Abstract
Isolation of bacterial small colony variants (SCVs) from clinical specimens is not uncommon and can fundamentally change the outcome of the associated infections. Bacterial SCVs often emerge with their normal colony phenotype (NCV) co-isolates in the same sample. The basis of SCV emergence in vivo is not well understood in Gram-negative bacteria. In this study, we interrogated the causal genetic lesions of SCV growth in three pairs of NCV and SCV co-isolates of Escherichia coli, Citrobacter freundii, and Enterobacter hormaechei. We confirmed SCV emergence was attributed to limited genomic mutations: 4 single nucleotide variants in the E. coli SCV, 5 in C. freundii, and 8 in E. hormaechei. In addition, a 10.2 kb chromosomal segment containing 11 genes was deleted in the E. hormaechei SCV isolate. Each SCV had at least one coding change in a gene associated with bacterial oxidative respiration and another involved in iron capture. Chemical and genetic rescue confirmed defects in heme biosynthesis for E. coli and C. freundii and lipoic acid biosynthesis in E. hormaachei were responsible for the SCV phenotype. Prototrophic growth in all 3 SCV Enterobacteriaceae species was unaffected under anaerobic culture conditions in vitro, illustrating how SCVs may persist in vivo.
Subject terms: Clinical microbiology, Microbial communities
Introduction
To survive in the hostile host environment, bacteria may take two separate paths. The first and most commonly discussed is an arms race of iron competition and acquisition of antimicrobial resistance genes and pathogenicity factors1–3. The alternative path is to adapt to persist through reductions in metabolic needs and an attenuated growth rate. The isolates that display this alternative phenotype are known as small colony variants (SCVs). Bacterial SCVs were first described in Salmonella typhi over a hundred years ago, prior to the antibiotic era4. Isolation of SCVs is especially common in recurrent or persistent infections involving the respiratory tract, urinary tract, mid-ear, foreign body-related implants, and bone and joint5–7. Emergence of bacterial SCVs from normal colony phenotype (NCV) parental isolates has been described in various clinical settings4. Previously characterized bacterial SCV species include Staphylococcus aureus, Escherichia coli, Neisseria gonorrhoeae, Stenotrophomonas maltophilia, Enterococcus, and Salmonella8–12. In addition to their decreased growth rate, bacterial SCV isolates are characterized by auxotrophism for components directly involved in the electron transfer chain, such as heme and menaquinone. SCVs may also display a nutritional dependency on thymidine or methionine8,13. From a treatment perspective, SCVs display a reduced response to antibiotics despite not carrying the associated antimicrobial resistance genes4,6,14,15. These degenerative changes allow SCVs to persist in vivo in the unique environment and selection pressures of the infected host.
SCVs have been best characterized among S. aureus isolates. Common gene lesions in S. aureus SCVs have been seen in the heme, menaquinone, and thymidine biosynthetic pathways6,7. In clinical strains, disruptions in menaquinone biosynthesis have been associated with mutations in menB, menC, menE and menF16. Laboratory-derived SCV S. aureus, Salmonella typhimurium, or E. coli with hemA, hemB, hemD, hemL, lipA, or ctaA mutations have been used for functional characterization of their changes in growth, metabolism, antimicrobial susceptibility, host invasion, and persistence17–21. In addition, mutations in transcriptional regulators in Staphylococcus spp. governing bacterial virulence factor expression, such as agr, sarA, sigB, and relA, have also been detected, suggesting attenuated cytotoxicity may enable bacterial persistence7,15,22,23. However, the basis of SCV formation and persistence in clinical isolates of Gram-negative bacteria has been less well characterized10,24.
Laboratory recognition, isolation, characterization and appropriate report of bacterial SCVs have suffered from a lack of established standards or guidelines. We previously reported a method practical in clinical laboratories for recognition and phenotypic characterization of SCV S. maltophilia from airway secretions of CF patients8. Our lab has since implemented a systematic, culture-based approach that checks not only for colony variation in size, texture, color, or hemolysis, but also inability to grow on the standard Mueller–Hinton (MH) medium for susceptibility testing. Using this systematic approach, we identified 3 pairs of clinical NCV and SCV Enterobacteriaceae co-isolates from blood and urine cultures. We then used whole genome sequencing to screen for the molecular mechanisms distinguishing the SCVs from their NCV co-isolates. Confirmatory chemical and genetic rescues were performed on the SCVs to determine which mutations were causal for the altered phenotype.
Methods
Isolation and characterization of SCV and NCV from clinical samples
This study was approved by Seattle Children’s Hospital Institutional Review Board with a consent waiver. Three clinical NCV and SCV co-isolate pairs of Escherichia coli, Citrobacter freundii, and Enterobacter hormaechei were obtained from urine or blood cultures. Colony variants were separated by sub-cultures and bacterial species identification was performed using MALDI-TOF (Bruker biotyper, Bruker Daltonics, Inc.). Of note, the SCVs isolates described here did not grow on Mueller–Hinton agar and, thus, were reported in the patient’s clinical record without antimicrobial susceptibility.
Case histories
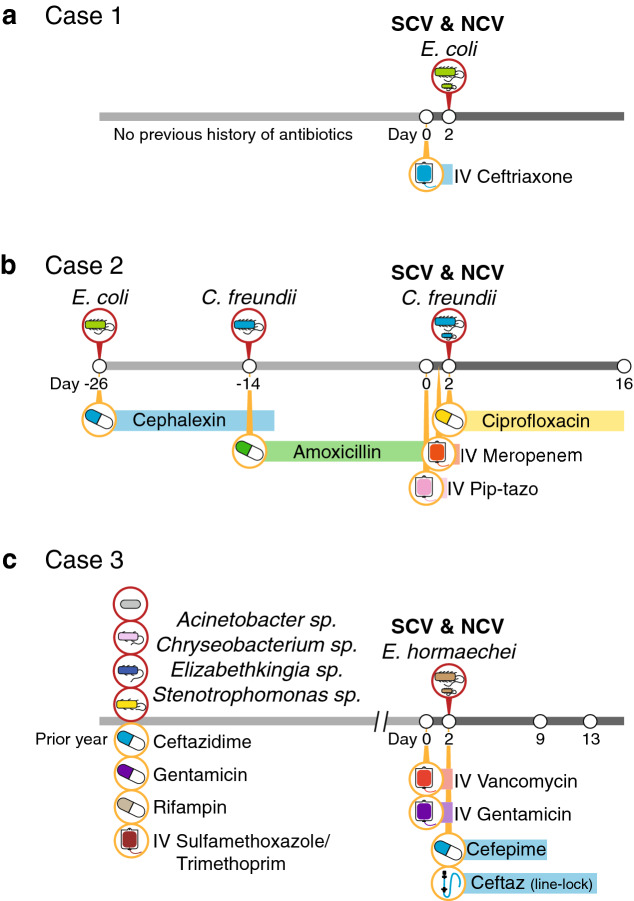
Case 1—A previously healthy 6-week-old male with no history of hospitalization or receipt of antibiotics, presented to the emergency department with fever. His white blood cell count was elevated at 21,600/ml and a 2 + urine leukocyte esterase at the time of emergency visit. The patient was admitted for a rule-out sepsis workup and the patient was started on empiric ceftriaxone. Urine cultures grew 103–104 cfu/mL Escherichia coli and 103–104 cfu/mL SCV Escherichia coli. It was felt the urine culture did not support the diagnosis of UTI, and no additional antibiotics were indicated. The patient recovered fully.
