Abstract
Objectives
The objectives were to describe the current procedural skill practices, attitudes toward procedural skill competency, and the role for educational skills training sessions among emergency medicine (EM) physicians within a geographic health zone.
Methods
This is a multicenter descriptive cross‐sectional survey of all EM physicians working at 12 emergency departments (EDs) within the Edmonton Zone in 2019. Survey items addressed current procedural skill performance frequency; perceived importance and confidence; current methods to maintain competence; barriers and facilitating factors to participation in a curriculum; preferred teaching methods; and desired frequency of practice for each procedural skill.
Results
Survey response rate was 53.6%. Variability in frequency of performed procedures was seen across the type of hospital sites. For the majority of skills, there was a significantly positive correlation between the frequency at which a skill was performed and the perceived confidence performing said skill. There was inconsistency and no significant correlation with perceived importance, perceived confidence or frequency performing a given skill, and the desired frequency of training for that skill. Course availability (76.2%) and time (72.8%) are the most common identified barriers to participation in procedural skills training.
Conclusions
This study summarized the current ED procedural skill practices among EM physicians in the Edmonton Zone and attitudes toward an educational curriculum for procedural skill competency. This represents a step toward targeted continuing professional development in staff physicians.
Procedural skills are a key component of an emergency medicine (EM) physician's practice. Procedures performed by an EM physician vary from high‐frequency low‐acuity procedures with small risk of complications to patients to high‐acuity low‐occurrence critical care skills that carry significant risks to patient safety. Physicians are expected to receive training to conduct these procedures during their medical school and/or residency program years. 1 , 2
Maintenance of procedural skills and ensuring physician competency are paramount to patient safety, highlighted by the increased mortality, morbidity, and prolonged hospitalizations that are associated with procedure‐related complications. 3 , 4 Confidence and refinement of these skills comes with procedural experience, 5 and such opportunities vary depending on the type of procedure, clinical volume, practice setting, and access to continuing medical education (CME). In some cases, rare procedures may never be performed on live or simulated patients until physicians are independent practitioners in the emergency department (ED). Similarly, there are often new skills introduced after the completion of a practitioners' residency training that may need to be integrated into their practice.
Competence‐based medical education (CBME) has become a significant component of postgraduate medical education (PGME) for curriculum and assessment in Canada. 6 , 7 , 8 With this paradigm, competence for a defined list of procedural skills is assessed in trainees 9 , 10 and the role of simulation in clinical education has become increasingly important. 6 Although this shift to a competency‐based assessment paradigm has been steadily integrated into postgraduate training programs, there is a paucity of data informing a comprehensive strategy for skills training and assessment strategies for staff EM physicians within the realm of continuing professional development (CPD) and CME.
Although there have been some recent studies that have looked at the frequency of performing procedural skills in postgraduate EM learners 11 and pediatric EM physicians, 12 these are not completely generalizable to a cohort of general emergency physicians with a wide variety of experience levels. A study performed in the Gippsland region of Victoria, Australia, reported on procedural skills comfort and frequency among a variety of their health care workers. 13 However, that study was not solely examining EM physicians and the results from their rural region may not be applicable to a larger health zone with both urban and rural departments. This highlights the impetus for a more updated assessment of the current procedural skills training needs amongst staff EM physicians in a variety of practice settings to better inform CME initiatives moving forward.
A well‐known model for curriculum development is described by Kern. 14 As we have analyzed the current literature on procedural skills training and curriculums, our general needs assessment has identified a gap for staff physicians. A targeted needs assessment would be an important step prior to implementing an educational initiative, such as a CPD/CME procedural skills curriculum, into an entire geographic health zone. 15 , 16 , 17 , 18 A geographic health zone is a governance model used by the province of Alberta, Canada, to administer and deliver public health care to residents within geographic boundaries. The Edmonton Zone is a group of 12 EDs (four rural community, five urban community, and three tertiary care) staffed by 274 emergency physicians located in one such geographic health zone in Edmonton, Canada. This geographic health zone serves a population of about 1.2 million.
We conducted a multicenter cross‐sectional targeted needs assessment survey of EM physicians within the Edmonton Zone to determine procedural skill performance frequency, confidence with performance, perceived importance of procedures, and educational needs. To ensure that all physician constituents in different practice settings were addressed, we specifically targeted tailored surveys to different types of EDs in the Edmonton Zone including rural community, urban community, and tertiary care hospital sites.
METHODS
From April 2019 to June 2019, we surveyed EM physicians in the Edmonton Zone in Alberta about their current procedural skills practices and their attitudes toward a procedural skills curriculum. This descriptive cross‐sectional survey followed the recommended methodologic guidelines for the design and conduct of self‐administered clinician surveys as outlined by Burns et al. 19 We developed the survey through numerous phases of panel reviews and pilot testing, along with review of relevant literature. This study was approved by the research ethics board at the University of Alberta.
