Probiotics are live microorganisms that, when consumed in adequate amounts, confer a health benefit on the host.1 The probiotics industry is growing rapidly, with sales in the United States alone expected to exceed $6 billion in 2020.2 However, probiotics are a source of significant cost with unclear benefit. Patients routinely ask clinicians whether they should be taking probiotics and, if so, which products. These questions present a dilemma, given that none of the probiotic preparations being studied are currently manufactured as drugs, that is, with the intent of treating, mitigating, or preventing disease. Rather, the typical classification of probiotics as dietary supplements has been associated with diminishment of the rigor of clinical studies, including capturing adverse events and efficacy end points. To date, general practitioners and gastroenterologists have minimal guidance regarding the use of probiotics for gastrointestinal disorders.
In this technical review, the American Gastroenterological Association (AGA) Institute reviews probiotic formulations that have been studied to prevent or treat common disorders of the gastrointestinal tract. This review provides evidence-based information to guide both clinicians and patients regarding whether probiotics might play a role in the management of these disorders. When sufficient evidence exists, this review also suggests which individual probiotic strains or combinations of strains might be superior to others, or which clinical contexts warrant further research with probiotics. Other microbiome-targeting therapies, including antibiotics and fecal microbiota transplantation, are beyond the scope of this project, which focuses exclusively on probiotics. Similarly, prebiotics and synbiotics have been omitted from this review in order to focus on single-strain and multispecies formulations of probiotics. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was employed to assess the quality of evidence and to inform the AGA’s development of the accompanying clinical guidelines regarding the role of probiotics in the management of gastrointestinal conditions.
Objectives of the Review
This technical review addresses the following focused clinical questions with respect to probiotic use for gastrointestinal conditions:
In symptomatic adults with confirmed Clostridioides difficile infection, should probiotics be used as part of the treatment regimen?
In adults and children receiving antibiotic therapy for any indication except C difficile infection, should probiotics be used to prevent C difficile–associated diarrhea?
In adults and children with Crohn’s disease, should probiotics be used for induction or maintenance of remission?
In adults and children with ulcerative colitis, should probiotics be used for induction or maintenance of remission?
In adults and children with ileal pouch–anal anastomosis for chronic ulcerative colitis, should probiotics be used for prevention or maintenance of remission of pouchitis?
In symptomatic children and adults with irritable bowel syndrome, should probiotics be used to improve global response or abdominal pain severity?
In children with acute infectious gastroenteritis, should probiotics be used to reduce the duration or severity of diarrhea?
In preterm, low-birth-weight newborns, should probiotics be used to prevent necrotizing enterocolitis, sepsis, and all-cause mortality?
Methods
Overview of the Systematic Review Process
This technical review was developed to support the development of AGA guidelines regarding the potential role of probiotic use in conditions frequently managed by gastroenterologists. The Technical Review Panel was composed of both clinical and methodological experts. The development of this systematic review included the following steps:
development of the research questions and identification of outcomes critical to decision-making;
search of the literature for high-quality previously published systematic reviews and primary studies;
risk-of-bias assessment;
quantitative meta-analysis or narrative synthesis; and
assessment and presentation of the certainty of evidence.
Methods for deriving focused clinical questions, systematically reviewing and rating the quality of evidence for each outcome, and rating the overall quality of evidence were based on the GRADE framework, which has been described in detail previously.
Formulation of Clinical Questions and Determining Outcomes of Interest
The Panel formulated and prioritized the questions to be addressed by this guideline using the PICO (population, intervention, comparison, outcomes) format.3 The final set of questions and statements was approved by the AGA Governing Board. Members of the Technical Review and Guideline Committees selected patient-important outcomes for each question a priori. The Panels rated the relative importance of each outcome for decision-making on a scale of 1–10. Outcomes receiving a score of 7–10 were considered critical for decision-making, 4–6 were considered important for decision-making, and 1–3 were considered less important for decision-making. The final list of PICO questions and outcomes deemed critical for decision-making are presented above.
Literature Search Strategy and Study Selection
Initially, the literature search was conducted to identify potentially relevant systematic reviews published on the PICO questions of interest that fit predetermined eligibility criteria and were of high methodological rigor. A systematic review was eligible for inclusion if it evaluated 1 or more of the previously determined patient-important outcomes of interest, provided a quantitative estimate of effect, and was rated by the Technical Review Panel to have Moderate or High confidence based on AMSTAR (A Measurement Tool to Assess Systematic Reviews) 2 criteria.4 During a face-to-face meeting, the Technical Review and Guideline Panels collectively re-evaluated the previously identified evidence base along with the new evidence and independently determined the certainty of evidence as outlined below. For 2 of the PICO questions, complementary and mutually exclusive systematic reviews were identified; thus, we included systematic reviews for both induction and maintenance of remission for Crohn’s disease and for ulcerative colitis. If relevant systematic reviews were identified, then additional searches were conducted through December 2018 for studies published since the systematic reviews. For questions not guided by a previously published systematic review, the literature search was conducted de novo.
A search of the medical literature was conducted by an information specialist using the following databases: MEDLINE (1950 to June 2018), EMBASE and EMBASE Classic (1947 to June 2018), and the Cochrane Central Register of Controlled Trials. This search was updated to include additional studies that were published from June to December 2018. The search strategy comprised controlled vocabulary, including the National Library of Medicine’s Medical Subject Headings and keywords. Search concepts common to all searches were “probiotics,” “probiotic agent,” “synbiotics,” “synbiotic agent,” “beneficial microbes,” and “beneficial bacteria.” We excluded trials exclusively conducted within populations harboring major comorbidities, including cancer, human immunodeficiency virus/acquired immune deficiency syndrome, cystic fibrosis, spinal cord injury, organ failure or transplantation, and other severe conditions. Methodological filters were applied to limit retrieval of trials that included only animals and not humans. Corresponding authors of studies were contacted to provide additional information on trials when required. Two attempts were made to contact the author. If there was no response after 2 attempts, the study was excluded based on incomplete information.
We included studies of children (younger than 18 years) and/or adults (18 years and older), depending on relevance to the clinical question and the amount of published evidence. Specifically, we excluded trials focusing on treatment of C difficile infection (CDI) exclusively in children or treatment of acute gastroenteritis exclusively in adults, whereas prevention of necrotizing enterocolitis (NEC) is relevant to neonates only. The interventions were orally ingested or rectally administered (for ulcerative colitis only) live microbes, either single-strain or multispecies, with defined species or strain and dose. The comparators were placebo or standard of care. Trials of synbiotics were included only when the non-microbial portion of the synbiotic was tested separately in a control arm, so that the specific effect of the probiotic could be evaluated. Comparative effectiveness studies were included only when an appropriate control arm existed. Given significant overlap between 2 groups of 3 PICO questions, for these groups we combined searches before sorting references according to the relevant PICO question. One combined search included treatment of CDI, prevention of C difficile–associated diarrhea (CDAD), and treatment of acute gastroenteritis. The other combined search included induction and maintenance of remission in Crohn’s disease, induction and maintenance of remission in ulcerative colitis, and treatment and prevention of pouchitis. Literature searches for the remaining PICO questions were performed individually.
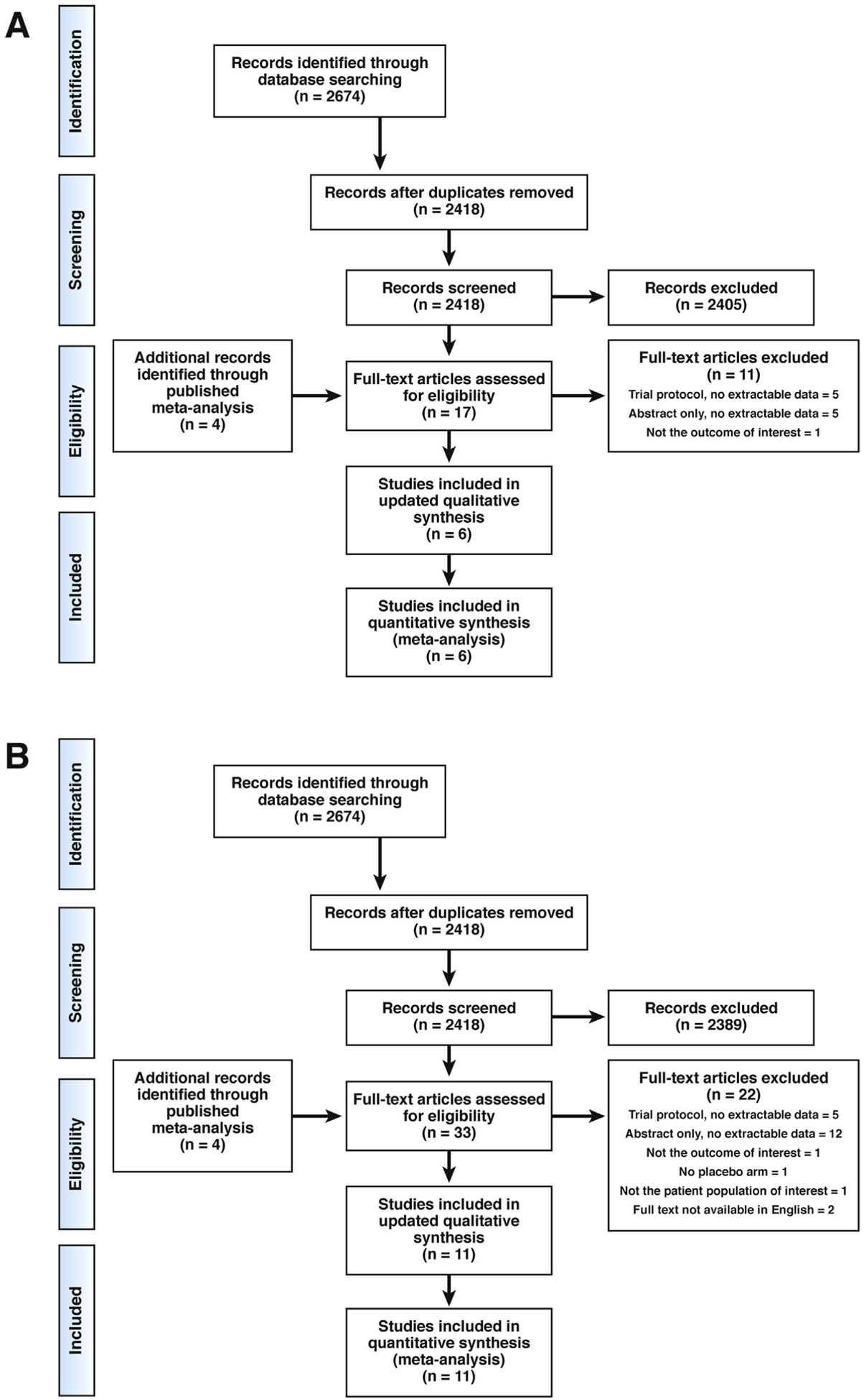
Studies were restricted to those written in the English language. Letters, notes, case reports, and comments were excluded. Abstracts of the citations identified by the initial search were evaluated independently and in duplicate by 2 or 3 authors (G.P., A.W., and P.K.) for eligibility. Full-text versions of all potentially relevant studies were obtained and evaluated in detail. Authors searched reference lists of eligible studies for additional references. The results of the literature search selection process are presented in Figures 1–7.
Figure 1.
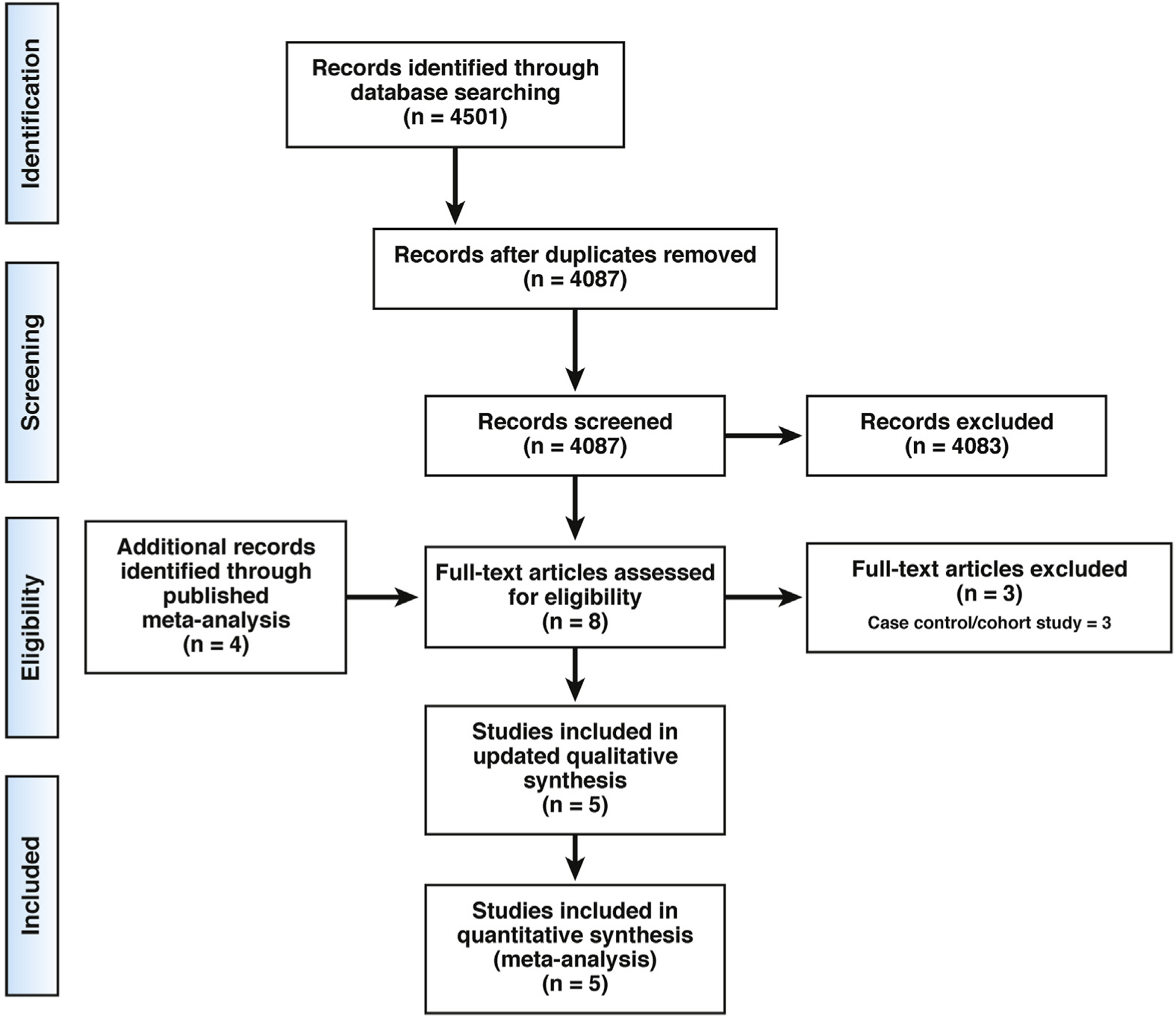
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 Probiotics to treat CDI.
Figure 7.
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 Probiotics to treat acute gastroenteritis.
Data Extraction and Risk-of-Bias Assessment
Data were extracted by 2 or 3 Panel members (G.P., A.W., and P.K.) to a Microsoft Excel spreadsheet (Microsoft, Redmond, WA). The following clinical data were extracted for each trial, if available: author last name, publication year, country of origin, funding source, protocol registration, study duration, strain and dose of probiotic, pediatric or adult subjects, and outcome measures, including adverse events. Authors assessed risk of bias of eligible studies independently and in duplicate using the Cochrane risk-of-bias tool for randomized controlled trials.5 Authors discussed risk-of-bias judgments to reach consensus; however, if consensus could not be reached, a third author provided consultation until a decision was made.
Analytic Approach
When possible, a pooled effect estimate was calculated for each comparison. If studies did not report means and SDs but reported medians and interquartile ranges, they were converted and added to the quantitative synthesis using methods from the Cochrane Handbook.5,6 Quantitative analyses were expressed as a relative risk (RR) or odds ratio (OR) for categorical variables and mean difference (MD) for continuous variables. The DerSimonian and Laird method for random-effect or fixed-effects models (when pooling <3 clinical trials) was applied to determine the overall effect size with 95% confidence intervals (CIs). When quantitative pooling was not possible, a narrative summary of the results was developed. Heterogeneity between studies was assessed using a χ2 test of homogeneity with a .10 significance level and I2 statistic. Subgroup analyses were performed to examine the effect for individual probiotic species/strains. When more than 10 studies were available in an analysis, publication bias was evaluated using funnel plot asymmetry. Review Manager (RevMan), version 5.3 (Rev-Man for Windows 2008; Nordic Cochrane Center, Copenhagen, Denmark) was used to conduct all statistical analyses and generate forest plots, risk-of-bias tables, and funnel plots.
Certainty of Evidence
The GRADE approach was used to assess the certainty (ie, quality) of evidence (CoE).7 Across each outcome, evidence from randomized controlled trials starts at high quality and can be downgraded due to concerns about risk of bias, inconsistency (or heterogeneity), indirectness, imprecision, and/or publication bias.8 Due to inherent limitations in observational studies (lack of a prognostic balance), evidence from observational studies starts at low quality and is potentially downgraded based on the aforementioned factors, or can be upgraded on the basis of a large magnitude of effect, a dose–response gradient, or opposing residual confounding. The quality of the evidence was first evaluated across the body of evidence for each outcome and then across outcomes for each PICO question. The quality of the evidence can be rated as “High,” “Moderate,” “Low,” or “Very Low.” Additionally, for each PICO question, an evidence profile, using the GRADEpro Guideline Development Tool (www.gradepro.org) was prepared. Recently published GRADE guidance on specific wording for narrative statements to reflect the CoE9 guided the description of the certainty in the Results section.
Question 1: In Symptomatic Adults With Confirmed C difficile Infection, Should Probiotics Be Used as Part of the Treatment Regimen?
Results
CDI is typically treated with oral antibiotics, such as vancomycin and fidaxomicin, but during the past decade there has been a significant rise in recurrent CDI,10 highlighting the need for novel adjunct therapies. The use of fecal microbiota transplantation to successfully treat multiple recurrent CDI provides proof-of-principle evidence that altering the gut microbiota can restore health in this context,11 although the body of evidence regarding probiotics has been less convincing. A Cochrane review published in 200812 included 4 studies that examined the use of probiotics in conjunction with conventional antibiotics for the treatment of an initial episode or of recurrence of CDI in adults.13–16 To update the evidence base, the Technical Review Panel reviewed 4501 titles and abstracts, assessed 4 new full-text articles for eligibility, and identified 1 additional study17 for inclusion (Figure 1).
In total, 5 randomized placebo-controlled trials evaluating probiotics in conjunction with conventional antibiotics, examining a total of 223 adults (probiotics, n = 110; placebo, n = 113), were included in this review. Four different probiotic formulations were tested, with only Saccharomyces boulardii being tested in more than 1 study.14,15 Enrollment criteria differed between the studies. One trial17 enrolled only patients with an initial case of CDI, 3 trials13,15,16 enrolled only patients with recurrent disease, and 1 trial14 enrolled patients with either initial or recurrent CDI. The antibiotics administered were metronidazole (n = 1), vancomycin (n = 1), or either of these 2 antibiotics (n = 3). All 5 published studies contained uncertain or high risk of bias regarding blinding of outcome assessment and selective reporting. Similar to the Cochrane review,12 data were not pooled for a combined analysis due to variations in recruitment criteria, outcome measures (eg, only 1 study16 reported bacteriological cure), clinical heterogeneity related to initial disease state and antibiotic therapy, high dropout rates, and type of probiotic used. The evidence is summarized in Appendix 1.
The largest study,14 which analyzed 124 subjects receiving metronidazole or vancomycin for initial or recurrent CDI, reported that S boulardii (1 g, 3 × 1010 cfu/d or placebo) may increase the cessation of diarrhea (RR, 1.33; 95% CI, 1.02–1.74, Low CoE), and may decrease the recurrence of diarrhea (RR, 0.59; 95% CI, 0.35–0.98, Low CoE). The second study15 that examined S boulardii (1 g/d, cfu not reported or placebo) among 32 adults with recurrent CDI receiving either metronidazole or high-dose (2 g/d) or low-dose (500 mg/d) vancomycin also reported decreased recurrence of diarrhea in the probiotic arm compared to placebo, but only among those receiving high-dose vancomycin, which was non-randomly assigned to the sickest patients, and the CI of this effect did cross 1.0. One study17 of 31 adults with initial CDI who were treated with either metronidazole or vancomycin and who received the 4-strain combination of Lactobacillus acidophilus ATCC 700396, Lactobacillus paracasei subsp paracasei ATCC 335, Bifidobacterium animalis subsp lactis ATCC SD5220, and B animalis subsp lactis ATCC SD5219 at a dose of 1.70 × 1010 cfu/d, reported that probiotics compared to placebo may reduce the duration of diarrhea, but the evidence is very uncertain (Very Low CoE). The other 2 studies each tested different strains of probiotic in even smaller trials. The first of these trials16 reported that Lactobacillus plantarum 299v at a dose of 5 × 1010 cfu/d may not increase events of cessation of diarrhea vs placebo, but the evidence is very uncertain (RR, 0.93; 95% CI, 0.73–1.19, Very Low CoE). The other trial13 reported that Lactobacillus rhamnosus ATCC 53103 may increase CDAD recurrence vs placebo, but the evidence is very uncertain (RR, 2.63; 95% CI, 0.35–19.85, Very Low CoE). The effect of specific probiotics was difficult to assess, given the small number of studies evaluated for each probiotic formulation. The most common adverse events reported were mild gastrointestinal symptoms, with 1 study14 reporting increased constipation among patients treated with S boulardii vs placebo. No serious adverse events were reported.
The overall CoE across all critical outcomes for probiotics as part of the treatment of C difficile infection was Low.
