Summary
The currently accepted assumption that most surgical site infections (SSIs) occurring after elective surgery under standard methods of antisepsis are due to an intraoperative contamination event, remains unproven. We examined the available evidence in which microbial cultures of surgical wounds were taken at the conclusion of an operation and determined that such studies provide more evidence to refute that an SSI is due to intraoperative contamination than support it. We propose that alternative mechanisms of SSI development should be considered, such as when a sterile postoperative wound becomes infected by a pathogen originating from a site remote from the operative wound—eg, from the gums or intestinal tract (ie, the Trojan Horse mechanism). We offer a path forward to reduce SSI rates after elective surgery that includes undertaking genomic-based microbial tracking from the built environment (ie, the operating room and hospital bed), to the patient’s own microbiome, and then to the surgical site. Finally, we posit that only by generating this dynamic microbial map can the true pathogenesis of SSIs be understood enough to inform novel preventive strategies against infection following elective surgery in the current era of asepsis.
Introduction
Surgical site infections (SSIs) most often develop at the operative site and include the deep spaces of the surgical field adjacent to the operated organ (hip, colon, pelvis, or brain) and the entry wound (fascia, subcutaneous tissue, or skin).1, 2 SSI experts including surgeons, infectious disease specialists, quality officers, and infection control nurses invariably consider SSIs to be a function of the microbial burden of a given tissue site balanced against the immune response of the host.3 Yet what is routinely dismissed in this simplistic framework is the common and routine observation that even when patients present with a high microbial burden (eg, perforated diverticulitis with peritonitis or penetrating trauma, etc), a SSI does not occur in most cases (>80%).2, 4, 5 Conversely, when a liver transplant patient develops an infection, it is attributed to the general immunosuppressed state of the patient. Again, what is routinely dismissed in this assertion is the fact that most liver transplant patients (>70%) do not develop SSIs despite opening of the intestinal track in a patient who is immunocompromised and colonised by health-care-associated pathogens.6
Are most SSIs caused by intraoperative contamination?
To suggest that the majority of SSIs are due to intraoperative contamination would require matching the exact organism present at the surgical site (eg, wound, peritoneum, hip, or thoracic cavity) at the end of the operation to the pathogen involved in the clinically evident SSI. Were today’s technology applied to such a study, not only would isolation of the species within the wound be possible, but the exact strain (subspecies with a genomic average nucleotide identity >98%; termed genotype) could be matched to the strain isolated within the SSI. This approach would then permit one to conclude that the very pathogen present in the wound at the end of the surgical procedure was the one that caused the SSI, because it is highly improbable that two strains with such high genomic synteny will be encountered in contiguous systems. Although genotypes of strains can be matched rapidly and accurately,7 this approach has not yet been reported for SSIs.
In the largest culture-based study reported to date,8 among 1852 patients, 120 (6·5%) developed SSIs.8 Within the 276 patients who had a positive intraoperative culture in this study, 38 (13·8%) subsequently developed wound infections. This finding indicates that more than 80% of patients with a positive wound culture at the end of surgery did not develop an infection. In addition, a substantial number of patients in whom the wound culture was negative developed an SSI. Although patients with positive intraoperative cultures had a relevant increased rate of infection, not only was the predictive value of the culture result low, but it also had a high false-positive rate. Furthermore, many, if not most, pathogens that caused postoperative SSIs in this study did not match those cultured at the end of the surgery. The authors concluded that the lack of culture concordance and a high proportion of false-positive and false-negative results effectively dissociates intraoperative contamination with postoperative SSI.
In an often-cited study of 100 consecutive colon surgeries, patients had culture swabs of their wounds taken after the operation and were prospectively followed up for SSI development.9 52 swabs were sterile and none of these patients developed a wound infection. In total, 48 were positive, of which only ten developed an SSI for a predictive rate for developing an SSI of 18%. Again, although more than 80% of the wounds that tested positive did not develop an SSI, the authors concluded that intraoperative contamination is a major cause of subsequent wound infection. They further concluded that intraoperative cultures “have the best predictive value for assessing the likelihood of subsequent wound infection”.9
Finally, before 1990, most cholecystectomies were done using an open incision that had an SSI rate (proportion of patients who developed an SSI) as high as 15%.10 Today, an elective laparoscopic cholecystectomy is an outpatient procedure with a more than 1·0% SSI rate, and many have suggested that prophylactic antibiotic use is unnecessary.11 Studies in which bile is routinely cultured during a laparoscopic or open cholecystectomy again show no correlation between the bile cultures and the pathogens involved in the SSI.12, 13
SSI and Staphylococcus aureus
The organism most commonly associated with a prosthetic-related orthopaedic SSI is Staphylococcus aureus, presumed to be from the skin adjacent to the surgical site.14, 15 When a S aureus SSI develops following a joint replacement operation, it is routinely concluded that the source of the organism must be from the adjacent skin or the operating room environment, resulting from either inadequate decontamination—eg, during skin preparation, inappropriate antibitoic choice, or breach in sterile technique. If a latent SSI develops (weeks to months following the initial operation), the same mechanism is invoked, only the strain is presumed to have remained dormant in a biofilm, and postulated to occur when an undefined immunosuppressive condition has emerged allowing the organism to cause an infection.16, 17
The results of multiple studies spanning over 30 years and across multiple countries repeatedly show that positive results from intraoperative swabs during joint replacement surgery do not predict the occurrence of a prosthetic joint SSI.18, 19, 20, 21 Even when PCR-based bacterial detection is used,22 the occurrence of false positive results is so high that it provides no insight into how clinical infections develop. Currently, the most popular trend for SSI prevention in orthopaedic surgery is to apply vancomycin powder at the conclusion of the operation, which is particularly popular in spinal surgery. The results of randomised trials of vancomycin powder in spinal surgery are mixed and inconclusive.20 None of the studies claims to understand how vancomycin is protective.
