22(15–16):2160–2171. doi: 10.1111/jocn.12251. [DOI] [PubMed] [Google Scholar]
- 29.Iavarone A, Ziello AR, Pastore F, Fasanaro AM, Poderico C. Caregiver burden and coping strategies in caregivers of patients with Alzheimer’s disease. Neuropsychiatr Dis Treat. 2014;10:1407–1413. doi: 10.2147/NDT.S58063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Folkman S, Lazarus RS. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- 31.Mitrousi S, Travlos A, Koukia E, Sofia Z. Theoretical approaches to coping. Int J Car Sci. 2013;6(2):131–37. [Google Scholar]
- 32.Nia HS, Sharif SP, Goudarzian AH, Allen KA, Jamali S, Gorji MAH. The relationship between religious coping and self-care behaviors in Iranian medical students. J Relig Health. 2017;56(6):2109–2117. doi: 10.1007/s10943-017-0376-2. [DOI] [PubMed] [Google Scholar]
- 33.Kelly MM, Tyrka AR, Price LH, Carpenter LL. Sex differences in the use of coping strategies: predictors of anxiety and depressive symptoms. Depress Anxiety. 2008;25(10):839–846. doi: 10.1002/da.20341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alnazly EK. Burden and coping strategies among J ordanian caregivers of patients undergoing hemodialysis. Hemodial Int. 2016;20(1):84–93. doi: 10.1111/hdi.12318. [DOI] [PubMed] [Google Scholar]
- 35.Hassan WA-N, Mohamed II, Sayed NE. Burden and coping strategies among caregivers of patients with mood disorders. Assiut Sci Nurs J. 2014;2(3):173–80. [Google Scholar]
- 36.Suriyamoorthi M, Pakkiyalakshmi N, Ravishankar J. A study on coping skills of caregivers of patients with bipolar disorder. Int J Res Med Sci. 2018;6(11):36–47. [Google Scholar]
- 37.Fink G. Stress: Concepts, cognition, emotion, and behavior: handbook of stress series, Volume 1: Academic Press; 2016.
- 38.Farnia V, Mousavi SA, Parsamehr A, Alikhani M, Golshani S, Nooripour R, et al. The mediating role of emotional intelligence in coping strategies and test anxiety in students of Kermanshah University of Medical Sciences, Kermanshah, Iran in 2013–2014. Iran J Psychiatry Behav Sci. 2017;11(4):e9254. doi: 10.5812/ijpbs.9254. [DOI] [Google Scholar]
- 39.Modaresifard F, Maredpour A. On the relationship of personality traits and coping strategies with drug abstinence self-efficacy in addicted youth. Res Addict. 2016;10(39):213–30. [Google Scholar]
- 40.Mahmoud AM, Khanjani Z, Bayat A. Comparing the coping strategies and emotion regulation of students with symptoms of anxiety-related emotional disorders and normal group. Res Addict. 2016;3(1):41–51. [Google Scholar]
- 41.Mirabzadeh A, Eftekhari MB, Forouzan AS, Sajadi H, Rafiee H. Relationship between ways of coping and quality of life in married women: toward mental health promotion. Iran Red Crescent Med J. 2013;15(8):743–748. doi: 10.5812/ircmj.12728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Bertolin DC, Pace AE, Kusumota L, Haas V. An association between forms of coping and the socio-demographic variables of people on chronic hemodialysis. Rev Esc Enferm USP. 2011;45(5):1070–1076. doi: 10.1590/S0080-62342011000500006. [DOI] [PubMed] [Google Scholar]
- 44.Abravani P, Gharibzadeh S. Coping strategies during COVID-19 outbreak in Islamic Republic of Iran. J Exp Clin Neurosci. 2020;7(2):1–5. [Google Scholar]
- 45.Soleimani MA, Bahrami N, Allen K-A, Alimoradi Z. Death anxiety in patients with cancer: a systematic review and meta-analysis. Eur J Oncol Nurs. 2020;48:101803. doi: 10.1016/j.ejon.2020.101803. [DOI] [PubMed] [Google Scholar]
- 46.Abdollahi A, Panahipour H, Allen KA, Hosseinian S. Effects of death anxiety on perceived stress in individuals with multiple sclerosis and the role of self-transcendence. OMEGA J Death Dying. 2019. (in press). [DOI] [PubMed]
- 47.Soleimani MA, Pahlevan Sharif S, Yaghoobzadeh A, Allen K-A, Sharif NH. An examination of psychometric characteristics and factor structure of death anxiety scale within a sample of Iranian patients with heart disease. Int J Epidemiol Res. 2017;4(4):260–266. doi: 10.15171/ijer.2017.14. [DOI] [Google Scholar]