Discussion
The most recent Cochrane review12 was published more than a decade ago, and an updated literature search identified just 1 additional trial17 that evaluated an additional 31 participants. Therefore, the conclusions drawn by the previous meta-analysis were not markedly changed. The spectrum of enrolled subjects was not large enough to identify specific or potentially serious harms, and few total events were reported. Furthermore, the data contained substantial indirectness due to differences in enrollment criteria, with both initial and recurrent disease being studied, and due to differences in study design, with comparators ranging from placebo to low-dose or high-dose antibiotics. There also was a potential risk of publication bias due to multiple registered trials that were not linked to a published report. Finally, none of these studies enrolled children, so it is unclear whether these findings are generalizable to the pediatric population. A considerably larger body of evidence exists regarding a potential role for probiotics in the prevention of CDI among those taking antibiotics for other conditions; this evidence is reviewed in the next section.
Question 2: In Adults and Children Receiving Antibiotic Therapy for any Indication Except C difficile Infection, Should Probiotics Be Used to Prevent C difficile–Associated Diarrhea?
Results
Compared to the sparse body of data relevant to the treatment of CDI, the role of probiotics for the prevention of CDAD has been investigated more thoroughly. This review includes 39 studies18–53 (M. Miller, unpublished data, 2008a, 2008b; S. Rafiq, unpublished data, 2007), all of which were identified in a Cochrane review published in 2017.54 These studies evaluated a total of 9955 participants, although the baseline populations were remarkably heterogeneous: children, adults, and the elderly; inpatients and outpatients; high and low baseline risks of developing CDAD; and various antibiotic regimens prescribed for a wide range of clinical indications. Among the key findings from the published meta-analysis,54 a complete case analysis of the 31 trials that reported incidence of CDAD (probiotics, n = 4525; placebo, n = 4147) revealed that reduce the risk of CDAD vs placebo (RR, 0.40; 95% CI, 0.30–0.52, Moderate CoE). Subgroup analysis revealed stratification of the effect size by baseline risk of CDAD. The Cochrane review defined baseline risk as the event rate in the control arm, and divided this risk post hoc into 3 groups (0%–2%, 3%–5%, and >5%), corresponding with low-, moderate-, and high-risk clinical scenarios.54 Specifically, trials that enrolled patients with a >5% baseline risk of developing CDAD demonstrated a large risk reduction (RR, 0.30; 95% CI, 0.21–0.42, Moderate CoE), whereas a similar benefit was not identified among trials enrolling patients with a lower baseline risk of 3%–5% (RR, 0.53; 95% CI, 0.16–1.77, Moderate CoE) or a baseline risk of 0%–3% (RR, 0.77; 95% CI, 0.45–1.32, Moderate CoE). Among the 15 trials that reported on the detection of C difficile in the stool, probiotics did not reduce fecal detection rates (RR, 0.86; 95% CI, 0.67–1.10, Moderate CoE). Finally, among the 32 studies that reported adverse events, probiotics might reduce the risk of adverse events vs placebo (RR, 0.83; 95% CI, 0.71–0.97, Very Low CoE).54
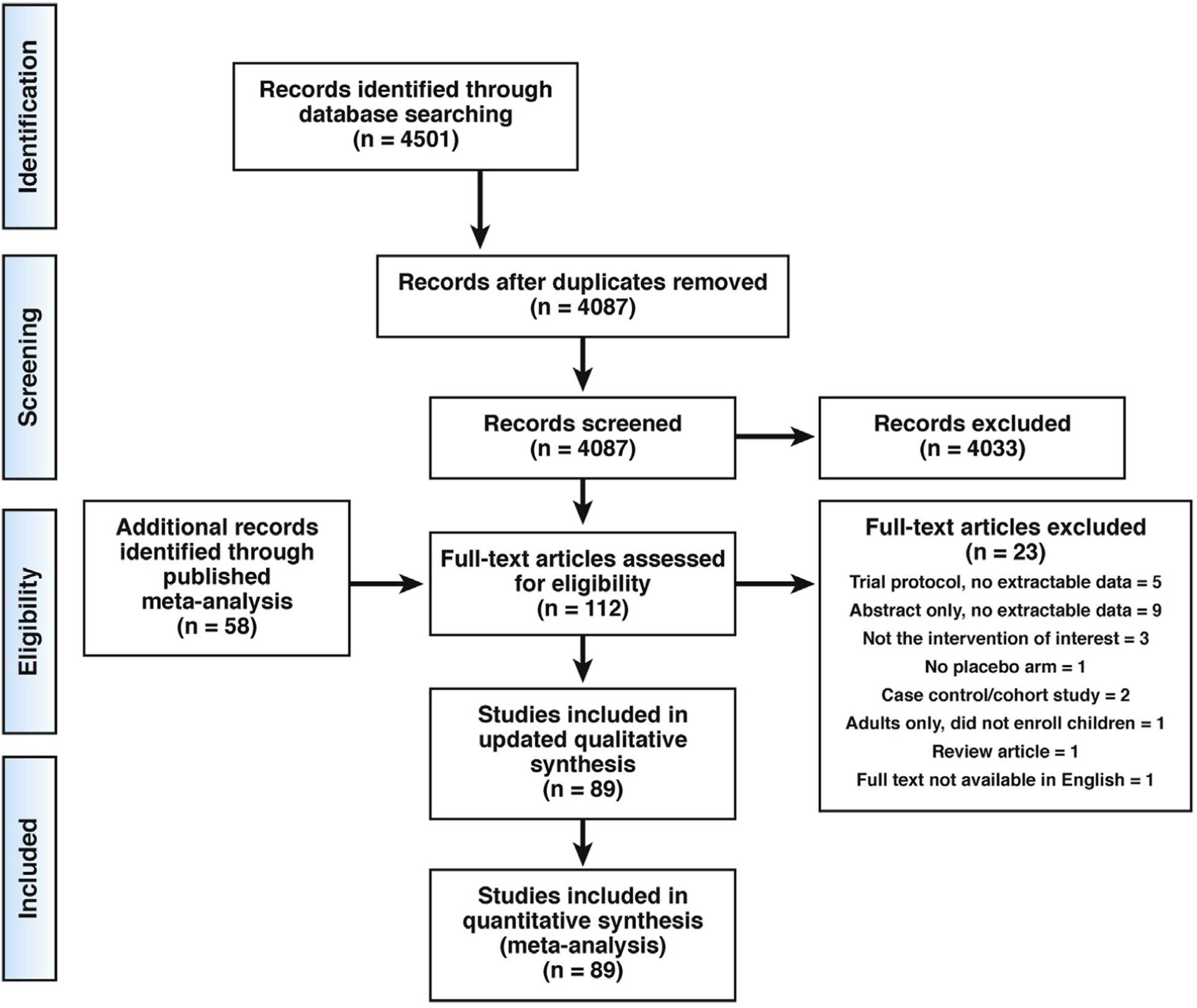
The Technical Review Panel performed an updated search, reviewed 4501 titles and abstracts, assessed 24 new full-text articles for eligibility, and did not identify any more recent studies for inclusion (Figure 2). However, the team considered several factors in its decision to downgrade the overall CoE from Moderate to Low. Of the 39 studies included in the published meta-analysis,54 226,39 were published in abstract form only and 3 were unpublished data (M. Miller, unpublished data, 2008a, 2008b; S. Rafiq, unpublished data, 2007). Only 2 of the 39 studies were determined to have low risk of bias across all domains for all outcomes assessed. The Technical Review Panel also highlighted the potential risk of publication bias, given the large volume of registered trial protocols that were not associated with subsequent peer-reviewed publications. Furthermore, the overall effect estimate was heavily weighted by 5 trials enrolling patients with a >15% baseline risk of developing CDAD. Finally, the analysis of studies that reported incidence of CDI contained a wide CI that includes the potential for some benefit as well as some harm.
Figure 2.
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 Probiotics to prevent CDAD.
Subgroup analyses of individual probiotic formulations revealed that S boulardii (RR, 0.41; 95% CI, 0.22–0.79, Low CoE); the 2-strain combination of L acidophilus CL1285 and Lactobacillus casei LBC80R (RR, 0.22; 95% CI, 0.11–0.42, Low CoE); the 3-strain combination of L acidophilus, Lactobacillus delbrueckii subsp bulgaricus, and Bifidobacterium bifidum (RR, 0.35; 95% CI, 0.15–0.85, Low CoE); and the 4-strain combination of L acidophilus, L delbrueckii subsp bulgaricus, B bifidum, and Streptococcus salivarius subsp thermophilus (RR, 0.28; 95% CI, 0.11–0.67, Low CoE) might all reduce the risk of CDAD vs placebo. The complete body of evidence is presented in Appendix 2.
The overall CoE across all critical outcomes for probiotics, based on the best available evidence from S boulardii; or the 2-strain combination of L acidophilus CL1285 and L casei LBC80R; or the 3-strain combination of L acidophilus, L delbrueckii subsp bulgaricus, and B bifidum; or the 4-strain combination of L acidophilus, L delbrueckii subsp bulgaricus, B bifidum, and S salivarius subsp thermophilus, for the prevention of CDAD in adults and children was Low.
Discussion
The overall evidence is promising for probiotics in general, and for certain strains and combinations of strains in particular, as a means of preventing CDAD after antibiotic use. Most of the included trials do not describe whether the probiotic formulations were rationally selected based on evidence of probiotic survival despite exposure to the prescribed antibiotics. The yeast S boulardii was the only single-strain probiotic to demonstrate a significant effect in reducing the incidence of CDAD. Antibiotics do not kill yeast typically, but they can increase the growth of some resident yeast by decreasing bacterial colonization; however, the exact mechanism by which S boulardii exerts a protective effect remains unclear. The rationale for using probiotics along with antibiotics is to accelerate recovery of a disrupted gut microbiota and prevent opportunistic pathogens from being able to exploit the open niches resulting from antibiotic use. However, recent studies have shown that probiotics may alter the recovery path of gut microbiota after antibiotic use when compared to no intervention.55 The clinical implications of such altered recovery remain to be determined. Furthermore, diet also may alter recovery after antibiotic use,56 but clinical trials with probiotics typically do not account for dietary differences among participants.
A recently published network meta-analysis evaluated probiotics for the prevention of antibiotic-associated diarrhea.57 The analysis included 51 trials enrolling 9565 participants receiving 10 different probiotic interventions and concluded that L rhamnosus ATCC 53103 had the highest probability of being the top-ranked intervention in terms of both effectiveness and tolerability. This result highlights how subtle differences in outcome measures—specifically, CDAD vs antibiotic-associated diarrhea—can affect how various treatments perform in meta-analyses.
Despite the relatively large number of published trials relevant to this PICO question, we did not identify any new trials published in the 20 months spanning from the conclusion of the search reported in the Cochrane review54 to the conclusion of our updated literature search in December 2018. Our assessment of the previously identified trials raised significant concerns regarding risk of bias, significant population heterogeneity, and unknown potential for adverse events. Thus, the Technical Review Panel concluded that the overall CoE for this PICO question is Low.
Question 3: In Adults and Children With Crohn’s Disease, Should Probiotics Be Used for Induction or Maintenance of Remission?
Results
Inflammatory bowel diseases (IBDs) encompass a heterogeneous group of immune-mediated diseases that are distinct in pathogenesis, manifestations, risk factors, and response to therapy. The etiology of IBDs is multifactorial, with contributions from genetic alterations, immune disturbances, environmental factors, and gut microbiota. Current treatment strategies rely primarily on targeting the immune system with pharmacologic agents, although there is increasing focus on microbiota-directed therapies. Disruptions of the gut microbiome have been well described at the compositional and functional levels in IBD, but whether they serve as the initial inciting event, function to perpetuate the underlying inflammation, or simply result from the altered gastrointestinal niche in IBD remains unclear. While there are multiple microbiome-targeting strategies, including diet, fecal microbiota transplantation, and prebiotics, this technical review focuses on the current evidence for use of probiotics in IBD.
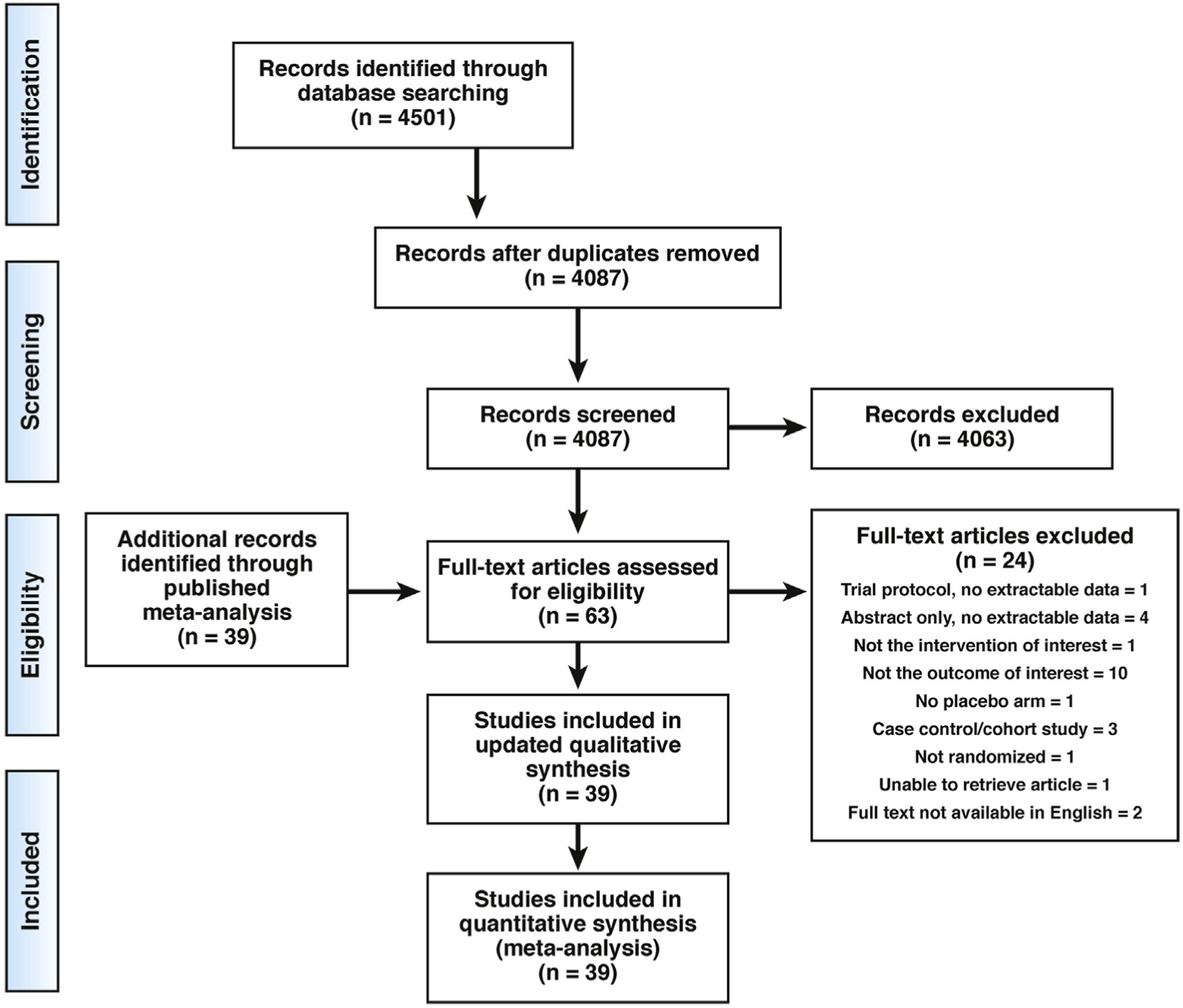
Microbiota alterations are particularly well described for Crohn’s disease,58–60 a relapsing and remitting form of IBD characterized by segmental, asymmetrical, and transmural lesions throughout the gastrointestinal tract; by frequent surgical complications, including strictures, fistulas, and abscesses; and by extraintestinal manifestations.61 A 2008 Cochrane Review62 examining probiotics for the induction of remission in children and adults with Crohn’s disease identified just 1 study63 that evaluated a total of 11 patients. This study did not show certain benefit with administration of L rhamnosus ATCC 53103 (OR, 0.80; 95% CI, 0.04–17.20, Very Low CoE). The review authors cited concerns regarding the study design, including lack of a power calculation and allowing concurrent use of corticosteroids. Furthermore, the study lacked detail regarding how and when induction was assessed, and the risk of bias with respect to allocation concealment was unclear. To bring the evidence base up to date, the Technical Review Panel assessed 2674 titles and abstracts and assessed 9 new full-text articles for eligibility, but did not find any more recent studies that met inclusion criteria (Figure 3A). Thus, this review contains a single small study (probiotics, n = 5; placebo, n = 6) relevant to induction of remission in Crohn’s disease.63
Figure 3.
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 (A) Probiotics to induce remission in CD. (B) Probiotics to maintain remission in CD.
In contrast, 11 trials are included in this technical review regarding the role of probiotics for maintenance of remission in children and adults with Crohn’s disease. Of these, 7 studies evaluating 248 adults and children63–69 were identified in a 2006 Cochrane review.70 The Technical Review Panel’s assessment of 2674 titles and abstracts and review of 12 new full-text articles identified an additional 4 studies71–74 for inclusion, which analyzed an additional 430 adults, for a total of 678 subjects (probiotics, n = 343; placebo, n = 335; Figure 3B). Two studies71,72 assessed the effectiveness of Lactobacillus johnsonii NCC 533 in preventing severe endoscopic relapse after surgical induction at either 12 weeks or 6 months in a total of 145 patients (probiotics, n = 71; placebo, n = 74). There was no difference between the probiotic and placebo (RR, 0.97; 95% CI, 0.52–1.83, Low CoE), and there was unclear risk of bias for random sequence generation and selective reporting in both studies. Another study74 administered the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, Bifidobacterium longum subsp longum, Bifidobacterium breve, B longum subsp infantis, and S salivarius subsp thermophilus after surgical induction in a total of 94 patients (probiotic, n = 43; placebo, n = 51) and found no difference in relapse at 3 months. There was unclear risk of bias for outcome assessment. A previously identified study presented in abstract form65 assessed 40 patients (probiotics, n = 20; mesalamine, n = 20) who received the same 8-strain combination or mesalamine after surgical induction. Similar to the larger published study, there was not a difference in endoscopic relapse at 12 months. However, the probiotic group received rifaximin for 3 months, followed by 9 months of probiotics, raising the possibility that results were confounded by the use of antibiotics. Furthermore, there was an unclear risk of bias for random sequence generation and allocation concealment and only the physicians participating in the study were blinded. A combined analysis of these 2 studies did not reveal a clear benefit for the 8-strain probiotic combination (RR, 0.54; 95% CI, 0.25–1.16, Very Low CoE). Finally, 2 studies66,73 examined the effectiveness of S boulardii in a total of 191 patients (probiotic, n = 96; placebo/mesalamine, n = 95). There was no clear benefit with S boulardii in preventing relapse of CD (RR, 0.51; 95% CI, 0.10–2.54, Very Low CoE) compared to placebo or mesalamine. There was unclear risk of bias with respect to random sequence generation and incomplete reporting in both studies. One study66 also had unclear risk of bias for allocation concealment and blinding, with the additional potential confounder that both groups received mesalamine but the probiotic group received a lower dose (2 g) compared to the control group (3 g). The evidence is summarized in Appendix 3.
The overall CoE across all critical outcomes for probiotics for the induction or maintenance of remission in children or adults with Crohn’s disease was Low.
Discussion
There is currently no evidence to suggest that probiotics are beneficial for the induction or maintenance of remission in children or adults with Crohn’s disease. None of the individual studies included in this technical review reported a significant benefit from probiotic therapy, and meta-analyses combining 2 studies each analyzing L johnsonii LA1, an 8-strain probiotic combination, or S boulardii revealed no clear benefit. However, the studies were heterogeneous with regard to patient population, probiotic tested, duration of treatment, concomitant therapy, and the control product. For maintenance of remission studies, the populations differed based on whether remission was induced by medical or surgical means. Most of the included studies enrolled small numbers of patients and might have lacked the statistical power to reveal clinically significant differences, should they exist. Only 1 study64 enrolled children. For induction of remission in Crohn’s disease, our finding of just 1 published study63 examining 11 subjects highlights the lack of well-designed prospective trials in this area. These findings are consistent with a recently published systematic review and meta-analysis that examined the use of probiotics for adults with IBD.75 Larger studies will be required to determine whether probiotics may be of benefit in Crohn’s disease.
Question 4: In Adults and Children With Ulcerative Colitis, Should Probiotics Be Used for Induction or Maintenance of Remission?
Results
Ulcerative colitis is a chronic form of IBD characterized by mucosal inflammation that typically extends from the rectum proximally; as in Crohn’s disease, extraintestinal manifestations are common.76 Also similar to Crohn’s disease, characteristic microbiome changes have been described for ulcerative colitis,59,60,77 lending promise to the notion that microbiome-targeting therapies, including probiotics and, more recently, fecal microbiota transplantation,78 might offer hope for patients.
This technical review includes 11 studies that examined the use of probiotics for induction of remission in children and adults with ulcerative colitis. A 2007 Cochrane review79 identified 4 studies examining 236 adult subjects (probiotics, n = 106; placebo, n = 130),80–83 although 1 of these studies80 tested a synbiotic—the combination of probiotic B longum subsp longum with prebiotics fructo-oligosaccharide and inulin—vs placebo. The Technical Review Panel assessed 2674 titles and abstracts. Of 29 new potentially eligible studies that were reviewed in full text, 7 placebo-controlled trials84–90 that examined probiotics in conjunction with conventional management for induction of remission of ulcerative colitis were identified and added to the evidence base (Figure 4A). These 7 more recently published trials enrolled a total of 532 patients, bringing the total evidence base to 768 subjects (probiotics, n = 399; placebo, n = 369). Two studies84,88 enrolled children exclusively, among them 184 that only included children newly diagnosed with ulcerative colitis. In all, 5 different probiotics were tested: the 2-strain combination of B breve with B bifidum81; B longum Reuter ATCC BAA-99990; Escherichia coli Nissle 191782,86,89; the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus83–85,87; and Lactobacillus reuteri ATCC 55730.88 The 8-strain combination was examined in 1 pediatric study84 and 3 adult studies,83,85,87 and E coli Nissle 1917 was tested in 3 studies—2 as an oral therapeutic82,89 and 1 as an enema.88 The other probiotics were tested in 1 study each: L reuteri ATCC 55730 as an enema88 and both B longum Reuter ATCC BAA-99990 and the 2-strain combination of B breve with B bifidum81 administered orally. Two studies86,88 administered probiotics as an enema. The duration of treatment was 7–12 weeks except in 1 study,84 in which the 8-strain probiotic combination was administered for 1 year. The standard treatments varied among studies, with 1 study89 utilizing antibiotics for treatment of ulcerative colitis.
