Abstract
This study updates an analysis of US mortality in 2020, including deaths due to COVID-19 as well as all other causes.
A study analyzing US mortality in March-July 2020 reported a 20% increase in excess deaths, only partly explained by COVID-19. Surges in excess deaths varied in timing and duration across states and were accompanied by increased mortality from non–COVID-19 causes.1 This study updates the analysis for the remainder of 2020.
Methods
The Supplement details the methods. A Poisson regression model used mortality data from 2014-2019 to predict US expected deaths in 2020. Observed deaths in weeks ending March 1, 2020, through January 2, 2021, were taken from provisional, unweighted death counts for the District of Columbia and 49 states, excluding North Carolina for insufficient data. Data sources included the National Center for Health Statistics2,3,4 and US Census Bureau.5 Data for 8 geographic regions were grouped into distinctive surge patterns. COVID-19 deaths included all deaths for which COVID-19 was cited as an underlying or contributing cause.
Temporal changes in mortality rates from non–COVID-19 causes (eg, Alzheimer disease/dementia, heart disease, diabetes, and 9 other grouped causes; see Supplement) were examined. Data included all deaths in which non–COVID-19 conditions were listed as the underlying cause of death (potentially including deaths for which COVID-19 was a contributing cause). The Joinpoint regression program version 4.8.0.1 (Statistical Research and Applications Branch, National Cancer Institute) was used to specify the weeks (joinpoints) when slopes changed (measured by the annual percentage change [APC]) and their statistical significance (2-sided test, α = .05 threshold).
Results
Between March 1, 2020, and January 2, 2021, the US experienced 2 801 439 deaths, 22.9% more than expected, representing 522 368 excess deaths (Table). The excess death rate was higher among non-Hispanic Black (208.4 deaths per 100 000) than non-Hispanic White or Hispanic populations (157.0 and 139.8 deaths per 100 000, respectively); these groups accounted for 16.9%, 61.1%, and 16.7% of excess deaths, respectively. The US experienced 4 surge patterns: in New England and the Northeast, excess deaths surged in the spring; in the Southeast and Southwest, in the summer and early winter; in the Plains, Rocky Mountains, and far West, primarily in early winter; and in the Great Lakes, bimodally, in the spring and early winter (Figure). Excess deaths were increasing in all regions at the end of 2020. The 10 states with the highest per capita rate of excess deaths were Mississippi, New Jersey, New York, Arizona, Alabama, Louisiana, South Dakota, New Mexico, North Dakota, and Ohio. New York experienced the largest relative increase in all-cause mortality (38.1%). Deaths attributed to COVID-19 accounted for 72.4% of US excess deaths.
Table. Excess Deaths, March 1, 2020, to January 2, 2021, US and Selected States and Regions.