- 48.Nia HS, Sharif SP, Lehto RH, Allen KA, Goudarzian AH, Yaghoobzadeh A, et al. Psychometric properties of the persian version of death depression scale-revised in Iranian patients with acute myocardial infarction. Iran J Psychiatry. 2017;12(3):172–181. [PMC free article] [PubMed] [Google Scholar]
- 49.Nayeri ND, Goudarzian AH, Herth K, Naghavi N, Nia HS, Yaghoobzadeh A, et al. Construct validity of the Herth hope index: a systematic review. Int J Health Sci. 2020;14(5):50–57. [PMC free article] [PubMed] [Google Scholar]
- 50.Soleimani MA, Allen KA, Herth KA, Sharif SP. The Herth Hope Index: a validation study within a sample of iranian patients with heart disease. Soc Health Behav. 2019;2(3):108–113. doi: 10.4103/SHB.SHB_4_19. [DOI] [Google Scholar]
- 51.Abdollahi A, Panahipour H, Hosseinian S, Allen KA. The effects of perceived stress on hope in women with breast cancer and the role of psychological hardiness. Psychooncology. 2019;28(7):1477–1482. doi: 10.1002/pon.5102. [DOI] [PubMed] [Google Scholar]
- 52.Yaghoobzadeh A, Gorgulu O, Yee B-L, Wibisono AH, Pahlevan Sharif S, Sharif Nia H, et al. A model of aging perception in Iranian elders with effects of hope, life satisfaction, and socioeconomic status: a path analysis. J Am Psychiatr Nurses Assoc. 2018;24(6):522–530. doi: 10.1177/1078390317753676. [DOI] [PubMed] [Google Scholar]
- 53.Yaghoobzadeh A, Soleimani MA, Allen KA, Chan YH, Herth KA. Relationship between spiritual well-being and hope in patients with cardiovascular disease. J Relig Health. 2018;57(3):938–950. doi: 10.1007/s10943-017-0467-0. [DOI] [PubMed] [Google Scholar]
- 54.Abdollahi A, Hosseinian S, Panahipour H, Allen KA. Cognitive behavioural therapy as an effective treatment for social anxiety, perfectionism, and rumination. Curr Psychol. 2019. (in press).
- 55.Frydenberg E, Deans J, Allen K-A. Developing children’s coping in the early years: Strategies for dealing with stress, change and anxiety. Bloomsbury Academic; 2012.
- 56.Eslahi Z, Bahrami N, Allen KA, Alimoradi Z. Spouse’s social support in the postpartum period, predictors and its relationship with postpartum depression in a sample of Iranian primiparous women. Int J Gynecol Obstet. 2020. (in press). [DOI] [PubMed]
- 57.Jafari A, Hesampoor F. The comparison of coping strategies and psychological hardiness between parents of children with cancer of positive and negative responding to treatment. Sci J Ilam Univ Med Sci. 2017;24(6):189–202. [Google Scholar]
- 58.Yaghoobzadeh A, Sharif Nia H, Pahlevan Sharif S, Hosseinigolafshani SZ, Mohammadi F, Oveisi S, et al. Role of sex, socioeconomic status, and emotional support in predicting aging perception among older adults. IntJ Aging Hum Dev. 2018;87(1):77–89. doi: 10.1177/0091415017727211. [DOI] [PubMed] [Google Scholar]
- 59.Ghandehari K. Epidemiology of stroke in Iran. Galen Med J. 2016;5(S1):3–9. [Google Scholar]
- 60.Hesamzadeh A, Dalvandi A, Maddah SB, Khoshknab MF, Ahmadi F. Family caregivers’ experiences of stroke recovery among older adults living in Iran: a qualitative study. Iran Red Crescent Med J. 2018;20(S1):1–9. [Google Scholar]
- 61.Pinedo S, SanMartin V, Zaldibar B, Miranda M, Tejada P, Erazo P, et al. Quality of life of stroke patients and their caregivers. Int J Phys Med Rehabil. 2017;5(1):1–6. [Google Scholar]
- 62.Al-Rawashdeh SY, Lennie TA, Chung ML. Psychometrics of the Zarit Burden Interview in caregivers of patients with heart failure. J Cardiovasc Nurs. 2016;31(6):E21. doi: 10.1097/JCN.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yap P. Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Ann Acad Med Singap. 2010;39:758–763. [PubMed] [Google Scholar]
- 64.Navidian A, Pahlavanzade S, M. Y. Family training effectiveness in mental burden of mentally disordered inpatients' domestic caregivers. J Psychiatry Clin Psychol. 2011;2(99):99–106.
- 65.Greenaway KH, Louis WR, Parker SL, Kalokerinos EK, Smith JR, Terry DJ. Measures of coping for psychological well-being. In Measures of personality and social psychological constructs. Elsevier; 2015. 322–51.
- 66.M. K. Normative question of coping devices Lazarus and Folkman and comparison between these devices in girls and boys students of Islamic Azad University Central Rodhen , Branch of Tehran Central; 2004.
