Abstract
Background:
The association between injury risk and skeletal maturity in youth soccer has received little attention.
Purpose:
To prospectively investigate injury patterns and incidence in relation to skeletal maturity in elite youth academy soccer players and to determine the injury risks associated with the skeletal maturity status, both overall and to the lower limb apophysis.
Study Design:
Descriptive epidemiology study.
Methods:
All injuries that required medical attention and led to time loss were recorded prospectively during 4 consecutive seasons in 283 unique soccer players from U-13 (12 years of age) to U-19 (18 years). The skeletal age (SA) was assessed in 454 player-seasons using the Fels method, and skeletal maturity status (SA minus chronological age) was classified as follows: late, SA >1 year behind chronological age; normal, SA ±1 year of chronological age; early, SA >1 year ahead of chronological age; and mature, SA = 18 years. An adjusted Cox regression model was used to analyze the injury risk.
Results:
A total of 1565 injuries were recorded; 60% were time-loss injuries, resulting in 17,772 days lost. Adjusted injury-free survival analysis showed a significantly greater hazard ratio (HR) for different status of skeletal maturity: early vs normal (HR = 1.26 [95% CI, 1.11-1.42]; P < .001) and early vs mature (HR = 1.35 [95% CI, 1.17-1.56]; P < .001). Players who were skeletally mature at the wrist had a substantially decreased risk of lower extremity apophyseal injuries (by 45%-61%) compared with late (P < .05), normal (P < .05), and early (P < .001) maturers.
Conclusion:
Musculoskeletal injury patterns and injury risks varied depending on the players’ skeletal maturity status. Early maturers had the greatest overall adjusted injury risk. Players who were already skeletally mature at the wrist had the lowest risk of lower extremity apophyseal injuries but were still vulnerable for hip and pelvis apophyseal injuries.
Keywords: football, biological age, injury prevention, growth plate injuries, apophysis
The development of a young athlete is a dynamic process during which biological maturition, physical growth, and behavioral development changes occur simultaneously, alongside the demands of sport.35 This complex interaction makes youth athlete development a unique and challenging environment for sports medicine practitioners and researchers.10,22 Musculoskeletal injuries occur within a dynamic environment and depend on both internal and external factors.13 Among the numerous risk factors, growth and maturition likely have an influence because these factors are inherent to this environment.21,50 Only a limited number of studies, using diverse noninvasive biological maturation assessment methods, have investigated the interaction of growth and maturition with regard to musculoskeletal injuries in youth soccer.4,6,8 Although skeletal maturition is recognized as a reliable method of determining biological maturity,35,53 current knowledge regarding musculoskeletal injury in relation to skeletal maturity status is sparse and inconclusive.50
Research from Europe suggests a link between skeletal maturity status, injury incidence, and injury pattern in elite youth soccer academies. In an English cohort, Johnson et al28 assessed skeletal age (SA) using the Fels method and suggested that skeletal maturity status, together with training and playing hours, could predict injury in youth players. In a study of elite French youth players, Le Gall et al32 used the Greulich-Pyle method to estimate skeletal maturity and found differences in type, location, and severity of injuries between maturity groups. During the growth spurt and before the closure of growth plates through adolescence, young athletes are vulnerable to a variety of traumatic and overuse injuries of the immature skeleton.17,36 However, physeal injuries remain underreported, and their association with biological maturity is often not considered.17,32 More prospective studies considering biological maturity in adolescent soccer players are needed to understand the association with musculoskeletal injury pattern. Identifying potential risk factors could provide valuable preventive and clinical insights for practitioners.34,50 The purpose of this study was to examine the extent and nature of injuries and the association of skeletal maturity with injury risk in a Middle Eastern elite youth soccer academy.
Methods
This study was approved by the scientific boards of ASPETAR and the Aspire Academy and conformed to the recommendations of the Declaration of Helsinki. Ethics approval was granted by the Anti-Doping Lab Qatar Institutional Review Board.
Study Design and Participants
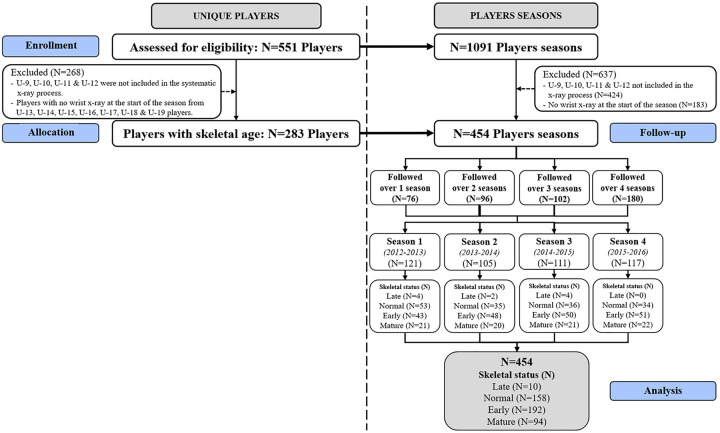
The original cohort consisted of 551 soccer players. Of these, 268 players were excluded because they did not undergo radiography to determine skeletal maturity at the beginning of the season. The prospective study included 283 youth male elite soccer players in 7 different age groups from 12 years (U-13) to <19 years (U-19) and was performed during 4 consecutive seasons (2012–2016), with a total of 454 player-seasons (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart illustrating the 4 seasons, on the left as unique players and on the right as player-seasons depicted by skeletal maturity status and number of seasons of follow-up.
The participants were training and playing at the National Training Center ASPIRE Academy in Doha, Qatar. All age groups trained for around 14 hours a week including combined soccer-specific training and competitive play, with a single rest day per week. This weekly load typically comprised 6 to 8 soccer training sessions, 1 strength training session, 1 or 2 conditioning sessions, and 1 domestic game per week. Additionally, players were engaged with the academy in 2 invited international games every 3 weeks. Participation in the screening was voluntary, and assurances were given that the players’ status in the academy would not be affected if they did not wish to undergo any aspects of the screening process. Signed parental and student consent for the screening and the use of regularly collected injury data for research purposes was obtained for all individual participants included in this original study.
Data Collection
All musculoskeletal injuries sustained were prospectively recorded by the academy medical staff in a standardized format. Each squad had an experienced dedicated physiotherapist (O.M.), and all injuries were examined together with the academy sports physician. Referral to a surgeon specialist or for imaging was requested on a case-by-case basis as necessary. Each team’s physiotherapist submitted injury information for all discharged injured players to the senior physiotherapist (O.M.), who reviewed and consolidated all data. Injuries sustained out of the context of the soccer program (training or game) and any data related to sickness or other general medical conditions were excluded from this study.
Injury Definitions
An injury was recorded as a result of any physical complaint resulting from a game or training that required the attention of the medical staff. A visit to the medical department requiring a clinical examination without missing a full training session or game was classified as a medical attention injury.24 A visit resulting in a player being unable to fully participate in the training session or game the following day was classified as a time-loss injury (TLI).24 Therefore, our dataset comprised not only TLIs but also all of the medical attention injuries. The layoff period (or player unavailability) was calculated by the number of days missed from the date of injury (day zero) until the day before the return to training participation and game availability.5 Growth-related injuries were not explicitly considered by the 2006 consensus statement on injury definitions.24 Therefore, because we wanted to prospectively collect data with an emphasis on uniformity and accuracy in recording all growth cartilage-related injuries, the injury surveillance system was customized with “growth-related injuries” (eg, apophyseal injuries) and “physeal fracture” added as new injury types. Muscle and functional muscle injuries were classified as per the Munich consensus statement.38 The final diagnosis was established by the sports physician, who considered the history, clinical examination, and imaging investigations or after further referral when performed.