Research Setting
Participants included all EM physicians practicing within the 12 EDs in the Edmonton Zone under Alberta Health Services. One of the tertiary hospitals was a pediatric ED and one was an adult‐only ED. All other departments were mixed patient populations.
Survey Instrument
The survey consisted of three sections: demographics, current procedural practice patterns, and future curriculum planning. Demographic data included age, sex, postgraduate training, years of experience as an attending physician, country of training, and number of shifts worked per month. Current procedural practice captured the frequency, perceived importance, and confidence for each skill. To facilitate future curriculum planning, we asked questions about current methods to maintain competence for procedural skills, barriers and facilitators to participation, and desired frequency of structured practice for each procedural skill. There was a mix of 5‐point Likert scale, ranking, multiple choice, and free text questions.
A list of 45 procedures used in a previous questionnaire reviewing procedural competencies in Canadian EM residents served as the initial foundation for our procedural skill list. 11 Two EM clinical directors for the Edmonton Zone reviewed the list of 45 procedural skills. In combination with input from the coinvestigators and the two clinical directors, a reduced list of 23 to 24 procedural skills was compiled for each group of tertiary, urban, and rural emergency centers based on knowledge of local resources, hospital services, and previous local administrative data. The final procedural skills list utilized in the surveys varied slightly between the tertiary, urban, and rural community sites based on input from the clinical directors and coinvestigators. All other survey items were identical.
The survey underwent several phases of review and modification, including item generation and reduction, pretesting, pilot testing, and clinical sensibility testing using the methodology described in Burns et al. 19 An expert panel composed of five EM physicians reviewed the survey question items to provide feedback on item generation and item reduction. These physicians were not coinvestigators and were selected because they had expertise in medical education and/or survey methodology. We subsequently piloted the survey in its Web‐based mode to six different EM physicians within our target population. Clinical sensibility testing occurred simultaneously with the pilot testing, using a template provided by Burns et al. 19 Through this one‐page questionnaire respondents addressed how well the survey met the intended objective; provided comments on flow, salience, acceptability, and administrative ease; and identified any poorly worded or redundant questions. Through this iterative process, we produced the final survey for distribution. A complete copy of the survey instrument for tertiary sites is available in the Data Supplement S1, Appendix S1 (available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10495/full).
Survey Administration
We collected and managed study data using REDCap hosted at the University of Alberta. 20 , 21 REDCap (Research Electronic Data Capture) is a secure, Web‐based application that provided the interface for data collection and entry as well as export for statistical analysis. The system autogenerated a unique, numerical record for each participant to allow anonymity of all survey responses; thus confidentiality was ensured and protected through REDCap. Consent to participate was implied in completion of the survey.
Survey distribution followed modified Dillman methodology with both Web‐based and paper‐based surveys. 22 , 23 , 24 Each physician was sent an individual e‐mail with a letter of introduction and prenotification on day 0, followed by the e‐mailed survey on day 7. On day 21, nonrespondents were sent follow‐up e‐mail reminders. Following electronic distribution, paper copies of the survey were delivered to mailboxes of the remaining nonrespondents on day 35. The paper survey had no identifying information such that responses could not be tracked. Sealed collection boxes at each ED site were picked up at approximately 4 weeks following delivery. To further ensure anonymity of the nonrespondents, only our research associate (AG) examined and collated the results from the final round of paper surveys as she did not know or work with any of the remaining respondents. Paper copies were not delivered to the pediatric tertiary ED staff.
Data Analysis
Survey responses were collected through the REDCap interface, which produced a spreadsheet that was exported for analysis in Microsoft Excel. We summarized survey responses using descriptive statistics, where categorical data are reported with frequency and proportions, and participant age is reported using mean and standard deviation. To assess for response bias, we compared demographics of early respondents to those of late respondents as previous findings suggest that characteristics of late respondents tend to approximate those of nonrespondents. 25 We examined associations between survey constructs using Spearman rho. All statistical analyses were completed using SAS version 9.4.
RESULTS
Response and Demographic Characteristics
The survey was distributed to 274 physicians at 12 EDs within the Edmonton Zone. Of the physicians invited to participate, 147 (53.6%) completed the survey. For the different site categories the response rates were 73 (62.9%), 32 (43.8%), and 42 (49.4%) for tertiary, urban community, and rural community hospitals, respectively.
Table 1 summarizes the demographic data of the respondents. The average age of respondents was 42.4 years, with 31.3% female. The majority of physicians were trained in Canada (91.8%), with 41.5% of respondents identifying as College of Family Physicians of Canada (CFPC‐EM) trained and 30.6% as Fellow of the Royal College of Physicians of Canada (FRCPC‐EM) trained.
Table 1.
