Abstract
The rapid increase of fatal opioid overdoses over the past two decades is a major U.S. public health problem, especially in non-metropolitan communities. The crisis has transitioned from pharmaceuticals to illicit synthetic opioids and street mixtures, especially in urban areas. Using latent profile analysis, we classify n = 3,079 counties into distinct classes using CDC fatal overdose rates for specific opioids in 2002–2004, 2008–2012, and 2014–2016. We identify three distinct epidemics (prescription opioids, heroin, and prescription-synthetic opioid mixtures) and one syndemic involving all opioids. We find that prescription-related epidemic counties, whether rural or urban, have been “left behind” the rest of the nation. These communities are less populated and more remote, older and mostly white, have a history of drug abuse, and are former farm and factory communities that have been in decline since the 1990s. Overdoses in these places exemplify the “deaths of despair” narrative. By contrast, heroin and opioid syndemic counties tend to be more urban, connected to interstates, ethnically diverse, and in general more economically secure. The urban opioid crisis follows the path of previous drug epidemics, affecting a disadvantaged subpopulation that has been left behind rather than the entire community. County data on opioid epidemic class membership are provided.
Introduction
Over the last two decades, fatal opioid overdoses have increased dramatically to become a major public health crisis in the United States (Jalal et al. 2018). Two-thirds of all overdose deaths involve opioids, killing roughly 47,600 people in 2017 and close to 360,000 since 1999 (CDC 2019). Unlike previous drug epidemics that have proliferated in inner cities, the opioid crisis has affected smaller communities. Fatal overdoses from opioids have increased by over 700 percent in both micropolitan and rural (non-core) counties, and by nearly 400 percent in metropolitan ones (CDC 2017). However, metro deaths have risen rapidly since 2014 due to fentanyl overdoses, and will soon eclipse non-metro opioid fatalities (CDC 2018). The opioid epidemic has placed heavy burdens on hospitals and emergency rooms (Weiss et al. 2016), local police and courts (Lurie 2017), social services agencies (Whalen 2016), and even the national economy with an economic impact estimated at 2.8 percent of GDP (Council of Economic Advisers 2017). The opioid crisis has also rapidly evolved from a prescription problem to one involving a myriad of opioid substances (CDC 2018; Ciccarone 2019; Scholl et al. 2019). In this sense, the crisis is like the multiple-headed Hydra of ancient Greek mythology, involving heroin, prescription, and synthetic opioids. As communities sever one head of the opioid problem, a new drug appears to take its place. For example, regulation of prescription opioids in many states has not slowed the crisis, as heroin and synthetic opioids from abroad have rapidly filled the void (DEA 2018; Monnat 2018).
Although the opioid crisis is covered extensively in the media and popular press, rigorous academic research on its social, structural, and spatial determinants is still emerging (Dasgupta, Beletsky, and Ciccarone 2018; Monnat and Rigg 2016; Spencer et al. 2018). There are several unanswered questions limiting our understanding of this public health and social problem, hence limiting community and policy responses. Is there a single opioid overdose epidemic or a series of multiple epidemics? Are opioid epidemics linked to drug risk factors like persistent drug overdoses, over-prescribing, and work disability; or driven by socioeconomic disorganization from job losses, poverty, and general community decline? Are there differences across rural and urban contexts? To address these questions, our exploratory analysis has three objectives. First, we document trends in drug overdose mortality by opioid type across the rural-urban continuum. Second, we identify distinct opioid overdose mortality epidemics (termed classes) at the county-level over time using latent profile analysis (LPA). Third, we describe the demographic, drug risk, social disorganization, and economic characteristics of communities affected by different opioid overdose epidemics.
Our analysis contributes to the rural health and community development literatures by speaking to place-based drug problems, their distribution, and dynamics. The public health burden may fall more heavily on smaller communities as they have limited health, social, and criminal justice resources to respond to drug crises (Rigg, Monnat, and Chavez 2018). Moreover, rural communities are not monolithic, having diverse socioeconomic and drug risk conditions (Monnat 2019). Evidence shows that drug addiction epidemics undermine the social and economic vitality of a community, the same vitality that is key to preventing drug epidemics, leading the community into a downward spiral (Rigg and Monnat 2015; Weisburd et al. 2016). This has led many state and local officials to see opioid abuse as the most pressing problem in rural America (Haegerich et al. 2014; Haffajee, Anupam, and Weiner 2015; NGA2016).
Previous Research and Conceptual Approach
Geography of the U.S. Opioid Overdose Crisis
The geography of the U.S. opioid overdose crisis has evolved dramatically over the past several decades, being higher in rural places in the 2000s before urban rates caught up in the mid-2010s due to synthetic opioid overdoses (Spencer et al. 2018). Rural opioid overdose mortality exhibits high spatial heterogeneity, as shown in Figure 1. Large swathes of the upper Midwest and Great Plains have some of the lowest rates of fatal overdoses. At the same time, Appalachia and parts of the Ohio River valley post some of the highest fatality rates in the nation, and have for some time (Jalal et al. 2018; Keyes et al. 2014; Ruhm 2017). Even rural places with a minor drug problem a decade ago are now experiencing high opioid overdose fatalities, in particular states in the Southwest, Eastern Great Lakes, and New England.
Figure 1.
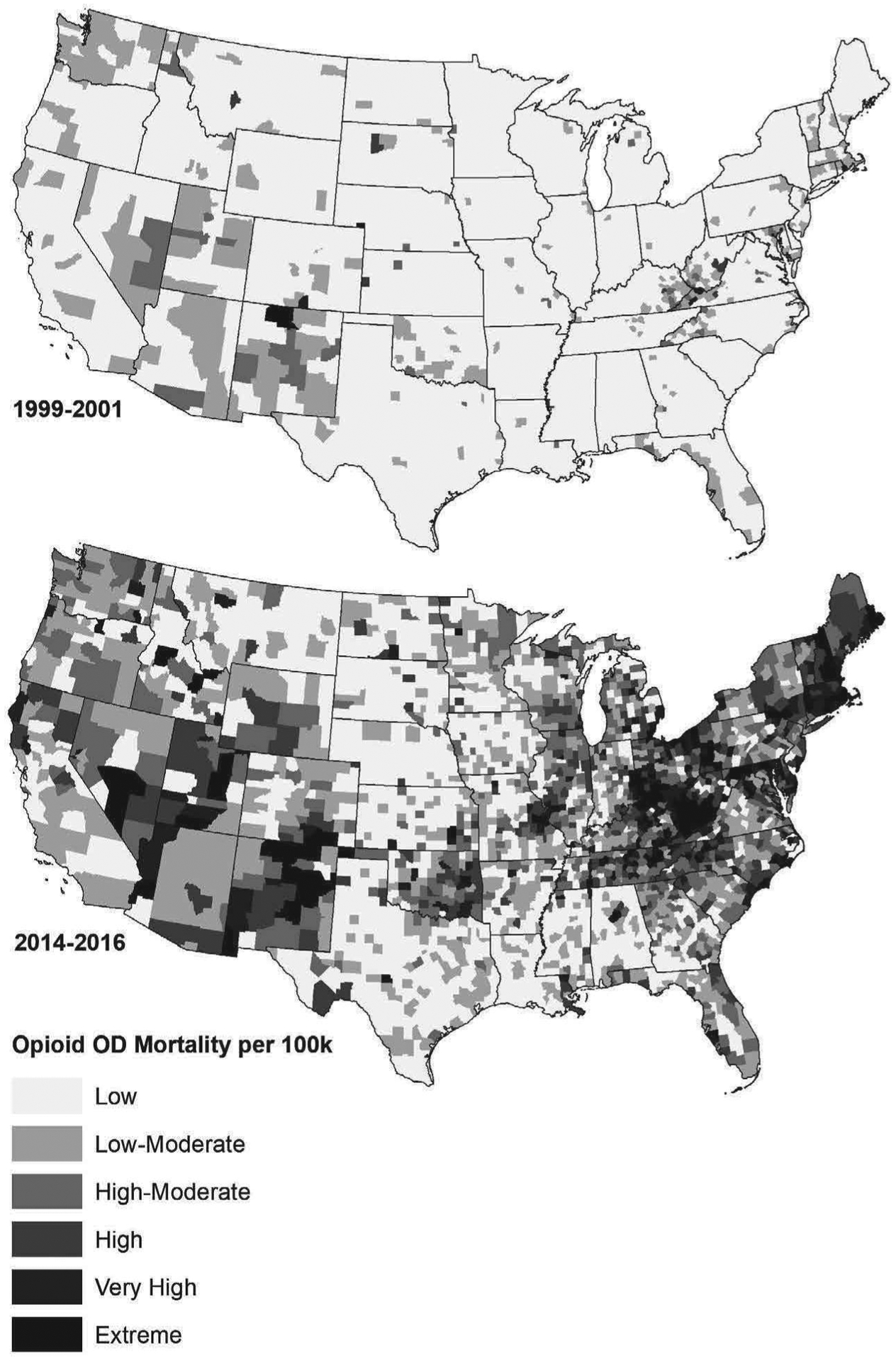
Opioid Overdose Mortality Rates per 100,000 (Age-Adjusted) in 1999–2001 (Top Panel) and 2014–2016 (Bottom Panel) for n = 3,079 Counties in the Conterminous U.S. Rates Not Reported Due to Confidentiality Restrictions.
Recent literature on the opioid overdose epidemic points to both compositional and contextual features of communities that are associated with spatial variation in fatal drug overdose rates. Compositional risk factors contributing to higher overdose rates include high rates of poverty, unemployment, disability, single parent families, divorce, and lower educational attainment (Monnat et al. 2019; Paulozzi and Annest 2007; Ruhm 2019). This work also finds that certain vulnerable demographic groups tend to have higher overdose rates, such as the elderly, military veterans, and Native Americans (Monnat 2018). Extant research identifies several contextual factors that influence drug use risk, including social norms, neighborhood disadvantage, social capital, the physical environment, availability of health and social resources, and policy and regulation (Dasgupta et al. 2018; Galea, Ahem, and Vlahov 2003). Monnat (2019) finds that higher rates of opioid prescribing, fentanyl exposure, economic distress, reliance on mining and service sector employment, and persistent population loss are associated with higher fatal drug overdose rates among non-Hispanic whites.
There appear to be strong linkages between macroeconomic conditions and fatal drug overdose rates. Case and Deaton (2017) suggest that the rise in fatal drug overdose rates over the past two decades is largely attributable to long-term changes, including progressively worsening labor market opportunities for individuals without a four-year college degree, marital disintegration and single-parenting, and reduced attachment to religious and other social capital promoting institutions. A large body of evidence shows that job loss and wage decline increase risk of depression and substance abuse (Galea et al. 2003; Kaplan et al. 2015; Kerr et al. 2017; Krueger 2017; Pierce and Schott 2017). For example, one study estimates that a one-percentage point increase in unemployment rates raises opioid mortality rates by 3.6 percent (Hollingsworth, Ruhm, and Simon 2017). However, recent work questions the role of macroeconomic conditions on rising drug overdose rates. Ruhm (2019) finds that unemployment rates since the early 2000s are only minimally associated with increase in drug overdose mortality rates at the county level.
An emerging body of research has begun to examine the relationship between drug mortality and employment in specific economic sectors. Betz and Jones (2018) find that both job and wage declines in lower skilled industries are associated with higher opioid overdose mortality rates, especially for rural white men in goods-producing sectors, but also for African Americans and women who work in the service sector. They also find that wage growth is an important protective factor, which suggests job quality (e.g. higher wages) matters as much as job quantity. The twin forces of industrial decline and farm concentration have eliminated many middle-skill and middle-wage jobs and replaced them with low-skill and low-wage ones in leisure and personal services, especially in non-metropolitan areas, resulting in growing poverty and inequality (David and Dorn 2013; Lobao and Stofferahn 2008; Moller, Alderson, and Nielson 2009; Peters 2009). Economic restructuring has not been uniform across the United States, leading to poverty in some places and prosperity in others (Peters 2013). For example, shocks to manufacturing labor demand have disproportionately negative impacts on male employment and wages, leading to a disproportionate increase in male mortality from drug and alcohol poisoning (Autor, Dorn, and Hanson 2018).
