Abstract
Introduction:
Drug sellers are often represented as morally bereft actors and as being, in part, responsible for North America’s overdose crisis. In Canada and the United States, drug sellers selling fentanyl and fentanyl-adulterated drugs have been charged with manslaughter when their clients fatally overdose, representing a retrenchment of drug war tactics. However, targeting drug sellers for drug checking interventions may have potential for reducing fentanyl-related harms. This study explores drug sellers’ negotiation of and engagement with drug checking technologies in Vancouver, Canada.
Methods:
Rapid ethnographic fieldwork was conducted from November 2018 to January 2019, including 26 semi-structured interviews with people who tested their drugs at an overdose prevention site to examine perceptions of the efficacy of drug checking. As drug sellers were also using the drug checking services, we specifically examined their perceptions of drug checking and the market aspects of the overdose crisis. Data were analyzed using Nvivo 12 and interpreted drawing on the concept of structural vulnerability.
Findings:
Drug sellers accessing drug checking services were concerned about the safety of their customers, and drug checking was one way of reducing the likelihood of harm. Drug sellers were embedded in the community, thereby, enmeshing practices of community care and ethics with the selling of drugs. When they had access to drug checking knowledge, sellers were able to modify risks related to the fentanyl market, including tailoring drugs sold to clients, returning dangerous batches and modifying fentanyl in order to make it safer to consume.
Conclusions:
Our findings reposition drug sellers as embedded within their communities and demonstrate their potential role in alleviating the dangers of the volatile fentanyl market. Policies that target people who sell drugs, particularly murder or manslaughter charges, are likely to make the crisis worse, and serious consideration should be put into harm reduction approaches with drug sellers.
INTRODUCTION
North America is experiencing an unprecedented overdose crisis that is now driven largely by the replacement of semi-synthetic opioids (i.e., heroin, and oxycodone) in the illegal drug supply with illicitly-manufactured synthetic opioids (i.e., fentanyl and its analogues, U-47770; Hedegaard, Minino and Warner 2017). Over the past several years, the drug market in the United States and Canada has seen fentanyl and heroin-fentanyl mixtures replace the traditional heroin market (Ciccarone 2017; Ciccarrone, Ondoscin and Mars 2017). Fentanyl is said to be approximately 40 times more potent than heroin (Ciccarone 2017), and fentanyl-heroin mixtures have varying degrees of potency. The variability and volatility of the drug market, have been exacerbated as new compounds with varying degrees of potency proliferate alongside each other (Ciccarrone, Ondoscin and Mars 2017). Between January 2016 and September 2018, approximately 10,000 people in Canada died of an opioid-related overdose, with 73% attributed to fentanyl and fentanyl analogues (Public Health Agency of Canada 2019). Meanwhile, 67.8% of the approximately 70,237 overdose deaths in the United States in 2017 were attributed to fentanyl (Scholl et al 2019).
In response to the overdose crisis, many jurisdictions in Canada and the United States have sought to implement harm reduction and addiction treatment interventions (Kilmer et al 2018), including take-home naloxone, overdose prevention sites (OPS) and opioid agonist therapy (Strike and Watson in press) to mitigate the harms associated with an unregulated and volatile drug supply. Socio-political dynamics (e.g., political opposition, drug laws) have limited the coverage of these interventions in jurisdictions in both countries and resulted in disparities in access (Kilmer et al 2018), particularly OPS (Kerr et al 2017), and communities continue to campaign for their implementation (Roth et al 2019). Amidst these ongoing efforts, drug checking is an emerging strategy that has garnered increased support as a tool to reduce the likelihood of drug-related harms associated with fentanyl and fentanyl analogues (Karamouzian et al 2018; Bardwell and Kerr 2018; Bardwell et al 2019a), and one that may be easier to implement than other harm reduction interventions (e.g., OPS). Drug checking technologies, specifically fentanyl testing strips (FTS), can be provided in some jurisdictions without violating drug laws (Goldman et al 2019), facilitating their expansion alongside political opposition to the expansion of other public health approaches to addressing adulteration within the drug supply (e.g., safer supply interventions) (Tyndall 2018).
Drug checking broadly refers to technologies or services where people who use drugs can test the contents of their drugs – for purity, adulterants, or for the presence of the desired drug depending on the technology (Harper, Powell and Pijl 2017). State-run drug checking has existed in some countries in Western Europe since the 1990s (Barratt et al 2018) but its introduction in North America is relatively new. Western European drug checking programs were created largely to address drugs used in nightlife and festival settings (Barratt et al 2018). However, the recent push to expand access to drug checking technologies in North America has been driven primarily to address people who use opioids, particularly, those who are either at risk of accidentally consuming fentanyl, or those who already do. The recent expansion of drug checking programs in the United States and Canada are part of a broader response to what researchers have termed the third wave of the opioid crisis (Ciccarone 2017). There are many options currently implemented internationally in terms of drug checking that can detect fentanyl and fentanyl analogues including but not limited to: Gas Chromatography Mass Spectroscopy, High-Performance Liquid Chromatography, Fourier-Transform Infrared Spectroscopy (FTIR) and fentanyl test strips (FTS; Barratt et al 2018; see Harper, Powell and Pijl 2017).
In relation to North America’s overdose crisis, drug checking programs first – and still most widely – have relied on the use of FTS. Earlier studies evaluating drug checking in Vancouver, Canada, have focused on the use of BTNX’s immunoassay FTS (Karamouzian et al 2018). FTS test for the presence of fentanyl and some fentanyl analogues, although they are limited in that they cannot differentiate between analogues or determine the percentage of fentanyl (Sherman et al 2018). Initially designed for urinary analysis of drugs (Amlani et al 2015), FTS for the purpose of drug checking primarily occurs using water and a small sample of the drug (Karamouzian et al 2018). Studies exploring prospective uptake of FTS in the past have found willingness to use FTS (Sherman et al 2019; Kennedy et al 2018), however, in research exploring the implementation of FTS at a supervised consumption facility in the Downtown Eastside uptake was relatively low (Karamouzian et al 2018). While there was initial enthusiasm with implementing FTS, the effectiveness of FTS is potentially limited by changes in the opioid market, particularly, when fentanyl has almost entirely replaced heroin (Willyard 2019; Pardo et al. 2019; BC Center for Disease Control 2018). In contrast to Vancouver, in Rhode Island, a setting where demand for fentanyl is low, researchers found a high willingness to use FTS and found that participants who received a positive fentanyl test were more likely to report changing behaviour before consumption (Krieger et al 2018).
