Editor—Although there is extensive discussion of COVID anaesthesia management and infection control in the operating theatre, there are few articles examining whether perioperative anaesthesia-related drugs could affect COVID-19. Here, we discuss this possibility.
SARS-CoV-2 binding sites (Fig. 1)
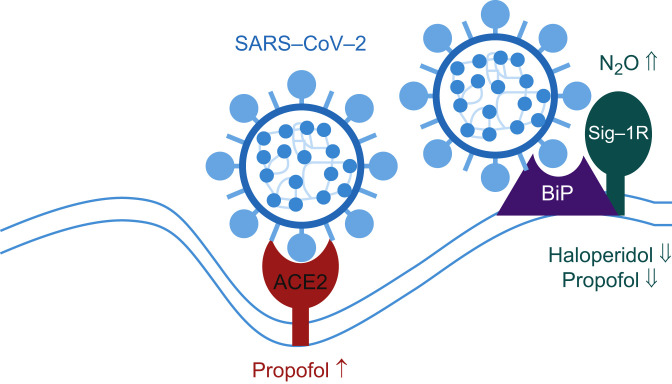
Fig 1.
Cellular SARS-CoV-2 binding sites. ACE2, angiotensin converting enzyme 2; BiP, heavy chain binding immunoglobulin protein, also known as glucose regulating protein 78 (GRP78) or heat shock 70 kDa protein 5 (HSPA5) in the endoplasmic reticulum (ER); Sig-1R, sigma-1 receptor; ↑, upregulation; ⇑, activation; ⇓, inhibition.
Angiotensin converting enzyme 2
Angiotensin converting enzyme 2 (ACE2) is the best-known target cell receptor for SARS-CoV-2 internalisation. It is widely distributed in human cells and tissues and highly expressed in the small intestine, testes, kidneys, heart, thyroid, lungs, salivary glands, and adipose tissues, but not in the vocal folds, epiglottis, and trachea.1
Sigma-1 receptor
SARS-CoV-2 interacts with sigma receptors via non-structural protein 6 and coronavirus open reading frame (Orf) 9c proteins to infect cells.2 Knockout and knockdown of sigma-1 receptor (Sig-1R), but not of Sig-2R, decreased SARS-CoV-2 replication. Modulation of Sig-1R may thus affect the early steps of viral endocytosis to change SARS-CoV-2 infection for immunologic enhancement.3
Famotidine and proton pump inhibitors
Famotidine is used for prophylaxis for stress ulcers in the ICU and for aspiration pneumonia as an anaesthetic premedication. A recent report4 suggests that famotidine may improve outcome in COVID-19 patients. Histamine H2 antagonists may activate the innate immune system to increase the count and bactericidal actions of neutrophils, enhance phagocytosis, and decrease adhesion and peroxide production. H2 antagonists also increase natural killer cell count and cytotoxicity, enhance production of interleukin (IL)-2, IL-13, and tumour necrosis factor-α, expression of major histocompatibility complex-2 (MHC-2) and caspase-1 in macrophages/monocytes, and increase MHC-1, CD40, CD80, CD89, and IL-12 in dendritic cells.5 Although these mechanism(s) have the potential to produce antiviral actions, this will require rigorous experimental evaluation. In contrast, and as shown in a meta-analysis, proton pump inhibitors (PPIs) may aggravate COVID-19 as there was an association between current PPI use and incidence of SARS-CoV-2 infection and severity of COVID-19 when a Korean study was excluded.6
Intravenous anaesthetic agents and sedatives
Propofol
ACE2 may be upregulated when tissues are exposed to sedative concentrations (≥10 μg ml−1) for >6 h.7 Propofol might inhibit SARS-CoV-2 entry as suggested for hydroxychloroquine.8 In addition, clinically relevant concentrations of propofol may have Sig-1R antagonistic properties.7 Moreover, propofol has both antioxidant and antiinflammatory actions and may reduce systemic inflammation and exert organ protection in COVID-19.7
Ketamine
Ketamine may interact with both Sig-1R and Sig-2R as an agonist. However, its affinities for Sig-1R (Ki=140 μM) and Sig-2R (Ki=26 μM) were in the supraclinical and clinical ranges, respectively.9 As Sig-1R is the more important target in SARS-CoV-2 infection,2 it is unlikely that ketamine exerts potent proviral actions. However, as ketamine has antiinflammatory actions, this agent may reduce the risk of SARS-CoV-2-induced cytokine storm.10
Haloperidol and droperidol
Clinically relevant concentrations of haloperidol, a butyrophenone, interacts with both Sig-1R and Sig-2R (Ki=0.33 nM and 26 nM, respectively)11 as an antagonist to produce SARS-CoV-2 antiviral actions.2 Droperidol, another butyrophenone, interacts with Sig-1R as an antagonist but with a Ki of 0.17 μM, which exceeds clinically relevant concentrations.12
Dexmedetomidine
Dexmedetomidine displaced (+)[3H]SKF-10047, a selective Sig-1R agonist, binding with a Ki of 5.7 μM12 which exceeds clinically relevant concentrations.13 Dexmedetomidine is therefore unlikely to affect SARS-CoV-2 infection via Sig-1R. However, the antiinflammatory and organ protective effects of dexmedetomidine14 may provide therapeutic advantages for COVID-19 patients with multi-organ dysfunction in the ICU. The mechanism may hypothetically be attributable to inhibition of neutrophil extracellular traps formation (NETosis) to prevent immune activation in COVID-19.14 Indeed, Stockton and Kyle-Sidell15 reported a case of dexmedetomidine improving oxygenation and avoidance of tracheal intubation in a patient with progressive hypoxaemia.
