ABSTRACT
Limited data exist regarding pneumococcal vaccination coverage among the elderly in Middle Eastern countries including Jordan. The pharmacists’ role in improving vaccine acceptance has become increasingly evident. Yet, large-scale studies of the assessment of the pharmacists’ role on pneumococcal vaccines acceptance among the elderly are scarce. Hence, we assessed for the first time the current state of knowledge and pneumococcal vaccination coverage among the elderly and the role of pharmacist-led educational intervention on the attitude, awareness, vaccine acceptance, and prompts for physician consultation regarding pneumococcal vaccines in Jordan. This interventional study enrolled 916 randomly selected adults aged ≥ 65 years in Amman, Jordan. We showed that only 3.9% of the participants have ever heard about pneumococcal disease with 0.5% vaccination coverage. Immediately after educational intervention, 21.7% of the participants perceived pneumococcal disease as a threat, 52.1% of them believed in the importance of the vaccine, and 93.9% of them were willing to consult a physician in this regard. At a two-month follow-up, 30.5% had a positive attitude toward the vaccine and 36% consulted their physician regarding the vaccine. Vaccination coverage was significantly increased to 1.9% (P value = 0.008). The main obstacles against vaccination were a negative attitude and that physicians had not recommended the vaccine. Vaccine uptake was significantly associated with physician consultation (P value = 0.011). Insurance, employment, attitude, and reading the booklet significantly predicted physician consultation. In conclusion, very low pneumococcal vaccination coverage was observed among the elderly in Jordan. Enrollment of pharmacists in immunization education and recommendation is suggested to improve pneumococcal vaccine coverage among the elderly in Jordan.
KEYWORDS: Pneumococcal vaccine, Streptococcus pneumoniae, elderly, pharmacist, vaccination, pharmacy practice, education, immunization, vaccine acceptance, vaccination coverage
Introduction
Streptococcus pneumoniae (S. pneumonia) infection is associated with major global health problems including bacterial pneumonia, meningitis, otitis media, and bacteremia.1,2 The groups at highest risk of this infection are pediatric, elderly, and immunocompromised patients.1,2 S. pneumoniae is the most frequently encountered microbial agent in community-acquired pneumonia (CAP).3,4,5 CAP is associated with considerable worldwide morbidity and mortality, especially among the elderly where the risk of death is associated with advanced age and the presence of comorbidities.3 According to the WHO and the Centers for Disease Control and Preventions in America (CDC), the morbidity and mortality rates due to pneumococcal disease are high in the developing countries in Africa and Asia.6,7
Due to the increased risk of pneumococcal disease among the elderly, the Advisory Committee on Immunization Practices (ACIP) recommended in 2019 that all adults aged ≥ 65 years should receive a single dose of pneumococcal polysaccharide vaccine 23 (PPSV23) while shared clinical decision-making is recommended regarding the administration of PCV13.8 Data on the global coverage of pneumococcal vaccine among the elderly is still not available. However, vaccine coverage among the elderly varies between 30 and 70% in different countries such as the United States, Australia, Japan, and France.9,10,11,12 In Middle Eastern countries, limited data exist on vaccine coverage among this age group. Thus, one of the aims of the current study was to assess pneumococcal vaccine coverage among the elderly in Jordan.
Vaccine acceptance and coverage are influenced by patient awareness and health care provider recommendations.13,14 Pneumococcal vaccine acceptance has been shown before to be significantly associated with elderly patients’ knowledge about the disease risk, the efficacy, and the availability of the vaccine in the United States.13 Various other reports addressed the knowledge, awareness, and practice (KAP) of the elderly in Pakistan, Germany and Singapore in regard to pneumococcal vaccines.14–16 However, there have been no such reports made in Middle Eastern countries including Jordan.
The role of health care providers in vaccine acceptance is crucial to attain optimum vaccine coverage.13 The role of pharmacists in immunization practice is increasingly accepted.17 Several countries authorize vaccinations in pharmacies and/or by pharmacists, such as the United Kingdom and the United States.18 However, in Jordan, pharmacists are only advocates to educate and motivate patients for vaccination.18 Recently, variable trends have been reported toward a positive impact of pharmacist/pharmacist intern or extender on pneumococcal vaccination rates among the elderly in a small scale-study,19 or in all vaccine-qualifying adults in the community.20 Therefore, there is a need to further clarify the role of pharmacist-led counseling on pneumococcal vaccine acceptance among the elderly in a large-scale study.
Given the current lack of data on vaccine coverage, KAP, and the role of pharmacist-led educational intervention regarding pneumococcal disease and its vaccine among the elderly in the Middle East, we sought in the current large-scale interventional study to assess for the first time pneumococcal vaccine coverage in Jordanian adults aged ≥ 65 and find out the determinants of vaccine uptake in this category of the Jordanian population. In addition, the impact of a pharmacist-led educational intervention on elderly patients’ attitude toward pneumococcal vaccines, willingness to get vaccinated, consultation of a physician in this matter, or vaccine uptake were also assessed.
Methods
Study design and setting
In this study, we assessed the coverage of pneumococcal vaccines (PPSV-23 and PCV13) among the elderly awareness of the pneumococcal disease and its vaccine, and the impact of pharmacist-led educational intervention in this group of patients on the two outcome measures of increasing vaccination coverage and encouraging participants to consult a physician regarding the vaccine. Influenza vaccine coverage among the participants was also assessed because of the higher risk of secondary pneumococcal infection in patients with influenza.21 Adults aged ≥ 65 years were recruited through the out-patient clinic in several hospitals and public places in Amman, the capital of Jordan. The study took place between June 2019 and February 2020. The Institutional Review Board (IRB) at the University of Jordan Hospital approved the study protocol and the questionnaire (IRB no. 215/2016).