Anthropometric Measurements
All anthropometric measures were taken in the morning (∼7:30 to 9:00 am) at the beginning of each season by an experienced assessor of the International Society for the Advancement of Kinanthropometry. Measures included standing and sitting height (±0.1 cm; Holtain Limited) and body mass (±0.1 kg; ADE Electronic Column Scales). We performed landmarking and summed measurements of the 7 skinfold sites (triceps, subscapular, biceps, supraspinale, abdominal, thigh, and medial calf) (±0.1 mm Harpenden skinfold caliper; Baty International) in accordance with international standards.41
Skeletal Age and Maturity Status
A plain anteroposterior radiograph of the left hand and wrist was taken by a trained technician as part of the preseason annual medical screening at the commencement of each new season. All SA measurements were assessed during the 4 seasons by a single experienced observer using the Fels protocol, which has previously demonstrated excellent intratester reliability (intraclass correlation coefficient = 0.998).28 The Fels method was used to estimate SA.46 The skeletal maturity status, calculated as SA minus chronological age, were classified as follows: late maturers, SA >1 year behind chronological age; normal maturers, SA ±1 year of chronological age; early maturers, SA >1 year ahead of chronological age; and mature, SA = 18 years (hand and wrist fully ossified).35 The players’ maturity status was updated in each successive season in line with their new radiological assessment.
Data Analysis
All of the periods throughout the season (excluding only the interseason break) were included for each age group’s seasonal plan. Then, on an individual basis, all time intervals were considered, including time to first injury, time between all subsequent injuries, and time through to the end of the season. The analysis carefully considered events where injury occurrence and return to play did not occur in the same season (time loss during the break was included). When the injury occurred outside of the soccer program with a related absence from the soccer program, time loss and exposure of the individual were excluded. The data were analyzed using STATA (Release 11; StataCorp LP). Descriptive statistics are presented as mean with standard deviation for continuous variables and as frequency and percentage for categorical variables. Poisson-based 95% CIs were computed, and differences between incidences were thus calculated.23 A stratified Cox proportional hazards model that stratifies the order of injuries, after adjusting the variances of hazard ratios (HRs) among recurrent events on the same participants, was performed to determine the effect of skeletal maturity. HR, adjusted HR, and 95% CI were calculated. Kaplan-Meier survival curves are presented for each of the growth and maturity groups. Statistical significance was set at P < .05. We performed a planned separate analysis for lower limb apophyseal injuries, as we hypothesized that these injuries would have the strongest association with skeletal maturity.
Results
Of the final cohort, 454 player-seasons were assessed relative to skeletal maturity. Participant demographics are outlined in Table 1. These players sustained a total of 1565 injuries: 632 (40%) were medical attention injuries and 933 (60%) were TLIs resulting in 17,772 days lost (Table 2). A total of 736 (47%) injuries occurred in training and 829 (53%) in games. Most injuries were noncontact for all of the skeletal maturity classifications (range, 58%-63%).
Table 1.
Demographic Characteristics by Skeletal Maturity Statusa
| Skeletal Maturity | |||||
|---|---|---|---|---|---|
| Late | Normal | Early | Mature | Overall | |
| (n = 10) | (n = 158) | (n = 192) | (n = 94) | (N = 454) | |
| Season | |||||
| 1 | 4 (3.3) | 53 (43.8) | 43 (35.5) | 21 (17.4) | 121 |
| 2 | 2 (1.9) | 35 (33.3) | 48 (45.7) | 20 (19.0) | 105 |
| 3 | 4 (3.6) | 36 (32.4) | 50 (45.0) | 21 (18.9) | 111 |
| 4 | 0 (0) | 34 (29.1) | 51 (43.6) | 32 (27.4) | 117 |
| Age, y | |||||
| Current | 14.1 ± 1.4 | 14.7 ± 1.6 | 14.7 ± 1.4 | 16.7 ± 1.0 | 15.0 ± 1.6 |
| Skeletal | 12.0 ± 1.7 | 14.6 ± 1.9 | 16.4 ± 1.5 | 18.0 ± 0.0 | 16.0 ± 2.0 |
| Anthropometry | |||||
| Height, cm | 151.1 ± 9.8 | 161.1 ± 10.4 | 167.7 ± 9.3 | 173.2 ± 6.3 | 166.1 ± 10.4 |
| Trunk height, cm | 77.0 ± 4.7 | 83.2 ± 5.7 | 88.1 ± 5.6 | 91.7 ± 3.2 | 86.8 ± 6.3 |
| Leg length, cm | 74.1 ± 6.2 | 78.1 ± 5.5 | 79.9 ± 4.4 | 81.5 ± 4.6 | 79.4 ± 5.1 |
| Arm span, cm | 154.3 ± 15.1 | 164.9 ± 12.0 | 171.9 ± 10.5 | 177.7 ± 7.3 | 170.0 ± 11.9 |
| Body mass, kg | 39.3 ± 7.9 | 48.8 ± 9.2 | 57.6 ± 10.0 | 66.6 ± 6.6 | 55.6 ± 11.2 |
| Body mass index, kg/m2 | 17.0 ± 1.2 | 18.6 ± 1.9 | 20.3 ± 2.1 | 21.9 ± 1.9 | 20.0 ± 2.3 |
| Sum of 7 skinfolds, mm | 48.8 ± 16.8 | 48.5 ± 16.7 | 54.1 ± 18.1 | 54.7 ± 12.4 | 52.6 ± 16.9 |
| Player position | |||||
| Goalkeeper | 1 (2.1) | 9 (18.8) | 23 (47.9) | 15 (31.3) | 48 |
| Defender | 1 (0.8) | 54 (41.9) | 50 (38.8) | 24 (18.6) | 129 |
| Forward | 4 (5.4) | 13 (17.6) | 39 (52.7) | 18 (24.3) | 74 |
| Midfielder | 3 (1.7) | 72 (39.8) | 69 (38.1) | 37 (20.4) | 181 |
| No position | 1 (4.5) | 10 (45.5) | 11 (50) | 0 (0) | 22 |
aData are reported as count (%) or mean ± SD.
Table 2.
Medical Attention and Time-Loss Injuries by Skeletal Maturity Statusa
| Skeletal Maturity | |||||
|---|---|---|---|---|---|
| Late | Normal | Early | Mature | Total | |
| Body part injured | |||||
| Head and trunk | 2 (6.3) | 39 (8.7) | 66 (9.5) | 26 (6.6) | 133 (8.5) |
| Upper limb | 1 (3.1) | 39 (8.7) | 62 (9.0) | 22 (5.6) | 124 (7.9) |
| Lower limb | 29 (90.6) | 368 (82.6) | 564 (81.5) | 347 (87.8) | 1308 (83.6) |
| Injury origin | |||||
| Training | 22 (68.8) | 205 (46.0) | 300 (43.4) | 209 (52.9) | 736 (47.1) |
| Match | 10 (31.3) | 241 (54.0) | 392 (56.6) | 186 (47.1) | 829 (52.9) |
| Injury type | |||||
| Contact | 12 (37.5) | 187 (41.9) | 287 (41.5) | 146 (37.0) | 632 (40.4) |
| Noncontact | 20 (62.5) | 259 (58.1) | 405 (58.5) | 249 (63.0) | 933 (59.6) |
| Severity | |||||
| Severe (>4 wk) | 4 (12.5) | 53 (11.9) | 57 (8.2) | 52 (13.2) | 166 (10.6) |
| Major (8-28 d) | 4 (12.5) | 77 (17.3) | 119 (17.2) | 53 (13.4) | 253 (16.2) |
| Moderate (4-7 d) | 6 (18.8) | 69 (15.5) | 70 (10.1) | 34 (8.6) | 179 (11.5) |
| Minor (1-3 d) | 5 (15.6) | 102 (22.9) | 162 (23.4) | 66 (16.7) | 335 (21.4) |
| Medical attention | 13 (40.6) | 145 (32.5) | 284 (41.0) | 190 (48.1) | 632 (40.4) |
| Total | 32 (2.0) | 446 (28.5) | 692 (44.2) | 395 (25.2) | 1565 (100) |
aData are reported as count (%).