Social Disorganization
Economic decline alone is insufficient to account for the rise in opioid and other drug problems. Criminologists view social disorganization as a key linkage between community economic disadvantage and local crime-related and deviance outcomes. Disorganization theory is an umbrella term for a number of related conceptual models linking social order to crime, with the three most common outlined below (Bruinsma et al. 2013). The classical model of social disorganization, grounded in Chicago school sociology, links crime and social problems in a community to lower socioeconomic status, high residential mobility, and ethnic heterogeneity, and has been expanded to include population density, urbanization, and family disruption (Bursik and Webb 1982). In short, disadvantaged communities have more structural barriers that limit prosocial behavior of residents. The social capital model of disorganization incorporates concepts of social trust, social networks, and organizational participation into the expanded classical model (Sampson and Groves 1989). These elements are thought to create shared norms and values in the community, which in turn reduces crime and social problems. A later iteration of social disorganization theory, the collective efficacy model, builds on the social capital model to include informal social control and shared community understandings (Sampson, Raudenbush, and Earls 1997). The model links how residents work together to keep and maintain order; and how accompanying ties formed by community investment enable the co-production of public safety by police and the community (Bursik and Grasmick 1993; Weisburd, Feucht, and Bruinsma 2009). Specifically, communities affected by acute economic distress tend to turn inward, causing local social networks to atrophy which leads to weakened informal control (Berg and Rengifo 2009; Hochstetler, DeLisi, and Peters 2016).
Decades of research in criminology supports the various models of disorganization theory (Sampson et al. 1997; Wikström and Sampson 2006; Wilson and Kelling 1982). This body of work finds increased crime to be positively associated with greater poverty and inequality, residential mobility, and ethnic heterogeneity. Together, these structural factors undermine informal social controls among residents, weaken trust in the criminal justice system, and give rise to disruptive community norms, all of which are associated with higher rates of crime and deviance (Hochstetler, Peters, and Copes 2017; Weisburd et al. 2016). Evidence indicates that drug markets, as indicated by accidental overdose deaths, are spatially linked to disorganization in large cities (Martinez, Rosenfeld, and Marez 2008). Further, self-reported community disorganization helps predict substance use and dependence (Berg and Lauritsen 2016; McLean 2016). However, relatively little is known about the effects of disorganization on drug-related outcomes in rural areas (Weisburd et al. 2016; Wikström and Sampson 2006).
Data and Methods
Units of analysis are n = 3,079 counties in the 48 conterminous U.S. based on 2000 Census geographies, with modifications to prevent breaks in the spatial time-series.1 Opioid overdose mortality is defined as fatal drug overdoses involving opioids plus deaths from opioid-related mental and behavioral disorders. We disaggregate four opioid mortality measures: heroin or opium overdoses; prescription opioid overdoses including methadone; overdoses from synthetic opioids or unknown narcotics; and multiple-cause deaths that include two or more opioid drugs or opioid-related behavioral disorders.2 Data are obtained from confidential cause-of-death mortality files from the National Vital Statistics System maintained by the U.S. Centers for Disease Control and Prevention (CDC 2017). Opioid mortality rates per 100,000 population (based on 2000 Census) are by residence of the decedent and are pooled over three-year periods between 1999 and 2016 to reduce annual fluctuations in small counties, as is standard in public health research (Rothman, Lash, and Greenland 2008). One limitation is a recognized opioid overdose undercount on death certificate data, where synthetic opioid analogs go undetected in toxicology reports (Ruhm 2018). Since there is no agreed upon method to correct this problem, our measures represent a lower-bound estimate of opioid mortality.
For our second objective, LPA is used to identify opioid overdose epidemics by classifying counties into classes based on mortality rates per 100,000 across four opioid types (heroin, prescription, synthetic, and multiple opioids) in three time periods (2002–2004, 2008–2010, and 2014–2016). Mortality rates are normalized using z-scores to facilitate comparisons across opioid types. Like all classification techniques, LPA is sensitive to extreme score, so data are Winsorized at the 0.5 and 99.5 percentiles that roughly correspond to ±2.6 standard deviations. LPA is part of a broader technique called finite mixture models. The procedure assumes observed data from a multivariate mixture collected from a number of mutually exclusive profiles, each with its own distribution (Lanza, Tan, and Bray 2013). We refer to the profiles as classes as this term is more common across disciplines. LPA offers some advantages over more common classification techniques like hierarchical cluster analysis (Morgan 2015).3 The estimated LPA density function is presented in Equation (1), where xi, are the 12 opioid mortality variables for county i, λk are the mixture weights for each variable in class k, and θk are the mean vectors and covariance matrices for each class or θk = (μk, Σk) (Collier and Leite 2017). The LPA is identified by having positive degrees of freedom, an information matrix that is positive definite, and uncorrelated indicators (Abar and Loken 2012; McLachlEin and Peel 2000).
| (1) |
Our third objective is to describe the demographic, drug risk, social disorganization, and economic characteristics of counties affected by different opioid overdose epidemics, and compare these across metropolitan and non-metropolitan contexts. A multivariate general linear model (traditionally MANOVA) is used to explore unconditional mean differences across a number of Variables using the Games-Howell test, which is robust to unequal group sizes and Variances (Johnson and Wichern 2007). Current indicators and change from 2000 are primarily obtained from the U.S. Census Bureau’s American Community Survey (2012–2016 ACS) and previous decennial Census periods, unless otherwise noted.4 We use 2003 Core-Based Statistical Area (CBSA) definitions for metropolitan and non-metropolitan. We use the terms non-metropolitan, non-metro, and rural interchangeably.
Demographics include population density, shares of those 25 and younger and 65 and older, minority population shares (Hispanic of any race, African American, and other/multiple races), and residence in another county five years previous. A number of locational factors are also explored. Natural amenities have been found to either help or hinder economic development (Pender et al. 2014), which may indirectly affect opioid overdose fatalities as documented in the literature (Betz and Jones 2018). Using data from USDA’s Economic Research Service, amenities include topographic variation and water area (z-scores). Density of interstate road lengths per square mile is calculated using ESRI files to model transportation access and drug trafficking corridors (DEA 2017). Drug risk factors are selected based on extant research (Monnat 2019; Rigg et al. 2018). Adjacent opioid overdose mortality captures spillover across neighboring counties, using queen contiguity spatial lags. Fatal non-opioid drug overdoses measure not only general drug abuse in the county, but also underreporting of unidentified opioid overdoses on death certificates. Prescription opioid dispensing rates per 100 people are used to measure supply, taken from QuintilesIMS Transactional Data Warehouse with modifications.5 Work-disabled individuals as a percent of the population are from the Social Security Administration’s OASDI program.
We use the social capital model of social disorganization to identify economic, community, and crime correlates (Bruinsma et al. 2013; Wikström and Sampson 2006). From the U.S. Census, we include the person poverty rate, the 80:20 income gap to measure inequality (quotient of income shares owned by the top and bottom 20th percentiles), and the percentage of housing units that are vacant to measure physical disorganization. Although single-headed families are found to be a significant predictor of drug overdoses in previous studies, we drop it from consideration due to its high correlation with poverty. Property crime rates per 100,000 people in the jurisdiction come from the Federal Bureau of Investigation’s Uniform Crime Reports, with modifications.6 Crime is typically an outcome in disorganization research, but we view property crime (includes burglary, larceny, vehicle theft, and arson) as an indicator of community disorder contributing to drug use and mortality. Social capital measuring organizational capacity includes the number of civic, work, and non-profit groups per 10,000. Social capital measuring engagement and participation includes voting and Census response rates. Items for both measures are converted to z-scores and summed, using 2014 data from the Northeast Regional Center for Rural Development.
Lastly, employment and economic restructuring is measured using current employment shares from the 2012–2016 ACS and change from the 1990 Census. We include change over two decades to capture long-term consequences of economic restructuring on opioid overdose mortality. Census employment is defined as employed persons (16 years and older) by place of residence in two-digit NAICS industry codes. Some service sectors are aggregated for comparability to 1990 data (Peters 2012). Our use of place-of-residence person employment is unique from existing studies that use place-of-work job counts. The former is preferable since it is consistent with CDC mortality data that are also reported by residence. Blue-collar employment sectors, with NAICS codes in parentheses, include: agriculture, forestry, and fishing (11); mining (21); construction (23); manufacturing (31–33); and transportation and warehousing (48–49). Lower skilled jobs characteristic of the post-industrial economy is measured by retail trade and leisure services (44–45, 71–72, 81). Healthcare and social assistance (62) employment is used to control the presence of these services in the county.
Results
Trends in Opioid Overdose Mortality
Our first objective describes the opioid overdose crisis and how it has changed across the rural-urban continuum, which is summarized by four charts in Figure 2. Deaths from prescription opioid overdoses rose sharply during the 2000s, rising from around one death per 100,000 in 1999 to a peak of four to seven deaths by 2010–2011. One reason for their widespread overdose is that prescription opioids have a legal distribution network in nearly every community, namely clinics of health professionals and retail pharmacies. Quinones (2015) was among the first to describe a tripartite system of aggressive yet false marketing of so-called non-addictive opioids by pharmaceutical firms; overprescribing by either unknowing or unethical physicians; and lax oversight by government officials, especially state Medicaid and professional licensing. In recent years, prescription deaths have fallen or remained stable, likely due to more strict prescribing rules and greater availability of cheaper illicit opioids like heroin (DEA 2017, 2018). However, prescription drugs still account for most opioid deaths, except in the largest cities. The prescription overdose crisis hits rural areas hardest, with rates peaking at 7.1 and then falling to the current rate of 4.8 per 100,000. Semi-rural and micropolitan areas follow a similar trend, but with slightly lower base rates. In short, the prescription drug crisis seems to be waning and deaths will most likely continue to fall. CDC terms this the first wave of the opioid overdose crisis (CDC 2019).
Figure 2.
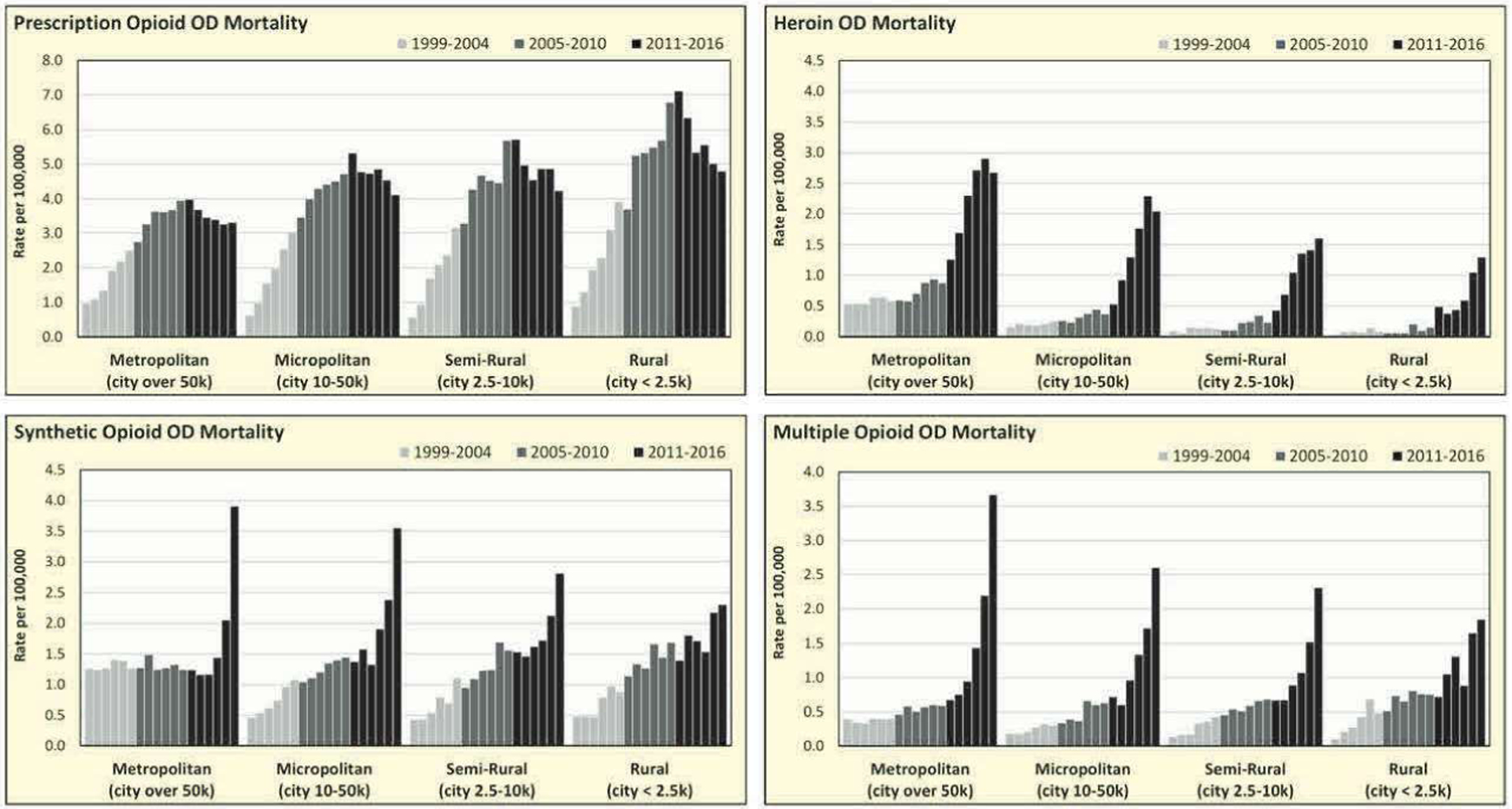
Overdose Mortality by Opioid Type per 100,000 (Age-Adjusted) by Modified Core-Based Statistical Areas (CBSAs) between 1999 and 2016 for n = 3,079 Counties in the Conterminous U.S. Synthetic Opioids Include Unknown Narcotics. Multiple Opioids Include Two or More Drugs or Opioid-Related Behavioral Deaths.