Demographic Characteristics of Edmonton Zone Emergency Physician Procedural Skill Survey Respondents in 2019
| All Sites | Tertiary (n = 73) | Urban (n = 32) | Rural (n = 42) | |
|---|---|---|---|---|
| Age (years) | ||||
| Mean (±SD) | 42.4 (±9.1) | 42.8 (±8.0) | 41.7 (±10.2) | 42.2 (±10.2) |
| Sex | ||||
| Female | 46 (31.3) | 29 (39.7) | 10 (31.3) | 7 (16.7) |
| Male | 99 (67.3) | 43 (58.9) | 21 (65.6) | 35 (83.3) |
| Prefer not to answer | 1 (0.01) | 1 (1.4) | 0 (0) | 0 (0) |
| No response | 1 (0.01) | 0 (0) | 1 (3.1) | 0 (0) |
| Postgraduate qualification | ||||
| CFPC | 16 (10.9) | 0 (0) | 1 (3.1) | 15 (35.7) |
| CFPC‐EM | 61 (41.5) | 19 (26.0) | 26 (81.3) | 16 (38.1) |
| FRCPC‐EM | 45 (30.6) | 40 (54.8) | 1 (3.1) | 4 (9.5) |
| Other | 24 (16.3) | 14 (19.2) | 3 (9.4) | 7 (16.7) |
| No response | 1 (0.01) | 0 (0) | 1 (3.1) | 0 (0) |
| Country of residency training | ||||
| Canada | 135 (91.8) | 71 (97.3) | 31 (96.9) | 33 (78.6) |
| USA | 3 (2.0) | 2 (2.7) | 1 (3.1) | 0 (0) |
| Other | 9 (6.1) | 0 (0) | 0 (0) | 9 (21.4) |
| Years of practice | ||||
| ≤5 | 42 (28.6) | 16 (21.9) | 12 (37.5) | 14 (33.3) |
| 6–10 | 26 (17.7) | 15 (20.6) | 5 (15.6) | 6 (14.3) |
| 11–20 | 52 (35.3) | 30 (41.1) | 8 (25.0) | 14 (33.3) |
| >20 | 27 (18.4) | 12 (16.4) | 7 (21.9) | 8 (19.1) |
| Number of shifts per month | ||||
| ≤5 | 8 (5.4) | 3 (4.1) | 1 (3.1) | 4 (9.5) |
| 6–10 | 54 (36.7) | 30 (41.1) | 6 (18.8) | 18 (42.9) |
| 11–15 | 79 (53.7) | 39 (53.4) | 21 (65.6) | 19 (45.2) |
| >15 | 6 (4.1) | 1 (1.4) | 4 (12.5) | 1 (2.4) |
Data are reported as n (%), unless otherwise reported.
Current Procedural Skills Practices
Table 2 lists the 12 procedures that were shared in common on the procedure list for all Edmonton Zone hospital sites, displaying proportions of all physicians who had not performed the procedure in more than 12 months or who had never performed the procedure on a live patient. Across all types of practice sites, there were certain skills that were infrequently performed (defined as 40% or more of physicians who had not performed the procedure in over 1 year or had never performed the procedure). These procedures included posterior nasal pack for epistaxis, vaginal delivery, intraosseous line insertion, pediatric endotracheal intubation, cricothyroidotomy, and extensor tendon repair. For two of these procedures (pediatric endotracheal intubation and cricothyroidotomy), more than 70% of physicians had either not performed the procedure in over a year or had never performed the procedure.
Table 2.
Time Since a Given Procedural Skill Was Last Performed by Emergency Physicians in the Edmonton Zone in 2019
| Procedure | Tertiary | Urban | Rural | |||
|---|---|---|---|---|---|---|
| >12 Months | Never Performed Live | >12 Months | Never Performed Live | >12 Months | Never Performed Live | |
| Adult endotracheal intubation | 12 (16.4) | 1 (1.4) | 3 (9.4) | 0 (0) | 7 (16.7) | 1 (2.4) |
| Arthrocentesis | 11 (15.1) | 1 (1.4) | 1 (3.1) | 0 (0) | 0 (0) | 0 (0) |
| Central line insertion (ultrasound guided) | 11 (15.1) | 6 (8.2) | 9 (28.1) | 1 (3.1) | 14 (33.3) | 3 (7.1) |
| Chest tube insertion | 25 (34.3) | 1 (1.4) | 7 (21.9) | 0 (0) | 10 (23.8) | 0 (0) |
| Corneal foreign‐body removal | 11 (15.1) | 2 (2.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Cricothyroidotomy | 20 (27.4) | 50 (68.5) | 6 (18.8) | 24 (75.0) | 9 (21.4) | 30 (71.4) |
| Extensor tendon repair | 46 (63.0) | 14 (19.1) | 8 (25.0) | 5 (15.6) | 9 (21.4) | 16 (38.1) |
| Intraosseous line insertion | 23 (31.5) | 6 (8.2) | 9 (28.1) | 5 (15.6) | 9 (21.4) | 8 (19.0) |
| Pediatric endotracheal intubation | 47 (64.4) | 6 (8.2) | 21 (65.6) | 3 (9.4) | 18 (42.9) | 11 (26.2) |
| Posterior nasal pack for epistaxis | 34 (46.6) | 23 (31.5) | 7 (21.9) | 9 (28.2) | 7 (16.7) | 10 (23.8) |
| Regional nerve block | 23 (31.5) | 6 (8.2) | 3 (9.4) | 4 (12.5) | 8 (19.0) | 1 (2.4) |
| Vaginal delivery | 63 (86.3) | 2 (2.7) | 21 (65.6) | 2 (6.3) | 26 (61.9) | 0 (0) |
Data are reported as n (%).