Study population
A target sample of 700 adults aged ≥ 65 was estimated based on the following equation: N = , where N is the sample size; Zα: type one error = 1.96 when α = 5%; Zβ: type two error = 1.28 when β = 10%; Q = 1-P: expected nonprevalence; P = proportion in the population possessing the characteristic of interest (based on the estimate that pneumococcal vaccine coverage is similar to the average of influenza vaccine coverage among adults in Jordan [20%]);22 and d = one-half of the desired interval of confidence in this study d = 5%. To account for possible dropouts, the sample size was inflated to 1,000 participants.
Consenting adults were eligible if they were ≥ 65 years old and were cognitively intact, as defined by a score of four or more correct items on a six-item cognitive screen.23,24 If cognitive impairment was likely (a score less than four), the care giver was interviewed. Participants were excluded if they were cognitively impaired and a care giver was not available.
Study procedure
The questionnaire and the educational booklet employed were built after reviewing related literature7,22,25 and were critically evaluated and face-validated by several colleagues in the field of clinical pharmacy. A pilot sample of 40 participants (5% of the target sample size) was conducted. Participants were first assessed for cognitive impairment by the researcher pharmacist, and when impairment was likely, the care giver was interviewed. The participants were then enrolled into a 30–45 min interview to elicit participants’ demographics and past medical history including self-reported health status, risk factors for invasive pneumococcal disease, risk factors for pneumococcal carriage, the number of medical provider visits during past 6 months, and current seasonal influenza and pneumococcal disease immunization status. If the participants had heard about the disease or its vaccine before, their knowledge and attitude in regard to pneumococcal disease and its vaccine were explored. Knowledge questions included awareness of the different forms of pneumococcal disease (pneumonia, otitis media, sinusitis, meningitis, and septicemia), the highest risk groups of this disease (children less than 2 years of age and adults aged ≥ 65 years), and the main prevention measures. Participants were then asked whether they thought they were at risk for pneumococcal diseases and whether they thought that pneumococcal vaccines are effective. Determinants of vaccine acceptance or refusal were also identified by asking the participants to choose from a list of reasons that encouraged them or discouraged them from being vaccinated. An educational booklet was provided to all participants and discussed by the pharmacist to disseminate the risk of the disease, the disease transmission, pneumococcal vaccines' (PPSV23 and PCV13) indications, and possible side effects as per guideline recommendations. Participants’ attitudes toward the vaccine and willingness for future vaccine acceptance or for consulting a physician about the vaccine were assessed immediately after the interview. Those with a positive attitude toward the vaccine were invited to provide a contact phone number. Two months later, participants were phoned to assess their reading of the booklet, their attitude toward pneumococcal vaccines, immunization status, whether they had consulted a physician regarding the vaccine, and to identify the obstacles against vaccinations if any. An identification text message and four phone call attempts on four different days were tried before considering the patient as nonrespondent.
Statistical analysis
Statistical analysis was carried out using SPSS version 20.0 (SPSS Inc., Chicago, IL). Categorical variables were presented as percentages with frequencies, whereas continuous variables were presented as median with an interquartile range (IQR). Bivariate analyses using Pearson’s chi-square, Fisher’s exact, or Eta tests were conducted as appropriate to find associations between the outcome measure of “physician consultation regarding pneumococcal vaccines” and the potential determinants. A multiple logistic regression was developed including the covariates that were identified through bivariate analyses to be significantly associated with the outcome measures. The “No” answer for physician consultation was encoded 0 and the “Yes” answer was encoded 1. The McNemar test was used to assess the outcome measure of “increasing vaccine uptake after the educational interventional” by comparing vaccine coverage before and after the educational intervention. All hypotheses testing were two-sided. A P value of < 0.05 was considered to be statistically significant. Participants’ responses regarding knowledge were measured using “yes,” “no,” and “I do not know” choices.
Results
General characteristics of participants
Of the 1,076 older adults approached, 936 consented to participate with 87% response rate. Twenty participants (2.1%) were excluded due to a violation of age criterion. Cognitive impairment was likely in 7.9% (n = 72) of the participants, but care givers were available and interviewed, so those participants were not excluded. Consequently, a total of 916 participants were enrolled in the study (Figure 1).
Figure 1.