While the focus on the utility of drug checking has been shaped by its efficacy as a harm reduction strategy for people who use drugs, drug sellers use of the technology has been largely overlooked. Whereas providing drug checking information to people who use drugs may allow them to return their drugs (Measham 2019), its impact could be increased were the people selling drugs to get their drugs tested before selling them. The positionality of drug sellers within the drug market make them an effective target for drug checking-related harm reduction interventions, as information for street-level drug contents could inform selling and communications strategies with buyers.
There are many different types of drug sellers, and their ability to access drug checking/harm reduction services and affect the drug supply is also likely different depending on their position in the drug market. Researchers often differentiate between ‘open’ and ‘closed’ markets (Mars et al 2015; Barnum et al 2017). Open markets refer to selling drugs visibly on the street, where people who use drugs must know the seller, and may take place in SROs (Kerr, Small and Wood 2005; Mars et al 2015). Further, there are also different typologies of drug sellers. Drug selling can include, “flipping” (Fast, Shoveller and Kerr 2017) or “middling” (Small et al 2013), where sellers obtain drugs for the purpose of reselling them to pay for their own use, small time drug selling, where individuals purchase drugs from a supplier to sell directly to people who use drugs, as well as sellers who may be higher up the distribution chain and sell in smaller quantities to other sellers and clients (what we refer to as mid-level sellers). As such, the distinction between drug seller and buyer is more fluid than conventional portrayals, even at different levels of the drug hierarchy (Boyd 2014).
A further complication is the stigma and possibility of incarceration, which may make it harder for drug sellers to access harm reduction services, such as drug checking. Drug sellers face specific challenges because they have been historically portrayed as exploiting people who use drugs (Boyd 2014; Carstairs 1999; Coomber 2006 23). With the increase in opioid-related overdose deaths, they have been implicated as responsible for the deaths of people who purchase their products (Peterson et al 2019; Dubinski 2019). Further, sellers have to operate in a market where trafficking of illegal substances can carry a high cost, such as imprisonment for life with a mandatory minimum sentence of one year (Controlled Drugs and Substances Act [CDSA] 1996, c19, 5), and stigmatization by society for their complicated role in selling opioids in a volatile drug market. The concept of structural vulnerability is further instructive in framing the risks incurred by drug sellers – here understood as how the position of groups and subgroups of people within social hierarchies on the basis of intersecting social and structural forces (e.g., stigma, racism, criminalization, etc.) produce vulnerability to harm (Rhodes et al 2012). For instance, the more visible nature of open markets means that they carry a greater risk of incarceration for seller and buyer in comparison to those working in closed markets (Barnum et al 2017).
Many of these issues and concerns coalesce in Vancouver, Canada, a city that has played a unique role in cultivating drug checking technologies in North America due to the large number of deaths occurring within the city (BC Coroner’s Report 2019) and its history of implementing novel harm reduction programs (Kerr 2019). Early detection of fentanyl began in Vancouver in 2015 using FTS, by testing urine samples of people using heroin (Amlani et al 2015). A pilot project was implemented in 2017 where the strips were used to test drug solution rather than urine (Karamouzian et al 2018) and was the sole form of drug checking up until the FTIR was introduced in 2017 (Tupper et al 2018). As of November 2017, the British Columbia Centre on Substance Use began drug checking using Bruker’s ATR-FT-IR (FTIR) in combination with FTS. The FTIR cannot detect substances below a 3-4% limit, hence the complementary use of FTS; like FTS it may can have trouble differentiating between analogues (Sherman et al 2018; McCrae, Tobias and Studen 2019). The FTIR can report approximate percentages for people using the service, although data on the effectiveness of the mixture analysis is limited (Tupper et al 2018). While the authors are unaware of any literature pertaining to implementation of FTIR drug checking in the United States, research by Glick et al (2019) found interest for drug checking implementation beyond FTS that was tempered by questions around implementation, as well as accuracy of results. Since its initial implementation, FTIR-based drug checking services have expanded, and now include several sites across British Columbia (BC Centre on Substance Use 2019). What makes Vancouver drug checking services different than others offered internationally (i.e. in The Netherlands) is that it has not attempted to preclude drug sellers from using drug checking (Smit-Rigter and van der Gouwe 2019).
While recent research has explored people who use drugs’ perceptions of sellers and drug checking (Bardwell et al 2019a), there is little research on drug sellers who use these services. In this article, we explore the discourses that drug sellers have about the drug market and how drug checking affects their understanding of the drugs they are selling and strategies they employ to reduce harm. Further, we explore how drug checking results play in to communication of the quality of drugs to clients, and how it works to modify the drug market.
METHODS
Rapid ethnographic fieldwork was undertaken between November 2018 and January 2019 to explore the experiences and perceptions of people who use drugs in relation to new drug-checking services implemented in Vancouver’s Downtown Eastside. Rapid ethnography is an approach that has proven particularly useful during public health emergencies. Whereas traditional ethnography relies on immersion within a community, often that one has no previous familiarity to, rapid ethnography uses a researcher’s familiarity with the context of the research site to produce specific insights about particular research questions (Johnson and Padros 2017). As drug checking in Vancouver continues to evolve and its efficacy in this context is unclear (Bardwell et al 2019a; Laing, Tupper and Fairbairn 2018), rapid ethnography was a valuable approach for quickly generating insights into its usefulness for people who use drugs to inform the wider overdose response.
