Abstract
Introduction
Surgical site infections (SSIs) are a significant source of morbidity and mortality in the Asia–Pacific region (APAC), adversely impacting patient quality of life, fiscal productivity and placing a major economic burden on the country’s healthcare system. This commentary reports the findings of a two-day meeting that was held in Singapore on July 30–31, 2019, where a series of consensus recommendations were developed by an expert panel composed of infection control, surgical and quality experts from APAC nations in an effort to develop an evidence-based pathway to improving surgical patient outcomes in APAC.
Methods
The expert panel conducted a literature review targeting four sentinel areas within the APAC region: national and societal guidelines, implementation strategies, postoperative surveillance and clinical outcomes. The panel formulated a series of key questions regarding APAC-specific challenges and opportunities for SSI prevention.
Results
The expert panel identified several challenges for mitigating SSIs in APAC; (a) constraints on human resources, (b) lack of adequate policies and procedures, (c) lack of a strong safety culture, (d) limitation in funding resources, (e) environmental and geographic challenges, (f) cultural diversity, (g) poor patient awareness and (h) limitation in self-responsibility. Corrective strategies for guideline implementation in APAC were proposed that included: (a) institutional ownership of infection prevention strategies, (b) perform baseline assessments, (c) review evidence-based practices within the local context, (d) develop a plan for guideline implementation, (e) assess outcome and stakeholder feedback, and (f) ensure long-term sustainability.
Conclusions
Reducing the risk of SSIs in APAC region will require: (a) ongoing consultation and collaboration among stakeholders with a high level of clinical staff engagement and (b) a strong institutional and national commitment to alleviate the burden of SSIs by embracing a safety culture and accountability.
Keywords: Surgical site infection, Healthcare-associated infection, Guidelines, Implementation, Asia–Pacific
The landscape of surgical site infections—a global perspective
Surgical site infections (SSIs) are defined as infections that occur at or near the surgical incision within 30 days following a procedure, or within 90 days if prosthetic materials are implanted at surgery [1]. Reported SSI rates vary according to the type of surgery, surgery length, surgical method (clean vs clean contaminated vs dirty; robotic vs conventional), size of facility (number of beds), and patient cohort age group [2–9]. SSI is one of the most frequently reported types and is the most common postoperative complication [2, 4, 10–12]. SSIs are associated with a poorer post-operative recovery, increased postoperative morbidity and mortality, and SSIs contribute to the spread of antibiotic resistance globally [13]. SSIs remain a significant global health problem that warrants prioritized efforts for prevention [14].
The incidence of SSI is difficult to establish because criteria are not always standardized [15]. A substantial proportion of infections is only detected post-discharge and may be treated in the community without notification [13]. According to the World Health Organization (WHO), the cumulative incidence of SSI is 0.9% in the USA (2014) and ranges between 0.75 and 9.5% across different types of surgery in Europe (2010–2011) [2, 16]. However, low-income countries carry a disproportionately greater SSI burden [3, 4, 9, 16–18]. The WHO reports a pooled SSI incidence in low- and middle-income countries (LMICs) of 11.8% [17]. In the APAC region, the reported incidence of SSI varies widely—cumulative incidences of 2.8% in Australia (2002–2013), 2.0–9.7% in the Republic of Korea, 4% in China (2000–2017), and 7.8% in South East Asia and Singapore (pooled; 2000–2012) [3, 17, 19–21].
The landscape of surgical site infections—an APAC perspective
On July 30–31, 2019 an SSI Prevention Symposium was held in Singapore where 10 stakeholders from across the region and North America representing infection control, surgical sciences, quality services and nursing met to discuss the need for the standardization of evidence-based practices to improve the surgical outcomes of patients in the Asia–Pacific region. The APAC region comprises a diverse range of countries with varying climates and cultural, religious, demographic, and healthcare funding landscapes. The distribution of microbial pathogens responsible for SSIs also varies across the region [16]. As such, APAC presents unique and wide-ranging challenges related to SSI prevention and control within in-patient and post-discharge environments.
While a significant number of recent studies on SSI from the region exists, information on how to utilize the data to improve SSI prevention is scarce. Some countries do not have contextually applicable national guidelines, and many lack standardized protocols and accountabilities for guideline implementation and SSI monitoring. Although some countries have mandatory requirements for SSI reporting that inform reimbursement decisions, several countries within APAC have inadequate infection prevention and control surveillance programs, standardized surveillance systems and accountabilities [3, 16]. SSI rates have been shown to strongly correlate with the degree of concordance to guidelines, and a large systematic review has estimated that half of all SSIs could be prevented through appropriate application of evidence-based strategies [22, 23]. The consensus expert panel that met in Singapore agreed that the burden of SSI in the region could be alleviated through implementation of the standardized SSI prevention guidelines and improved surveillance.
The Singapore symposium served as a platform to: (1) identify persistent gaps and barriers to SSI prevention in APAC, (2) discuss evidence-based SSI prevention strategies and solutions that demonstrated improved outcomes, elevating the standard of patient care, and (3) achieve consensus on the best ways to implement SSI prevention and surveillance guidelines across the APAC region.
Strategy for achieving consensus
Prior to the Symposium, a targeted literature review was performed to explore the evidence in four key areas—guidelines, implementation, surveillance and outcomes—particularly relevant to APAC, and to identify gaps in these areas. The following keywords were used: “surgical site infection”, “infection control”, “infection prevention”, “guidelines”, “implementation”, “surveillance”, “outcomes”, “economic”, “cost” AND “Asia Pacific”, “Asia”, “China”, “India”, Hong Kong”, “Singapore”, “Japan”, “Korea”, “Taiwan”, “Malaysia”, “Indonesia”, “Vietnam”, “Thailand”, “Philippines”, “Australia”, “New Zealand”. The search was limited to English language publications only, dated 2009–June 2019.
Based on this review, key questions on APAC-specific challenges and opportunities for SSI prevention were formulated and discussed during the Symposium, led by the multidisciplinary experts from Australia, India, Japan, Philippines, Singapore, South Korea and the USA. The delegates asked questions during the Symposium via the Pigeonhole Live® platform. The results presented in this manuscript are a result of both a comprehensive targeted literature review and the inputs/recommendations from the expert panel based on their clinical experience.