Figure 4.
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 (A) Probiotics for Induction of Remission in ulcerative colitis. (B) Probiotics to maintain remission in ulcerative colitis.
Combined analyses of the individual probiotic formulations revealed the following. First, the effectiveness of the 8-strain probiotic combination was evaluated in 4 trials evaluating 367 patients (probiotics, n = 186; mesalamine or balsalazide, n = 181), including 1 study84 that enrolled children. The duration of treatment varied among the studies and there was significant heterogeneity in study design. There was a potential for benefit, but it is very uncertain (RR, 1.72; 95% CI, 0.89–3.32, Very Low CoE), with significant heterogeneity in study design. For example, 1 trial87 used the anti-inflammatory drug balsalazide as the control. There were multiple concerns regarding bias, including unclear risk with respect to blinding in multiple studies, 1 study with higher than expected attrition, and another study with unclear risk of bias with respect to allocation concealment. Second, the effectiveness of orally administered E coli Nissle 1917 compared to mesalamine to induce remission in ulcerative colitis was analyzed in 2 studies82,89 evaluating 166 patients (probiotic, n = 82; mesalamine, n = 84). E coli Nissle 1917 suggested uncertain benefit (RR, 0.86; 95% CI, 0.49–1.49, Very Low CoE). One of the studies82 had a high risk of bias for randomization, unclear risk of bias for allocation concealment and blinding, a withdrawal rate of 8.9%, and patients received both steroids and gentamicin 80 mg 3 times per day for 1 week in addition to probiotic or placebo. In the more recent study,89 some of the patients received topical prednisolone as concomitant therapy at the time of enrollment. One other study86 administered E coli Nissle 1917 as an enema to a total of 88 patients (probiotic 10 mL, n = 23; 20 mL, n = 23; 40 mL, n = 22; placebo, n = 20) with mild-to-moderate distal ulcerative colitis. There was no clear benefit for any probiotic dose compared to placebo in intention-to-treat analysis. Finally, L reuteri ATCC 55730, in enema form, was studied among 31 children (probiotic, n = 16; placebo, n = 15) with active distal ulcerative colitis. Probiotic enemas may increase clinical response vs placebo (RR, 1.83; 95% CI, 1.14–2.92, Low CoE). The results from the other newly identified studies did not show a benefit in induction of remission; each study tested a unique probiotic formulation. The evidence profiles are presented individually in Appendix 4.
The Technical Review Panel next compiled evidence regarding the use of probiotics for maintenance of remission in adults and children with ulcerative colitis. A 2011 Cochrane review91 had identified 4 studies92–95 enrolling a total of 664 adult patients (probiotics, n = 367; placebo or mesalamine, n = 297). We reviewed 2674 titles and abstracts, assessed 13 new full-text articles for eligibility, and included 296,97 additional placebo-controlled trials examining probiotics for maintenance of remission (Figure 4B). These 2 studies analyzed an additional 241 adults, bringing the total to 905 subjects (probiotics, n = 488; placebo, n = 417). The new studies use different multispecies probiotic formulations administered for 48 weeks to 1 year, and there was unclear risk of bias with respect to outcome assessment. The 2-strain combination of B breve Yakult and L acidophilus97 did not show appreciable benefit (RR, 1.15; 95% CI, 0.66–1.98, Low CoE). Similarly, the 3-strain combination of Enterococcus faecalis T-111, Clostridium butyricum TO-A, and Bacillus mesentericus TO-A96 did not show clear benefit (RR, 1.33; 95% CI, 0.83–2.15, Low CoE), with a large CI, few events, and unclear risk of bias with respect to allocation concealment and blinding. The previous meta-analysis91 included 2 studies in which E coli Nissle 1917 was administered to a total of 430 patients (probiotics, n = 212; mesalamine, n = 218) and relapse was assessed at 12 weeks92 (RR, 1.79; 95% CI, 0.82–3.92) or 12 months93 (RR, 1.40; 95% CI, 0.90–2.18), showing no clear benefit compared to mesalamine. Both of these studies had unclear risk of bias with respect to allocation concealment and 1 of the studies93 reported significant attrition, with a dropout rate of 46.5%. The data from remaining studies were not pooled, given that no prior studies utilized the same probiotic formulation; therefore, the results from the individual trials are presented in the evidence profiles summarized in Appendix 4.
The overall CoE across all critical outcomes for probiotics for induction or maintenance of remission in children or adults with ulcerative colitis was Low.
Discussion
The literature search updates conducted for this technical review more than doubled the number of published prospective trials that were included in the most recent Cochrane reviews that evaluated probiotics for the induction78 and maintenance91 of remission in adults and children with ulcerative colitis. Despite the addition of these more recent studies to the evidence base, a knowledge gap remains regarding the role of probiotics in these contexts. The quality of existing evidence is limited in many cases by study designs characterized by small sample sizes and concerns regarding risk of bias. Furthermore, the use of mesalamine as a comparator drug might blunt any beneficial effect of probiotics. As with the other focused questions, there also remains the possibility of publication bias, given that published articles are typically skewed toward positive study findings.
Conventional therapy combined with a probiotic does not appear to improve overall remission rates in patients with mild-to-moderate ulcerative colitis, although there is limited evidence that probiotics may provide modest benefits in terms of reduction of disease activity in mild-to-moderate ulcerative colitis. The efficacy of probiotics for patients with severe disease, as well as the efficacy of probiotics as alternatives to existing therapies, remains unknown. As reported in a recent meta-analysis,75 among the promising individual formulations was the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus, which was reported in 2 prospective trials to be beneficial. However, this combination also was the most tested of all probiotic formulations for patients with ulcerative colitis, and combined case analyses of 4 studies did not reveal a clear benefit. Interestingly, the 2 trials that enrolled children exclusively reported a significant effect attributed to probiotics for induction of remission, suggesting that the pediatric population might potentially benefit more than adults with ulcerative colitis. Additional studies are needed to expand upon this observation.
Question 5: In Adults and Children With Ileal Pouch–Anal Anastomosis for Chronic Ulcerative Colitis, Should Probiotics Be Used for Prevention or Maintenance of Remission of Pouchitis?
Results
Refractory or complicated ulcerative colitis is often managed surgically by total abdominal proctocolectomy to remove the diseased bowel, with IPAA to facilitate passage of bowel movements without a stoma. Acute, relapsing, or chronic pouchitis is the most common post-surgical complication, occurring in more than one-half of patients.98 Although the etiology of pouchitis is poorly understood, gut microbiota have been suggested to play a role, based on altered fecal microbial communities that associate with disease activity,99 the use of antibiotics as the mainstay of pouchitis therapy,100 and the possible therapeutic role of fecal microbiota transplantation.101
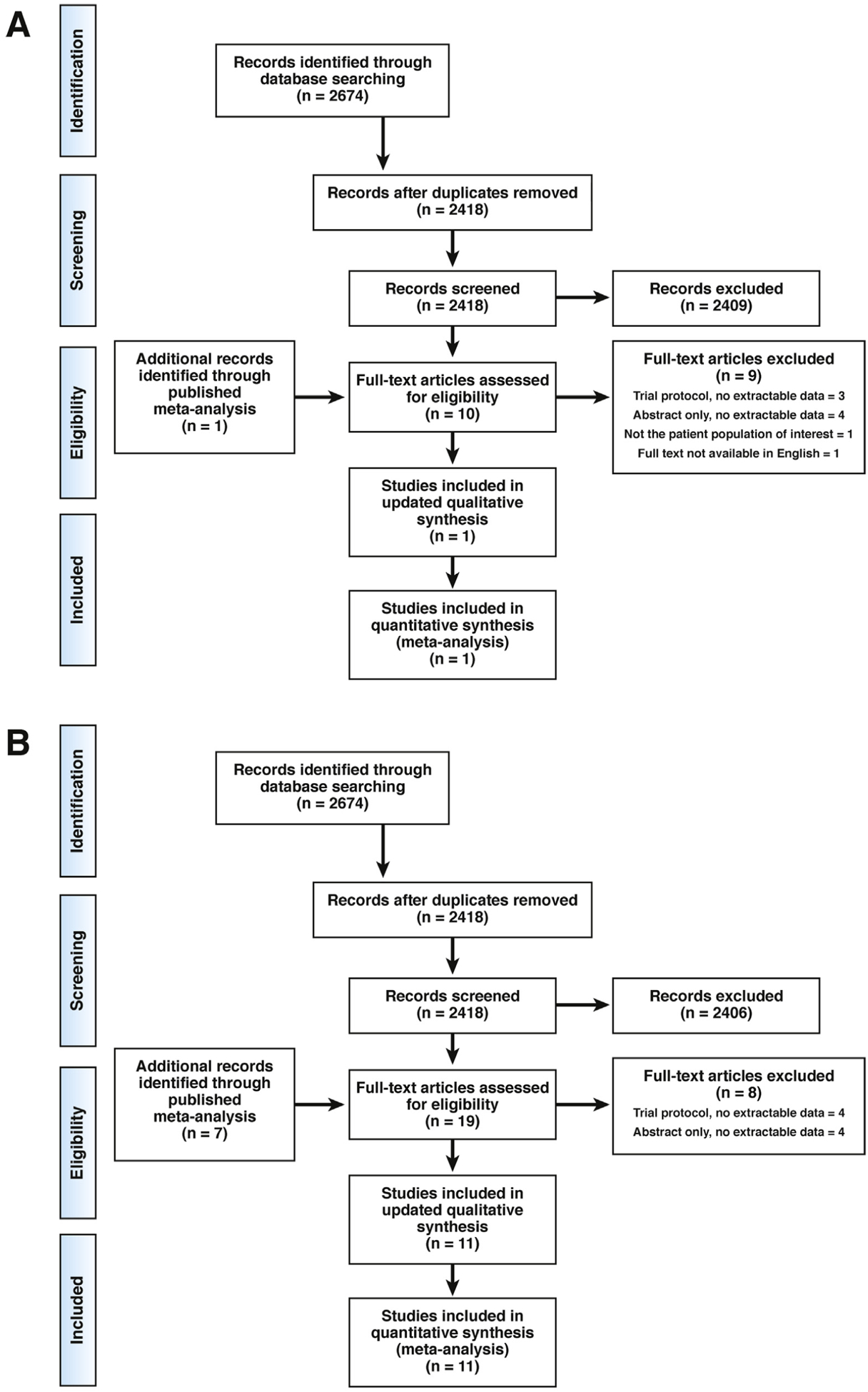
Of the 13 studies included in a comprehensive 2015 Cochrane review102 of multiple different therapies for the treatment and prevention of pouchitis among adults with IPAA for ulcerative colitis, 6 studies103–108 tested probiotics and were included in this technical review; these studies analyzed a total of 176 patients (probiotics, n = 93; placebo, n = 83). After screening 2674 titles and abstracts and assessing 2 new full-text articles, the Technical Review Panel added to the evidence base 1 trial109 (Figure 5), which assessed 17 adults, bringing the total to 193 subjects (probiotics, n = 102; placebo, n = 91). The newly identified study found uncertain benefit with administering C butyricum compared to placebo in preventing relapse of pouchitis (RR, 0.22; 95% CI, 0.03–1.60, Very Low CoE). There was unclear risk of bias with respect to random sequence generation, allocation concealment, and blinding, and this study had small enrollment and a low event rate.
Figure 5.
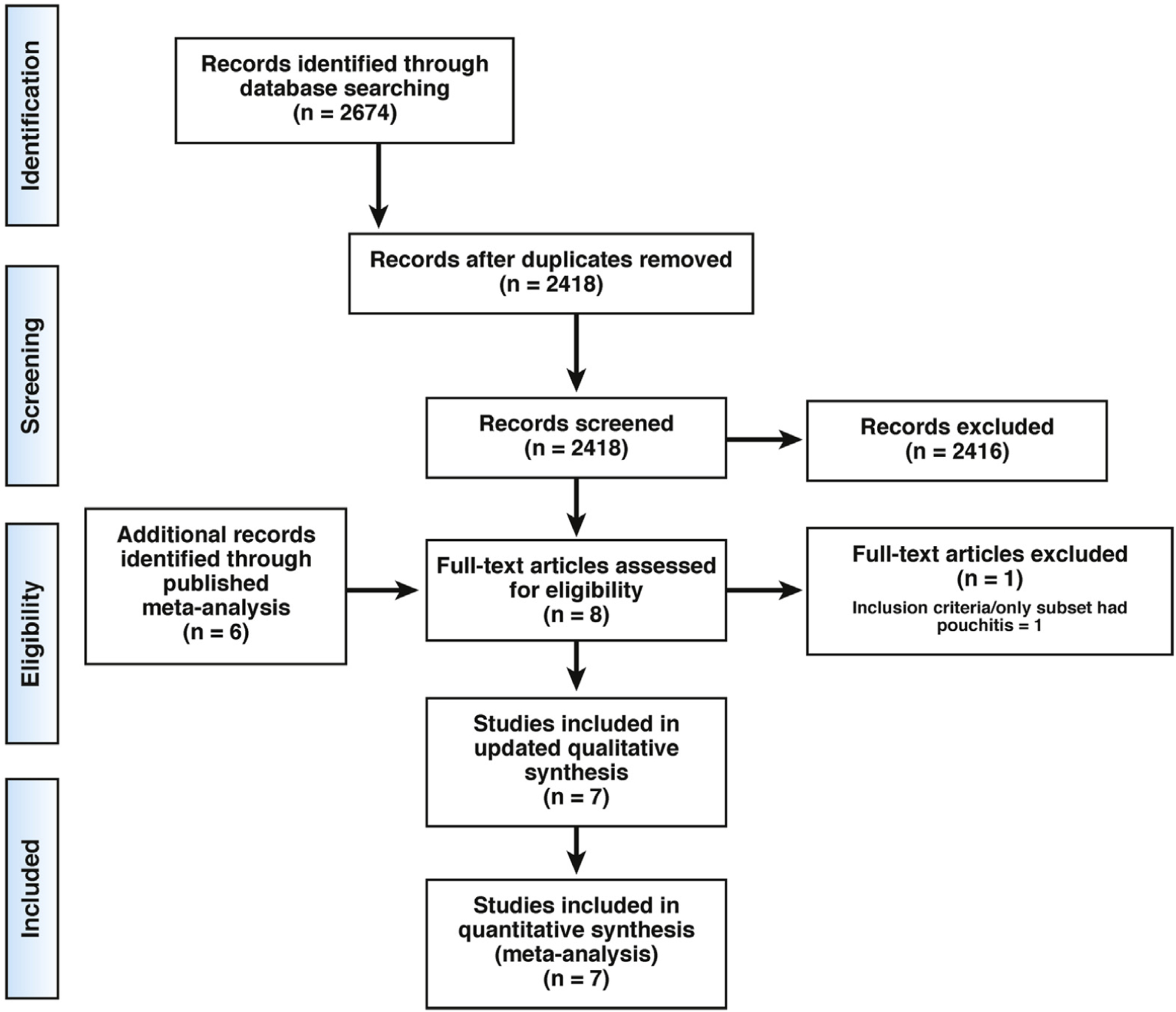
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 Probiotics for pouchitis.
In the previously published meta-anlaysis,102 the effectiveness of the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus was evaluated in 2 studies104,107 reporting on a total of 76 patients (probiotic, n = 40; placebo, n = 36) for maintenance of remission of chronic pouchitis. There may be a benefit in the proportion of patients who maintained remission at 9–12 months when this probiotic formulation was compared to placebo (RR, 20.24; 95% CI, 4.28–95.81, Low CoE). Two different studies105,108 tested the same 8-strain probiotic formulation against placebo or no treatment for the prevention of an initial episode of acute pouchitis among 68 patients (probiotic, n = 36; placebo/no treatment, n = 32). Patients receiving probiotics were more likely to have zero acute pouchitis episodes over 12 months compared to patients receiving placebo or no treatment (RR, 1.29; 95% CI, 1.03–1.61, Very Low CoE). Although 1 of these studies105 had a placebo arm, the second trial108 was an open-label study that contained a high risk of bias with respect to blinding; furthermore, the number of events was small. Smaller individual studies examining L rhamnosus ATCC 53103106 or B longum subsp longum103 found no clear benefit for either of these probiotics, although they were not likely powered adequately to detect a clinical effect, if one exists. The evidence is summarized in Appendix 5.
The overall CoE across all critical outcomes for probiotics, based on the best available evidence from the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus, for the prevention or maintenance of remission of pouchitis is Very Low.
Discussion
Four published studies examine the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus for adults with IPAA in the setting of chronic ulcerative colitis. These studies revealed a potential benefit for adults with ulcerative colitis and IPAA, both in preventing a first episode of acute pouchitis and in maintaining remission after treatment for pouchitis. However, there has been concern regarding the commercial availability of this formulation, given that litigation between the manufacturer and patent holder has been ongoing. Whether other formulations of this 8-strain probiotic, or other strains or combinations of probiotics, might demonstrate similar beneficial effects in the setting of pouchitis is unclear, given that no other formulation has been tested as rigorously. It also remains unclear whether a potential benefit might exist for patients with IPAA resulting from familial adenomatous polyposis or other intestinal disorders, or for children with IPAA.
Question 6: In Symptomatic Children and Adults With Irritable Bowel Syndrome, Should Probiotics Be Used to Improve Global Response or Abdominal Pain Severity?
Results
Irritable bowel syndrome (IBS) is a chronic gastrointestinal disorder with fluctuating symptoms that include abdominal pain or discomfort and alteration of stool form or frequency.110 Diagnosis is based on symptoms outlined in the Rome criteria. The prevalence of IBS is approximately 20% in North America,111 although the global prevalence is much lower,112 especially if the most recent diagnostic criteria are applied.113 The pathophysiology of IBS is incompletely understood, although multiple peripheral and central mechanisms have been implicated. These mechanisms include altered gastrointestinal motility, sensation, secretion, and barrier function, as well as abnormal brain–gut communication.114
The gut microbiota influence the majority of these physiological processes.114 Transfer of gut bacteria from IBS patients to germ-free rodents can transfer pathologic phenotypes, including altered gastrointestinal transit time or decreased pain threshold.115–117 Several studies have illustrated differences in gut microbiota composition between patients with IBS and healthy controls, with decreased α-diversity being the most consistent observation. However, a similar observation has been made in other chronic conditions, suggesting that this finding is not specific to IBS.113 The lack of known mechanisms by which probiotics may improve symptoms in IBS has not precluded their use, which is quite prevalent based on a survey of clinicians.118 These findings highlight the need for further guidance to facilitate an evidence-based approach to the use of probiotics for IBS. In this technical review, we have compiled evidence from well-conducted randomized placebo-controlled clinical trials of probiotics in IBS to determine whether the use of probiotics is justified in IBS patients.
The Technical Review Panel did not identify a previously published systematic review that assessed the efficacy of probiotics for both children and adults with IBS; thus, we conducted a review of the literature from database inception through December 2018. The team screened 1617 titles and abstracts, assessed 216 full-text articles, and included 55 references119–173 in this review (Figure 6). These studies analyzed a total of 5301 patients (probiotics, n = 2768; placebo, n = 2533). These 55 trials tested 44 different probiotic species/strains or combinations of species/strains; thus, for the majority of probiotics, the total body of evidence is derived from a single trial.
Figure 6.
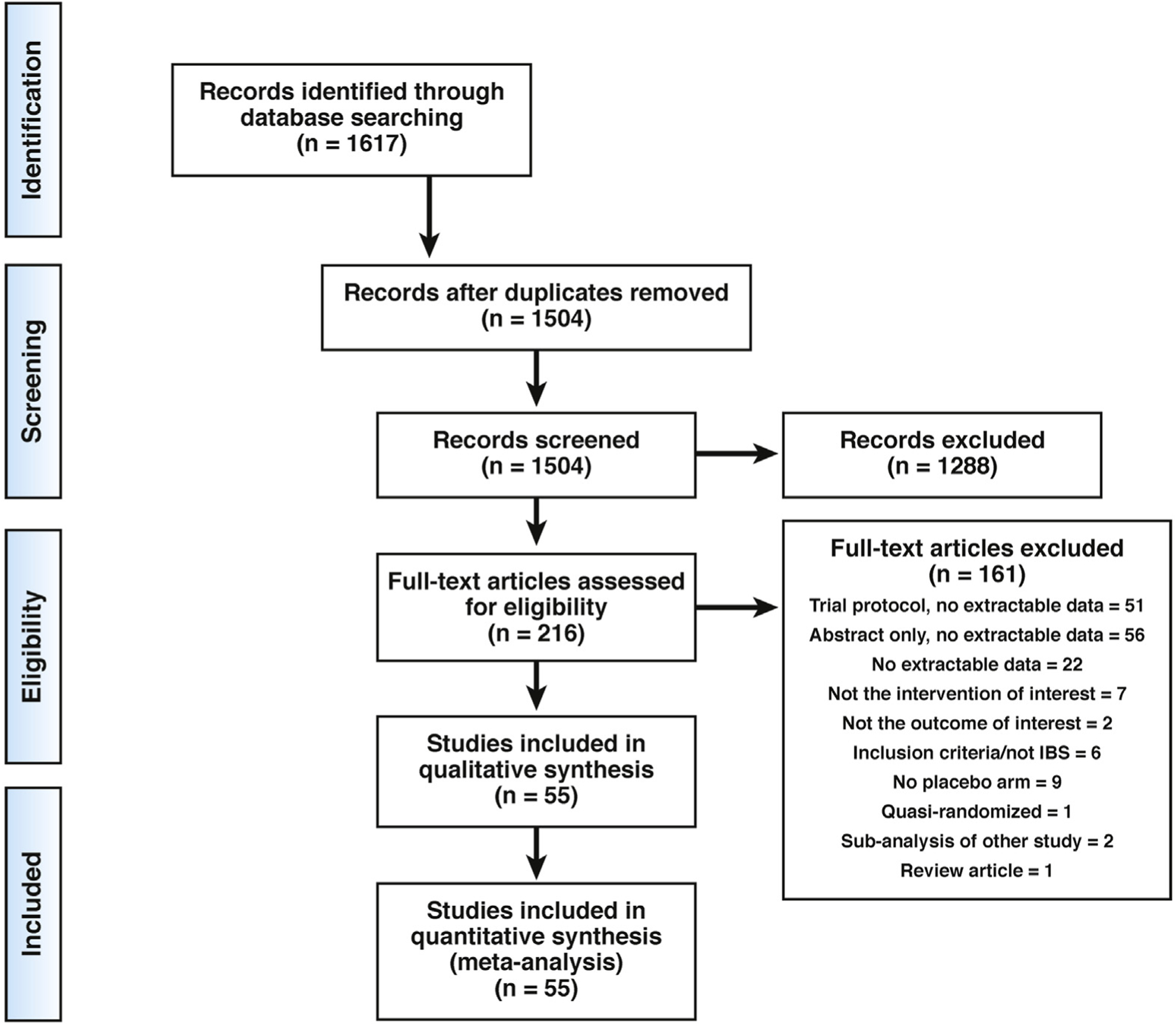
Preferred Reporting Items for Systemic Reviews and Meta-Analysis flow diagram.339 Probiotics to treat IBS.
