Abstract
Parents play a critical role in the development of children’s eating behaviors and weight status, serving as providers, models, and regulators of the food environment. Many research reviews have focused on the robust body of evidence on coercive control in feeding: how parenting practices such as restriction and pressure to eat increase children's risk for developing undesirable eating behaviors and unhealthy weight outcomes. Fewer reviews adopt a strengths-based perspective focusing on the ways that parents can actively support the development of healthy eating behaviors and weight trajectories. Emerging research on such positive parenting styles and practices offers solutions beyond the avoidance of coercive control, as well as opportunities to highlight parallels between research on food parenting and the broader, well-established developmental literature on positive parenting. The focus of this review is to summarize what is known regarding benefits of positive parenting styles and practices for child eating and weight outcomes and discuss recommendations for future research. Current evidence supports starting with responsive feeding and parenting during infancy and incorporating structure and limit setting in early childhood, with mealtime structure remaining important during middle childhood and adolescence. Areas for future research include: 1) further examination of the implications of identified food parenting practices and styles among diverse groups and caregivers; 2) increased consideration of child factors (e.g., temperament) as moderators or mediators; and 3) further clarification of the relationship between general parenting and food parenting.
Keywords: Positive parenting, parent feeding, infancy, childhood, adolescence
Introduction
Currently, 18.5% of children ages 2–19 years have obesity, with prevalence differing by race and socioeconomic status (SES) 1. While obesity is a multifactorial disease, parents have a substantial influence on child weight status 2. In fact, parent weight status remains one of the most robust predictors of child weight status 3. In addition to their genetic contribution, parents play a critical role in the development and maintenance of children’s weight outcomes as well as their eating behaviors by shaping the eating environment 4 through several roles 5. Parents control home food availability (e.g., buying food, controlling access to food, preparing food), serve as role models, adopt feeding styles that set the overall emotional climate related to feeding, and use goal-directed feeding practices to shape the types and amounts of food their children consume 5.
A critical question when considering the substantial influences of parents on children’s eating and weight outcomes is: on which aspects of parenting should we focus? Many research reviews have focused on the robust body of evidence on coercive control in feeding: how parent feeding practices such as restriction and pressure to eat increase children's risk for developing undesirable eating behaviors and unhealthy weight outcomes 5–7. Fewer reviews adopt a strengths-based perspective focusing exclusively on the ways that parents can actively support the development of healthy eating behaviors and weight trajectories. Emerging research on such parenting styles and practices offers solutions beyond the avoidance of coercive control, as well as opportunities to highlight parallels between research on food parenting and the broader, well-established developmental literature on positive parenting.
As literature linking parenting with eating and weight has grown, disagreement in the identification, definition, and measurement of key constructs has become evident. A food parenting working group was formed to address these issues, and in 2013, the working group published their consensus report, which included the identification and definition of three separate constructs – general parenting styles, feeding styles, and food parenting practices8. General parenting styles reflect parent-child interactions across all domains, whereas feeding styles reflect parent-child interactions specific to the feeding domain. Both general parenting styles and feeding styles are assessed by examining parents’ demandingness and responsiveness. Demandingness is defined as behavioral control and monitoring (i.e., structure and limit setting), and responsiveness is defined as warmth and awareness of a child’s specific needs and requests to help foster autonomy 9. Feeding styles describe the degree to which a parent’s approach reflects demandingness and responsiveness within feeding contexts 10. Within research on general parenting styles and feeding styles, these dimensions are often used to classify parents into one of four feeding styles, which are based on Maccoby and Martin’s general parenting styles classifications 11: authoritative (high demandingness, high responsiveness), authoritarian (high demandingness, low responsiveness), permissive/indulgent (low demandingness, high responsiveness), and neglectful (low demandingness, high responsiveness) 10.
In contrast to the overarching nature of general parenting and feeding styles, food parenting practices include specific behaviors that parents use when feeding their child. Food parenting practices are goal-oriented behaviors used in the context of feeding that reflect overarching constructs of coercive control, structure, and autonomy support 7. Some researchers have argued that general parenting styles should be conceptualized as contextual moderators of the impact of specific parenting practices, both in and outside the feeding domain 12,13. Parents’ food parenting practices, such as limit setting, may be more likely to be successful and predict healthier outcomes in the context of a generally authoritative parenting style that couples demandingness and responsiveness. However, application of this idea in the realm of food parenting is newer, and research is limited.
The most commonly-used food parenting constructs are outlined in Table 1. In this review, we use the term food parenting to encompass both feeding styles and food parenting practices. We focus on positive general and food parenting constructs, using “positive” to refer to general parenting styles, feeding styles, and food parenting practices that are developmentally appropriate and contribute to an effective balance between parental demandingness and responsiveness. This parallels terminology used in the developmental psychology literature, in which there is a robust evidence base on “positive parenting” approaches that promote adaptive child outcomes more broadly14. Looking to the developmental literature can move child feeding research forward. A focus on positive parenting is one way to do this and builds upon prior influences of the developmental literature on the understanding of child feeding, such as in the realm of measurement.
Table 1.
Definitions and examples of feeding styles and food parenting practices, adapted from Vaughn et al. (2016).7
| Construct | Definitions and Examples | |
|---|---|---|
| POSITIVE FEEDING STYLES | ||
| Refer to child-centered, responsive feeding styles, in which parents provide a high degree of structure, guidance, respect for children’s autonomy over their eating, and promotion of independence in eating | ||
| Authoritative Style | High demandingness, high responsiveness; high degree of involvement, structure and control, high child autonomy support responsiveness * During early infancy (i.e., the first 4–6 months postpartum when the infant is exclusively mild-fed) infancy, a style high in responsiveness and low in demandingness is appropriate |
|
| POSITIVE FOOD PARENTING PRACTICES | ||
| Include a set of practices high in structure and autonomy support which have been shown to support children’s food acceptance, awareness of hunger and fullness cues (appetite regulation), nutrition knowledge, healthy food choices and diet quality | ||
| STRUCTURE | Monitoring and Engagement | Provides age-appropriate monitoring of the child’s eating and food purchasing behaviors; offers guided choices at meals and snacks; offers appropriate portion sizes; allows child to make contribute ideas for meals and snacks |
| Rules and Limit Setting | Places reasonable limits on the child’s intake and purchase of unhealthy foods; conveys expectations regarding mealtimes and participation in family meals; limits frequent snacking | |
| Establishes Routines | Establishes feeding routines; provides developmentally-appropriate feeding environment; provides opportunities for regular family meals; offer meals and snacks at consistent times | |
| Provision of Healthy Foods | Introduces a variety of healthful foods to child; makes healthy foods available and accessible at meals and snacks | |
| Covert Control | Controls a child’s food intake in ways that are less obvious to the child (e.g., not purchasing unhealthy foods or avoiding unhealthy restaurants) | |
| AUTONOMY SUPPORT | Responsiveness to Cues | Awareness and respect for child’s hunger and fullness cues; terminates feeding/no longer offers food in response to fullness cues; does not pressure child to eat; does not demand that children clean their plates |
| Praise and Encouragement | Praises child’s efforts for trying new foods or eating specific foods; encourages children to try new foods, without coercion; encourages children to develop more autonomy over eating (meal preparation, food shopping), and applauds efforts | |
| Social Modeling | Uses own behavior, knowledge and values to influence child’s eating; provides opportunities for child to learn about healthy eating; involves child in food preparation, food preparation and food shopping; provides knowledge about nutrition and health; models a preference/liking for healthy foods | |
| NEGATIVE FEEDING STYLES | ||
| Refer to parent-centered, coercive and unstructured feeding styles related to either a controlling or permissive general parenting style, in which parents place too many or too little demands on children’s self-regulation and behavior, and enforce too much or too little control over children’s eating in ways that undermine food acceptance and appetite regulation | ||
| aAuthoritarian | High demandingness, low responsiveness; high control, low support for child autonomy in eating | |
| aPermissive/Indulgent | Low demandingness, high responsiveness; low control, high support for child autonomy in eating | |
| aUninvolved | Low demandingness, low responsiveness; lack of support, structure and control | |
| NEGATIVE FOOD PARENTING PRACTICES | ||
| Include a set of practices that are high in coercive control and low in structure which have been shown to undermine children’s autonomy over their eating, and pose risk for the development of problematic eating behaviors and poor diet quality | ||
| COERCIVE CONTROL | Overt Control | Controls the child’s intake in a way that is more obvious to the child (e.g., strict rules regarding what and how much the child should eat); controls the amount and types of foods the child is offered |
| Restriction | Restricts the child’s access to or intake of certain foods, often energy-dense foods; keeps certain foods out of reach or hidden | |
| Intrusive Monitoring | Monitors the types and amounts of food that the child consumes in ways that correspond to overt control; keeps track of the child’s intake of certain foods (sweets, snacks, high-fat) | |
| Pressure | Pressures the child to consume more food and specific foods (e.g., vegetables); demands that the child clean his/her plate | |
| Emotional Feeding | Offers food in response to the child’s negative emotions or distress; uses food to soothe or combat boredom | |
| Instrumental Feeding | Uses food as a reward, or withholds food as a punishment; uses bribes and threats to influence the child’s eating | |
| UNSTRUCTURED | Neglect | Abdicates responsibility in feeding; lacks involvement and oversight for children’s eating; unaware of what, how much or how often child is eating (low monitoring and engagement); limits availability of nutrient-dense foods; lacks consistency in meal and snack times and routines |
| Indulgence | Allows child complete control over eating; inconsistent mealtimes, allows child to eat/snack frequently and at will; provides large/unlimited portion sizes; provides unlimited availability of low-nutrient dense foods and low availability of nutrient-dense foods; acts as a short-order cook; does not monitor child’s food purchases | |
Notes: Definitions and examples of feeding styles and food parenting practices were adapted from Vaughn et al. 7, and align with general parenting practices described by Maccoby and Martin 11, and applied to the feeding domain by Hughes and colleagues 10. Within positive feeding styles and food parenting practices, structure aligns with demandingness, and autonomy support aligns with responsiveness. Within negative feeding styles and food parenting practices, coercive control aligns with high demandingness and low responsiveness. Unstructured practices are low in demandingness; neglect is also low in responsiveness, while indulgence is high in responsiveness.