The average TLI incidence for a squad of 25 players was 51 injuries per squad-season with a burden of 979 days lost per squad-season. Contusions (23%) were the most prevalent TLI, followed by ligament sprain injuries (17%), growth-related injuries (16%), and functional muscle disorders (15%). Frequency, prevalence, and incidences per squad-season for injury types and injury locations were stratified by skeletal maturity status and are shown in Tables 3 and 4.
Table 3.
Frequency and Incidence per Squad-Season of Injury Types According to Skeletal Maturity Status
| Late | Normal | Early | Mature | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Injury Type | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, |
| n (%)a | n (%) [Incidenceb] | n (%)a | n (%) [Incidenceb] | n (%)a | n (%) [Incidenceb] | n (%)a | n (%) [Incidenceb] | n (%)a | n (%) | |
| Contusion/bruise/hematoma | 11 (34.4) | 3 (15.8) [7.5] | 156 (35.0) | 85 (28.2) [13.4] | 230 (33.2) | 90 (22.1) [11.7] | 122 (30.9) | 37 (18.0) [9.8] | 519 (33.2) | 215 (23.0) |
| Sprain/ligament | 2 (6.3) | 2 (10.5) [5.0] | 44 (9.9) | 31 (10.3) [4.9e,m] | 96 (13.9) | 76 (18.6) [9.9n] | 66 (16.7) | 52 (25.4) [13.8n] | 208 (13.3) | 161 (17.3) |
| Growth-related | 6 (18.8) | 5 (26.3) [12.5m] | 84 (18.8) | 68 (22.6) [10.8m] | 83 (12.0) | 63 (15.4) [8.2m] | 25 (6.3) | 14 (6.8) [3.7n,e,l] | 198 (12.7) | 150 (16.1) |
| Functional muscle disorder | 5 (15.6) | 3 (15.8) [7.5] | 69 (15.5) | 36 (12.0) [5.7e] | 134 (19.4) | 77 (18.9) [10.0n] | 81 (20.5) | 27 (13.2) [7.2] | 289 (18.5) | 143 (15.3) |
| Muscle strain/rupture | 2 (6.3) | 2 (10.5) [5.0] | 28 (6.3) | 28 (9.3) [4.4m] | 31 (4.5) | 30 (7.4) [3.9m] | 30 (7.6) | 30 (14.6) [8.0n,e] | 91 (5.8) | 90 (9.6) |
| Overuse (nonspecific) | 2 (6.3) | 1 (5.3) [2.5] | 16 (3.6) | 13 (4.3) [2.1] | 43 (6.2) | 24 (5.9) [3.1] | 23 (5.8) | 12 (5.9) [3.2] | 84 (5.4) | 50 (5.4) |
| Physeal fracture | — | — | 15 (3.4) | 15 (5.0) [2.4m] | 12 (1.7) | 11 (2.7) [1.4] | 1 (0.3) | 1 (0.5 [0.3n] | 28 (1.8) | 27 (2.9) |
| Fracture (nonphyseal) | 1 (3.1) | 1 (5.3) [2.5] | 9 (2.0) | 9 (3.0) [1.4] | 12 (1.7) | 11 (2.7) [1.4] | 5 (1.3) | 5 (2.4) [1.3] | 27 (1.7) | 26 (2.8) |
| Other bone injury | 1 (3.1) | 1 (5.3) [2.5e] | 8 (1.8) | 7 (2.3) [1.1e,m] | 4 (0.6) | 2 (0.5) [0.3n,m,l] | 14 (3.5) | 13 (6.3) [3.5n,e] | 27 (1.7) | 23 (2.5) |
| Meniscal/cartilage lesion | — | — | 1 (0.2) | 1 (0.3) [0.2m] | 7 (1.0) | 7 (1.7) [0.9] | 4 (1.0) | 4 (2.0) [1.1n] | 12 (0.8) | 12 (1.3) |
| Other injury | 1 (3.1) | — | 7 (1.6) | 4 (1.3) [0.6] | 21 (3.0) | 5 (1.2) [0.7] | 8 (2.0) | 3 (1.5) [0.8] | 37 (2.4) | 12 (1.3) |
| Concussion | — | — | 2 (0.4) | 1 (0.3) [0.2] | 8 (1.2) | 6 (1.5) [0.8] | 1 (0.3) | 1 (0.5) [0.3] | 11 (0.7) | 8 (0.9) |
| Tendinopathy | 1 (3.1) | 1 (5.3) [2.5n,e] | 4 (0.9) | 1 (0.3) [0.2l] | 6 (0.9) | 2 (0.5) [0.3l] | 8 (2.0) | 3 (1.5) [0.8] | 19 (1.2) | 7 (0.8) |
| Synovitis/effusion | — | — | 1 (0.2) | 1 (0.3) [0.2] | 2 (0.3) | 1 (0.2) [0.1] | 6 (1.5) | 2 (1.0) [0.5] | 9 (0.6) | 4 (0.4) |
| Abrasion/laceration | — | — | 2 (0.4) | 1 (0.3) [0.2] | 2 (0.3) | 2 (0.5) [0.3] | — | — | 4 (0.3) | 3 (0.3) |
| Dislocation/subluxation | — | — | — | — | 1 (0.1) | 1 (0.2) [0.1] | 1 (0.3) | 1 (0.5) [0.3] | 2 (0.1) | 2 (0.2) |
| Total | 32 (100) | 19 (100) [47.5] | 446 (100) | 301 (100) [47.6E,M] | 692 (100) | 408 (100) [53.1N] | 395 (100) | 205 (100) [54.5N] | 1565 (100) | 933 (100) |
aIncludes all medical attention and time-loss injuries. —, none.
bIncidence is expressed per squad-season and established for a squad of 25 players.
Significantly different from late maturers: LP < .001; lP < .05.
Significantly different from normal maturers: NP < .001; nP < .05.
Significantly different from early maturers: EP < .001; eP < .05.
Significantly different from mature: MP < .001; mP < .05.
Table 4.