| Jurisdiction | Expected deaths (95% CI)a | Observed deaths (ratio of observed to expected) | Excess deaths, No. (95% CI) | Excess deaths/100 000b | COVID-19 deathsc | Excess deaths attributed to COVID-19, %c |
|---|---|---|---|---|---|---|
| USd | 2 279 071 (2 278 117 to 2 280 026) | 2 801 439 (1.23) | 522 368 (521 413 to 523 322) | 164.4 | 378 039 | 72.4 |
| Alabama | 43 621 (43 495 to 43 747) | 54 361 (1.25) | 10 740 (10 614 to 10 866) | 219.0 | 6767 | 63.0 |
| Alaska | 3740 (3719 to 3761) | 4205 (1.12) | 465 (444 to 486) | 63.6 | 167 | 35.9 |
| Arizona | 50 305 (50 166 to 50 443) | 66 378 (1.32) | 16 073 (15 935 to 16 212) | 220.8 | 9523 | 59.2 |
| Arkansas | 26 652 (26 561 to 26 742) | 32 300 (1.21) | 5648 (5558 to 5739) | 187.2 | 4077 | 72.2 |
| California | 223 220 (222 892 to 223 548) | 273 584 (1.23) | 50 364 (50 036 to 50 692) | 127.5 | 34 350 | 68.2 |
| Colorado | 33 680 (33 573 to 33 787) | 40 636 (1.21) | 6956 (6849 to 7063) | 120.8 | 5123 | 73.6 |
| Connecticut | 25 837 (25 749 to 25 925) | 32 379 (1.25) | 6542 (6454 to 6630) | 183.5 | 6222 | 95.1 |
| Delaware | 7618 (7582 to 7654) | 9278 (1.22) | 1660 (1624 to 1696) | 170.5 | 914 | 55.0 |
| District of Columbia | 5104 (5078 to 5130) | 6370 (1.25) | 1266 (1240 to 1292) | 179.4 | 927 | 73.2 |
| Florida | 175 117 (174 826 to 175 409) | 206 940 (1.18) | 31 823 (31 531 to 32 114) | 148.2 | 22 013 | 69.2 |
| Georgia | 71 514 (71 341 to 71 687) | 88 079 (1.23) | 16 565 (16 392 to 16 738) | 156.0 | 10 449 | 63.1 |
| Hawaii | 9735 (9692 to 9778) | 10 012 (1.03) | 277 (234 to 320) | 19.6 | 281 | 101.4 |
| Idaho | 11 721 (11 671 to 11 771) | 14 117 (1.20) | 2396 (2346 to 2446) | 134.1 | 1506 | 62.9 |
| Illinois | 88 632 (88 436 to 88 829) | 110 524 (1.25) | 21 892 (21 695 to 22 088) | 172.8 | 16 843 | 76.9 |
| Indiana | 55 892 (55 743 to 56 040) | 66 603 (1.19) | 10 711 (10 563 to 10 860) | 159.1 | 9602 | 89.6 |
| Iowa | 25 336 (25 249 to 25 424) | 30 368 (1.20) | 5032 (4944 to 5119) | 159.5 | 4814 | 95.7 |
| Kansas | 22 059 (21 980 to 22 138) | 26 506 (1.20) | 4447 (4368 to 4526) | 152.6 | 3527 | 79.3 |
| Kentucky | 40 166 (40 046 to 40 286) | 47 241 (1.18) | 7075 (6955 to 7195) | 158.4 | 4651 | 65.7 |
| Louisiana | 38 475 (38 358 to 38 591) | 48 468 (1.26) | 9993 (9877 to 10 110) | 215.0 | 7068 | 70.7 |
| Maine | 12 415 (12 363 to 12 468) | 13 086 (1.05) | 671 (618 to 723) | 49.9 | 356 | 53.1 |
| Maryland | 41 068 (40 947 to 41 190) | 51 296 (1.25) | 10 228 (10 106 to 10 349) | 169.2 | 6805 | 66.5 |
| Massachusetts | 48 764 (48 630 to 48 899) | 58 723 (1.20) | 9959 (9824 to 10 093) | 144.5 | 10 237 | 102.8 |
| Michigan | 81 079 (80 892 to 81 265) | 98 891 (1.22) | 17 812 (17 626 to 17 999) | 178.4 | 12 372 | 69.5 |
| Minnesota | 38 264 (38 147 to 38 381) | 44 383 (1.16) | 6119 (6002 to 6236) | 108.5 | 5897 | 96.4 |
| Mississippi | 26 185 (26 096 to 26 275) | 33 919 (1.30) | 7734 (7644 to 7823) | 259.9 | 5142 | 66.5 |
| Missouri | 53 505 (53 361 to 53 649) | 64 960 (1.21) | 11 455 (11 311 to 11 599) | 186.6 | 8052 | 70.3 |