Given that the early food parenting literature sought to elucidate effects of coercive control such as pressure to eat and restriction, it is not surprising that first generation of measures of food parenting, such as the Child Feeding Questionnaire (CFQ) 15, the Comprehensive Feeding Practices Questionnaire 16, and the Infant Feeding Style Questionnaire 17, typically focused on these negative aspects of feeding. More recently, new survey instruments such as the Structure and Control in Parent Feeding 18 and the Food Parenting Inventory 19 have been developed that expand upon classic measures by allowing measurement of other potentially more supportive aspects of control in parent feeding, such as structure and limit setting 20, as well as practices that provide support for children’s autonomy in eating, including responsiveness to children’s hunger and fullness. This development follows the differentiation among types of parental control in the broader parenting literature 21. These refined child feeding measures provide opportunities to deepen our understanding of these more positive aspects of food parenting.
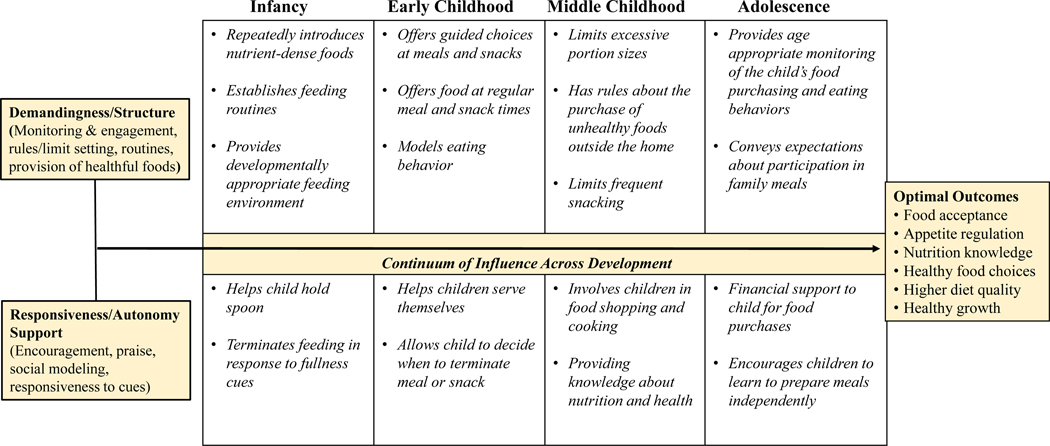
The focus of this narrative review is to use strengths-based and developmental perspectives to examine associations between the use of positive parenting styles and practices and child eating and weight outcomes from infancy to adolescence, and to offer directions for future research. While decades of research in developmental sciences illustrate that the parent-child relationship in the feeding domain is bidirectional, with the parent influencing the child’s behavior and the child influencing the parent’s behavior 22, we focus primarily on parent contributions – both general and food-specific -- in the current review. Figure 1 presents central dimensions of positive food parenting from infancy to adolescence that support the development of healthy eating behaviors and weight outcomes. Across development, there is a need for both parental demandingness (e.g., structure and limit-setting, monitoring) and responsiveness (e.g., autonomy support, encouragement). However, the expression of each changes as the child’s needs and abilities change. We propose that exposure to positive parenting styles and practices - both general and food-specific - can shape children’s food preferences and acceptance, responsiveness to hunger and satiation, healthy eating behaviors, and intake of nutrient-dense foods over time. These child factors may, in turn, confer protection from obesity. Additionally, given that behavior change precedes weight gain, it may be that positive behavior change (e.g., increases in fruit and vegetables, decreases in sugar-sweetened beverage consumption) is observed without any weight change in the short-term, but rather the attainment of optimal weight observed over the long-term. As such, we focus on both eating and weight outcomes. Following discussion of links between general and food parenting and these outcomes in each developmental stage, directions for future research are presented.
Figure 1. Examples of positive food parenting across development.
Legend. Parental demandingness/structure and responsive/autonomy support are critical at every developmental stage (i.e., there is a continuum of influence). Examples of developmentally appropriate positive food parenting practices reflecting overarching dimensions of demandingness/structure and responsiveness/autonomy support. Examples are illustrative and neither exhaustive nor limited to a particular stage. There may be cumulative impact of parenting, such that parenting at early developmental stages may continue to impact children at later developmental stages.
Methods
Authors with expertise in each developmental period under consideration (infancy: AKV; early childhood: SAF; middle childhood: LAF; adolescence: KNB) developed the initial draft of the corresponding section. These authors reviewed seminal and recent review articles and perspectives and also identified relevant empirical articles with rigorous designs. For example, in drafting the early childhood section, recent and key reviews and perspectives on food parenting in early childhood were reviewed (e.g., 7,23,24) and given the availability of studies with rigorous designs during this time period, the author of this section focused on longitudinal studies that included observational measures of parenting constructs and subsequent eating and/or weight outcomes, as well as randomized studies of general parenting interventions as described below. Because the extant research and parenting considerations differ by developmental period, this approach allows us to represent and articulate these differences. The writing team reviewed and refined each other’s sections, allowing for a consensus about the definition and organization of constructs, key take-home points, and areas for future research across developmental periods.
As noted in other key narrative reviews in the field (e.g., 7), there are strengths and limitations to such an approach. This work is not a systematic review and should not be interpreted as such. However, we would argue that there is value in bringing together a diverse team of content experts and arriving at a consensus about the state of the field and directions for future research. In addition, general and food parenting are often studied separately, and the present review uses the concept of “positive parenting” from the developmental sciences to bring together constructs like authoritative parenting styles, authoritative feeding styles, structure, and autonomy supportive practices. We argue that there is much to be learned from the decades of successful parenting research in the developmental sciences, and as such, we also discuss available evidence regarding how evidence-based general positive parenting interventions might impact child eating and weight status. We also apply developmental perspectives to illustrate how central dimensions of feeding styles and practices change with development, communicating which components of responsiveness and/or demandingness become particularly relevant with each new developmental period.
Infancy
When considering Maccoby and Martin’s parenting framework 11, the dimension that is most relevant during infancy is parental responsiveness. A primary goal of early feeding interactions should be to support the infant’s developing abilities to self-regulate within feeding and eating contexts. Previous research suggests infants exhibit some evidence of intake regulation in response to growth needs from birth 25. However, this compensation is only partial in the first few months postpartum, improving across the first year and as the infant matures 26, with evidence of subsequent decline in eating self-regulation by 15 months of age 27, though there is likely individual variation in this timeline.
Optimal feeding styles and food parenting practices during infancy ensure the infant is fed in a way that preserves and promotes his or her developing capacities to self-regulate (see Figure 1). To this end, current recommendations focus on promoting responsive food parenting, defined within this developmental period as feeding styles and food parenting practices that are infant-led and responsive to infant cues (e.g., 23,28) across all modes of infant feeding (e.g., breastfeeding, bottle feeding, introduction of complementary foods). During the period of exclusive milk feeding (for the first 4–6 months), a caregiver engaging in responsive feeding is attentive to the infant’s cues. The caregiver only offers the breast or bottle and engages the infant when s/he is receptive and also allows the infant to disengage or take breaks as needed. Thus, the caregiver paces the feeding, as well as the social interaction that occurs during the feeding, in response to infant cues. The caregiver may gently prompt the infant to eat, especially during the introduction of complementary foods and beverages when the infant is exposed to novel foods, but the caregiver withdraws if the infant refuses or shows clear disengagement cues and refrains from using coercion or force to encourage the infant to eat.