Three studies135,138,150 tested S boulardii among a total of 232 adults with IBS (probiotic, n = 117; placebo, n = 115). The 3 studies used different outcome measures, but all reported an abdominal pain score. There was no difference between S boulardii and placebo (standardized MD, 0.26; 95% CI, −0.09 to 0.61, Very Low CoE), and there was unclear risk of reporting bias for all 3 studies. Two trials121,124 assessed the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus for abdominal pain, assessed by visual analog scale, among a total of 73 adults with IBS (probiotic, n = 36; placebo, n = 37). This 8-strain combination may decrease abdominal pain (mean decrease, −3.78; 95% CI, −4.93 to −2.62, Very Low CoE). These studies contained a small overall sample size, wide CIs, and enrolled patients that varied with respect to IBS subtype. Furthermore, there was unclear risk of selection, reporting, and detection bias. S boulardii and the 8-strain combination were the only 2 probiotics or combinations of probiotics that had more than 1 trial measure the same outcome, thus facilitating combined case analyses.
For a number of other probiotics, a single trial found that probiotics may be beneficial in adults with IBS. For improvement of global IBS symptoms, these probiotics included L plantarum 299v143; Saccharomyces cerevisiae CNCM I-3856160; E coli DSM 17252130; the 4-strain combination S salivarius subsp thermophilus, L delbrueckii subsp bulgaricus, L acidophilus, and B longum subsp longum129; the 7-strain combination L acidophilus KCTC 11906BP, L plantarum KCTC 11876BP, L rhamnosus KCTC 11868BP, B breve KCTC 11858BP, B animalis subsp lactis KCTC 11903BP, B longum subsp longum KCTC 11860BP, and S salivarius subsp thermophilus KCTC 11870BP144; B bifidum MIMBb75136; the 3-strain combination of L plantarum CECT7484, L plantarum CECT7485, and Pediococcus acidilactici CECT7483152; the 14-strain combination of Bacillus subtilis PXN 21, B bifidum PXN 23, B breve PXN 25, B longum subsp infantis PXN 27, B longum subsp longum PXN 30, L acidophilus PXN 35, L delbrueckii subsp bulgaricus PXN 39, L casei PXN 37, L plantarum PXN 47, L rhamnosus PXN 54, Lactobacillus helveticus PXN 45, Lactobacillus salivarius PXN 57, Lactococcus lactis PXN 63, and S salivarius subsp thermophilus PXN 66166; C butyricum172; and the 4-strain combination B animalis subsp lactis Bb12, L acidophilus LA-5, L delbrueckii subsp bulgaricus LBY-27, and S salivarius subsp thermophilus.151 In contrast to the above studies that report a positive benefit, the 6-strain combination of B longum subsp longum, B bifidum, B animalis subsp lactis, L acidophilus, L rhamnosus, and S salivarius subsp thermophilus, was found to be inferior to placebo for global relief of symptoms in adults with IBS.156
Probiotics shown in a single trial to improve abdominal pain scores in adults with IBS included L plantarum 299v143; L rhamnosus ATCC 53103119; Bacillus coagulans MTCC 5856168; the 2-strain combination of L acidophilus SDC 2012 and SDC 2013128; E coli DSM 17252130; the 4-strain combination of S salivarius subsp thermophilus, L delbrueckii subsp bulgaricus, L acidophilus, and B longum subsp longum129; the 4-strain combination of L rhamnosus NCIMB 30174, L plantarum NCIMB 30173, L acidophilus NCIMB 30175, and Enterococcus faecium NCIMB 30176153; the 3-strain combination of B longum subsp infantis M-63, B breve M-16V, and B longum Reuter ATCC BAA-999162; and the 2-strain combination of B longum subsp longum and L acidophilus.141
For children with IBS, the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus,133 as well as L rhamnosus ATCC 53103,132 may improve abdominal pain scores, and B coagulans Unique IS2 may reduce pain intensity and abdominal discomfort compared to no probiotics.171
Most importantly, the CoE in each of these individual trials was either Low or Very Low. The complete set of analyses is presented in Appendix 6.
The overall CoE across all critical outcomes for probiotics for the treatment of children and adults with IBS was Low.
Discussion
Mechanisms by which probiotics might improve symptoms in IBS remain largely unknown; hence, the choice of which probiotic to test in clinical studies has been largely empiric. This notion is reflected in our finding of 44 distinct probiotics or combinations of probiotics, which results in the majority of evidence for this PICO question derived from a single published trial with relatively small sample sizes and variable quality and risk of bias. Furthermore, the results from these clinical studies can be difficult to interpret due to lack of standardization, differences in study design, lack of subtype stratification, and differences in the dose or duration of therapy.
Our results are consistent overall with a recent meta-analysis of 53 trials that evaluated probiotics among a total of 5545 adults with IBS; the review authors did not find significant benefit in global symptom or abdominal pain scores when trials of single-strain probiotics were grouped and analyzed at the genus level, although the authors did report a potentially significant benefit from a combined case analysis of 19 trials that tested multistrain probiotics.174 Another recent systematic review and meta-analysis focusing on the 8-strain combination of L paracasei subsp paracasei, L plantarum, L acidophilus, L delbrueckii subsp bulgaricus, B longum subsp longum, B breve, B longum subsp infantis, and S salivarius subsp thermophilus also reported no significant benefit of the probiotics in terms of overall response.175 Given the numerous individual probiotic strains that demonstrated benefit in the context of a single trial, one cannot exclude a potential benefit of probiotics for children and adults with IBS. However, the Technical Review Panel also identified numerous registered protocols that had neither peer-reviewed publications nor raw data available for review, highlighting the potential for publication bias. Although the breadth of data regarding probiotic use for IBS is substantial, no single strain or combination has been studied in a sufficiently rigorous manner.
Question 7: In Children With Acute Infectious Gastroenteritis, Should Probiotics Be Used to Reduce the Duration or Severity of Diarrhea?
Results
Acute infectious gastroenteritis is responsible for more than 1.5 million outpatient visits and 200,000 hospitalizations in the United States each year, and remains an important cause of global child mortality.176 Although typically a self-limited condition, acute gastroenteritis extends its economic toll through daycare or school absences and caretakers’ missed days of work. Currently, probiotics are administered in many outpatient, emergency center, and inpatient settings for the treatment of acute gastroenteritis in otherwise healthy infants and children.177–179 A Cochrane review published in 2010180 included 63 randomized and quasi-randomized trials enrolling a total of 8014 adults and children with acute diarrhea of presumed infectious origin that compared probiotics against placebo or no probiotic. From these 63 trials, the 58 studies181–235 (K. Kowalska-Duplaga, unpublished data, 1999; M. Oandasan, unpublished data, 1999; A. Carague-Orendain, unpublished data, 2010) that enrolled infants and children younger than 18 years were included in this technical review. More than one-half of all children studied were enrolled in trials originating in just 3 countries—India, Italy, and Poland—while none of these 58 trials were conducted in the United States or Canada. Forty-one of these studies tested a single probiotic strain, while 17 studies tested combinations of between 2 and 8 organisms. The Cochrane review authors’ meta-analyses revealed that probiotic use was associated with reductions in the mean duration of diarrhea, the mean stool frequency on day 2, and the risk of diarrhea lasting 4 or more days. The individual strains L rhamnosus ATCC 53103, E faecium SF68, and S boulardii each showed benefit in 1 or more of these primary outcomes. Importantly, the authors cited significant concerns regarding potential for bias in multiple domains in the majority of these studies.180
To bring this evidence up to date, the Technical Review Panel screened 4501 titles and abstracts, reviewed 54 new full-text articles, and identified an additional 31 trials236–266 for inclusion (Figure 7). These more recent studies enrolled an additional 5873 participants and were conducted in 15 different countries, with 14 of the 31 trials originating in India, Turkey, and Pakistan. Of these 31 studies, the majority reported beneficial effects associated with probiotics, although 27 of these contained 1 or more concerns regarding risk of bias. Two of the studies with low risk of bias were large, multicenter, randomized, double-blind, placebo-controlled trials conducted in North America. The first, conducted by the Pediatric Emergency Care Applied Research Network,265 enrolled 943 children from 10 emergency departments in the United States; L rhamnosus ATCC 53103 was given at a dose of 1 × 1010 cfu twice daily for 5 days. The second, conducted by Pediatric Emergency Research Canada,266 enrolled 827 children from 6 emergency departments in Canada; the 2-strain combination of L rhamnosus R0011 and L helveticus R0052 was given in a 95:5 ratio at a total dose of 4 × 109 cfu twice daily for 5 days. The primary outcome in both studies was the occurrence of moderate-to-severe gastroenteritis, defined as a total modified Vesikari scale symptom score (which ranges from 0 to 20, with higher scores indicating more severe disease) of 9 or higher. Neither study found a significant difference between the placebo and probiotic groups in the primary outcome. The 2-strain combination had been tested previously in a smaller multicenter study in Canada, and was found to not significantly alter the primary outcome of daycare absenteeism.255 A fourth trial from this region, a single-center study conducted in the United States,245 reported that L rhamnosus ATCC 53103 was no more effective than placebo in reducing the median time to normal stool consistency, or the number of diarrheal stools among 129 patients enrolled at a pediatric emergency department.
Of the 89 total studies included in this review, 58 reported on the duration of diarrhea as an outcome. Taken together, probiotics may decrease the mean duration of diarrhea by 21.91 hours (95% CI, 16.17–27.64, Low CoE). Among the 30 studies reporting on diarrhea lasting more than 3 days, probiotics may decrease the risk of prolonged diarrhea (RR, 0.62; 95% CI, 0.56–0.70, Low CoE), and among the 29 studies reporting on diarrhea lasting more than 4 days, probiotics may decrease the risk of prolonged diarrhea (RR, 0.50; 95% CI, 0.40–0.62, Low CoE). However, no significant differences between probiotic and placebo were found in a combined analysis of 20 studies that reported mean stool frequency on day 2, or in a combined analysis of 14 studies that reported mean stool frequency on day 3. In each of these combined case analyses, the evidence was uncertain.
The most frequently studied probiotic was S boulardii, which has been evaluated in 22 trials enrolling children with acute gastroenteritis. Ten of these 22 studies reported on mean duration of diarrhea, and analysis of this subset revealed that probiotics may reduce the number of hours with diarrhea (mean 28.77 fewer hours; 95% CI, 40.35 fewer hours to 17.18 fewer hours), but the CoE was Very Low. Eight of these 22 studies reported on the number of children with diarrhea lasting >4 days; similarly, S boulardii may reduce the frequency of prolonged diarrhea (RR, 0.45; 95% CI, 0.32–0.64, Very Low CoE). Another single-strain probiotic with a large body of evidence in the context of acute gastroenteritis was L rhamnosus ATCC 53103, which was evaluated in 19 trials, including the large multicenter trial conducted in the United States that was described above.265 Combined case analysis of the 14 studies that reported on mean duration of diarrhea revealed that L rhamnosus ATCC 53103 may reduce the number of hours with diarrhea (mean 23.13 fewer hours; 95% CI, 33.94 fewer hours to 12.33 fewer hours), but the CoE was Low. Although L rhamnosus ATCC 53103 may reduce the proportion of children with diarrhea lasting more than 4 days (RR, 0.38; 95% CI, 0.27 to 0.54, Low CoE), these analyses did not reveal a difference between probiotic and placebo in terms of mean stool frequency on day 2 of illness, rates of severe infection defined by the Vesikari scale, or rates of hospitalization.
L acidophilus was studied in 7 trials. However, 4 of these studies, all identified in the 2010 Cochrane review, tested heat-killed preparations that do not meet the strict definition of probiotics. L acidophilus may reduce the number of hours with diarrhea (mean 7.79 fewer hours; 95% CI, 23.85 fewer hours to 8.28 more hours, Very Low CoE) and may reduce the rate of diarrhea lasting more than 3 days (RR, 0.59; 95% CI, 0.33 to 1.05, Low CoE), but the evidence is very uncertain. Similarly, L reuteri was studied as a single probiotic agent in 5 trials. L reuteri may reduce the number of hours with diarrhea (mean 24.36 fewer hours; 95% CI, 33.55 fewer hours to 13.17 fewer hours, Low CoE) and may reduce the proportion of children with prolonged diarrhea of more than 3 days (RR, 0.67; 95% CI, 0.47 to 0.95, Low CoE), based on the 4 trials that reported these 2 outcomes.
Of the combination probiotic therapies, the most frequently tested was the 2-species combination of L acidophilus and B bifidum, which has been studied in 7 trials enrolling children with acute gastroenteritis. Of the 6 trials that reported on duration of diarrhea, this combination may reduce the number of hours with diarrhea (mean 28.44 fewer hours; 95% CI, 45.72 fewer hours to 11.15 fewer hours), but the CoE was Low. On the other hand, the 2-strain combination of L helveticus R0052 with L rhamnosus R0011 was examined in 3 trials, including the large Canadian multicenter study described above. Combined analyses of these data reveal that probiotics may not affect the duration of diarrhea in hours (mean 1.72 fewer hours; 95% CI, 9.27 fewer hours to 5.83 more hours, Low CoE), and although they may increase hospitalization rates (RR, 1.52; 95% CI, 0.91 to 2.55, Moderate CoE), probiotics do not increase the risk of adverse events (RR, 0.85; 95% CI, 0.71 to 1.02, Moderate CoE). Other probiotic combinations were tested in fewer numbers of trials with smaller numbers of patients; the complete set of analyses is presented in Appendix 7.
The overall CoE across all critical outcomes suggesting that probiotics are not beneficial for the treatment of children with acute gastroenteritis is Moderate on the evidence from studies conducted in the United States and Canada.
Discussion
Guidelines published by multiple professional societies currently support the use of probiotics for otherwise healthy children who present with symptoms consistent with acute gastroenteritis.177–179 These previous guidelines were supported by evidence primarily derived from studies conducted outside of North America; the majority of these studies report a beneficial effect due to probiotics in 1 or more outcomes. Many of these trials have risk of bias in 1 or more critical domains. Perhaps even more importantly, our team highlighted uncertainty with respect to indirectness of results, given that the majority of trials were conducted in eastern Europe and Asia. Thus, the generalizability of these results to the North American population is unclear. In addition to differences in host genetics and dietary practices, North America differs from these other global regions with respect to the endemic pathogens that most frequently cause acute infectious gastroenteritis in children. Our team did not identify a single trial conducted in the United States or Canada that reported a beneficial effect for a probiotic in the context of acute gastroenteritis in children. Thus, the applicability of findings from the trials that did report a beneficial effect is very uncertain.
The results of our combined case analyses are consistent with other systematic reviews and meta-analyses. A recent network meta-analysis reported that the majority of studies showing a beneficial effect for probiotics in the context of acute gastroenteritis had low to very low evidence quality.267 In addition, a small number of species- or strain-specific systematic reviews and meta-analyses have been published. Consistent with our findings, previous analyses have reported limited evidence for the efficacy of L acidophilus LB,268 along with the potential for benefit with probiotics L reuteri269 and S boulardii.270 None of the trials included in these 3 strain-specific systematic reviews were conducted in North America.
The Technical Review Panel identified multiple other concerns among the 89 trials included in this portion of the review. These concerns included many studies with very small sample size and the potential for reporting bias due to the lack of a pre-published registered protocol. We also identified among these studies a higher frequency compared to the studies included in the other 7 PICO questions, of high risk and unclear risk of bias within the 6 domains assessed. Taken together, our team found very little evidence in the published literature to support the continued routine use of probiotics for children with acute gastroenteritis in North America.
Question 8: In Preterm, Low-Birth-Weight Newborns, Should Probiotics Be Used to Prevent Necrotizing Enterocolitis, Sepsis, and All-Cause Mortality?
Preterm birth, defined as delivery before 37 weeks gestational age, affects 1 in 10 newborns in the United States and 15 million pregnancies worldwide each year. Prematurity places infants at increased risk of mortality and multiple morbidities, including sepsis and NEC.271 NEC is an inflammatory necrosis of a portion of the bowel, most typically the terminal ileum and proximal ascending colon, that predisposes survivors to long-term sequelae, such as short bowel syndrome, parenteral nutrition–associated liver injury, and impaired neurodevelopment. Although the etiology of NEC remains unclear, distinct fecal microbiota signatures in infants with NEC compared to otherwise healthy preterm, low-birth-weight infants provide rationale that targeting the gut microbiota with probiotics might prevent morbidity and mortality in this population.272 We identified a recent systematic review and network meta-analysis comparing various probiotics for the prevention of mortality and morbidity in preterm infants.273 This study identified 63 trials274–336 examining 15,712 infants that compared single- and multiple-strain probiotics to placebo for the patient-important outcomes of severe NEC (stage II or higher based on Bell’s criteria), all-cause mortality, culture-proven sepsis, NEC-related mortality, duration of hospitalization, weight at 37 weeks gestational age or at discharge, time to establish full enteral feeds (days), and feeding intolerance.
Combinations of Lactobacillus spp and Bifidobacterium spp (L rhamnosus ATCC 53103 and B longum subsp infantis; or L casei and B breve; or L acidophilus and B longum subsp infantis; or L acidophilus and B bifidum; or L rhamnosus ATCC 53103 and B longum Reuter ATCC BAA-999; or the 4-strain combination of L acidophilus, B bifidum, B animalis subsp lactis, and B longum subsp longum) proved to be the only interventions with moderate- or high-quality evidence of reduced all-cause mortality relative to placebo (OR, 0.56; 95% CI, 0.39–0.80, High CoE). Compared to placebo, combinations of Lactobacillus spp and Bifidobacterium spp (L rhamnosus ATCC 53103 and B longum subsp infantis; or L casei and B breve; or L rhamnosus, L acidophilus, L casei, B longum subsp infantis, B bifidum, and B longum subsp longum; or L acidophilus and B longum subsp infantis; or L acidophilus and B bifidum; or L rhamnosus ATCC 53103 and B longum Reuter ATCC BAA-999; or L acidophilus, B bifidum, B animalis subsp lactis, and B longum subsp longum; OR, 0.35; 95% CI, 0.20–0.59; High CoE), B animalis subsp lactis (including DSM 15954; OR, 0.31; 95% CI, 0.13–0.74; High CoE), L reuteri (DSM 17938 or ATCC 55730; OR, 0.55; 95% CI, 0.34–0.91; High CoE), and L rhamnosus (ATCC 53103 or ATC A07FA or Lcr35; OR, 0.44; 95% CI, 0.21–0.90; Moderate CoE) were the interventions with moderate- or high-quality evidence that significantly reduced rates of severe NEC (stage II or higher). Whereas combinations of Lactobacillus spp, Bifidobacterium spp, and Enterococcus spp (L acidophilus, B longum subsp longum, and E faecalis; or Lactobacillus gasseri PTA-5845, B longum subsp infantis PTA-5843, and E faecium PTA-5844; or L acidophilus, B longum subsp longum, and E faecium; or L acidophilus, B longum subsp infantis, and E faecalis; OR, 0.28; 95% CI, 0.16–0.49; Low CoE), combinations of Bifidobacterium spp and S salivarius subsp thermophilus (B longum subsp infantis, B bifidum, and S salivarius subsp thermophilus; or B longum subsp infantis DSM 33361, B animalis subsp lactis DSM 15954, and S salivarius subsp thermophilus TH-4; OR, 0.38; 95% CI, 0.19–0.75; Low CoE), and the 2-strain combination of a B subtilis and E faecium (OR, 0.23; 95% CI, 0.08–0.63; Low CoE) were the interventions with low- or very low-quality evidence of reduction in NEC when compared to placebo.
Among the interventions with moderate- or high-quality evidence relative to placebo, combinations of Lactobacillus spp, Bifidobacterium spp, and S boulardii (L rhamnosus, L acidophilus, B longum subsp longum, and S boulardii; or L acidophilus, B bifidum, and S boulardii; MD, −3.30; 95% CI, −5.91 to −0.69; High CoE) significantly reduced days to reach full enteral feeds. Combinations of Lactobacillus spp and Bifidobacterium spp (L casei and B breve; or L rhamnosus, L acidophilus, L casei, B longum subsp infantis, B bifidum, and B longum subsp longum; or L acidophilus and B bifidum; or L acidophilus, B bifidum, B animalis subsp lactis, and B longum subsp longum; MD, −2.15; 95% CI, −3.78 to −0.51; Low CoE) and L reuteri (DSM 17938 or ATCC 55730; MD, −2.62; 95% CI, −4.53 to −0.71; Low CoE) demonstrated low- or very-low-quality evidence for significant reduction in days to reach full enteral feeds. B animalis subsp lactis (MD, −13.00; 95% CI, −22.71 to −3.29; High CoE) and L reuteri (DSM 17938 or ATCC 55730; MD, −7.89; 95% CI, −11.60 to −4.17; High CoE) were the only interventions with moderate- or high-quality evidence of a significant reduction in days of hospitalization compared to placebo. The evidence is summarized in Appendix 8.