Frequency and Incidences per Squad-Season of Injuries by Location According to Skeletal Maturity Status
| Late | Normal | Early | Mature | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Body part | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, | Total, | Time-loss, |
| n (%)a | n (%) [Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%) | |
| Ankle | 7 (21.9) | 5 (26.3) [12.5] | 48 (10.8) | 38 (12.6) [6.0m] | 84 (12.1) | 62 (15.2) [8.1] | 57 (14.4) | 41 (20.0) [10.9n] | 196 (12.5) | 146 (15.6) |
| Knee | 7 (21.9) | 4 (21.1) [10.0] | 79 (17.7) | 55 (18.3) [8.7] | 83 (12.0) | 54 (13.2) [7.0] | 56 (14.2) | 32 (15.6) [8.5] | 225 (14.4) | 145 (15.5) |
| Pelvis/hip/groin | 2 (6.3) | 2 (10.5) [5.0] | 52 (11.7) | 37 (12.3) [5.9] | 84 (12.1) | 61 (15.0) [7.9] | 42 (10.6) | 28 (13.7) [7.4] | 180 (11.5) | 128 (13.7) |
| Hamstring | 3 (9.4) | 3 (15.8) [7.5] | 39 (8.7) | 28 (9.3) [4.4] | 57 (8.2) | 41 (10.0) [5.3] | 36 (9.1) | 23 (11.2) [6.1] | 135 (8.6) | 95 (10.2) |
| Quadriceps | 3 (9.4) | 1 (5.3) [2.5] | 40 (9.0) | 33 (11.0) [5.2] | 72 (10.4) | 40 (9.8) [5.2] | 38 (9.6) | 15 (7.3) [4.0] | 153 (9.8) | 89 (9.5) |
| Foot/toes | 2 (6.3) | 1 (5.3) [2.5] | 45 (10.1) | 32 (10.6) [5.1] | 59 (8.5) | 35 (8.6) [4.6] | 33 (8.4) | 13 (6.3) [3.5] | 139 (8.9) | 81 (8.7) |
| Adductor | — | — | 14 (3.1) | 11 (3.7) [1.7m] | 33 (4.8) | 25 (6.1) [3.3] | 33 (8.4) | 20 (9.8) [5.3n] | 80 (5.1) | 56 (6.0) |
| Abdomen/lumbar spine | — | — | 23 (5.2) | 16 (5.3) [2.5] | 37 (5.3) | 22 (5.4) [2.9] | 17 (4.3) | 5 (2.4) [1.3] | 77 (4.9) | 43 (4.6) |
| Lower leg | 1 (3.1) | — | 30 (6.7) | 18 (6.0) [2.8] | 42 (6.1) | 14 (3.4) [1.8] | 22 (5.6) | 6 (2.9) [1.6] | 95 (6.1) | 38 (4.1) |
| Calf/Achilles tendon | 2 (6.3) | 1 (5.3) [2.5] | 15 (3.4) | 6 (2.0) [0.9] | 45 (6.5) | 16 (3.9) [2.1] | 20 (5.1) | 4 (2.0) [1.1] | 82 (5.2) | 27 (2.9) |
| Hand/fingers | — | — | 23 (5.2) | 8 (2.7) [1.3] | 29 (4.2) | 10 (2.5) [1.3] | 14 (3.5) | 7 (3.4) [1.9] | 66 (4.2) | 25 (2.7) |
| Forearm/wrist | — | — | 8 (1.8) | 7 (2.3) [1.1] | 14 (2.0) | 7 (1.7) [0.9] | 5 (1.3) | 4 (2.0) [1.1] | 27 (1.7) | 18 (1.9) |
| Head/face | — | — | 5 (1.1) | 1 (0.3) [0.2e] | 16 (2.3) | 10 (2.5) [1.3n] | 1 (0.3) | 1 (0.5) [0.3] | 22 (1.4) | 12 (1.3) |
| Shoulder/clavicle | 2 (6.3) | 1 (5.3) [2.5m] | 7 (1.6) | 3 (1.0) [0.5] | 13 (1.9) | 4 (1.0) [0.5] | — | — | 22 (1.4) | 8 (0.9) |
| Thigh | 2 (6.3) | 1 (5.3) [2.5e] | 6 (1.3) | 3 (1.0) [0.5] | 5 (0.7) | 1 (0.2) [0.1l] | 10 (2.5) | 3 (1.5) [0.8l] | 23 (1.5) | 8 (0.9) |
| Ribs/thoracic spine | — | — | 7 (1.6) | 3 (1.0) [0.5] | 9 (1.3) | 2 (0.5) [0.3] | 6 (1.5) | 2 (1.0) [0.5] | 22 (1.4) | 7 (0.8) |
| Elbow | 1 (3.1) | — | 1 (0.2) | — | 5 (0.7) | 3 (0.7) [0.4] | 3 (0.8) | 1 (0.5) [0.3] | 10 (0.6) | 4 (0.4) |
| Neck/cervical spine | — | — | 4 (0.9) | 2 (0.7) [0.3] | 4 (0.6) | 1 (0.2) [0.1] | 2 (0.5) | — | 10 (0.6) | 3 (0.3) |
| Upper arm | — | — | — | — | 1 (0.1) | — | — | — | 1 (0.1) | — |
| Total | 32 (100) | 19 (100) [47.5] | 446 (100) | 301 (100) [47.6E,M] | 692 (100) | 408 (100) [53.1N] | 395 (100) | 205 (100) [54.5N] | 1565 (100) | 933 (100) |
aIncludes all medical attention and time-loss injuries. —, none.
bIncidence is expressed per squad-season and established for a squad of 25 players.
Significantly different from late maturers: LP < .001; lP < .05.
Significantly different from normal maturers: NP < .001; nP < .05.
Significantly different from early maturers: EP < .001; eP < .05.
Significantly different from mature: MP < .001; mP < .05.
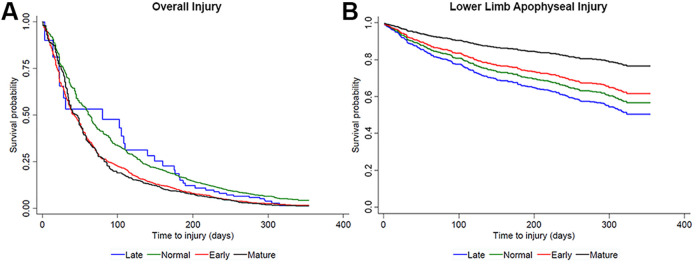
Among the growth-related injuries, 94% were related to an apophysis of the lower limb and 75% were TLIs (Table 5). Anterior inferior iliac spine osteochondrosis (16%), Osgood-Schlatter disease (28%), and Sever disease (6%) were the most prevalent apophyseal injuries for the hip/pelvis, knee, and foot/ankle, respectively. Figure 2 displays the injury-free survival analysis for the overall injury risk and the lower limb apophyseal injury risk. After adjustment for age and other confounders such as playing position, anthropometric characteristics, and season, chronological age was positively associated with a higher injury risk in the Cox regression analysis (HR, 1.17; 95% CI, 1.13-1.22; P < .001). Early maturers had a significant 26% to 35% greater HR for overall injury risk compared with normal maturers and mature players, respectively (P < .001 for both) (Table 6). Players who were skeletally mature had a significantly decreased risk of lower extremity apophyseal injuries compared with late (P < .05), normal (P < .05), and early maturers (P < .001), by 45% to 61% (Table 6).
Table 5.