Examining procedures that were listed only on the surveys for tertiary care sites and/or urban community sites, 37.0 and 45.2% of EM physicians had never performed pericardiocentesis or thoracotomy, respectively, on live patients. A lateral canthotomy had never been performed on a live patient by 87.5 and 64.4% physicians at urban and tertiary sites, respectively.
Table 2 also demonstrated variability among the types of hospital sites for frequency in which procedures are performed. Some procedures such as corneal foreign body removal, regional nerve blocks, and chest tube insertion were more likely to have been performed in the past year by physicians working in urban and rural community sites. Conversely, procedures such as a central line insertion with ultrasound guidance were more likely to have been performed in the past year by physicians working at tertiary sites.
Perceptions on Procedural Skill Performance
We compared the perceived importance and confidence performing given procedural skills among EM physicians at the various sites (Figure 1). Only one skill, central line insertion, had a statistically significant difference in the perceived importance of the procedure between the site types, with tertiary and urban sites rating it higher in importance than rural sites.
Figure 1.
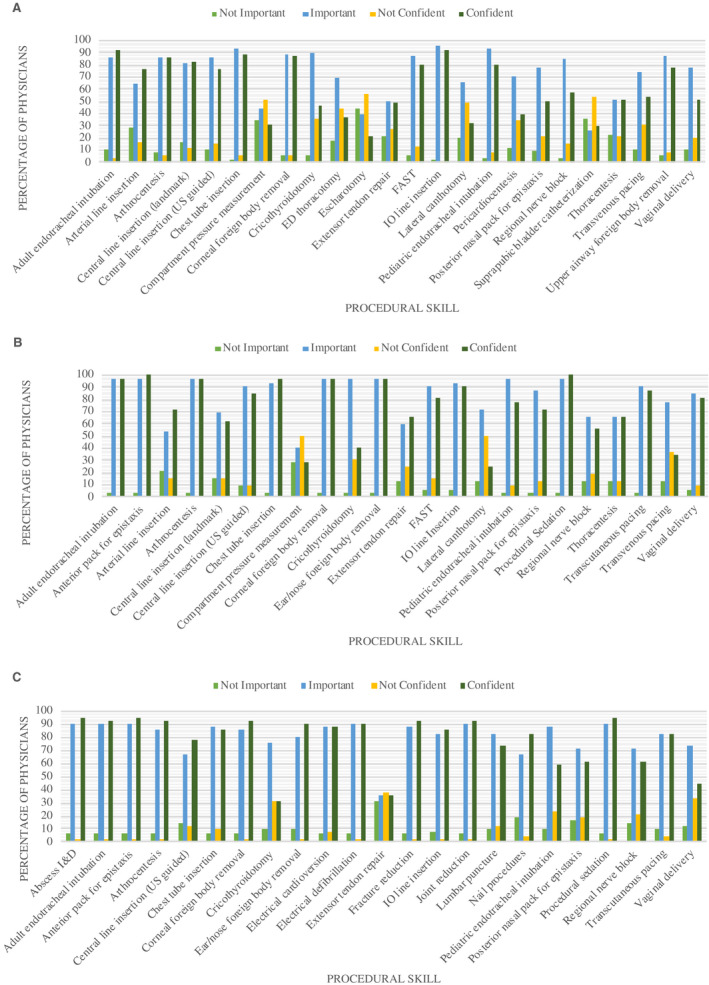
Perceived importance and confidence performing procedural skills in clinical practice for emergency physician respondents at (A) tertiary hospitals; (B) urban community hospitals; and (C) rural community hospitals. FAST = Focused Assessment with Sonography for Trauma; I&D = incision and drainage; IO = intraosseous; US = ultrasound.
We assessed the correlation between EM physician responses on procedural skills performance frequency, perceived importance, perceived confidence, and desired frequency of training. These correlations can be found in Tables 1, 2, 3 in the Data Supplement S1, Appendix S2. For the majority of skills, there was a significantly positive correlation between the frequency at which a skill was performed and the perceived confidence performing said skill. There were no significant correlations between desired frequency of training for a given skill and the perceived importance, frequency, or perceived confidence performing that skill.