During early feeding, potential bidirectional influences between feeding mode (at the breast versus via a bottle) and food parenting styles and practices are important to consider; caregivers’ food parenting styles and practices likely influence feeding choices, but feeding mode may also influence food parenting styles and practices. There is some evidence that mothers who initially exhibit greater levels of sensitivity to their infants are more likely to initiate breastfeeding and have longer breastfeeding durations29,30. Moreover, studies comparing feeding interactions of breastfeeding and bottle-feeding dyads during early infancy demonstrate breastfeeding mothers exhibit more warmth, sensitivity to infant cues, and behavioral synchrony during infant feeding compared to bottle-feeding mothers 31. However, the experience of breastfeeding may also promote responsive feeding because, to a certain extent, successful breastfeeding is inherently infant-led, requiring the infant to play an active role in initiating the feeding by signaling hunger and effectively latching onto the breast, and maintaining the feeding by sustaining proper positioning, suction, and nutritive sucking 32. In addition, because the breastfeeding mother cannot readily assess the amount consumed by the infant at the breast, she must learn her infants’ cues and behaviors to decide when to terminate the feed and whether the infant is satiated. Longitudinal studies consistently demonstrate that longer durations of breastfeeding are associated with self-reports of higher responsive feeding practices and styles, greater use of structure-related food parenting practices during complementary-food feedings, and lower pressuring feeding style during later childhood 31. Although the largely correlational nature of this evidence precludes the ability to disentangle potential bidirectional effects and confounders, it is possible that mothers with greater propensity toward responsive feeding are more likely to breastfeed and that the experience of breastfeeding further promotes use of responsive food parenting practices and styles.
In contrast, mothers who report more controlling feeding practices at birth are more likely to formula-feed 33, perhaps because bottle-feeding affords the caregiver more control over the feeding and assurance about how much the child has consumed 32,34. The caregiver can exert more control over the initiation or pacing of the feed by pushing the nipple into the infant’s mouth or positioning the bottle in a way that increases milk flow and reduces the amount of infant effort exerted. When using clear bottles, caregivers have more information about how much expressed breast milk or formula is offered and consumed and thus may be less reliant on infant cues and behaviors to decide when to terminate the feeding. This may lead to overfeeding and poorer infant self-regulation of intake if the caregiver encourages the infant to consume more milk than needed. However, bottle-feeding does not lead to overfeeding for all dyads as greater levels of responsive feeding are associated with lower intakes during bottle-feeding 35. Recent experimental research illustrates that, in the short term, replacing conventional, clear bottles with opaque, weighted bottles promotes maternal sensitivity to infant cues and helps mothers feed their infants less expressed breast milk or formula at a slower rate 36. Thus, strategies to promote responsive feeding during bottle-feeding may help reduce risk for overfeeding and excess weight gain during infancy, and offer the potential to reach vulnerable families who are more likely to bottle-feed formula given contextual barriers to breast-feeding (e.g., need to return to work, lack of resources such as time and supplies for using a breast pump, or maternal obesity that are associated with lactation challenges 37).
During the introduction to complementary foods and beverages, responsive feeding remains important for supporting infant self-regulation of intake while also promoting preferences for nutrient-dense foods 28. Because this developmental period is characterized by significant oral-motor development 38 and a rapid transition in the child’s dietary exposures, components of responsive feeding expand to include feeding practices that are infant-led, while guiding the infant to accept and enjoy a wide array of nutrient-dense foods. As humans are predisposed to prefer sweet, umami, and salty tastes over bitter and sour, preferences for novel flavors and foods develop via learning, including: 1) repeated exposure, wherein foods are repeatedly offered to and consumed by the child, increasing their familiarity; 2) associative conditioning, wherein a novel food is paired with a familiar, already preferred food or with a positive social context; and 3) social modeling, wherein the child observes parents, siblings, or peers consume and enjoy the food 39.
Baby-led weaning (BLW) is a less commonly used approach to the introduction to complementary foods. At the heart of BLW is the concept of infant self-feeding and autonomy. In strict BLW, infants self-feed only finger foods, whereas other adaptations of BLW allow for the infant to self-feed using utensils and pureed food. This emphasis on self-feeding is congruent with responsive feeding, including the ideas that: 1) the infant should be provided the autonomy to explore novel foods by him or herself and at his or her own pace and 2) the infant’s initial rejection of novel foods is reframed within the context of trusting the child to eat when he or she is ready with repeated exposure. Within BLW, parents wait to introduce complementary foods and beverages until their infant exhibits developmental signs of readiness to self-feed (i.e., ability to sit-up unsupported, with good head and neck control), which generally occurs around 6 months of age. While BLW is increasing in popularity, research on this approach is limited and is confounded by the fact that many children who primarily self-feed may also be spoon-fed to some extent by caregivers 40. Some evidence for potential benefits of BLW on infant eating outcomes (such as improved satiety responsiveness in later toddlerhood 41) exists, as well as evidence that BLW may have other benefits for the family, such as lower maternal anxiety related to feeding 42 Findings on implications for weight outcomes are mixed 41,43. Given that 4–6 months may be a sensitive period for food and flavor learning 44 as well as an important time for early and frequent consumption of foods for allergy prevention 45, delaying introduction of complementary foods until an infant displays all of the necessary readiness signs of BLW may have some downsides. Thus, more research on this approach and its congruence with responsive feeding and healthy eating and weight outcomes is warranted. Notably, BLW was included in the recent National Academies of Sciences, Engineering, and Medicine expert report on feeding infants and children from birth to 24 months as a research gap in the infant feeding domain46.
Taken together, support for infant self-regulation of intake through responsive feeding and parenting comprise an important foundation for supporting healthy weight gain trajectories during early infancy 47. Indeed, randomized controlled trials illustrate that promoting responsive feeding and parenting styles and practices promotes healthy weight gain trajectories during infancy and lower risk for overweight during infancy and early childhood 48. The promotion of responsive parenting beyond the feeding domain during this period may further support healthy eating and weight 49,50, which highlights an opportunity for further integration between the developmental and obesity sciences.
Early Childhood
As children move from infancy to early childhood, the demandingness dimension of Maccoby and Martin’s framework 11 becomes increasingly relevant. It is recommended that parents continue responsiveness to child cues, coupling it with structure and limit setting to achieve a parenting style that is authoritative, rather than indulgent/permissive. As shown in Figure 1, this structure should be developmentally appropriate.
Emerging evidence shows that parental provision of structure predicts healthy eating and weight in young children. In a longitudinal study of 207 Australian families, reports of greater structure-related food parenting practices, including family meals and structured meal timing, at 2 and 3.7 years of age predicted lower food fussiness later in early childhood 51. Findings from a large cohort study also support the importance of structure in the form of routines with positive outcomes across multiple domains: three-year-old children who had regular bedtimes, mealtimes, and screen-time limits had increased emotion regulation; poor early childhood emotion regulation was predictive of obesity 8 years later 52. Yet in a prospective, longitudinal study assessing structure in feeding with mothers of 2- to 5- year-olds, mothers who rated children higher on satiety responsiveness at age 2 were more likely to report structured meal timing later in development, suggesting a potential bidirectional association between the child’s ability to self-regulate intake and the family’s propensity toward structured meals.
One possible mechanism linking structure and limit setting with eating and weight is that young children encountering fewer demands on feeding may grow up in environments in which energy-dense salty and sweet foods are routinely available and accessible, though this still needs to be examined. Such foods correspond with children’s genetic taste predispositions, making it likely that children would select them over healthier alternatives, potentially interfering with repeated exposures to nutrient-dense foods 39. In contrast, incorporation of limit setting through approaches like constrained or guided choices (in which the parent provides developmentally-appropriate food and decides when it is time to eat while the child can self-serve and decide what and how much to eat) is an example of a feeding style that couples demandingness with responsiveness to the child’s hunger, satiation, and growing autonomy 7. Such approaches may also support children’s development of self-regulation around eating.
The literature on general parenting styles corroborates the importance of parents’ provision of structure and limits. Of the four styles from Maccoby and Martin’s framework 11, the indulgent/permissive style is most consistently linked with poorer dietary patterns and elevated weight status in early childhood 6, suggesting that in early childhood, responsiveness in the absence of demandingness confers risk for unhealthy eating and weight outcomes. In a longitudinal study combining observational and self-report measures of general parenting style, children experiencing a permissive/indulgent parenting style at age 4.5 years were most likely to be at risk for subsequent elevated weight outcomes 53. Evidence in support of causal pathways comes from an intervention promoting authoritative feeding styles within a sample of primarily Black, low-income mothers of preschoolers 54. This intervention resulted in decreases in children’s daily consumption of solid fats and added sugar and increases in authoritative parenting practices during a laboratory test meal 54.