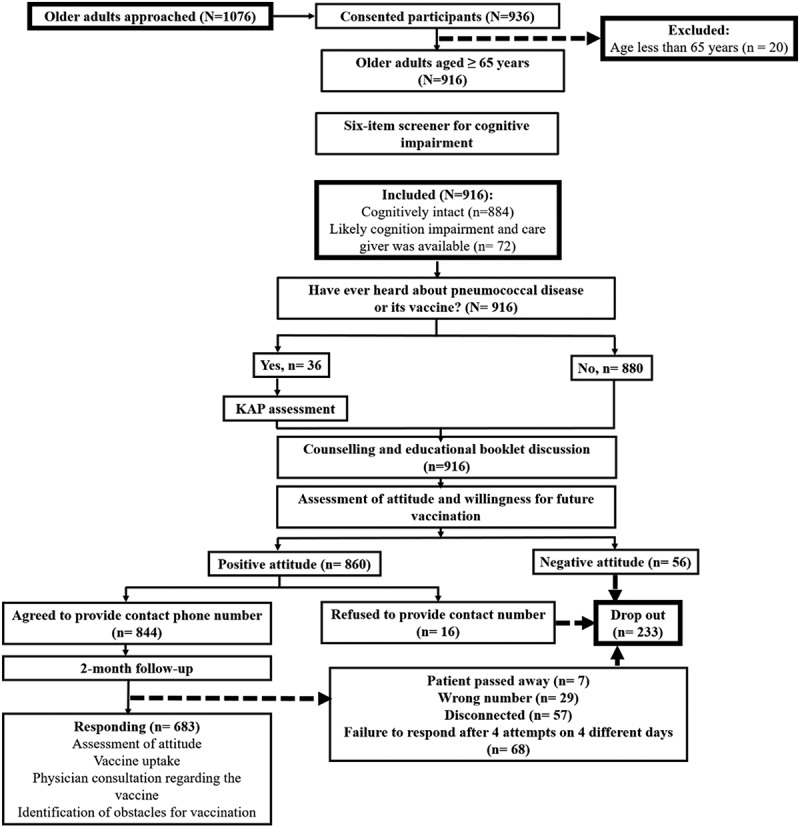
Flowchart of participant enrollment, data collection, educational interview, and follow-up. KAP; knowledge, attitude, and practice
The median age of the participants was 70 ± 7 (IQR) years (65–90 years). The sociodemographic characteristics of the participants are shown in Table 1. Only 3.9% (n = 36) had ever heard about pneumococcal pneumonia and its vaccine. Twenty-three % (n = 211) had had a seasonal influenza vaccine before.
Table 1.
Sociodemographic characteristics of the participants and their association with the outcome measure “A physician consultation regarding pneumococcal vaccines”
| %a(n) | %b(n) | P-valuec | |
|---|---|---|---|
| Age (median ± IQR)d | 70.0 ± 7 | 70.0 ± 7 | 0.188 |
| Gendere | |||
| Male | 19.3% (177) | 21.2% (145) | 0.007* |
| Female | 80.7% (739) | 78.8% (538) | |
| Cognitive impairmente | |||
| Impairment likely | 7.9% (n = 72) | 7.8% (53) | 0.786 |
| Impairment less likely | 92.1% (n = 844) | 92.2% (630) | |
| Educational levele | |||
| ≤High school | 72.6% (665) | 71.7% (490) | 0.027* |
| ≥College or higher | 27.4% (251) | 28.3% (193) | |
| Incomee | |||
| ≤500 JD | 83.1% (761) | 83% (567) | 0.005* |
| >500 JD | 16.9% (155) | 17% (116) | |
| Employmente | |||
| Full or part time | 3.2% (29) | 4% (28) | 0.001* |
| Unemployed | 96.8% (887) | 96% (655) | |
| Working in the medical fielde | |||
| Yes | 2.8% (26) | 2.8% (19) | 0.296 |
| No | 97.2% (890) | 97.2% (664) | |
| Marital statuse | |||
| Married | 62.6% (573) | 65.9% (450) | 0.393 |
| Others (widow, divorced, single) | 37.4% (343) | 34.1% (233) | |
| Number of sonse | |||
| ≤ 3 | 14.2% (130) | 14.1% (96) | 0.089 |
| >3 | 85.8% (786) | 85.9% (587) | |
| Medical insurancee | |||
| Yes | 94.2% (863) | 94% (642) | 0.000* |
| No | 5.8% (53) | 6% (41) | |
| Smoking statuse | |||
| Yes | 5.5% (50) | 6.1% (42) | 0.171 |
| No | 94.5% (866) | 93.9% (641) | |
| Self-described health statuse | |||
| Excellent | 4.4% (40) | 5% (34) | 0.955 |
| Very good | 12.6% (115) | 12.7% (87) | |
| Good | 66.2% (606) | 67.4% (460) | |
| Poor | 15.3% (140) | 14.2% (97) | |
| Very poor | 1.6% (15) | 0.7% (5) | |
| Medical provider visits during the past 6 monthse | |||
| ≤ 3 | 54.5% (499) | 55.9% (382) | 0.385 |
| >3 | 45.5% (417) | 44.1% (301) | |
| Having care giver at homee | |||
| Yes | 48.9% (448) | 47.6% (325) | 0.343 |
| No | 51.1% (468) | 52.4% (358) | |
| Having ever heard about pneumococcal pneumonia and its vaccinee | |||
| Yes | 3.9% (36) | 4% (27) | 0.01* |
| No | 96.1% (880) | 96% (656) | |
| Seasonal influenza vaccine uptakee | |||
| Yes | 23.0% (211) | 23.7% (162) | 0.044* |
| No or not sure | 77% (705) | 76.3% (521) |
IQR: interquartile range; JD: Jordanian Dinar.
avalid percent of the whole study population (N = 916).
bvalid percent of the participants who completed the study (n = 683)
cA Pvalue of less than 0.05 indicate a significant association of the covariate with a high likelihood of a physician consultation among the participants who completed the study (n = 683)
dEta test, Eta coefficient is presented.
ePearson’s chi-square test.