Case 2—A 2-month-old female with right duplicated collection system presented to the emergency department with fever and foul-smelling urine. The patient had experienced two urinary tract infections (UTIs) in the previous month (Escherichia coli and Citrobacter spp.) that were treated with amoxicillin and cephalexin, respectively. Given that the patient was currently receiving antibiotics for the previous Gram-negative UTI, the decision was made to admit the patient for likely IV antibiotic treatment, and the patient was started on empiric piperacillin-tazobactam. Her urine leukocyte esterase was 3 + with elevated red and white blood cells in urine at the time of culture. Urine cultures grew > 105 cfu/mL Citrobacter spp. and 5 × 104–105 cfu/mL SCV Citrobacter spp. and therapy was switched to ciprofloxacin. The patient completed 14 days of therapy and recovered fully.
Case 3—A 6 year-old male with end stage renal disease managed with renal dialysis presented to dialysis clinic with fever, hypotension, and tachycardia. The patient had a history of multiple bloodstream infections treated with ceftazidime, rifampin, gentamicin, or intravenous trimethoprim-sulfamethoxazole. The patient was admitted to the hospital and started on empiric vancomycin and gentamicin. Blood cultures grew out Enterobacter cloacae and SCV Enterobacter cloacae by MALDI-TOF and therapy was switched to cefepime. Additionally, the patient received ceftazidime line-lock therapy. The patient completed treatment and recovered fully. Though the isolates were resulted out as E. cloacae, they were later identified as E. hormaechei based on whole genome sequencing.
Whole genome sequencing of isolates
Whole genome sequencing and assembly of the resulting sequencing reads for the NCV and SCV co-isolates were performed as previously described25,26. Briefly, DNA was extracted from using the MoBio UltraClean Microbial DNA Isolation kit. DNA was diluted to 1 ng/uL and tagmented using quarter-volume reactions of Nextera XT with 15 cycles of PCR amplification. Libraries were sequenced on a 2 × 300 bp run on an Illumina MiSeq to achieve > 1 million paired-end reads per sample. Reads were quality and adapter-trimmed using cutadapt (Q30) and de novo assembled using SPAdes using default parameters. For each pair of isolates, the NCV assembly was annotated using prokka and the reads from the paired isolate were mapped to the annotated assembly in Geneious v9.1. Variants were called using a minimum coverage of 7X and a minimum allele frequency of 75%27. All variants were manually curated and variants within 10 bp of the edge of a contig were removed.
Recombinant bacterial strains, cloning, and plasmid preparation
The ASKA library is a comprehensive GFP-tagged E. coli K-12 ORF plasmid library available from the National BioResource Project. The ASKA clone library is based on the E. coli K-12 strain AG1 and individual genes were cloned into the pCA24N vector28. The E. coli strain K-12 carrying pCA24N::hemL, hemN, hemF, fes, fepC, araC, cysD, udk, pta, mprA, cusA, cusB, cusF, cspE, crcB, tatE, lipA, entD, tolC, rnr, hyfB and pCA24N plasmid itself were obtained from the National BioResource Project. These E. coli strains were grown at 35 °C for 18 h in TSY broth (Remel) with chloramphenicol (50 µg/ml). Plasmids were isolated using the ZymoPure Plasmid MiniPrep kit (Zymo Research) and then transformed into the clinical strains of E.coli, C.freundii, and E. hormaechei as described below.
One of the affected genes, pqqB, in the SCV E. hormaechei isolates was unavailable from the ASKA strain library as an ortholog of this gene is not present in E. coli K-12. This gene was amplified from the NCV E. hormaechei isolate with CloneAmp HiFi polymerase (Takara) and the following primers: 5′-TCC GGC CCT GAG GCC TAT GGC CTT TAT TAA AGT CCT CGG TTC C-3′ and 5′-TCC TTT ACT TGC GGC CGG GGT CCT GAA GCG TGA TGT TCA T-3′. These PCR products were cloned into pCA24N with a C-terminal GFP tag using the In-Fusion HD enzyme kit (Takara). Clones were selected on TSA plates with 50 µg/ml chloramphenicol. Sanger sequencing was conducted on the resulting plasmid to confirm cloning.
Preparation of competent cells and electroporation
To prepare electro-competent cells of E.coli, C.freundii, and E. hormaechei, 5 mL of TSY broth inoculated with a single colony was grown overnight with vigorous aeration (150 rpm/min) at 35 °C. The following day, 30 µl of overnight culture was diluted into 15 ml of SOC media and grown at 37 °C with constant shaking (180 rpm/min) until 0.5–0.8 OD600. Cells were harvested by centrifugation at 2000 g for 10 min at 4 °C and washed twice with 10 ml sterile ice-cold 10% glycerol. The supernatant was removed and the cell suspension was concentrated 50-fold in 3% glycerol.
For bacterial transformation, 100 uL of electrocompetent cells were mixed with 100 ng DNA in 0.1 cm cuvettes. Electroporation was carried out using a Gene Pulser with the following parameters: 2.5 kV, 25 µF and 200 Ω for the NCV and SCV E. coli, NCV and SCV E. hormaechei and SCV C. freundii. The following parameters were used to transform the NCV C. freundii: 2.5 kV, 25 µF and 600 Ω. Immediately after pulsing, 0.9 ml of SOC media was added to each cuvette, the cell suspension was transferred to a test tube and then was incubated for 30 min at 37 °C with constant shaking. Transformed clones were selected on TSA plates with 50 µg/ml chloramphenicol.
Chemical and genetic rescue and cross-feeding
Unlike their NCV co-isolates, SCVs cannot grow on M9 minimal media. We took advantage of this to study the additional nutritional requirements of SCVs and determine which mutations were casual for the auxotrophic phenotypes. To study the nutritional requirements of each SCV, a 0.5 McFarland solution of the isolate was plated on M9 media. A disk impregnated with heme (Remel), δ-aminolevulinic acid (Oxoid), L-glutamate (Sigma-Aldrich, 30 mM), lipoic acid (Sigma-Aldrich, 5 µg/mL) or pyrroloquinoline quinone (Sigma-Aldrich, 3 µM) was placed onto the media. For each chemical rescue, the corresponding NCV co-isolate and a blank disk were included as controls. The M9 plates were examined after incubation for 20–24 h at 35 °C. Of note, NCV and SCV C. freundii carrying pCA24N were used in place of the untransformed NCV and SCV C. freundii due to the instability of the SCV isolate.
To examine the causal mutations responsible for the SCV phenotype, 0.5 McFarland solutions of each of the complemented strains were plated on to M9 media (Teknova). The M9 plates were examined after incubation for 20–24 h at 35 °C. We examined whether the NCV could restore the growth of its SCV co-isolates by growing the strains adjacent to one another on M9 media. A 0.5 McFarland standard of each isolate was streaked on an M9 agar plate. This plate was examined after incubation for 20–24 h at 35 °C. Anaerobic cultures were also performed at 35 °C using the AnaeroPack system (Mitsubishi Gas Chemical) and growth was observed at 48 h.