One of the most interesting findings in this series of studies is the emergence of non-S aureus, polymicrobial Gram-negative, postoperative infections23 with the use of vancomycin powder—a classic tradeoff scenario.20 Although S aureus is clearly the most common pathogen associated with a postoperative spinal SSI (45%), what remains unclear is the exact source of the pathogen. When no vancomycin is administered, the high prevalence of S aureus is presumed to be from environmental contamination—eg, from the skin adjacent to the wound or instruments used to perform the surgery. However, when vancomycin is used and Gram-negative bacteria appear, no explanation is offered. This bias is the reason that most prevention strategies (eg, barrier protectors, irrigants, high-efficiency particulate air-filters, space suits, and vacuum-assisted wound-closure systems) are aimed at reducing environmental wound contamination,24, 25 but lack culture or sequence-based evidence to show that lower intraoperative wound contamination can be causally linked to lower SSI incidence. Again, most data generated from prosthetic-related SSIs refute the concept that direct intraoperative contamination is indeed the major cause of SSI. In some cases, the use of space suits and vancomycin powder has increased wound infections rates.26, 27
We have introduced the so-called Trojan Horse hypothesis to explain SSI pathogenesis and inconsistencies in the literature.28 This hypothesis proposes that pathogens remote from the SSI area—such as within the teeth, gums, or gastrointestinal tract—can be taken up by immune cells (macrophages or neutrophils) and travel to the wound site where they cause wound infections. We showed this mechanism in mice using methicillin-resistant S aureus (MRSA) and observed that gut MRSA can be taken up by neutrophils, travel via the bloodstream to a wound site, and cause an SSI. This mechanism may explain why some infections occur latently following surgery and are due to organisms not found in the wound at the end of the operation.29 This mechanism may also explain why oral hygiene practices applied to patients before major surgery prevents surgical site infections.30 New genotyping and in-situ visualisation approaches (eg, CLASI-FISH) are now poised to formally test the Trojan Horse hypothesis of SSI.31 Although the Trojan Horse hypothesis has been proposed in other fields, its application to SSIs has not been previously considered.32 This mechanism has also been applied to explain the pathogenesis of Alzheimer’s disease.33 However, amid the excitement that a gum and tooth pathogen (eg, Porphyromonas gingivalis) has been isolated in the brain tissue of humans with Alzheimer’s disease, is the striking lack of any discussion on how these neuron-destroying, dementia-producing organisms silently find their way from the mouth to the brain. Although harbouring potential infection-causing organisms in protected niches (eg, periodontal tissue or caecal crypts)34 might increase the risk of disease, such analyses remain probabilistic and not deterministic. For example, while intestinal bacteria can produce amyloid, they also can affect wound healing remote from the intestine.35, 36 Therefore the precise mechanism of Alzheimer’s disease and the role of the microbiome has yet to be determined, and multiple contingencies must be fulfilled for a pathogen to result in a clinical infection or a particular disease phenotype (Figure).
Figure. Trojan Horse hypothesis of surgical site infection.