Risk factors for invasive pneumococcal disease and pneumococcal carriage
The study participants were assessed for the risk factors for invasive pneumococcal disease as described by ACIP8 (Table 2). Aside from being elderly, 5.5% were smokers, and 70.7% had at least one risk factor for invasive pneumococcal disease. The most frequently reported risk factors were diabetes (n = 478, 52.2%), coronary artery disease (n = 159, 17.4%), and myocardial infarction (n = 120, 13.1%). Immunocompromising conditions (chronic kidney disease, nephrotic syndrome, leukemia, lymphoma, drug- or radiation-induced immunosuppression, and solid organ transplant) were documented in 9% (n = 83) of the participants. None of the participants had Hodgkin disease, multiple myeloma, generalized malignancy, cerebrospinal fluid leak, cochlear implant, congenital or acquired immunodeficiency, or spleen dysfunction.
Table 2.
Risk factors for invasive pneumococcal disease and pneumococcal carriage (N = 916)
| Factor | %a(n) |
|---|---|
| Risk factors for invasive pneumococcal disease | |
| Chronic kidney disease | 4.4% (40) |
| Nephrotic syndrome | 0.1%(1) |
| leukemia | 0.3% (3) |
| lymphoma | 0.3% (3) |
| Cerebrovascular disease | 2.7% (25) |
| Liver disease | 0.9%(8) |
| Drug- or radiation- induced immunosuppression | 3.8% (35) |
| Solid organ transplant | 0.1% (1) |
| Sickle cell disease and hemoglobinopathies | 0.2% (2) |
| Myocardial Infarction | 13.1% (120) |
| Coronary artery disease | 17.4% (159) |
| Peripheral vascular disease | 1.6% (15) |
| Asthma | 7.0%(64) |
| COPD | 0.4% (4) |
| Diabetes | 52.2% (478) |
| Risk factors for pneumococcal carriage | |
| Contact with children aged <2 at least once a month. | 62.6% (573) |
| Contact with children aged 2–12 at least once a month. | 87.2% (799) |
| Sharing bedroom with other family members. | 34.2% (313) |
| Antibiotic use within the past 6 months. | 47.8% (438) |
aValid percent.
The study participants were also checked for the risk factors for pneumococcal carriage.24 Besides smoking, almost the whole study population had risk factors for carriage (n = 876, 95.6%). The majority of them had contact with children at least once a month and almost half of them had used antibiotics within the past 6 months.
Baseline vaccination coverage and knowledge about pneumococcal disease and its vaccine
Only 3.9% (n = 36) of the study population had ever heard about pneumococcal disease or its vaccine, and only 0.5% (n = 5) had ever had a pneumococcal vaccine (n = 3, 0.3% of PCV13 and n = 2, 0.2% of PPSV23). Of those who had heard about the disease, 52.8% (n = 19) had taken seasonal influenza vaccine. In addition, 52.8% (n = 19) thought that they were at risk of pneumococcal disease and 61.1% (n = 22) believed in the efficacy and health benefits of the vaccine. The two reported factors for pneumococcal vaccine uptake were worries of catching pneumonia (n = 2) and following physician advice (n = 3).
As presented in Table 3, more than half of those who had heard about pneumococcal disease correctly recognized the definition of pneumococcal infection and knew the availability of an effective vaccine. The majority of them recognized the high risk group of this infection (elderly and children younger than 2 years old) and the route of transmission.
Table 3.
Knowledge of participants who have heard about pneumococcal disease and its vaccine and the obstacles and determinants of vaccine uptake (n = 36)
| Knowledge about pneumococcal infection | %a(n) |
|---|---|
| Pneumococcal infection is the principal causative agent of bacterial pneumonia, otitis media, sinusitis, meningitis and septicemia. | 55.6% (20) |
| Children younger than 2 years old are at high risk of these infection. | 77.8% (28) |
| Elderly aged ≥65 years are at risk of invasive pneumococcal disease. | 80.6% (29) |
| Pneumococcal bacteria can spread from person to person by direct contact with respiratory secretions, like saliva or mucus. | 94.4% (34) |
| Effective vaccine is available to prevent invasive pneumococcal disease in elderly. | 55.6% (20) |
| Washing hands with soap and water after coughing/sneezing can prevent the spread of the disease. | 97.2% (35) |
| Reasons for not getting vaccinated (as specified by those who have not had the vaccine before) | |
| Unaware of its importance. | 19.4% (7) |
| Healthy people do not need it. | 16.7% (6) |
| Do not think that the vaccine is effective. | 5.6% (2) |
| Fear of contracting illness. | 8.3% (3) |
| Unaware of vaccine availability. | 47.2% (17) |
| Concerns of the side effects of the vaccine. | 16.7% (6) |
| Do not consider pneumococcal illness as a threat. | 2.8% (1) |
| Cost of the vaccine. | 8.3% (3) |
| Factors that would encourage the participants to get vaccinated in the future (as specified by all the participants regardless of vaccination status) | |
| If it is provided by the government for free. | 86.1% (31) |
| If the vaccine was tested more thoroughly for safety and efficacy. | 94.4% (34) |
| If it is recommended by a physician. | 97.2% (35) |
| If it is cheaper. | 83.3% (30) |
aValid percent.
The most commonly reported obstacle against vaccine uptake was the unawareness of vaccine availability (n = 17, 47.2%) and unawareness of its importance (n = 7, 19.4%). The most important determinant of vaccine uptake in the future was physician recommendation (n = 35, 97.2%; Table 3).
The reported sources of information were books (n = 14, 38.9%), friends (n = 10, 27.8%), physician office (n = 7, 19.4%), television (n = 3, 8.3%), internet (n = 1, 2.85), and social media (n = 1, 2.8%).