There are several rigorously-tested, evidence-based positive parenting training programs in early childhood that can provide insight as to how general parenting, eating, and weight status may be linked. Studies of these general parenting interventions, which incorporate elements of demandingness and responsiveness, have strong internal validity supporting linkages between positive parenting and adaptive child outcomes, traditionally those in the socioemotional domain. Strategies promoted in these general parenting interventions include child-directed play; verbal responsiveness; allocating attention to positive behaviors and ignoring undesirable behavior; and descriptive, task-oriented praise (e.g., “I really liked how you cleaned up your blocks when you were done playing”) 55. Secondary data analyses reveal the potential of such general parenting interventions to impact weight over time. A randomized study using the Parent Program of the Incredible Years Series to promote parenting competence and child socioemotional development was conducted in a sample of low-income parents of preschoolers at high risk for conduct problems 56. Findings included that intervention-group children had lower BMI z-scores than controls in middle childhood 56. Similarly, at-risk children randomized to a ParentCorps intervention group during pre-Kindergarten had lower BMIs than controls at age 8 years 56, and implementation of the Family Check-Up intervention during toddlerhood impacted children’s BMI trajectories into middle childhood, with evidence of mediation by parents’ positive behavior support (e.g., structuring play periods, prompting and reinforcing positive behavior) during toddlerhood 57. In contrast, when implementing parent, child, and classroom components of Incredible Years in an attempt to improve self-regulation and weight outcomes among preschoolers enrolled in Head Start, Lumeng and colleagues 58 did not observe effects on preschoolers’ weight outcomes. The authors noted that these null results may have been due to low parent participation in this trial, with another possibility being that effects on weight could emerge at a later time. Overall, these randomized studies of well-established general parenting interventions suggest the potential of general parenting styles to impact eating and weight through either direct effects or interactions with more proximal predictors like feeding practices. It is possible that impacts on weight may emerge when the child becomes even more autonomous and with the transition to school entry.
In sum, when considering implications of parenting during early childhood, there is evidence to support recommendations to: provide structure (such as a structured eating environment and consistent meal time routines), set limits (such as setting the range of nutrient-dense food options that are available), and incorporate both demandingness and responsiveness into general parenting, to support child development of healthy eating and weight 24.
Middle Childhood
Middle childhood refers to a time in which school-aged children are undergoing a period of tremendous growth in autonomy, identity development, and perceived competence across various domains of development 59,60. With the transition to school comes newfound independence, giving children greater responsibility for what, how much, and whether they eat, while ideally when and where children eat remains structured and fixed. Children’s food preferences are likely well-established in middle childhood, and requests for energy-dense foods high in sugar, sodium, and fat are often at odds with parents’ desires for dietary variety and children’s intake of nutrient-dense foods. Furthermore, self-regulatory capacity and appetitive traits become more established in middle childhood and give rise to more autonomous eating 61. As such, parents’ food parenting strategies should shift towards increasing support for children’s autonomy with continued structure (e.g., establishing rules regarding the purchase of unhealthy foods at school) and responsiveness (e.g., increased child involvement in food shopping and cooking). As shown in Figure 1, with increasing independence in middle childhood, positive food parenting strategies encompass limit-setting and rules regarding food and eating (devoid of harsh psychological or behavioral control and monitoring), along with developmentally appropriate autonomy support, provision of ample opportunities for children to make their own choices, and inclusion of children in decisions about food and eating. With the shift towards increased child autonomy, parents may start to increase their monitoring (tracking and surveillance of child behavior) of the child’s food intake. Parental monitoring has been consistently linked to positive child outcomes in the general parenting literature 62. Monitoring is important as it allows the parent to notice early signs of concerning behavior and to make adjustments accordingly.
Studies linking general parenting styles to obesity in middle childhood suggest that eating behavior, appetitive traits, food parenting practices and other food- or eating-related factors may be potential mechanisms through which parenting influences obesity risk 7. Research has provided evidence for lower rates of emotional eating behaviors in children with authoritative parents, and in children who rate their parent-child relationship as more positive 62. Burke and colleagues 63 measured dietary quality using the Healthy Eating Index in a low-income, food insecure sample of youth ages 9 to 15 years. An authoritative parenting style was associated with greater dietary quality, while authoritarian (controlling) and permissive (indulgent) parenting styles were associated with lower dietary quality. Likewise, findings from related studies showed that both controlling and permissive parenting styles were associated with lower fruit and vegetable consumption and greater consumption of sugar-sweetened beverages 64,65.
Relations between general parenting style and dietary intake and patterns may also be linked to the family mealtime environment. Family mealtimes have been shown to be an important context for family socialization and functioning 66. Mealtimes provide an opportunity for transmission of family routines, values and customs related to food and eating, as well as an opportunity for parents to model healthy eating behaviors and dietary practices. Lopez and colleagues found that in parents of 8- to 12-year-old children, authoritative parenting was associated with the presence of more positive mealtime structural practices (e.g., more frequent family dinners; less eating during television viewing) and reports of greater parent modeling of healthy eating behaviors (e.g., child sees parent eating healthy snacks) 65.
There also is evidence that feeding style has an impact on child weight. In a mixed-methods, cross-sectional study with 174 Mexican parents and their 8- to 10-year-old children 67, parents’ greater use of positive parental involvement practices (e.g., monitoring intake, limiting high-calorie foods) was associated with lower child BMI, whereas restriction of children’s intake was associated with increased child BMI. In a study with 99 rural parents and their children (average age = 9 years), a permissive feeding style was associated with greater energy intake in children, while parents with an authoritative feeding style had children with lower intakes of energy-dense foods 68.
Findings from studies linking feeding styles and food parenting practices to children’s dietary intake and quality are mixed. In a longitudinal study with more than 1200 parent-child dyads in the Netherlands, the authors measured parents’ overt control (e.g., deciding how many snacks the child should have), and covert control (e.g. avoiding buying unhealthy foods) and their relation to weight- and eating-related outcomes in 9-year-olds 69. Greater use of both forms of control was associated with decreased energy-dense snacking and intake of sugar-sweetened beverages, and covert control was related to increased fruit consumption. Moreover, this study provides some evidence that general parenting may moderate the relationship between food parenting and child outcome. Covert control was related to increases in BMI over a 1-year period in children with parents who reported using a high degree of psychological control (e.g., guilt/shame).
Taken together, authoritative parenting styles and positive food parenting strategies, such as involving children in food preparation and cooking and setting limits on food purchased outside the home, are associated with better eating-, dietary- and weight-related outcomes in school-age children. Mixed findings across studies may be due to differences in measures used to assess food parenting practices or styles, differences in diversity or composition of study population, differences in the assessment of general parenting, and/or to the bidirectional nature of parent-child interactions. A small body of work exists that illustrates positive general parenting interventions have effects on child weight status during middle childhood. General parenting interventions in early childhood have demonstrated effects on child weight status in middle childhood57; there is also a version for middle childhood that could be examined Given the continued emergence of autonomy during this developmental period, parents are encouraged to provide more opportunities for children to develop the skills needed to make healthy decisions about food and eating when parents are not present, such as at school and in other settings in which independent eating occurs. With the transition from middle childhood to preadolescence to adolescence, and changing roles of food and eating, a distinct shift in parenting in the eating domain is likely to occur.
Adolescence
Adolescence is a developmental time period marked by both increasing autonomy and decreased parental influence as children begin spending more independent time with peers. As such, the expression of demandingness and responsiveness shifts as children enter into adolescence. Regarding demandingness, parental use of structure and limit setting continues to be important. With respect to responsiveness, parenting that adjusts to the adolescent’s need for increased autonomy can foster the successful development of independence, 70,71 enhance parent-child communication, 72 and may support adolescents’ learning and development of healthful eating (see Figure 1 for examples). Moreover, parental monitoring becomes increasingly important, especially given that parents have less control over structure and limit setting during adolescence due to the continued widening of the child’s ecology (see Figure 1). Some discussion focuses on how and whether the nature of monitoring results in effective adoption of social norms and expectations by adolescents. In the developmental literature, Statin and Kerr 72 suggest that monitoring based in part upon knowledge derived from the adolescent, as opposed to heavy parental surveillance and control, may facilitate better adoption of prosocial behaviors. Whether and how this applies to healthy eating habits is, as yet, undetermined. In addition, there may be a curvilinear relationship between level of monitoring and child outcome; there is emerging evidence that a moderate level of monitoring results in the most positive child outcomes among adolescents with overweight 73, with relationships less clear among those of other weight statuses. Levels of monitoring that are too high (i.e., controlling) can inhibit the adolescent’s ability to develop autonomy. Moderate monitoring involves observance of child eating behaviors, paying attention to any concerning behaviors, and includes direct communication with the adolescent regarding eating choices and behaviors (in a way that is not shameful or judging), and then subsequently adjusting parenting accordingly. Moreover, it is likely that the most helpful level of monitoring for any given child will depend on a number of child characteristics, such as temperament, food responsiveness, and obesity risk.