Challenges for SSI guideline implementation in the APAC region
Several countries in APAC have national guidelines, including the Australian Guidelines for the Prevention and Control of Infection in Healthcare, the Chinese guideline for the Prevention of Surgical Site Infection, the Indian Council of Medical Research guideline, the Thailand Surgical Infection Society guidelines, and Ministry of Health guidelines from Indonesia, Singapore, Malaysia and the Philippines [24–31]. Japan has no official government SSI guideline; however, two Japanese professional organizations have relevant publications [32, 34]. The expert panel outlined several key recommendations for selecting, adapting and disseminating guidelines (Table 1). The successful application of these key recommendations was demonstrated through the development of the Australian national guidelines (2019), which was based on local context and published online using an interactive ‘living guideline platform’ [24]. Each recommendation is listed with its strength of recommendation, key evidence regarding benefits/harm, rationale and specific suggestions for decision making and implementation.
Table 1.
Expert panel key recommendations for guideline selection, adaptation and dissemination
| Guideline selection, adaptation and dissemination—expert recommendations |
|---|
| 1. Systems and governance for SSI prevention and surveillance within APAC should be consistent with global and/or national guidelines. Guidelines should be implemented at both the national and individual hospital level |
| 2. Professional societies within respective countries may also formulate their own guidelines using frameworks provided by global guidelines and should be consistent with their national guidelines. National guidelines should be situationally applicable and adaptable to an institution’s cultural, socioeconomic, clinical, health economic and political context [40] |
| 3. Where possible, local systems and processes for SSI prevention and surveillance should be developed and standardised based on local evidence to ensure contextual relevance and long-term sustainability |
| 4. Guidelines should be actively disseminated to stakeholders who are in a position to make impactful changes |
| 5. Guidelines should be ‘living documents’, updated on an ongoing basis as new evidence is accumulated |
Non-concordance with SSI prevention guidelines was strongly correlated with SSI rate [22]. A key challenge for SSI prevention in the APAC region is achieving widespread and consistent guideline implementation. In many APAC countries, both developed and developing, recent data on guideline adherence and implementation of tools such as SSI bundles are lacking. During the meeting, the expert panel identified several common institutional and individual challenges that could hinder the successful implementation of evidence-based SSI guidelines within the APAC region.
Human resource constraints Hospitals invariably battle time, workforce and workload constraints, leaving little time or priority for adequate training and protocol modifications. A lack of SSI prevention education among healthcare workers, high nursing staff turnover, limitations in language competency, and even a lack of data interpretation skills can hamper efforts to implement systems that are congruent with the guidelines [16, 34, 35].
Lack of adequate policies and procedures Absence of, or poor knowledge concerning written policies, checklists or care bundles can negatively affect guideline implementation [36, 37]. Some government health authorities in the APAC region do not have adequate laws or policies to encourage SSI prevention and control.
Lack of strong safety culture The panel emphasized that cultivation of a strong, sustainable institutional safety culture is imperative when working toward SSI prevention [38]. Obstacles detracting from a safety culture include complacency, a lack of interest or skills/education among staff, self-protective attitudes, or resistance to changing established behaviors [38–41]. Studies have shown that effective communication and teamwork in the operating room are associated with fewer errors [42]. Good administrative support is also essential in establishing a safety culture. The leadership of senior surgeons is critical to the success of SSI prevention planning. Initiatives are more likely to gain traction with active involvement from senior leadership – particularly surgeons – who are prepared to champion the development and implementation of guidelines and influence a culture shift toward process improvement [38].
Limitations in funding and other resources Reimbursement is an important consideration for medical and surgical practice patterns in the APAC region [16, 43]. A wide spectrum of funding scenarios exists across the region, and inadequate levels of dedicated financial support and infrastructure in some countries is a common barrier to the successful implementation of SSI guidelines. Some low-income countries may also lack the necessary microbiological and diagnostic tools and laboratory resources.
Cultural considerations Varying cultural norms exist across APAC, some of which may limit the applicability of selective guideline components. For example, in India and Japan, hospital stays can often be long by patient choice. Clipping of hair is culturally less acceptable in some countries. Cultural tendencies toward smoking may also increase SSI risks.
Poor patient awareness and responsibility Suboptimal patient compliance or thoroughness regarding preoperative self-showering/bathing can interfere with even the best SSI prevention efforts. In addition, in some areas, there may be a lack of awareness among patients and families regarding post-operative care instructions, increasing the risk of SSI following discharge [16].
Strategies for guideline implementation: an expert panel recommendation
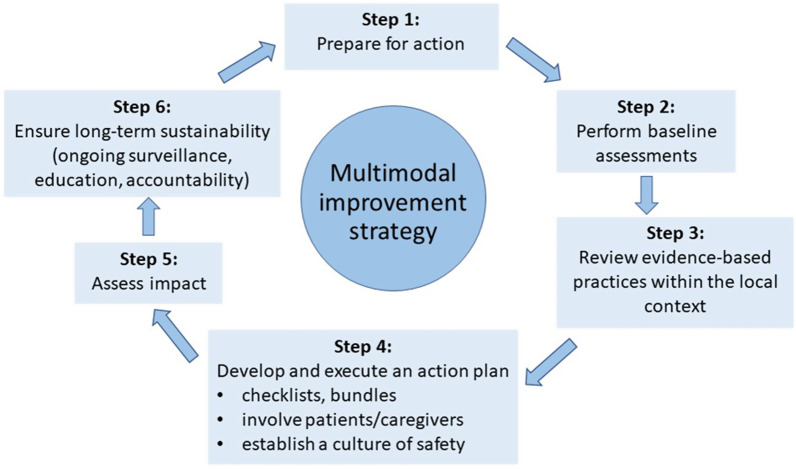
The expert panel recommends that every hospital works actively toward improving the implementation of applicable guidelines, through embedding appropriate SSI prevention programs within their work processes. Such changes should be situationally appropriate, measurable and sustainable over the long term. Regardless of the current level of SSI prevention initiatives, we suggest a stepwise approach based on the WHO’s ‘cycle of continuous improvement’ (Fig. 1) [13]. Moving forward, the expert panel has formulated the following evidence-based recommendations.