| Montana | 8642 (8602 to 8681) | 10 254 (1.19) | 1612 (1573 to 1652) | 150.9 | 1231 | 76.3 |
| Nebraska | 14 075 (14 018 to 14 132) | 16 867 (1.20) | 2792 (2735 to 2849) | 144.3 | 2258 | 80.9 |
| Nevada | 21 547 (21 469 to 21 626) | 26 780 (1.24) | 5233 (5154 to 5311) | 169.9 | 3576 | 68.3 |
| New Hampshire | 10 212 (10 167 to 10 257) | 11 491 (1.13) | 1279 (1234 to 1324) | 94.0 | 768 | 60.1 |
| New Jersey | 60 594 (60 440 to 60 749) | 82 871 (1.37) | 22 277 (22 122 to 22 431) | 250.8 | 18 180 | 81.6 |
| New Mexico | 15 294 (15 233 to 15 354) | 19 466 (1.27) | 4172 (4112 to 4233) | 199.0 | 2792 | 66.9 |
| New York | 126 811 (126 571 to 127 050) | 175 160 (1.38) | 48 349 (48 110 to 48 589) | 248.5 | 38 596 | 79.8 |
| North Dakota | 6079 (6049 to 6109) | 7590 (1.25) | 1511 (1481 to 1541) | 198.3 | 1428 | 94.5 |
| Ohio | 100 843 (100 632 to 101 054) | 123 114 (1.22) | 22 271 (22 060 to 22 482) | 190.5 | 15 178 | 68.2 |
| Oklahoma | 32 559 (32 455 to 32 662) | 39 410 (1.21) | 6851 (6748 to 6955) | 173.1 | 5254 | 76.7 |
| Oregon | 30 551 (30 451 to 30 650) | 34 063 (1.11) | 3512 (3413 to 3612) | 83.3 | 1558 | 44.4 |
| Pennsylvania | 109 953 (109 732 to 110 173) | 133 247 (1.21) | 23 294 (23 074 to 23 515) | 182.0 | 18 690 | 80.2 |
| Rhode Island | 8719 (8679 to 8759) | 10 408 (1.19) | 1689 (1649 to 1729) | 159.4 | 1873 | 110.9 |
| South Carolina | 41 606 (41 483 to 41 729) | 50 518 (1.21) | 8912 (8789 to 9035) | 173.1 | 5545 | 62.2 |
| South Dakota | 6882 (6849 to 6915) | 8766 (1.27) | 1884 (1851 to 1917) | 213.0 | 1666 | 88.4 |
| Tennessee | 62 606 (62 446 to 62 765) | 75 504 (1.21) | 12 898 (12 739 to 13 058) | 188.9 | 8027 | 62.2 |
| Texas | 168 716 (168 432 to 168 999) | 218 242 (1.29) | 49 526 (49 243 to 49 810) | 170.8 | 33 828 | 68.3 |
| Utah | 15 985 (15 922 to 16 048) | 18 905 (1.18) | 2920 (2857 to 2983) | 91.1 | 1618 | 55.4 |
| Vermont | 4837 (4812 to 4862) | 5217 (1.08) | 380 (355 to 405) | 60.9 | 106 | 27.9 |
| Virginia | 57 788 (57 637 to 57 940) | 67 478 (1.17) | 9690 (9538 to 9841) | 113.5 | 6244 | 64.4 |
| Washington | 47 196 (47 063 to 47 328) | 53 159 (1.13) | 5963 (5831 to 6096) | 78.3 | 3662 | 61.4 |
| West Virginia | 18 970 (18 899 to 19 041) | 21 332 (1.12) | 2362 (2291 to 2433) | 131.8 | 1535 | 65.0 |
| Wisconsin | 45 013 (44 884 to 45 143) | 53 256 (1.18) | 8243 (8113 to 8372) | 141.6 | 6325 | 76.7 |
| Wyoming | 3890 (3869 to 3912) | 4734 (1.22) | 844 (822 to 865) | 145.8 | 416 | 49.3 |
Seasonally adjusted death counts predicted by regression model (see Methods).
Values shown are not annual mortality rates. The numerator counts only excess deaths that occurred between March 1, 2020, and January 2, 2021.
COVID-19 deaths include deaths in which COVID-19 was identified as the underlying or a contributing cause of death (among multiple causes of death). COVID-19 deaths in Hawaii, Massachusetts, and Rhode Island exceeded the estimate for excess deaths, in part because observed deaths from other causes were lower than would be predicted according to historic norms.