Frequency and Incidences per Squad-Season of Lower Limb Apophyseal Injuries by Location and Diagnosis According to Skeletal Maturity Status
| Late | Normal | Early | Mature | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Total, | Time-Loss, | Total, | Time-Loss, | Total, | Time-Loss, | Total, | Time-Loss, | Total, | Time-Los s, |
| n (%)a | n (%)[Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%)[Incidenceb] | n (%)a | n (%) | |
| Hip/Pelvis | ||||||||||
| AIIS osteochondrosis | 1 (16.7) | 1 (20.0) [2.5] | 12 (15.4) | 8 (12.7) [1.3] | 17 (21.8) | 13 (22.4) [1.7m] | 3 (12.0) | 1 (7.1) [0.3e] | 33 (17.6) | 23 (16.4) |
| Pubis osteochondrosis | — | — | 7 (9.0) | 5 (7.9) [0.8] | 12 (15.4) | 11 (19.0) [1.4] | 4 (16.0) | 3 (21.4) [0.8] | 23 (12.3) | 19 (13.6) |
| Lesser trochanter osteochondrosis | — | — | 4 (5.1) | 4 (6.3) [0.6] | 10 (12.8) | 10 (17.2) [1.3] | 2 (8.0) | 2 (14.3) [0.5] | 16 (8.6) | 16 (11.4) |
| ASIS osteochondrosis | 1 (16.7) | 1 (20.0) [2.5] | 4 (5.1) | 3 (4.8) [0.5] | 5 (6.4) | 4 (6.9) [0.5] | 2 (8.0) | 2 (14.3) [0.5] | 12 (6.4) | 10 (7.1) |
| AIIS avulsion | — | — | 7 (9.0) | 7 (11.1) [1.1e] | 1 (1.3) | 1 (1.7) [0.1n] | 1 (4.0) | 1 (7.1) [0.3] | 9 (4.8) | 9 (6.4) |
| Ischium osteochondrosis | — | — | 2 (2.6) | 2 (3.2) [0.3] | 2 (2.6) | — | 2 (8.0) | 2 (14.3) [0.5e] | 6 (3.2) | 4 (2.9) |
| Iliac crest osteochondrosis | — | — | — | — | 4 (5.1) | 2 (3.4) [0.3] | — | — | 4 (2.1) | 2 (1.4) |
| ASIS avulsion | — | — | 1 (1.3) | 1 (1.6) [0.2] | — | — | 1 (4.0) | 1 (7.1) [0.3] | 2 (1.1) | 2 (1.4) |
| Iliac crest avulsion | — | — | — | — | 1 (1.3) | 1 (1.7) [0.1] | — | — | 1 (0.5) | 1 (0.7) |
| Ischium avulsion | — | — | — | — | 1 (1.3) | 1 (1.7) [0.1] | — | — | 1 (0.5) | 1 (0.7) |
| Total | 2 (33.3) | 2 (40.0) [5.0] | 37 (47.4) | 30 (47.6) [4.7] | 53 (67.9) | 43 (74.1) [5.6] | 15 (60.0) | 12 (85.7) [3.2] | 107 (57.2) | 87 (62.1) |
| Knee | ||||||||||
| Osgood-Schlatter | 4 (66.7) | 3 (60.0) [7.5e,M] | 27 (34.6) | 22 (34.9) [3.5e,m] | 20 (25.6) | 12 (20.7) [1.6n,l] | 10 (40.0) | 2 (14.3) [0.5n,L] | 61 (32.6) | 39 (27.9) |
| Sinding-Larson | — | — | 4 (5.1) | 3 (4.8) [0.5] | 1 (1.3) | — | 5 (2.7) | 3 (2.1) | ||
| Total | 4 (66.7) | 3 (60.0) [7.5e,M] | 31 (39.7) | 25 (39.7) [4.0e,M] | 21 (26.9) | 12 (20.7) [1.6n,l] | 10 (40.0) | 2 (14.3) [0.5N,L] | 66 (35.3) | 42 (30.0) |
| Foot/Ankle | ||||||||||
| Sever disease | — | — | 9 (11.5) | 7 (11.1) [1.1e,m] | 2 (2.6) | 1 (1.7) [0.1n] | — | — | 11 (5.9) | 8 (5.7) |
| Kohler disease | — | — | 1 (1.3) | 1 (1.6) [0.2] | 1 (1.3) | 1 (1.7) [0.1] | — | — | 2 (1.1) | 2 (1.4) |
| Iselin avulsion | — | — | — | — | 1 (1.3) | 1 (1.7) [0.1] | — | — | 1 (0.5) | 1 (0.7) |
| Total | — | — | 10 (12.8) | 8 (12.7) [1.3m] | 4 (5.1) | 3 (5.2) [0.4] | — | — | 14 (7.5) | 11 (7.9) |
| Overall total | 6 (100) | 5 (100) [12.5m] | 78 (100) | 63 (100) [10.0M] | 78 (100) | 58 (100) [7.5m] | 25 (100) | 14 (100) [3.7N,e,l] | 187 (100) | 140 (100) |
aIncludes all medical attention and time-loss injuries. AIIS, antero inferior iliac spine; ASIS, antero superior iliac spine; —, none.
bIncidence is expressed per squad-season and established for a squad of 25 players.
Significantly different from late maturers: LP < .001; lP < .05.
Significantly different from normal maturers: NP < .001; nP < .05.
Significantly different from early maturers: EP < .001; eP < .05.
Significantly different from mature: MP < .001; mP < .05.
Figure 2.
Kaplan-Meier analysis estimates of (A) overall injury risk and (B) lower limb apophyseal injury risk. Time to injury was compared between the different skeletal maturity groups.
Table 6.
Cox Regression Analysis Estimates of Injury Risk Overall and for Lower Limb Apophyseal Injuries According to Skeletal Maturity Statusa
| Late | Normal | Early | Mature | |
|---|---|---|---|---|
| Overall Injury Risk | ||||
| Unadjusted HR (95% CI) | ||||
| Late | — | 1.15 (0.81-1.65) | 0.87 (0.61-1.24) | 0.82 (0.58-1.18) |
| Normal | 0.86 (0.60-1.24) | — | 0.75 (0.67-0.85)b | 0.71 (0.62-0.82)b |
| Early | 1.15 (0.81-1.64) | 1.33 (1.18-1.50)b | — | 0.95 (0.84-1.08) |
| Mature | 1.21 (0.84-1.74) | 1.40 (1.22-1.60)b | 1.05 (0.93-1.19) | — |
| Adjusted HR (95% CI) | ||||
| Late | — | 1.23 (0.86-1.78) | 0.98 (0.68-1.40) | 1.32 (0.91-1.93) |
| Normal | 0.81 (0.56-1.17) | — | 0.79 (0.70-0.90)b | 1.07 (0.92-1.25) |
| Early | 1.02 (0.71-1.46) | 1.26 (1.11-1.42)b | — | 1.35 (1.17-1.56)b |
| Mature | 0.76 (0.52-1.10) | 0.93 (0.80-1.09) | 0.74 (0.64-0.86)b | — |
| Lower Limb Apophyseal Injury Risk | ||||
| Unadjusted HR (95% CI) | ||||
| Late | — | 1.19 (0.52-2.73) | 1.40 (0.61-3.20) | 2.50 (1.02-6.05)c |
| Normal | 0.84 (0.37-1.92) | — | 1.17 (0.86-1.60) | 2.08 (1.33-3.27)b |
| Early | 0.71 (0.31-1.64) | 0.85 (0.63-1.16) | — | 1.78 (1.13-2.78)c |
| Mature | 0.40 (0.16-0.98)c | 0.48 (0.31-0.75)b | 0.56 (0.36-0.88)b | — |
| Adjusted HR (95% CI) | ||||
| Late | — | 1.20 (0.52-2.76) | 1.41 (0.61-3.24) | 2.56 (1.01-6.51)c |
| Normal | 0.83 (0.36-1.91) | — | 1.17 (0.86-1.60) | 2.14 (1.30-3.50)c |
| Early | 0.71 (0.31-1.63) | 0.85 (0.63-1.16) | — | 1.82 (1.11-2.97)c |
| Mature | 0.39 (0.15-0.99)c | 0.47 (0.29-0.77)c | 0.55 (0.34-0.90)b | — |
aHR, hazard ratio; —, none.
bStatistically significant at P < .001.
cStatistically significant at P < .05.
Discussion
This is the first epidemiological study examining associations between skeletal maturity and injuries in elite youth soccer players from Middle East and Asia. The most common types of TLIs were contusions, sprains, and growth-related injuries. Once the analysis was adjusted for confounders, early-maturing players had the highest injury risk. Players who were skeletally mature at the wrist had the lowest risk of lower limb apophyseal injury. Furthermore, they were vulnerable to apophyseal injuries around the hip and pelvis, involving a high prevalence of the pubic apophysis.