Table 3.
Top 6 Procedures Selected for a Procedural Skills Curriculum by Edmonton Zone Emergency Physicians in 2019
| Procedural Skill | All Sites | Tertiary | Urban | Rural |
|---|---|---|---|---|
| ED thoracotomy | 46 (31.3) | 46 (59.0) | ||
| Pericardiocentesis | 35 (23.8) | 35 (44.9) | ||
| Pediatric endotracheal intubation | 75 (51.0) | 42 (53.8) | 33 (75.0) | |
| Transvenous pacing | 53 (36.1) | 34 (43.6) | 19 (59.4) | |
| Chest tube insertion | 65 (44.2) | 26 (33.3) | 11 (34.4) | 28 (63.6) |
| Cricothyroidotomy | 112 (76.2) | 54 (69.2) | 27 (84.4) | 31 (70.5) |
| Adult endotracheal intubation | 37 (25.2) | 11 (34.4) | 26 (65.9) | |
| Central line insertion (ultrasound guided) | 38 (25.9) | 12 (37.5) | 26 (59.1) | |
| Lateral canthotomy | 19 (12.9) | 19 (59.4) | ||
| Extensor tendon repair | 13 (8.8) | 13 (40.6) | ||
| Vaginal delivery | 15 (10.2) | 15 (34.1) |
Data are reported as n (%).
Attitudes Toward a Procedural Skills Curriculum
Table 3 summarizes the top six procedures respondents self‐selected for a hypothetical procedural skills curriculum. The two procedures consistently selected by all three types of sites were chest tube insertion and cricothyroidotomy. Other top procedures selected by at least two of the site types were adult and pediatric endotracheal intubation, central line insertion with ultrasound guidance, and transvenous pacing.
Table 4 summarizes the attitudes and perceptions of EM physicians regarding a procedural skills curriculum. The current methods that Edmonton EM physicians use to maintain procedural competency were repeated clinical practice (97.3%; T, 91.0%; U, 96.9%; R, 75.9%), observation via clinical, peer consult, reading, video review (83.7%; T, 76.9%; U, 84.4%; R, 66.7%), and formal courses (73.5%; T, 62.8%; U, 84.4%; R, 59.3%). If a procedural skills course was offered, most respondents preferred either a full‐day (48.3%) or half‐day course (43.5%) rather than a 2‐day course (7.5%).
Table 4.
Edmonton Zone Emergency Physician Preferences for Procedural Skills Curriculum Development in 2019
| All Sites | Tertiary | Urban | Rural | |
|---|---|---|---|---|
| Current methods to maintain competence | ||||
| Repeated clinical practice | 143 (97.3) | 71 (91.0) | 31 (96.9) | 41 (75.9) |
| Observation (clinical, peer consult, reading, video review) | 123 (83.7) | 60 (76.9) | 27 (84.4) | 36 (66.7) |
| Simulation | 75 (51.0) | 29 (37.2) | 20 (62.5) | 26 (48.2) |
| Formal course | 108 (73.5) | 49 (62.8) | 27 (84.4) | 32 (59.3) |
| Other | 8 (5.4) | 4 (5.1) | 1 (3.1) | 3 (5.6) |
| None of the above | 1 (0.01) | 1 (1.3) | 0 (0) | 0 (0) |
| Preferred length of procedural skills course | ||||
| Half a day | 64 (43.5) | 37 (50.7) | 11 (34.4) | 16 (38.1) |
| Full day | 71 (48.3) | 30 (41.1) | 19 (59.4) | 22 (52.4) |
| Two days | 11 (7.5) | 5 (6.8) | 2 (6.3) | 4 (9.5) |
| No response | 1 (0.01) | 1 (1.4) | 0 (0) | 0 (0) |
| Barriers to participation in procedural skills curriculum | ||||
| Cost | 31 (21.1) | 14 (18.0) | 4 (12.5) | 13 (24.1) |
| Availability of courses | 112 (76.2) | 61 (78.2) | 23 (71.9) | 28 (51.9) |
| Time | 107 (72.8) | 51 (65.4) | 21 (65.6) | 35 (64.8) |
| Lack of department/site support | 28 (19.0) | 16 (20.5) | 4 (12.5) | 8 (14.8) |
| Other | 5 (3.4) | 2 (2.6) | 1 (3.1) | 2 (3.7) |
| Facilitators to participation in procedural skills curriculum | ||||
| CME credit | 120 (81.6) | 61 (78.2) | 26 (76.5) | 33 (61.1) |
| Financial support | 56 (38.1) | 27 (34.6) | 14 (41.2) | 15 (27.8) |
| On site location of course | 112 (76.2) | 61 (78.2) | 22 (64.7) | 29 (53.7) |
| Academic promotion | 24 (16.3) | 12 (15.4) | 5 (14.7) | 7 (13.0) |
| Other | 9 (6.1) | 3 (3.9) | 1 (2.9) | 5 (9.3) |
Data are reported as n (%).