The US total was calculated as the sum of results for 49 states and the District of Columbia. North Carolina was omitted because of delays in reporting.
Figure. Excess Deaths by Regions, March 1, 2020, to January 2, 2021.
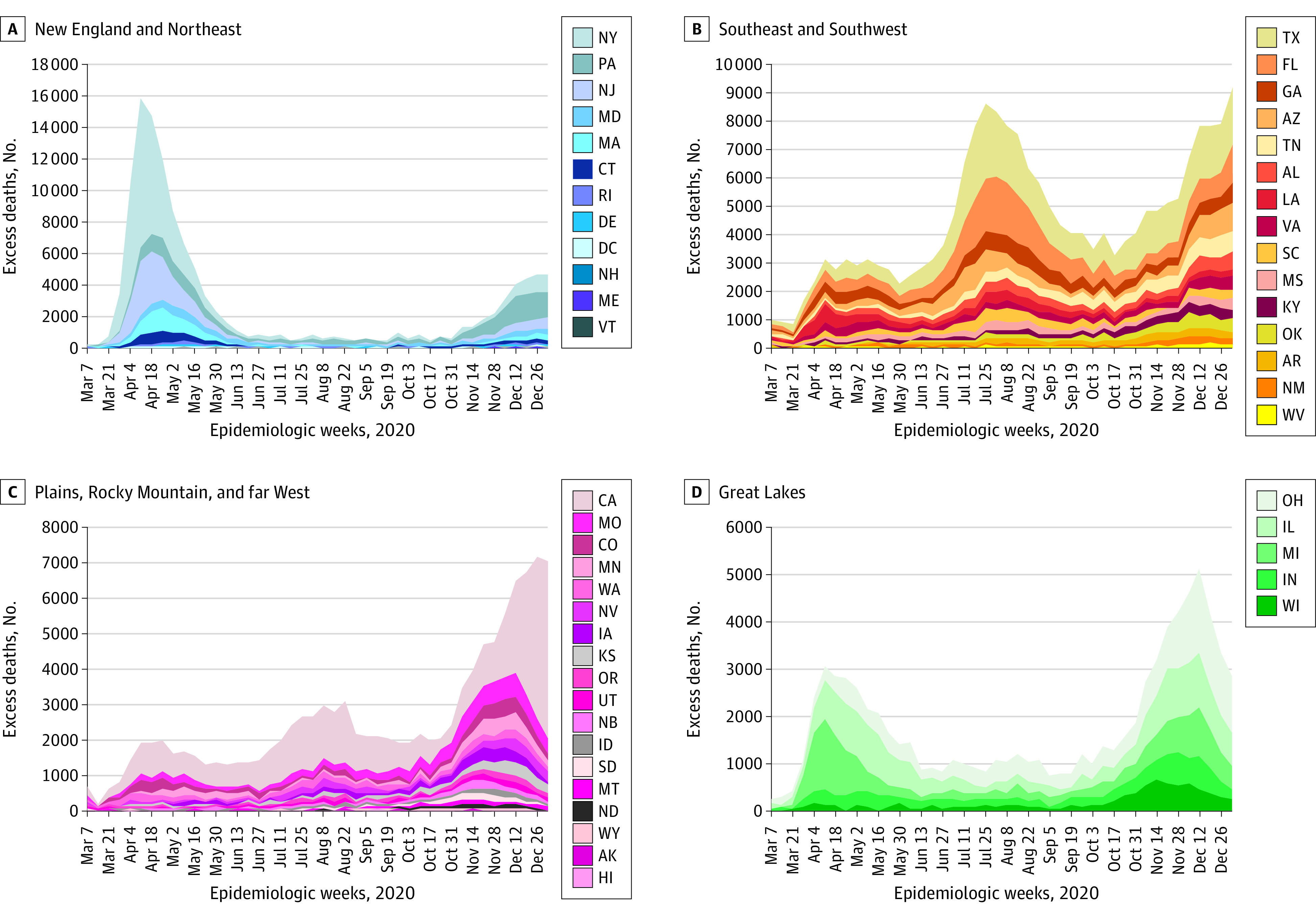
State data plotted from 8 regions, as defined by the US Bureau of Economic Analysis. Surge patterns were independently examined for each of the 8 regions (Supplement); epidemic patterns were similar and could be merged as shown, except a bimodal pattern in the Great Lakes region was distinctive and plotted separately. Negative excess deaths were plotted as zero. State-level data are available on request.