“Mature” When Considering Maturity Status
Previous studies that investigated associations between skeletal maturity and injuries in young players were limited by the age range of their cohort (U-9 to U-16), where skeletally immature players were included (late, normal, and early) but skeletally mature status players were not included. In youth academy development, maturity distributions shift toward players with advanced skeletal maturity with increasing chronological age during adolescence.35 This could explain the low number of late-maturing players and the high proportion of early maturers in the elite sports setting.35 Because a part of our cohort reached the boundary of the Fels estimation method, we believed that it was appropriate to use the term mature when the wrist was fully fused. Indeed, this is a biological landmark and a clear cutoff in the magnitude of how far an individual has progressed toward full maturity.35 However, various secondary ossification centers appear around late puberty and generally fuse during late adolescence and early adulthood, especially around the hip and pelvis. These are at risk of injury, and therefore the “mature” status is relative.31,42,47
Medical Attention and Time-Loss Injury Characteristics
The TLI incidence was 51 injuries per squad-season in our study; although substantial, this incidence is lower than the 63 injuries per squad-season reported by Le Gall et al32 but similar to the reported range of incidences (51-55 injuries per squad-season) in previous research in youth soccer players.8,33 The mean layoff period was 19 days per injury, and players were absent from training and matches for an average of 39 days per player-season, which is similar to the 17 days per injury and 44 days per player-season reported in youth French elite players.32 Similar to Le Gall et al,32 we found no significant difference in the incidence of TLIs between the different maturity groups. However, when considering the overall incidence, we noted a substantial increase from normal to early-maturing players and then to mature players, indicating greater use of medical support as the players matured. The injury risk in soccer is directly associated with playing actions and incidents1; therefore, the higher incidence in more mature players might be due to greater competitiveness and physical aggressiveness during playing.4
Early-maturing players had more TLIs in matches compared with late maturers. These results differ from previous studies that found no differences in both training and match injuries between maturity groups.4,32 This discrepancy might potentially come from a statistical type I error due to the small number of late-maturing players in our study. However, it might also highlight the tendency of coaching staff to rely more on early-maturing players and would reinforce the idea that in elite youth soccer, players should theoretically be matched according to their skeletal maturity status to avoid an increasing risk of injury.14 Independent from the relative age effect, SA has been shown to be a robust factor influencing players’ selection to a team.29 Across all skeletal maturity groups, the 11% prevalence of severe injuries in our cohort was similar to the prevalence of severe injuries in the French National Football Institute (10%).32 However, the percentage of severe injuries that we found was lower than the 29% reported in other academies in Europe and South America.11,25 Le Gall et al32 reported a significantly higher incidence of severe injury in late maturers compared with early maturers. This is in contrast with our study, in which mature players had more severe injuries compared with normal and early maturers. This difference may be due to the absence of players who reached “mature” status in the French study.32
Overall Injury Risk and Skeletal Maturity
The primary aim of this study was to evaluate injury risk in relation to skeletal maturity. In that regard, injuries can be recurrent or subsequent, and players may experience more than 1 injury during 1 or more seasons. To adequately address repeated injury events in the same players, we used the Cox proportional hazards model with generalization to recurrent data,51 considering each individual player per season and over the 4-year period (when appropriate).
To date, only 2 studies have considered the effect of skeletal maturity on injury in elite youth soccer players.28,32 Although Le Gall et al32 did not use the same method as us and Johnson to assess bone age, neither study found a significant difference in overall injury incidence between players classified into the different maturity groups. Nevertheless, both investigations found a similar tendency of higher injury incidence in early maturers. When Johnson et al28 used the means of training time, match playing time, and difference in maturity status as covariables, all 3 variables were significantly associated with injury occurrence. This finding is in line with our study, which showed that once the analysis was adjusted for age and other covariables, early maturers had a significant 26% and 35% greater HR compared with normal maturers and mature players, respectively. In contrast with earlier investigations,32 we believe it was important to adjust for the potential influence of chronological age while analyzing the effect of skeletal maturity on injuries.50 This is because the age span of the participants is wide and the literature suggests that injury rates generally increase with increasing chronological age.4,21,30,44 Anecdotally, the late maturers had a nonsignificant but higher HR than normal and mature players. This should be interpreted with caution given the small number of late-maturing players.
Lower Limb Apophyseal Injuries and Skeletal Maturity
Among the growth-related injuries, 94% were related to an apophysis of the lower limb and 75% were TLIs. Our study showed that the risk of lower limb apophyseal injury, ranging from 45% to 61%, was lower in mature players compared with players at the 3 skeletally immature status. Although there were no significant differences in the adjusted injury risk between the 3 skeletally immature status, the late maturers had a nonsignificant but higher incidence of apophyseal injuries. This trend may have failed to achieve significance because of the small number of late maturers, as a result of selection processes in the academy. A comparable, lower risk of growth plate injuries was found in elite athletes with more advanced skeletal maturity.54
Recently, in a Basque soccer academy, growth-related injuries were predominantly found in players before they reached 96% of their final adult height estimation.37 Similar to a study of elite French players,32 our results indicate a greater incidence of Osgood-Schlatter disease in late and normal maturers in comparison with early maturers and mature players. Intuitively, one might hypothesize that advanced skeletally maturity and mature adolescent players are less prone to physeal and apophyseal injuries. This was the case in our cohort, where players who were skeletally mature at the wrist had less risk of lower limb apophyseal injuries. The remaining TLIs of the lower limb apophyses in this group occurred significantly more at the hip and pelvis (P = .008). Likewise, a higher frequency of lower limb apophyseal injuries at the hip and pelvis was found in the early maturers (P > .001). The inconsistency in the location of the apophyseal injuries in our study compared with the results of Le Gall et al32 comes initially from the single age group of early adolescents (U-14) included in their study. A wide range of early adolescents can be at the endochondral ossification stage of some apophyses (eg, knee) and at the same time at the cartilaginous stage in other apophyses (eg, hip or pelvis),40,42 consequently presenting dissimilar risks of apophyseal injury location.19
Our cohort presented a broad level of skeletal maturity from early to late adolescents. The high proportion of hip and pelvic apophyseal injuries in mature players, with the pubic apophysis as the most prevalent (21%), could be explained by the ossification process. Although intraindividual variability in musculoskeletal growth and skeletal maturity is wide,35 the apophyseal ossification chronology of the lower limb remains sequential. The apophyses commonly fuse from distal to proximal, with substantial differences between upper and lower limbs.42 Within this sequence, each apophysis has its own morphological pattern of maturation.42 Consequently, when the wrist reaches complete ossification, other apophyses of both upper and lower limbs remain open.42 This is the case for several types of pelvic apophyses (eg, iliac crest, pubic), for which fusion will not occur before 25 years of age.40,42 Therefore, hip and pelvic apophyseal injuries will likely arise (1) in mid- to late adolescence, (2) in young adulthood, (3) in adolescents with advanced skeletal maturity level, or (4) in young adults with late maturity, as recently observed in Australian footballers.31,47 This reinforces the idea that periods of rapid growth should not be systematically considered an etiological factor for apophyseal injury.50