Aerobic and anaerobic growth curves
Growth kinetics of NCV and SCV co-isolates, along with genetically rescued SCV isolates, were assessed in aerobic and anaerobic conditions. For aerobic growth curves, overnight cultures were diluted in a microplate containing 200 µL of Luria–Bertani (LB) broth (Gibco) such that the starting OD600 of the culture was approximately 0.01. The microplate was then incubated at 37 °C and OD600 readings were taken every 15 min using SpectraMax 190 operated with the SpectraMax Pro software version 4.3. A 10-s shaking was completed prior to each reading. For anaerobic growth curves, overnight cultures from each strain were diluted into four tubes containing 5 mL of pre-reduced LB broth to an OD600 of approximately 0.01. The cultures were then incubated at 35 °C in a sealed container containing an AnaeroPack anaerobic gas generator. Every 1.5 h, OD600 measurements were taken using one of the four initially noculated cultures. Aerobic growth curves were completed in biological triplicate and anaerobic growth curves were completed in biological duplicate for each strain.
Results
Clinical cases and isolates
Case histories are depicted in Fig. 1 and described in the Methods. Briefly, the paired E. coli isolates were from a urine culture on a 6-week old otherwise healthy term male infant with fever. His white blood cell count was elevated at 21,600/ml and a 2 + urine leukocyte esterase at the time of emergency visit. The C. freundii isolates were from a urine culture on a 2-month old female infant with complex urological anomalies for duplicated collecting system and grade 3 vesicoureteral reflux. Her urine leukocyte esterase was 3 + with elevated red and white blood cells in urine at the time of culture. The E. hormaechei isolates were from multiple blood cultures, both arterial line and peripheral venous draw, spanning 3 days on a 6-year old male child with end stage renal disease receiving hemodialysis and multiple prior bloodstream infections in the prior year. Of note, these isolates were originally resulted out as E. cloacae based on MALDI-TOF species identification.
Figure 1.
Case histories. Relevant past clinical microbiological and antibiotic selective pressures are indicated in the line histories for the isolation of NCV and SCV in Escherichia coli (a), Citrobacter freundii (b), and Enterobacter hormaechei (c).
Antimicrobial resistance pattern is explained by ampC
Co-isolation of both NCV and SCV of the Enterobacteriaceae strains were common to all 3 cultures during routine culture workups. The antibiotic susceptibility patterns for the three NCV isolates are shown in Table 1 and followed expected patterns of resistance given the case histories. All three corresponding SCV isolates failed to grow on MH medium for susceptibility testing.
Table 1.
Antibiotic susceptibility by disk diffusion of normal colony variant for each isolate based on CLSI M100-S29 breakpoints.
| Disk content | Zone diameter | Escherichia coli | Citrobacter freundii | Enterobacter hormaechei | ||
|---|---|---|---|---|---|---|
| S* | I* | R* | Result (mm) | Result (mm) | Result (mm) | |
| Ampicillin (10 μg) | ≥ 17 | 14–16 | ≤ 13 | R (15) | R (6) | R (6) |
| Augmentin (20/10 μg) | ≥ 18 | 14–17 | ≤ 13 | I (17) | R (7) | R (10) |
| Cefazolin | ≥ 23 | 20–22 | ≤ 19 | I (21) | R (6) | R (6) |
| Cefazolin (urine breakpoint) | ≥ 15 | ≤ 14 | S (21) | R (6) | R (6) | |
| Ceftazidime | ≥ 21 | 18–20 | ≤ 17 | S (31) | R (14) | S (27) |
| Ceftriaxone | ≥ 23 | 20–22 | ≤ 19 | S (32) | R (16) | S (27) |
| Cefuroxime (IV) | ≥ 18 | 14–17 | ≤ 13 | S (20) | R (8) | R (6) |
| Cefepime | ≥ 25 | 19–24 | ≤ 18 | S (33) | S (32) | S (33) |
| Piperacillin-tazobactam | ≥ 21 | 18–20 | ≤ 17 | S (28) | S (21) | S (27) |
| Meropenem | ≥ 23 | 20–22 | ≤ 19 | S (30) | S (29) | S (28) |
| Ciprofloxacin | ≥ 31 | 21–30 | ≤ 20 | S (33) | I (23) | S (34) |
| Gentamicin | ≥ 15 | 13–14 | ≤ 12 | S (23) | S (23) | S (20) |
| Nitrofurantoin (urine breakpoint) | ≥ 17 | 15–16 | ≤ 14 | S (26) | S (21) | N.D |
| Trimethoprim-sulfamethoxazole | ≥ 16 | 11–15 | ≤ 10 | S (29) | S (27) | S (25) |
*"S" sensitive, "I" intermediate, and "R" resistant.
Genomic sequencing of the NCV isolates confirmed the presence of chromosomal ampC in all isolates, explaining the antibiotic susceptibility patterns recovered. Analysis of contigs with higher copy number revealed one small 4 kb plasmid in Escherichia coli, three small 2.5–4 kb plasmids in Enterobacter hormachei, as well as > 80 kb of phage sequence in the Citrobacter freundii assembly but no plasmids. No specific antimicrobial resistance genes were contained on these plasmids.
Whole genome sequencing of paired isolates reveals parsimonious variants accounting for small colony phenotype
The Escherichia coli NCV assembly yielded 81 contigs > 200 bp with an N50 of 360,223 bp. Mapping of the Escherichia coli SCV reads to the NCV assembly yielded only 4 variants, including 2 variants in heme-related genes (Table 2). The 272-amino acid enterobactin siderophore transport system ATP-binding protein (fepC) gene had an internal stop codon at amino acid 169. The hemL gene had a W59R coding change and the hemF gene had an in-frame 6-bp deletion resulting in the loss of an arginine and glutamic acid at amino acids 132 and 133. In addition, the transcriptional repressor mprA gene had a P84S coding change. No intergenic variants were recovered in the Escherichia coli SCV strain relative to the NCV strain.
Table 2.
Genomic variants isolated from paired clinical co-isolates of Escherichia coli, Citrobacter freundii, Enterobacter hormaechei.