Between November 2018 and January 2019, the lead and second authors (AB, JV) conducted approximately 50 hours of rapid ethnographic observation at an OPS in the Downtown Eastside. Participants were eligible for the study if they had used a drug checking service. All participants had used the drug checking service at the OPS where fieldwork was conducted and some had used at Insite or at another OPS in Vancouver. Participants were recruited from one OPS that offered FTIR drug checking in combination with test strips for fentanyl, benzodiazepines and LSD. We aimed to recruit a heterogeneous sample of people accessing drug-checking services. Semi-structured interviews were facilitated by the use of an interview guide. Some of this time was spent sitting in the drug checking “lobby” (a corner of the OPS partitioned off with a desk and chairs for those waiting to get their drugs check or for results). We spent time with both the drug checker and those waiting in the lobby. This allowed for informal conversations about motivations, use, interest and results and would take short notes which would later be extended into full field notes. We also often invited participants for an interview once they were done and also received referrals from peer workers at the OPS. Questions in the interview guide ranged from experiences with fentanyl, questions around overdose, and perspectives on the utility of drug checking, as well as areas where access to drug checking could be improved. Participants provided written and informed consent and received a $30 cash honoraria prior to beginning the interview. Interviews ranged from 15 to 45 minutes. Interviews were recorded and transcribed verbatim and participants were assigned a pseudonym to ensure anonymity. Ethical approval for the research project was obtained from the Providence Health Care / University of British Columbia Research Ethics Board.
Of the 26 semi-structured interviews conducted for this study, 14 reported having sold drugs in the last 30 days. The demographics of the larger study sample and the sub-sample of people selling drugs are reported in Table 1. Analysis of study data included both the larger sample and the sub-sample of participants, and aimed to explore the perspectives of drug sellers and the perceptions that people who did not sell drugs had about drug sellers who tested their substances. An initial coding scheme for the larger dataset were developed based on discussions among team members based on emerging observations (e.g., “Motivations for testing”, “instrumental use of results”, “trust in sellers”), as well as relevant topic areas from the interview guide. Data specifically from and related to sellers were coded using an iterative and inductive approach (Corbin and Strauss 2008).
Table 1:
Participant Demographics
| Drug Sellers n (%) | Full Sample n (%) | |
|---|---|---|
| N=14 | N=26 | |
| Age | ||
| Median | 38.5 | 40 |
| Range | 26-53 | 26-53 |
| Race | ||
| White | 8 (57) | 15 (58) |
| Indigenous | 5 (36) | 9 (35) |
| Other | 1 (7) | 2 (8) |
| Gender | ||
| Men | 8 (57) | 13 (50) |
| Women | 6 (43) | 13 (50) |
| Other Forms of Income in Last 30 Daysa | ||
| Binning | 3 (21) | 4 (15) |
| Full time | 1 (7) | 5 (19) |
| Part time | 4 (29) | 11 (42) |
| Panhandling | 3 (21) | 4 (15) |
| Sex work | 3 (21) | 4 (15) |
| Social assistance | 12 (86) | 19 (73) |
| Other | 4 (29) | 7 (27) |
Note. Demographics of participants who had used drug checking including subsample of participants who identified having made income selling drugs in the last 30 days.
Participants could report more than one source of income
The researchers recognize that in the act of constituting an account one is engaging in a representation (Tallbear 2009), as are the participants. In that sense the accounts are shaped by the conditions and history of research in the Downtown Eastside (Haraway 1988; Culhane 2011). Data were interpreted by drawing on the concept of structural vulnerability to situate their experiences in relation to overlapping social and structural oppressions that shape the lives of drug-using populations, including drug criminalization and poverty (Rhodes et al. 2012). Nvivo 12 was used to organize and code the data into themes and sub-themes.
FINDINGS
Situating the Risks of Selling Drugs
Within the context of a criminalized drug market, participants had to balance several competing risks, namely structural vulnerabilities. These structural vulnerabilities stemmed from the need to balance risks associated with drug law enforcement (i.e., arrest and incarceration) against the need to make money to support themselves and their drug use within in a wider social system that limits employment opportunities for PWUD (Boyd et al., 2018) and in a city that lacks affordable housing (York et al 2019). Intensive police presence, combined with widespread fentanyl adulteration within Vancouver’s drug market, can create extra risks for sellers in the Downtown Eastside (Collins et al 2019; Bardwell et al 2019a). Police presence near the OPS was noticeable during fieldwork and, in several instances, police were parked adjacent to the OPS. Participants engaged in perceived harm reduction tactics in an attempt to negate some of the risks of being a person that used and sold drugs within this context. ‘John’, for example, had had his heroin tested to make sure that it did not contain fentanyl:
When I first started with fentanyl, I didn’t want fentanyl in my heroin, so I went and I got the spectrometer to test. They said there was no fentanyl in it. I went out, I got arrested with the no-fentanyl heroin that I had, and they sent it to Health Canada and Health Canada said there was 00. – 0.10… like the smallest amount of fentanyl in it, and I already got it tested there. There was none. With this strip and everything, and there was no fentanyl in it. [35-year-old white man]
He later explained that he had been charged with a higher penalty than if he had just been carrying heroin. He expressed that, because of the overdose crisis, people selling drugs faced potentially harsher penalties such as manslaughter charges. Despite being unaware that he was carrying fentanyl at all, he believed that he had been perceived as ‘morally culpable’, viewed as part of the problem driving the overdose crisis.
Motivations for testing
Sellers as a source of harm reduction
Whereas sellers are often characterized as morally bereft actors preying on people who use drugs (Boyd 2014; Coomber 2006), sellers articulated how they attempted to mitigate the risks associated with a volatile drug market. Participants both used the drugs that they sold and brought them in for testing despite the potential legal ramifications associated with a police presence surrounding OPS sites – here prioritizing the need to maximize safety over their structural vulnerability to arrest. For those buying and selling small amounts of drugs or whose suppliers were inconsistent, drug-checking operated as a tool for avoiding “bunk” (i.e., drugs containing substances such as drywall with no fentanyl, drugs with undesired substances). As well as dealing with the risk of arrest, some participants worried about the impacts that their drug selling could have on friends and community members. Sellers accounts demonstrate that they were embedded within the Downtown Eastside community rather than being sellers who did not use their drugs or who were not members of this community.