The overall CoE across all critical outcomes for probiotics for the prevention of NEC, sepsis, and all-cause mortality among preterm, low-birth-weight newborns, based on the best available evidence from the 2-genus combination of 1 or more Lactobacillus spp plus 1 or more Bifidobacterium spp, B animalis subsp lactis, L reuteri (DSM 17938 or ATCC 55730), and L rhamnosus (ATCC 53103 or ATC A07FA or Lcr35) is Moderate/High.
Discussion
The depth and breadth of quality data supporting the use of probiotics for preterm infants is noteworthy. Probiotics typically are used with caution among immunocompromised, critically ill, or otherwise fragile populations, primarily due to concerns regarding potential translocation of the ingested live microbes from the intestine into the bloodstream. In this vulnerable population of premature infants, however, these data strongly suggest that probiotics may protect from mortality and do not increase rates of sepsis. Nonetheless, risks and benefits should be considered carefully, given the possibility of manufacturing contaminants, such as the fungal contaminant that led to a fatal case of gastrointestinal mucormycosis in a preterm infant,337 and given that some centers already have very low rates of NEC due to other standard practices, such as robust donor breast milk feeding programs.338
Moderate- to high-certainty evidence demonstrates the superiority of combinations of Lactobacillus spp and Bifidobacterium spp, B animalis subsp lactis, L reuteri, and L rhamnosus over alternative preventive probiotic treatments. Combinations of Lactobacillus spp, Bifidobacterium spp, and Enterococcus spp, as well as the combination of B subtilis and E faecium, provide the largest reduction in NEC; however, this is supported by low- to very low-certainty evidence. Prioritization of these strains in future trials may be informative, as would be studies that define optimal doses, timing, and frequency of administration. Overall, these data suggest that microbiome-targeting therapies have the potential to reduce mortality, morbidity, length of hospital stay, and other significant costs associated with preterm birth.
Summary and Conclusions
While probiotics have become an integral part of clinical care, we found that, in the majority of the 8 contexts that were examined, there was either insufficient evidence to recommend the use of probiotics as a part of clinical practice or there was a significant knowledge gap that precluded us from making any conclusions. We did, however, find potential utility for the use of individual or combinations of specific probiotic strains in the prevention of NEC and all-cause mortality among preterm, low-birth-weight infants with Moderate/High CoE, prevention of CDAD with Low CoE, and prevention of pouchitis with Very Low CoE. On the other hand, we found that probiotics are not beneficial for treatment of acute gastroenteritis in children in North America with Moderate CoE. It is important to note that although the technical review findings are based on the highest quality of clinical evidence currently available, the potential benefit of probiotic strains or lack thereof is not based on a mechanistic understanding of how probiotics exert such effects. Hence, with additional studies in the future, these conclusions may change. In this technical review, we focused on specific gastrointestinal conditions in which probiotics were being used routinely for adults and children, and in which sufficient clinical studies were available to evaluate their utility. However, this does not imply that such evidence does not exist for other gastrointestinal and non-gastrointestinal disorders. In fact, there is accumulating evidence in support of probiotic use in liver and metabolic diseases, as well as Helicobacter pylori infection, among other conditions, and these could be explored in subsequent technical reviews.
There are several systematic reviews and meta-analyses that have examined the utility of probiotics in disease states, but the results vary based on the approach of the reviews and the quality of the clinical studies included in the analyses. Therefore, it is not surprising that some of our conclusions differ from those of previous reviews on the topic. It is becoming increasingly clear that the effect of a probiotic strain cannot be extrapolated to all probiotics and, in fact, the biological effect of probiotics is species- and strain-specific. Thus, we felt it would not be appropriate to combine the clinical effects of diverse strains under a single umbrella termed probiotics when assessing their utility. Our decision to assess the utility of individual or specific combinations of probiotic strains, rather than the effect of probiotics as a group, was one of the key considerations in our review and represents a key point of difference compared to other recent reviews. Of note, some published trials, most notably many of the earlier studies, did not describe the tested probiotic species at the strain level. Thus, our analyses might not have captured all studies that evaluated a particular organism.
Other unique aspects of our approach may explain differences in our conclusions compared to other reviews. We only included randomized, placebo-controlled trials in our updating of existing evidence from high-quality systematic reviews, and we performed a de novo analysis to include both adults and children in the context of IBS. Additionally, we used the GRADE approach, which considers the risk of bias, inconsistency (or heterogeneity), indirectness, imprecision, and/or publication bias when assessing the certainty of evidence. Among the challenges we faced was lack of appropriate reporting by some authors, due in part to the fact that requirements for reporting clinical trials have evolved over the past few decades, as well as the difficulty with assessing publication bias, given that findings from a large number of registered protocols were never published, potentially skewing the body of evidence toward positive results.
Despite the specificity and stringency of our methods, there are nonetheless limitations in our technical review. We considered the strain specificity when evaluating the outcomes but there are inherent differences in the study design of probiotic trials that could not be completely accounted for in our review. These include differences in dosing and duration of treatment, study population, inclusion and exclusion criteria, use of adjunctive therapies, and outcome measurements. In addition, the lack of large multicenter studies in the majority of instances makes it difficult to assess reproducibility across populations.
The lack of regulatory requirements for over-the-counter probiotics, which are largely considered dietary supplements, affects the quality of results from clinical studies. There are attributes that are unique to probiotic studies and require consideration as they are inadequately and inconsistently addressed in clinical studies. Currently, there are no guidelines for reporting data on product testing in clinical trials, which would include but would not be limited to manufacturing conditions, such as specific media type and culture conditions, strain viability, and shelf life of the product. As a result, it is difficult to compare results of the same strain if it is marketed by different manufacturers. In addition, for the majority of the available probiotics, there is a lack of understanding of the mechanism by which it exerts a biological effect. Finally, there is inadequate harms reporting in the majority of published studies of probiotics.
Knowledge Gaps and Future Directions
Our review not only highlights the challenges in making clinically actionable conclusions from probiotic studies, but also offers an opportunity to implement changes to future studies to improve the utility of such results.
In addition to the existing guidance on reporting findings from a clinical trial, there is a pressing need for guidelines that are specific for probiotic studies to improve transparency, reliability, and clinical applicability. In addition to better characterization and reporting of the probiotic strains, these would include ways to address heterogeneity among studies and uniform harms reporting.
The scientific rationale for use of specific probiotic strains in disease states needs to be better defined and this would require understanding the mechanism and the site of action of probiotic strains or their products, the need for engraftment of probiotic strains and, if required, the conditions needed to facilitate engraftment, and potential off-target effects.
Multicenter studies must be appropriately designed to assess the clinical efficacy of specific probiotic strains.
Supplementary Material
Acknowledgments
The authors sincerely thank Ms Kellee Kaulback, Medical Information Officer, Health Quality Ontario, for helping in the literature search for this technical review.
Funding
NIH support for Geoffrey Preidis:National Institutes of Health, USA (K08 DK113114) and for Purna Kashyap NIH DK114007.
Abbreviations used in this paper:
- AGA
American Gastroenterological Association
- CDAD
Clostridioides difficile–associated diarrhea
- CDI
Clostridioides difficile infection
- CI
confidence interval
- CoE
certainty of evidence
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- IBD
inflammatory bowel disease
- IBS
irritable bowel syndrome
- IPAA
ileal pouch–anal anastomosis
- MD
mean difference
- NEC
necrotizing enterocolitis
- OR
odds ratio
- PICO
population, intervention, comparison, outcomes
- RR
relative risk
Footnotes
Conflicts of interest
These authors disclose the following: Adam V. Weizman has served on an advisory board for Abbvie and Ferring Pharmaceuticals and as a speaker for Janssen, Abbvie and Ferring. Purna C. Kashyap serves on the advisory board of Novome Biotechnologies and is an ad hoc consultant for Otsuka Pharmaceuticals and Pendulum Therapeutics. The remaining authors disclose no conflicts. All members were required to complete disclosure statement. These statements are maintained at the American Gastroenterological Association Institute (AGA) headquarters in Bethesda, Maryland. Panel members disclosed all potential conflicts of interest according to the AGA Institute policy. No Guideline Panel member was excused from participation in the process owing to disqualifying conflict.
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at http://dxdoi.org/10.1053/j.gastro.2020.05.060.
References
- 1.Food and Agricultural Organization of the United Nations (FAO)/World Health Organization (WHO). Health and Nutritional Properties of Probiotics in Food including Powder Milk with Live Lactic Acid Bacteria. Report of a Joint FAO/WHO Expert Consultation on Evaluation of Health and Nutritional Properties of Probiotics in Food Including Powder Milk with Live Lactic Acid Bacteria Cordoba, Argentina; October 1–5 2001. [Google Scholar]
- 2.Probiotics Market Size, Share & Trends Analysis Report By Product (Food & Beverages, Dietary Supplements), By Ingredient (Bacteria, Yeast), By End Use, By Distribution Channel, and Segment Forecasts, 2019–2025. Available at: https://www.grandviewresearch.com/industry-analysis/probiotics-market. Accessed October 5, 2019.
- 3.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol 2011;64:395–400. [DOI] [PubMed] [Google Scholar]
- 4.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011. Available at: www.handbook.cochrane.org. Updated March 2011. Accessed June 21, 2020. [Google Scholar]
- 6.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–394. [DOI] [PubMed] [Google Scholar]
- 8.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–406. [DOI] [PubMed] [Google Scholar]
- 9.Santesso N, Glenton C, Dahm P, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 2020;119:126–135. [DOI] [PubMed] [Google Scholar]
- 10.Martin JS, Monaghan TM, Wilcox MH. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat Rev Gastroenterol Hepatol 2016;13:206–216. [DOI] [PubMed] [Google Scholar]
- 11.Vaughn BP, Rank KM, Khoruts A. Fecal Microbiota transplantation: current status in treatment of GI and liver disease. Clin Gastroenterol Hepatol 2019;17:353–361. [DOI] [PubMed] [Google Scholar]
- 12.Pillai A, Nelson R. Probiotics for treatment of Clostridium difficile-associated colitis in adults. Cochrane Database Syst Rev 2008:CD004611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawrence SJ, Korzenik JR, Mundy LM. Probiotics for recurrent Clostridium difficile disease. J Med Microbiol 2005;54:905–906. [DOI] [PubMed] [Google Scholar]
- 14.McFarland LV, Surawicz CM, Greenberg RN, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA 1994;271:1913–918. [PubMed] [Google Scholar]
- 15.Surawicz CM, McFarland LV, Greenberg RN, et al. The search for a better treatment for recurrent Clostridium difficile disease: use of high-dose vancomycin combined with Saccharomyces boulardii. Clin Infect Dis 2000;31:1012–1017. [DOI] [PubMed] [Google Scholar]
- 16.Wullt M, Hagslatt ML, Odenholt I. Lactobacillus plantarum 299v for the treatment of recurrent Clostridium difficile-associated diarrhoea: a double-blind, placebo-controlled trial. Scand J Infect Dis 2003;35:365–367. [DOI] [PubMed] [Google Scholar]
- 17.Barker AK, Duster M, Valentine S, et al. A randomized controlled trial of probiotics for Clostridium difficile infection in adults (PICO). J Antimicrob Chemother 2017;72:3177–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allen SJ, Wareham K, Wang D, et al. Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2013;382:1249–1257. [DOI] [PubMed] [Google Scholar]
- 19.Arvola T, Laiho K, Torkkeli S, et al. Prophylactic Lactobacillus GG reduces antibiotic-associated diarrhea in children with respiratory infections: a randomized study. Pediatrics 1999;104:e64. [DOI] [PubMed] [Google Scholar]
- 20.Beausoleil M, Fortier N, Guenette S, et al. Effect of a fermented milk combining Lactobacillus acidophilus Cl1285 and Lactobacillus casei in the prevention of antibiotic-associated diarrhea: a randomized, double-blind, placebo-controlled trial. Can J Gastroenterol 2007;21:732–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bravo MV, Bunout D, Leiva L, et al. [Effect of probiotic Saccharomyces boulardii on prevention of antibiotic-associated diarrhea in adult outpatients with amoxicillin treatment]. Rev Med Chil 2008;136:981–988. [PubMed] [Google Scholar]
- 22.Can M, Besirbellioglu BA, Avci IY, et al. Prophylactic Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea: a prospective study. Med Sci Monit 2006;12:PI19–PI22. [PubMed] [Google Scholar]
- 23.Cindoruk M, Erkan G, Karakan T, et al. Efficacy and safety of Saccharomyces boulardii in the 14-day triple anti-Helicobacter pylori therapy: a prospective randomized placebo-controlled double-blind study. Helicobacter 2007;12:309–316. [DOI] [PubMed] [Google Scholar]
- 24.Duman DG, Bor S, Ozutemiz O, et al. Efficacy and safety of Saccharomyces boulardii in prevention of antibiotic-associated diarrhoea due to Helicobacterpylori eradication. Eur J Gastroenterol Hepatol 2005;17:1357–1361. [DOI] [PubMed] [Google Scholar]
- 25.Ehrhardt S, Guo N, Hinz R, et al. Saccharomyces boulardii to prevent antibiotic-associated diarrhea: a randomized, double-masked, placebo-controlled trial. Open Forum Infect Dis 2016;3:ofw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fominykh Y, Aakharenko S, Koning C, et al. The effect of a multispecies probiotic on the intestinal microbiotia during antibiotic therapy. United Eur Gastroenterol J 2013;1S:A248. [Google Scholar]
- 27.Gao XW, Mubasher M, Fang CY, et al. Dose-response efficacy of a proprietary probiotic formula of Lactobacillus acidophilus CL1285 and Lactobacillus casei LBC80R for antibiotic-associated diarrhea and Clostridium difficile-associated diarrhea prophylaxis in adult patients. Am J Gastroenterol 2010;105:1636–1641. [DOI] [PubMed] [Google Scholar]
- 28.Georgieva M, Pancheva R, Rasheva N, et al. Use of the probiotic Lactobacillus reuteri DSM 17938 in the prevention of antibiotic-associated infections in hospitalized Bulgarian children: a randomized, controlled trial. J IMAB 2015;21:895–900. [Google Scholar]
- 29.Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ 2007;335:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imase K, Takahashi M, Tanaka A, et al. Efficacy of Clostridium butyricum preparation concomitantly with Helicobacter pylori eradication therapy in relation to changes in the intestinal microbiota. Microbiol Immunol 2008;52:156–161. [DOI] [PubMed] [Google Scholar]
- 31.Klarin B, Wullt M, Palmquist I, et al. Lactobacillus plantarum 299v reduces colonisation of Clostridium difficile in critically ill patients treated with antibiotics. Acta Anaesthesiol Scand 2008;52:1096–1102. [DOI] [PubMed] [Google Scholar]
- 32.Koning CJ, Jonkers DM, Stobberingh EE, et al. The effect of a multispecies probiotic on the intestinal microbiota and bowel movements in healthy volunteers taking the antibiotic amoxycillin. Am J Gastroenterol 2008;103:178–189. [DOI] [PubMed] [Google Scholar]
- 33.Kotowska M, Albrecht P, Szajewska H. Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther 2005;21:583–590. [DOI] [PubMed] [Google Scholar]
- 34.Lewis SJ, Potts LF, Barry RE. The lack of therapeutic effect of Saccharomyces boulardii in the prevention of antibiotic-related diarrhoea in elderly patients. J Infect 1998;36:171–174. [DOI] [PubMed] [Google Scholar]
- 35.Lonnermark E, Friman V, Lappas G, et al. Intake of Lactobacillus plantarum reduces certain gastrointestinal symptoms during treatment with antibiotics. J Clin Gastroenterol 2010;44:106–112. [DOI] [PubMed] [Google Scholar]
- 36.McFarland LV, Surawicz CM, Greenberg RN, et al. Prevention of beta-lactam-associated diarrhea by Saccharomyces boulardii compared with placebo. Am J Gastroenterol 1995;90:439–448. [PubMed] [Google Scholar]
- 37.Nord CE, Lidbeck A, Orrhage K, et al. Oral supplementation with lactic acid-producing bacteria during intake of clindamycin. Clin Microbiol Infect 1997;3:124–132. [DOI] [PubMed] [Google Scholar]
- 38.Ouwehand AC, DongLian C, Weijian X, et al. Probiotics reduce symptoms of antibiotic use in a hospital setting: a randomized dose response study. Vaccine 2014;32:458–463. [DOI] [PubMed] [Google Scholar]
- 39.Pancheva R, Stoeva K, Georgieva M, et al. A randomized controlled trial on the effect of a combination of Lactobacillus acidophilus, Lactobacillus delbruecki subsp. bulgaricus and Bifidobacterium bifidum in the prophylaxis of vomiting and diarrhea of hospitalized children 1 to 7 years of age. J Pediatr Gastroenterol Nutr 2009;38:E111. [Google Scholar]
- 40.Plummer S, Weaver MA, Harris JC, et al. Clostridium difficile pilot study: effects of probiotic supplementation on the incidence of C. difficile diarrhoea. Int Microbiol 2004;7:59–62. [PubMed] [Google Scholar]
- 41.Pozzoni P, Riva A, Bellatorre AG, et al. Saccharomyces boulardii for the prevention of antibiotic-associated diarrhea in adult hospitalized patients: a single-center, randomized, double-blind, placebo-controlled trial. Am J Gastroenterol 2012;107:922–931. [DOI] [PubMed] [Google Scholar]
- 42.Sampalis J, Psaradellis E, Rampakakis E. Efficacy of BIO K+ CL1285 in the reduction of antibiotic-associated diarrhea—a placebo controlled double-blind randomized, multi-center study. Arch Med Sci 2010;6:56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruszczynski M, Radzikowski A, Szajewska H. Clinical trial: effectiveness of Lactobacillus rhamnosus (strains E/N, Oxy and Pen) in the prevention of antibiotic-associated diarrhoea in children. Aliment Pharmacol Ther 2008;28:154–161. [DOI] [PubMed] [Google Scholar]
- 44.Safdar N, Barigala R, Said A, et al. Feasibility and tolerability of probiotics for prevention of antibiotic-associated diarrhoea in hospitalized US military veterans. J Clin Pharm Ther 2008;33:663–668. [DOI] [PubMed] [Google Scholar]
- 45.Selinger CP, Bell A, Cairns A, et al. Probiotic VSL#3 prevents antibiotic-associated diarrhoea in a double-blind, randomized, placebo-controlled clinical trial. J Hosp Infect 2013;84:159–165. [DOI] [PubMed] [Google Scholar]
- 46.Shan LS, Hou P, Wang ZJ, et al. Prevention and treatment of diarrhoea with Saccharomyces boulardii in children with acute lower respiratory tract infections. Benef Microbes 2013;4:329–334. [DOI] [PubMed] [Google Scholar]
- 47.Shimbo I, Yamaguchi T, Odaka T, et al. Effect of Clostridium butyricum on fecal flora in Helicobacter pylori eradication therapy. World J Gastroenterol 2005;11:7520–7524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Siitonen S, Vapaatalo H, Salminen S, et al. Effect of Lactobacillus GG yoghurt in prevention of antibiotic associated diarrhoea. Ann Med 1990;22:57–59. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan A, Johansson A, Svenungsson B, et al. Effect of Lactobacillus F19 on the emergence of antibiotic-resistant microorganisms in the intestinal microflora. J Antimicrob Chemother 2004;54:791–797. [DOI] [PubMed] [Google Scholar]
- 50.Surawicz CM, Elmer GW, Speelman P, et al. Prevention of antibiotic-associated diarrhea by Saccharomyces boulardii: a prospective study. Gastroenterology 1989;96:981–988. [DOI] [PubMed] [Google Scholar]