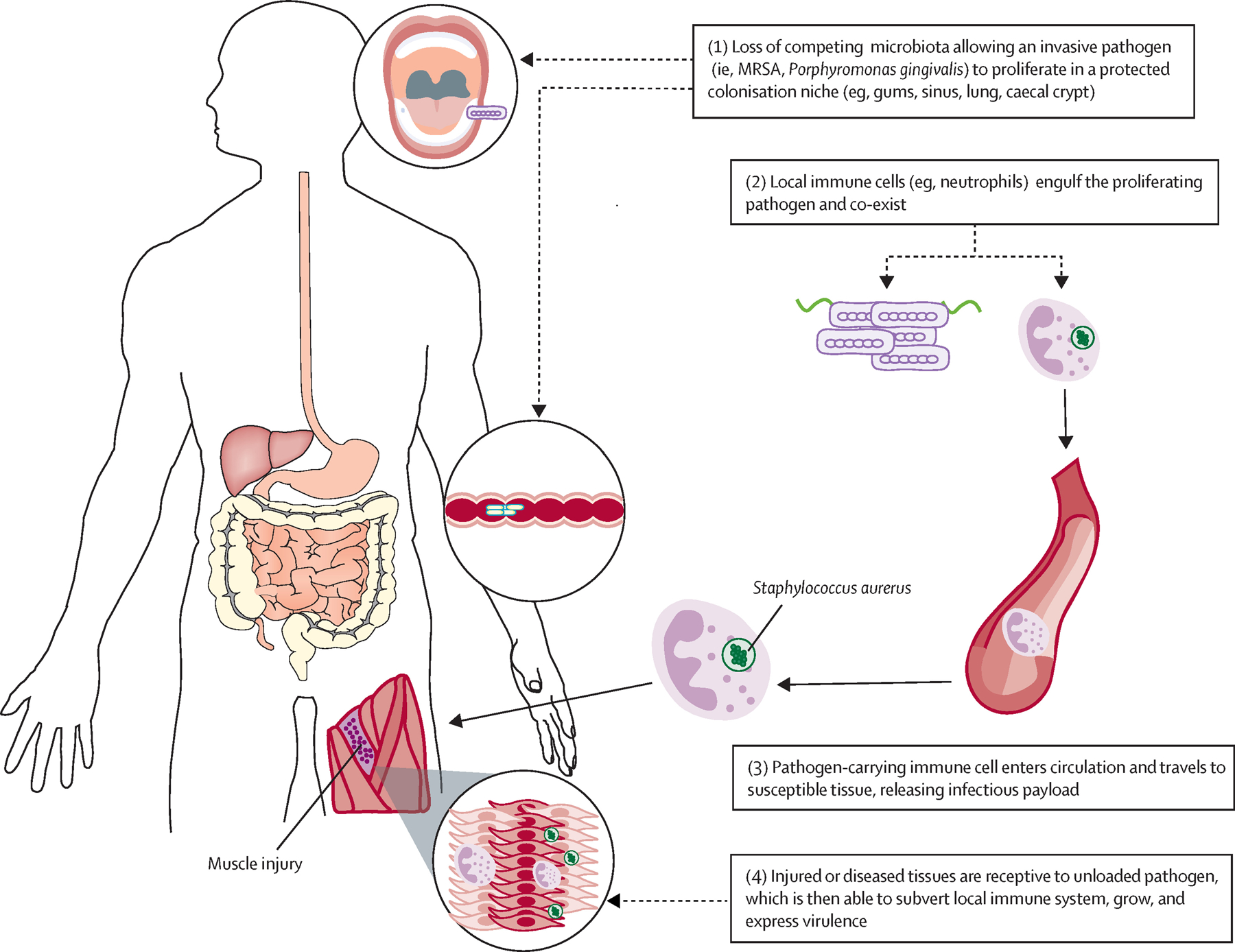
Representation of the mechanisms by which microbes remote from the site of actual infection can cause a surgical site infection. MRSA=methicillin-resistant Staphylococcus aureus.
Understanding the role of individual elements within bundled care
Most complex gastrointestinal surgery—such as colon resection, pancreaticoduodenectomy, and liver transplantation—now experience unprecedented low lengths of stay of 3–5 days. Much of this improvement is attributed to bundled care within enhanced recovery programmes.37, 28 The main pillars of enhanced recovery programmes include use of bowel preparation, minimally invasive approaches, avoidance of opioids, and feeding with solid food as early as possible.39 If we breakdown each of these care processes, it becomes obvious that enhanced recovery programmes may be a method to socialise the application of advanced medicine to patients across various hospitals and health-care providers.40, 41 Enhanced recovery programmes could reduce SSI rates by enforcing the use of mechanical bowel-preparation (ie, less intraoperative contamination), by earlier discharge from the hospital (ie, less possibility for contamination with health-care-associated pathogens), use of minimally invasive surgery (ie, smaller incisions made and less chance for direct contamination), and less use of opioids (ie, which cause immunosuppression and activate bacterial virulence).43, 44, 45, 46, 47 All these proposed mechanisms make sense; however, none is actually proven to be causally linked to lower SSI rates in patients entered into enhanced recovery programmes.48
In most studies applying enhanced recovery programmes to reduce SSIs, results are compared with a historical control group whose aggregate SSI rate is often between 10% and 15%, which is considered to be high.2, 49 Application of enhanced recovery after surgery (ERAS) reduces the SSI rate to around 7% (considered a median SSI rate, even for non-ERAS hospitals), thus realising a near 50% reduction in SSI. Yet there is no accounting for the within-group differences.50 For example, why did 85% of the historical controls not develop an SSI? Conversely, even when ERAS was applied in such studies, what is the mechanism by which the remaining 7% developed SSIs?