When asked if they had attended a procedural skills course in the past 2 years, 57.5% respondents reported that they had not. The main barriers to participating in a procedural skills curriculum identified by respondents were availability of courses (76.2%) and time (72.8%). Conversely, the major facilitating factors for curriculum participation included CME credit (81.6%) and on‐site location of courses (76.2%).
DISCUSSION
We completed a targeted needs assessment as described by Kern's curriculum development approach for a comprehensive procedural skills curriculum for staff emergency physicians within an entire geographic health zone. As the goal is to design a curriculum applicable to rural, urban and tertiary care providers, we incorporated perspectives from all practice settings within our health region.
A need for a defined procedural skills curriculum is particularly pressing considering the finding that greater than 50% of all physicians in our geographic health zone who completed our survey had not participated in a procedural skills course in the past 2 years. The survey respondents' opinions on the barriers and facilitators support the need for a local curriculum and that efforts need to be directed to making these courses in region for physicians, at convenient and variable times, and with CME credit. 26 , 27 , 28 These findings also justify the need for a geographic health zone to develop a specific strategy for producing and delivering a strategic procedural skills curricula that all its' members, in rural, urban community, and tertiary settings can access.
There were definite differences in the frequency and comfort level between rural, urban, and tertiary ED settings for certain ED procedures. However, there were also several procedures that all emergency physicians across all practice sites had not performed frequently, if at all. The similarities and the differences discovered in procedure performance between practice sites have implications for the content development and implementation of a procedural skills course within a geographic health zone. While there are certainly tailored curricula that need to be implemented in individual EDs and practice settings, there is also a need for curricula that can address common needs shared between physicians from all types of ED settings. As delivery of procedural skills curricula can be very resource intensive, having one common curriculum with shared resources for physicians within an entire geographic health zone will result in a more concentrated and time‐efficient program that will meet the needs of the largest group of physicians. This is particularly important as a recent symposium paper from the Canadian Association of Emergency Physicians on relationships between academic and rural EDs noted that rural/regional physicians identified shared CME as a high‐value item. 29
For most procedures in this study, we found no statistically significant differences in practices and attitudes toward perceived importance of procedural skills between the tertiary, urban, and rural sites. Only central line insertion (both landmark and ultrasound guided methods) was significantly different in perceived importance between the three practice sites. The reason for this finding is unclear, although the safety of using peripheral intravenous lines for vasopressor delivery and the usage of intraosseous lines for vascular access may be contributing to rural emergency physicians' lower perceived importance for central line training.
Similar to prior studies, we found the most consistent association was a significantly positive correlation between the frequency at which a skill was performed and the perceived confidence performing the respective skill. 5 In addition, for most skills we included, there was a positive relationship between years of practice in medicine and confidence performing a given skill. Interestingly though, there was a small group of select skills that showed an inverse relationship between years of practice and confidence in performance (e.g., ultrasound guided central lines, regional nerve block, FAST, arterial line insertions). While reasons for this were not captured in the survey, we hypothesize that this may be attributed to the growing role of ultrasound integration within the ED and residency program curricula, to complement physical examination, diagnosis, and procedural skills. 30 The introduction of point‐of‐care ultrasound in the ED is still relatively recent and it is possible that physicians who trained before the widespread use of ultrasound have had less exposure and practice with this modality. Point‐of‐care ultrasound has been an area supported by CPD and likely warrants ongoing focused training during this time. 31 This finding supports the importance of CME to support physicians as they keep up to date with changes in practice. 32
While it has been suggested that skills can be retained with relatively infrequent practice, the accepted recommendations on procedural skill training frequency for practice and the mode of practice remain unanswered. 12 , 33 Our results corroborate this; our survey respondents did not agree on an ideal frequency of practice for the procedural skills. The timeline for repetition and practice for procedural skills sessions in a geographic health zone is likely to rest more on logistic factors such as ensuring that shared modules are delivered to as many physicians as possible up front with practice sessions scheduled in parallel to allow individual practitioners flexibility for repetition as their schedules permit.
Procedural competency in clinical practice for staff physicians is the responsibility of a health region, department, hospital, and the individual physician. 34 This is particularly challenging given the many different types of settings current emergency physicians practice in (tertiary, urban community, rural community). When designing CPD, it is of paramount importance that health regions factor in the similarities and differences in procedural skills needs for emergency practitioners in different types of practice settings. By performing this needs assessment in our geographic health zone, it will ensure that our subsequent procedural skills CME sessions will be relevant to all learner's needs, resource‐efficient, and target the broadest range of practitioners to effect positive change in professional practice. 17 , 35 , 36 Moving forward, our next steps will be to use this targeted needs assessment to develop goals and objectives, educational strategies, implementation, and evaluation for both 1) a common procedural skills curriculum relevant to all members of our geographic health zone and 2) subcourses of curricula tailored to meet the individualized needs of the different sites.