Intensive training schedules have been suggested as a factor in apophyseal injuries; the pathogenesis of training-related injuries is not well understood, but these injuries are recognized to be specific for each apophysis.32,34 Changes in hip angular velocities, adductor muscle force, and inertia have been suggested to increase stress on the adductors’ apophyses in U-15 soccer players.20 For Osgood-Schlatter disease, alongside regular sports practice, many intrinsic factors such as height, mass, body mass index, and muscle group tightness have been identified as risk factors.15,39,52 History of previous osteochondrosis is recognized as a risk factor for subsequent osteochondrosis in a different unfused apophysis, suggesting a probable ethnicity component behind an abnormal response of the endochondral ossification center to certain mechanical stresses.12,18,39,48,49,52 Furthermore, the potential impact of vitamin D deficiency is an additional intrinsic factor that needs to be considered in Middle Eastern sporting populations.26
Skeletal Maturity and Other Types of Injury
In U-14 elite French players, a higher incidence of tendinopathy and groin strains was reported in early-maturing players.32 In our cohort, early maturers had more time loss due to functional muscle disorders than normal maturers but not when compared with mature players. One explanation could be that early-maturing players are more physiologically advanced in the maturity process and capable of performing more intensive work, resulting in higher muscle damage2 and consequent (perceived) delayed-onset muscle soreness (DOMS).16,27 Mature players may have attained a certain level of sport-specific muscle adaptation, reducing the incidence of DOMS.45
A higher incidence of ligament sprain, strain, and adductor injuries was observed in mature players. Monasterio et al37 found similar injury patterns, with the majority of these injuries occurring in players closer to their final estimated height (median, 97.9%-99%). Several explanations may be suggested for this higher incidence of muscle strains and adductor injuries. Mature players have a greater body mass, and an increased risk of lower limb muscle strains has been observed in soccer players with a higher body mass.43 In soccer players, increased thigh muscle tightness and lower hip abduction have been found to increase the risk of hamstring, quadriceps, and groin strains.3,55 In more mature players, the limbs may be heavier and require more force to move them. Mature players, owing to their greater body size, have been found to have higher movement and match running performances than their “younger,” less mature teammates. This may increase the chance of strain injuries by evolving in a more demanding context.3,7
A higher prevalence and incidence of physeal fractures were observed in normal maturers compared with early maturers and in early maturers compared with mature players. Although physeal fractures are not infrequent in youth sports, they have been previously disregarded in youth soccer epidemiology studies.9 In players of the same chronological age, normal maturers have a more open physis than early maturers and therefore are at greater risk of physeal fractures. Mature players might have more physical power and aggressiveness on the field,1 leading to more contact injuries, but because most of their physes are closed, these players seem less vulnerable to physeal fractures. Last, we hypothesize that in contact sports, the size differences associated with the skeletal maturity level for the same chronological age might expose the less mature players to a mechanical disadvantage on the field.
More prospective investigations of large cohorts are required to improve the understanding of injury patterns in relation to growth, maturation, and training load in elite youth soccer development. The present research should be extended to diverse regions of the world to appreciate variations with ethnicity and environment.
Strength and Limitations
Care should be taken in generalizing the findings of this study beyond the specific cohort and methodological approach used, and there are some limitations that should be acknowledged. With regard to skeletal maturity assessment, the ethnic variation of this cohort with other studies requires some consideration.35 Also, individual exposure time was not recorded, and therefore the injury incidence in relation to exposure time cannot be calculated. However, the latest International Olympic Committee consensus statement has suggested expressing the incidences of injury per number of players per period of the concerned sports.5 Unlike the majority of research in this field, the consideration of confounders in our study limited potential bias in the interpretation of the results.50 Additionally, the inclusion of specific additional items related to pediatric injuries in the injury surveillance system provided a more accurate and consistent record, probably leading to a greater clinical contribution, as previously recommended.5
Conclusion
Our large, prospective study is the first to investigate the association between skeletal maturity and musculoskeletal injuries in youth male elite soccer players from the Middle East. Musculoskeletal injury patterns and injury risks varied depending on the players’ skeletal maturity. Early-maturing players had the greatest overall injury risk. Players who were skeletally mature at the wrist were at the lowest risk of lower extremity apophyseal injuries but were still vulnerable to hip and pelvic apophyseal injuries. Incidence of muscle strain per squad-season was 2 times higher in mature players than in normal maturers and early maturers. Considering skeletal maturity can benefit all players and has important implications in injury prevention and clinical management.
Acknowledgment
The authors gratefully thank Dr Amanda Johnson for the assessment of skeletal maturity status in this study. This work would not have been achieved without the commitment of all football physiotherapists of Aspire Academy and their uniform accuracy and consistency in data collection over the years.
Footnotes
Final revision submitted December 3, 2020; accepted January 5, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Anti-Doping Lab Qatar Institutional Review Board (ref No. SCH-ADL-070).
References
- 1. Andersen TE, Larsen O, Tenga A, Engebretsen L, Bahr R. Football incident analysis: a new video based method to describe injury mechanisms in professional football. Br J Sports Med. 2003;37(3):226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Armstrong N, Barker AR, McManus AM. Muscle metabolism changes with age and maturation: how do they relate to youth sport performance? Br J Sports Med. 2015;49(13):860–864. [DOI] [PubMed] [Google Scholar]
- 3. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1_suppl):5S–16S. [DOI] [PubMed] [Google Scholar]
- 4. Backous DD, Friedl KE, Smith NJ, Parr TJ, Carpine WD, Jr. Soccer injuries and their relation to physical maturity. Am J Dis Child. 1988;142(8):839–842. [DOI] [PubMed] [Google Scholar]
- 5. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. 2020;54(6):372–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baxter-Jones A, Maffulli N, Helms P. Low injury rates in elite athletes. Arch Dis Child. 1993;68(1):130–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buchheit M, Mendez-Villanueva A. Effects of age, maturity and body dimensions on match running performance in highly trained under-15 soccer players. J Sports Sci. 2014;32(13):1271–1278. [DOI] [PubMed] [Google Scholar]
- 8. Bult HJ, Barendrecht M, Tak IJR. Injury risk and injury burden are related to age group and peak height velocity among talented male youth soccer players. Orthop J Sports Med. 2018;6(12):2325967118811042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Caine D. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40(9):749–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caine DJ. Are kids having a rough time of it in sports? Br J Sports Med. 2010;44(1):1–3. [DOI] [PubMed] [Google Scholar]