Inhalation anaesthetic agents
Nitrous oxide, a Sig-R agonist,16 might aggravate SARS-CoV-2 infection via Sig-R interaction. Regarding volatile anaesthetic agents, there are no reports detailing an interaction with ACE2 or Sig-R. A COVID-19 case series showed that isoflurane provided sufficient sedation and significant improvement in oxygenation without any adverse events.17
Local anaesthetic agents
COVID-19 patients often show high serum concentrations of citrullinated histone H3 (Cit-H3) which is a biomarker of NETosis. As serum from COVID-19 patients induces neutrophil extracellular traps (NETs) release from control neutrophils, COVID-19 may create a cellular environment for promotion of NETosis. I.V. lidocaine reduces blood neutrophil myeloperoxidase and Cit-H318; this has the potential to attenuate an associated immunological storm.19
Opioids
Although chronic use or misuse of opioids leading to immunosuppression might increase the risk of SARS-CoV-2 infection,20 opioids may attenuate respiratory symptoms in COVID-19 patients, such as shortness of breath and cough.21 Moreover, opioids used in substitution therapy may aid in the maintenance of antioxidant capacity.21 Opioids have the potential to exert both ‘theoretical’ beneficial and detrimental actions; further evaluation is required.
NSAIDs and paracetamol
WHO initially recommended that ibuprofen and other NSAIDs should be avoided in the management of COVID-19 symptoms, as there were anecdotal reports that NSAIDs such as ibuprofen could worsen the effects of SARS-CoV-2 during the early phase of COVID-19.22 WHO later withdrew their recommendation because of a lack of clinical evidence.22 Indeed, Rinott and colleagues23 reported that ibuprofen use was not associated with worse clinical outcomes when compared with paracetamol or no antipyretic use.
Neuromuscular blocking drugs and their antagonists
Although neuromuscular blocking drugs and sugammadex are routinely used in the ICU and operating theatres, we are not aware of any reports showing proviral or antiviral actions of these agents in SARS-CoV-2.
Vasoactive drugs
It has been reported that β2-adrenergic receptor activation produces antiinflammatory actions and suppresses immune function to impair bacterial clearance.24 Vasoactive agents with a β2-adrenergic profile possess a theoretical risk for SARS-CoV-2 proliferation.
In conclusion, several in vitro experiments are suggestive that a number of anaesthetics and sedatives might affect SARS-CoV-2 infection via the ACE2 and Sig-R systems. Anaesthetists are concerned with potential risks of perioperative and ICU drugs; we have briefly covered potential risks in COVID-19 patients. Further studies to evaluate anaesthetic drug effects on (i) the ability of SARS-CoV-2 to infect and (ii) the ability of patients to mount an appropriate immune reaction are needed. Do anaesthetic agents exacerbate or ameliorate the effects of immune activation that have the potential to transition COVID-19 to long COVID?
Declarations of interest
DGL is Chairman of BJA. KH has no conflicts of interest to declare.