Participants who sold drugs often requested the mixture analysis to determine the percentage of fentanyl contained in their samples. Sellers considered the percentages fairly reliable, and trusted the effectiveness of the technology (although some wished for more accuracy below the 5% limit due in part to the existence of carfentanil a highly potent fentanyl analogue). Determining the potency of fentanyl-adulterated drugs provided sellers with information that they could give customers as a harm reduction strategy:
Amber: People are wanting to know, like, you know what I mean? Like, how much fentanyl and it’s kind of better to say to someone, “Well, mine tested at this many percent,” right? … So then people know what they’re taking, and whether there’s more or less, right? …
Interviewer: Do you use the numbers that you get from here to let people know?
Amber: It’s good to be able to tell people. Because it can help you, or it can maybe not help you. [33 year-old white woman]
Participants noted a growing interest among customers for drug checking results. While customer interest may play a role in why people choose to disseminate information about their drug checking results, there were other reasons that drug sellers were interested in testing their drugs.
Participants expressed that they were motivated to keep their customers alive amidst day-to-day variations of fentanyl-adulteration within the illegal drug supply that could impact customers differently based on their opioid tolerance levels. Notably, overdose vulnerability is amplified by the intersection of structural conditions and experiences of opioid re-initiation and withdrawal (e.g., following release from prison, addiction treatment or hospital, when precarious drug use patterns are interrupted), leading to differences in opioid tolerance (Joudrey et al 2019). Participants reported that information on fentanyl content and potency obtained from the FTIR impacted what drugs they sold and to whom:
I was just curious on what the percentage of my dope was, just because I wanted to make sure when I’m selling it to somebody, that I’m selling them not only the right amount but I’m not selling to somebody who has a very low tolerance and might die, as opposed to somebody like myself, like who use a lot, a lot of drugs [Sam, 40 year-old, Indigenous, man]
Participants reported that knowing the potency of their product allowed them to tailor their drug-selling approaches so as to avoid accidentally killing customers, particularly those with heightened overdose vulnerability. Participants had lost friends and family and noted that the Downtown Eastside community had been negatively impacted by the number of fentanyl-related overdoses. Even amidst concerns about their role as sellers, participants expressed resignation surrounding an overdose crisis driven by adulterated drugs and awareness of the structural vulnerabilities produced by criminalization. One participant who sold small amounts of methamphetamine and was observed regularly attending the OPS noted that he did not sell fentanyl:
I couldn’t live with killing one of my friends, or anybody. Anybody’s kid. […] Anybody’s kid out there. Because a lot of us just don’t want to die. A lot of us just want to get out of our own heads for a couple hours, right? [Neil, 38 year-old, Indigenous, man]
Communication and Trust
In a market with a large number of drug sellers, having a consistent supply can be important for distinguishing oneself as a ‘good drug seller’ that people want to buy from and building trust in contrast to a ‘bad drug seller’, who sells low quality, or “bunk” drugs. Some participants noted that one of the ways trust is developed is through consuming their own products. ‘Sarah’, 33-year old white woman, explained how her own consumption played into establishing trust:
I wouldn’t… I just don’t ever sell dope that’s not that great, because I just… I’m not… I’m known for actually having decent… because people know that I won’t sell stuff that I don’t do
The results from the drug checking service are given to drug checking clients on a slip (see figure 1) of paper. The slips have the potential to be used by drug sellers to prove the contents of their drugs to potential buyers. ‘Nick’, a 43-year-old Indigenous man who used drugs but did not sell them, first pointed out to us that sellers may be using the slips to establish trust between them and their clients:
I first heard about [drug checking] on the street from people. People were talking about it, you can go test your drugs. Because [they] really respect the dealer that is going to go and check his drugs before he puts it out there. That shows a lot about somebody. […] It’s really important. Instead of everybody having to check it, the dealer just checks it, and you save a lot of problems right there. […] They take out their piece of paper and some people use it as a leverage also – kind of like, ‘my dope is stronger and safer… ’ and you can choose people that [way].
Figure 1:
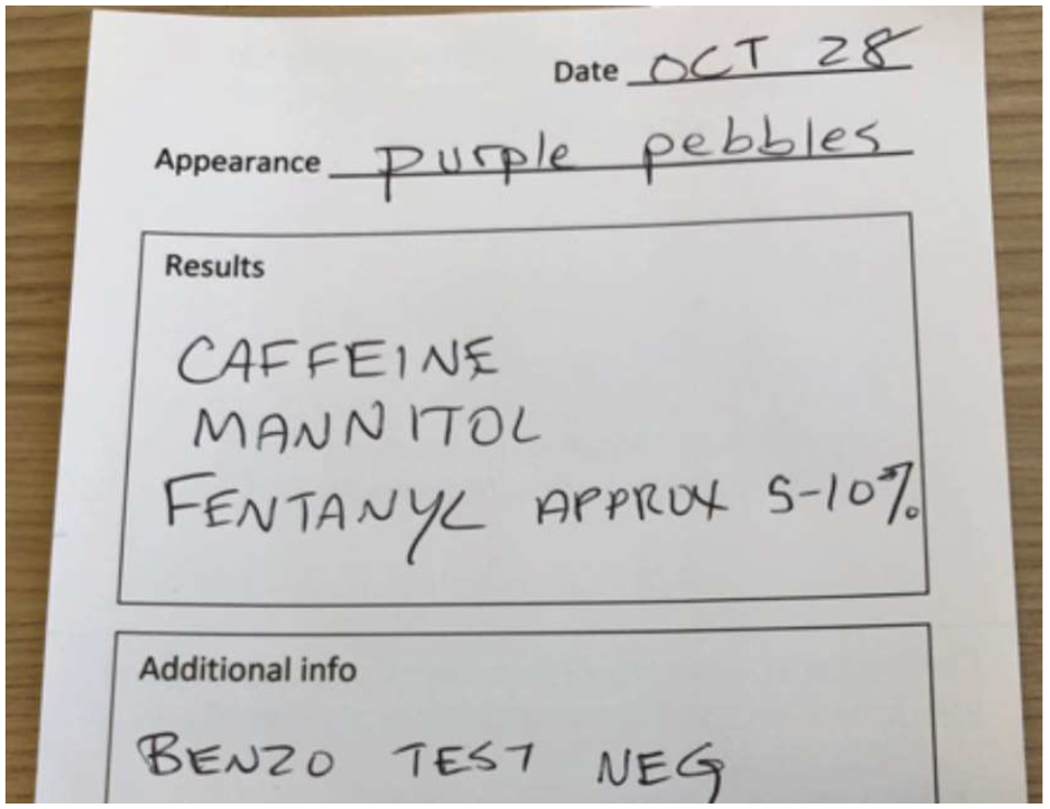
Example of drug checking results
Nick suggested that drug sellers were using the test results to demonstrate purity and a stable supply. Another participant who sold drugs referred to sellers that tested their drugs back when only FTS were available as sellers who “had ethics”. Rather than a primary tool for trust, however, drug checking slips were one tool among many used by sellers to establish and maintain trust.