- 51.Thomas MR, Litin SC, Osmon DR, et al. Lack of effect of Lactobacillus GG on antibiotic-associated diarrhea: a randomized, placebo-controlled trial. Mayo Clin Proc 2001;76:883–889. [DOI] [PubMed] [Google Scholar]
- 52.Wenus C, Goll R, Loken EB, et al. Prevention of antibiotic-associated diarrhoea by a fermented probiotic milk drink. Eur J Clin Nutr 2008;62:299–301. [DOI] [PubMed] [Google Scholar]
- 53.Wong S, Jamous A, O’Driscoll J, et al. A Lactobacillus casei Shirota probiotic drink reduces antibiotic-associated diarrhoea in patients with spinal cord injuries: a randomised controlled trial. Br J Nutr 2014;111:672–678. [DOI] [PubMed] [Google Scholar]
- 54.Goldenberg JZ, Yap C, Lytvyn L, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst 2017;12(12):CD006095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suez J, Zmora N, Zilberman-Schapira G, et al. Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell 2018;174:1406–1423.e16. [DOI] [PubMed] [Google Scholar]
- 56.Ng KM, Aranda-Diaz A, Tropini C, et al. Recovery of the gut microbiota after antibiotics depends on host diet, community context, and environmental reservoirs. Cell Host Microbe 2019;26:650–665.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cai J, Zhao C, Du Y, et al. Comparative efficacy and tolerability of probiotics for antibiotic-associated diarrhea: systematic review with network meta-analysis. United Eur Gastroenterol J 2018;6:169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khanna S, Raffals LE. The microbiome in Crohn’s Disease: role in pathogenesis and role of microbiome replacement therapies. Gastroenterol Clin N Am 2017;46:481–492. [DOI] [PubMed] [Google Scholar]
- 59.Sartor RB, Wu GD. Roles for intestinal bacteria, viruses, and fungi in pathogenesis of inflammatory bowel diseases and therapeutic approaches. Gastroenterology 2017;152:327–339.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cohen LJ, Cho JH, Gevers D, Chu H. Genetic factors and the intestinal microbiome guide development of microbe-based therapies for inflammatory bowel diseases. Gastroenterology 2019;156:2174–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Torres J, Mehandru S, Colombel JF, et al. Crohn’s disease. Lancet 2017;389:1741–1755. [DOI] [PubMed] [Google Scholar]
- 62.Butterworth AD, Thomas AG, Akobeng AK. Probiotics for induction of remission in Crohn’s disease. Cochrane Database Syst Rev 2008; (3):CD006634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schultz M, Timmer A, Herfarth HH, et al. Lactobacillus GG in inducing and maintaining remission of Crohn’s disease. BMC Gastroenterol 2004;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bousvaros A, Guandalini S, Baldassano RN, et al. A randomized, double-blind trial of Lactobacillus GG versus placebo in addition to standard maintenance therapy for children with Crohn’s disease. Inflamm Bowel Dis 2005;11:833–839. [DOI] [PubMed] [Google Scholar]
- 65.Campieri M, Rizzello F, Venturi A, et al. Combination of antibiotic and probiotic treatment is efficacious in prophylaxis of post-operative recurrence of Crohn’s disease: a randomized controlled study vs mesalamine. Gastroenterology 2000;118:A781. [Google Scholar]
- 66.Guslandi M, Mezzi G, Sorghi M, et al. Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci 2000;45:1462–1464. [DOI] [PubMed] [Google Scholar]
- 67.Malchow HA. Crohn’s disease and Escherichia coli. A new approach in therapy to maintain remission of colonic Crohn’s disease? J Clin Gastroenterol 1997;25:653–658. [DOI] [PubMed] [Google Scholar]
- 68.Prantera C, Scribano ML, Falasco G, et al. Ineffectiveness of probiotics in preventing recurrence after curative resection for Crohn’s disease: a randomised controlled trial with Lactobacillus GG. Gut 2002;51:405–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zocco MA, Zileri Dal Verme L, Armuzzi A, et al. Comparison of Lactobacillus GG and mesalazine in maintaining remission of ulcerative colitis and Crohn’s disease. Gastroenterology 2003;124:A201. [Google Scholar]
- 70.Rolfe VE, Fortun PJ, Hawkey CJ, et al. Probiotics for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev 2006;4:CD004826. [DOI] [PubMed] [Google Scholar]
- 71.Marteau P, Lemann M, Seksik P, et al. Ineffectiveness of Lactobacillus johnsonii LA1 for prophylaxis of post-operative recurrence in Crohn’s disease: a randomised, double blind, placebo controlled GETAID trial. Gut 2006;55:842–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Gossum A, Dewit O, Louis E, et al. Multicenter randomized-controlled clinical trial of probiotics (Lactobacillus johnsonii, LA1) on early endoscopic recurrence of Crohn’s disease after lleo-caecal resection. Inflamm Bowel Dis 2007;13:135–142. [DOI] [PubMed] [Google Scholar]
- 73.Bourreille A, Cadiot G, Le Dreau G, et al. Saccharomyces boulardii does not prevent relapse of Crohn’s disease. Clin Gastroenterol Hepatol 2013;11:982–987. [DOI] [PubMed] [Google Scholar]
- 74.Fedorak RN, Feagan BG, Hotte N, et al. The probiotic VSL#3 has anti-inflammatory effects and could reduce endoscopic recurrence after surgery for Crohn’s disease. Clin Gastroenterol Hepatol 2015;13:928–935 e2. [DOI] [PubMed] [Google Scholar]
- 75.Derwa Y, Gracie DJ, Hamlin PJ, et al. Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther 2017;46:389–400. [DOI] [PubMed] [Google Scholar]
- 76.Feuerstein JD, Moss AC, Farraye FA. Ulcerative colitis. Mayo Clin Proc 2019;94:1357–1373. [DOI] [PubMed] [Google Scholar]
- 77.Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology 2014;146:1489–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Paramsothy S, Kamm MA, Kaakoush NO, et al. Multi-donor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet 2017;389:1218–1228. [DOI] [PubMed] [Google Scholar]
- 79.Mallon P, McKay D, Kirk S, et al. Probiotics for induction of remission in ulcerative colitis. Cochrane Database Syst Rev 2007;4:CD005573. [DOI] [PubMed] [Google Scholar]
- 80.Furrie E, Macfarlane S, Kennedy A, et al. Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: a randomised controlled pilot trial. Gut 2005;54:242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kato K, Mizuno S, Umesaki Y, et al. Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther 2004;20:1133–1141. [DOI] [PubMed] [Google Scholar]
- 82.Rembacken BJ, Snelling AM, Hawkey PM, et al. Nonpathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet 1999;354:635–639. [DOI] [PubMed] [Google Scholar]
- 83.Tursi A, Brandimarte G, Giorgetti GM, et al. Low-dose balsalazide plus a high-potency probiotic preparation is more effective than balsalazide alone or mesalazine in the treatment of acute mild-to-moderate ulcerative colitis. Med Sci Monit 2004;10:PI126–PI131. [PubMed] [Google Scholar]
- 84.Miele E, Pascarella F, Giannetti E, et al. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol 2009;104:437–443. [DOI] [PubMed] [Google Scholar]
- 85.Sood A, Midha V, Makharia GK, et al. The probiotic preparation, VSL#3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin Gastroenterol Hepatol 2009;7:1202–1209; 9 e1. [DOI] [PubMed] [Google Scholar]
- 86.Matthes H, Krummenerl T, Giensch M, et al. Clinical trial: probiotic treatment of acute distal ulcerative colitis with rectally administered Escherichia coli Nissle 1917 (EcN). BMC Complement Altern Med 2010;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tursi A, Brandimarte G, Papa A, et al. Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL#3 as adjunctive to a standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 2010;105:2218–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Oliva S, Di Nardo G, Ferrari F, et al. Randomised clinical trial: the effectiveness of Lactobacillus reuteri ATCC 55730 rectal enema in children with active distal ulcerative colitis. Aliment Pharmacol Ther 2012;35:327–334. [DOI] [PubMed] [Google Scholar]
- 89.Petersen AM, Mirsepasi H, Halkjaer SI, et al. Ciprofloxacin and probiotic Escherichia coli Nissle add-on treatment in active ulcerative colitis: a double-blind randomized placebo controlled clinical trial. J Crohns Colitis 2014;8:1498–1505. [DOI] [PubMed] [Google Scholar]
- 90.Tamaki H, Nakase H, Inoue S, et al. Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: a randomized, double-blinded, placebo-controlled multicenter trial. Dig Endosc 2016;28:67–74. [DOI] [PubMed] [Google Scholar]
- 91.Naidoo K, Gordon M, Fagbemi AO, et al. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev 2011;12:CD007443. [DOI] [PubMed] [Google Scholar]
- 92.Kruis W, Schutz E, Fric P, et al. Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 1997;11:853–858. [DOI] [PubMed] [Google Scholar]
- 93.Kruis W, Fric P, Pokrotnieks J, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004;53:1617–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wildt S, Nordgaard I, Hansen U, et al. A randomised double-blind placebo-controlled trial with Lactobacillus acidophilus La-5 and Bifidobacterium animalis subsp. lactis BB-12 for maintenance of remission in ulcerative colitis. J Crohns Colitis 2011;5:115–121. [DOI] [PubMed] [Google Scholar]
- 95.Zocco MA, dal Verme LZ, Cremonini F, et al. Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 2006;23:1567–1574. [DOI] [PubMed] [Google Scholar]
- 96.Yoshimatsu Y, Yamada A, Furukawa R, et al. Effectiveness of probiotic therapy for the prevention of relapse in patients with inactive ulcerative colitis. World J Gastroenterol 2015;21:5985–5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Matsuoka K, Uemura Y, Kanai T, et al. Efficacy of Bifidobacterium breve fermented milk in maintaining remission of ulcerative colitis. Dig Dis Sci 2018;63:1910–1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dalal RL, Shen B, Schwartz DA. Management of pouchitis and other common complications of the pouch. Inflamm Bowel Dis 2018;24:989–996. [DOI] [PubMed] [Google Scholar]
- 99.Reshef L, Kovacs A, Ofer A, et al. Pouch inflammation is associated with a decrease in specific bacterial taxa. Gastroenterology 2015;149:718–727. [DOI] [PubMed] [Google Scholar]
- 100.Dubinsky V, Reshef L, Bar N, et al. Predominantly antibiotic-resistant intestinal microbiome persists in patients with pouchitis who respond to antibiotic therapy. Gastroenterology 2020;158:610–624.e13. [DOI] [PubMed] [Google Scholar]
- 101.Paramsothy S, Paramsothy R, Rubin DT, et al. Faecal microbiota transplantation for inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis 2017;11:1180–1199. [DOI] [PubMed] [Google Scholar]
- 102.Singh S, Stroud AM, Holubar SD, et al. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev 2015;11:CD001176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Brown SJ, Megan J, Smith S, et al. Bifidobacterium longum BB-536 and prevention of acute pouchitis. Gastroenterology 2004;126:S465. [Google Scholar]
- 104.Gionchetti P, Rizzello F, Venturi A, et al. Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology 2000;119:305–309. [DOI] [PubMed] [Google Scholar]
- 105.Gionchetti P, Rizzello F, Helwig U, et al. Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology 2003;124:1202–1209. [DOI] [PubMed] [Google Scholar]
- 106.Kuisma J, Mentula S, Jarvinen H, et al. Effect of Lactobacillus rhamnosus GG on ileal pouch inflammation and microbial flora. Aliment Pharmacol Ther 2003;17:509–515. [DOI] [PubMed] [Google Scholar]
- 107.Mimura T, Rizzello F, Helwig U, et al. Once daily high dose probiotic therapy (VSL#3) for maintaining remission in recurrent or refractory pouchitis. Gut 2004;53:108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pronio A, Montesani C, Butteroni C, et al. Probiotic administration in patients with ileal pouch-anal anastomosis for ulcerative colitis is associated with expansion of mucosal regulatory cells. Inflamm Bowel Dis 2008;14:662–668. [DOI] [PubMed] [Google Scholar]
- 109.Yasueda A, Mizushima T, Nezu R, et al. The effect of Clostridium butyricum MIYAIRI on the prevention of pouchitis and alteration of the microbiota profile in patients with ulcerative colitis. Surg Today 2016;46:939–949. [DOI] [PubMed] [Google Scholar]
- 110.Ford AC, Lacy BE, Talley NJ. Irritable bowel syndrome. N Engl J Med 2017;376:2566–2578. [DOI] [PubMed] [Google Scholar]
- 111.Saito YA, Schoenfeld P, Locke GR 3rd. The epidemiology of irritable bowel syndrome in North America: a systematic review. Am J Gastroenterol 2002;97:1910–1915. [DOI] [PubMed] [Google Scholar]
- 112.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol 2014;6:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Palsson OS, Whitehead WE, van Tilburg MA, et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology 2016;150:P1481–P1491. [Google Scholar]
- 114.Bhattarai Y, Muniz Pedrogo DA, Kashyap PC. Irritable bowel syndrome: a gut microbiota-related disorder? Am J Physiol Gastrointest Liver Physiol 2017;312:G52–G62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Crouzet L, Gaultier E, Del’Homme C, et al. The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota. Neurogastroenterol Motil 2013;25:e272–e282. [DOI] [PubMed] [Google Scholar]
- 116.Touw K, Ringus DL, Hubert N, et al. Mutual reinforcement of pathophysiological host-microbe interactions in intestinal stasis models. Physiol Rep 2017;5(6):e13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.De Palma G, Lynch MD, Lu J, et al. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci Transl Med 2017;9(379):eaaf6397. [DOI] [PubMed] [Google Scholar]
- 118.Williams MD, Ha CY, Ciorba MA. Probiotics as therapy in gastroenterology: a study of physician opinions and recommendations. J Clin Gastroenterol 2010;44:631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.O’Sullivan M, O’Morain C. Bacterial supplementation in the irritable bowel syndrome. A randomised double-blind placebo-controlled crossover study. Dig Liver Dis 2000;32:294–301. [DOI] [PubMed] [Google Scholar]
- 120.Niedzielin K, Kordecki H, Birkenfeld B. A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299V in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol 2001;13:1143–1147. [DOI] [PubMed] [Google Scholar]
- 121.Kim H, Camilleri M, McKinzie S, et al. A randomized controlled trial of a probiotic, VSL#3, on gut transit and symptoms in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2003;17:895–904. [DOI] [PubMed] [Google Scholar]
- 122.Bauserman M, Bausserman M, Michail S. The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. J Pediatr 2005;147:197–201. [DOI] [PubMed] [Google Scholar]
- 123.Kajander K, Hatakka K, Poussa T, et al. A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6-month intervention. Aliment Pharmacol Ther 2005;22:387–394. [DOI] [PubMed] [Google Scholar]
- 124.Kim H, Vazquez RM, Camilleri M, et al. A randomized controlled trial of a probiotic combination VSL# 3 and placebo in irritable bowel syndrome with bloating. Neurogastroenterol Motil 2005;17:687–696. [DOI] [PubMed] [Google Scholar]
- 125.Gawronska A, Dziechciarz P, Horvath A, et al. A randomized double-blind placebo-controlled trial of Lactobacillus GG for abdominal pain disorders in children. Aliment Pharmacol Ther 2007;25:177–184. [DOI] [PubMed] [Google Scholar]
- 126.Guyonnet D, Chassany O, Ducrotte P, et al. Effect of a fermented milk containing Bifidobacterium animalis DN-173 010 on the health-related quality of life and symptoms in irritable bowel syndrome in adults in primary care: a multicentre, randomized, double-blind, controlled trial. Aliment Pharmacol Ther 2007;26:475–486. [DOI] [PubMed] [Google Scholar]
- 127.Drouault-Holowacz S, Bieuvelet S, Burckel A, et al. A double blind randomized controlled trial of a probiotic combination in 100 patients with irritable bowel syndrome. Gastroenterol Clin Biol 2008;32:147–152. [DOI] [PubMed] [Google Scholar]
- 128.Sinn D, Song J, Kim H, et al. Therapeutic effect of Lactobacillus acidophilus-SDC 2012, 2013 in patients with irritable bowel syndrome. Dig Dis Sci 2008;53:2714–2718. [DOI] [PubMed] [Google Scholar]
- 129.Zeng J, Li Y, Zuo X, et al. Clinical trial: effect of active lactic acid bacteria on mucosal barrier function in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2008;28:994–1002. [DOI] [PubMed] [Google Scholar]
- 130.Enck P, Zimmermann K, Menke G, et al. Randomized controlled treatment trial of irritable bowel syndrome with a probiotic E.-coli preparation (DSM17252) compared to placebo. Z Gastroenterol 2009;47:209–214. [DOI] [PubMed] [Google Scholar]
- 131.Williams E, Stimpson J, Wang D, et al. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Aliment Pharmacol Ther 2009;29:97–103. [DOI] [PubMed] [Google Scholar]
- 132.Francavilla R, Miniello V, Magistà A, et al. A randomized controlled trial of Lactobacillus GG in children with functional abdominal pain. Pediatrics 2010;126:e1445–e1452. [DOI] [PubMed] [Google Scholar]
- 133.Guandalini S, Magazzu G, Chiaro A, et al. VSL#3 improves symptoms in children with irritable bowel syndrome: a multicenter, randomized, placebo-controlled, double-blind, crossover study. J Pediatr Gastroenterol Nutr 2010;51:24–30. [DOI] [PubMed] [Google Scholar]
- 134.Simrén M, Ohman L, Olsson J, et al. Clinical trial: the effects of a fermented milk containing three probiotic bacteria in patients with irritable bowel syndrome—a randomized, double-blind, controlled study. Aliment Pharmacol Ther 2010;31:218–227. [DOI] [PubMed] [Google Scholar]
- 135.Choi C, Jo S, Park H, et al. A randomized, double-blind, placebo-controlled multicenter trial of Saccharomyces boulardii in irritable bowel syndrome: effect on quality of life. J Clin Gastroenterol 2011;45:679–683. [DOI] [PubMed] [Google Scholar]
- 136.Guglielmetti S, Mora D, Gschwender M, et al. Randomised clinical trial: Bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life–a double-blind, placebo-controlled study. Aliment Pharmacol Ther 2011;33:1123–1132. [DOI] [PubMed] [Google Scholar]
- 137.Hong KS, Kang HW, Im JP, et al. Effect of probiotics on symptoms in Korean adults with irritable bowel syndrome. Gut Liver 2009;3:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kabir M, Ishaque S, Ali M, et al. Role of Saccharomyces boulardii in diarrhea predominant irritable bowel syndrome. Mymensingh Med J 2011;20:397–401. [PubMed] [Google Scholar]
- 139.Michail S, Kenche H. Gut microbiota is not modified by randomized, double-blind, placebo-controlled trial of VSL#3 in diarrhea-predominant irritable bowel syndrome. Probiotics Antimicrob Proteins 2011;3:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ringel-Kulka T, Palsson O, Maier D, et al. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study. J Clin Gastroenterol 2011;45:518–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cui S, Hu Y. Multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Int J Clin Exp Med 2012;5:238–244. [PMC free article] [PubMed] [Google Scholar]
- 142.Dapoigny M, Piche T, Ducrotte P, et al. Efficacy and safety profile of LCR35 complete freeze-dried culture in irritable bowel syndrome: a randomized, double-blind study. World J Gastroenterol 2012;18:2067–2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ducrotté P, Sawant P, Jayanthi V. Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World J Gastroenterol 2012;18:4012–4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ki CB, Mun JS, Hwan CC, et al. The effect of a multispecies probiotic mixture on the symptoms and fecal microbiota in diarrhea-dominant irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. J Clin Gastroenterol 2012;46:220–227. [DOI] [PubMed] [Google Scholar]
- 145.Kruis W, Chrubasik S, Boehm S, et al. A double-blind placebo-controlled trial to study therapeutic effects of probiotic Escherichia coli Nissle 1917 in subgroups of patients with irritable bowel syndrome. Int J Colorectal Dis 2012;27:467–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Murakami K, Habukawa C, Nobuta Y, et al. The effect of Lactobacillus brevis KB290 against irritable bowel syndrome: a placebo-controlled double-blind crossover trial. Biopsychosoc Med 2012;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Amirimani B, Nikfam S, Albaji M, et al. Probiotic vs. placebo in irritable bowel syndrome:a randomized controlled trial. Middle East J Dig Dis 2013;5:98–102. [PMC free article] [PubMed] [Google Scholar]
- 148.Begtrup LM, de Muckadell OBS, Kjeldsen J, et al. Long-term treatment with probiotics in primary care patients with irritable bowel syndrome—a randomised, double-blind, placebo controlled trial. Scand J Gastroenterol 2013;48:1127–1135. [DOI] [PubMed] [Google Scholar]
- 149.Roberts L, McCahon D, Holder R, et al. A randomised controlled trial of a probiotic ‘functional food’ in the management of irritable bowel syndrome. BMC Gastroenterol 2013;13:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Abbas Z, Yakoob J, Jafri W, et al. Cytokine and clinical response to Saccharomyces boulardii therapy in diarrhea-dominant irritable bowel syndrome: a randomized trial. Eur J Gastroenterol Hepatol 2014;26:630–639. [DOI] [PubMed] [Google Scholar]
- 151.Jafari E, Vahedi H, Merat S, et al. Therapeutic effects, tolerability and safety of a multi-strain probiotic in Iranian adults with irritable bowel syndrome and bloating. Arch Iran Med 2014;17:466–470. [PubMed] [Google Scholar]