- 11. Cezarino LG, Gruninger B, Scattone Silva R. Injury profile in a Brazilian first-division youth soccer team: a prospective study. J Athl Train. 2020;55(3):295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Collins M. Genetic risk factors for soft-tissue injuries 101: a practical summary to help clinicians understand the role of genetics and “personalised medicine.” Br J Sports Med. 2010;44(13):915–917. [DOI] [PubMed] [Google Scholar]
- 13. Cook C. Predicting future physical injury in sports: it’s a complicated dynamic system. Br J Sports Med. 2016;50(22):1356–1357. [DOI] [PubMed] [Google Scholar]
- 14. Cumming SP, Brown DJ, Mitchell S, et al. Premier League academy soccer players’ experiences of competing in a tournament bio-banded for biological maturation. J Sports Sci. 2018;36(7):757–765. [DOI] [PubMed] [Google Scholar]
- 15. de Lucena GL, dos Santos Gomes C, Guerra RO. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents. Am J Sports Med. 2010;39(2):415–420. [DOI] [PubMed] [Google Scholar]
- 16. De Ste Croix M, Lehnert M, Maixnerova E, et al. Does maturation influence neuromuscular performance and muscle damage after competitive match-play in youth male soccer players? Eur J Sport Sci. 2019;19(8):1130–1139. [DOI] [PubMed] [Google Scholar]
- 17. DiFiori JP, Benjamin HJ, Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48(4):287–288. [DOI] [PubMed] [Google Scholar]
- 18. Doral MN, Aydog ST, Tetik O, Atay OA, Turhan E, Demirel HA. Multiple osteochondroses and avulsion fracture of anterior superior iliac spine in a soccer player. Br J Sports Med. 2005;39(3):e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Duong MM, Nicholson AD, Li SQ, Gilmore A, Cooperman DR, Liu RW. Relationship between Sever disease and skeletal maturity. J Pediatr Orthop. 2020;40(2):93–96. [DOI] [PubMed] [Google Scholar]
- 20. Dupre T, Lysdal FG, Funken J, et al. Groin injuries in soccer: investigating the effect of age on adductor muscle forces. Med Sci Sports Exerc. 2020;52(6):1330–1337. [DOI] [PubMed] [Google Scholar]
- 21. Faude O, Rossler R, Junge A. Football injuries in children and adolescent players: are there clues for prevention? Sports Med. 2013;43(9):819–837. [DOI] [PubMed] [Google Scholar]
- 22. Fortington LV, van der Worp H, van den Akker-Scheek I, Finch CF. Reporting multiple individual injuries in studies of team ball sports: a systematic review of current practice. Sports Med. 2017;47(6):1103–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Frome EL, Checkoway H. Epidemiologic programs for computers and calculators: use of Poisson regression models in estimating incidence rates and ratios. Am J Epidemiol. 1985;121(2):309–323. [DOI] [PubMed] [Google Scholar]
- 24. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 2006;16(2):83–92. [DOI] [PubMed] [Google Scholar]
- 25. Hall ECR, Larruskain J, Gil SM, et al. An injury audit in high-level male youth soccer players from English, Spanish, Uruguayan and Brazilian academies. Phys Ther Sport. 2020;44:53–60. [DOI] [PubMed] [Google Scholar]
- 26. Hamilton B, Grantham J, Racinais S, Chalabi H. Vitamin D deficiency is endemic in Middle Eastern sportsmen. Public Health Nutr. 2010;13(10):1528–1534. [DOI] [PubMed] [Google Scholar]
- 27. Hotfiel T, Freiwald J, Hoppe MW, et al. Advances in delayed-onset muscle soreness (DOMS), part I: pathogenesis and diagnostics. Sportverletz Sportschaden. 2018;32(4):243–250. [DOI] [PubMed] [Google Scholar]
- 28. Johnson A, Doherty PJ, Freemont A. Investigation of growth, development, and factors associated with injury in elite schoolboy footballers: prospective study. BMJ. 2009;338:B490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson A, Farooq A, Whiteley R. Skeletal maturation status is more strongly associated with academy selection than birth quarter. Sci Med Football. 2017;2(1):1–7. [Google Scholar]
- 30. Jones S, Almousa S, Gibb A, et al. Injury incidence, prevalence and severity in high-level male youth football: a systematic review. Sports Med. 2019;49(12):1879–1899. [DOI] [PubMed] [Google Scholar]
- 31. Koh E, Boyle J. Pubic apophysitis in elite Australian Rules football players: MRI findings and the utility of VIBE sequences in evaluating athletes with groin pain. Clin Radiol. 2020;75(4):293–301. [DOI] [PubMed] [Google Scholar]
- 32. Le Gall F, Carling C, Reilly T. Biological maturity and injury in elite youth football. Scand J Med Sci Sports. 2007;17(5):564–572. [DOI] [PubMed] [Google Scholar]
- 33. Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. 2006;34(6):928–938. [DOI] [PubMed] [Google Scholar]
- 34. Longo UG, Ciuffreda M, Locher J, Maffulli N, Denaro V. Apophyseal injuries in children’s and youth sports. Br Med Bull. 2016;120(1):139–159. [DOI] [PubMed] [Google Scholar]
- 35. Malina RM, Rogol AD, Cumming SP, Coelho e Silva MJ, Figueiredo AJ. Biological maturation of youth athletes: assessment and implications. Br J Sports Med. 2015;49(13):852–859. [DOI] [PubMed] [Google Scholar]
- 36. Merkel DL. Youth sport: positive and negative impact on young athletes. Open Access J Sports Med. 2013;4:151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Monasterio X, Gil SM, Bidaurrazaga-Letona I, et al. Injuries according to the percentage of adult height in an elite soccer academy. J Sci Med Sport. 2021;24(3):218–223. [DOI] [PubMed] [Google Scholar]
- 38. Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47(6):342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nakase J, Goshima K, Numata H, Oshima T, Takata Y, Tsuchiya H. Precise risk factors for Osgood-Schlatter disease. Arch Orthop Trauma Surg. 2015;135(9):1277–1281. [DOI] [PubMed] [Google Scholar]
- 40. Nicholson AD, Liu RW, Sanders JO, Cooperman DR. Relationship of calcaneal and iliac apophyseal ossification to peak height velocity timing in children. J Bone Joint Surg Am. 2015;97(2):147–154. [DOI] [PubMed] [Google Scholar]
- 41. Norton K, Marfell-Jones M, Whittingham N. Anthropometric assessment protocols. In: Gore JC, ed. Physiological Testing for Elite Athletes. Human Kinetics; 2000:66–85. [Google Scholar]
- 42. Ogden JA. Skeletal Injury in the Child. Vol 1. W.B. Saunders; 2000. [Google Scholar]
- 43. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300–303. [DOI] [PubMed] [Google Scholar]
- 44. Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5_suppl):S51–S57. [DOI] [PubMed] [Google Scholar]
- 45. Proske U, Morgan DL. Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J Physiol. 2001;537(pt_2):333–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Roche AF, Thissen D, Chumlea W. Assessing Skeletal Maturity of the Hand-Wrist: Fels Method. Charles C Thomas; 1988. [DOI] [PubMed] [Google Scholar]
- 47. Sailly M, Whiteley R, Read JW, Giuffre B, Johnson A, Holmich P. Pubic apophysitis: a previously undescribed clinical entity of groin pain in athletes. Br J Sports Med. 2015;49(12):828–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sakai T, Sairyo K, Suzue N, Kosaka H, Yasui N. Incidence and etiology of lumbar spondylolysis: review of the literature. J Orthop Sci. 2010;15(3):281–288. [DOI] [PubMed] [Google Scholar]
- 49. Segawa H, Omori G, Koga Y. Multiple osteochondroses of bilateral knee joints. J Orthop Sci. 2001;6(3):286–289. [DOI] [PubMed] [Google Scholar]
- 50. Swain M, Kamper SJ, Maher CG, Broderick C, McKay D, Henschke N. Relationship between growth, maturation and musculoskeletal conditions in adolescents: a systematic review. Br J Sports Med. 2018;52(19):1246–1252. [DOI] [PubMed] [Google Scholar]
- 51. Ullah S, Gabbett TJ, Finch CF. Statistical modelling for recurrent events: an application to sports injuries. Br J Sports Med. 2014;48(17):1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Watanabe H, Fujii M, Yoshimoto M, et al. Pathogenic factors associated with Osgood-Schlatter disease in adolescent male soccer players: a prospective cohort study. Orthop J Sports Med. 2018;6(8):2325967118792192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Weinstein SL, Flynn JM. Lovell and Winter’s Pediatric Orthopaedics. 7th ed. Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 54. Wik EH, Martinez-Silvan D, Farooq A, Cardinale M, Johnson A, Bahr R. Skeletal maturation and growth rates are related to bone and growth plate injuries in adolescent athletics. Scand J Med Sci Sports. 2020;30(5):894–903. [DOI] [PubMed] [Google Scholar]
- 55. Witvrouw E, Danneels L, Asselman P, D’Have T, Cambier D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players: a prospective study. Am J Sports Med. 2003;31(1):41–46. [DOI] [PubMed] [Google Scholar]