-
Prepare for action
Hospitals should systematically identify core principles and relevant key questions that can prompt action and drive infection control as a top priority [24]. Establishing a surgical wound task force can be helpful to gain important insights into local infection cause and prevention, and to facilitate relationships, discussion and understanding. Teams should meet regularly and include all relevant disciplines, including surgeons, surgical nurses, anesthetists, pharmacists, and managers from Infection Prevention and Control (IPC), Healthcare Quality, Facilities, and Environmental Services [44]. It will be crucial to gain buy-in from senior surgeons who are prepared to champion the cause of SSI guideline implementation and disseminate important information; infection prevention and control teams need to proactively build trust with surgeons and place them at the forefront of discussions [45]. Surgeons are most likely to become engaged when presented with robust evidence-based data on SSI rates, compliance with processes and guidelines, antibiotic resistance and appropriate stewardship, and hand hygiene compliance. Surgeons need to be aware of their own SSI data and how these compare with those from other institutions and currently established benchmarks. Some institutions in the region, such as India, encourage surgeons and their teams by recognizing their SSI prevention work with awards or other public recognition, or showcasing their efforts to modify practices and behavior.
-
Perform baseline assessments
A robust data collection system is crucial to the success of reducing the risk of SSIs. For countries or institutions currently without adequate and proactive SSI prevention systems, the expert panel recommends initially performing a gap analysis or point prevalence survey to assess specific process indicators. For example, current adherence to operating room preparation or postoperative dressing change protocols can be measured and recorded as a baseline against which improvement can be quantified. The key is to start small, evaluate specific indicators of interest, collect small groups of data and tackle a few issues at a time. Systematic tools for the assessment of infection control exist, including a WHO Electronic Assessment Tool, the US Infection Control Assessment Tool (ICAT), and the IPC Assessment Framework (IPCAF) [36, 46–48]. These tools can assist in clearly identifying targets for cost-effective system improvements, including in low-resource facilities.
-
Review evidence-based practices within the local context
A thorough review of available guidelines will help identify improvements that are most urgent, necessary and cost-effective. For highly cost-sensitive economies and smaller hospitals, improvements must be made within current financial constraints. However, the expert panel notes that it is important to consider real overall costs—e.g., what are the projected overall long-term savings from investing in new equipment (e.g. electronic hand hygiene alert systems at or near the hand rub), employing more SSI prevention staff, or using antimicrobial sutures?
-
Develop and execute an action plan
Efforts should be made to implement guidelines using clearly defined strategies that consider expert consensus, country experience and the specific needs and goals of the facility. To build a system change, it may be useful to initially choose four or five evidence-based practices, standardize interventions into well-defined tasks to facilitate uptake, and establish key performance indicators to monitor improvement.
-
Use of standardized, measurable outcome tools
Several practical tools to support guideline implementation and best practice are available, including implementation guides, checklists, surgical bundles, risk stratification tools, and standardized protocols. The expert panel recommends careful consideration of how these tools can best inform local practice.-
Implementation guides
-
ChecklistsUse of surgical safety checklists can successfully draw attention to SSI prevention. Patients exposed to a checklist have a lower risk of postoperative infection and death than patients not exposed to a checklist, although this finding could also simply reflect the quality of care in hospitals where checklists are routinely used [51–53]. The global WHO surgical safety checklist is designed to support SSI prevention at the facility level. This checklist comprises 19 items in 3 domains (before anesthesia, before incision, and before the patient leaves the operating room). It has been widely adopted and adapted worldwide and is often considered a surrogate marker for the quality of patient care [53, 54]. Implementation of the WHO checklist has also been evaluated in several APAC countries, including Thailand, India, Cambodia, Pakistan and Indonesia. Variability in awareness and compliance has been highlighted, as well as differences in subjective clinical decision making and cultural norms [51, 55–58].
-
Surgical bundlesThe ‘bundle’ approach has become a commonly accepted and effective method of incorporating best practice measures into routine clinical care [59, 60]. National guidelines from India, Indonesia, Singapore and Australia describe and recommend the use of a bundle approach [24, 26, 28, 29]. No single SSI prevention bundle, however, can be applied to all settings. Bundles are built from usually three to five specific high-quality evidence-based practices (high level of evidence/class 1A; Table 2) [24, 60–62]. Prevention bundles should be constructed based on identified local gaps that are thought to be contributing to higher-than-desirable SSI rates [63]. Consistent use of care bundles has been shown to achieve substantial SSI rate reductions and healthcare cost benefits [64–70]. Use of bundles in APAC countries (e.g. Japan, India, China and Singapore) has been reported to reduce SSI incidence by 22–93% [71–75]. The expert panel strongly recommends that implementation of an evidence-based surgical care bundle be supported by a robust compliance program, since outcome failures following bundle implementation are often associated with poor compliance to individual bundle components [76].
-
Other tools
-
-
Involvement of patients and caregivers—making all parties part of the solution
The expert panel recognizes that both the patient and caregiver play a major role in optimizing clinical outcome recommendations. Patients should be fully engaged and empowered with a full understanding of preoperative preparation, as well as infection risk during wound healing [81]. In the Philippine General Hospital, a dedicated pathway (via text messages or email) is established for patients to inform physicians if any problems arise before their designated follow-ups. Patient-reported outcomes (PROs) may be gathered by way of app-based checklists and phone calls. Studies have documented that wound photography can be a useful tool for SSI diagnosis, in addition to chart review and telephone consultation, in improving SSIs diagnostic accuracy and confidence [82–84].
-
Establishing an institutional safety culture
Implementation of checklists and tools is not likely to impact SSI rates without consistent institution-wide buy-in. A cultural shift toward increased willingness to follow established local protocols drives the effectiveness of checklists and protocols and is strongly associated with improved outcomes [44, 84]. As opposed to enforced mandates which breed only superficial compliance, the preference is to encourage an institutional safety culture wherein staff are impelled, rather than compelled, to be vigilant. Hospitals with a strong organizational safety culture embrace innovation, promote education, collaboration and communication, engage and empower their health professionals, and foster a no-blame, non-punitive climate [85]. Efforts from ‘surgical champions’ to drive the adoption of a safety culture may include modelling safety-focused behavior, making regular safety rounds, initiating daily ‘safety huddles’, direct communication with staff and patients, and participation in quality improvement meetings [38].
-
Assess impact: evaluation and feedback
The expert panel strongly encourages ongoing evaluation and feedback as crucial aspects of SSI prevention. Feedback of clinical performance data helps create a sense of accountability and motivation [44]. Data-derived surveillance activities are used to identify areas for further practice improvement and research, prioritize action plans, inform policy and practice, and measure the effect of interventions. Regular data feedback to key stakeholders, including frontline providers and hospital leadership, helps support SSI improvement efforts [44]. Demonstrating consistent cost savings—more importantly, overall cost benefits—can help ensure ongoing financial support.