As part of their increasing independence and the diminution of parent control, adolescents often experience increased responsibilities, such as working a part-time job and spending increased time participating in extracurricular activities. Such activities often result in significant eating outside the family home. To this point, many adolescents decrease their time spent engaging in family meals and start consuming more convenience foods, partially explaining the average decline in overall diet quality from early childhood to adolescence 74. Parents can help counter this decline in diet quality by continuing to provide nutrient-dense foods for their adolescents, though more research is needed to identify whether this approach translates into adoption by the adolescent and subsequent increases in dietary quality.
Cross-sectional studies suggest positive mealtime structure not only supports adolescents’ development and maintenance of healthy eating and weight outcomes but has additional psychological benefits 75–77. Research by Berge and colleagues indicated a positive association between maternal and paternal authoritative parenting style and adolescent-reported family meal frequency 75. However, when results were examined longitudinally, the relationship only persisted with opposite-sex dyads (i.e., mothers and sons, fathers and daughters). While the average family meal frequency often decreases during adolescence, parents can still engage in efforts to make family meals a priority, as there may still be protective benefits to eating together even if less frequently, as family meals have been cross-sectionally associated with lower obesity risk and increased diet quality and fruit and vegetable intake 76,77. Moreover, there is evidence that it is the quality, not quantity, of family meals during adolescence that has an impact on health outcomes 78. However, these relationships need to be confirmed using longitudinal and intervention study designs 79, which are limited to date and have not yet determined whether family meals are causally associated with positive outcomes or the mechanisms by which these effects may occur.
The small body of research examining the influence of general parenting style on adolescent weight status has provided mixed findings. One study by Berge and colleagues reported that an authoritative parenting style was associated with lower BMIs in both daughters and sons 80. Another study identified a unique relationship between parenting style and adolescent weight status. While adolescents of authoritative parents had higher BMI trajectories during adolescence, they had less steep increases in BMI as they transitioned into emerging adulthood 81. This finding indicates that the skills learned via an authoritative parenting style (e.g., increased autonomy and independence that supports adoption of healthy lifestyle behaviors) may be protective against excessive weight gain as children transition out of the family home. As such, it may be that the effects of parenting are not always immediate but may become pronounced during transition periods of increased autonomy. Moreover, there may also be differences based on the sex of the parent and adolescent in the dyad. In one study, maternal parenting style only was related to their adolescent son’s, but not daughter’s, BMI, with no relationship between paternal parenting style and adolescent BMI 82. Unlike the earlier developmental periods where evidence supports that general parenting interventions may have a positive impact on child eating and weight outcomes, limited studies have examined this in adolescence. There was an indirect effect of the Family Check-Up during adolescence (age 12–15) on weight status in young adulthood (age 22). The Family Check-Up increased parent-adolescent relationship quality, which reduced maladaptive eating attitudes, which reduced obesity risk 83.
Less work has examined how general parenting style is associated with adolescent eating behavior. One study investigating the relationship between general parenting style and fruit consumption found that adolescents with an authoritative parent had the greatest fruit intake, followed by adolescents of indulgent parents, with adolescents of authoritarian and neglectful parents consuming the least fruit 84, suggesting a benefit of high responsiveness. However, this finding needs to be replicated in other samples and with other eating- and nutrition-related variables of interest, using longitudinal and randomized study designs.
In sum, during adolescence, parents can continue efforts to focus on structuring the adolescenťs food environment so that it is responsive to their child’s needs (e.g., provision of convenient nutrient-dense foods and being mindful of the availability in the home of foods that undermine healthful eating). Given the increased independence that marks adolescence, monitoring may be especially important during this time.
Discussion
Across all developmental periods, parents play a critical role in the development and maintenance of child eating behavior and weight status. Parents act as key agents of socialization for children’s eating behaviors through their roles as providers (i.e., brings food into the home), models (i.e., shows the child how to eat), and regulators (i.e., decides what to purchase and serve, directs the child’s behavior). While the literature has traditionally focused on the impacts of coercive control in parent feeding on child eating and weight status, researchers have started to shift toward examination of more “positive” facets of food parenting. We use “positive” to refer to general parenting styles, feeding styles, and food parenting practices that are developmentally appropriate and contribute to an effective balance between parental demandingness and responsiveness. This parallels terminology used in the developmental psychology literature, in which there is a robust evidence base on “positive parenting” approaches that promote adaptive child outcomes more broadly. We aimed to build upon a history of the parenting literature from the developmental sciences influencing the study of child feeding, adopting a strengths-based perspective in considering ways that parents can actively support the development of healthy eating behaviors and weight trajectories, and incorporating learnings from evidence-based general parenting interventions alongside our consideration of food parenting specifically. While there is evidence in support of many of the positive practices and styles highlighted in Table 1, many opportunities remain to build upon the extant research and expand the extent to which we can leverage what is known about positive parenting to promote healthy child outcomes across various periods of child development and sociodemographic groups (Table 2).
Table 2.
Recommendations for Future Research on Positive Food Parenting
| 1. Improve Measurement of Key Constructs |
| 1a. Operationalize and investigate positive food parenting constructs (e.g., structure and limit setting) via observational assessments |
| 1b. Develop additional objective measures of child eating behavior |
| 1c. Develop measures that are developmentally appropriate across several age groups, allowing for comparison over time |
| 1d. Evaluate the cultural appropriateness and relevant of measures in diverse populations |
| 1e. Validate of measures of positive food parenting and child eating behavior in diverse populations |
| 2. Expand Research on Understudied Aspects of Positive Food Parenting |
| 2a. Examine possible associations between weaning approaches (e.g., baby-led weaning) and eating and weight outcomes during infancy |
| 2b. Better understand the nature and role of parental monitoring in promoting healthy eating behaviors during middle childhood, and adolescence |
| 2c. Determine, through longitudinal and intervention studies, whether family meals are causally associated with positive child eating and weight outcomes during early childhood, middle childhood, and adolescence |
| 2d. Expand the body of research examining impacts of positive food parenting and general parenting on eating behaviors and weight status during middle childhood and adolescence |
| 2e. Across all developmental periods, increase the number of studies that include (or exclusively focus on) fathers and other non-maternal caregivers, single parents, and same-gender parents |
| 3. Conduct Longitudinal Research to Understand Stability vs. Change in Positive Food Parenting across Development |
| 3a. Understand stability vs. change in caregivers’ feeding practices and styles across early feeding modes, including breastfeeding, bottle-feeding, and introduction to complementary foods |
| 3b. Understand stability vs. change in feeding practices and styles across infancy, early childhood, middle childhood, and adolescence |
| 3c. Identify potential predictors and impacts of stability vs. change in feeding practices and styles across development |
| 4. Employ Longitudinal and Experimental Designs to Understand Bidirectional Associations and Causality |
| 4a. Across all developmental stages, examine directionality and causality in the context of longitudinal and interventional designs to clarify the bidirectional nature of the parent-child relationship within feeding and eating contexts |
| 5. Further Examine Possible Mediators and Moderators of Effects of Positive Food Parenting |
| 5a. Consider child temperament or appetitive traits as moderators or mediators of how parenting influences child eating and weight outcomes |
| 5b. Understand whether and how parental weight status mediates or moderates effects of parenting styles and practices |
| 5c. Incorporate measures of both food-specific parenting and general parenting to better understand how general parenting practices and styles may mediate or moderate effects of food-specific practices and styles on child feeding and weight outcomes |
| 5d. Examine the implications of positive parent practices and styles among diverse socioeconomic and racial/ethnic groups, single parents, same-gender parents, and fathers |
| 6. Develop and Evaluate Evidence-Based Interventions to Promote Positive Food Parenting at Specific Developmental Stages and Across all Stages |
| 6a. Identify evidence-based strategies for promoting responsive feeding among mothers and other caregivers (e.g., fathers, day care providers) to infants |
| 6b. Examine the potential of existing positive parenting programs to improve children’s and adolescents’ eating- and weight-related outcomes |
| 6c. Develop and evaluate multifactorial interventions that blend the fields of developmental and obesity sciences to understand how to promote positive food parenting and healthy eating and weight-related outcomes |
In addition to evidence within specific developmental periods, findings from the few longitudinal studies spanning developmental periods indicate that general parenting style in early life may have implications for future child weight status. For example, high maternal sensitivity during the first three years of life appears to be protective against obesity at age 15 years 52. Other work indicates that interactions between parenting style and child self-regulation in early life have implications for weight status in adolescence 85. Among boys with poorer abilities to delay gratification at age 4, having a mother with an authoritarian parenting style increased risk for an elevated weight status at age 15. Hence, the influence of early parenting on child eating and weight outcomes may not be observed until later in development, emphasizing the need for more longitudinal studies that measure parenting, potential mediators, and weight status across developmental stages. In particular, many of the studies on parenting and eating/weight outcomes during middle childhood and adolescence are cross-sectional, precluding the ability to draw conclusions about the bidirectional parent-child feeding relationship. Future research in this area should continue to move toward examining directionality and causality in the context of longitudinal, experimental, and interventional designs, which are critical to clarify the interplay of parenting styles, feeding styles, food parenting practices, and child outcomes. Moreover, rigorous operationalization of the bidirectional nature of the parent-child relationship is needed, as well as operationalization and investigation of positive parenting constructs and eating behaviors that may mediate links between parenting and weight. As such, there is a need to continue to develop and invest in experimental and objective measures of eating behavior so that research does not rely mostly on parent- and self-reported dietary intake. Another measurement issue that the field will need to address is the paucity of measures that are developmentally appropriate across several age groups, allowing for comparison over time. It is also recommended that future research prioritize use of observational measures of parenting, with a consideration of the appropriateness and validity of these and other measures in diverse contexts, as described below.