| Location | CDS codon number | CDS position | Nucleotide change | Protein effect | Coverage | Product | Genetic restoration on M9? |
|---|---|---|---|---|---|---|---|
| Escherichia coli | |||||||
| hemF | ER232– | 694 | –GAGCGC | Deletion | 142 | Coproporphyrinogen-III oxidase, aerobic | No |
| hemL | W59R | 175 | A– > T | Substitution | 117 | Glutamate-1-semialdehyde 2,1-aminomutase | Yes |
| fepC | E169X | 505 | C– > A | Truncation | 132 | putative siderophore transport system ATP-binding protein YusV | No |
| mprA | P84S | 250 | G– > A | Substitution | 147 | Transcriptional repressor MprA | No |
| Citrobacter freundii | |||||||
| 181 bp upstream of hemF | N/A | N/A | A– > C | N/A | 26 | N/A | |
| hemL | 18 | 54 | –G | Frame Shift | 44 | Glutamate-1-semialdehyde 2,1-aminomutase | Yes |
| fes | C306X | 918 | T– > A | Truncation | 67 | Enterochelin esterase | Yes |
| araC | P7L | 20 | C– > T | Substitution | 10 | Arabinose operon regulatory protein | No |
| fdnG | P778T | 2332 | C– > A | Substitution | 51 | Formate dehydrogenase, nitrate-inducible, major subunit precursor | N.D |
| pta | Q303L | 908 | T– > A | Substitution | 72 | Phosphate acetyltransferase | No |
| Enterobacter hormaechei | |||||||
| hemN | L366Q | 1097 | A– > T | Substitution | 34 | Oxygen-independent coproporphyrinogen-III oxidase 1 | No |
| pqqB | C224W | 672 | C– > A | Substitution | 57 | Coenzyme PQQ synthesis protein B | No |
| entD | D21A | 62 | C– > A | Substitution | 44 | 4′-phosphopantetheinyl transferase (enterobacin biosynthesis complex) | No |
| cysD | G291S | 871 | T– > C | Substitution | 41 | Sulfate adenylyltransferase subunit 2 | No |
| lsrK | T403S | 1207 | A– > T | Substitution | 35 | Autoinducer 2 kinase LsrK | No |
| rcsC | I362T | 1085 | G– > A | Substitution | 38 | Sensor histidine kinase RcsC | No |
| udk | D74H | 220 | G– > C | Substitution | 62 | Uridine kinase | No |
| Deletions of the following genes | |||||||
| lipA | Lipoyl Synthase | Yes | |||||
| cusF | Cation efflux system protein | No | |||||
| cusB | Cation efflux system protein | No | |||||
| cusA | Cation efflux system protein | No | |||||
| pagP | Lipid A palmitoyltransferase | N.D | |||||
| cspE | Cold shock-like protein | No | |||||
| crcB | Putative fluoride ion transporter | No | |||||
| yafV | 2-oxoglutaramate amidase | N.D | |||||
| tatE | Sec-independent protein translocase protein | No | |||||
| Hypothetical protein | Hypothetical protein | N.D | |||||
| Hypothetical protein | Hypothetical protein | N.D | |||||
Sequencing the Citrobacter freundii NCV strain yielded an assembly of 220 contigs > 200 bp with an N50 of 61,653 bp. Mapping of the Citrobacter freundii SCV reads to the NCV assembly yielded a total of 6 variants (Table 2). Two of these variants were related to heme-producing genes. Most notable among these were a 1 bp deletion in the glutamate-1-semialdehyde 2,1-aminomutatase (hemL) gene that resulted in frame shift and stop codon at amino acid 75, as well as a premature stop codon at amino acid 918 of the enterochelin esterase (fes) gene. An additional heme-related variant included an intergenic mutation of unclear significance, 181 bp upstream of the aerobic coproprohphyrinogen-III oxidase (hemF) gene. The three remaining variants resulted in coding changes in genes unrelated to heme production, including a Q303L mutation in the phosphate acetyltransferase (pta) gene, a P778T mutation in the major subunit precursor of the nitrate-inducible formate dehydrogenase (fdnG) gene, and a P7L mutation in an arabinose operon regulatory protein (araC) gene.
The Enterobacter hormaechei NCV assembly yielded 60 contigs longer than 200 bp. Mapping of the Enterobacter hormaechei SCV reads to the NCV assembly yielded 7 single nucleotide coding variants, one of which was in a gene related to heme production and one involved in enterobactin synthesis. The oxygen-independent coproporphyrinogen-III oxidase (hemN) gene had a L366Q mutation, while the 4′-phosphopantetheinyl transferase (entD) involved in enterobactin synthesis complex had a D21A mutation. Multiple unrelated coding changes were found between the SCV and the NCV Enterobacter hormaechei strains, including a G291S mutation in the sulfate adenylyltransferase subunit 2 (cysD) gene, a C224W mutation in the coenzyme PQQ synthesis protein B (pqqB), a I362T mutation in the sensor histidine kinase (rcsC), a T403S mutation in the autoinducer 2 kinase (lsrK), and a D74H mutation in uridine kinase (udk). An intergenic G- > A mutation 45 bp downstream of a hypothetical protein was also identified. A 10.2 kb chromosomal deletion disrupting 11 genes was also found in the SCV assembly as compared to the NCV assembly. These genes included lipoyl synthase (lipA), cation efflux system locus (cusA, cusB, cusF), lipid A palmitoyltransferase (pagP), cold shock-like protein (cspE), putative fluoride ion transporter (crcB), Sec-independent protein translocase (tatE), 2-oxoglutaramate amidase (yafV), and two hypothetical proteins.
Chemical and genetic rescue reveals causal SCV lesions
To determine which of the above lesions were responsible for the defects in growth observed in vitro, we performed chemical and genetic rescue experiments on the three SCV clones. We also tested the ability of the NCV isolates to rescue SCV growth by cross-feeding to further confirm that a diffusible factor was responsible for limited growth. All experiments were performed on M9 minimal medium.
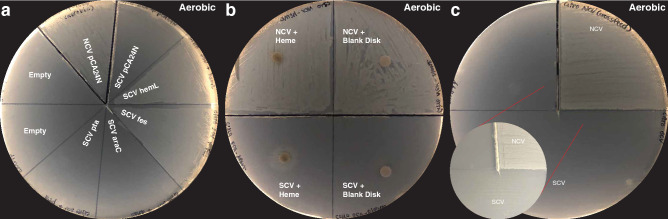
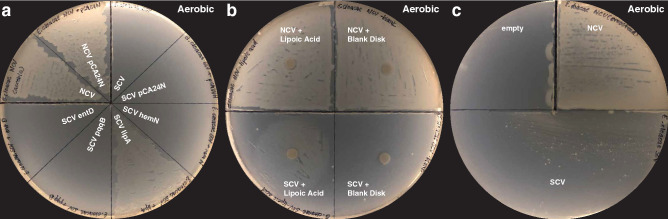
Escherichia coli SCV prototrophic growth was restored with overexpression of hemL, but not hemF, fepC, or mprA (Fig. 2a). SCV growth was also rescued by the presence of heme (Fig. 2b) or δ-aminolevulinic acid (ALA) (Supplementary Figure S1), but not L-glutamate, lipoic acid, or pyrroloquinolone quinone (PQQ) (Supplementary Figure S1). The SCV clone was also able to cross-feed from NCV (Fig. 2c). These results are all consistent with the genetic deletion in hemL being responsible for the limited growth in our E. coli clone.
Figure 2.
Heme biosynthesis lesion as cause of small colony phenotype in Escherichia coli isolated from urinary tract infection. Genomic sequencing of the paired NCV and SCV isolates revealed genomic lesions in fepC, hemF, hemL, and mprA. (a) Only genetic rescue with hemL rescued normal growth from the Escherichia coli SCV. (b) Chemical rescue with heme partially restored normal growth in Escherichia coli SCV. (c) Cross-feeding from Escherichia coli NCV partially restores growth of SCV, consistent with a diffusible factor required for growth. All plates in this figure were incubated under aerobic conditions.
SCVs often revert to the NCV phenotype when serially passaged in vitro. We identified an E. coli SCV that reverted to a normal growth phenotype over the course of our study. We performed WGS on this SCV revertant to understand the individual mutations that resulted in wild type growth. This isolate had an NCV-like hemL sequence, but retained the SCV coding mutations in hemF, fepC and mprA. No additional mutations were observed in the reverted isolate. This further supports the results of our chemical and genetic rescues, and further highlights the importance of an intact hemL for normal growth.
Genetic and chemical rescue of C. freundii SCV growth showed similar results. C. freundii SCV prototrophic growth was restored with overexpression of hemL or fes, but not araC or pta (Fig. 3a). The same chemical rescue results were seen as in the E. coli SCV, as heme (Fig. 3b) or ALA (Supplementary Figure S2) were able to restore growth, but L-glutamate, lipoic acid, or PQQ failed to do so (Supplementary Figure S2). Moderate cross-feeding rescue with co-culture with the NCV clone was observed (Fig. 3c). These results also indicate that deficiencies in heme synthesis and iron transport were responsible for the small colony growth phenotype seen in our C. freundii isolate.