- 152.Lorenzo-Zuniga V, Llop E, Suarez C, et al. I.31, a new combination of probiotics, improves irritable bowel syndrome-related quality of life. World J Gastroenterol 2014;20:8709–8716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ludidi S, Jonkers DM, Koning CJ, et al. Randomized clinical trial on the effect of a multispecies probiotic on visceroperception in hypersensitive IBS patients. Neurogastroenterol Motil 2014;26:705–714. [DOI] [PubMed] [Google Scholar]
- 154.Sisson G, Ayis S, Sherwood R, et al. Randomised clinical trial: a liquid multi-strain probiotic vs. placebo in the irritable bowel syndrome—a 12 week double-blind study. Aliment Pharmacol Ther 2014;40:51–62. [DOI] [PubMed] [Google Scholar]
- 155.Stevenson C, Blaauw R, Fredericks E, et al. Randomized clinical trial: effect of Lactobacillus plantarum 299 v on symptoms of irritable bowel syndrome. Nutrition 2014;30:1151–1157. [DOI] [PubMed] [Google Scholar]
- 156.Yoon JS, Sohn W, Lee OY, et al. Effect of multispecies probiotics on irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. J Gastroenterol Hepatol 2014;29:52–59. [DOI] [PubMed] [Google Scholar]
- 157.Pineton de Chambrun G, Neut C, Chau A, et al. A randomized clinical trial of Saccharomyces cerevisiae versus placebo in the irritable bowel syndrome. Dig Liver Dis 2015;47:119–124. [DOI] [PubMed] [Google Scholar]
- 158.Yoon H, Park YS, Lee DH, et al. Effect of administering a multi-species probitic mixture on the change in facial microbiota and symptoms of irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. J Clin Biochem Nutr 2015;57:129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Majeed M, Nagabhushanam K, Natarajan S, et al. Bacillus coagulans MTCC 5856 supplementation in the management of diarrhea predominant irritable bowel syndrome: a double blind randomized placebo controlled pilot clinical study. Nutr J 2016;15:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Spiller R, Pelerin F, Cayzeele DA, et al. Randomized double blind placebo-controlled trial of Saccharomyces cerevisiae CNCM I-3856 in irritable bowel syndrome: improvement in abdominal pain and bloating in those with predominant constipation. United Eur Gastroenterol J 2016;4:353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Thijssen A, Clemens C, Vankerckhoven V, et al. Efficacy of Lactobacillus casei Shirota for patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol 2016;28:8–14. [DOI] [PubMed] [Google Scholar]
- 162.Giannetti E, Maglione M, Alessandrella A, et al. A mixture of 3 bifidobacteria decreases abdominal pain and improves the quality of life in children with irritable bowel syndrome. J Clini Gastroenterol 2017;51:e5–e10. [DOI] [PubMed] [Google Scholar]
- 163.Jadrešin O, Hojsak I, Mišak Z, et al. Lactobacillus reuteri DSM 17938 in the treatment of functional abdominal pain in children: RCT study. J Pediatr Gastroenterol Nutr 2017;64:925–929. [DOI] [PubMed] [Google Scholar]
- 164.Pinto-Sanchez M, Hall G, Ghajar K, et al. Probiotic Bifidobacterium longum NCC3001 reduces depression scores and alters brain activity: a pilot study in patients with irritable bowel syndrome. Gastroenterology 2017;153:448–459.e8. [DOI] [PubMed] [Google Scholar]
- 165.Cremon C, Guglielmetti S, Gargari G, et al. Effect of Lactobacillus paracasei CNCM I-1572 on symptoms, gut microbiota, short chain fatty acids, and immune activation in patients with irritable bowel syndrome: a pilot randomized clinical trial. United Eur Gastroenterol J 2018;6:604–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ishaque S, Khosruzzaman S, Ahmed D, et al. A randomized placebo-controlled clinical trial of a multi-strain probiotic formulation (Bio-Kult) in the management of diarrhea-predominant irritable bowel syndrome. BMC Gastroenterol 2018;18:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kim JY, Park YJ, Lee HJ, et al. Effect of Lactobacillus gasseri BNR17 on irritable bowel syndrome: a randomized, double-blind, placebo-controlled, dose-finding trial. Food Sci Biotechnol 2018;27:853–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Majeed M, Nagabhushanam K, Arumugam S, et al. Bacillus coagulans MTCC 5856 for the management of major depression with irritable bowel syndrome: a randomised, double-blind, placebo controlled, multi-centre, pilot clinical study. Food Nutr Res 2018;62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Preston K, Krumian R, Hattner J, et al. Lactobacillus acidophilus CL1285, Lactobacillus casei LBC80R and Lactobacillus rhamnosus CLR2 improve quality-of-life and IBS symptoms: a double-blind, randomised, placebo-controlled study. Benef Microbes 2018;9:697–706. [DOI] [PubMed] [Google Scholar]
- 170.Shin SP, Choi YM, Kim WH, et al. A double blind, placebo-controlled, randomized clinical trial that breast milk derived-Lactobacillus gasseri BNR17 mitigated diarrhea-dominant irritable bowel syndrome. J Clin Biochem Nutr 2018;62:179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Sudha MR, Jayanthi N, Aasin M, et al. Efficacy of Bacillus coagulans unique IS2 in treatment of irritable bowel syndrome in children: a double blind, randomised placebo controlled study. Benefic Microbes 2018;9:563–572. [DOI] [PubMed] [Google Scholar]
- 172.Sun YY, Li M, Li YY, et al. The effect of Clostridium butyricum on symptoms and fecal microbiota in diarrhea-dominant irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. Sci Rep 2018;8:2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Yoon JY, Cha JM, Oh JK, et al. Probiotics ameliorate stool consistency in patients with chronic constipation: a randomized, double-blind, placebo-controlled study. Dig Dis Sci 2018;63:2754–2764. [DOI] [PubMed] [Google Scholar]
- 174.Ford AC, Harris LA, Lacy BE, et al. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment Pharmacol Ther 2018;48:1044–1060. [DOI] [PubMed] [Google Scholar]
- 175.Connell M, Shin A, James-Stevenson T, et al. Systematic review and meta-analysis: efficacy of patented probiotic, VSL#3, in irritable bowel syndrome. Neurogastroenterol Motil 2018;30:e13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.King CK, Glass R, Bresee JS, et al. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep 2003;52:1–16. [PubMed] [Google Scholar]
- 177.Guarino A, Ashkenazi S, Gendrel D, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr 2014;59:132–152. [DOI] [PubMed] [Google Scholar]
- 178.Szajewska H, Guarino A, Hojsak I, et al. Use of probiotics for management of acute gastroenteritis: a position paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr 2014;58:531–539. [DOI] [PubMed] [Google Scholar]
- 179.Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea. Clin Infect Dis 2017;65:1963–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev 2010;11:CD003048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Basu S, Chatterjee M, Ganguly S, Chandra PK. Efficacy of Lactobacillus rhamnosus GG in acute watery diarrhoea of Indian children: a randomised controlled trial. J Paediatr Child Health 2007;43:837–842. [DOI] [PubMed] [Google Scholar]
- 182.Basu S, Paul DK, Ganguly S, et al. Efficacy of high-dose Lactobacillus rhamnosus GG in controlling acute watery diarrhea in Indian children: a randomized controlled trial. J Clin Gastroenterol 2009;43:208–213. [DOI] [PubMed] [Google Scholar]
- 183.Bhatnagar S, Singh KD, Sazawal S, et al. Efficacy of milk versus yogurt offered as part of a mixed diet in acute noncholera diarrhea among malnourished children. J Pediatr 1998;132:999–1003. [DOI] [PubMed] [Google Scholar]
- 184.Billoo AG, Memon MA, Khaskheli SA, et al. Role of a probiotic (Saccharomyces boulardii) in management and prevention of diarrhoea. World J Gastroenterol 2006;12:4557–4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Boudraa G, Benbouabdellah M, Hachelaf W, et al. Effect of feeding yogurt versus milk in children with acute diarrhea and carbohydrate malabsorption. J Pediatr Gastroenterol Nutr 2001;33:307–313. [DOI] [PubMed] [Google Scholar]
- 186.Boulloche J, Mouterde O, Mallet E. Management of acute diarrhoea in infants and young children. Controlled study of the anti-diarrheal efficacy of killed L. acidophilus (LB strain) versus a placebo and a reference drug (loperamide). Ann Pediatr 1994;41:457–463. [Google Scholar]
- 187.Canani RB, Cirillo P, Terrin G, et al. Probiotics for treatment of acute diarrhoea in children: randomised clinical trial of five different preparations. BMJ 2007;335:340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Cetina-Sauri G, Sierra Basto G. Evaluation of Saccharomyces boulardii in children with acute diarrhea [Evaluation therapeutique de Saccharomyces boulardii chez des enfants souffrant de diarrhee aigue]. Ann Pediatr 1994;41:397–400. [Google Scholar]
- 189.Chapoy P. Treatment of acute infantile diarrhea: controlled trial of Saccharomyces boulardii [Traitement des diarrhées aiguës infantiles]. Ann Pediatr 1985;32:561–563. [PubMed] [Google Scholar]
- 190.Chen CC, Kong MS, Lai MW, et al. Probiotics have clinical, microbiologic, and immunologic efficacy in acute infectious diarrhea. Pediatr Infect Dis J 2010;29:135–138. [DOI] [PubMed] [Google Scholar]
- 191.Costa-Ribeiro H, Ribeiro TC, Mattos AP, et al. Limitations of probiotic therapy in acute, severe dehydrating diarrhea. J Pediatr Gastroenterol Nutr 2003;36:112–115. [DOI] [PubMed] [Google Scholar]
- 192.Czerwionka-Szaflarska M, Murawska S, Swincow G. Evaluation of influence of oral treatment with probiotic and/or oral rehydration solution on course of acute diarrhoea in children. Prz Gastroenterol 2009;4:166–172. [Google Scholar]
- 193.D’Apuzzo V, Salzberg R. The treatment of acute diarrhoea in paediatrics using Streptococcus faecium: results of a double blind trial [Die Behandlung der akuten Diarrho in der Padiatrie mit Streptococcus faecium: Resultae einer doppleblindstudie]. Ther Umschau 1982;39:1033–1035. [PubMed] [Google Scholar]
- 194.Dubey AP, Rajeshwari K, Chakravarty A, et al. Use of VSL#3 in the treatment of rotavirus diarrhea in children: preliminary results. J Clin Gastroenterol 2008;42(Suppl 3 Pt 1):S126–S129. [DOI] [PubMed] [Google Scholar]
- 195.Frigerio G. A lactic acid producer enterococcus in the prevention of antibiotic-associated diarrhoea and in the treatment of acute diarrhoeal disorders: a double-blind multicentre placebo-controlled clinical trial (abstract). Dig Dis Sci 1986;31:496. [Google Scholar]
- 196.Grandi G, Medina M, Soria R, et al. Probiotics in the management of acute rotavirus diarrhea in Bolivian children: a randomized, double-blind, controlled trial of two different preparations. Pediatr Res 2009;67:447; (abstract 10). [Google Scholar]
- 197.Guandalini S, Pensabene L, Zikri MA, et al. Lactobacillus GG administered in oral rehydration solution to children with acute diarrhea: a multicenter European trial. J Pediatr Gastroenterol Nutr 2000;30:54–60. [DOI] [PubMed] [Google Scholar]
- 198.Guarino A, Canani RB, Spagnuolo MI, et al. Oral bacterial therapy reduces the duration of symptoms and of viral excretion in children with mild diarrhea. J Pediatr Gastroenterol Nutr 1997;25:516–519. [DOI] [PubMed] [Google Scholar]
- 199.Hafeez A, Tariq P, Ali S, et al. The efficacy of Saccharomyces boulardii in the treatment of acute watery diarrhoea in children: a multicentre randomized controlled trial. J Coll Physicians Surg Pak 2002;12:432–434. [Google Scholar]
- 200.Henker J, Laass M, Blokhin BM, et al. The probiotic Escherichia coli strain Nissle 1917 (EcN) stops acute diarrhoea in infants and toddlers. Eur J Pediatr 2007;166:311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Henker J, Laass MW, Blokhin BM, et al. Probiotic Escherichia coli Nissle 1917 versus placebo for treating diarrhea of greater than 4 days duration in infants and toddlers. Pediatr Infect Dis J 2008;27:494–499. [DOI] [PubMed] [Google Scholar]
- 202.Hernandez CL, Pineda EE, Jimenez MIR, et al. Clinical therapeutic affect of Saccharomyces boulardii on children with acute diarrhea. Rev Enferm Infecc Pediatr 1998;11:87–89. [Google Scholar]
- 203.Htwe K, Yee KS, Tin M, et al. Effect of Saccharomyces boulardii in the treatment of acute watery diarrhea in Myanmar children: a randomized controlled study. Am J Trop Med Hyg 2008;78:214–216. [PubMed] [Google Scholar]
- 204.Isolauri E, Kaila M, Mykkanen H, et al. Oral bacteriotherapy for viral gastroenteritis. Dig Dis Sci 1994;39:2595–2600. [DOI] [PubMed] [Google Scholar]
- 205.Jasinski C, Tanzi MN, Schelotto F, et al. Efficacy of Lactobacillus GG in oral rehydration solution [Efecto del Lactobacillus casei administrado en el suero de rehidratacion oral, en el tratamiento de la enfermedad diarreica aguda]. Pediatrika 2002;22:231–243. [Google Scholar]
- 206.Khanna V, Seema A, Ashraf M, et al. Efficacy of tyndalized lactobacillus acidophilus in acute diarrhoea. Indian J Pediatr 2005;72:935–938. [DOI] [PubMed] [Google Scholar]
- 207.Kianifar HR, Farid R, Ahanchian H, et al. Probiotics in the treatment of acute diarrhea in young children. Iran J Med Sci 2009;34:204–207. [Google Scholar]
- 208.Kowalska-Duplaga K, Krzysztof F, Szajewska H, et al. Efficacy of Trilac® in the treatment of acute diarrhoea in infants and young children—a multicentre, randomised, double blind placebo-controlled study. Pediatr Wspolc Gastroenterol Hepatol Zyw Dziecka 2004;6:295–299. [Google Scholar]
- 209.Kurugol Z, Koturoglu G. Effects of Saccharomyces boulardii in children with acute diarrhoea. Acta Paediatr 2005;94:44–47. [DOI] [PubMed] [Google Scholar]
- 210.Lee MC, Lin LH, Hung KL, et al. Oral bacterial therapy promotes recovery from acute diarrhea in children. Acta Paediatr Taiwan 2001;42:301–305. [PubMed] [Google Scholar]
- 211.Lievin-Le Moal V, Sarrazin-Davila LE, Servin AL. An experimental study and a randomized, double-blind, placebo-controlled clinical trial to evaluate the anti-secretory activity of Lactobacillus acidophilus strain LB against nonrotavirus diarrhea. Pediatrics 2007;120:e795–e803. [DOI] [PubMed] [Google Scholar]
- 212.Mao M, Yu T, Xiong Y, et al. Effect of a lactose-free milk formula supplemented with bifidobacteria and streptococci on the recovery from acute diarrhoea. Asia Pac J Clin Nutr 2008;17:30–34. [PubMed] [Google Scholar]
- 213.Misra S, Sabui TK, Pal NK. A randomized controlled trial to evaluate the efficacy of lactobacillus GG in infantile diarrhea. J Pediatr 2009;155:129–132. [DOI] [PubMed] [Google Scholar]
- 214.Narayanappa D. Randomized double blinded controlled trial to evaluate the efficacy and safety of Bifilac in patients with acute viral diarrhea. Indian J Pediatr 2008;75:709–713. [DOI] [PubMed] [Google Scholar]
- 215.Ozkan TB, Sahin E, Erdemir G, et al. Effect of Saccharomyces boulardii in children with acute gastroenteritis and its relationship to the immune response. J Int Med Res 2007;35:201–212. [DOI] [PubMed] [Google Scholar]
- 216.Pant AR, Graham SM, Allen SJ, et al. Lactobacillus GG and acute diarrhoea in young children in the tropics. J Trop Pediatr 1996;42:162–165. [DOI] [PubMed] [Google Scholar]
- 217.Pashapour N, Iou SG. Evaluation of yogurt effect on acute diarrhea in 6–24-month-old hospitalized infants. Turk J Pediatr 2006;48:115–118. [PubMed] [Google Scholar]
- 218.Rafeey M, Ostadrahimi A, Boniadi M, et al. Lactobacillus acidophilus yogurt and supplement in children with acute diarrhea: a clinical trial. Res J Med Sci 2008;2:13–18. [Google Scholar]
- 219.Raza S, Graham SM, Allen SJ, et al. Lactobacillus GG promotes recovery from acute nonbloody diarrhea in Pakistan. Pediatr Infect Dis J 1995;14:107–111. [DOI] [PubMed] [Google Scholar]
- 220.Ritchie BK, Brewster DR, Tran CD, et al. Efficacy of Lactobacillus GG in aboriginal children with acute diarrhoeal disease: a randomised clinical trial. J Pediatr Gastroenterol Nutr 2010;50:619–624. [DOI] [PubMed] [Google Scholar]
- 221.Rosenfeldt V, Michaelsen KF, Jakobsen M, et al. Effect of probiotic Lactobacillus strains in young children hospitalized with acute diarrhea. Pediatr Infect Dis J 2002;21:411–416. [DOI] [PubMed] [Google Scholar]
- 222.Rosenfeldt V, Michaelsen KF, Jakobsen M, et al. Effect of probiotic Lactobacillus strains on acute diarrhea in a cohort of nonhospitalized children attending day-care centers. Pediatr Infect Dis J 2002;21:417–419. [DOI] [PubMed] [Google Scholar]
- 223.Sarker SA, Sultana S, Fuchs GJ, et al. Lactobacillus paracasei strain ST11 has no effect on rotavirus but ameliorates the outcome of nonrotavirus diarrhea in children from Bangladesh. Pediatrics 2005;116:e221–e228. [DOI] [PubMed] [Google Scholar]
- 224.Sepp E, Tamm E, Torm S, et al. Impact of a Lactobacillus probiotic on the faecal microflora in children with shigellosis. Microecol Ther 1995;23:74–80. [Google Scholar]
- 225.Shornikova AV, Isolauri E, Burkanova L, et al. A trial in the Karelian Republic of oral rehydration and Lactobacillus GG for treatment of acute diarrhoea. Acta Paediatr 1997;86:460–465. [DOI] [PubMed] [Google Scholar]
- 226.Shornikova AV, Casas IA, Mykkanen H, et al. Bacteriotherapy with Lactobacillus reuteri in rotavirus gastroenteritis. Pediatr Infect Dis J 1997;16:1103–1107. [DOI] [PubMed] [Google Scholar]
- 227.Shornikova AV, Casas IA, Isolauri E, et al. Lactobacillus reuteri as a therapeutic agent in acute diarrhea in young children. J Pediatr Gastroenterol Nutr 1997;24:399–404. [DOI] [PubMed] [Google Scholar]
- 228.Simakachorn N, Pichaipat V, Rithipornpaisarn P, et al. Clinical evaluation of the addition of lyophilized, heat-killed Lactobacillus acidophilus LB to oral rehydration therapy in the treatment of acute diarrhea in children. J Pediatr Gastroenterol Nutr 2000;30:68–72. [DOI] [PubMed] [Google Scholar]
- 229.Sugita T, Togawa M. Efficacy of Lactobacillus preparation Bioloactis powder in children with rotavirus enteritis. Japan J Pediatr 1994;47:2755–2762. [Google Scholar]
- 230.Szymanski H, Pejcz J, Jawien M, et al. Treatment of acute infectious diarrhoea in infants and children with a mixture of three Lactobacillus rhamnosus strains—a randomized, double-blind, placebo-controlled trial. Aliment Pharmacol Ther 2006;23:247–253. [DOI] [PubMed] [Google Scholar]
- 231.Teran CG, Teran-Escalera CN, Villarroel P. Nitazoxanide vs. probiotics for the treatment of acute rotavirus diarrhea in children: a randomized, single-blind, controlled trial in Bolivian children. Int J Infect Dis 2009;13:518–523. [DOI] [PubMed] [Google Scholar]
- 232.Taborska J, Pazdiora P. Smecta and Lactobacillus acidophilus ND in the treatment of acute diarrhoea in children [Smecta a Lactobacillus acidophilus ND v lécbe akutních detských prujmu]. Ceskoslov Pediatr 1997;52:29–33. [Google Scholar]
- 233.Urganci N, Polat T, Uysalol M, Cetinkaya F. Evaluation of the efficacy of Saccharomyces boulardii in children with acute diarrhoea. Arch Gastroenterohepatol 2001;20:81–83. [Google Scholar]
- 234.Villarruel G, Rubio DM, Lopez F, et al. Saccharomyces boulardii in acute childhood diarrhoea: a randomized, placebo-controlled study. Acta Paediatr 2007;96:538–541. [DOI] [PubMed] [Google Scholar]
- 235.Vivatvakin B, Kowitdamrong E. Randomized control trial of live Lactobacillus acidophilus plus Bifidobacterium infantis in treatment of infantile acute watery diarrhea. J Med Assoc Thai 2006;89(Suppl 3):S126–S133. [PubMed] [Google Scholar]
- 236.Grandy G, Medina M, Soria R, et al. Probiotics in the treatment of acute rotavirus diarrhoea. A randomized, double-blind, controlled trial using two different probiotic preparations in Bolivian children. BMC Infect Dis 2010;10:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Rerksuppaphol S, Rerksuppaphol L. Lactobacillus acidophilus and Bifidobacterium bifidum stored at ambient temperature are effective in the treatment of acute diarrhoea. Ann Trop Paediatr 2010;30:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Correa NB, Penna FJ, Lima FM, et al. Treatment of acute diarrhea with Saccharomyces boulardii in infants. J Pediatr Gastroenterol Nutr 2011;53:497–501. [DOI] [PubMed] [Google Scholar]
- 239.Dalgic N, Sancar M, Bayraktar B, et al. Probiotic, zinc and lactose-free formula in children with rotavirus diarrhea: Are they effective? Pediatr Int 2011;53:677–682. [DOI] [PubMed] [Google Scholar]
- 240.Dutta P, Mitra U, Dutta S, et al. Randomised controlled clinical trial of Lactobacillus sporogenes (Bacillus coagulans), used as probiotic in clinical practice, on acute watery diarrhoea in children. Trop Med Int Health 2011;16:555–561. [DOI] [PubMed] [Google Scholar]
- 241.Abbaskhanian A, Rezai MS, Karami H, et al. The effect of fermented yogurt on rotavirus diarrhea in children. HealthMED 2012;6:1600–1604. [Google Scholar]
- 242.Erdogan O, Tanyeri B, Torun E, et al. The comparition of the efficacy of two different probiotics in rotavirus gastroenteritis in children. J Trop Med 2012;2012:787240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Francavilla R, Lionetti E, Castellaneta S, et al. Randomised clinical trial: Lactobacillus reuteri DSM 17938 vs. placebo in children with acute diarrhoea—a double-blind study. Aliment Pharmacol Ther 2012;36:363–369. [DOI] [PubMed] [Google Scholar]
- 244.Khan A, Javed T, Chishti AL. Clinical efficacy of use of probiotic “Saccharomyces boulardii” In children with acute watery diarrhea. Pak Paediatr J 2012;36:122–127. [Google Scholar]