Studies in which laparoscopic colectomy is compared with open surgery demonstrate that “the reduction in morbidity seems to be due to laparoscopy rather than [enhanced recovery programmes]”.51 Laparoscopy is known to reduce postoperative pain and thus this alone could select for patients who can eat normal (ie, solid and unprocessed) food earlier because their ileus is less, their inflammatory response is less, and thus they are more resilient and recover sooner. Therefore, it is time to establish why, at the individual patient level, SSIs develop in the first place.48
Oral antibiotics in colon surgery
The introduction of oral non-absorbable antibiotics before colon surgery was a major advance in reducing SSI, anastomotic leaks, and even mortality, which in the early 1970s approached 20%.52, 53 It seemed intuitive that during colon surgery, direct peritoneal and wound contamination by stool would be the major cause of SSI and peritonitis, although again, wound cultures did not predict postoperative SSIs even in these earlier studies.52 From the 1980s to the 1990s, wound and peritoneal cultures showed that microbial species present in the SSIs were mostly members of the colonic microbiota, confirming the bias that oral antibiotic decontamination of the colon microbiota reduces direct contamination of the wound during surgery.52, 53, 54, 55 Yet animal studies show that intestinal bacteria, which resemble the species that the oral antibiotics target, can translocate from the normal gut and infect otherwise sterile material placed into the peritoneal cavity.56 This study and others raised the suspicion that simply culturing species in an infected wound that resemble those normally present in the gut does not necessarily imply that they caused the SSI via direct environmental wound contamination.
As SSI rates and mortality rates rapidly diminished in the 1990s and broader single agent parenteral antibiotics entered the market, surgeons began to question the need for oral antibiotics and purgative cleansing before colon surgery. Furthermore, with improvements in anaesthesia and laparoscopy, surgeons became emboldened to eliminate both oral antibiotics and purgative cleansing of the bowel.57, 58, 59 Yet in the past 10 years, at least in the USA, oral antibiotics before colon surgery have made a major comeback and are now considered to be standard of care.60, 61, 62, 63 However, in Europe, surgeons remain sceptical. A 2019 prospective randomised trial from Finland showed no difference in SSI rates or anastomotic leak rates between oral antibiotic or purgative cleansing treated versus non-treated patients,64 whereas a study from the Netherlands challenged this result.65 Few, if any of such studies have provided meaningful microbiological analyses to explain this disparity. This is unfortunate given that approximately 50% of the microbes causing SSI today have been shown to be resistant to the antibiotics used for prophylaxis.66
Additional wound protection during surgery
From the time of Semmelweis and Lister to today, maintaining sterility in the operating room has been an effective priority to limit SSI. Thanks to these efforts, today SSI rates are at a historic low when such rigorous standards are applied. We do not argue against the importance of current methods to maintain sterility in the operating room, but rather assert that at current rates where SSIs are less common, a strategy of enforcing a greater degree of sterility to further reduce infection lacks a scientific premise. For example, if wound protectors prevent SSIs, is the mechanism proven to be due to additional shielding against environmental pathogens? Or does the wound protector cause less trauma and ischaemia to the tissues rendering them less vulnerable to subsequent bacterial invasion?
Along this line of reasoning, infection following breast augmentation surgery is again assumed to be a result of local wound contamination during surgery.67, 68 Such infections occur at a rate of 1–3% with many infections developing weeks to months following surgery. To date, all efforts to reduce breast implant infections are aimed at limiting intraoperative contamination—alternative mechanisms of infection incorporating the Trojan Horse hypothesis of SSI have not been considered.
Finally, when clinical SSI rates are retrospectively mapped to the use of high-efficiency particulate air (HEPA) filters, space suits, or the use of head covering bouffants, they typically lack any meaningful wound culture data and often show no effect on clinical SSI rates.69, 70 The sophistry of these debates, as recently documented regarding the use of head-covering bouffants and perioperative disposable jackets, shows how recommendations are made in the complete absence of critical pathogen-identification data.71, 72
Conclusion
In the Memoirs of Sherlock Holmes by Sir Arthur Conan Doyle written in 1892, one of the stories is Silver Blaze. It involves the disappearance of a famous racehorse the night before a race and the murder of the horse’s trainer. The mystery is ultimately solved by Mr Holmes, in part, by recognising that no one he interviewed as part of his investigation mentioned hearing the watchdog bark during the night. The Scotland Yard detective remarked: “is there any other point to which you would wish to draw my attention?” Holmes replied: “to the curious incident of the dog in the night-time”. The response: “the dog did nothing in the night-time.” Holmes: “that was the curious incident.” The idea that there was actually no response by the watchdog was the curious incident that ended up solving the mystery.
The curious incident in the operating room is that breaches in sterile technique regularly occur yet, in most cases, an SSI does not. The fact that the “dog did nothing”—meaning the intraoperative contamination event (ie, such as the spillage of bowel contents, treatment of gross peritonitis, etc) did not cause an infection, is not only remarkable, but tells an important part of the story of how SSIs might actually develop in the first place.