The second wave substituted heroin, white powder in the east and black tar in the west, for prescription opioids. Heroin is considered an illicit drug under federal law because it has no accepted medical use, unlike prescription pain-killers. Heroin overdoses were low and stable until 2011, when deaths began to rise rapidly in more urbanized places. Heroin is an attractive alternative for individuals addicted to prescription opioids because it is cheaper and more readily available, but it is unclear if limited supply due to pharmacy regulation drove heroin usage. Heroin overdose fatalities are a problem in larger metros, but are relatively rare in rural communities. Death rates peaked in 2015–2016 at 3.0 per 100,000 in large metros, with lower peaks in smaller metros and micropolitans (2.0 to 2.3) and rural areas (1.5). Most heroin enter through the southern border, as Mexican drug trafficking organizations (DTOs) now dominate the wholesale distribution of heroin in the U.S. (DEA 2017). However, the heroin wave was soon supplanted, some say exacerbated, by synthetic opioids.
The third wave is often called the synthetic opioid overdose crisis by CDC and others (Ciccarone 2019), but in reality it is a multiple opioid crisis. Synthetic opioids are manufactured entirely from inorganic chemicals, with the most common being fentanyl analogs (e.g. furnayl, acryl, and valeryl), carfentanil, and various U-477 formulations. According to federal drug enforcement data, prescription synthetics are tightly controlled and very little of it is diverted to illegal drug markets (DEA 2018). Instead, most street synthetics are non-prescription analogs produced abroad. China is the primary source of synthetic analogs in the United States, shipped either in small quantities through the postal system, or in larger amounts to Mexico for distribution in the north. It comes across the southern border and through U.S. ports of entry in the northeast.
Most synthetics are powerful narcotics, with pure fentanyl 100 times more potent and pure carfentanil 10,000 times more potent than morphine, with lethal doses as small as one milligram (DEA 2018). Synthetic analogs are inexpensive to produce, and DTOs are replacing prescription opioids with synthetics to create counterfeit pills, unbeknown to the user, who Can easily overdose on these highly potent mixtures with unpredictable dosage. Synthetics are also used to replace more expensive heroin, often mixed with inert ingredients or other powered drugs like cocaine. Overdose deaths from synthetic and multiple-opioids have increased exponentially in urban areas since 2014. Synthetic death rates are highest in large metros and micropolitans (about 4.0 per 100,000), slightly lower in small metros and semi-rural places (about 3.0), and lowest in completely rural areas (2.3), where fatal overdoses are growing slower. In summary, the current opioid overdose crisis in the United States is driven by highly potent synthetic opioid mixtures due to their lower cost and greater availability.
Identifying Opioid Epidemics and Syndemics
Our second objective is to identify opioid overdose mortality epidemics at the county level using LPA. The procedure classified 3,079 counties into six latent classes, each having a distinct distribution of opioid overdose mortality. Each latent class represents a distinct opioid epidemic. The initial LPA estimated five classes, but examination of class means indicated that the heroin class had two distinct subpopulations, with similar shapes but different elevations. For substantive interpretation, we split the heroin class into an above average group and a high group, resulting is six classes. Detailed results of the LPA are presented in the appendix. To ensure high internal consistency, we exclude any county not having a posterior probability (i.e. likelihood of correct classification) above 0.70 on at least one latent class, resulting in 149 unclassified counties. Means of standardized opioid mortality rates in 2014–2016 and change from 2002 to 2004 across the six latent classes are presented in Figure 3 and Table 1. The spatial distribution of the opioid overdose mortality classes is shown in Figure 4.
Figure 3.
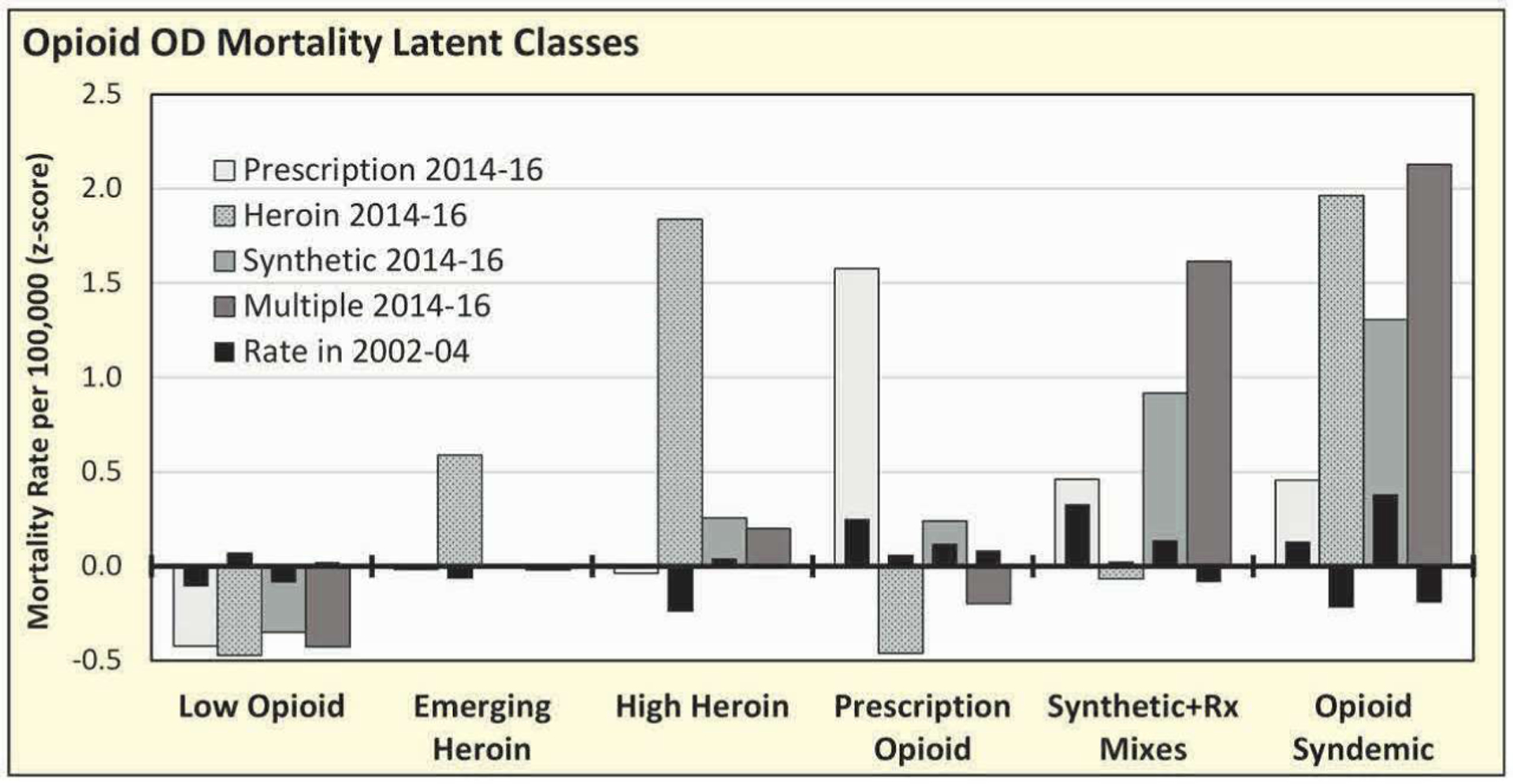
Means of Standardized Mortality per 100,000 (Age-Adjusted) by Opioid Overdose Latent Classes in 2002–2004 and 2014–2016 for n = 3,079 Counties in the Conterminous U.S. Unclassified Counties Not Reported.
Table 1.
Means of Standardized Opioid Overdose Mortality Rates by Latent Class by Core-Based Statistical Area (CBSA) for n = 3,079 Counties in the Conterminous U.S.
| Low Opioid | Emerging Heroin | High Heroin | Prescription Opioid | Synthetic + Rx Mixes | Opioid Syndemic | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OD Mortality Rate 2014–2016 (z) | Metro n = 476 | Non Metro n = 1,227 | Metro n = 224 | Non Metro n = 224 | Metro n = 72 | Non Metro n = 92 | Metro n = 67 | Non Metro n = 208 | Metro n = 80 | Non Metro n = 131 | Metro n = 82 | Non Metro n = 47 |
| Prescription opioid | −0.31 | −0.46* | −0.05 | 0.01 | 0.08 | −0.07 | 1.47 | 1.86* | 0.37 | 0.81* | 0.40 | 0.81* |
| Change from 2002 to 2004 | −0.26 | −0.38* | −0.02 | 0.03 | −0.05 | 0.00 | 1.36 | 1.75* | 0.23 | 0.20 | 0.21 | 0.70* |
| Heroin | −0.35 | −0.52* | 0.58 | 0.60 | 1.84 | 2.33* | −0.38 | −0.49* | 0.10 | −0.17* | 2.29 | 2.66 |
| Change from 2002 to 2004 | −0.37 | −0.49* | 0.53 | 0.62* | 1.74 | 2.42* | −0.35 | −0.46* | 0.03 | −0.16* | 2.14 | 2.47 |
| Synthetic opioid | −0.31 | −0.34 | 0.00 | 0.01 | 0.45 | 0.13* | 0.18 | 0.36 | 1.46 | 0.92* | 1.50 | 1.48 |
| Change from 2002 to 2004 | −0.23 | −0.27 | 0.01 | −0.01 | 0.34 | 0.13 | 0.11 | 0.21 | 1.10 | 0.82 | 1.07 | 1.29 |
| Multiple-opioids | −0.34 | −0.46* | 0.10 | −0.14* | 0.45 | 0.01* | −0.10 | −0.23* | 1.76 | 1.75 | 2.81 | 2.67 |
| Change from 2002 to 2004 | −0.31 | −0.43* | 0.10 | −0.13* | 0.38 | 0.03* | −0.15 | −0.32* | 1.02 | 1.31 | 2.75 | 2.60 |
| Prescription + heroin | −0.21 | −0.27* | 0.07 | −0.07* | 0.39 | 0.07* | −0.21 | −0.17 | 1.02 | 1.31 | 1.06 | 2.06* |
| Change from 2002 to 2004 | −0.21 | −0.24* | 0.03 | −0.09* | 0.32 | 0.09 | −0.17 | −0.14 | 0.98 | 1.30 | 1.00 | 1.91* |
| Prescription + synthetic | −0.24 | −0.35* | −0.03 | −0.12* | 0.07 | −0.15* | 0.20 | −0.02* | 1.32 | 1.96* | 1.44 | 1.83 |
| Change from 2002 to 2004 | −0.17 | −0.30* | 0.02 | −0.09* | 0.03 | −0.09 | 0.07 | −0.17* | 1.19 | 1.60 | 1.32 | 1.65 |
| Heroin + synthetic | −0.27 | −0.34* | 0.20 | −0.09* | 0.57 | 0.16* | −0.31 | −0.31 | 1.30 | 0.68* | 3.28 | 2.01* |
| Change from 2002 to 2004 | −0.27 | −0.33* | 0.19 | −0.08* | 0.51 | 0.12* | −0.30 | −0.31 | 1.28 | 0.67* | 3.25 | 2.01* |
| Rx + heroin + synthetic | −0.17 | −0.22* | 0.02 | −0.08 | 0.28 | 0.01* | −0.09 | −0.23* | 1.38 | 0.80* | 1.51 | 1.02 |
| Change from 2002 to 2004 | −0.17 | −0.22* | 0.01 | −0.08 | 0.28 | 0.02* | −0.09 | −0.22* | 1.37 | 0.80* | 1.48 | 1.03 |
| Non-opioid drugs | 0.04 | −0.11* | −0.12 | 0.18* | −0.08 | 0.09 | 0.08 | 0.29 | −0.07 | 0.23* | 0.01 | 0.42* |
| Change from 2002 to 2004 | −0.03 | 0.01 | −0.14 | 0.17* | −0.11 | 0.02 | −0.12 | 0.03 | −0.06 | 0.05 | −0.11 | 0.18* |
Notes: Overdose mortality rates (age-adjusted) per 100,000.