-
Ensure long-term sustainability
When evidence-based peri- and postoperative practices result in measurable improvement, further steps should be taken to build on this foundation by setting forward new goals. Ongoing education, accountability, and active efforts to engage all stakeholders—particularly where staff turnover is high—can ensure the longevity of SSI prevention programs at a regional, national and APAC-wide level.
Fig. 1.
Multimodal SSI prevention and control improvement strategy. Expert panel assessment of multimodal SSI prevention and control improvement strategy.
Adapted from: World Health Organization. Implementation manual to support the prevention of surgical site infections at the facility level—turning recommendations into practice (interim version) [13]
Table 2.
Evidence-based care bundle elements.
Adapted from lecture “A Speciality or Global Approach to SSI Prevention: Clean, Clean-Contaminated and Contaminated Procedures” delivered by Dr Charles E Edmiston, Jr., at the APAC Surgical Site Infection Prevention Symposium (Singapore, 31 July 2019)
| Bundle elements | Classa | Mechanistic benefits |
|---|---|---|
| Evidence-based interventions | ||
| Normothermia | 1A | Less bleeding/preserve immune function in wound bed/enhanced wound healing |
| Perioperative weight-based antimicrobial prophylaxis | 1A | Tissue antisepsis/intraoperative conc > MIC [90] wound pathogens |
| Glycaemic control | 1A | Preserve granulocytic immune function/enhance wound healing |
| Antimicrobial (triclosan) coated sutures (fascia/subcuticular closure) | 1A | Mitigate nidus of infection/local tissue antisepsis |
| Preadmission CHG showering/bathing | 1B | Skin antisepsis/reduce skin bioburden |
| Perioperative skin prep with 2% CHG/70% alcohol | 1A | Skin antisepsis/reduce skin bioburden |
| Separate wound closure tray | II | Mitigate instrument contamination |
| Glove change prior to fascia/subcuticular closure | II | Disrupt cross-contamination across tissue planes |
| Supplemental evidence-based interventions | ||
| Supplemental oxygen (colorectal surgery) | 1A | Enhanced tissue oxygenation and immune function/ metabolic benefits/wound healing |
| Oral antibiotics/mechanical bowel prep (colorectal surgery) | 1A | Reduce bioburden within the bowel lumen and on brush border surfaces |
| Wound edge protector (colorectal, vascular and OB/GYN surgeries) | 1B | Intraoperative wound antisepsis/minimising wound contamination |
| Staphylococcal decolonization (orthopaedic and CT surgeries) | 1A | Mitigate S. aureus and MRSA pathogenicity |
| Smoking cessation (orthopaedic, neurological, CT, and likely all surgeries) | 1B | Preserve angiogenesis/reduce risk of dehiscence/enhance wound healing |
| Intraoperative irrigation of the surgical wound with 0.05% CHG | II | Mitigate wound contamination prior to closure |
| OR traffic control – minimize door openings | No recommendation/unresolved | Reduce OR air bioburden |
CHG, chlorhexidine gluconate; CT, cardiothoracic; MRSA, methicillin-resistant Staphylococcus aureus; OB/GYN, obstetrics/gynaecology; OR, operating room, conc > MIC [90], concentration greater than the minimal inhibitory concentration required to inhibit the growth of 90% of surgical wound pathogens
aColumn 2: Interventional evidence-based criteria derived from “CDC SSI Guidelines Evidence-Based Criteria documentation and Wisconsin Division of Public Health Service Supplemental Guidance for the Prevention of Surgical Site Infections: An Evidence-based Perspective [60–62]. CDC categories: 1A = strong recommendation supported by high to moderate–quality evidence suggesting net clinical benefits or harms; 1B = strong recommendation supported by low-quality evidence suggesting net clinical benefits or harms or an accepted practice (eg, aseptic technique) supported by low to very low–quality evidence; 1C = A strong recommendation required by state or federal regulation; Category II = weak recommendation supported by any quality evidence suggesting a trade-off between clinical benefits and harms; No recommendation/unresolved issue = An issue for which there is low to very low–quality evidence with uncertain trade-offs between the benefits and harms or no published evidence on outcomes deemed critical to weighing the risks and benefits of a given intervention
Moving forward—the future is now
The future of SSI prevention globally and in the APAC region lies in ongoing consultation and collaboration between stakeholders, a high level of staff engagement, cultivation of a strong safety culture within institutions and nationally, and forging further research opportunities that can inform ongoing improvements in procedures and systems. The purpose of the Singapore SSI Symposium was to bring together sentinel stakeholders to develop an evidence-based action plan that cuts across the vast geographical, cultural and economic diversity that define the APAC region. Moving forward, the expert panel has identified that further work is needed in the areas of awareness/education, training improvements, audits, simplifying and standardizing practices, and setting achievable standards for accreditation. Ongoing information-sharing regarding effective interventions and differences in epidemiology will be imperative as we work together to reduce SSI risk across the region.
It is also imperative for us to better understand the most effective ways to involve patients and their caregivers in SSI prevention and management. In the future, innovations such as semi-automated or automated surveillance systems, use of vaccines and molecular therapies, implant/suture product developments, and use of dispersion signals and matrix degraders may be employed to reduce SSI risk [86–91]. It is also anticipated that artificial intelligence will be increasingly used to capture surveillance data and will become an integral part of transformative innovation in the future prevention of SSI [92]. Finally, as we have seen during the current pandemic period, telehealth technologies hold a promising future for the implementation and compliance of peri- and postoperative surgical care-processes [93–95].
Acknowledgements
Medical editorial assistance was provided by In Vivo Communications (Asia).
Authors' contributions
All authors listed on the title page of the manuscript were involved in the: (1) Development, (2) Writing, and (3) Final review of the consensus manuscript prior to submission. All authors read and approved the final manuscript.
Funding
The Asia Pacific Masters Surgical Site Infection Prevention Symposium and this subsequent manuscript were kindly sponsored by ETHICON, a member of the Johnson and Johnson Family of Companies.
Availability of data and materials
No datasets were used in the development of this consensus manuscript.
Declarations
Ethics approval and consent to participate
There is no need for ethical approval in this consensus document.