Other potential areas of focus for future research are to build the evidence base in areas in which the evidence is more limited (see Table 2, part 2). More recently, a movement in the field to study food parenting and general parenting together has been initiated 86–88, which may help clarify relationships between the two. General parenting may serve as a moderator or mediator of the impact of food parenting on weight and eating behaviors. Alternatively, for some groups differing in sex, gender, SES, and race/ethnicity, there might be direct effects of parenting style, whereas for others parenting style might moderate impacts of specific practices. To further elucidate the role of general parenting styles, food parenting research could also leverage knowledge learned from developmental science. Interventions targeting general parenting (e.g., parental warmth and sensitivity, limit setting, autonomy support) have been shown to be efficacious in reducing children’s BMI and weight-related eating and activity behaviors 89 with potential effects extending into adulthood 90. Less is known about impacts of these more general parenting interventions among adolescents. . Future research is needed to better understand the interplay between general parenting styles and specific food parenting practices during early childhood, including studies of families from various sociodemographic and cultural backgrounds, given some evidence that SES and race/ethnicity may moderate impacts of parenting style on weight 91.
In addition, other potential moderators of the impact of parenting on child eating and weight include child temperament and appetitive traits. This child factors can be examined as potential moderators in analyses or can be considered in implementation of interventions in the first place. During infancy, interventions have been developed that promote responsive parenting to all participating families, regardless of variability in factors such as child cues or temperament. Yet this variability is acknowledged within the intervention approach itself by teaching about temperament, giving examples of child hunger/fullness cues, and demonstrating responses to these cues in the moment with the target child 92. These positive parenting interventions have led to improvements in both infant dietary patterns 50 and weight status which have persisted into early childhood 49. Moreover, this general parenting intervention also resulted in greater maternal use of responsive food parenting 93.
SES and cultural influences may play a large role in feeding but often not captured or are confounded in past research. Further, while there are an increasing number of studies in underrepresented and under-resourced populations, the majority of evidence to date is based on predominantly white and well-resourced samples. Mixed findings in the extant literature may be driven, in part, by the failure to reflect cultural and socioeconomic diversity. This issue likely also impacts the sensitivity of existing measurement tools to these influences. Work in low-income Black and Hispanic samples has reported poor fit when testing for factorial invariance with common measures of parent feeding practices 94,95, suggesting that further clarification of the cultural appropriateness and relevance of these measures should be undertaken. Further, the experience of food insecurity and/or low SES may alter food availability, which may influence feeding style or food parenting practices in a way that cannot be captured with most existing measurement tools. Two notable exceptions to this are the Caregiver Feeding Styles Questionnaire 10, which was developed for use with low-income minority parents, and the Parenting around SNAcking Questionnaire 96, which was developed using qualitative studies with low-income White, Black, and Hispanic mothers of preschoolers. In addition, researchers are beginning to examine the effectiveness of parenting interventions in more diverse samples that may be at increased risk for developing obesity. Current work is investigating whether an adaptation of a responsive parenting intervention that was effective among a mostly-white population can prevent rapid infant weight gain among first-time Black parents 97. However, much more additional research is needed in diverse samples to elucidate the relationships between race, SES, general parenting, food parenting, and child eating and weight outcomes.
Another overarching challenge within the field of food parenting research is the underrepresentation of fathers 98. While half of published studies in food parenting research have included fathers, most data from these studies have been reported by the mother, with fathers making up only 17% of study participants 98. There are a variety of reasons for this, including that mothers are more likely the primary caregiver and able to attend research visits, and that mothers are often in charge, or perceived to be in charge, of child feeding. However, given that there may be gender-specific associations of parenting on child eating and weight outcomes 82, and that multiple primary caregivers can influence the child’s weight status 99, it is vital to collect data on both caregivers in dual-parent households to help elucidate the relationship between food parenting and child eating and weight outcomes. In addition, given the known relationship between parental and child weight status2, it is critical to collect and include both paternal and maternal child weight status when examining associations between parenting and child weight status. Moreover, there is paucity of research among single parents or same-gender parents.
In conclusion, research supports the use of general parenting styles, feeding styles, and food parenting practices that are high in both responsiveness and demandingness, with benefits seen for both eating behavior and weight status across the developmental spectrum. While promotion of early positive parenting shows promise, controlling practices are a common well-intentioned response to concern about actual or perceived obesity risk 5. Parents will likely need tools and resources to replace controlling parenting practices with positive parenting practices. Parents can benefit from anticipatory guidance on responsive feeding and the use of structure and limit setting early in the child’s life to prevent the use of overt restriction and other controlling feeding practices. The existing evidence can inform continued development of related interventions and materials, and future research can build on current evidence by broadening the populations under study (e.g., fathers, single parents, same gender parents, culturally and socioeconomically-diverse samples), incorporating longitudinal follow-up and consideration of potential effect moderators, and leveraging intervention research, including well-established general parenting interventions from the developmentally sciences, to bolster internal validity. Interdisciplinary collaboration between developmental and obesity sciences offers the potential to better understand how positive parenting may benefit both physical and socioemotional well-being and the mechanisms through which this might occur. Continuing to bolster the research in this area can further scientific understanding of how to help support parents and caregivers and promote healthier outcomes among populations at greatest risk.
Acknowledgements
The authors would like to thank Dr. Leann Birch for her invaluable mentorship. As a trailblazer in this field, much of the research cited here can be traced back to Leann’s influence. Dr. Birch continues to be a source of inspiration for many researchers in this field, including the authorship team. The authors would also like to thank Dr. Madeleine Sigman-Grant for her critical feedback. This work was supported by K01 DK120778 (KNB).
Footnotes
Conflicts of Interest
The authors report no conflict of interest.