References
- 1.Hirota K. Air contamination with SARS-CoV-2 in the operating room. J Anesth Adv. 2020 doi: 10.1007/s00540-020-02814-7. Access Published June 19, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon D.E., Jang G.M., Bouhaddou M. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583:459–468. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vela J.M. Repurposing sigma-1 receptor ligands for COVID-19 therapy? Front Pharmacol. 2020;11:582310. doi: 10.3389/fphar.2020.582310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedberg D.E., Conigliaro J., Wang T.C., Tracey K.J., Callahan M.V., Abrams J.A., Famotidine Research Group Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: a propensity score matched retrospective cohort study. Gastroenterology. 2020;159:1129–1131. doi: 10.1053/j.gastro.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosh R., Chatterjee S., Dubey S., Lavie C.J. Famotidine against SARS-CoV2: a hope or hype? Mayo Clin Proc. 2020;95:1797–1799. doi: 10.1016/j.mayocp.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li G.F., An X.X., Yu Y. Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis. Gut Adv. 2020 doi: 10.1136/gutjnl-2020-323366. Access Published November 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirota K., Lambert D.G. Propofol and SARS-CoV-2 infection. Br J Anaesth. 2020;125:e475–e476. doi: 10.1016/j.bja.2020.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei P., Zheng Q., Ye H., Lyu W., Li J., Yang J. Putative antiviral effects of propofol in COVID-19. Br J Anaesth Adv. 2021 doi: 10.1016/j.bja.2021.02.006. Access Published February 13, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zanos P., Moaddel R., Morris P.J. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70:621–660. doi: 10.1124/pr.117.015198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ortoleva J. Consider adjunctive ketamine in mechanically ventilated COVID-19 patients. J Cardiothorac Vasc Anesth. 2020;34:2580. doi: 10.1053/j.jvca.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaen J.C., Caprathe B.W., Pugsley T.A., Wise L.D., Akunne H. Evaluation of the effects of the enantiomers of reduced haloperidol, azaperol, and related 4-amino-1-arylbutanols on dopamine and sigma receptors. J Med Chem. 1993;36:3929–3936. doi: 10.1021/jm00076a022. [DOI] [PubMed] [Google Scholar]
- 12.Yamada M., Nakao S., Sakamoto S. Propofol acts at the sigma-1 receptor and inhibits pentazocine-induced c-Fos expression in the mouse posterior cingulate and retrosplenial cortices. Acta Anaesthesiol Scand. 2006;50:875–881. doi: 10.1111/j.1399-6576.2006.01033.x. [DOI] [PubMed] [Google Scholar]
- 13.Angst M.S., Ramaswamy B., Davies M.F., Maze M. Comparative analgesic and mental effects of increasing plasma concentrations of dexmedetomidine and alfentanil in humans. Anesthesiology. 2004;101:744–752. doi: 10.1097/00000542-200409000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Jain A., Lamperti M., Doyle D.J. Dexmedetomidine: another arrow in the quiver to fight COVID-19 in intensive care units. Br J Anaesth. 2021;126:e35–e38. doi: 10.1016/j.bja.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stockton J., Kyle-Sidell C. Dexmedetomidine and worsening hypoxemia in the setting of COVID-19: a case report. Am J Emerg Med. 2020;38:2247. doi: 10.1016/j.ajem.2020.05.066. e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gillman M.A. Analgesic (sub anesthetic) nitrous oxide interacts with the endogenous opioid system: a review of the evidence. Life Sci. 1986;39:1209–1221. doi: 10.1016/0024-3205(86)90181-5. [DOI] [PubMed] [Google Scholar]
- 17.Flinspach A.N., Zacharowski K., Ioanna D., Adam E.H. Volatile isoflurane in critically ill coronavirus disease 2019 patients-a case series and systematic review. Crit Care Explor. 2020;2 doi: 10.1097/CCE.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galo E.V., Tat T.F., Popa R. Neutrophil extracellular trapping and angiogenesis biomarkers after intravenous or inhalation anaesthesia with or without intravenous lidocaine for breast cancer surgery: a prospective, randomised trial. Br J Anaesth. 2020;125:712–721. doi: 10.1016/j.bja.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Finnerty D.T., Buggy D.J. A novel role for lidocaine in COVID-19 patients? Br J Anaesth. 2020;125:e391–e394. doi: 10.1016/j.bja.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lambert D.G. Opioids and the COVID-19 pandemic: does chronic opioid use or misuse increase clinical vulnerability? Br J Anaesth. 2020;125:e382–e383. doi: 10.1016/j.bja.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eagleton M., Stokes S., Fenton F., Keenan E. Does opioid substitution treatment have a protective effect on the clinical manifestations of COVID-19? Br J Anaesth. 2021;126:e114–e116. doi: 10.1016/j.bja.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cabbab I.L.N., Manalo R.V.M. Anti-inflammatory drugs and the renin-angiotensin-aldosterone system: current knowledge and potential effects on early SARS-CoV-2 infection. Virus Res. 2021;291:198190. doi: 10.1016/j.virusres.2020.198190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.RinottE, Kozer E., Shapira Y., Bar-Haim A., Youngster I. Ibuprofen use and clinical outcomes in COVID-19 patients. Clin Microbiol Infect. 2020;26:1259. doi: 10.1016/j.cmi.2020.06.003. e5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stolk R.F., Naumann F., van der Pasch E. Phenylephrine impairs host defence mechanisms to infection: a combined laboratory study in mice and translational human study. Br J Anaesth. 2021;126:652–664. doi: 10.1016/j.bja.2020.11.040. [DOI] [PubMed] [Google Scholar]