Significant difference at p < .05 (Games-Howell test) from metropolitan counties.
Figure 4.
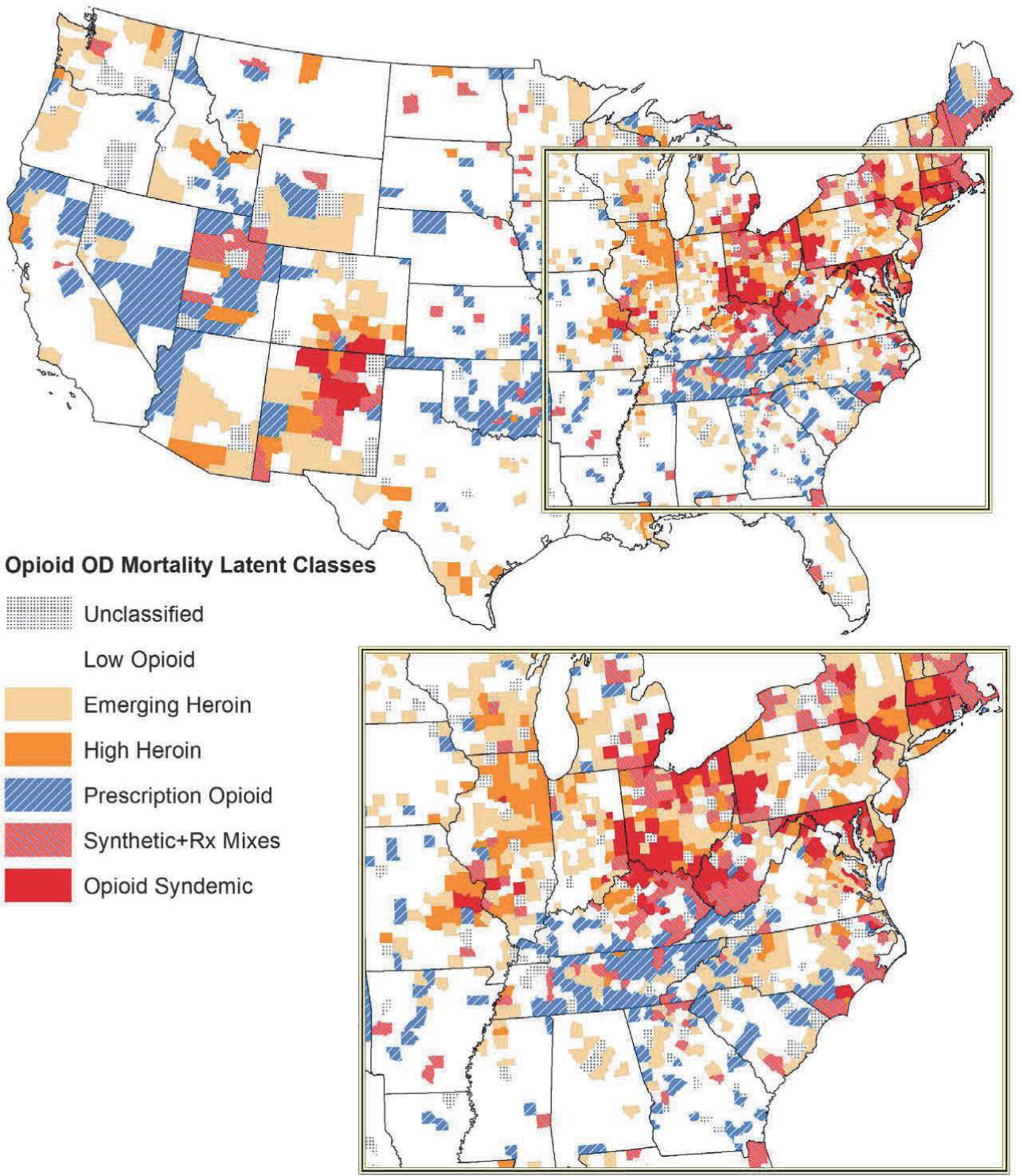
Opioid Overdose Mortality Latent Classes in 2002–2004, 2008–2010, and 2014–2016 for n = 3,079 Counties in the Conterminous U.S. Unclassified Counties have Posterior Class Probabilities below Pr < .7.
The majority of counties in the United States (n = 1,701) have low opioid overdose mortality, with standardized rates ranging from −0.30 to −0.50 below the national average. The remaining counties are classified into specific opioid mortality classes. The 448 counties in the emerging heroin class have above average fatal overdose rates (z = 0.59), but are not yet at crisis levels. By contrast, the high heroin epidemic class (also n = 448 counties) has extremely high heroin overdose fatalities (z = 1.84) that spiked between 2008–2010 and 2014–2016. More than half of high heroin counties are classified as non-metro (35.4 percent rural, 20.7 percent micropolitan), having overdoses significantly above the metropolitan rate. Both the emerging and high heroin classes are widespread across the country, tending to follow interstates and known drug trafficking corridors (DEA 2018). Heroin is concentrated in the northeastern states of Delaware, New Jersey, Pennsylvania, and New York. Deaths are also concentrated in two corridors following interstates, with one running from central Missouri through St. Louis to Chicago and the other running from El Paso north to Denver.
The prescription opioid epidemic class of counties reflects the public narrative of the opioid crisis, with three-quarters of the 275 counties in this class being non-metro (54.9 percent rural, 20.7 percent micropolitan). Prescription overdose deaths in these places have grown steadily over the past decade and a half, with prescription mortality in 2014–2016 being 1.86 standard deviations above average in non-metro counties and 1.47 in metro ones. There is a noticeable absence of heroin in these places, likely reflecting remote locations away from drug trafficking corridors. Over one-third of counties in Tennessee, Oklahoma, Nevada, and Utah fall into this epidemic. Unlike heroin, prescription overdose deaths seem to follow state boundaries, indicating that different state regulations may be a factor.
Many counties formerly in the prescription epidemic class have transitioned to the synthetic and prescription opioid mixes epidemic class (hereafter referred to as synthetic + Rx). These 211 counties always had above average prescription mortality (z = 0.46), but what distinguishes this epidemic is the rapid rise in multiple-cause (z = 1.62) and synthetic opioid (z = 0.92) overdose deaths—a clear sign of opioid street mixtures such as counterfeit prescription pills or adulterated heroin. For the 62.1 percent of non-metro counties in this class, deaths are driven by prescription-synthetic and prescription-heroin mixes. By contrast, in metro areas, synthetics play a much larger role. The synthetic + Rx epidemic is a major problem in New England states, affecting half the counties in Rhode Island, New Hampshire, Maine, and Massachusetts. Synthetic + Rx counties also predominate in Utah, West Virginia, Vermont, Kentucky, Maryland, and New Mexico.
The preceding classes can be termed epidemics, as only one or two opioids are responsible for most overdose fatalities. However, our analysis finds a group of counties with co-occurring epidemics that overlap and reinforce each other, what public health research terms syndemics (Ciccarone 2019; Singer et al. 2017). The 129 counties in the opioid syndemic class have coinciding epidemics involving prescriptions, heroin, synthetics, and mixes of the three. The 82 metropolitan syndemic counties post very high overdose mortality rates from heroin-synthetic mixes (z = 3.28) and heroin alone (z = 2.29). Non-metro syndemic places follow a similar pattern, except prescriptions which play a larger role in these 47 counties, with heroin (z = 2.66) and prescription-heroin mixes (z = 2.06) topping the list. Non-metro syndemics also have above average rates of overdose fatalities from non-opioid drugs, potentially indicating an undercount of unidentified opioid substances on death certificates. As a share of counties, the opioid syndemic has hit the eastern one-third of the nation hardest. The northeast syndemic cluster includes Connecticut, Maryland, and Massachusetts. Another syndemic cluster is located in the greater Appalachia region, concentrated in Ohio, West Virginia, northern Kentucky, Maryland, and western Pennsylvania. Many of these communities were “ground zero” of the opioid crisis in 1999 (Spencer et al. 2018). This cluster also extends into eastern Indiana and southeastern Michigan. The southwest syndemic cluster is located in New Mexico, centered around Santa Fe.
Distribution of opioid overdose classes varies across the rural-urban continuum as shown in Figure 5. The share of low opioid overdose counties increases as one moves from large metros to completely rural counties, accounting for over 60 percent of non-metropolitan non-adjacent counties. The emerging and high heroin classes together account for over 33 percent of metropolitan counties with over 250,000 people, and also in larger non-metro counties that are adjacent to metropolitans. The prescription opioid class becomes more common as counties become more rural, with the largest shares in non-metro counties under 20,000 people. The synthetic + Rx opioid class has a large presence at both ends of the rural-urban continuum, in the largest metros and also in the smallest rural places. Lastly, opioid syndemic counties trend with greater urbanization, with 10 percent of metros over one million people experiencing a syndemic. By contrast, syndemic counties are relatively rare in rural areas.
Figure 5.
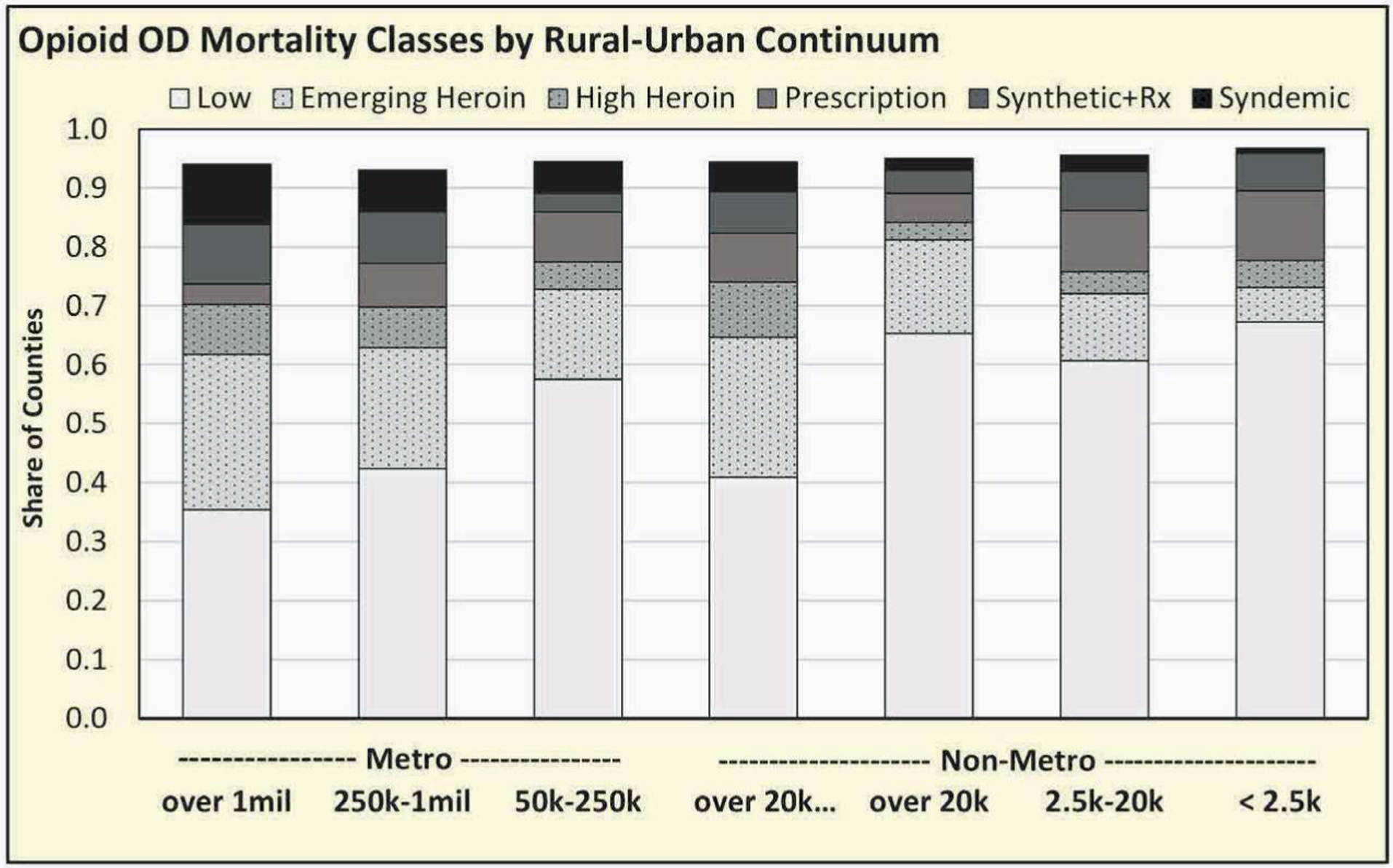
County Shares of Opioid Overdose Latent Classes by Modified Rural-Urban Continuum Codes for n = 3,079 Counties in the Conterminous U.S. Adjacent Denotes Metropolitan Adjacency. Unclassified Counties Not Reported.