Consent for publication
No individual person’s data in any form (including any individual details, images or videos) is presented in this consensus document. No case studies are reported.
Competing interests
All authors, except LML, have received travel and accommodation supports from ETHICON (a member of the Johnson and Johnson Family of Companies) to attend and participate in the Asia Pacific Masters Surgical Site Infection Prevention symposium. KM has no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials disclosed in this manuscript. KYL is a consultant of Johnson and Johnson. MC has no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials disclosed in this manuscript. LML received an educational grant from 3 M for the development of the APSIC Guidelines for Prevention of SSI; however, 3 M was not involved in providing any input to the guidelines. PLR is the President of the Australasian College for Infection Prevention and Control. He is a member of the COVID Evidence Taskforce Steering Committee, the Infection Control Expert Group to the Department of Health, the Australian Strategic and Technical Advisory Group on AMR, the Healthcare Associated Infection Advisory Committee to the Australian Commission on Safety and Quality in Health Care, and a member of the Australian College of Nursing. He is also the recipient of a NHMRC Early Career Fellowship and has received research funding from the Rosemary Norman Foundation, Cardinal Health, Australian College of Nursing and the Cabrini Institute. ES has been invited as speaker and has on few occasions received honoraria from ETHICON and 3 M. MS is a member of the J&J Ethicon Speakers Bureau. WD is Director of Ethicon Global Health Economics and Market Access, a subsidiary of Johnson and Johnson, manufacturer of surgical sutures and wound closure devices. AS is Associate Director at Johnson and Johnson. CEE is a member of the J&J Ethicon Speakers Bureau.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reference
- 1.Centers for Disease Control and Prevention. Surgical Site Infection (SSI) Event. Procedure-associated module. 2020. https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscSSIcurrent.pdf. Accessed 1 June 2020.
- 2.European Centre for Disease Prevention and Control. Annual epidemiological report 2013. Reporting on 2011 surveillance data and 2012 epidemic intelligence data. 2013. https://www.ecdc.europa.eu/en/publications-data/annual-epidemiological-report-2013-2011-data. Accessed 6 Feb 2020.
- 3.Curcio D, Cane A, Fernández F, Correa J. Surgical site infection in elective clean and clean-contaminated surgeries in developing countries. Int J Infect Dis. 2019;80:34–45. doi: 10.1016/j.ijid.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Collaborative GlobalSurg. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 2018;18(5):516–525. doi: 10.1016/S1473-3099(18)30101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morikane K, Honda H, Suzuki S. Factors associated with surgical site infection following gastric surgery in Japan. Infect Control Hosp Epidemiol. 2016;37(10):1167–1172. doi: 10.1017/ice.2016.155. [DOI] [PubMed] [Google Scholar]
- 6.Morikane K, Konishi T, Harihara Y, Nishioka M, Kobayashi H. Implementation and establishment of nationwide surgical site infections surveillance in Japan. Am J Infect Control. 2005;33(5):e175–e176. doi: 10.1016/j.ajic.2005.04.226. [DOI] [Google Scholar]
- 7.Rosenthal VD, Richtmann R, Singh S, et al. Surgical site infections, International Nosocomial Infection Control Consortium (INICC) report, data summary of 30 countries, 2005–2010. Infect Control Hosp Epidemiol. 2013;34(6):597–604. doi: 10.1086/670626. [DOI] [PubMed] [Google Scholar]
- 8.Hermsen E, Hinze T, Rupp M, Sayles H, Sholtz L, Hermsen E. Incidence of Surgical Site Infection (SSI) Associated with Robotic Surgery. In: IDSA 2009. https://idsa.confex.com/idsa/2009/webprogram/Paper29278.html. [DOI] [PubMed]
- 9.Du M, Liu B, Li M, et al. Multicenter surveillance study of surgical site infection and its risk factors in radical resection of colon or rectal carcinoma. BMC Infect Dis. 2019;19(1):411. doi: 10.1186/s12879-019-4064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Types of healthcare-associated infections. https://www.cdc.gov/hai/infectiontypes.html. Accessed 9 Dec 2019.
- 11.Russo PL, Stewardson AJ, Cheng AC, Bucknall T, Mitchell BG. The prevalence of healthcare associated infections among adult inpatients at nineteen large Australian acute-care public hospitals: a point prevalence survey. Antimicrob Resist Infect Control. 2019;8:114. doi: 10.1186/s13756-019-0570-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai Y, Venkatachalam I, Tee NW, et al. Prevalence of healthcare-associated infections and antimicrobial use among adult inpatients in Singapore acute-care hospitals: results from the first national point prevalence survey. Clin Infect Dis. 2017;64(suppl 2):S61–S67. doi: 10.1093/cid/cix103. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Implementation manual to support the prevention of surgical site infections at the facility level—turning recommendations into practice (interim version). 2018. https://www.who.int/infection-prevention/publications/implementation-manual-prevention-surgical-site-infections.pdf?ua=1. Accessed 11 Feb 2020.
- 14.Berrios-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–791. doi: 10.1001/jamasurg.2017.0904. [DOI] [PubMed] [Google Scholar]
- 15.Medscape. What is the global prevalence of surgical site infections (SSIs)? https://www.medscape.com/answers/188988-82339/what-is-the-global-prevalence-of-surgical-site-infections-ssis. Accessed 8 Dec 2019.
- 16.Asia Pacific Society of Infection Control. APSIC guidelines for the prevention of surgical site infections. 2019. https://apsic-apac.org/wp-content/uploads/2019/02/APSIC-SSI-Prevention-guideline-Feb-2019.pdf. Accessed 9 Nov 2019. [DOI] [PMC free article] [PubMed]
- 17.World Health Organization. Report on the burden of endemic health care-associated infection worldwide. 2011. https://apps.who.int/iris/bitstream/handle/10665/80135/9789241501507_eng.pdf. Accessed 17 Dec 2019.
- 18.World Bank. List of Economies 2018. https://www.acpe-accredit.org/pdf/ISP/WorldBankData-CountryClassifications.pdf. Accessed 9 Nov 2019.