- 67.Ramzi L, Sepehri Shamloo Z, Ali Pour A, Zare H. The effectiveness of group reality therapy in coping strategies. J Fam Psychol. 2015;1(2):19–30. [Google Scholar]
- 68.Kumar R, Kaur S, Reddemma K. Burden and coping strategies in caregivers of stroke survivors. J Neurol Neurosci. 2015;6(5):1–5. [Google Scholar]
- 69.Rawat M, Sharma R, Goel D. Burden of stroke survivors on caregiver and quality of life. Int J Curr Res. 2017;9:60683–60686. [Google Scholar]
- 70.Baumann M, Lurbe-Puerto K, Alzahouri K, Aïach P. Increased residual disability among poststroke survivors and the repercussions for the lives of informal caregivers. Top Stroke Rehabil. 2011;18(2):162–171. doi: 10.1310/tsr1802-162. [DOI] [PubMed] [Google Scholar]
- 71.Hosseiny R, Bastani F, Sayahi S, Momen AH, Alijanpoor AM. The effect of educational-counseling program on general health of women as caregivers of patient, with Alzheimerdisease. Top Stroke Rehabil. 2011;13(5):83–92. [Google Scholar]
- 72.Salmani N, Ashketorab T, Hasanvand S. The burden of caregiver and related factors of oncology patients of shahvali hospital. Adv Nurs Midw. 2014;23(84):7–11. [Google Scholar]
- 73.Nazari S, Rashedi V, Mohammadi H, Yousefi M. Relationship between cognitive status and activities of daily living among the elderly of nursing homes. J Kermanshah Univ Med Sci. 2015;18(12):744–746. [Google Scholar]
- 74.Unver V, Basak T, Tosun N, Aslan O, Akbayrak N. Care burden and self-efficacy levels of family caregivers of elderly people in Turkey. Holist Nurs Pract. 2016;30(3):166–173. doi: 10.1097/HNP.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 75.Yeşil T, Uslusoy E, Korkmaz M. Examining of the life quality and care burden of those who are looking after the patients suffering from chronic diseases. Gümüşhane Univ J Health Sci. 2016;5(4):54–66. [Google Scholar]
- 76.Friedemann M-L, Buckwalter KC. Family caregiver role and burden related to gender and family relationships. J Fam Nurs. 2014;20(3):313–336. doi: 10.1177/1074840714532715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Orak OS, Sezgin S. The investigation of caregiver burden in family members of cancer patients. J Psychiatr Nurs. 2015;6(1):33–39. [Google Scholar]
- 78.Sanuade OA, Boatemaa S. Caregiver profiles and determinants of caregiving burden in Ghana. Public Health. 2015;129(7):941–947. doi: 10.1016/j.puhe.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 79.Sousa MFB, Santos RL, Turró-Garriga O, Dias R, Dourado MC, Conde-Sala JL. Factors associated with caregiver burden: comparative study between Brazilian and Spanish caregivers of patients with Alzheimer's disease (AD) Int Psychogeriatr. 2016;28(8):1363–1374. doi: 10.1017/S1041610216000508. [DOI] [PubMed] [Google Scholar]
- 80.Mathew V. 988–Coping strategies among primary caregivers of hiv/aids infected individuals. Eur Psychiatry. 2013;28:1. doi: 10.1016/S0924-9338(13)76124-8. [DOI] [Google Scholar]
- 81.García-Alberca JM, Cruz B, Lara JP, Garrido V, Lara A, Gris E. Anxiety and depression are associated with coping strategies in caregivers of Alzheimer's disease patients: results from the MALAGA-AD study. Int Psychogeriatr. 2012;24(8):1325–1334. doi: 10.1017/S1041610211002948. [DOI] [PubMed] [Google Scholar]
- 82.Papastavrou E, Charalambous A, Tsangari H. How do informal caregivers of patients with cancer cope: a descriptive study of the coping strategies employed. Eur J Oncol Nurs. 2012;16(3):258–263. doi: 10.1016/j.ejon.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 83.Abbasi A, Shamsizadeh M, Asayesh H, Rahmani H, Hosseini SA, Meidhat T. The relationship between caregiver burden with coping strategies in Family caregivers of cancer patients. Iran J Psychiatric Nurs. 2013;1(3):62–71. [Google Scholar]
- 84.Jaracz K, Grabowska-Fudala B, Górna K, Kozubski W. Caregiving burden and its determinants in Polish caregivers of stroke survivors. Arch Med Sci. 2014;10(5):941–950. doi: 10.5114/aoms.2014.46214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kameli D, Hojjat S, Jajarmi M, Abedi A, Kameli T. Comparison between personality traits and copying strategies in Substance dependent men and non dependent group. J N Khorasan Univ Med Sci. 2014;5(4):813–819. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Caregivers burden and coping strategies. SA Motalebi, Sup. data.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [supplementary file:SPSS file].