Today, under currently accepted standards, the SSI rate following clean, clean-contaminated, contaminated, and dirty procedures are 1·76%, 3·94%, 4·75%, and 5·16%, respectively, according to a recent analysis of over 600 000 cases.2 Almost all new products, including irrigants, wound protectors, gels, topical antibiotics in collagen sponges and powders, tapes, and skin glues are designed to reduce SSI rates by decreasing intraoperative and postoperative direct environmental wound contamination.73 These approaches belie the observation that when surgeons make a colostomy, suture the colon to the skin and place a bag over it (ie, creating the so-called greenhouse effect) almost never does this area become infected.
To conclude, we recommend undertaking next-generation microbial sequencing at the strain level, to track microbial movement across the built environment (eg, wards, beds, and operating room) to the hair and skin of the operating-room personnel, to the exposed surgical wound and operative field, and then finally to the actual clinical SSI.74 With the use of metagenomics and RNA sequencing technology, exact sequence variants can be tracked and a dynamic map of the migration of individual microbes and their associated communities from their original site of colonisation to the surgical wound and to the actual clinical infection site can be drawn.75 With this critical information, several points of interdiction can be identified and novel therapies rationally designed. These may include application of mouth hygiene, personalised diets and bowel preparations, faecal transplants to eliminate multidrug resistant pathogens, and the development of non-antibiotic agents that seek to collaborate with the microbiome rather than non-selectively eliminate it.
Acknowledgments
John C Alverdy is supported by a grant from National Institutes of Health (5R01GM062344–18).
Footnotes
Declaration of interests
JCA is co-founder of Covira Surgical and is past consultant with Applied Medical. JG is president of BiomeSense Inc. NH declares no conflicts of interests.
References
- 1.Waltz PK, Zuckerbraun BS. Surgical site infections and associated operative characteristics. Surg Infect (Larchmt), 18 (2017), pp. 447–450 [DOI] [PubMed] [Google Scholar]
- 2.Ortega G, Rhee DS, Papandria DJ, et al. An evaluation of surgical site infections by wound classification system using the ACS-NSQIP. J Surg Res, 174 (2012), pp. 33–38 [DOI] [PubMed] [Google Scholar]
- 3.Bashaw MA, Keister KJ. Perioperative strategies for surgical site infection prevention. AORN J, 109 (2019), pp. 68–78 [DOI] [PubMed] [Google Scholar]
- 4.Leaper DK. Evidence update on prevention of surgical site infection. Curr Opin Infect Dis, 28 (2015), pp. 158–163 [DOI] [PubMed] [Google Scholar]
- 5.Azoury SC, Farrow NE, Hu QL, et al. Postoperative abdominal wound infection—epidemiology, risk factors, identification, and management. Chronic Wound Care M, 2 (2015), pp. 137–148 [Google Scholar]
- 6.Natori Y, Kassar R, Iaboni A, et al. Surgical site infections after liver transplantation: prospective surveillance and evaluation of 250 transplant recipients in Canada. Infect Control Hosp Epidemiol, 38 (2017), pp. 1084–1090 [DOI] [PubMed] [Google Scholar]
- 7.Gardy JL, Loman NJ. Towards a genomics-informed, real-time, global pathogen surveillance system. Nat Rev Genet, 19 (2018), pp. 9–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garibaldi RA, Cushing D, T Lerer. Predictors of intraoperative-acquired surgical wound infections. J Hosp Infect, 18 (1991), pp. 289–298 [DOI] [PubMed] [Google Scholar]
- 9.Fa-Si-Oen PR, Kroeze F, Verhoef LH, Verwaest C, Roumen RM. Bacteriology of abdominal wounds in elective open colon surgery: a prospective study of 100 surgical wounds. Clin Microbiol Infect, 11 (2005), pp. 155–157 [DOI] [PubMed] [Google Scholar]
- 10.Pollock AV, Evans M. Wound sepsis after cholecystectomy: effect of incidental appendicectomy. BMJ, 1 (1977), pp. 20–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomez-Ospina JC, Zapata-Copete JA, Bejarano M, Garcia-Perdomo HA. Antibiotic prophylaxis in elective laparoscopic cholecystectomy: a systematic review and network meta-analysis. J Gastrointest Surg, 22 (2018), pp. 1193–1203 [DOI] [PubMed] [Google Scholar]
- 12.den Hoed PT, Boelhouwer RU, Veen HF, Hop WC, Bruining HA. Infections and bacteriological data after laparoscopic and open gallbladder surgery. J Hosp Infect, 39 (1998), pp. 27–37 [DOI] [PubMed] [Google Scholar]