Participant attitudes and beliefs toward pneumococcal disease and its vaccine after the educational interview
All participants (n = 916) were interviewed and counseled by the pharmacist and were administered an educational booklet. Participants’ attitude and beliefs were assessed immediately after the educational interview where 21.7% (n = 199) of them perceived pneumococcal disease as a health threat and more than half of the participants (n = 477, 52.1%) believed in the health benefits of pneumococcal vaccines. The majority of the participants (n = 860, 93.9%) were willing to consult their physician to get the vaccine. Eighty-one % of the participants (n = 742) provided a contact phone number for a follow up phone call. The perception of pneumococcal disease as a health threat and the belief in the health benefits of the vaccine were significantly associated with a high likelihood of physician consultation regarding pneumococcal vaccines (Pearson’ chi-square test, P value = 0.000, 0.002, respectively).
Participants’ attitudes, beliefs, and practice at two-month follow-up
Two months later, patients were phoned, and 683 participants responded and completed the whole study protocol with a response rate of 74.6%. Of them, 46.1% (n = 315) read the educational booklet again, 30.5% (n = 208) thought that the vaccine was important for their health, and 36% (n = 246) consulted their physician regarding the vaccine. Reading the booklet and the belief in the importance of the health benefits of the vaccine were associated with a higher likelihood of physician consultation (Pearson’s chi-square, P value < 0.005, P value < 0.005, respectively).
Regarding pneumococcal vaccine uptake, a statistically significant increase in vaccine coverage was observed, where 1.9% (n = 13) had had a pneumococcal vaccine (n = 8, 1.2% of PCV-13 and n = 5, 0.6% of PPSV23) by the two-month follow-up as compared to the base-line level of 0.5% (n = 5) (McNemar test, P value = 0.008, OR = 84.88, CI = 42.62–169). Therefore, the pharmacist- administered educational intervention significantly improved pneumococcal vaccine coverage. The practice of getting the vaccine by the two-month follow-up was significantly associated with a high likelihood of physician consultation with 75% (n = 9) of those who got vaccinated had consulted the physician before (Fisher’s Exact test, P value = 0.011).
Assessment of the obstacles against vaccination revealed that other than the negative attitude toward the importance of the vaccine, the most commonly reported obstacle was that physicians had not recommended the vaccine after consultation, followed by the concern of side effects and the price (Table 4).
Table 4.
Obstacles against pneumococcal vaccine uptake (n = 683)
| Factor | %a(n) |
|---|---|
| Do not think the vaccine is important for their health. | 45.5% (311) |
| The physician had not recommended it | 25.6% (175) |
| Concern of side effects. | 23.1% (158) |
| Price. | 22.3% (152) |
| Fear of contracting illness. | 13.8% (94) |
| Time limitation. | 8.8% (55) |
| Not convinced of its efficacy. | 4.4% (30) |
| Availability of the vaccine. | 1.6% (11) |
| Do not consider pneumococcal disease as a threat. | 1.5% (10) |
Multiple logistic regression model for the predictors associated with a high likelihood of physician consultation regarding pneumococcal vaccines
The covariates which were identified to be significantly associated with a high likelihood of physician consultation through bivariate analyses were entered into a multiple logistic regression model. The results in Table 5 show four predictors with significant influence on the outcome measure. Participants who were employed (full or part time) or insured were almost 3.5 times and 5 times more likely to consult a physician, respectively. Those who believed in the health benefits of pneumococcal vaccines and those who had read the booklet were almost three times and two times more likely to consult a physician regarding the vaccine, respectively.
Table 5.
Multiple logistic regression results for the covariates associated with a high likelihood of a physician consultation regarding pneumococcal vaccine among the participants who completed the study
| B | S.E | Pvalue | OR | 95% C.I. | |
|---|---|---|---|---|---|
| Gender Male femalea |
−0.077 | 0.249 | .756 | 0.926 | 0.568–1.509 |
| Level of education High school or lower College or highera |
0.203 | 0.230 | .378 | 1.225 | 0.781–1.922 |
| Income ≤500 JD >500 JDa |
−0.347 | 0.249 | .164 | 0.707 | 0.434–1.152 |
| Employment Full or part time unemployeda |
1.252 | 0.484 | .010 | 3.497 | 1.355–9.029 |
| Insurance Yes Noa |
1.564 | 0.562 | .005 | 4.780 | 1.590–14.368 |
| Having ever heard about pneumococcal pneumonia and its vaccine Yes Noa |
0.308 | 0.439 | .484 | 1.360 | 0.575¬-3.218 |
| The perception of pneumococcal disease as a health threat Yes No or Not surea |
0.386 | 0.205 | .059 | 1.471 | 0.985¬-2.196 |
| The belief in the health benefits of the vaccine (educational interview) Yes No or Not surea |
0.134 | 0.184 | .466 | 1.143 | 0.798–1.639 |
| The belief in the health benefits of the vaccine (two-months follow-up) Yes No or Not surea |
1.192 | 0.195 | .000 | 3.294 | 2.247–4.827 |
| Reading the booklet Yes Noa |
0.666 | 0.186 | .000 | 1.947 | 1.351–2.806 |
| Constant | −2.883 | 0.645 | .000 | 0.056 |
OR; odds ratio.
aReference category.
*Significant at P value < 0.05.
Dropouts of the study
At the end of the first educational interview, 56 participants (6.1% of 916) were not willing to contact a physician regarding the vaccine and they refused to participate in the two-month follow up. Thus, 860 participants (93.9%) were willing to contact a physician regarding the vaccine. However, 1.86% (n = 16) of the participants refused to give a follow-up contact phone number, 3.37% (n = 29) of them provided a wrong phone number, 6.63% (n = 57) had disconnected phone numbers, 7.90% (n = 68) did not answer their phones after four attempts on four different days and after sending an identification text message, and 0.81% (n = 7) passed away. Therefore, of the whole study population, 683 were enrolled in the two-month follow-up and completed the study (Figure 1).