Understanding and Interpreting Testing Results
Some participants reported wanting to test their drugs so that they could compare across different batches purchased from different suppliers. Whereas some drug sellers were looking for what they perceived to be middle-range fentanyl to sell (~15-20% fentanyl to mannitol/caffeine), others were looking for a consistently strong dose (~ >30%).There are many factors that affect optimal dose and as such, percentage may be the preferred way of obtaining information about the potency of one’s drugs (Bardwell et al 2019b). Drug checking acted as a way of informing future purchases, or for the purposes of identifying inferior or dangerous product (e.g., potent batches or batches adulterated with synthetic cannabinoids or benzodiazepines). As one seller noted:
I’ve gone through every dealer. I’ve always tried, I wanted the very best, so we know roughly that I’m the top two or three dealers that got the strongest fentanyl, just by trying, going through people’s stuff and then using that spectrometer too. [Sandra, 43 year-old white woman]
Drug checking results could be used to test across different batches of drugs, potentially acting as quality control in a volatile and unpredictable drug market.
While drug sellers sometimes directly relayed these percentages to potential customers, some translated those percentages into more easily interpretable language, such as “strong” (i.e., high level of fentanyl) or “weak” (low level of fentanyl). The onsite technician relayed that about 10-18% was the average strength of fentanyl found in Vancouver, and shared this information with participants to raise awareness of the expected strength of fentanyl locally. Participants did not seem to use the results from drug checking slips primarily for the purposes of marketing and instead relied on more traditional forms of trust to convey the quality of their product. Having a good reputation was considered a stronger determinant of quality than the piece of paper given to people who had their drugs tested. A few drug sellers noted that people trusted the quality of their drugs by their reputation – including their own standards of the drugs they themselves use and consistency of reported potency in their supply.
Modifying Markets
Participants used the drug checking as a form of quality control and as a tool to return undesired drugs. In two cases, participants reported modifying the potency of their fentanyl to make it sellable to consumers. Fentanyl modification possibly is a strategy for supplying drugs that meet consumer demands.
Returning Fentanyl – “It’s good business”
Participants varied in their capacity to return drugs, which was determined by their level within the distribution chain and level of trust with suppliers. Drug sellers that could return drugs framed the ability to return undesired drugs primarily as an example of good business practice. John bought approximately $2000 CAD of fentanyl at a time and referred to being able to return his drugs as how business was done. The drugs of concern that participants mentioned during fieldwork were benzodiazepines, dimethyltryptamine (DMT) and synthetic cannabinoids. One of the exemplar “bad” drug batches that was discussed during the fieldwork was “trippy dope” – that is, a batch that was said to contain DMT and was associated with hallucinations. When one of the participants was asked why he used drug checking, he noted he used it to make sure that the correct adulterants were in it as opposed to DMT. When asked what he would do were he to have gotten trippy dope, John said:
[I would have] Taken it back to my person where I get them from and got my money back. […] It’s fine, yeah. It’s proper business. I shouldn’t have a problem returning their product.
Others agreed that they could normally return a product if the product they were being sold was not what they expected. For example, ‘Nick’, a 40-year old Indigenous man, submitted drugs to be checked when we started the interview. Testing was taking longer that day, likely because a text alert had gone out through an emergency alert system (Real-time Drug Alert & Response text alert system operated by Vancouver Coastal Health and the British Columbia Centre for Disease Control; Vancouver Coastal Health 2019) warning of a batch of purple fentanyl alleged to be carfentanil. It was his first time testing his drugs, and the FTIR had been unable to find any fentanyl in his sample though FTS had. Nick at first expressed curiosity about testing his drugs, but his interest increased once his test results provided him with justification for returning his drugs:
Yes, [his supplier] would [take the drugs back], absolutely. I don’t see why not. I’d be like, ‘Look dude, you try it.’ Don’t want to spend my money on something that’s not even what it’s…It’s like going to a store to buy milk and you end up walking out with something else, you know what I mean? Like yogurt or something.
There were, however, two examples where participants could not return their drugs. In both cases, the participants did not sell drugs in large quantities, occupied low levels within dealing hierarchies, and it was unclear whether they were referring to drugs that they purchased primarily for personal consumption or for the purposes of selling. They referenced suppliers questioning their trustworthiness with the drugs they had purchased. For those where low levels of trust intersect with a low positionality within the market, dangerous drugs had to be disposed of, consumed, or presumably sold despite the risks.
Fentanyl Modification
Two drug sellers reported modifying fentanyl using mannitol (sugar) and caffeine based on drug checking results. One participant explicitly said that he was purchasing fentanyl in bulk, whereas the other participant noted that he would modify his fentanyl if its percentage was not in the range (15-20%) that his clients expected. A couple of other participants also reported that modification was beginning to occur with more frequency. As many participants noted, mannitol and caffeine have become the standard excipients for fentanyl in Vancouver – that is, working as fillers for an extremely potent substance in the same way that one might purchase tablets from a pharmaceutical company (although more crudely). John, who purchased 60-80% pure fentanyl and then used mannitol and caffeine to make the fentanyl less dangerous for consumers explained the process for mixing mannitol, fentanyl and caffeine together. Rather than being only concerned about making money, John expressed concern about his role within the overdose crisis.