Figure 3.
Heme biosynthesis along with iron availability lesion as cause of small colony phenotype in Citrobacter freundii isolated from urinary tract infection. Genomic sequencing of the paired NCV and SCV isolates revealed genomic lesions in araC, fdnG, fes, hemL, pta, and in the intergenic region upstream of the hemF gene. (a) Genetic rescue with fes and hemL rescued normal growth from the Citrobacter freundii SCV. (b) Chemical rescue with heme restored normal growth in Citrobacter freundii SCV. (c) Cross-feeding from Citrobacter freundii NCV partially restores growth of SCV, consistent with a diffusible factor required for growth. All plates in this figure were incubated under aerobic conditions.
Over the course of the rescue experiments, the C. freundii SCV also reverted to normal growth. This clone had NCV-like fes and hemL sequence, while the same SCV coding mutations were seen in araC, fdnG, and pta, as well as the intergenic mutation upstream of hemF. The C. freundii revertant also had a new R100H mutation in the cytochrome bd-I ubiquinol oxidase subunit 2 gene (CydB) relative to both the SCV and NCV clones. These results further confirm the genetic and chemical rescue performed above, illustrating the importance of the heme pathway for normal growth.
Finally, despite also containing lesions in the heme biosynthesis pathway, the E. hormaechei SCV produced a radically different pattern of chemical and genetic rescue. Here, overexpression of lipA was the only gene that yielded prototrophic growth (Fig. 4a), while all other disrupted genes failed to rescue growth (Fig. 4a, Supplementary Figure S3). Complementation with lipoic acid restored growth (Fig. 4b) along with co-culture with E. hormaechei NCV (Fig. 4c), while PQQ, heme and its biosynthetic intermediates L-glutamate and ALA failed to increase SCV growth (Supplementary Figure S3). These results conclusively demonstrate that disruption of the lipoylation pathway was responsible for the small growth phenotype in our E. hormaechei SCV isolate. We did not observe reversion to normal growth for the E. hormaechei SCV.
Figure 4.
Lipoic acid biosynthesis as cause of small colony phenotype in Enterobacter hormaechei isolated from a bloodstream infection in a patient with end-stage renal disease. Genomic sequencing of the paired NCV and SCV isolates revealed multiple genomic lesions including single nucleotide substitutions in entD, hemN, and pqqB along with large-scale rearrangements leading to disruption of the lipA gene. (a) Genetic rescue with lipA restored normal growth from the Enterobacter hormaechei SCV. (b) Chemical rescue with lipoic acid restored normal growth in Enterobacter hormaechei SCV. (c) Cross-feeding from Enterobacter hormaechei NCV restores growth of SCV, consistent with a diffusible factor required for growth. All plates in this figure were incubated under aerobic conditions.
Genetic rescue of the heme or lipoic acid biosynthesis pathway restores the growth kinetics of SCVs
In addition to unique colony morphologies and auxotrophy, a hallmark of the SCV phenotype is diminished growth kinetics compared to their NCV counterparts. We performed a growth curve analysis using the NCV and SCV co-isolates and the genetically complemented SCV strains which displayed prototrophic growth on M9 media: hemL for E. coli, hemL and fepC for C. freundii, and lipA for E. hormaechei. The E. coli and C. freundii SCV isolates both displayed an extended lag phase and exhibited a lower OD600 in the stationary phase compared to their NCV co-isolates (Fig. 5a,b). The E. hormaechei SCV did not displayed an extended lag phase compared its NCV co-isolate (Fig. 5c). However, the E. hormaechei SCV exited the exponential growth phase earlier than its NCV co-isolate and exhibited a lower OD600 during the stationary phase.
Figure 5.
Growth curve analysis in aerobic conditions demonstrates hemL fully restores the impaired growth kinetics of (a) Escherichia coli SCV and (b) Citrobacter freundii SCV isolates. The Citrobacter freundii SCV isolate was not rescued by fes. (c) Growth kinetics of the Enterobacter hormaechei SCV isolate are partially restored by overexpression of lipA.
The growth kinetics of the E. coli SCV and C. freundii SCV isolates were completely rescued through overexpression hemL (Fig. 5a,b). Genetic complementation with fes did not rescue the growth kinetic of the C. freundii isolate. The growth kinetics of the E. hormaechei SCV isolate were partially restored by complementation with lipA (Fig. 5c); however, the genetically complemented strain still exited the exponential growth phase earlier than the NCV isolate and exhibited a lower OD600 during the stationary phase.
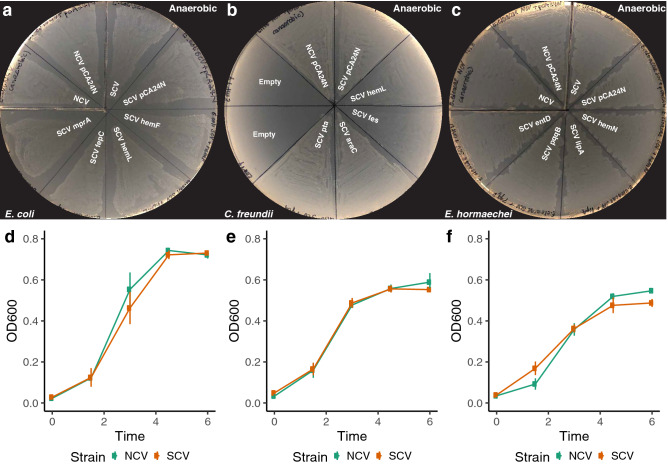
SCVs demonstrate prototrophic growth and unaltered growth kinetics under anaerobic conditions
Based on recurrent isolation of mutants in aerobic respiration pathways, along with the genetic and chemical rescue experiments demonstrating their causality, we hypothesized that SCV isolates might not demonstrate growth defects under anaerobic conditions. We cultured NCV and SCV isolates for each of the three species along with the transformed genetic rescue clones under anaerobic conditions for 48 h. Anaerobic conditions rescued SCV growth in all cases (Figs. 6a–c, S3h–j). These results were also independent of every genetic construct transformed.
Figure 6.
SCV E. coli (a), C. freundii (b), and E. hormaechei (c) isolates grow on minimal media without additional chemical or genetic supplementation in anaerobic conditions. NCV and SCV E. coli (d), C. freundii (e), and E hormaechei (f) co-isolates display similar growth kinetics in anaerobic conditions.
We next performed a growth curve analysis under anaerobic conditions with the NCV and SCV co-isolates. For all three pairs, similar growth kinetics were displayed between the NCV and SCV co-isolates (Fig. 6d–f).