- 13.Grande M, Torquati A, Farinon AM. Wound infection after cholecystectomy. Correlation between bacteria in bile and wound infection after operation on the gallbladder for acute and chronic gallstone disease. Eur J Surg, 158 (1992), pp. 109–112 [PubMed] [Google Scholar]
- 14.Alamanda VK, Springer BD. The prevention of infection. Bone Joint J, 101-B (2019), pp. 3–9 [DOI] [PubMed] [Google Scholar]
- 15.Alamanda VK, Springer BD. Perioperative and modifiable risk factors for periprosthetic joint infections (PJI) and recommended guidelines. Curr Rev Musculoskelet Med, 11 (2018), pp. 325–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller KE, Hontanilla B, Cabello A, Marre D, Armendariz L, Leiva J. The effect of late infection and antibiotic treatment on capsular contracture in silicone breast implants: a rat model. J Plast Reconstr Aesthet Surg, 69 (2016), pp. 70–76 [DOI] [PubMed] [Google Scholar]
- 17.Koo H, Allan RN, Howlin RP, Stoodley P, Hall-Stoodley L. Targeting microbial biofilms: current and prospective therapeutic strategies. Nat Rev Microbiol, 15 (2017), pp. 740–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andrade N, Schmiedt CW, Cornell K, et al. Survey of intraoperative bacterial contamination in dogs undergoing elective orthopedic surgery. Vet Surg, 45 (2016), pp. 214–222 [DOI] [PubMed] [Google Scholar]
- 19.Gelalis ID, Arnaoutoglou CM, Politis AN, Batzaleksis NA, Katonis PG, Xenakis TA. Bacterial wound contamination during simple and complex spinal procedures. A prospective clinical study. Spine J, 11 (2011), pp. 1042–1048 [DOI] [PubMed] [Google Scholar]
- 20.Kang DG, Holekamp TF, Wagner SC, Lehman RA Jr. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J, 15 (2015), pp. 762–770 [DOI] [PubMed] [Google Scholar]
- 21.Parvizi J, Barnes S, Shohat N, Edmiston CE Jr. Environment of care: is it time to reassess microbial contamination of the operating room air as a risk factor for surgical site infection in total joint arthroplasty? Am J Infect Control, 45 (2017), pp. 1267–1272 [DOI] [PubMed] [Google Scholar]
- 22.Panousis K, Grigoris P, Butcher I, Rana B, Reilly JH, Hamblen DL. Poor predictive value of broad-range PCR for the detection of arthroplasty infection in 92 cases. Acta Orthop, 76 (2005), pp. 341–346 [PubMed] [Google Scholar]
- 23.Grabel ZJ, Boden A, Segal DN, Boden S, Milby AH, Heller JG. The impact of prophylactic intraoperative vancomycin powder on microbial profile, antibiotic regimen, length of stay, and reoperation rate in elective spine surgery. Spine J, 19 (2019), pp. 261–266 [DOI] [PubMed] [Google Scholar]
- 24.Jain S, Reed M. Laminar air flow handling systems in the operating room. Surg Infect (Larchmt), 20 (2018), pp. 151–158 [DOI] [PubMed] [Google Scholar]
- 25.Papaconstantinou HT, Birnbaum EH, Ricciardi R, et al. Impact of a novel surgical wound protection device on observed versus expected surgical site infection rates after colectomy using the national surgical quality improvement program risk calculator. Surg Infect (Larchmt), 20 (2019), pp. 35–38 [DOI] [PubMed] [Google Scholar]
- 26.Vijaysegaran P, Knibbs LD, L Morawska, Crawford RW. Surgical space suits increase particle and microbiological emission rates in a simulated surgical environment. J Arthroplasty, 33 (2018), pp. 1524–1529 [DOI] [PubMed] [Google Scholar]
- 27.Gande A, Rosinski A, Cunningham T, Bhatia N, Lee YP. Selection pressures of vancomycin powder use in spine surgery: a meta-analysis. Spine J, 19 (2019), pp. 1076–1084 [DOI] [PubMed] [Google Scholar]
- 28.Krezalek MA, Hyoju S, Zaborin A, et al. Can methicillin-resistant Staphylococcus aureus silently travel from the gut to the wound and cause postoperative infection? Modeling the “Trojan horse hypothesis”. Ann Surg, 267 (2018), pp. 749–758 [DOI] [PubMed] [Google Scholar]
- 29.Garvin KL, Miller RE, Gilbert TM, White AM, Lyden ER. Late reinfection may recur more than 5 years after reimplantation of THA and TKA: analysis of pathogen factors. Clin Orthop Relat Res, 476 (2018), pp. 345–352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nobuhara H, Yanamoto S, Funahara M, et al. Effect of perioperative oral management on the prevention of surgical site infection after colorectal cancer surgery: a multicenter retrospective analysis of 698 patients via analysis of covariance using propensity score. Medicine (Baltimore), 97 (2018), Article e12545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valm AM, Mark Welch JL, Rieken CW, et al. Systems-level analysis of microbial community organization through combinatorial labeling and spectral imaging. Proc Natl Acad Sci USA, 108 (2011), pp. 4152–4157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thwaites GE, Gant V. Are bloodstream leukocytes Trojan horses for the metastasis of Staphylococcus aureus? Nat Rev Microbiol, 9 (2011), pp. 215–222 [DOI] [PubMed] [Google Scholar]