In one instance, we saw a person being treated by medical staff when we arrived at the OPS. OPS staff told us that, the person had consumed a ‘light-green’ fentanyl and when the overdose occurred, it presented in such a way that it seemed like the person’s “heart looked like it would come out of their chest” (i.e., excessive heart palpitations). John, who had some of the light-green fentanyl offered to test his for the OPS staff, as the person overdosing had used all of theirs. When asked what would happen if he received a high-test result on his fentanyl, John explained that he would cut it to make it safer for street purchases:
John: You’re supposed to [cut it] because it’s too strong to put out as is.
Interviewer: Oh, okay. So, you do that to make sure that it’s like kind of…
John: It’s street level, yeah.
I: So, how much? Like, can you just give me an average – like, how much do you have to cut it down to make it like street level?
John: Eight to one. […] So, if I got one 8-ball of this stuff, I have to put eight more 8-balls with it of mannitol and caffeine.
I: So, you must be getting like super potent… basically like you’re just getting fentanyl?
John: 80 percent. It should be.
Participants mixing their own fentanyl cited mannitol as an effective excipient for hardening fentanyl, and John noted that it might provide for better mixing. Participants operate in an ambiguous space between the desire to make money and not kill their customers while also navigating the illegality of drugs and preparation processes under drug criminalization. As noted in the quote above, modifying the percentage of the fentanyl was about achieving an ideal strength that would both position one’s fentanyl as strong enough and yet strong enough to be dangerous. Another drug seller noted that, if he were to purchase a really weak batch of fentanyl, he would probably recut it to make it sellable on the market.
Some drug sellers sought to modify either overly potent batches of fentanyl or extremely weak batches for the purposes of being able to give clients a consistent strength of fentanyl rather than a variable one. Achieving a consistent strength served as a way of establishing a good reputation within an illicit market where the drug potency and contents are highly volatile. The modification and branding of fentanyl (by making fentanyl particular colours), however, might not be as consistent as they may expect. One seller, who pointed out that people were “mixing their own fentanyl,” noted that she had acquired two different batches of fentanyl that had tested differently on the FTIR:
Because this time, this batch that I have now, is not as strong as the other batch was, from the same people. I think they’re mixing their own dope. [Participant 5: 43 year-old white woman]
DISCUSSION
In summary, our findings demonstrate that drug sellers used information from drug checking to minimize the harms associated with fentanyl. Drug sellers sought ways to provide quality products, and drug checking was one tool among many that they used to tailor the strength of their fentanyl to reduce risk and maintain trust with their clients. While some drug sellers reported that they could return ‘bunk’ drugs to their suppliers, others operating on lower rungs of the drug selling hierarchy and who were already deemed less trustworthy lacked that capacity. Finally, some drug sellers used the drug checking service to test the quality of their supply, as well as to inform efforts to modify fentanyl (e.g., adding mannitol and caffeine) in an effort to make it safer for clients and reduce overdose risk.
Previous research has indicated that the inconsistencies in drug supply produce risk alongside the potency of individual drugs (Ciccarone et al 2017). Our findings indicate that drug sellers recognized the risks associated with the volatility of the illegal drug supply, and attempted to mitigate risks for clients even when such information could negatively affect their drug selling transactions. While previous literature has recognized this as a possibility, it has normally situated drug sellers using drug checking services as something to be avoided (Measham 2019). In examining drug sellers use of these technologies, our study supports calls by drug policy reformers and harm reductionists to include drug sellers as part of the solution to reducing harms from the fentanyl-driven overdose crisis (Blanchard 2019). One of the major barriers to including drug sellers within a harm reduction framework is the high-risk nature of drug sellers accessing OPS (Collins et a 2019; Bardwell et al 2019a). Drug sellers navigate structural vulnerabilities that include the potential of facing harsher penalties for selling fentanyl than other drugs, thereby increasing barriers to accessing harm reduction services (Dubinski 2019). It seems unlikely that higher penalties (e.g., manslaughter charges, longer jail sentences) are reasonable given considering the structural vulnerability that sellers face, nor will they be effective in removing fentanyl from the drug market (Peterson et al 2019; Beletsky 2018), especially given that drug selling is often one of the few income generating opportunities available to people who use drugs (Kerr et al 2008). Rather, to reduce the harms created by a volatile drug market in the absence of urgently needed measures to expand access to a regulated supply of drugs, public health should lower barriers to access including providing drug checking in settings where sellers can access them with less fear of arrest.
Sellers have frequently been portrayed as villains during the overdose crisis (Drug Policy Alliance 2019; CBC News 2017) and law enforcement officials in North America have increasingly prosecuted sellers with manslaughter and homicide charges (Dubinski 2019; Ramsay 2019). Our findings challenge these portrayals by demonstrating that drug sellers are diverse, with moral codes that shape selling practices and, among our participants, seek to reduce overdose risks even while balancing their structural vulnerability to arrest and incarceration (Palamer et al 2019; Bourgois 2003; Fast, Shoveller and Kerr 2017). Further, they extend recent research by Palamer et al. (2019), where drug sellers were found to act in a way that was driven both by market self-interest and through what the authors describe as altruism. Rather than situating drug sellers’ motivations within a complicated ethics of altruism, we argue for evaluating their motivations through a lens in which drug selling and harm reduction are embedded within a notion of community care (Race 2007) – that sees care as a practice actors do for themselves and their communities (relationality), while recognizing the barriers that affect/shape that care (Duff 2015). In a market where fentanyl has replaced heroin, sellers have few choices other than to sell fentanyl and yet were motivated to check the potency of their drugs and relay that information to clients. More research is needed to explore how drug sellers may implement harm reduction in the midst of an overdose crisis, where options for protecting their clients are limited by a volatile drug supply.