LIMITATIONS
This study is not without limitations. First, we used an abbreviated list of the nearly 130 procedures outlined for competence by the Royal College of Physicians and Surgeons. We based this on prior literature, along with our zone clinical directors and coinvestigators, to establish a relevant list of both critical care and low‐acuity skills and to avoid an excessively long list that would affect survey response. Second, it is not uncommon for Edmonton emergency physicians to work at multiple sites, which may include both tertiary and community sites. The survey type (tertiary, urban, or rural) was sent based on current administrative data for the main site that the physician worked at. Given the variability in sites in which a physician may practice, this introduces a possible bias to their survey responses. However, this reflects the common practice pattern of many physicians who likely work at multiple types of sites during their careers. Third, the Edmonton Zone includes one pediatric ED. This group was included in the survey distribution as a twelfth site, within the tertiary group. However, this group did not receive the paper survey phase, and as a result this may have lowered our response rate. We did not isolate pediatric and general EM physician responses as we wanted to capture a population generalizable to other health authorities. Finally, our survey cannot account for differences between responders and nonresponders in procedural experience and attitudes toward curriculum development; however, we did attempt to assess for nonresponse bias. We compared demographic characteristics of early respondents to late respondents (survey completion after 35 days), because research has suggested that late respondents approximate those of nonrespondents; we found no significant difference between these groups. 25
CONCLUSIONS
A needs assessment demonstrated that a locally developed and implemented procedural skills curriculum is important for the emergency physicians working in our geographic health zone. We identified procedural skills needs that could inform a common continuing medical education curriculum relevant to all practitioners working in rural community, urban community, and tertiary care EDs as well as procedural skills needs that could inform continuing medical education curriculum more specific to individual practice sites. These findings will inform a broad procedural skills curriculum implementation initiative to all the emergency physicians within our geographic health zone. This study can provide a template for other health authorities to help determine the current needs of their own EM physicians at all types of practice sites and to inform subsequent procedural skills curricula for their members.
The authors thank the Edmonton Zone EM Clinical Directors and the EM physicians who participated in our expert panel and pilot testing for survey development.
Supporting information
Data Supplement S1. Supplemental material.
AEM Education and Training 2021;5:1–11
Methodology was presented preliminarily at the Annual Department of Emergency Medicine Research Day, Edmonton, Alberta, Canada. June 11, 2019. No results from the manuscript were included. Recipient of the top resident research award.
The authors have no relevant financial information or potential conflicts of interest to disclose.
Author contributions: RS, BS, AG, and DH conceptualized the study design and participated in data analysis and interpretation; RS and AG acquired the data; AG provided statistical expertise and administrative support; RS drafted the manuscript; and BS, AG, and DH critically reviewed the manuscript for important intellectual content.
Supervising Editor: Teresa Chan, MD, MHPE.
References
- 1. Farion K, Morrison LJ. Redefining emergency medicine procedures: Canadian competence and frequency survey. Acad Emerg Med 2001;8:731–8. [DOI] [PubMed] [Google Scholar]
- 2. Royal College of Physicians and Surgeons of Canada . Objectives of Training in the Specialty of Emergency Medicine. Ottawa: The Royal College of Physicians and Surgeons of Canada, 2014. [Google Scholar]
- 3. Nettleman MD, Bock MJ, Nelson AP, Fieselmann J. Impact of procedure‐related complications on patient outcome on a general medicine service. J Gen Intern Med 1994;9:66–70. [DOI] [PubMed] [Google Scholar]
- 4. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients: results of the Harvard medical practice study II. N Engl J Med 1991;324:377–84. [DOI] [PubMed] [Google Scholar]
- 5. Mourad M, Kohlwes J, Maselli J, Auerbach AD. Supervising the supervisors—procedural training and supervision in internal medicine residency. J Gen Intern Med 2010;25:351–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Epstein R. Assessment in medical education. N Engl J Med 2007;356:387–96. [DOI] [PubMed] [Google Scholar]
- 7. Kane MT. The validity of assessments of professional competence. Eval Health Prof 1992;15:163–82. [DOI] [PubMed] [Google Scholar]
- 8. Frank JR, Snell LS, Ten Cate O, et al. Competency‐based medical education: theory to practice. Med Teach 2010;32:638–45. [DOI] [PubMed] [Google Scholar]