Describing Opioid Epidemic Classes
Non-metropolitan counties.
To understand the characteristics of rural and micropolitan counties affected by the current opioid overdose crisis, we conduct mean difference tests across a number of demographic, drug risk, social disorganization, and economic conditions identified in the literature. The non-metro results are presented in Table 2. Starting with demographics, non-metro opioid epidemic classes are more densely populated compared to the low overdose group, with the syndemic class having the highest population densities in 2016, and the prescription epidemic class having the lowest. Most opioid epidemic places are older and less diverse than their low overdose counterparts having fewer shares of younger people under age 25, faster gains in elders over age 65, smaller shares of African Americans, and slow growing minority populations, notably Hispanics. However, rural prescription epidemic counties stand out by having more people of other races, in particular Native Americans. For locational factors, rural syndemic and heroin-related classes are more likely to be adjacent to metropolitan areas. By contrast, prescription-related epidemics (synthetic + Rx and prescription opioid classes) are more rural and possess more varied topography (plains with hills and mountains), likely exacerbating their remoteness from urban centers.
Table 2.
Socioeconomic Indicators by Opioid Overdose Mortality Latent Classes for n = 1,929 Non-Metropolitan Counties in the Conterminous U.S.
| (a) Opioid Syndemic | (b) Synthetic + Rx | (c) Prescription Opioid | (d) High Heroin | (e) Emerging Heroin | (f) Low Opioid | |
|---|---|---|---|---|---|---|
| Non-Metropolitan Areas, Percent in 2016 | n = 47 | n = 131 | n = 208 | n = 92 | n = 224 | n = 1,225 |
| Demographic and Location | ||||||
| Population density (mi2) | 84.83bcdf | 55.31acf | 40.52abef | 49.33af | 63.17cf | 30.48 |
| Age 25 and younger | 30.25 | 29.84f | 30.16f | 29.95 | 30.4f | 31.44 |
| Age 65 and older | 18.03c | 19.15 | 19.75af | 19.24 | 18.82 | 18.73 |
| African American | 3.51f | 4.60f | 5.77f | 4.17f | 5.66f | 9.29 |
| Hispanic, any race | 9.48 | 4.97df | 6.10f | 12.18b | 7.84 | 9.39 |
| Other or multiple races | 2.87cf | 4.18 | 6.54aef | 3.82 | 4.02c | 4.24 |
| Lived elsewhere 5 years ago | 26.88cf | 30.05 | 32.94a | 33.42 | 31.44 | 33.03 |
| Topographic variation (z) | 0.21 | 0.42f | 0.38f | 0.16 | 0.29f | −0.13 |
| Water area (z) | −0.17 | 0.01 | −0.06 | −0.19 | 0.14f | −0.18 |
| Micropolitan | 0.51 | 0.31c | 0.27e | 0.37 | 0.49bcf | 0.30 |
| Metro adjacent | 0.79bcf | 0.50a | 0.56a | 0.67f | 0.65f | 0.47 |
| Interstate density (mi2*100) | 1.54 | 1.49f | 1.07 | 1.55 | 1.40f | 0.87 |
| Drug Bisk and Social Disorganization | ||||||
| Adjacent opioid OD rate (100 k) | 22.53bcdef | 17.47acdef | 11.77abf | 12.98abf | 10.67abf | 5.87 |
| Non-opioid drug OD rate (100 k) | 10.50f | 9.21f | 9.63f | 8.26 | 8.91f | 6.96 |
| Dispensing rate 2011–2013 (per 100) | 117.30def | 112.99def | 115.23def | 84.86abc | 91.47abc | 87.70 |
| Dispensing rate 2014–2016 (per 100) | 95.33df | 97.41df | 98.47def | 68.93abce | 83.39cdf | 72.54 |
| Work disabled population | 4.40def | 4.70def | 4.48def | 3.68abc | 3.72abc | 3.46 |
| Poverty rate | 17.24 | 18.35e | 18.89def | 16.51c | 16.27bc | 17.38 |
| 80:20 income gap | 13.47 | 13.13 | 13.47d | 12.27cf | 12.76f | 13.63 |
| Vacant housing units | 18.85 | 23.12 | 23.37 | 22.26 | 21.47 | 20.82 |
| Property crime rate (100 k) | 425.77 | 354.83 | 366.78 | 523.46 | 491.95 | 367.74 |
| Social capital, organizations (z) | 0.07 | −0.11f | −0.26def | 0.63c | 0.31c | 0.54 |
| Social capital, engagement (z) | −0.57e | −0.51e | −0.53e | −0.40e | 0.19abcdf | −0.29 |
| Employment | ||||||
| Labor force participation | 41.59 | 40.45ef | 39.73def | 41.96c | 43.23bc | 42.98 |
| Agriculture, forestry and fishing | 2.58bcdef | 4.10acf | 5.71abef | 5.19af | 3.88acf | 8.46 |
| Mining | 1.20 | 2.58 | 2.44 | 2.73 | 1.62 | 2.29 |
| Construction | 6.71 | 7.53 | 7.35 | 7.19 | 7.26 | 7.23 |
| Manufacturing | 14.83 | 11.95e | 12.07e | 13.74 | 14.74bcf | 11.96 |
| Transportation and warehousing | 4.44 | 3.92 | 3.98 | 4.00 | 3.90 | 4.21 |
| Retail trade and leisure services | 24.57 | 25.40f | 24.79f | 23.80 | 25.22f | 23.15 |
| Healthcare and social assistance | 15.25cf | 14.99cf | 13.79ab | 14.09 | 14.06 | 13.39 |
| Change from 2000 | ||||||
| Population density (mi2) | 0.02 | 0.02 | 0.02 | 0.01 | 0.03 | 0.01 |
| Age 25 and younger | −3.17 | −3.10 | −2.83 | −3.61f | −3.09 | −2.75 |
| Age 65 and older | 3.58f | 3.55f | 3.26f | 3.72f | 3.43f | 2.42 |
| Minority population | 1.90cdef | 2.35cf | 3.41ab | 3.67a | 3.15af | 3.99 |
| Lived elsewhere 5 years ago | 10.43 | 12.77 | 13.87 | 15.83 | 12.11f | 14.16 |
| Non-opioid drug OD rate (100 k) | 6.27 | 5.77 | 5.67 | 5.07 | 5.88f | 4.16 |
| Dispensing rate 2011–2013 (per 100) | 11.42 | 7.56 | 15.34 | 10.29 | 12.84 | 10.91 |
| Dispensing rate 2014–2016 (per 100) | −10.56e | −8.03e | −1.42 | −5.64e | 4.76abdf | −4.24 |
| Work disabled population | 1.82ef | 1.60f | 1.54f | 1.49 | 1.47af | 1.30 |
| Poverty rate | 3.44f | 1.94 | 2.71f | 2.45 | 2.97f | 1.35 |
| 80:20 income gap | 1.44 | 0.20 | 0.49 | 0.95 | 0.97 | 0.88 |
| Vacant housing units | 4.96 | 4.12 | 5.16 | 4.25 | 4.34 | 4.34 |
| Property crime rate (100 k) | −49.30 | −37.05 | −42.72 | −278.2 | −239.2 | −111.8 |
| Social capital, organizations (z) | −0.26 | 0.03 | 0.00 | 0.12 | −0.08 | 0.05 |
| Social capital, engagement (z) | −0.20 | 0.09f | −0.12e | −0.43e | 0.34cdf | −0.39 |
| Labor force participation | −2.28f | −1.12 | −1.97f | −1.43 | −1.24f | −0.38 |
| Change from 1990 | ||||||
| Agriculture, forestry and fishing | −2.88f | −2.95f | −3.62f | −3.49f | −2.96f | −4.94 |
| Mining | −0.56 | −1.22f | −0.55f | −0.27 | −0.14 | 0.24 |
| Construction | −0.74f | 0.17f | 0.17f | 0.17 | 0.30f | 0.81 |
| Manufacturing | −6.07 | −7.30f | −7.42f | −6.11 | −6.59f | −4.79 |
| Transportation and warehousing | −0.17 | −0.03 | 0.11 | −0.02 | 0.08f | 0.38 |
| Retail trade and leisure services | 2.65 | 4.00 | 4.00f | 3.47 | 3.26 | 2.99 |
| Healthcare and social assistance | 7.25ef | 7.40cef | 6.46b | 6.73 | 6.23ab | 5.97 |
Notes: Significant difference at p < .05 (Games-Howell test) from the following opioid latent classes denoted by:
opioid syndemic,
synthetic + prescription,
prescription opioid,
high heroin,
emerging heroin, and
low opioid.
Drug risk factors play an important role in distinguishing between places impacted by opioids from those that are not. Non-metro counties affected by the opioid crisis are located near each other geographically, evidenced by high adjacent mortality. This is especially the case for the syndemic and synthetic + Rx classes, with neighboring counties having overdose death rates around 20 per 100,000 versus only 5.9 in the low group. In addition, drug overdose fatalities are high for other non-narcotic drugs, compounding the opioid problem in rural communities. Non-opioid fatalities are especially high in opioid syndemic and prescription-related classes, killing roughly 10 people per 100,000 (versus 7 per 100,000 in the low overdose group).
Retail pharmacy dispensing rates of opioids were high in the syndemic, synthetic + Rx, and prescription opioid classes during the period 2011–2013, with roughly 115 prescriptions filled per 100 residents, indicating greater supply than in the heroin and low overdose classes. However, dispensing rates have been falling, suggesting more stringent regulation by government and less generous prescribing practices by healthcare providers. Worryingly, dispending rates are growing in emerging heroin communities, which may indicate a future heroin-prescription epidemic in the coming years. Pain prescriptions and work disability are found to be strongly correlated with opioid mortality in the literature (Monnat 2019). We find evidence of this in multiple-opioid and prescription-opioid class counties, where disability rates are high and growing over time. Conversely, disability rates are lower in heroin-related counties, indicating that the opioid-disability linkage does not generally apply to heroin. In short, we find rural opioid epidemic counties to be spatially clustered, over-prescribed, work disabled, and have a growing fatal drug overdose problem, indicating that unknown opioid-like substances are circulating in the community.
Social disorganization only affects the rural prescription opioid epidemic, not other classes. Prescription opioid counties are economically distressed with low labor force participation and high poverty rates. They possess lower social capital in the form of fewer civic, social, and non-profit organizations. Limited financial and social resources likely hinder the ability of these communities to effectively respond to the rural prescription problem.
For employment, manufacturing job shares dropped by −7.3 percentage points in both synthetic + Rx and prescription opioid class counties, almost double that experienced by low overdose communities. This finding is consistent with previous research implicating industrial decline for the rise in opioid deaths (Monnat et al. 2019). More generally, non-metro counties impacted by opioid overdoses have falling labor force participation rates, indicating general economic distress as jobs have disappeared or people have stopped looking for work.
Metropolitan counties.
We next turn our attention to metropolitan counties, where socioeconomic differences are presented in Table 3. Demographically, most metro opioid epidemic classes are similar in population density, the exception being prescription opioid counties that have very low densities for an urban area (131.4 people per square mile). Syndemic and prescription-related opioid epidemic classes tend to have fewer youth, fewer Hispanics, and slower growing minority populations compared to the low overdose group and heroin-related classes. In terms of location, prescription opioid epidemic counties occur in suburban or exurban portions of metropolitan areas, are less likely to contain a principal city, and have lower miles of interstate roads. By contrast, opioid syndemic and heroin-related counties look more like typical metropolitan areas, with high population densities, primary cities, and more interstate highways.
Table 3.