Within a rapidly evolving illicit drug market, establishing trust with one’s seller is paramount both for the client and the seller in order to remain competitive (Bardwell et al 2019a; Carrol et al 2017). Drug sellers must weigh making profit with keeping return customers (Mars et al 2015). Rather than being the primary tool for establishing trust, drug checking results were seen as one of many things used to initiate and maintain trust with their clients (e.g., personal consumption of one’s drugs, retaining drug-checking results) and rather seemed useful only once trust had been established. Sellers might share the direct results from drug checking, but also communicate percentages to clients through vaguer language such as “strong” or “weak”, suggesting that drug checking may be more of a useful heuristic for determining potency. This research builds on previous literature exploring drug selling, drug checking and trust (Bardwell et al 2019a), namely how drug checking could potentially work as a tool for trust with sellers and is likely situated within a broader regime of honesty and transparency.
In contrast to previous research in the US (Mars, Rosenblum and Ciccarone 2018), our findings suggest that a number of mid-level dealers in Vancouver might be modifying drugs containing fentanyl. Rather than typical narratives of adulteration – where sellers do so to increase profit (Morelato et al 2019), mannitol and caffeine were used as excipients. Equipped with information about the contents of their drugs, drug sellers could play an important harm reduction role in removing highly potent batches of fentanyl from the market, as well as other dangerous substances such as synthetic cannabinoids and benzodiazepines (Blanchard 2019). That fentanyl is being mixed at lower levels of the drug market, provides opportunities for harm reduction interventions that involve sellers in reducing harm. At minimum, better availability of drug checking services, particularly more advanced methods that provide more accurate information (e.g., High-Performance Liquid Chromatography), could be used for more effective drug checking, including the identification of new adulterants such as benzodiazepines (Kerr and Tupper 2017). In doing so, public health must reimagine the relationship between harm reduction and drug sellers to more directly affect the fentanyl drug market and be accompanied by reforms, including drug decriminalization, that maximize their effectiveness. However, while drug checking represents one way of lowering risk, it cannot replace more comprehensive programs, such the implementation of interventions providing access to a regulated supply of currently illicit drugs, that must be pursued to more fully address the current public health crisis (Tyndall 2018).
This study has several limitations. Participants were recruited from one OPS and therefore, our findings might not transfer to sellers who check their drugs in other settings or contexts. Sellers in our subsample might have been less concerned regarding potential arrest as they were already accessing the OPS and these spaces are perceived as safe (McNeil & Small, 2014), whereas sellers in other contexts might report policing as a barrier to accessing drug checking. Further, as is consistent with the wider literature (Bourgois 2002), social desirability might have influenced participant responses.
In conclusion, our findings suggest that some drug sellers play an important role in regulating the drug market in lieu of effective state regulation of drugs. Rather than the caricaturized villains portrayed in the media, sellers desired the capacity to keep their clients safe – drug checking was one such way that they did that even as the structural violence faced by drug sellers threatened to constrain their engagement with harm reduction. While drug sellers have not frequently been targeted for harm reduction interventions, as the overdose crisis continues to worsen, all options for reducing harm should be explored including providing services for drug sellers to reduce harm to the best of their ability. Stronger enforcement of drug laws at the expense of low and mid-level drug sellers who are attempting to mitigate harm to the best of their ability is counterintuitive to the goal of reducing overdose deaths. Unless safe supply is implemented, and the structural barriers that require one to sell drugs are addressed, drug checking can provide an effective harm reduction tool for addressing some of the dangers of a volatile drug market.
Acknowledgements
The authors would like to thank everyone who contributed their time, stories, and expertise to this research. This study was funded by the National Institute on Drug Abuse (R01DA044181). RM is supported by a Canadian Institute of Health Research New Investigator Award and a Michael Smith Foundation for Health Research Scholar Award. GB is supported by a CIHR fellowship award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflicts declared.
REFERENCES
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, & Buxton JA (2015). Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduction Journal, 12(1), 54. 10.1186/s12954-015-0088-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell G, Boyd J, Arredondo J, McNeil R, & Kerr T (2019a). Trusting the source: The potential role of drug dealers in reducing drug-related harms via drug checking. Drug and Alcohol Dependence, 198, 1–6. 10.1016/j.drugalcdep.2019.01.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell G, Boyd J, Tupper KW, & Kerr T (2019b). “We don’t got that kind of time, man. We’re trying to get high!”: Exploring potential use of drug checking technologies among structurally vulnerable people who use drugs. International Journal of Drug Policy, 71, 125–132. 10.1016/j.drugpo.2019.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell G, & Kerr T (2018). Drug checking: A potential solution to the opioid overdose epidemic? Substance Abuse Treatment, Prevention, and Policy, 73(1), 20. 10.1186/s13011-018-0156-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BC Centre on Substance Use. (2019). Drug Checking in British Columbia: January 2019. Retrieved from https://www.bccsu.ca/wp-content/uploads/2019/03/2019-01-BC-Drug-Checking-Report-Jan2019.pdf
- Barnum JD, Campbell WL, Trocchio S, Caplan JM, & Kennedy LW (2017). Examining the Environmental Characteristics of Drug Dealing Locations. Crime & Delinquency, 63(13), 1731–1756. 10.1177/0011128716649735 [DOI] [Google Scholar]