Discussion
Here, we used genomic screening of paired isolates to understand the molecular mechanism of the small colony growth phenotype in Gram-negative bacteria encountered in the clinical microbiology laboratory as well as bacterial persistence in vivo. Unlike the NCVs, all three corresponding bacterial SCV isolates were auxotrophic, thus unable to grow in glucose only M9 medium. Using genetic, chemical rescue, as well as NCV cross-feeding, we found heme-production pathway lesions to be responsible for the SCV phenotype in two of the three isolates, while lipoic acid synthesis was responsible for the third. In the E. coli SCV, both W59R in hemL and two-amino acid deletion in hemF could impact heme production, but only complementation of hemL rescued growth on M9 media. In the SCV C. freundii, the truncation of hemL blocked ALA production. In E. hormaechei SCV, the lipA gene was interrupted by large-scale genomic deletion and, correspondingly, complementation with lipA or lipoic acid restored prototrophic growth. Each of the SCV isolates displayed diminished growth kinetics compared to the corresponding NCV co-isolate. We demonstrated the growth kinetics of the E.coli SCV and C. freundii SCV isolates could both be completed restored by overexpression of hemL, while the growth kinetics of E. hormaechi were only partially restored by overexpression of lipA. Intriguingly, growth of the SCVs was not impaired under anaerobic conditions, consistent with the role of heme as an essential cofactor for the electron transport chain and lipoic acid’s role in the Krebs cycle. Of note, this is the first report of whole genome comparison of paired NCV and SCV Enterobacteriaceae isolates associated with clinical bloodstream and urinary tract infections from pediatric patients and the first report of detection of gene lesions associated with bacterial iron acquisition. Gene truncations in enterochelin esterase (fes) in the SCV C. freundii, a putative siderophore transport system ATP-binding protein (fepC) in the SCV E. coli, and D21A in entD of E. hormaechei were novel findings with potential implications for bacterial lifestyle changes upon host selection. Notably, despite the significant genetic lesions recovered here—two truncations and a coding mutation never previously recovered in any Enterobacter hormaechei—complementation with fepC and entD genes from E. coli failed to rescue prototrophic growth. Future work will need to characterize the effect of these mutations on protein function, as it is possible that these mutations result in dominant negative phenotypes.
The antibiotic exposure history or the choices for certain specific agent(s) used for the treatment in the 3 patients at the time could not explain a common pattern of selective pressure for the emergence of bacterial SCV. The patient underlying illnesses also ranged from the first episode of a potential E. coli urosepsis in a newborn, a recurrent C. freundii UTI in a 2-month old, and a presumed E. hornaechei occult renal system infection in a 6-year old patient with end stage renal disease pending kidney transplant. The second and the third cases both had significant prior antimicrobial exposure to multiple classes of agents with beta-lactams being the most common agent, but first new born case had no prior treatment ever. Although prior exposure to aminoglycosides or sulfamethoxazole-trimethoprim has been reported as selective pressure for selection of bacterial SCVs4,29, these two agents were only used in the third case. Therefore, antibiotic use alone may not be the major contributor for SCV selection.
Pairwise sequencing of the NCV and SCV genomes for SCV mutational characterization was based on the assumption that both NCV and SCV descended from the same strain. While the NCV is likely the closest representative of the parental strain, SCV diverged from this strain with distinctive mutations that were absent in NCV. The functional M9 growth studies in vitro have clearly demonstrated that deficiencies in bacterial synthesis of heme, lipoic acid, and/or iron acquisition apparatus were the primary contributors to SCV auxotrophism. Our analysis suggests that both the oxidative respiration and iron acquisition may be counter-selected by the host during the subacute or perhaps chronic infections. Moreover, the extent of SCV genomic mutations could vary depending on the clinical course of the infective illnesses. For example, the E. coli SCV urinary tract isolate from a 6 week old infant had 4 SNVs, the repeat C. freundii SCV urinary tract isolate from a 2 month old patient with urological anomalies had 6 SNVs, and the blood stream E. hormaechei SCV isolate from a 6 year old patient with end stage renal disease had 8 SNVs plus an 11-gene deletion.
The selective loss of oxidative respiration and iron acquisition we observed in the SCV isolates sharply contrasts with conventionally held beliefs about microbial pathogens. Rather than rapidly dividing and completing fiercely for iron, SCVs take a unique approach for evading the host defense response, which includes iron starvation and oxidative stress1,2. In response to the iron-limiting condition, it has been well documented that the bacterial ferric uptake regulator (Fur) system is activated to strengthen microbial ability to capture iron for energetic growth and pathogenesis3. Regardless of iron availability, Enterobacteriaceae are facultative anaerobes, and they are fully capable of growth under various oxygen tensions with oxidative respiration being significantly more robust for energetic growth in vitro30. Therefore, change in oxygen tension itself in the infected host environment may not be the major selective pressure for SCV development. Our finding of mutations in oxidative respiration related genes was consistent with the overwhelming reports of bacterial SCV deficiencies in heme, menaquinone, and lipoic acid synthesis4,21,31,32. Thus, an overarching impression of the SCV degenerative mutations is their association with the essential elements of aerobic living which demands more iron33. The SCV isolates in this study, regardless of heme, lipoic acid, and/or iron transport deficiencies, were all able to grow anaerobically on M9 without nutrient supplementation. In fact, the selective loss of aerobic respiration under iron limiting and oxidative stress conditions is indicative of a microbial survival mechanism by “retreating to anaerobic habitats” in order to persist inside a single affected host without clonal dissemination into the host population4,34–36. Hence, resorting to anaerobic living may be an alternative response to iron limitation and oxidative stress37. This alternative survival mechanism would be opposite to the well-known “superbugs” survival strategy of head-on iron competition and host population dissemination38,39. It also shares similarities with the immunoevasion strategies of tumors via hypoxia-induced immune exhaustion and T-cell anergy40.
Iron is an essential nutrient for all forms of life41. However, some free-living and obligate parasitic bacteria (e.g. Borrelia burgdorferi) employ a unique iron-independent redox-active metal such as manganese (Mn) to deal with oxidative stress, which allows them to bypass host iron defense42. E. coli maintains a Mn-SOD (superoxide dismutase) system which is also regulated by Fur43. All three SCV isolates contained an intact sodA, though expression and functional anti-oxidant activities were not examined. It is conceivable that the inactivation of iron uptake apparatus in bacterial SCVs may be indicative of bacterial transition into a parasitic lifestyle by means of iron bypass42. Alternatively, the genetic lesions described here, particularly in E. hormaechei, could also be indicative of evolution to a more symbiotic lifestyle, as evidenced by the cross-feeding and gene decay44. The co-obligate symbiotic bacterium Serratia symbiotica, known for its minimal genome (~ 143 kb), has lost the ability to synthesize both heme and enterobactin and, additionally, lacks an iron uptake apparatus, similar to the changes observed in our SCV isolates45,46.
This study is limited by our focus only on mutations that were associated with auxotrophism on M9 medium without analyzing other mutations that could potentially affect many other aspects of bacterial functions. For example, a ~ 10.2-kb deleted fragment in E. hormaechei SCV contained cusF, cusB, and cusA in tandem where CusCFBA is a membrane-bound proton antiporter for Cu/Ag efflux47. As this efflux system carries out ATP-demanding activities, we speculate that this function encounters the same counter-selective pressure as a result of reduced ATP production assuming SCV anaerobic lifestyle. The exact host factor(s) that was critical for selection of SCV mutations is still unknown. Ideally, host selective factors could be identified if we could recreate the bacterial SCVs from the wildtype using host materials for bacterial growth in vitro or in animal models.
Antimicrobial resistance and iron competition as mechanisms for bacterial survival have attracted a great deal of interest48. These isolates are now readily recognized in the clinical microbiology laboratory due to their robust growth and detectable resistance phenotypes using standard in vitro testing. Clinical isolates such as SCVs that lack these growth characteristics may be easily missed due to their small colony size and failure to grow on standard susceptibility testing media. The role of these alternatively pathways of survival in clinical infections may be significantly underestimated32. Future work must address the totality of bacterial survival mechanisms, including mechanisms of bacteria persistence via resistance to host iron immunity and oxidative stress by means of anaerobiosis and iron bypass.