- 245.Nixon AF, Cunningham SJ, Cohen HW, et al. The effect of Lactobacillus GG on acute diarrheal illness in the pediatric emergency department. Pediatr Emerg Care 2012;28:1048–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Riaz M, Alam S, Malik A, et al. Efficacy and safety of saccharomyces boulardii in acute childhood diarrhea: a double blind randomised controlled trial. Indian J Pediatr 2012;79:478–482. [DOI] [PubMed] [Google Scholar]
- 247.Phavichitr N, Puwdee P, Tantibhaedhyangkul R. Cost-benefit analysis of the probiotic treatment of children hospitalized for acute diarrhea in Bangkok, Thailand. Southeast Asian J Trop Med Public Health 2013;44:1065–1071. [PubMed] [Google Scholar]
- 248.Aggarwal S, Upadhyay A, Shah D, et al. Lactobacillus GG for treatment of acute childhood diarrhoea: an open labelled, randomized controlled trial. Indian J Med Res 2014;139:379–385. [PMC free article] [PubMed] [Google Scholar]
- 249.Dinleyici EC, Vandenplas Y. Lactobacillus reuteri DSM 17938 effectively reduces the duration of acute diarrhoea in hospitalised children. Acta Paediatr 2014;103:e300–e305. [DOI] [PubMed] [Google Scholar]
- 250.Huang YF, Liu PY, Chen YY, et al. Three-combination probiotics therapy in children with salmonella and rotavirus gastroenteritis. J Clin Gastroenterol 2014;48:37–42. [DOI] [PubMed] [Google Scholar]
- 251.Sindhu KNC, Sowmyanarayanan TV, Paul A, et al. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2014;58:1107–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Dinleyici EC, Dalgic N, Guven S, et al. Lactobacillus reuteri DSM 17938 shortens acute infectious diarrhea in a pediatric outpatient setting. J Pediatr 2015;91:392–96. [DOI] [PubMed] [Google Scholar]
- 253.Dinleyici EC, Kara A, Dalgic N, et al. Saccharomyces boulardii CNCM I-745 reduces the duration of diarrhoea, length of emergency care and hospital stay in children with acute diarrhoea. Benefic Microbes 2015;6:415–421. [DOI] [PubMed] [Google Scholar]
- 254.El-Soud NHA, Said RN, Mosallam DS, et al. Bifidobacterium lactis in treatment of children with acute diarrhea. A randomized double blind controlled trial. Maced J Med Sci 2015;3:403–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Freedman SB, Sherman PM, Willan A, et al. Emergency department treatment of children with diarrhea who attend day care: a randomized multidose trial of a Lactobacillus helveticus and Lactobacillus rhamnosus combination probiotic. Clin Pediatr 2015;54:1158–1166. [DOI] [PubMed] [Google Scholar]
- 256.Hegar B, Waspada IMI, Gunardi H, et al. A double blind randomized trial showing probiotics to be ineffective in acute diarrhea in Indonesian children. Indian J Pediatr 2015;82:410–414. [DOI] [PubMed] [Google Scholar]
- 257.Lee DK, Park JE, Kim MJ, et al. Probiotic bacteria, B. longum and L. acidophilus inhibit infection by rotavirus in vitro and decrease the duration of diarrhea in pediatric patients. Clin Res Hepatol Gastroenterol 2015;39:237–244. [DOI] [PubMed] [Google Scholar]
- 258.Das S, Gupta PK, Das RR. Efficacy and safety of Saccharomyces boulardii in acute rotavirus diarrhea: double blind randomized controlled trial from a developing country. J Trop Pediatr 2016;62:464–470. [DOI] [PubMed] [Google Scholar]
- 259.Dash DK, Dash M, Mohanty MD, et al. Efficacy of probiotic Saccharomyces boulardii as an adjuvant therapy in acute childhood diarrhoea. J Nepal Paediatr Soc 2016;36:250–255. [Google Scholar]
- 260.Sharif MR, Kashani HH, Ardakani AT, et al. The effect of a yeast probiotic on acute diarrhea in children. Probiotics Antimicrob Proteins 2016;8:211–214. [DOI] [PubMed] [Google Scholar]
- 261.Burki MFK, Jabeen F. Efficacy of Saccharomyces boullardii in children with acute diarrhea. Med Forum Monthly 2017;28:112–116. [Google Scholar]
- 262.Khan MA, Khattak MB, Munir A, et al. Efficacy of Lactobacillus reuteri in acute watery diarrhea. Med Forum Monthly 2017;28:7–11. [Google Scholar]
- 263.Park M, Kwon B, Ku S, Ji G. The efficacy of Bifidobacterium longum BORI and Lactobacillus acidophilus AD031 probiotic treatment in infants with rotavirus infection. Nutrients 2017;9(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Chau TTH, Chau NNM, Le NTH, et al. A double-blind, randomized, placebo-controlled trial of Lactobacillus acidophilus for the treatment of acute watery diarrhea in Vietnamese children. Pediatr Infect Dis J 2018;37:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Schnadower D, Tarr PI, Casper TC, et al. Lactobacillus rhamnosus GG versus placebo for acute gastroenteritis in children. N Engl J Med 2018;379:2002–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Freedman SB, Williamson-Urquhart S, Farion KJ, et al. Multicenter trial of a combination probiotic for children with gastroenteritis. N Engl J Med 2018;379:2015–2026. [DOI] [PubMed] [Google Scholar]
- 267.Florez ID, Veroniki AA, Al Khalifah R, et al. Comparative effectiveness and safety of interventions for acute diarrhea and gastroenteritis in children: a systematic review and network meta-analysis. PLoS One 2018;13:e0207701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Szajewska H, Ruszczynski M, Kolacek S. Meta-analysis shows limited evidence for using Lactobacillus acidophilus LB to treat acute gastroenteritis in children. Acta Paediatr 2014;103:249–255. [DOI] [PubMed] [Google Scholar]
- 269.Szajewska H, Urbanska M, Chmielewska A, et al. Meta-analysis: Lactobacillus reuteri strain DSM 17938 (and the original strain ATCC 55730) for treating acute gastroenteritis in children. Benef Microbes 2014;5:285–293. [DOI] [PubMed] [Google Scholar]
- 270.Szajewska H, Skorka A. Saccharomyces boulardii for treating acute gastroenteritis in children: updated meta-analysis of randomized controlled trials. Aliment Pharmacol Ther 2009;30:960–961. [DOI] [PubMed] [Google Scholar]
- 271.Purisch SE, Gyamfi-Bannerman C. Epidemiology of preterm birth. Semin Perinatol 2017;41:387–391. [DOI] [PubMed] [Google Scholar]
- 272.Frost BL, Modi BP, Jaksic T, et al. New medical and surgical insights into neonatal necrotizing enterocolitis: a review. JAMA Pediatr 2017;171:83–88. [DOI] [PubMed] [Google Scholar]
- 273.Morgan RL, Preidis GA, Kashyap PC, et al. Probiotics reduce mortality and morbidity in preterm, low-birth-weight infants: a systematic review and network meta-analysis of randomized trials. Gastroenterology 2020;159:467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Zhou N. The observation of effect of probiotics in the prevention of neonatal necrotizing enterocolitis. Chin J Ethnomed Ethnopharm 2012;21:81. [Google Scholar]
- 275.Yang S, Haiying Y, Bin G, et al. The clinical application value of endangered preterm infants given earlier amounts of micro feedings and adding probiotics. J Pediatr Pharm 2011;3. [Google Scholar]
- 276.Xu L, Wang Y, Fu J, et al. A double-blinded randomized trial on growth and feeding tolerance with Saccharomyces boulardii CNCM I-745 in formula-fed preterm infants. J Pediatr 2016;92:296–301. [DOI] [PubMed] [Google Scholar]
- 277.Xiao-yuan Z, Lian-qiao LI, Xuan-xuan GAO, et al. Relative factors of neonatal necrotizing enterocolitis and preventive effect of microeco-preparation. J Appl Clin Pediatr 2007;18. [Google Scholar]
- 278.Wejryd E, Marchini G, Frimmel V, et al. Probiotics promoted head growth in extremely low birthweight infants in a double-blind placebo-controlled trial. Acta Paediatr 2019;108:62–69. [DOI] [PubMed] [Google Scholar]
- 279.Van Niekerk E, Nel DG, Blaauw R, et al. Probiotics reduce necrotizing enterocolitis severity in HIV-exposed premature infants. J Trop Pediatr 2015;61:155–164. [DOI] [PubMed] [Google Scholar]
- 280.Van Niekerk E, Kirsten GF, Nel DG, et al. Probiotics, feeding tolerance, and growth: a comparison between HIV-exposed and unexposed very low birth weight infants. Nutrition 2014;30:645–653. [DOI] [PubMed] [Google Scholar]
- 281.Totsu S, Yamasaki C, Terahara M, et al. Bifidobacterium and enteral feeding in preterm infants: cluster-randomized trial. Pediatr Int 2014;56:714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Tewari VV, Dubey SK, Gupta G. Bacillus clausii for prevention of late-onset sepsis in preterm infants: a randomized controlled trial. J Trop Pediatr 2015;61:377–384. [DOI] [PubMed] [Google Scholar]
- 283.Stratiki Z, Costalos C, Sevastiadou S, et al. The effect of a bifidobacter supplemented bovine milk on intestinal permeability of preterm infants. Early Human Dev 2007;83:575–579. [DOI] [PubMed] [Google Scholar]
- 284.Sinha A, Gupta SS, Chellani H, et al. Role of probiotics VSL#3 in prevention of suspected sepsis in low birth-weight infants in India: a randomised controlled trial. BMJ Open 2015;5(7):e006564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Shashidhar A, Suman Rao PN, Nesargi S, et al. Probiotics for promoting feed tolerance in very low birth weight neonates—a randomized controlled trial. Indian Pediatr 2017;54:363–367. [DOI] [PubMed] [Google Scholar]
- 286.Shadkam MN, Jalalizadeh F, Nasiriani K. Effects of probiotic Lactobacillus reuteri (DSM 17938) on the incidence of necrotizing enterocolitis in very low birth weight premature infants. Iran J Neonatol 2015;6:15–20. [Google Scholar]
- 287.Serce O, Benzer D, Gursoy T, et al. Efficacy of saccharomyces boulardii on necrotizing enterocolitis or sepsis in very low birth weight infants: a randomised controlled trial. Early Human Dev 2013;89:1033–1036. [DOI] [PubMed] [Google Scholar]
- 288.Sari FN, Dizdar EA, Oguz S, et al. Oral probiotics: Lactobacillus sporogenes for prevention of necrotizing enterocolitis in very low-birth weight infants: a randomized, controlled trial. Eur J Clin Nutr 2011;65:434–439. [DOI] [PubMed] [Google Scholar]
- 289.Samanta M, Sarkar M, Ghosh P, et al. Prophylactic probiotics for prevention of necrotizing enterocolitis in very low birth weight newborns. J Trop Pediatr 2009;55:128–131. [DOI] [PubMed] [Google Scholar]
- 290.Saengtawesin V, Tangpolkaiwalsak R, Kanjanapattankul W. Effect of oral probiotics supplementation in the prevention of necrotizing enterocolitis among very low birth weight preterm infants. J Med Assoc Thai 2014;97:S20–S25. [PubMed] [Google Scholar]
- 291.Sadowska-Krawczenko I, Korbal P, Polak A, et al. Lactobacillus rhamnosus ATC A07FA for preventing necrotizing enterocolitis in very-low-birth-weight preterm infants: a randomized controlled trial (preliminary results). Pediatr Pol 2012;87:139–145. [Google Scholar]
- 292.Roy A, Chaudhuri J, Sarkar D, et al. Role of enteric supplementation of probiotics on late-onset sepsis by candida species in preterm low birth weight neonates: a randomized, double blind, placebo-controlled trial. N Am J Med Sci 2014;6:50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Rouge C, Piloquet H, Butel MJ, et al. Oral supplementation with probiotics in very-low-birth-weight preterm infants: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 2009;89:1828–1835. [DOI] [PubMed] [Google Scholar]
- 294.Romeo MG, Romeo DM, Trovato L, et al. Role of probiotics in the prevention of the enteric colonization by Candida in preterm newborns: incidence of late-onset sepsis and neurological outcome. J Perinatol 2011;31:63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Rojas MA, Lozano JM, Rojas MX, et al. Prophylactic probiotics to prevent death and nosocomial infection in preterm infants. Pediatrics 2012;130:e1113–e1120. [DOI] [PubMed] [Google Scholar]
- 296.Reuman PD, Duckworth DH, Smith KL, et al. Lack of effect of Lactobacillus on gastrointestinal bacterial colonization in premature infants. Pediatr Infect Dis 1986;5:663–668. [DOI] [PubMed] [Google Scholar]
- 297.Ren B. Preventive effect of Bifidobacterium tetravaccine tablets in premature infants with necrotizing enterocolitis. J Pediatr Pharm 2010;16:24–25. [Google Scholar]
- 298.Qiao LX, Zhu WY, Zhang HY, et al. Effect of early administration of probiotics on gut microflora and feeding in pre-term infants: a randomized controlled trial. J Matern Fetal Neonatal Med 2017;30:13–16. [DOI] [PubMed] [Google Scholar]
- 299.Punnahitananda S, Thaithumyanon P, Soongsawang K. Nosocomial infection and necrotizing enterocolitis in preterm neonates treated with Lactobacillus acidophilus and Bifidobacterium infantis in a neonatal intensive care unit: a randomized controlled study. Paper presented at: 14th Congress of the Federation of Asia Oceania Perinatal Societies; October 1–5, 2006; Bangkok, Thailand. [Google Scholar]
- 300.Patole S, Keil AD, Chang A, et al. Effect of Bifidobacterium breve M-16V supplementation on fecal bifidobacteria in preterm neonates—a randomised double blind placebo controlled trial. PLoS One 2014;9: e89511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Oncel MY, Sari FN, Arayici S, et al. Lactobacillus reuteri for the prevention of necrotising enterocolitis in very low birthweight infants: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 2014;99:F110–F115. [DOI] [PubMed] [Google Scholar]
- 302.Mohan R, Koebnick C, Schildt J, et al. Effects of Bifidobacterium lactis Bb12 supplementation on body weight, fecal pH, acetate, lactate, calprotectin, and IgA in preterm infants. Pediatr Res 2008;64:418–422. [DOI] [PubMed] [Google Scholar]
- 303.Millar MR, Bacon C, Smith SL, et al. Enteral feeding of premature-infants with Lactobacillus GG. Arch Dis Child 1993;69:483–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Mihatsch WA, Vossbeck S, Eikmanns B, et al. Effect of Bifidobacterium lactis on the incidence of nosocomial infections in very-low-birth-weight infants: a randomized controlled trial. Neonatology 2010;98:156–163. [DOI] [PubMed] [Google Scholar]
- 305.Manzoni P, Meyer M, Stolfi I, et al. Bovine lactoferrin supplementation for prevention of necrotizing enterocolitis in very-low-birth-weight neonates: a randomized clinical trial. Early Human Dev 2014;90:S60–S65. [DOI] [PubMed] [Google Scholar]
- 306.Lin HC, Su BH, Chen AC, et al. Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants. Pediatrics 2005;115:1–4. [DOI] [PubMed] [Google Scholar]
- 307.Lin HC, Hsu CH, Chen HL, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight preterm infants: a multicenter, randomized, controlled trial. Pediatrics 2008;122:693–700. [DOI] [PubMed] [Google Scholar]
- 308.Kitajima H, Sumida Y, Tanaka R, et al. Early administration of Bifidobacterium breve to preterm infants: randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 1997;76:F101–F107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Ke D, Su Z, Li L. Effects of Bifido supplement for prevention of necrotizing enterocolitis in preterm infants: a randomized controlled trial. Chin Pediatr Emerg Med 2008;12:69–71. [Google Scholar]
- 310.Kanic Z, Micetic Turk D, et al. Influence of a combination of probiotics on bacterial infections in very low birth-weight newborns. Wien Klin Wochenschr 2015;127:210–215. [DOI] [PubMed] [Google Scholar]
- 311.Jacobs SE, Tobin JM, Opie GF, et al. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics 2013;132:1055–1062. [DOI] [PubMed] [Google Scholar]
- 312.Indrio F, Riezzo G, Tafuri S, et al. Probiotic supplementation in preterm: feeding intolerance and hospital cost. Nutrients 2017;9:965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Huang B, Yang H, Huang X. Probiotics supplementation for prevention of necrotizing enterocolitis in very low-birth-weight neonates: a randomized, controlled trial. J Guangdong Med Coll 2009;27:37–39. [Google Scholar]
- 314.Hua XT, Tang J, Mu DZ. Effect of oral administration of probiotics on intestinal colonization with drug-resistant bacteria in preterm infants. Chin J Contemp Pediatr 2014;16:606–609. [PubMed] [Google Scholar]
- 315.Hikaru H, Koichi K, Yayoi Y, et al. Bifidobacteria prevents preterm infants from developing infection and sepsis. Int J Probiotics Prebiotics 2010;5:33–36. [Google Scholar]
- 316.Hernández-Enríquez NP, Rosas-Sumano AB, Monzoy-Ventre MA, et al. Lactobacillus reuteri DSM 17938 en la prevención de enterocolitis necrosante en recién nacidos prematuros. Estudio piloto de eficacia y seguridad. Rev Mex Pediatr 2016;83:37–43. [Google Scholar]
- 317.Hays S, Jacquot A, Gauthier H, et al. Probiotics and growth in preterm infants: a randomized controlled trial, PREMAPRO study. Clin Nutr 2016;35:802–811. [DOI] [PubMed] [Google Scholar]
- 318.Hariharan D, Balasubramanian L, Kannappan V, et al. Probiotic supplementation in VLBW preterm infants improves feeding tolerance and reduces risk of gram negative sepsis. J Pediatr Gastroenterol Nutr 2016;62:655. [Google Scholar]
- 319.Fujii T, Ohtsuka Y, Lee T, et al. Bifidobacterium breve enhances transforming growth factor beta1 signaling by regulating Smad7 expression in preterm infants. J Pediatr Gastroenterol Nutr 2006;43:83–88. [DOI] [PubMed] [Google Scholar]
- 320.Fernández-Carrocera LA, Solis-Herrera A, Cabanillas-Ayón M, et al. Double-blind, randomised clinical assay to evaluate the efficacy of probiotics in preterm newborns weighing less than 1500 g in the prevention of necrotising enterocolitis. Arch Dis Child Fetal Neonatal Ed 2013;98:F5–F9. [DOI] [PubMed] [Google Scholar]
- 321.Dutta S, Ray P, Narang A. Comparison of stool colonization in premature infants by three dose regimes of a probiotic combination: a randomized controlled trial. Am J Perinatol 2015;32:733–740. [DOI] [PubMed] [Google Scholar]
- 322.Dongol Singh S, Klobassa D, Resch B, et al. Placebo controlled introduction of prophylactic supplementation of probiotics to decrease the incidence of necrotizing enterocolitis at Dhulikhel Hospital in Nepal. Kathmandu Univ Med J 2017;60:319–323. [PubMed] [Google Scholar]
- 323.Dilli D, Aydin B, Fettah ND, et al. The propre-save study: effects of probiotics and prebiotics alone or combined on necrotizing enterocolitis in very low birth weight infants. J Pediatr 2015;166:545–551. [DOI] [PubMed] [Google Scholar]
- 324.Di M, Li X. Effects of Bifidobacterium supplementation for prevention of necrotizing enterocolitis in preterm infants: a randomized, controlled trial. Zhong Guo She Qu Yi Shi 2010:231. [Google Scholar]
- 325.Deng J, Chen K. Early minimal feeding combined with probiotics to prevent necrotizing enterocolitis in preterm infant. Chin J Modern Drug Appl 2010;4:13–14. [Google Scholar]
- 326.Demirel G, Erdeve O, Celik IH, et al. Saccharomyces boulardii for prevention of necrotizing enterocolitis in preterm infants: a randomized, controlled study. Acta Paediatr 2013;102:e560–e565. [DOI] [PubMed] [Google Scholar]
- 327.Dashti AS, Afjeh SA, Basiry A, et al. Prophylactic probiotics for prevention of necrotizing enterocolitis (NEC) in low birth weight neonates. Arch Pediatr Infect Dis 2014;2:174–179. [Google Scholar]
- 328.Dani C, Biadaioli R, Bertini G, et al. Probiotics feeding in prevention of urinary tract infection, bacterial sepsis and necrotizing enterocolitis in preterm infants. A prospective double-blind study. Biol Neonate 2002;82:103–108. [DOI] [PubMed] [Google Scholar]
- 329.Costeloe K, Hardy P, Juszczak E, et al. Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet 2016;387:649–660. [DOI] [PubMed] [Google Scholar]
- 330.Costalos C, Skouteri V, Gounaris A, et al. Enteral feeding of premature infants with Saccharomyces boulardii. Early Human Dev 2003;74:89–96. [DOI] [PubMed] [Google Scholar]
- 331.Chrzanowska-Liszewska D, Seliga-Siwecka J, Kornacka MK. The effect of Lactobacillus rhamnosus GG supplemented enteral feeding on the microbiotic flora of preterm infants-double blinded randomized control trial. Early Human Dev 2012;88:57–60. [DOI] [PubMed] [Google Scholar]
- 332.Chowdhury T, Ali MM, Hossain MM, et al. Efficacy of probiotics versus placebo in the prevention of necrotizing enterocolitis in preterm very low birth weight infants: a double-blind randomized controlled trial. J Coll Physicians Surg Pak 2016;26:770–774. [PubMed] [Google Scholar]
- 333.Braga TD, Da Silva GAP, De Lira PIC, et al. Efficacy of Bifidobacterium breve and Lactobacillus casei oral supplementation on necrotizing enterocolitis in very-low-birth-weight preterm infants: a double-blind, randomized, controlled trial. Am J Clin Nutr 2011;93:81–86. [DOI] [PubMed] [Google Scholar]
- 334.Bin-Nun A, Bromiker R, Wilschanski M, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr 2005;147:192–196. [DOI] [PubMed] [Google Scholar]
- 335.Arora S, Khurana MS, Saini R. To study the role of probiotics in the prevention of necrotizing enterocolitis in preterm neonates. Int J Contemp Pediatr 2017;4:1792–1797. [Google Scholar]
- 336.Al-Hosni M, Duenas M, Hawk M, et al. Probiotics-supplemented feeding in extremely low-birth-weight infants. J Perinatol 2012;32:253–259. [DOI] [PubMed] [Google Scholar]
- 337.Vallabhaneni S, Walker TA, Lockhart SR, et al. Notes from the field: fatal gastrointestinal mucormycosis in a premature infant associated with a contaminated dietary supplement—Connecticut, 2014. MMWR Morb Mortal Wkly Rep 2015;64:155–156. [PMC free article] [PubMed] [Google Scholar]
- 338.Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev 2019;7(7):CD002971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systemic Reviews and Meta-Analysis: The PRISMA Statement. PLoS Med 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