- 33.Wu Z, Nakanishi H. Connection between periodontitis and Alzheimer’s disease: possible roles of microglia and leptomeningeal cells. J Pharmacol Sci, 126 (2014), pp. 8–13 [DOI] [PubMed] [Google Scholar]
- 34.Zaborin A, Krezalek M, Hyoju S, et al. Critical role of microbiota within cecal crypts on the regenerative capacity of the intestinal epithelium following surgical stress. Am J Physiol Gastrointest Liver Physiol, 312 (2017), pp. G112–G122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Canesso MC, Vieira AT, Castro TB, et al. Skin wound healing is accelerated and scarless in the absence of commensal microbiota. J Immunol, 193 (2014), pp. 5171–5180 [DOI] [PubMed] [Google Scholar]
- 36.Poutahidis T, Kearney SM, Levkovich T, et al. Microbial symbionts accelerate wound healing via the neuropeptide hormone oxytocin. PLoS One, 8 (2013), Article e78898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGee MF, Kreutzer L, Quinn CM, et al. Leveraging a comprehensive program to implement a colorectal surgical site infection reduction bundle in a statewide quality improvement collaborative. Ann Surg, 270 (2019), pp. 701–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weiser MR, Gonen M, Usiak S, et al. Effectiveness of a multidisciplinary patient care bundle for reducing surgical-site infections. Br J Surg, 105 (2018), pp. 1680–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg, 152 (2017), pp. 292–298 [DOI] [PubMed] [Google Scholar]
- 40.Ji HB, Zhu WT, Wei Q, Wang XX, Wang HB, Chen QP. Impact of enhanced recovery after surgery programs on pancreatic surgery: a meta-analysis. World J Gastroenterol, 24 (2018), pp. 1666–1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg, 101 (2014), pp. 172–188 [DOI] [PubMed] [Google Scholar]
- 43.Bell KL, Shohat N, Goswami K, Tan TL, Kalbian I, Parvizi J. Preoperative opioids increase the risk of periprosthetic joint infection after total joint arthroplasty. J Arthroplasty, 33 (2018), p. 3246 51.e1 [DOI] [PubMed] [Google Scholar]
- 44.Amodeo G, Bugada D, Franchi S, et al. Immune function after major surgical interventions: the effect of postoperative pain treatment. J Pain Res, 11 (2018), pp. 1297–1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meng J, Banerjee S, Li D, et al. Opioid exacerbation of gram-positive sepsis, induced by gut microbial modulation, is rescued by IL-17A neutralization. Sci Rep, 5 (2015), Article 10918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang F, Meng J, Zhang L, Johnson T, Chen C, Roy S. Morphine induces changes in the gut microbiome and metabolome in a morphine dependence model. Sci Rep, 8 (2018), Article 3596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Babrowski T, Holbrook C, Moss J, et al. Pseudomonas aeruginosa virulence expression is directly activated by morphine and is capable of causing lethal gut-derived sepsis in mice during chronic morphine administration. Ann Surg, 255 (2012), pp. 386–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bogue TL, Bogue RL. Unbundling the bundles: using apparent and systemic cause analysis to prevent health care-associated infection in pediatric intensive care units. Crit Care Nurs Clin North Am, 29 (2017), pp. 217–231 [DOI] [PubMed] [Google Scholar]
- 49.Keenan JE, Speicher PJ, Thacker JK, Walter M, Kuchibhatla M, Mantyh CR. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg, 149 (2014), pp. 1045–1052 [DOI] [PubMed] [Google Scholar]
- 50.Alverdy JC. Microbiome medicine: this changes everything. J Am Coll Surg, 226 (2018), pp. 719–729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc, 29 (2015), pp. 3443–3453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bartlett JG, Condon RE, Gorbach SL, Clarke JS, Nichols RL, Ochi S. Veterans administration cooperative study on bowel preparation for elective colorectal operations: impact of oral antibiotic regimen on colonic flora, wound irrigation cultures and bacteriology of septic complications. Ann Surg, 188 (1978), pp. 249–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clarke JS, Condon RE, Bartlett JG, Gorbach SL, Nichols RL, Ochi S. Preoperative oral antibiotics reduce septic complications of colon operations: results of prospective, randomized, double-blind clinical study. Ann Surg, 186 (1977), pp. 251–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nichols RL, Condon RE. Role of the endogenous gastrointestinal microflora in postoperative wound sepsis. Surgery Annu, 7 (1975), pp. 279–293 [PubMed] [Google Scholar]