References
- 1.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. Jama. 2018;319(16):1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faith MS, Van Horn L, Appel LJ, et al. Evaluating parents and adult caregivers as “agents of change” for treating obese children: evidence for parent behavior change strategies and research gaps: a scientific statement from the American Heart Association. Circulation. 2012;125(9):1186–1207. [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. New England journal of medicine. 1997;337(13):869–873. [DOI] [PubMed] [Google Scholar]
- 4.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(Supplement 2):539–549. [PubMed] [Google Scholar]
- 5.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. The Journal of law, medicine & ethics. 2007;35(1):22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vollmer RL, Mobley AR. Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight. A review. Appetite. 2013;71:232–241. [DOI] [PubMed] [Google Scholar]
- 7.Vaughn AE, Ward DS, Fisher JO, et al. Fundamental constructs in food parenting practices: a content map to guide future research. Nutrition reviews. 2016;74(2):98–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes SO, Frankel LA, Beltran A, et al. Food parenting measurement issues: working group consensus report. Child Obes. 2013;9 Suppl(Suppl 1):S95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baumrind D Current patterns of parental authority. Developmental psychology. 1971;4(1p2):1. [Google Scholar]
- 10.Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. [DOI] [PubMed] [Google Scholar]
- 11.Maccoby E, Martin A. Socialization in the context of the family: parent-child interactions. Hetherington EM & Mussen PH (eds.). Socialization, personality and social development. Handbook of child psychology, Vol. IV. Cap. 9: 1–102. New York: Wiley; 1983. [Google Scholar]
- 12.Larsen JK, Sleddens EF, Vink JM, Fisher JO, Kremers SP. General parenting styles and children's obesity risk: Changing focus. Frontiers in psychology. 2018;9:2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darling N, Steinberg L. Parenting style as context: An integrative model. Psychological bulletin. 1993;113(3):487. [Google Scholar]
- 14.Bornstein MH. Positive parenting and positive development in children. Handbook of applied developmental science: Promoting positive child, adolescent, and family development through research, policies, and programs. 2003;1:187–209. [Google Scholar]
- 15.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201–210. [DOI] [PubMed] [Google Scholar]
- 16.Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. Journal of pediatric psychology. 2007;32(8):960–972. [DOI] [PubMed] [Google Scholar]
- 17.Thompson AL, Mendez MA, Borja JB, Adair LS, Zimmer CR, Bentley ME. Development and validation of the infant feeding style questionnaire. Appetite. 2009;53(2):210–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savage JS, Rollins BY, Kugler KC, Birch LL, Marini ME. Development of a theory-based questionnaire to assess structure and control in parent feeding (SCPF). International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Power TG, Johnson SL, Beck AD, Martinez AD, Hughes SO. The Food Parenting Inventory: Factor structure, reliability, and validity in a low-income, Latina sample. Appetite. 2019;134:111–119. [DOI] [PubMed] [Google Scholar]
- 20.Heller RL, Mobley AR. Instruments assessing parental responsive feeding in children ages birth to 5 years: A systematic review. Appetite. 2019. [DOI] [PubMed] [Google Scholar]
- 21.Grolnick WS, Pomerantz EM. Issues and Challenges in Studying Parental Control: Toward a New Conceptualization. Child Development Perspectives. 2009;3(3):165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ventura AK, Birch LL. Does parenting affect children's eating and weight status? International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. The Journal of nutrition. 2011;141(3):490–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eneli IU, Crum PA, Tylka TL. The trust model: a different feeding paradigm for managing childhood obesity. Obesity. 2008;16(10):2197. [DOI] [PubMed] [Google Scholar]
- 25.Fomon SJ, Filer LJ Jr., Thomas LN, Anderson TA, Nelson SE. Influence of formula concentration on caloric intake and growth of normal infants. Acta Pediatrica Scandinavica. 1975;64(2):172–181. [DOI] [PubMed] [Google Scholar]
- 26.Cohen RJ, Brown KH, Canahuati J, Rivera LL, Dewey KG. Effects of age of introduction of complementary foods on infant breast milk intake, total energy intake, and growth: a randomised intervention study in Honduras. Lancet. 1994;344(8918):288–293. [DOI] [PubMed] [Google Scholar]
- 27.Brugaillères P, Issanchou S, Nicklaus S, Chabanet C, Schwartz C. Caloric compensation in infants: developmental changes around the age of 1 year and associations with anthropometric measurements up to 2 years. The American journal of clinical nutrition. 2019;109(5):1344–1352. [DOI] [PubMed] [Google Scholar]
- 28.Perez-Escamilla R, Segura-Perez S, Lott M, on behalf of the RWJF HER Expert Panel on Best Practices for Promoting Healthy Nutrition FP, and Weight Status for Infants and Toddlers from Birth to 24 Months. Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approach. Durham, NC: Healthy Eating Research. Available at: healthyeatingresearch.org.;2017. [Google Scholar]
- 29.Brown A, Lee M. Breastfeeding is associated with a maternal feeding style low in control from birth. PloS one. 2013;8(1):e54229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cernadas JM, Noceda G, Barrera L, Martinez AM, Garsd A. Maternal and perinatal factors influencing the duration of exclusive breastfeeding during the first 6 months of life. Journal of human lactation : official journal of International Lactation Consultant Association. 2003;19(2):136–144. [DOI] [PubMed] [Google Scholar]
- 31.Ventura AK. Associations between Breastfeeding and Maternal Responsiveness: A Systematic Review of the Literature. Adv Nutr. 2017;8(3):495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ventura AK, Terndrup H. Breasts versus bottles for infant feeding: Whaťs the difference? In: Worobey J, ed. Infant Feeding: Parental Perceptions, Behaviors, and Health Effects. Hauppauge, NY: Nova Publishers; 2016:103–128. [Google Scholar]
- 33.Brown A, Lee M. Breastfeeding is associated with a maternal feeding style low in control from birth. PloS one. 2013;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright P, Fawcett J, Crow R. The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behavioural Processes. 1980;5(1):1–20. [DOI] [PubMed] [Google Scholar]
- 35.Ventura AK, Mennella JA. An experimental approach to study individual differences in infants' intake and satiation behaviors during bottle-feeding. Child Obes. 2017;13(1):44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ventura AK, Hernandez A. Effects of opaque, weighted bottles on maternal sensitivity and infant intake. Matern Child Nutr. 2019;15(2):e12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bever Babendure J, Reifsnider E, Mendias E, Moramarco MW, Davila YR. Reduced breastfeeding rates among obese mothers: a review of contributing factors, clinical considerations and future directions. International breastfeeding journal. 2015;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson SL, Hayes JE. Developmental Readiness, Caregiver and Child Feeding Behaviors, and Sensory Science as a Framework for Feeding Young Children. Nutrition Today. 2017;52(2):S30–S40. [Google Scholar]
- 39.Anzman-Frasca S, Ventura AK, Ehrenberg S, Myers KP. Promoting healthy food preferences from the start: A narrative review of food preference learning from the prenatal period through early childhood. Obes Rev. 2018. [DOI] [PubMed] [Google Scholar]
- 40.D'Auria E, Bergamini M, Staiano A, et al. Baby-led weaning: what a systematic review of the literature adds on. Italian journal of pediatrics. 2018;44(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brown A, Lee MD. Early influences on child satiety-responsiveness: the role of weaning style. Pediatric Obesity. 2015;10(1):57–66. [DOI] [PubMed] [Google Scholar]
- 42.Brown A, Lee M. A descriptive study investigating the use and nature of baby‐led weaning in a UK sample of mothers. Maternal & child nutrition. 2011;7(1):34–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lakshman R, Clifton EA, Ong KK. Baby-Led Weaning-Safe and Effective but Not Preventive of Obesity. JAMA pediatrics. 2017;171(9):832–833. [DOI] [PubMed] [Google Scholar]
- 44.Coulthard H, Harris G, Fogel A. Exposure to vegetable variety in infants weaned at different ages. Appetite. 2014;78:89–94. [DOI] [PubMed] [Google Scholar]
- 45.Greer FR, Sicherer SH, Burks AW. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of allergenic complementary foods. Pediatrics. 2019;143(4):e20190281. [DOI] [PubMed] [Google Scholar]
- 46.National Academies of Sciences E, Medicine. Feeding Infants and Children from Birth to 24 Months: Summarizing Existing Guidance. Washington, DC: The National Academies Press; 2020. [PubMed] [Google Scholar]
- 47.DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. Int J Obes (Lond). 2011;35(4):480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spill MK, Callahan EH, Shapiro MJ, et al. Caregiver feeding practices and child weight outcomes: a systematic. Am J Clin Nutr. 2019;109(Suppl):990S–1002S. [DOI] [PubMed] [Google Scholar]
- 49.Paul IM, Savage JS, Anzman-Frasca S, et al. Effect of a responsive parenting educational intervention on childhood weight outcomes at 3 years of age: the INSIGHT randomized clinical trial. Jama. 2018;320(5):461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hohman EE, Paul IM, Birch LL, Savage JS. INSIGHT responsive parenting intervention is associated with healthier patterns of dietary exposures in infants. Obesity. 2017;25(1):185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mallan KM, Jansen E, Harris H, Llewellyn C, Fildes A, Daniels LA. Feeding a fussy eater: examining longitudinal bidirectional relationships between child fussy eating and maternal feeding practices. Journal of pediatric psychology. 2018;43(10):1138–1146. [DOI] [PubMed] [Google Scholar]