Socioeconomic Indicators by Opioid Overdose Mortality Latent Classes for n= 1,001 Metropolitan Counties in the Conterminous U.S.
| (a) Opioid Syndemic | (b) Synthetic + Rx | (c) Prescription Opioid | (d) High Heroin | (e) Emerging Heroin | (f) Low Opioid | |
|---|---|---|---|---|---|---|
| Metropolitan Areas, Percent in 2016 | n = 82 | n = 80 | n = 67 | n = 72 | n = 224 | n = 476 |
| Demographic and Location | ||||||
| Population density (mi2) | 773.88c | 640.54 | 131.43adef | 582.13c | 950.91c | 404.21 |
| Age 25 and younger | 30.84ef | 31.44f | 31.41f | 32.15 | 32.52a | 33.39 |
| Age 65 and older | 16.30ef | 16.36 | 17.03ef | 15.58 | 14.99ac | 14.99 |
| African American | 9.50 | 7.76f | 6.95f | 9.15 | 10.43 | 12.63 |
| Hispanic, any race | 4.75ef | 5.76ef | 4.39def | 8.50c | 10.31abc | 11.95 |
| Other or multiple races | 4.05ef | 4.64 | 4.56 | 4.40e | 5.55ad | 5.34 |
| Lived elsewhere 5 years ago | 27.15bef | 32.57a | 31.88f | 29.64f | 33.04af | 36.61 |
| Topographic variation (z) | 0.22df | −0.09c | 0.39bdef | −0.27ac | −0.06c | −0.16 |
| Water Area (z) | 0.57cf | 0.55c | 0.08ab | 0.43 | 0.39 | 0.27 |
| Primary metro county | 0.71c | 0.59 | 0.36adef | 0.63c | 0.67c | 0.57 |
| Interstate density (mi2*100) | 6.79cf | 4.41 | 2.56ade | 4.83cf | 4.74cf | 2.96 |
| Drug Risk and Social Disorganization | ||||||
| Adjacent opioid OD rate (100 k) | 25.04bcdef | 18.83acdef | 12.45abdf | 15.35abcef | 11.40abdf | 7.27 |
| Non-opioid drug OD rate (100 k) | 7.79 | 7.25 | 8.22 | 7.18 | 6.93 | 7.94 |
| Dispensing rate 2011–2013 (per 100) | 97.39cef | 90.65c | 116.77abdef | 92.26c | 83.54ac | 84.06 |
| Dispensing rate 2014–2016 (per 100) | 84.79ef | 75.36c | 99.08bef | 81.62 | 73.65ac | 73.98 |
| Work disabled population | 3.58cef | 3.36ce | 4.48abdef | 3.18c | 2.90abc | 3.10 |
| Poverty rate | 14.16c | 13.28c | 17.17abdef | 13.63c | 13.38cf | 15.24 |
| 80:20 income gap | 13.87 | 13.31 | 12.80 | 13.20 | 13.36 | 13.57 |
| Vacant housing units | 12.12 | 13.29 | 14.80def | 11.56c | 10.99cf | 12.51 |
| Property crime rate (100 k) | 471.98 | 516.45 | 455.79 | 650.19 | 546.22 | 479.93 |
| Social capital, organizations (z) | −0.02c | −0.36c | −1.48abdef | −0.65c | −0.66c | −0.71 |
| Social capital, engagement (z) | 0.44 | 0.52 | 0.03de | 0.66c | 0.70c | 0.41 |
| Employment | ||||||
| Labor force participation | 46.38cf | 46.34c | 41.89abdef | 46.68cf | 46.97cf | 44.85 |
| Agriculture, forestry and fishing | 0.80cef | 1.37f | 2.43ad | 1.17cf | 1.44af | 2.63 |
| Mining | 0.5Sf | 0.59 | 1.18d | 0.34cf | 0.51f | 1.04 |
| Construction | 6.44cf | 6.98 | 7.91ae | 6.91 | 6.77cf | 7.27 |
| Manufacturing | 12.28c | 11.56c | 15.58abef | 13.21 | 11.96c | 11.55 |
| Transportation and warehousing | 4.11 | 4.05 | 4.58 | 4.28 | 4.26 | 4.13 |
| Retail trade and leisure services | 25.56c | 25.51 | 24.13a | 25.13 | 25.44 | 25.15 |
| Healthcare and social assistance | 15.20cef | 14.30 | 13.30a | 14.51 | 13.78a | 13.68 |
| Change from 2000 | ||||||
| Population density (mi2) | 0.14 | 0.44 | 0.16ef | 0.33e | 0.89cd | 0.56 |
| Age 25 and younger | −2.56 | −2.79 | −2.74 | −2.56 | −2.35f | −2.74 |
| Age 65 and older | 2.78c | 3.05 | 3.92aef | 3.13 | 2.87c | 2.69 |
| Minority population | 3.87ef | 4.00ef | 3.24def | 5.17c | 5.92abc | 5.64 |
| Lived elsewhere 5 years ago | 10.02f | 12.35 | 11.21 | 9.83f | 10.90f | 13.62 |
| Non-opioid drug OD rate (100 k) | 3.93 | 4.12 | 4.02 | 3.32 | 3.33f | 4.56 |
| Dispensing rate 2011–2013 (per 100) | 7.99 | 8.34 | 14.74 | 10.33 | 8.55 | 9.85 |
| Dispensing rate 2014–2016 (per 100) | −4.60 | −6.95 | −2.94 | −0.31 | −1.33 | −0.24 |
| Work disabled population | 1.50ef | 1.35ce | 1.70bdef | 1.29c | 1.11abc | 1.21 |
| Poverty rate | 3.38 | 3.03 | 3.69f | 3.68f | 3.17 | 2.61 |
| 80:20 income gap | 2.04c | 1.75c | 0.66abdef | 2.21cf | 2.00cf | 1.54 |
| Vacant housing units | 3.14 | 3.40 | 4.12ef | 3.00 | 2.83c | 2.93 |
| Property crime rate (100 k) | −12.04 | −4.76 | 60.48def | −202.3c | −68.56c | −49.78 |
| Social capital, organizations (z) | −0.10 | 0.01 | 0.09 | −0.09 | −0.07 | −0.04 |
| Social capital, engagement (z) | 0.15c | 0.13c | 0.73abd | 0.19c | 0.40 | 0.43 |
| Labor force participation | −0.38c | −0.81c | −3.10abdef | −1.08c | −0.87c | −0.81 |
| Change from 1990 | ||||||
| Agriculture, forestry and fishing | −1.48f | −1.93 | −2.22 | −1.77 | −1.73f | −2.50 |
| Mining | −0.08 | −0.17 | 0.10 | −0.14f | −0.12f | 0.11 |
| Construction | −0.74cf | −0.32 | 0.24a | 0.06 | −0.31 | 0.10 |
| Manufacturing | −7.81cf | −7.76c | −10.75abef | −8.57f | −7.56cf | −6.36 |
| Transportation and warehousing | −0.46c | −0.33 | 0.31a | 0.03 | −0.10 | −0.12 |
| Retail trade and leisure services | 3.33 | 3.32 | 4.09 | 3.32 | 3.60 | 3.41 |
| Healthcare and social assistance | 6.39 | 6.35 | 6.23 | 6.47f | 5.93 | 5.71 |
Notes: Significant difference at p < .05 (Games-Howell test) from the following opioid latent classes denoted by:
opioid syndemic,
synthetic + prescription,
prescription opioid,
high heroin,
emerging heroin, and
low opioid.
Metro drug risk factors are similar to rural and micropolitan counties. Compared to the low group, adjacent opioid overdose mortality is high, especially in syndemic and synthetic + Rx class counties. Work disability is a problem in the syndemic and prescription opioid classes, but is largely absent in emerging heroin and low opioid overdose metros. The well-established linkage between dispensing rates and work disability is only found to occur in prescription opioid metros. There are no statistical differences in non-opioid drug overdoses across metro epidemic and low opioid counties.
Social disorganization is only apparent in metro counties impacted by prescription opioids. These counties have depressed labor markets with low and falling labor force participation rates, stagnant incomes with higher poverty yet slower growing inequality, physical disorder with more vacant housing units, social disorder by gains in property crime (burglary, larceny, vehicle theft, and arson), and less social capital with fewer non-profit, civic, and social organizations. All of this points to metro prescription opioid counties being economically and socially disadvantaged. However, one bright spot is growing community engagement since 1997, suggesting that residents have become more active in local affairs.
Despite the severity of opioid overdose deaths, other metro opioid classes show few signs of economic distress. For example, metro syndemic and heroin-related class counties have high rates of labor force participation, and exhibit no differences in poverty, crime, or social capital. There are also few major differences in employment structure. Manufacturing is in decline in most high opioid metro counties, similar to what is observed in non-metros. In particular, metro counties in the prescription opioid class are more manufacturing dependent compared to other groups, having the largest manufacturing job share yet also experiencing the fastest decline since 1990.
Discussion and Conclusion
The objectives of our exploratory analysis are to describe fatal opioid overdose trends, identify opioid mortality epidemics at the county level, and to describe characteristics of opioid overdose epidemics across the rural-urban continuum. We summarize our key findings and discuss their implications below. To begin, the opioid crisis is no longer a prescription crisis, or even a heroin crisis, but has transitioned to synthetic opioids and multiple-opioid mixtures. This transition began in 2014 and has continued apace, resulting in higher fatal overdose rates in urban areas. Next, there is not a single opioid overdose epidemic, rather multiple and overlapping ones. About 25 percent of counties nationally is severely impacted by opioid overdose fatalities, but not in the same manner as we identify distinct epidemics. The prescription opioid epidemic is the most common (8.9 percent of counties) and is overwhelmingly located in rural counties. A number of counties have transitioned to a synthetic-prescription mixture epidemic (6.9 percent), affecting both large urban cities and small rural places. The heroin epidemic is concentrated in the nation’s larger metropolitan and smaller micropolitan cities (5.3 percent), but these illicit drugs are still relatively rare in rural counties. Lastly, a small share of counties (4.2 percent) are experiencing three coinciding epidemics of prescriptions, heroin, and synthetics—what we term an opioid overdose syndemic. Many central Appalachia counties suffer from an opioid syndemic, where the crisis began in the 1990s and has only worsened since.
Some common characteristics connect counties impacted by opioid overdose deaths across the rural-urban continuum. First, non-metropolitan opioid overdose epidemics also have a non-opioid drug overdose problem. This suggests that the current rural opioid crisis is part of a broader drug problem, taking root in smaller communities with an existing drug user population and/or socioeconomic conditions favorable to drug abuse. While it is possible that fatal overdoses Can be linked to actual non-opioid drugs (such as cocaine, methamphetamine, or prescription sedatives), it is more likely such deaths are attributable to unknown opioid-like substances that escape detection by rural medical examiners, who may not have the resources to run more detailed toxicology tests. Ruhm (2018) argues that the official CDC opioid overdose count is underreported due to these undetected opioids. Our work only partially supports this argument and only in non-metropolitan counties. Second, places affected by opioid overdose epidemics tend to be older, less diverse in terms of race and ethnicity, and have a declining industrial base. Such places are remnants of the 20th century industrial economy that are becoming increasingly dissimilar from the rest of the nation demographically, economically, and culturally—what some sociologists term “the left behind” places (Wuthnow 2018). These two findings are consistent with existing public health research (Monnat 2019; Rigg et al. 2018; Ruhm 2017).
Prescription opioid and synthetic-prescription opioid mixture epidemics tend to occur in smaller and more remote counties. These include suburban and exurban portions of metropolitan areas, as well as sparsely populated rural counties distant from urban centers. They are also less connected to interstate highways and are located in regions with low mountainous, making these places more remote and isolated. Remoteness can hinder economic development and result in local economies dominated by resource-based industries that have high rates of workplace injury and disability (BLS 2017; Pender et al. 2014), placing these communities at risk for prescription opioid use and potential overdose fatality (Monnat et al. 2019). However, remoteness also limits the presence of DTOs that supply illicit opioids like heroin and synthetics, leaving narcotics supplied by local pharmacies as the primary source (DEA 2018). By contrast, opioid syndemic counties are more densely populated and more connected to transportation infrastructure, allowing DTOs based in larger cities to supply a wide array of illicit opioids, other drugs, and multiple-drug street mixtures. The linkage between drug networks and urbanization is well supported in criminology (Berg and Lauritsen 2016).