Joinpoint analyses revealed an increase in weekly mortality from non–COVID-19 causes, including heart disease from March 15 to April 11, 2020 (APC, 4.9 [95% CI, 0.7-9.3]), and from October 11, 2020, to January 2, 2021 (APC, 1.1 [95% CI, 0.8-1.4]); Alzheimer disease/dementia from March 15 to April 11, 2020 (APC, 7.1 [95% CI, 2.4-12.0]), from May 31 to August 15, 2020 (APC, 1.2 [95% CI, 0.7-1.6]), and from September 6, 2020, to January 2, 2021 (APC, 1.3 [95% CI, 1.1-1.5]); and diabetes from March 8 to April 11, 2020 (APC, 6.5 [95% CI, 2.8-10.3]), from May 31 to July 11, 2020 (APC, 2.6 [95% CI, 0.2-5.0]), and from October 18, 2020, to January 2, 2021 (APC, 2.2 [95% CI, 1.6-2.8]).
Discussion
The 22.9% increase in all-cause mortality reported here far exceeds annual increases observed in recent years (≤2.5%). The percentage of excess deaths among non-Hispanic Black individuals (16.9%) exceeded their share of the US population (12.5%),5 reflecting racial disparities in COVID-19 mortality. Excess deaths surged in the east in April, followed by extended summer and early winter surges concentrated in southern and western states, respectively. Many of these states weakly embraced, or discouraged, pandemic control measures and lifted restrictions earlier than other states.1,6
Excess deaths not attributed to COVID-19 could reflect either immediate or delayed mortality from undocumented COVID-19 infection, or non–COVID-19 deaths secondary to the pandemic, such as from delayed care or behavioral health crises. Death rates from several non–COVID-19 diseases (eg, heart disease, Alzheimer disease) increased during surges. The model does not adjust directly for population aging, which could contribute to an overestimate of excess deaths. Other study limitations include reliance on provisional data, inaccurate death certificates, and modeling assumptions.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
eTable. Grouped Cause Data Reported by the Centers for Disease Control and Prevention
eFigure. Analysis of Regional Patterns
eReferences
References
- 1.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324(15):1562-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weekly counts of deaths by state and select causes, 2014-2019. Centers for Disease Control and Prevention. Accessed January 22, 2021. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/3yf8-kanr
- 3.Weekly counts of deaths by state and select causes, 2020-2021. Centers for Disease Control and Prevention. Accessed March 10, 2021. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/muzy-jte6
- 4.Weekly counts of deaths by jurisdiction and race and Hispanic origin. Centers for Disease Control and Prevention. Accessed March 10, 2021. https://data.cdc.gov/NCHS/Weekly-counts-of-deaths-by-jurisdiction-and-race-a/qfhf-uhaa
- 5.Single-race population estimates 2010-2019. CDC WONDER. Accessed February 17, 2021. http://wonder.cdc.gov/single-race-single-year-v2019.html
- 6.Chaney S, Mackrael K. With fewer Covid-19 restrictions, South’s economy outperforms nation. Wall Street Journal. Published October 17, 2020. Accessed March 10, 2021. https://www.wsj.com/articles/with-fewer-covid-restrictions-souths-economy-outperforms-nation-11602927000
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Grouped Cause Data Reported by the Centers for Disease Control and Prevention
eFigure. Analysis of Regional Patterns
eReferences