- 9. Bancroft GN, Basu CB, Leong M, Mateo C, Hollier LH Jr, Stal S. Outcome‐based residency education: teaching and evaluating the core competencies in plastic surgery. Plast Reconstruct Surg 2008;121:441e–8. [DOI] [PubMed] [Google Scholar]
- 10. Sherbino J, Bandiera G, Frank JR. Assessing competence in emergency medicine trainees: an overview of effective methodologies. CJEM 2008;10:365–71. [DOI] [PubMed] [Google Scholar]
- 11. Petrosoniak A, Herold J, Woolfrey K. Emergency medicine procedural skills: what are residents missing? CJEM 2013;15:241–8. [DOI] [PubMed] [Google Scholar]
- 12. Craig SS, Auerbach M, Cheek JA, et al. Preferred learning modalities and practice for critical skills: a global survey of paediatric emergency medicine clinicians. Emerg Med J 2019;36:273–80. [DOI] [PubMed] [Google Scholar]
- 13. Campbell D, Shepherd I, McGrail M, et al. Procedural skills practice and training needs of doctors, nurses, midwives and paramedics in rural Victoria. Adv Med Educ Pract 2015;6:183–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kern DE. A six‐step approach to curriculum development. In: Thomas P, Kern D, Hughes M, Chen B, editors. Curriculum Development for Medical Education: A Six‐step Approach. Baltimore: Johns Hopkins University Press, 2016. pp. 5‐9. [Google Scholar]
- 15. Druck J, Valley MA, Lowenstein SR. Procedural skills training during emergency medicine residency: are we teaching the right things? West J Emerg Med 2009;10:152–6. [PMC free article] [PubMed] [Google Scholar]
- 16. Grant J. Learning needs assessment: assessing the need. BMJ 2002;324:156–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mazmanian PE, Davis DA. Continuing medical education and the physician as a learner: guide to the evidence. JAMA 2002;288:1057–60. [DOI] [PubMed] [Google Scholar]
- 18. Ingrassia PL, Barozza LG, Franc JM. Prioritization in medical school simulation curriculum development using survey tools and desirability function: a pilot experiment. Adv Simul (Lond) 2018;3:2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self‐administered surveys of clinicians. CMAJ 2008;179:245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dillman DA. Mail and Telephone Surveys : The Total Design Method. New York: Wiley, 1978. [Google Scholar]
- 23. Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. New York: Wiley, 2000. [Google Scholar]
- 24. Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed Mode Surveys: The Tailored Design Method. 4th ed. Hoboken, NJ: John Wiley & Sons Inc, 2014. [Google Scholar]
- 25. Ullman JB, Newcomb MD. Eager, reluctant, and nonresponders to a mailed longitudinal survey: attitudinal and substance use characteristics differentiate respondents 1. J Appl Soc Psychol 1998;28:357–75. [Google Scholar]
- 26. Cook DA, Blachman MJ, Price DW, West CP, Berger RA, Wittich CM. Professional development perceptions and practices among U.S. physicians: a cross‐specialty national survey. Acad Med 2017;92:1335–45. [DOI] [PubMed] [Google Scholar]
- 27. Stewart GD, Khadra MH. The continuing medical education activities and attitudes of Australian doctors working in different clinical specialties and practice locations. Aust Health Rev 2009;33:47–56. [DOI] [PubMed] [Google Scholar]
- 28. Goodyear‐Smith F, Whitehorn M, McCormick R. Experiences and preferences of general practitioners regarding continuing medical education: a qualitative study. New Zeal Med J 2003;116:U399‐U. [PubMed] [Google Scholar]
- 29. Johnston A, Booth K, Christenson J, et al. Building and strengthening relationships between academic departments/divisions of emergency medicine and rural and regional emergency departments. CJEM 2019;21:595–9. [DOI] [PubMed] [Google Scholar]
- 30. Olszynski P, Kim DJ, Chenkin J, Rang L; CAEP Emergency Ultrasound Committee curriculum working group . The CAEP emergency ultrasound curriculum – objectives and recommendations for implementation in postgraduate training: executive summary. CJEM 2018;20:736–8. [DOI] [PubMed] [Google Scholar]
- 31. Lewis D, Rang L, Kim D, et al. Recommendations for the use of point‐of‐care ultrasound (POCUS) by emergency physicians in Canada. CJEM 2019;21:721–6. [DOI] [PubMed] [Google Scholar]
- 32. Laine C, Weinberg DS. How can physicians keep up‐to‐date? Annu Rev Med 1999;50:99–110. [DOI] [PubMed] [Google Scholar]
- 33. Allen JA, Currey J, Considine J. Annual resuscitation competency assessments: a review of the evidence. Aust Crit Care 2013;26:12–7. [DOI] [PubMed] [Google Scholar]
- 34. Tran V, Cobbett J, Brichko L. Procedural competency in emergency medicine training. Emerg Med Australas 2018;30:103–6. [DOI] [PubMed] [Google Scholar]
- 35. Candy PC. Self‐Direction for Lifelong Learning. A Comprehensive Guide to Theory and Practice. San Francisco: Jossey‐Bass, 1991. [Google Scholar]
- 36. Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor‐Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999;282:867–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Supplemental material.