Previous research clearly demonstrates dispensing rates and work disability increases a community’s opioid supply and mortality risk (Dasgupta et al. 2018; Monnat 2019). However, we find the disability-dispensing-ouerdose pathway only holds for rural and micropolitan counties, and not for metropolitan ones. Rural industrial decline left a legacy of unemployed and underemployed people with some form of work disability. It is a plausible treatment for work-related pain, likely involving opioids prescribed by a health provider, helped start the cycle of opioid addiction that would culminate in the current opioid overdose crisis in rural America (Frasquilho et al. 2016; Quinones 2015). Reasons why we fail to detect this linkage in metropolitan counties may be due to greater availability of non-drug pain management options in larger cities, stricter prescribing and dispensing practices in urban areas with a history of drug crimes, and a larger and more diversified job base in less injury-prone sectors. More research is needed to address this inconsistency between our findings and extant literature.
Lastly, we only find evidence to support the “deaths of despair” narrative in counties where the prescription opioid epidemic prevails, and not in places affected by heroin or the opioid syndemic. Further, evidence for this narrative is stronger in metropolitan than in rural and micropolitan counties. For example, metro counties in the prescription opioid class show the greatest signs of drug risk (high dispensing and disability), economic distress (high poverty and low labor participation), injury-prone blue-collar job losses (especially mining and manufacturing, see BLS 2017), and social disorganization (vacant homes, low social capital, and growing property crime). Non-metro counties score high on economic distress, but not on social disorganization.
We explain this discrepancy by arguing prescription epidemic counties, whether rural or urban, have been “left behind” the rest of the nation. These communities are sparsely populated, remote, older and mostly white, have a history of drug abuse, and are former farm and factory communities that have been in decline since the 1990s. Opioids cure likely obtained from local pharmacies and illegally traded among drug users, separate from DTOs. By contrast, high heroin and opioid syndemic counties tend to be more urban, connected, diverse, and in general more economically secure. The urban opioid crisis likely follows the path of previous drug epidemics, where DTOs sell illicit drugs to certain segments of the population, typically existing drug users or the urban underclass. It is disadvantaged subpopulations in the community, not the urban community itself, that has been left behind and vulnerable to opioid addiction.
In conclusion, our findings point to several policy recommendations, despite some methodological limitations.7 First, all communities impacted by opioid overdose epidemics need expanded drug addiction and treatment services, especially critical services advocated by CDC like immediate medication-assisted treatment (MAT) in emergency departments using buprenorphine, expanded beds for long-term MAT along with automatic insurance authorization, and targeted naloxone distribution to first responders and social services providers (Carroll, Green, and Noonan 2018). Second, tighter regulation of opioid prescribing and dispensing practices will have little effect on the current overdose crisis, now dominated by illicit drugs like heroin and synthetic opioids. Further, greater drug interdiction efforts to stop the flow of illicit opioids will also meet with limited success. Previous supply-side initiatives have not stopped drug usage in the United States. Instead, we argue that policy should reduce the demand for drugs domestically. For example, the PROSPER (2019) program links adolescents and parents within local organizations (in particular schools) to promote prosocial interactions to reduce substance abuse and other social problems. Our third recommendation is to assist “left behind” communities by creating: economic security by stabilizing middle-skill and middle wage jobs; social order by reducing crime, poverty, and social inequalities; and physical order by maintenance of housing and infrastructure. However, such initiatives require long-term investments that are unlikely to have an immediate effect on overdose fatalities. In summary, multiple opioid epidemics require multiple intervention strategies. Our analysis provides needed information to communities allowing them to better understand their local opioid problem and the socioeconomic conditions linked to it. To this end, we have provided a data file listing the opioid epidemic classes for every county in the conterminous U.S.
Supplementary Material
Acknowledgments
We thank the reviewers for their constructive comments that focused and improved our manuscript. This work is supported by the USDA National Institute of Food and Agriculture, Agricultural and Food Research Initiative Competitive Program (Agriculture Economics and Rural Communities), Grant # 2018-68006-27640
Appendix
Results of the LPA on n = 3,079 counties find evidence for five or six classes. Expectation-maximization is used to obtain maximum likelihood a posterior estimates using 10,000 starting values (Marsh et al. 2009). The sample size adjusted Bayesian information criterion (BIC) is a relative fit index based on log-likelihoods, adjusted for parameters and sample size, with lower values indicating better fit. The rate of decrease in BICs slows between classes six and eight, indicating a range of ideal solutions. All classes exhibit good separation based on relative entropy scores, where values above 0.8 indicate a high degree of certainty in classification (Collier and Leite 2017). Both the Vuong-Lo-Mendell-Rubin and Lo-Mendell-Rubin adjusted likelihood ratio test the null hypothesis that k number of classes fits just as well and k − 1 classes. Both tests are non-significant at the sixth class stage, indicating the presence of five classes. However, examination of latent means shows the heroin class includes two distinct subpopulations that have similar shape but different elevations (z = 0.5 and z > 1.5). We decided that the two heroin classes are substantively different and favor the six-class solution based on interpretability.
Table A1.
Fit Statistics from Latent Profile Analysis on Standardized Opioid Overdose Mortality between 2002–2004, 2008–2010, and 2014–2016 for n = 3,079 Counties in the Conterminous U.S.
| Class Stage | BIC | BIC Change | Relative Entropy | VLMR Test | LMR Test |
|---|---|---|---|---|---|
| 1 | 59,670 | n.a. | 1.000 | n.a. | n.a. |
| 2 | 51,830 | −13.139% | 0.696 | 7,884*** | 7,776*** |
| 3 | 49,006 | −5.449% | 0.952 | 2,867*** | 2,828*** |
| 4 | 46,613 | −4.883% | 0.967 | 2,437** | 2,404** |
| 5 | 44,873 | −3.733% | 0.947 | 1,784*** | 1,760*** |
| 6 | 43,360 | −3.372% | 0.943 | 1,557 | 1,535 |
| 7 | 42,128 | −2.841% | 0.950 | 1,276 | 1,258 |
| 8 | 41,239 | −2.110% | 0.944 | 932 | 920 |
| 9 | 40,192 | −2.539% | 0.945 | 876 | 864 |
| 10 | 39,227 | −2.401% | 0.947 | 1,007† | 993† |
| 11 | 38,616 | −1.558% | 0.951 | 654† | 645† |
| 12 | 38,049 | −1.468% | 0.950 | 611 | 603 |
Notes: BIC is the sample size adjusted Bayesian information criterion. VLMR is the Vuong-Lo-Mendell-Rubin Likelihood Ratio Test. LMR is the Lo-Mendell-Rubin Likelihood Ratio Test.
p< .10;
p< .05;
p< .01;
p< .001.
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article at the publisher’s web site.
First, independent cities in Virginia with populations under 65,000 are merged back into their respective counties, resulting in 29 fewer county-level equivalents. Second, Broomfield County in Colorado, newly created in 2003, is disaggregated back into its four original counties based on population-weighted geographic shares. The above modifications result in a time series of 3,079 counties back to 1990, down from the original 3,109 counties, but with no loss of information as data are merged and not dropped. All data used in this study conform to these spatial units.
International Classification of Diseases (ICD-10) codes defining opioid overdose and use mortality include: drug poisonings (X40–44, X60–64, X85, or Y10–14) plus the presence of one or more opioids (T40.0–40.6); or opioid-related mental and behavioral disorders (F11.0–11.9). Mortality is disaggregated by heroin or opium (T40.0 or T40.1), prescription opioids including methadone (T40.2 or T40.3), and synthetic opioids or unknown narcotics (T40.4 or T40.6). By including behavioral deaths, we expand upon the CDC opioid overdose definition, but this raises mortality counts by just under one percent or around 1,000 additional deaths nationally between 2014 and 2016.
LPA provides hypothesis tests of class structure and model fit statistics, whereas cluster analysis relies on subjective heuristics. Cluster analysis can result in very different solutions depending on the type of distance metrics and linkage rules used, whereas LPA relies on a single estimation technique. More importantly, LPA estimates classification uncertainty using posterior probabilities obtained using Bayes theorem. By contrast, cluster analysis incorrectly assumes perfect certainty in classification, failing to recognize that cases may fit into multiple clusters.
ACS estimates for most counties exhibit relatively low error, even in counties with small populations, with most coefficients of variation around 25 percent and only a few nearing 50 percent. Variables with larger errors include agriculture and mining employment. We drop two counties (Kenedy and Loving counties in Texas) due to large errors on many variables.
QuintilesiMS data only include prescriptions obtained from retail pharmacies and exclude high-volume prescribing pain clinics. Missing cells are imputed using a Markov Chain Monte Carlo model with 500 multiple imputations (Carpenter and Kenward 2013). All imputed values exhibit high consistency, with coefficients of variation below 33 percent.
VCR data from FBI suffer from two limitations: delayed release of CUITent data and non-reporting by local law enforcement to FBI. First, 2016 data were just released in January 2019 after a long delay, and 2015 data have yet to be released. To address this issue, we mean substitute 2015 data as the average of 2014 and 2016. Second, missing cells due to non-reporting to FBI are addressed in a number of ways. Dlinois and Florida did not report any crime data to FBI for a number of years, so crime counts are taken from state agencies. State reports generally adhere to FBI guidelines for index crimes (e.g. violent and property crime). Next, attempts were made to impute other missing cells using Markov Chain Monte Carlo models, but this failed to provide consistent values (coefficients of variation were typically over 100 percent). Finally, missing cells are substituted with state averages disaggregated by urban influence code.
One major limitation is a recognized opioid overdose death undercount, where official CDC tallies are estimated to be underreported by 20 percent (Ruhm 2018). There is no agreed upon method to correct this problem, thus official CDC counts used in our analysis should be considered as a conservative estimate of opioid overdose mortality. A second limitation is relatively poor classification of counties into the high heroin class. We urge caution in drawing broad conclusions from our analysis on the correlates of the heroin epidemic. Future research should explore ways to address these two issues.