Discussion
Limited data exist on pneumococcal vaccination coverage in Middle Eastern countries including Jordan. As vaccination coverage is influenced by patient awareness and health care provider’s recommendation,13,17 we assessed in this study, for the first time in the Middle East, pneumococcal vaccination coverage among the elderly in Jordan and their awareness and attitude regarding the pneumococcal disease and its vaccine. Small-scale studies were conducted before regarding the impact of pharmacists on pneumococcal vaccine uptake among the elderly.17,19 Worldwide, this is the first large-scale study to investigate the impact of pharmacist-driven educational intervention on pneumococcal vaccine uptake among the elderly, and it is the first study to evaluate the role of pharmacists in promoting vaccination in the Middle East. The results of this study provide implications for health policy makers regarding pneumococcal vaccination coverage among the elderly in Jordan, determinants and factors that might increase vaccine uptake, and insights into the role of pharmacists in promoting patient awareness, attitude, and vaccine uptake or physician consultation in this regard.
In this report, we showed that the majority of the elderly population in Jordan have at least one risk factor for invasive pneumococcal disease (70%) including diabetes (52.2%), coronary artery disease and myocardial infarction (30.5%), and immunocompromising conditions (9%). Besides these, they have at least one risk factor for pneumococcal carriage (95.6%) where most of them have at least monthly contact with a child younger than 12 years old. This is critically important knowing that PCV13 is not included in the child national immunization program in Jordan and that pediatric PCV13 uptake in Amman was 12.5% in 2016.26 This might negatively influence the herd immunity effect child vaccination impart on elderly protection. In addition, only 23% of the population in this study had a seasonal influenza vaccine before suggesting that the majority of them are at risk of pneumococcal superinfection which is greater in individuals who develop influenza.21 Of note, influenza vaccination coverage among elderly obtained in this study is comparable to the one observed among adults before (20%).22 Despite this high risk of pneumococcal disease and its complications among the elderly in Jordan, only 3.9% of the participants had ever heard about pneumococcal disease and its vaccine and only 0.5% had ever been administered a pneumococcal vaccine. This indicates a state of severe knowledge and awareness deficit that participants have regarding this condition. This could justify the very low vaccination coverage in this category of the population where pneumococcal vaccine acceptance among the elderly was shown before to be significantly associated with patients’ knowledge and awareness about the disease and its vaccine in the United States and Germany.15,17 In a study in Germany, 28.2% of the elderly participants were aware that a pneumococcal vaccine is recommended for them, this was associated with a vaccination rate of 11.5%.15 Compared to worldwide vaccination rates, the vaccination rate among elderly in Jordan was much lower than that reported in other countries, which ranges between 7.8% and 75%.9–12,14-16
Our data shows that half to almost the majority of those who had heard about pneumococcal disease correctly recognized the knowledge questions asked, and those who were vaccinated in this study belong to this category of participants (who had heard about pneumococcal disease or its vaccine). Valid inferential statistics related to this subgroup of the study population could not be performed due to their small proportion.
In this report, the approach followed in pharmacist intervention relied on the current advocate role pharmacists have in Jordan which does not legally comprise authorization for vaccine prescription or administration.18 The principal pharmacist intervention in this study was to counsel the participants and to administer an educational booklet that increases disease risk perception, raises the awareness regarding the importance of the vaccine, and motivates the participants to consult the physician. This was reflected in prompting participants to consult a physician in regard to the vaccine, and consequently, vaccine uptake. Of note, the assessment of the baseline of the participants’ knowledge, attitude, and perception toward the disease and its vaccine prior to the educational intervention was only performed for 36 participants who had heard about the disease or its vaccine before. However, for the majority of the study population (96.1%), the assessment of the attitude and perception prior to the educational intervention could not be performed as they have never heard about the disease and its vaccine before. Immediately after the educational interview, pharmacist interventions resulted in about a quarter of the participants’ perceived pneumococcal disease as a health threat, half of them believed in the health benefit of the vaccine, and the majority of them were willing to consult a physician in this regard. At the two-month follow-up, almost one-third of the participants thought that the vaccine was important for their health and consulted a physician regarding the vaccine. Interestingly, we showed that the practice of getting the vaccine at the two-month follow-up was significantly associated with a high likelihood of physician consultation. Subsequently, vaccination coverage was significantly increased from 0.5% to 1.9% with the main reported obstacle for not having received the vaccine was that a physician had not recommended the vaccine upon consultation. Therefore, it is suggested that health authorities should highlight the disease vulnerability of this category of the population and encourage pneumococcal vaccination practice by physicians. In addition, the pharmacist-led educational intervention employed in this study improved participants’ attitude, awareness, physician consultation regarding the pneumococcal vaccine, and contributed to the improved vaccine acceptance. Hence, it is suggested to engage pharmacists in pneumococcal vaccine immunization programs in Jordan. Globally, several opportunities for pharmacists to recommend and administer routine vaccines were documented.27 In particular, pharmacists have consistently been shown to increase pneumococcal vaccination rates in the United States.27 Among the elderly, a positive perception toward the acceptance of pneumococcal vaccines following pharmacist recommendation was shown in small-scale studies in the United States.13,19
The results of the multiple logistic regression model in the current report demonstrated that a physician consultation regarding pneumococcal vaccines was associated with socioeconomic factors such as being insured or employed. In a study in Pakistan, the elderly with a low socioeconomic status had less awareness and lower vaccination rates than those with a higher socioeconomic status.14 In Singapore, a higher level of education and higher monthly household income were associated with pneumococcal vaccine uptake among the elderly.16 In the current study, participants’ attitude toward the vaccine and reading the educational booklet were also significantly associated with high likelihood of consulting a physician which implies that awareness and attitude are important factors in modifying individual practice.