- 55.Smith MB, Goradia VK, Holmes JW, McCluggage SG, Smith JW, Nichols RL. Suppression of the human mucosal-related colonic microflora with prophylactic parenteral and/or oral antibiotics. World J Surg, 14 (1990), pp. 636–641 [DOI] [PubMed] [Google Scholar]
- 56.Mora EM, Cardona MA, Simmons RL. Enteric bacteria and ingested inert particles translocate to intraperitoneal prosthetic materials. Arch Surg, 126 (1991), pp. 157–163 [DOI] [PubMed] [Google Scholar]
- 57.Soeters PB. The enhanced recovery after surgery (ERAS) program: benefit and concerns. Am J Clin Nutr, 106 (2017), pp. 10–11 [DOI] [PubMed] [Google Scholar]
- 58.Zmora O, Mahajna A, Bar-Zakai B, et al. Colon and rectal surgery without mechanical bowel preparation: a randomized prospective trial. Ann Surg, 237 (2003), pp. 363–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Basson MD. Oral antibiotics for colon surgery: the questions remain the same, as do the answers. JAMA Surg, 153 (2018), pp. 121–122 [DOI] [PubMed] [Google Scholar]
- 60.Rollins KE, Javanmard-Emamghissi H, Acheson AG, Lobo DN. The role of oral antibiotic preparation in elective colorectal surgery: a meta-analysis. Ann Surg, 270 (2019), pp. 43–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Klinger AL, Green H, Monlezun DJ, et al. The role of bowel preparation in colorectal surgery: results of the 2012–2015 ACS-NSQIP Data. Ann Surg, 269 (2019), pp. 671–677 [DOI] [PubMed] [Google Scholar]
- 62.Kiran RP, Murray AC, Chiuzan C, Estrada D, Forde K. Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg, 262 (2015), pp. 416–425 [DOI] [PubMed] [Google Scholar]
- 63.Scarborough JE, Mantyh CR, Sun Z, Migaly J. Combined mechanical and oral antibiotic bowel preparation reduces incisional surgical site infection and anastomotic leak rates after elective colorectal resection: an analysis of colectomy-targeted ACS NSQIP. Ann Surg, 262 (2015), pp. 331–337 [DOI] [PubMed] [Google Scholar]
- 64.Koskenvuo L, Lehtonen T, Koskensalo S, et al. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (MOBILE): a multicentre, randomised, parallel, single-blinded trial. Lancet, 394 (2019), pp. 840–848 [DOI] [PubMed] [Google Scholar]
- 65.Abis GSA, Stockmann H, Bonjer HJ, et al. Randomized clinical trial of selective decontamination of the digestive tract in elective colorectal cancer surgery (SELECT trial). Br J Surg, 106 (2019), pp. 355–363 [DOI] [PubMed] [Google Scholar]
- 66.Teillant A, Gandra S, Barter D, Morgan DJ, Laxminarayan R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modelling study. Lancet Infect Dis, 15 (2015), pp. 1429–1437 [DOI] [PubMed] [Google Scholar]
- 67.Rieger UM, Djedovic G, Pattiss A, et al. Presence of biofilms on polyurethane-coated breast implants: preliminary results. J Long Term Eff Med Implants, 26 (2016), pp. 237–243 [DOI] [PubMed] [Google Scholar]
- 68.Rieger UM, Raschke GF, Frei R, Djedovic G, Pierer G, Trampuz A. Role of bacterial biofilms in patients after reconstructive and aesthetic breast implant surgery. J Long Term Eff Med Implants, 24 (2014), pp. 131–138 [DOI] [PubMed] [Google Scholar]
- 69.Gaines S, Luo JN, Gilbert J, Zaborina O, Alverdy JC. Optimum operating room environment for the prevention of surgical site infections. Surg Infect (Larchmt), 18 (2017), pp. 503–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Farach SM, Kelly KN, Farkas RL, et al. Have recent modifications of operating room attire policies decreased surgical site infections? An American College of Surgeons NSQIP review of 6,517 patients. J Am Coll Surg, 226 (2018), pp. 804–813 [DOI] [PubMed] [Google Scholar]
- 71.Rios-Diaz AJ, Chevrollier G, Witmer H, et al. The art and science of surgery: do the data support the banning of surgical skull caps? Surgery, 164 (2018), pp. 921–925 [DOI] [PubMed] [Google Scholar]
- 72.Stapleton EJ, Frane N, Lentz JM, et al. Association of disposable perioperative jackets with surgical site infections in a large multicenter health care organization. JAMA Surg (2019) [DOI] [PMC free article] [PubMed]
- 73.Bennett-Guerrero E, Pappas TN, Koltun WA, et al. Gentamicin-collagen sponge for infection prophylaxis in colorectal surgery. N Engl J Med, 363 (2010), pp. 1038–1049 [DOI] [PubMed] [Google Scholar]
- 74.Lax S, Sangwan N, Smith D, et al. Bacterial colonization and succession in a newly opened hospital. Sci Transl Med, 9 (2017), Article eaah6500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gilbert JA, Lynch SV. Community ecology as a framework for human microbiome research. Nat Med, 25 (2019), pp. 884–889 [DOI] [PMC free article] [PubMed] [Google Scholar]