Contributor Information
David J. Peters, Department of Sociology, Iowa State University
Shannon M. Monnat, Maxwell School of Citizenship and Public Affairs, Syracuse University
Andrew L. Hochstetler, Department of Sociology, Iowa State University
Mark T. Berg, Department of Sociology and Criminology, University of Iowa
References
- Abar B and Loken E. 2012. “Consequences of Fitting Nonidentified Latent Class Models.” Structural Equation Modeling 19: 1–15. [Google Scholar]
- Autor D, Dorn D, and Hanson G. 2018. When Work Disappears: Manufacturing Decline and the Falling Marriage Market Value of Young Men (Working Paper No. 7010). Munich, Germany: CESifo. Retrieved July 21, 2019 (https://www.ifo.de/DocDL/cesifol_wp7010.pdf). [Google Scholar]
- BLS. 2017. Injuries, Illnesses, and Fatalities Program, Bureau of Labor Statistics (Web Database). Washington, DC: U.S. Department of Labor. Retrieved August 1, 2018 (https://www.bls.gov/iif/oshsum.htm). [Google Scholar]
- Berg M and Lauritsen J. 2016. “Telling a Similar Story Twice? NCVS/UCR Convergence in Serious Violent Crime Rates in Rural, Suburban, and Urban Places 1973–2010.” Journal of Quantitative Criminology 32: 61–87. [Google Scholar]
- Berg M and Rengifo A. 2009. “Rethinking Community Organization and Robbery: Considering Illicit Market Dynamics.” Quarterly 26: 211–37. [Google Scholar]
- Betz M and Jones L. 2018. “Wage and Employment Growth in America’s Drug Epidemic: Is All Growth Created Equal?” American Journal of Agricultural Economics 100:1357–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bursik R and Grasmick H. 1993. Neighborhoods and Crime: The Dimensions of Effective Community Control Lanham, MD: Lexington Books. [Google Scholar]
- Bursik R and Webb j.. 1982. “Community Change and Patterns of Delinquency.” American Journal of Sociology 88: 24–42. [Google Scholar]
- Bruinsma GJ, Pauwels LJ, Weerman FM, and Bemasco W. 2013. “Social Disorganization, Social Capital, Collective Efficacy, and the Spatial Distribution of Crime and Offenders.” British Journal of Criminology 53: 942–63. [Google Scholar]
- CDC. 2017. National Vital Statistics System, Microdata Access, U.S. Centers for Disease Control and Prevention (Database). Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- CDC. 2018. 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes - United States (Surveillance Special Report, U.S. Centers for Disease Control and Prevention). Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- CDC. 2019. Opioid Overdose, U.S. Centers for Disease Control and Prevention (Web Database). Atlanta, GA: U.S. Department of Health and Human Services. Retrieved March 18, 2019 (https://www.cdc.gov/drugoverdose/opioids/index.html). [Google Scholar]
- Carpenter J and Kenward M. 2013. Multiple Imputation and its Application. Chichester, UK: Wiley. [Google Scholar]
- Carroll J, Green T, and Noonan R. 2018. Evidence-Based Strategies for Preventing Opioid Overdoses: What’s Working in the United States (U.S. Centers for Disease Control and Prevention). Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Case A and Deaton A. 2017. Mortality and Morbidity in the 21st Century (Brookings Paper on Economic Activity, Spring 2017). Washington, DC: Brookings Institution. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D 2019. “The Triple Wave Epidemic: Supply and Demand Drivers of the U.S. Opioid Overdose Crisis.” International Journal of Drug Policy. 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier Z and Leite W. 2017. “A Comparison of Three-Step Approaches for Auxiliary Variables in Latent Class and Latent Profile Analysis.” Structural Equation Modeling 24: 819–30. [Google Scholar]
- Council of Economic Advisers. 2017. The Underestimated Costs of the Opioid Crisis. Washington, DC: Executive Office of the President of the United States. Retrieved July 21, 2019 (https://www.whitehouse.gov/briefings-statements/cea-report-underestimated-cost-opioid-crisis). [Google Scholar]
- Dasgupta N, Beletsky L, and Ciccarone D. 2018. “Opioid Crisis: No Easy Fix to its Social and Economic Determinants.” American Journal of Public Health 108: 182–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David H and Dorn D. 2013. “The Growth of Low-Skill Service Jobs and the Polarization of the U.S. Labor Market.” American Economic Review 103: 1553–97. [Google Scholar]
- DEA. 2017. 2017National Drug Threat Assessment (DEA-DCT-DIR-040–17, Drug Enforcement Agency). Washington, DC: U.S. Department of Justice. [Google Scholar]
- DEA. 2018. 2018 National Drug Threat Assessment (DEA-DCT-DIR-032–18, Drug Enforcement Agency). Washington, DC: U.S. Department of Justice. [Google Scholar]
- Frasquilho D, Matos M, Salonna F, Guerreiro D, Storti C, Caspar T, andCaldasde-Almeida j.. 2016. “Mental Health Outcomes in Times of Economic Recession: A Systematic Literature Review.” BMC Public Health 16(115): 1–10. 10.1186/s12889-016-2720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, and Vlahov D. 2003. “Contextual Determinants of Drug Use Risk Behavior: A Theoretic Framework.” Journal of Urban Health 80: 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haegerich T, Paulozzi L, Manns B, and Jones C. 2014. ‘What We Know, and Don’t Know, About the Impact of State Policy and System-Level Interventions on Prescription Drug Overdose.” Drug and Alcohol Dependency 145: 37–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffajee R, Anupam J, and Weiner S. 2015. “Mandatory Use of Prescription Drug Monitoring Programs.” Journal of the American Medical Association 313: 891–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochstetler A, DeLisi M, and Peters D. 2016. “Classifying Risk Development and Predicting Parolee Recidivism with Growth Mixture Models.” American Journal of Criminal Justice Al: 1–29. [Google Scholar]
- Hochstetler A, Peters D, and Copes H. 2017. “Supervisory Experience and Data Points: Implementation Barriers, Risk Assessment and Correctional Professionals.” Criminal Justice Studies 30: 240–56. [Google Scholar]
- Hollingsworth A, Ruhm C, and Simon K. 2017. “Macroeconomic Conditions and Opioid Abuse.” Journal of Health Economics 56: 222–33. [DOI] [PubMed] [Google Scholar]
- Jalal H, Buchanich J, Roberts M, Balmert L, Zhang K, and Burke D. 2018. “Changing Dynamics of the Drug Overdose Epidemic in the United States from 1979 through 2016.” Science 361 (6408): 1–7. 10.1126/science.aaull84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R and Wichern D. 2007. Applied Multivariate Statistical Analysis. Upper Saddle River, NJ: Pearson Prentice Hall. [Google Scholar]
- Kaplan M, Huguet N, Caetano R, Giesbrecht N, Kerr W, and McFarland B. 2015. “Economic Contraction, Alcohol Intoxication and Suicide: Analysis of the National Violent Death Reporting System.” Injury Prevention 21: 35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr W, Kaplan M, Huguet N, Caetano R, Giesbrecht N, and McFarland B. 2017. “Economic Recession, Alcohol, and Suicide Rates: Comparative Effects of Poverty, Foreclosure, and Job Loss.” American Journal of Preventive Medicine 52: 469–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K, Cerda M, Brady J, Havens J, and Galea S. 2014. “Understanding the Rural-Urban Differences in Nonmedical Prescription Opioid use and Abuse in the United States.” American Journal of Public Health 104(2): e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger A 2017. Where Have All the Workers Gone? An Inquiry into the Decline of U.S. Labor Force Participation (Brookings Papers on Economic Activity). Washington, DC: Brookings Institution. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S, Tan X, and Bray B. 2013. “Latent Class Analysis with Distal Outcomes: A Flexible Model-Based Approach.” Structural Equation Modeling 20: 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobao L and Stofferahn C. 2008. “The Community Effects of Industrialized Farming.” Agriculture and Human Values 25: 219–40. [Google Scholar]
- Lurie J 2017. “Children of the Opioid Epidemic are Flooding Foster Homes. America is Turning a Blind Eye.” Mother Jones. Retrieved July 5, 2017 (http://www.motherjones.com/politics/20l7/07/children-ohio-opioid-epidemic). [Google Scholar]
- Marsh H, Liidtke O, Trautwein U, and Morin A. 2009. “Classical Latent Profile Analysis of Academic Self-Concept Dimensions: Synergy of Person- and Variable-Centered Approaches to Theoretical Models of Self-Concept” Structural Equation Modeling 16: 191–225. [Google Scholar]
- Martinez R, Rosenfeld R, and Marez D. 2008. “Social Disorganization, Drug Market Activity, and Neighborhood Violent Crime.” Urban Affairs Review 43: 846–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLachlan G and Peel D. 2000. Finite Mixture Models. New York: Wiley. [Google Scholar]
- McLean K 2016. ‘“There’s Nothing Here’: Deindustrialization as Risk Environment for Overdose.” International Journal of Drug Policy 29: 19–26. [DOI] [PubMed] [Google Scholar]
- Moller S, Alderson A, and Nielsen F. 2009. “Changing Patterns of Income Inequality in U.S. Counties, 1970–2000.” American Journal of Sociology 114: 1037–101. [DOI] [PubMed] [Google Scholar]
- Monnat S 2018. “Factors Associated With County-Level Differences in U.S. Drug-Related Mortality Rates.” American Journal of Preventive Medicine 54: 611–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat S 2019. “The Contributions of Socioeconomic and Opioid Supply Factors to U.S. Drug Mortality Rates: Urban-Rural and Within-Rural Differences.” Journal of Rural Studies 68: 319–35. [Google Scholar]
- Monnat S, Peters D, Berg M, and Hochstetler A. 2019. “Using Census Data to Understand County-Level Differences in Overall Drug Mortality and Opioid-Related Mortality by Opioid Type.” American Journal of Public Health 109: 1084–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat S and Rigg K. 2016. “Examining Rural/Urban Differences in Prescription Opioid Misuse Among U.S. Adolescents.” journal of Rural Health 32: 204–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan G 2015. “Mixed Mode Latent Class Analysis: An Examination of Fit Index Performance for Classification.” Structural Equation Modeling 22: 76–86. [Google Scholar]
- NGA 2016. “A Compact to Fight Opiate Addiction.” National Governor’s Association. Retrieved July 13, 2017 (https://www.nga.org/cms/news/2016/opioid-compact). [Google Scholar]
- Paulozzi L and Annest J. 2007. “Unintentional Poisoning Deaths - United States, 1999–2004.” Morbidity and Mortality Weekly Report 56: 93–96. [PubMed] [Google Scholar]
- Pender J, Weber B, Johnson T, and Fannin J. 2014. Rural Wealth Creation. New York: Routledge. [Google Scholar]
- Peters D 2009. “Typology of American Poverty.” International Regional Science Review 32: 19–39. [Google Scholar]
- Peters D 2012. “Understanding Micro and Meso Scale Income Inequality in the Midwestern United States, 1979–2009.” Rural Sociology 77: 171–202. [Google Scholar]
- Peters D 2013. “American Income Inequality Across Economic and Geographic Space, 1970–2010.” Social Science Research 42: 1490–504. [DOI] [PubMed] [Google Scholar]
- Pierce J and Schott P. 2017. Trade Liberalization and Mortality: Evidence from U.S. Counties (Finance and Economics Discussion Series, Divisions of Research and Statistics and Monetary Affairs, Vol. 2016–094). Washington, DC: Federal Reserve Board. [Google Scholar]
- PROSPER. 2019. PROmoting School-community-university Partnerships to Enhance Resilience, Partnerships in Prevention Science Institute (Website). Ames, IA: Iowa State University. Retrieved August 20, 2019 (http://helpingkidsprosper.org). [Google Scholar]
- Quinones S 2015. Dreamland: The True Tale of America’s Opiate Epidemic. New York: Bloomsbury Press. [Google Scholar]
- Rigg K and Monnat S. 2015. “Urban vs. Rural Differences in Prescription Opioid Misuse Among Adults in the United States: Informing Region Specific Drug Policies and Interventions.” International Journal of Drug Policy 26: 484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg K, Monnat S, and Chavez M. 2018. “Opioid-Related Mortality in Rural America: Geographic Heterogeneity and Intervention Strategies.” International Journal of Drug Policy 57: 119–29. [DOI] [PubMed] [Google Scholar]
- Rothman K, Lash T, and Greenland S. 2008. Modem Epidemiology. Philadelphia, PA: Lippincott, Williams & Wilkins. [Google Scholar]
- Ruhm C 2017. “Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates.” American Journal of Preventive Medicine 53: 745–53. [DOI] [PubMed] [Google Scholar]
- Ruhm C 2018. “Corrected US Opioid-Involved Drug Poisoning Deaths and Mortality Rates, 1999–2015.” Addiction 113:1339–44. [DOI] [PubMed] [Google Scholar]
- Ruhm C 2019. “Drivers of the Fatal Drug Epidemic.” Journal of Health Economics 64: 25–42. [DOI] [PubMed] [Google Scholar]
- Sampson R and Groves W. 1989. “Community Structure and Crime: Testing Social-Disorganization Theory.” American Journal of Sociology 94: 774–802. [Google Scholar]
- Sampson R, Raudenbush S, and Earls F. 1997. “Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy.” Science 277(5328): 918–24. [DOI] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, and Baldwin G. 2019. “Drug and Opioid-Involved Overdose Deaths - United States, 2013–2017.” Morbidity and Mortality Weekly Report 67:1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, Bulled N, Ostrach B, and Mendenhall E. 2017. “Syndemics and the Biosocial Conception of Health.” The Lancet 389: 941–50. [DOI] [PubMed] [Google Scholar]
- Spencer JC, Wheeler SB, Rotter JS, and Holmes GM. 2018. “Decomposing Mortality Disparities in Urban and Rural U.S. Counties.” Health Services Research 53: 4310–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisburd D, Eck J, Braga A, Telep C, Cave B, Bowers K, Bruinsma G, Gill C, Groff E, Hinkle J, Hibdon J, Johnson S, Lawton B, Lum C, Ratcliffe J, Rengert G, Taniguchi T, and Yang S. 2016. Place Matters: Criminology for the 21st Century. New York: Cambridge University Press. [Google Scholar]
- Weisburd D, Feucht T, and Bruinsma G. 2009. Putting Crime in Its Place: Units of Analysis in Spatial Crime Research. New York: Springer Verlaag. [Google Scholar]
- Weiss A, Elixhauser A, Barrett M, Steiner C, Bailey M, and O’Malley L. 2016. Opioid-Related Inpatient Stays and Emergency Visits by State, 2009–2014 (Statistical Brief #219, Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality). Rockville, MD: U.S. Department of Health and Human Services. [Google Scholar]
- Whalen J 2016. “For Small Town Cops, Opioid Scourge Hits Close to Home.” Wall Street Journal Retrieved April 18, 2017 (https://www.wsj.com/articles/for-small-town-cops-opioid-scourge-hits-close-to-home-1475074699). [Google Scholar]
- Wikström PO and Sampson R. 2006. The Explanation of Crime: Context, Mechanisms, and Development. New York: Cambridge University Press. [Google Scholar]
- Wilson J and Kelling G. 1982. “Broken Windows: The Police and Neighborhood Safety.” Atlantic Monthly 249: 29–38. [Google Scholar]
- Wuthnow R 2018. The Left Behind: Decline and Rage in SmaUrTown America. Princeton, NJ: Princeton University Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