Supplementary Information
Acknowledgements
We thank National BioResource Project NBRP E.coli Strain, Japan for the E. coli plasmid library (https://shigen.nig.ac.jp/ecoli/strain/). We also thank Seattle Children’s Microbiology team for their effort in standardization of bacterial SCV identification and quality documentation of these paired isolates.
Author contributions
Conceptualization—A.L.G., X.Q., Amin Addetia; data curation—A.L.G., Amin Addetia, Amanda Adler, X.Q.; formal analysis—A.L.G., Amin Addetia, X.Q.; funding acquisition—A.L.G., X.Q.; resources—A.L.G., X.Q.; investigation—A.L.G., Amin Addetia, Y.T.; methodology—A.L.G., Amin Addetia, X.Q.; project administration—A.L.G., X.Q., Amin Addetia; Visualization—A.L.G., Amin Addetia, X.Q.; supervision—A.L.G., X.Q.; validation—A.L.G., Amin Addetia, X.Q.; writing—original draft—A.L.G., Amin Addetia, X.Q.; writing—reviewing and editing—all authors.
Data availability
All genome assemblies are available from NCBI BioProject PRJNA523376.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Alexander L. Greninger and Amin Addetia.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-86764-4.
References
- 1.Cassat JE, Skaar EP. Iron in infection and immunity. Cell Host Microbe. 2013;13:509–519. doi: 10.1016/j.chom.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skaar EP. The battle for iron between bacterial pathogens and their vertebrate hosts. PLoS Pathog. 2010;6:e1000949. doi: 10.1371/journal.ppat.1000949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porcheron G, Dozois CM. Interplay between iron homeostasis and virulence: Fur and RyhB as major regulators of bacterial pathogenicity. Vet. Microbiol. 2015;179:2–14. doi: 10.1016/j.vetmic.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 4.Proctor RA, von Eiff C, Kahl BC, Becker K, McNamara P, Herrmann M, Peters G. Small colony variants: A pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat. Rev. Microbiol. 2006;4:295–305. doi: 10.1038/nrmicro1384. [DOI] [PubMed] [Google Scholar]
- 5.Grant SS, Hung DT. Persistent bacterial infections, antibiotic tolerance, and the oxidative stress response. Virulence. 2013;4:273–283. doi: 10.4161/viru.23987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia LG, Lemaire S, Kahl BC, Becker K, Proctor RA, Denis O, Tulkens PM, Van Bambeke F. Antibiotic activity against small-colony variants of Staphylococcus aureus: Review of in vitro, animal and clinical data. J. Antimicrob. Chemother. 2013;68:1455–1464. doi: 10.1093/jac/dkt072. [DOI] [PubMed] [Google Scholar]
- 7.Kahl BC, Becker K, Löffler B. Clinical significance and pathogenesis of staphylococcal small colony variants in persistent infections. Clin. Microbiol. Rev. 2016;29:401–427. doi: 10.1128/CMR.00069-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson SW, Stapp JR, Burns JL, Qin X. Characterization of small-colony-variant stenotrophomonas maltophilia isolated from the sputum specimens of five patients with cystic fibrosis. J. Clin. Microbiol. 2007;45:529–535. doi: 10.1128/JCM.01444-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wellinghausen N, Chatterjee I, Berger A, Niederfuehr A, Proctor RA, Kahl BC. Characterization of clinical Enterococcus faecalis small-colony variants. J. Clin. Microbiol. 2009;47:2802–2811. doi: 10.1128/JCM.00485-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roggenkamp A, Sing A, Hornef M, Brunner U, Autenrieth IB, Heesemann J. Chronic prosthetic hip infection caused by a small-colony variant of Escherichia coli. J. Clin. Microbiol. 1998;36:2530–2534. doi: 10.1128/JCM.36.9.2530-2534.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Săsărman A, Sanderson KE, Surdeanu M, Sonea S. Hemin-deficient mutants of Salmonella typhimurium. J. Bacteriol. 1970;102:531–536. doi: 10.1128/JB.102.2.531-536.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morton HE, Shoemaker J. The Identification of Neisseria gonorrhoeae by means of bacterial variation and the detection of small colony forms in clinical material. J Bacteriol. 1945;50:585–587. doi: 10.1128/JB.50.5.585-587.1945. [DOI] [PubMed] [Google Scholar]
- 13.Kriegeskorte A, Block D, Drescher M, Windmüller N, Mellmann A, Baum C, Neumann C, Lorè NI, Bragonzi A, Liebau E, Hertel P, Seggewiss J, Becker K, Proctor RA, Peters G, Kahl BC. Inactivation of thyA in Staphylococcus aureus attenuates virulence and has a strong impact on metabolism and virulence gene expression. MBio. 2014;5:e01447–e11414. doi: 10.1128/mBio.01447-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choby JE, Skaar EP. Heme synthesis and acquisition in bacterial pathogens. J. Mol. Biol. 2016;428:3408–3428. doi: 10.1016/j.jmb.2016.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dean MA, Olsen RJ, Long SW, Rosato AE, Musser JM. Identification of point mutations in clinical Staphylococcus aureus strains that produce small-colony variants auxotrophic for menadione. Infect. Immun. 2014;82:1600–1605. doi: 10.1128/IAI.01487-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lannergård J, von Eiff C, Sander G, Cordes T, Seggewiss J, Peters G, Proctor RA, Becker K, Hughes D. Identification of the genetic basis for clinical menadione-auxotrophic small-colony variant isolates of Staphylococcus aureus. Antimicrob. Agents Chemother. 2008;52:4017–4022. doi: 10.1128/AAC.00668-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clements MO, Watson SP, Poole RK, Foster SJ. CtaA of Staphylococcus aureus is required for starvation survival, recovery, and cytochrome biosynthesis. J. Bacteriol. 1999;181:501–507. doi: 10.1128/JB.181.2.501-507.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pränting M, Andersson DI. Escape from growth restriction in small colony variants of Salmonella typhimurium by gene amplification and mutation. Mol. Microbiol. 2011;79:305–315. doi: 10.1111/j.1365-2958.2010.07458.x. [DOI] [PubMed] [Google Scholar]
- 19.von Eiff C, Heilmann C, Proctor RA, Woltz C, Peters G, Götz F. A site-directed Staphylococcus aureus hemB mutant is a small-colony variant which persists intracellularly. J. Bacteriol. 1997;179:4706–4712. doi: 10.1128/JB.179.15.4706-4712.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramiro RS, Costa H, Gordo I. Macrophage adaptation leads to parallel evolution of genetically diverse Escherichia coli small-colony variants with increased fitness in vivo and antibiotic collateral sensitivity. Evol. Appl. 2016;9:994–1004. doi: 10.1111/eva.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santos V, Hirshfield I. The physiological and molecular characterization of a small colony variant of Escherichia coli and its phenotypic rescue. PLoS ONE. 2016;11:e0157578. doi: 10.1371/journal.pone.0157578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sifri CD, Baresch-Bernal A, Calderwood SB, von Eiff C. Virulence of Staphylococcus aureus small colony variants in the Caenorhabditis elegans infection model. Infect. Immun. 2006;74:1091–1096. doi: 10.1128/IAI.74.2.1091-1096.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Painter KL, Strange E, Parkhill J, Bamford KB, Armstrong-James D, Edwards AM. Staphylococcus aureus adapts to oxidative stress by producing H2O2-resistant small-colony variants via the SOS response. Infect. Immun. 2015;83:1830–1844. doi: 10.1128/IAI.03016-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tada T, Uechi K, Nakasone I, Miyazato Z, Shinzato T, Shimada K, Tsuchiya M, Kirikae T, Fujita J. A hemin auxotrophic Enterobacter cloacae clinical isolate with increased resistance to carbapenems and aminoglycosides. J. Med. Microbiol. 2018;67:29–32. doi: 10.1099/jmm.0.000655. [DOI] [PubMed] [Google Scholar]