The most important barriers against vaccine acceptance in this study were a negative attitude regarding the importance of the vaccine and that a physician had not recommended the vaccine upon consultation. These barriers were listed amongst the reasons of vaccine hesitancy among the elderly.28 Physician recommendation has always been considered a critical contributor to patients’ awareness concerning infectious diseases and their vaccines.22,25,29,30 The lack of awareness about the need for the vaccine and the absence of physician recommendation were the most important reasons for not having received the vaccine among the elderly in United States,17 and that the presence of a regular family doctor to consult for health problems was associated with higher pneumococcal vaccine uptake among the elderly in Singapore.16 In a study in Germany, the majority of the participating elderly perceived physicians to be an appropriate source of information regarding vaccinations.15 Thus, a physician consultation is the most important determinant of pneumococcal vaccine uptake among the elderly. However, physicians’ vaccine hesitancy might be a problem against maintaining successful vaccination programs.31 Future studies are therefore required to address physicians’ knowledge and attitude regarding the pneumococcal vaccine and its health benefits for elderly. In our study, the majority of the participants had good health care access with almost half of them having had more than three medical provider visits in the past 6 months. Therefore, access to health care services was not a barrier against vaccination. Other reported barriers against vaccine uptake in our study were the concern of side effects and the price of the vaccine. Therefore, reassuring the elderly population about the safety of the vaccine and offering the vaccine at reduced prices through national or international support are recommended.
Although we present here interesting findings, this study has some limitations. Data should be carefully generalized as the study was conducted in Amman only and therefore may not be necessarily representative of the whole elderly population in Jordan. In addition, the assessment of the attitude and perception prior to the educational intervention could not be performed for the majority of the participants as they had never heard about the disease and its vaccine before. Out-of-pocket expenses for insured patients were not checked in this study while this might contribute to participants’ acceptance or refusal of the vaccine.
In conclusion, a severe knowledge and awareness deficit present among the elderly in Jordan explains the very low vaccine coverage. Pharmacist-led educational intervention improved participants’ awareness and attitude regarding the disease and its vaccine which was significantly associated with a physician consultation in this regard. This was reflected in a significant improvement in pneumococcal vaccine coverage with the main obstacle against vaccination was that a physician had not recommended the vaccine upon consultation. Enrollment of pharmacists in immunization practice would probably increase vaccination rates among the elderly in Jordan. Further studies are required to assess patients’ perceptions toward the pharmacists’ role as immunizers.
Acknowledgments
We would like to thank the Deanship of Scientific Research (DSR) at the University of Jordan for the financial support of this work. This work has been carried out during sabbatical leave granted to the author (Eman Y Abu-rish) from the University of Jordan during the academic year 2019/2020.
Funding Statement
This work was supported by the Deanship of Scientific Research (DSR) at the University of Jordan.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Engholm DH, Kilian M, Goodsell DS, Andersen ES, Kjærgaard RS.. A visual review of the human pathogen Streptococcus pneumoniae. FEMS Microbiol Rev. 2017;41(6):854–79. doi: 10.1093/femsre/fux037. [DOI] [PubMed] [Google Scholar]
- 2.Daniels CC, Rogers PD, Shelton CM. Review of pneumococcal vaccines: current polysaccharide vaccine recommendations and future protein antigens. J Pediatr Pharmacol Ther. 2016;21(1):27–35. doi: 10.5863/1551-6776-21.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax. 2012;67(1):71–79. doi: 10.1136/thx.2009.129502. [DOI] [PubMed] [Google Scholar]
- 4.Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva GG, Anderson EJ, Courtney DM, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–27. doi: 10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Troeger C, Blacker B, Khalil IA, Rao PC, Cao J, Zimsen SRM, Albertson SB, Deshpande A, Farag T, Abebe Z, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1191–210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . The weekly epidemiological record. 2012. [accessed 19May 2020]. http://www.who.int/wer
- 7.Centers for Disease Control and Prevention . Global pneumococcal disease and vaccine. 2020. [accessed 19May 2020]. https://www.cdc.gov/pneumococcal/global.html