- 52.Anderson SE, Sacker A, Whitaker RC, Kelly Y. Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. International Journal of Obesity. 2017;41(10):1459–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lane SP, Bluestone C, Burke CT. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. British journal of health psychology. 2013;18(1):66–82. [DOI] [PubMed] [Google Scholar]
- 54.Fisher JO, Serrano EL, Foster GD, et al. Efficacy of a food parenting intervention for mothers with low income to reduce preschooler’s solid fat and added sugar intakes: a randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2019;16(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of abnormal child psychology. 2008;36(4):567–589. [DOI] [PubMed] [Google Scholar]
- 56.Brotman LM, Dawson-McClure S, Huang K-Y, et al. Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics. 2012;129(3):e621–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith JD, Montaño Z, Dishion TJ, Shaw DS, Wilson MN. Preventing weight gain and obesity: Indirect effects of the family check-up in early childhood. Prevention Science. 2015;16(3):408–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lumeng JC, Miller AL, Horodynski MA, et al. Improving Self-regulation for Obesity Prevention in Head Start: A Randomized Controlled Trial. Pediatrics. 2017. [DOI] [PubMed] [Google Scholar]
- 59.Erikson E Childhood and Society.(rev. ed.) Harmondsworth. England: Penguin. 1963. [Google Scholar]
- 60.Eccles JS. The development of children ages 6 to 14. The future of children. 1999:30–44. [PubMed] [Google Scholar]
- 61.Francis LA, Riggs NR. Executive function and self-regulatory influences on Children's eating. Pediatric food preferences and eating behaviors: Elsevier; 2018:183–206. [Google Scholar]
- 62.Topham GL, Hubbs-Tait L, Rutledge JM, et al. Parenting styles, parental response to child emotion, and family emotional responsiveness are related to child emotional eating. Appetite. 2011;56(2):261–264. [DOI] [PubMed] [Google Scholar]
- 63.Burke MP, Jones SJ, Frongillo EA, Blake CE, Fram MS. Parenting styles are associated with overall child dietary quality within low-income and food-insecure households. Public health nutrition. 2019;22(15):2835–2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Langer SL, Seburg E, JaKa MM, Sherwood NE, Levy RL. Predicting dietary intake among children classified as overweight or at risk for overweight: Independent and interactive effects of parenting practices and styles. Appetite. 2017;110:72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lopez NV, Schembre S, Belcher BR, et al. Parenting styles, food-related parenting practices, and children's healthy eating: A mediation analysis to examine relationships between parenting and child diet. Appetite. 2018;128:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fiese BH, Foley KP, Spagnola M. Routine and ritual elements in family mealtimes: Contexts for child well‐being and family identity. New directions for child and adolescent development. 2006;2006(111):67–89. [DOI] [PubMed] [Google Scholar]
- 67.Tschann JM, Gregorich SE, Penilla C, et al. Parental feeding practices in Mexican American families: initial test of an expanded measure. The international journal of behavioral nutrition and physical activity. 2013;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hennessy E, Hughes SO, Goldberg JP, Hyatt RR, Economos CD. Parent behavior and child weight status among a diverse group of underserved rural families. Appetite. 2010;54(2):369–377. [DOI] [PubMed] [Google Scholar]
- 69.Rodenburg G, Kremers SP, Oenema A, van de Mheen D. Associations of parental feeding styles with child snacking behaviour and weight in the context of general parenting. Public Health Nutrition. 2014;17(5):960–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen Y, Haines J, Charlton BM, VanderWeele TJ. Positive parenting improves multiple aspects of health and well-being in young adulthood. Nature human behaviour. 2019;3(7):684–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Coatsworth JD, Duncan LG, Greenberg MT, Nix RL. Changing Parenťs Mindfulness, Child Management Skills and Relationship Quality With Their Youth: Results From a Randomized Pilot Intervention Trial. Journal of child and family studies. 2010;19(2):203–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child development. 2000;71(4):1072–1085. [DOI] [PubMed] [Google Scholar]
- 73.Mellin AE, Neumark-Sztainer D, Story M, Ireland M, Resnick MD. Unhealthy behaviors and psychosocial difficulties among overweight adolescents: the potential impact of familial factors. Journal of Adolescent Health. 2002;31(2):145–153. [DOI] [PubMed] [Google Scholar]
- 74.Lytle LA, Seifert S, Greenstein J, McGovern P. How do children's eating patterns and food choices change over time? Results from a cohort study. American journal of health promotion. 2000;14(4):222–228. [DOI] [PubMed] [Google Scholar]
- 75.Berge JM, Wall M, Neumark-Sztainer D, Larson N, Story M. Parenting Style and Family Meals: Cross-Sectional and 5-Year Longitudinal Associations. Journal of the American Dietetic Association. 2010;110(7):1036–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fulkerson JA, Neumark‐Sztainer D, Hannan PJ, Story M. Family meal frequency and weight status among adolescents: cross‐sectional and 5‐year longitudinal associations. Obesity. 2008;16(11):2529–2534. [DOI] [PubMed] [Google Scholar]
- 77.Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. Journal of the American Dietetic Association. 2007;107(9):1502–1510. [DOI] [PubMed] [Google Scholar]
- 78.Dallacker M, Hertwig R, Mata J. Quality matters: A meta-analysis on components of healthy family meals. Health Psychology. 2019;38(12):1137. [DOI] [PubMed] [Google Scholar]
- 79.Middleton G, Golley R, Patterson K, Le Moal F, Coveney J. What can families gain from the family meal? A mixed-papers systematic review. Appetite. 2020;153:104725. [DOI] [PubMed] [Google Scholar]
- 80.Berge JM, Wall M, Loth K, Neumark-Sztainer D. Parenting style as a predictor of adolescent weight and weight-related behaviors. Journal of Adolescent Health. 2010;46(4):331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fuemmeler BF, Yang C, Costanzo P, et al. Parenting styles and body mass index trajectories from adolescence to adulthood. Health Psychology. 2012;31(4):441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Berge JM, Wall M, Bauer KW, Neumark‐Sztainer D. Parenting characteristics in the home environment and adolescent overweight: A latent class analysis. Obesity. 2010;18(4):818–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Van Ryzin MJ, Nowicka P. Direct and indirect effects of a family-based intervention in early adolescence on parent− youth relationship quality, late adolescent health, and early adult obesity. Journal of Family Psychology. 2013;27(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kremers SP, Brug J, de Vries H, Engels RC. Parenting style and adolescent fruit consumption. Appetite. 2003;41(1):43–50. [DOI] [PubMed] [Google Scholar]
- 85.Connell LE, Francis LA. Positive parenting mitigates the effects of poor self-regulation on body mass index trajectories from ages 4–15 years. Health Psychology. 2014;33(8):757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Patrick H, Hennessy E, McSpadden K, Oh A. Parenting styles and practices in children's obesogenic behaviors: scientific gaps and future research directions. Childhood obesity. 2013;9(s1):S-73–S-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kremers S, Sleddens E, Gerards S, et al. General and food-specific parenting: measures and interplay. Childhood obesity. 2013;9(s1):S-22–S-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jennings KM, Loth KA, Tate AD, Miner MH, Berge JM. Application of latent profile analysis to define subgroups of parenting styles and food parenting practices. Appetite. 2019;139:8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.West F, Sanders MR, Cleghorn GJ, Davies PS. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behaviour research and therapy. 2010;48(12):1170–1179. [DOI] [PubMed] [Google Scholar]
- 90.Brody GH, Yu T, Miller GE, Ehrlich KB, Chen E. Preventive parenting intervention during childhood and young black adults’ unhealthful behaviors: a randomized controlled trial. Journal of Child Psychology and Psychiatry. 2019;60(1):63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mech P, Hooley M, Skouteris H, Williams J. Parent‐related mechanisms underlying the social gradient of childhood overweight and obesity: a systematic review. Child: care, health and development. 2016;42(5):603–624. [DOI] [PubMed] [Google Scholar]
- 92.Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Mindell JA, Birch LL. INSIGHT responsive parenting intervention and infant sleep. Pediatrics. 2016;138(1):e20160762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Savage JS, Hohman EE, Marini ME, Shelly A, Paul IM, Birch LL. INSIGHT responsive parenting intervention and infant feeding practices: randomized clinical trial. International Journal of Behavioral Nutrition and Physical Activity. 2018;15(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Boles RE, Nelson TD, Chamberlin LA, et al. Confirmatory factor analysis of the Child Feeding Questionnaire among low-income African American families of preschool children. Appetite. 2010;54(2):402–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kong A, Vijayasiri G, Fitzgibbon ML, Schiffer LA, Campbell RT. Confirmatory factor analysis and measurement invariance of the Child Feeding Questionnaire in low-income Hispanic and African-American mothers with preschool-age children. Appetite. 2015;90:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Davison K, Blake C, Kachurak A, et al. Development and preliminary validation of the Parenting around SNAcking Questionnaire (P-SNAQ). Appetite. 2018;125:323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lavner JA, Stansfield BK, Beach SR, Brody GH, Birch LL. Sleep SAAF: a responsive parenting intervention to prevent excessive weight gain and obesity among African American infants. BMC pediatrics. 2019;19(1):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Davison KK, Gicevic S, Aftosmes-Tobio A, et al. Fathers’ representation in observational studies on parenting and childhood obesity: a systematic review and content analysis. American Journal of Public Health. 2016;106(11):e14–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. The American journal of clinical nutrition. 2010;91(6):1560–1567. [DOI] [PubMed] [Google Scholar]