- 25.Greninger AL, Langelier C, Cunningham G, Keh C, Melgar M, Chiu CY, Miller S. Two rapidly growing mycobacterial species isolated from a brain abscess: First whole-genome sequences of mycobacterium immunogenum and mycobacterium llatzerense. J. Clin. Microbiol. 2015;53:2374–2377. doi: 10.1128/JCM.00402-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Addetia A, Greninger AL, Adler A, Yuan S, Makhsous N, Qin X, Zerr DM. A novel, widespread qacA allele results in reduced chlorhexidine susceptibility in Staphylococcus epidermidis. Antimicrob. Agents Chemother. 2019;63:e02607–e02618. doi: 10.1128/AAC.02607-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greninger AL, Streithorst J, Golden JA, Chiu CY, Miller S. Complete genome sequence of sequential Pandoraea apista isolates from the same cystic fibrosis patient supports a model of chronic colonization with in vivo strain evolution over time. Diagn. Microbiol. Infect. Dis. 2017;87:1–6. doi: 10.1016/j.diagmicrobio.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 28.Kitagawa M, Ara T, Arifuzzaman M, Ioka-Nakamichi T, Inamoto E, Toyonaga H, Mori H. Complete set of ORF clones of Escherichia coli ASKA library (a complete set of E. coli K-12 ORF archive): Unique resources for biological research. DNA Res. 2005;12:291–299. doi: 10.1093/dnares/dsi012. [DOI] [PubMed] [Google Scholar]
- 29.Melter O, Radojevič B. Small colony variants of Staphylococcus aureus—Review. Folia Microbiol. (Praha) 2010;55:548–558. doi: 10.1007/s12223-010-0089-3. [DOI] [PubMed] [Google Scholar]
- 30.Gonzalez JE, Long CP, Antoniewicz MR. Comprehensive analysis of glucose and xylose metabolism in Escherichia coli under aerobic and anaerobic conditions by 13C metabolic flux analysis. Metab. Eng. 2017;39:9–18. doi: 10.1016/j.ymben.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Eiff C, Peters G, Becker K. The small colony variant (SCV) concept—The role of staphylococcal SCVs in persistent infections. Injury. 2006;37(Suppl 2):S26–33. doi: 10.1016/j.injury.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Park YJ, Le Phuong N, Pinto NA, Kwon MJ, D’Souza R, Byun J-H, Sung H, Yong D. Urinary tract infection caused by a small colony variant form of capnophilic Escherichia coli leading to misidentification and non-reactions in antimicrobial susceptibility tests. Antimicrob. Resist. Infect. Control. 2018;7:139. doi: 10.1186/s13756-018-0438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beauchene NA, Myers KS, Chung D, Park DM, Weisnicht AM, Keleş S, Kiley PJ. Impact of anaerobiosis on expression of the iron-responsive fur and RyhB regulons. MBio. 2015;6:e01947–e11915. doi: 10.1128/mBio.01947-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Imlay JA. Iron-sulphur clusters and the problem with oxygen. Mol. Microbiol. 2006;59:1073–1082. doi: 10.1111/j.1365-2958.2006.05028.x. [DOI] [PubMed] [Google Scholar]
- 35.Qin X. Chronic pulmonary pseudomonal infection in patients with cystic fibrosis: A model for early phase symbiotic evolution. Crit. Rev. Microbiol. 2016;42:144–157. doi: 10.3109/1040841X.2014.907235. [DOI] [PubMed] [Google Scholar]
- 36.Proctor RA, Kriegeskorte A, Kahl BC, Becker K, Löffler B, Peters G. Staphylococcus aureus small colony variants (SCVs): A road map for the metabolic pathways involved in persistent infections. Front. Cell Infect. Microbiol. 2014;4:99. doi: 10.3389/fcimb.2014.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dukan S, Nyström T. Oxidative stress defense and deterioration of growth-arrested Escherichia coli cells. J. Biol. Chem. 1999;274:26027–26032. doi: 10.1074/jbc.274.37.26027. [DOI] [PubMed] [Google Scholar]
- 38.Miller HK, Auerbuch V. Bacterial iron-sulfur cluster sensors in mammalian pathogens. Metallomics. 2015;7:943–956. doi: 10.1039/C5MT00012B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peltier F, Choquet M, Decroix V, Adjidé CC, Castelain S, Guiheneuf R, Pluquet E. Characterization of a multidrug-resistant Klebsiella pneumoniae ST607-K25 clone responsible for a nosocomial outbreak in a neonatal intensive care unit. J. Med. Microbiol. 2019;68:67–76. doi: 10.1099/jmm.0.000884. [DOI] [PubMed] [Google Scholar]
- 40.Noman MZ, Hasmim M, Messai Y, Terry S, Kieda C, Janji B, Chouaib S. Hypoxia: A key player in antitumor immune response. A review in the theme: Cellular responses to hypoxia. Am. J. Physiol. Cell Physiol. 2015;309:C569–579. doi: 10.1152/ajpcell.00207.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cairo G, Bernuzzi F, Recalcati S. A precious metal: Iron, an essential nutrient for all cells. Genes Nutr. 2006;1:25–39. doi: 10.1007/BF02829934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Posey JE, Gherardini FC. Lack of a role for iron in the Lyme disease pathogen. Science. 2000;288:1651–1653. doi: 10.1126/science.288.5471.1651. [DOI] [PubMed] [Google Scholar]
- 43.Fee JA. Regulation of sod genes in Escherichia coli: Relevance to superoxide dismutase function. Mol. Microbiol. 1991;5:2599–2610. doi: 10.1111/j.1365-2958.1991.tb01968.x. [DOI] [PubMed] [Google Scholar]
- 44.Gil R, Sabater-Muñoz B, Latorre A, Silva FJ, Moya A. Extreme genome reduction in Buchnera spp.: Toward the minimal genome needed for symbiotic life. Proc. Natl. Acad. Sci. USA. 2002;99:4454–4458. doi: 10.1073/pnas.062067299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burke GR, Moran NA. Massive genomic decay in Serratia symbiotica, a recently evolved symbiont of aphids. Genome Biol. Evol. 2011;3:195–208. doi: 10.1093/gbe/evr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manzano-Marín A, Latorre A. Settling down: the genome of Serratia symbiotica from the aphid Cinara tujafilina zooms in on the process of accommodation to a cooperative intracellular life. Genome Biol. Evol. 2014;6:1683–1698. doi: 10.1093/gbe/evu133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Franke S, Grass G, Rensing C, Nies DH. Molecular analysis of the copper-transporting efflux system CusCFBA of Escherichia coli. J. Bacteriol. 2003;185:3804–3812. doi: 10.1128/JB.185.13.3804-3812.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Broberg CA, Palacios M, Miller VL. Klebsiella: A long way to go towards understanding this enigmatic jet-setter. F1000Prime Rep. 2014;6:64. doi: 10.12703/P6-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All genome assemblies are available from NCBI BioProject PRJNA523376.