- 19.Worth LJ, Bull AL, Spelman T, Brett J, Richards MJ. Diminishing surgical site infections in Australia: time trends in infection rates, pathogens and antimicrobial resistance using a comprehensive Victorian surveillance program, 2002–2013. Infect Control Hosp Epidemiol. 2015;36(4):409–416. doi: 10.1017/ice.2014.70. [DOI] [PubMed] [Google Scholar]
- 20.Lee KY, Coleman K, Paech D, Norris S, Tan JT. The epidemiology and cost of surgical site infections in Korea: a systematic review. J Korean Surg Soc. 2011;81(5):295–307. doi: 10.4174/jkss.2011.81.5.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ling ML, Apisarnthanarak A, Madriaga G. The burden of healthcare-associated infections in Southeast Asia: a systematic literature review and meta-analysis. Clin Infect Dis. 2015;60(11):1690–1699. doi: 10.1093/cid/civ095. [DOI] [PubMed] [Google Scholar]
- 22.Young B, Ng TM, Teng C, Ang B, Tai HY, Lye DC. Nonconcordance with surgical site infection prevention guidelines and rates of surgical site infections for general surgical, neurological, and orthopedic procedures. Antimicrob Agents Chemother. 2011;55(10):4659–4663. doi: 10.1128/AAC.00562-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32(2):101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- 24.National Health and Medical Research Council. Australian Commission on Safety and Quality in Healthcare. Australian guidelines for the prevention and control of infection in healthcare. 2019. https://www.nhmrc.gov.au/about-us/publications/australian-guidelines-prevention-and-control-infection-healthcare-2019. Accessed 9 Dec 2019.
- 25.Care CS of SI and I. Chinese guideline for the prevention of surgical site infection [Chinese language]. Zhonghua Wei Chang Wai Ke Za Zhi. 2019;22(4):301–14. [DOI] [PubMed]
- 26.Indian Council of Medical Research. Hospital infection control guidelines. 2016. https://www.icmr.nic.in/sites/default/files/guidelines/Hospital_Infection_control_guidelines.pdf. Accessed 9 Dec 2019.
- 27.Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat D, et al. Guidelines for the prevention of surgical site infection: the surgical infection society of Thailand recommendations. J Med Assoc Thai. 2020;103(1):99–105. [Google Scholar]
- 28.Indonesian Ministry of Health. Guidelines on the prevention and management of infections [local language]. 2017. http://ditjenpp.kemenkumham.go.id/arsip/bn/2017/bn857-2017.pdf. Accessed 9 Dec 2019.
- 29.Singapore Ministry of Health. National infection prevention and control guidelines for acute healthcare facilities. 2017. https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/guidelines/national-infection-prevention-and-control-guidelines-for-acute-healthcare-facilities---2017.pdf.
- 30.Malaysia Ministry of Health. Policies and procedures on infection control. 2010. http://www.moh.gov.my/moh/images/gallery/Polisi/infection_control.pdf. Accessed 9 Dec 2019.
- 31.Philippines Department of Health. National standards in infection control for healthcare facilities. https://www.doh.gov.ph/sites/default/files/publications/NATIONAL_STANDARDS_IN_INFECTION_CONTROL_FOR_HEALTH.pdf. Accessed 9 Dec 2019.
- 32.National and Public University Infection Control Consortium (Japan). Infection prevention and control guideline [article in Japanese]. 2018. https://kansen.med.nagoya-u.ac.jp/general/gl/gl2018/gl2018.html. Accessed 6 Feb 2020.
- 33.Japan Society for Surgical Infection. Perioperative management guideline for gastrointestinal SSI prevention. 2018. http://www.gekakansen.jp/pdf/guideline2018.pdf. Accessed 1 June 2020. (Article in Japanese).
- 34.Ayub Khan MN, Verstegen DML, Bhatti ABH, Dolmans D, van Mook WNA. Factors hindering the implementation of surgical site infection control guidelines in the operating rooms of low-income countries: a mixed-method study. Eur J Clin Microbiol Infect Dis. 2018;37(10):1923–1929. doi: 10.1007/s10096-018-3327-2. [DOI] [PubMed] [Google Scholar]
- 35.Barker AK, Brown K, Siraj D, Ahsan M, Sengupta S, Safdar N. Barriers and facilitators to infection control at a hospital in northern India: a qualitative study. Antimicrob Resist Infect Control. 2017;6:35. doi: 10.1186/s13756-017-0189-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinshel K, Dramowski A, Hajdu A, et al. Gap analysis of infection control practices in low- and middle-income countries. Infect Control Hosp Epidemiol. 2015;36(10):1208–1214. doi: 10.1017/ice.2015.160. [DOI] [PubMed] [Google Scholar]
- 37.Sandrawati J, Supriyanto S, Nurul T. Recommendations to improve the implementation compliance of surgical safety checklist in surgery rooms. Bul Penelit Sist Kesehat. 2013;17(1):71–79. [Google Scholar]
- 38.Birk S. Accelerating the adoption of a safety culture. Heal Exec. 2015;30(2):18–20, 22–4, 26. [PubMed]
- 39.Wang Z, Chen J, Wang P, et al. surgical site infection after gastrointestinal surgery in China: a multicenter prospective study. J Surg Res. 2019;240:206–218. doi: 10.1016/j.jss.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 40.Zhou J, Ma X. Cost-benefit analysis of craniocerebral surgical site infection control in tertiary hospitals in China. J Infect Dev Ctries. 2015;9(2):182–189. doi: 10.3855/jidc.4482. [DOI] [PubMed] [Google Scholar]
- 41.Morikane K. Infection control in healthcare settings in Japan. J Epidemiol. 2012;22(2):86–90. doi: 10.2188/jea.JE20110085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Catchpole KR, Godden PJ, Giddings AEB, Hirst G, Dale T, Utley M, Gallivan S, de Leval M. Identifying and reducing errors in the operating theatre. Patient Safety Research Programme. 2005. https://www.academia.edu/1319567/Identifying_and_reducing_errors_in_the_operating_theatre. Accessed 1 June 2020.
- 43.Kurup A, Liau KH, Ren J, et al. Antibiotic management of complicated intra-abdominal infections in adults: the Asian perspective. Ann Med Surg. 2014;3(3):85–91. doi: 10.1016/j.amsu.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ariyo P, Zayed B, Riese V, et al. Implementation strategies to reduce surgical site infections: a systematic review. Infect Control Hosp Epidemiol. 2019;40(3):287–300. doi: 10.1017/ice.2018.355. [DOI] [PubMed] [Google Scholar]
- 45.Sartelli M, Kluger Y, Ansaloni L, et al. Knowledge, awareness, and attitude towards infection prevention and management among surgeons: identifying the surgeon champion. World J Emerg Surg. 2018;13:37. doi: 10.1186/s13017-018-0198-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Organization WH. Electronic assessment tool for infection prevention and control. 2012. http://www.emro.who.int/surveillance-forecasting-response/surveillance-infocus/electronic-assessment-tool.html. Accessed 7 Feb 2020.