- 8.Matanock A, Lee G, Gierke R, Kobayashi M, Leidner A, Pilishvili T. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68(46):1069–75. doi: 10.15585/mmwr.mm6846a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stoecker C, Kobayashi M, Matanock A, Cho BH, Pilishvili T. Cost-effectiveness of continuing pneumococcal conjugate vaccination at age 65 in the context of indirect effects from the childhood immunization program. Vaccine. 2020;38(7):1770–77. doi: 10.1016/j.vaccine.2019.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Frank O, De Oliveira Bernardo C, González-Chica DA, Macartney K, Menzies R, Stocks N. Pneumococcal vaccination uptake among patients aged 65 years or over in Australian general practice. Hum Vaccin Immunother. 2020;16(4):965–71. doi: 10.1080/21645515.2019.1682844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawakami K, Nakamura A, Wakana A, Folaranmi TA, Iino T. A Japanese nationwide survey of 23-valent pneumococcal capsular polysaccharide vaccine (PPSV23) coverage among patients with chronic medical condition aged 50 and older. Hum Vaccin Immunother. 2019;4:1–8. doi: 10.1080/21645515.2019.1690332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richard C, Le Garlantezec P, Lamand V, Rasamijao V, Rapp C. Anti-pneumococcal vaccine coverage for hospitalized risk patients: assessment and suggestions for improvements. Ann Pharm Fr. 2016;74(3):244–51. doi: 10.1016/j.pharma.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Baig SA, Hassan M, Ahmed SM, Moazzam W, Inayat A. A cross-sectional study to investigate pneumococcal vaccination in the elderly in a low income county: patient knowledge, awareness, and attitudes of vaccination and prevalence rates by socioeconomic status. Hum Vaccin Immunother. 2014;10(4):1024–27. doi: 10.4161/hv.27697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klett-Tammen CJ, Krause G, Seefeld L, Ott JJ. Determinants of tetanus, pneumococcal and influenza vaccination in the elderly: a representative cross-sectional study on knowledge, attitude and practice (KAP). BMC Public Health. 2016;16:121. doi: 10.1186/s12889-016-2784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ang LW, Cutter J, James L, Goh KT. Epidemiological characteristics associated with uptake of pneumococcal vaccine among older adults living in the community in Singapore: results from the National Health Surveillance Survey 2013. Scand J Public Health. 2018;46(2):175–81. doi: 10.1177/1403494817720105. [DOI] [PubMed] [Google Scholar]
- 17.Wong-Beringer A, Brodetsky E, Quist R. Pneumococcal vaccination in hospitalized elderly patients: role of the pharmacist. Pharmacotherapy. 2003;23(2):199–208. doi: 10.1592/phco.23.2.199.32085. [DOI] [PubMed] [Google Scholar]
- 18.International Pharmaceutical Federation . An overview of current pharmacy impact on immunization, a global report. 2016. [accessed 19May 2020]. https://www.fip.org/files/fip/publications/FIP_report_on_Immunisation.pdf
- 19.Queeno BV. Evaluation of inpatient influenza and pneumococcal vaccination acceptance rates with pharmacist education. J Pharm Pract. 2017;30(2):202–08. doi: 10.1177/0897190016628963. [DOI] [PubMed] [Google Scholar]
- 20.Percy JN, Crain J, Rein L, Hohmeier KC. The impact of a pharmacist-extender training program to improve pneumococcal vaccination rates within a community chain pharmacy. J Am Pharm Assoc. 2003;60(1):39–46. doi: 10.1016/j.japh.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Metersky ML, Masterton RG, Lode H, File TM, Babinchak T. Epidemiology, microbiology, and treatment considerations for bacterial pneumonia complicating influenza. Int J Infect Dis. 2012;16(5):e321–31. doi: 10.1016/j.ijid.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Abu-Rish EY, Elayeh ER, Mousa LA, Butanji YK, Albsoul-Younes AM. Knowledge, awareness and practices towards seasonal influenza and its vaccine: implications for future vaccination campaigns in Jordan. Fam Pract. 2016;33(6):690–97. doi: 10.1093/fampra/cmw086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–81. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Becker-Dreps S, Kistler CE, Ward K, Killeya-Jones LA, Better OM, Weber DJ, Weber DJ, Zimmerman S, Nicholson BP, Woods CW, et al. Pneumococcal carriage and vaccine coverage in retirement community residents. J Am Geriatr Soc. 2015;63(10):2094–98. doi: 10.1111/jgs.13651. [DOI] [PubMed] [Google Scholar]
- 25.Abu-Rish EY, Elayeh ER, Albsoul-Younes AM. The role of the Middle East in ZIKA virus circulation: implications of a cross-sectional study in Jordan. Am J Trop Med Hyg. 2019;100(4):974–80. doi: 10.4269/ajtmh.18-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Lahham A, Khanfar N. Resistance of Streptococcus pneumoniae in Jordanian pediatric carriers, 2015-2016. Int J Infect Dis. 2016;53S:4–163. doi: 10.1016/j.ijid.2016.11.098. [DOI] [Google Scholar]
- 27.Isenor JE, Bowles SK. Opportunities for pharmacists to recommend and administer routine vaccines. Can Pharm J (Ott). 2019;152(6):401–05. doi: 10.1177/1715163519878473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guzman-Holst A, DeAntonio R, Prado-Cohrs D, Juliao P. Barriers to vaccination in Latin America: A systematic literature review. Vaccine. 2020;38(3):470–81. doi: 10.1016/j.vaccine.2019.10.088. [DOI] [PubMed] [Google Scholar]
- 29.Abu-Rish EY, Elayeh ER, Browning MJ. Travelers to U.S.: Zika virus knowledge, attitudes, and determinants of practices in the Middle East-insights for future awareness campaigns. Int J Environ Res Public Health. 2019;16(14):pii: E2517. doi: 10.3390/ijerph16142517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abu-Rish EY, Elayeh ER, Browning MJ. Physicians’ knowledge, attitudes and practices towards Zika virus infection in Jordan. J Infect Dev Ctries. 2019;13(7):584–90. doi: 10.3855/jidc.11356. [DOI] [PubMed] [Google Scholar]
- 31.Dubé E. Addressing vaccine hesitancy: the crucial role of healthcare providers. Clin Microbiol Infect. 2017;23(5):279–80. doi: 10.1016/j.cmi.2016.11.007. [DOI] [PubMed] [Google Scholar]