- 47.Management Sciences for Health. Infection control assessment tool, 2nd ed. 2009. http://siapsprogram.org/wp-content/uploads/2012/05/ICAT-composite_FINAL_May-2009.pdf. Accessed 1 June 2020.
- 48.World Health Organization. Infection prevention and control assessment framework at the facility level. 2018. https://www.who.int/infection-prevention/tools/core-components/IPCAF-facility.PDF. Accessed 15 Dec 2019.
- 49.World Health Organization. Preventing surgical site infections: implementation approaches for evidence-based recommendations. 2018. https://apps.who.int/iris/handle/10665/273154. Accessed 11 Feb 2020.
- 50.World Health Organization. Global guidelines for the prevention of surgical site infection. World Health Organization. 2018. http://apps.who.int/bookorders. Accessed 9 Nov 2019.
- 51.Shankar R. Implementation of the WHO Surgical Safety Checklist at a teaching hospital in India and evaluation of the effects on perioperative complications. Int J Heal Plann Manag. 2018;33(4):836–846. doi: 10.1002/hpm.2533. [DOI] [PubMed] [Google Scholar]
- 52.Abbott TEF, Ahmad T, Phull MK, et al. The surgical safety checklist and patient outcomes after surgery: a prospective observational cohort study, systematic review and meta-analysis. Br J Anaesth. 2018;120(1):146–155. doi: 10.1016/j.bja.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 53.Bergs J, Hellings J, Cleemput I, et al. Systematic review and meta-analysis of the effect of the World Health Organization surgical safety checklist on postoperative complications. Br J Surg. 2014;101(3):150–158. doi: 10.1002/bjs.9381. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization. WHO surgical safety checklist. 2009. https://www.who.int/patientsafety/safesurgery/checklist/en/. Accessed 9 Dec 2019.
- 55.Chaudhary N, Varma V, Kapoor S, Mehta N, Kumaran V, Nundy S. Implementation of a surgical safety checklist and postoperative outcomes: a prospective randomized controlled study. J Gastrointest Surg. 2015;19(5):935–42. [DOI] [PubMed]
- 56.Kasatpibal N, Norgaard M, Jamulitrat S. Improving surveillance system and surgical site infection rates through a network: a pilot study from Thailand. Clin Epidemiol. 2009;1:67–74. doi: 10.2147/CLEP.S5507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garland NY, Kheng S, De Leon M, et al. Using the WHO surgical safety checklist to direct perioperative quality improvement at a surgical hospital in Cambodia: the importance of objective confirmation of process completion. World J Surg. 2017;41(12):3012–3024. doi: 10.1007/s00268-017-4198-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Minhas MS, Muzzammil M, Effendi J. Assessment of safety levels in operation rooms at two major tertiary care public hospitals of Karachi. “Safe Surgery Saves Life”. J Ayub Med Coll Abbottabad. 2017;29(4):580–586. [PubMed] [Google Scholar]
- 59.Leaper DJ, Tanner J, Kiernan M, Assadian O, Edmiston CE., Jr Surgical site infection: poor compliance with guidelines and care bundles. Int Wound J. 2015;12(3):357–362. doi: 10.1111/iwj.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Umscheid CA, Agarwal RK, Brennan PJ. Healthcare Infection Control Practices Advisory Committee. Updating the guideline development methodology of the Healthcare Infection Control Practices Advisory Committee (HICPAC) Am J Infect Control. 2010;38:264–273. doi: 10.1016/j.ajic.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 61.Berrıos-Torres SI. Evidence-based update to the U.S. centers for disease control and prevention and healthcare infection control practices advisory committee guideline for the prevention of surgical site infection: developmental process. Surg Infect. 2016;17:256–261. doi: 10.1089/sur.2015.264. [DOI] [PubMed] [Google Scholar]
- 62.Wisconsin Division of Public Health Service. Supplemental guidance for the prevention of surgical site infections: an evidence-based perspective. Wisconsin Department of Health Services Web site. https://www.dhs.wisconsin.gov/publications/p01715.pdf. Accessed 25 July 2020.
- 63.Agency for Healthcare Research and Quality. Building your SSI prevention bundle: slide presentation. 2017. https://www.ahrq.gov/professionals/quality-patient-safety/hais/tools/surgery/modules/onboarding/build_ssibundle-slides.html. Accessed 9 Dec 2019.
- 64.Keenan JE, Speicher PJ, Thacker JK, Walter M, Kuchibhatla M, Mantyh CR. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014;149(10):1045–1052. doi: 10.1001/jamasurg.2014.346. [DOI] [PubMed] [Google Scholar]
- 65.Tanner J, Padley W, Assadian O, Leaper D, Kiernan M, Edmiston C. Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8,515 patients. Surgery. 2015;158(1):66–77. doi: 10.1016/j.surg.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 66.Zywot A, Lau CSM, Stephen Fletcher H, Paul S. Bundles prevent surgical site infections after colorectal surgery: meta-analysis and systematic review. J Gastrointest Surg. 2017;21(11):1915–1930. doi: 10.1007/s11605-017-3465-3. [DOI] [PubMed] [Google Scholar]
- 67.Waits SA, Fritze D, Banerjee M, et al. Developing an argument for bundled interventions to reduce surgical site infection in colorectal surgery. Surgery. 2014;155(4):602–606. doi: 10.1016/j.surg.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 68.Taylor JS, Marten CA, Munsell MF, et al. The DISINFECT initiative: decreasing the incidence of surgical INFECTions in gynecologic oncology. Ann Surg Oncol. 2017;24(2):362–368. doi: 10.1245/s10434-016-5517-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koek MBG, Hopmans TEM, Soetens LC, et al. Adhering to a national surgical care bundle reduces the risk of surgical site infections. PLoS ONE. 2017;12(9):e0184200. doi: 10.1371/journal.pone.0184200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gorgun E, Rencuzogullari A, Ozben V, et al. An effective bundled approach reduces surgical site infections in a high-outlier colorectal unit. Dis Colon Rectum. 2018;61(1):89–98. doi: 10.1097/DCR.0000000000000929. [DOI] [PubMed] [Google Scholar]
- 71.Liu H, Dong X, Yin Y, Chen Z, Zhang J. Reduction of surgical site infections after cranioplasty with perioperative bundle. J Craniofac Surg. 2017;28(6):1408–12. [DOI] [PubMed]
- 72.Manivannan B, Gowda D, Bulagonda P, Rao A, Raman SS, Natarajan SV. Surveillance, auditing, and feedback can reduce surgical site infection dramatically: Toward zero surgical site infection. Surg Infect (Larchmt). 2018;19(3):313–20. [DOI] [PubMed]
- 73.Miyahara K, Matsuura A, Takemura H, Mizutani S, Saito S, Toyama M. Implementation of bundled interventions greatly decreases deep sternal wound infection following cardiovascular surgery. J Thorac Cardiovasc Surg. 2014;148(5):2381–88. [DOI] [PubMed]
- 74.Yamada K, Abe H, Higashikawa A, et al. Evidence-based care bundles for preventing surgical site infections in spinal instrumentation surgery. Spine (Phila Pa 1976). 2018;43(24):1765–73. [DOI] [PubMed]
- 75.Mok WQ, Ullal MJ, Su S, et al. An integrative care bundle to prevent surgical site infections among surgical hip patients: A retrospective cohort study. Am J Infect Control. 2019;47(5):540–44. [DOI] [PubMed]
- 76.Leaper D, Tanner J, Kiernan M, Assadian O, Edmiston CE. Surgical site infection: poor compliance with guidelines and care bundles. Int J Wound Med. 2015;12:357–362. doi: 10.1111/iwj.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Joint Commission International. Evidence-based principles and practices for preventing surgical site infections. Joint Commission International. 2018. https://www.jointcommissioninternational.org/assets/3/7/JCI_SSI_Toolkit.pdf. Accessed 9 Dec 2019.
- 78.Morikane K, Honda H, Yamagishi T, Suzuki S, Aminaka M. Factors associated with surgical site infection in colorectal surgery: the Japan nosocomial infections surveillance. Infect Control Hosp Epidemiol. 2014;35(6):660–666. doi: 10.1086/676438. [DOI] [PubMed] [Google Scholar]
- 79.Amri R, Dinaux AM, Kunitake H, Bordeianou LG, Berger DL. Risk stratification for surgical site infections in colon cancer. JAMA Surg. 2017;152(7):686–690. doi: 10.1001/jamasurg.2017.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chakravarthy M, Rangaswamy S, George A, Anand T, Senthilkumar P, Arul RS. Risk stratification of surgical site infection in a Tertiary Care Hospital: a prospective case-control study. J Patient Saf Infect Control. 2017;5(2):73–77. [Google Scholar]
- 81.Tartari E, Weterings V, Gastmeier P, et al. Patient engagement with surgical site infection prevention: an expert panel perspective. Antimicrob Resist Infect Control. 2017;6:45. doi: 10.1186/s13756-017-0202-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Totty JP, Harwood AE, Wallace T, Smith GE, Chetter IC. Use of photograph-based telemedicine in postoperative wound assessment to diagnose or exclude surgical site infection. J Wound Care. 2018;27(3):128–135. doi: 10.12968/jowc.2018.27.3.128. [DOI] [PubMed] [Google Scholar]
- 83.Kummerow Broman K, Gaskill CE, Faqih A, et al. Evaluation of wound photography for remote postoperative assessment of surgical site infections. JAMA Surg. 2019;154(2):126–132. doi: 10.1001/jamasurg.2018.3861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Haynes AB, Weiser TG, Berry WR, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf. 2011;20(1):102–107. doi: 10.1136/bmjqs.2009.040022. [DOI] [PubMed] [Google Scholar]
- 85.van Buijtene A, Foster D. Does a hospital culture influence adherence to infection prevention and control and rates of healthcare associated infection? A literature review. J Infect Prev. 2019;20(1):5–17. doi: 10.1177/1757177418805833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Van Mourik MSM, Perencevich EN, Gastmeier P, Bonten MJM. Designing surveillance of healthcare-associated infections in the era of automation and reporting mandates. Clin Infect Dis. 2018;66(6):970–976. doi: 10.1093/cid/cix835. [DOI] [PubMed] [Google Scholar]
- 87.Van Rooden SM, Tacconelli E, Pujol M, et al. A framework to develop semiautomated surveillance of surgical site infections: an international multicenter study. Infect Control Hosp Epidemiol. 2019;41(2):194–201. doi: 10.1017/ice.2019.321. [DOI] [PubMed] [Google Scholar]
- 88.Mohamed N, Wang MY, Le Huec JC, et al. Vaccine development to prevent Staphylococcus aureus surgical-site infections. Br J Surg. 2017;104(2):e41–e54. doi: 10.1002/bjs.10454. [DOI] [PubMed] [Google Scholar]
- 89.Reinbold J, Uhde AK, Ller IM, et al. Preventing surgical site infections using a natural, biodegradable, antibacterial coating on surgical sutures. Molecules. 2017;22(9):1–15. doi: 10.3390/molecules22091570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arora A, Aggarwal G, Chander J, Maman P, Nagpal M. Drug eluting sutures: a recent update. J Appl Pharm Sci. 2019;9(7):111–123. doi: 10.7324/JAPS.2019.90716. [DOI] [Google Scholar]
- 91.Fleming D, Rumbaugh K. Approaches to dispersing medical biofilms. Microorganisms. 2017;5(2):15. doi: 10.3390/microorganisms5020015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fitzpatrick F, Doherty A, Lacey G. Using artificial intelligence in infection prevention. Curr Treat Options Infect Dis. 2020 doi: 10.1007/s40506-020-00216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Paik AM, Granick MS, Scott S. Plastic surgery telehealth consultation expedites Emergency Department treatment. J Telemed Telecare. 2017;23(2):321–327. doi: 10.1177/1357633X16639459. [DOI] [PubMed] [Google Scholar]
- 94.Parisien RL, Shin M, Constant M, Saltzman BM, Li X, Levine WN, Trofa DP. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28(11):e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hung AJ, Chen J, Shah A, Gill IS. Telementoring and telesurgery for minimally invasive procedures. J Urol. 2018;199(2):355–369. doi: 10.1016/j.juro.2017.06.082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were used in the development of this consensus manuscript.