- Barratt MJ, Kowalski M, Maier LJ, & Ritter A (2018). Global review of drug checking services operating in 2017. Drug Policy Modelling Program Bulletin No. 24. Sydney, Australia: National Drug and Alcohol Research Centre, UNSW Sydney. [Google Scholar]
- BC Coroner’s Report. (2019). Fentanyl-Detected Illicit Drug Overdose Deaths January 1, 2012 to March 31, 2019. Retrieved from British Columbia Coroner’s Service; website: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/fentanyl-detected-overdose.pdf [Google Scholar]
- BC Centre for Disease Control. (2018). Knowledge Update: Findings from the 2018 B.C. Harm Reduction Client Survey. BC Centre for Disease Control. Retrieved from http://www.bccdc.ca/resource-gallery/Documents/Statistics%20and%20Research/Statistics%20and%20Reports/Overdose/20181221_BCCDC%20Knowledge%20Update_2018%20BC%20Harm%20Reduction%20Survey.pdf [Google Scholar]
- Beletsky L (2019). America’s Favorite Antidote: Drug-Induced Homicide in the Age of the Overdose Crisis. SSRN Electronic Journal, 10.2139/ssrn.3185180 [DOI] [Google Scholar]
- Bourgois P (2002). Anthropology and epidemiology on drugs: The challenges of cross-methodological and theoretical dialogue. International Journal of Drug Policy, 13(4), 259–269. 10.1016/S0955-3959(02)00115-9 [DOI] [Google Scholar]
- Bourgois PI (2003). In Search of Respect: Selling Crack in El Barrio (2nd ed). New York: Cambridge University Press. [Google Scholar]
- Boyd J, Richardson L, Anderson S, Kerr T, Small W, & McNeil R (2018). Transitions in income generation among marginalized people who use drugs: A qualitative study on recycling and vulnerability to violence. International Journal of Drug Policy, 59, 36–43. 10.1016/j.drugpo.2018.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd S (2014). The Criminal Addict: Canadian Radio Documentary Discourse, 1957–1969. Contemporary Drug Problems, 41(2), 201–232. 10.1177/009145091404100204 [DOI] [Google Scholar]
- Brunt T (2017). Drug checking as a harm reduction tool for recreational drug users: Opportunities and challenges. Retrieved from European Monitoring Centre for Drugs and Addiction website:http://www.emcdda.europa.eu/system/files/attachments/6339/EuropeanResponsesGuide2017_BackgroundPaper-Drug-checking-harm-reduction_0.pdf [Google Scholar]
- Carroll JJ, Marshall BDL, Rich JD, & Green TC (2017). Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. International Journal of Drug Policy, 46, 136–145. 10.1016/j.drugpo.2017.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstairs C (1999). Deporting “Ah Sin” to Save the White Race: Moral Panic, Racialization, and the Extension of Canadian Drug Laws in the 1920s. Canadian Bulletin of Medical History, 16( 1), 65–88. 10.3138/cbmh.16.1.65 [DOI] [PubMed] [Google Scholar]
- CBC News. (2017, January 27). Don’t trust drug dealers for quality control, police warn. CBC. Retrieved from https://www.cbc.ca/news/canada/saskatchewan/drug-dangers-fentanyl-1.3956266
- Controlled Drugs and Substances Act [CDSA]. SC 1996. c. 19. Retrieved from https://laws-lois.justice.gc.ca/PDF/C-38.8.pdf [Google Scholar]
- Ciccarone D (2017). Fentanyl in the US heroin supply: A rapidly changing risk environment. International Journal of Drug Policy, 46, 107–111. 10.1016/j.drugpo.2017.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Ondocsin J, & Mars SG (2017). Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin.’ International Journal of Drug Policy, 46, 146–155. 10.1016/j.drugpo.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins AB, Boyd J, Cooper HLF, & McNeil R (2019). The intersectional risk environment of people who use drugs. Social Science & Medicine, 234, 112384. 10.1016/j.socscimed.2019.112384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culhane D (2011). Stories and Plays: Ethnography, Performance and Ethical Engagements. Anthropologica, 53(2), 257–274. Retrieved May 28, 2020, from www.jstor.org/stable/41473878 [Google Scholar]
- Coomber R (2006). Pusher Myths: Re-situating the Drug Dealer. London: Free Association Books. [Google Scholar]
- Corbin JM & Strauss AL (2008). Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory (3rd ed). Los Angeles: Calif: Sage Publications, Inc. [Google Scholar]
- Drug Policy Alliance. (2019). Rethinking the ‘Drug Dealer.’” Rethinking the “Drug Dealer. Retrieved July 27, 2019, from http://www.drugpolicy.org/drugsellers [Google Scholar]
- Dubinski K (2019, May 3). Should fentanyl dealers be charged with manslaughter if their customers die? CBC. Retrieved from https://www.cbc.ca/news/canada/london/london-ontairo-fentanyl-should-dealers-be-charqed-with-manslauqhter-1.5120166
- Duff C (2015). Governing drug use otherwise: For an ethics of care. Journal of Sociology, 51( 1), 81–96. 10.1177/1440783314562502 [DOI] [Google Scholar]
- Fast D, Shoveller J, & Kerr T (2017). The material, moral, and affective worlds of dealing and crime among young men entrenched in an inner city drug scene. International Journal of Drug Policy, 44, 1–11. 10.1016/j.drugpo.2017.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick JL, Christensen T, Park JN, McKenzie M, Green TC, & Sherman SG (2019). Stakeholder perspectives on implementing fentanyl drug checking: Results from a multi-site study. Drug and Alcohol Dependence, 194, 527–532. 10.1016/j.drugalcdep.2018.10.017 [DOI] [PubMed] [Google Scholar]
- Harper L, Powell J, & Pijl EM (2017). An overview of forensic drug testing methods and their suitability for harm reduction point-of-care services. Harm Reduction Journal, 14(1), 52. 10.1186/s12954-017-0179-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief, no 329. Hyattsville, MD: National Center for Health Statistics. 2018. [Google Scholar]
- Johnson GA, & Vindrola-Padros C (2017). Rapid qualitative research methods during complex health emergencies: A systematic review of the literature. Social Science & Medicine, 189, 63–75. 10.1016/j.socscimed.2017.07.029 [DOI] [PubMed] [Google Scholar]
- Joudrey PJ, Khan MR, Wang EA, Scheidell JD, Edelman EJ, McInnes DK, & Fox AD (2019). A conceptual model for understanding post-release opioid-related overdose risk. Addiction Science & Clinical Practice, 14(1), 17. 10.1186/s13722-019-0145-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun JH, & Fairbairn N (2018). Integrating injectable opioid agonist treatment into a drug treatment court program: A case study. Substance Abuse, 39(4), 493–496. 10.1080/08897077.2018.1485129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamouzian M, Dohoo C, Forsting S, McNeil R, Kerr T, & Lysyshyn M (2018). Evaluation of a fentanyl drug checking service for clients of a supervised injection facility, Vancouver, Canada. Harm Reduction Journal, 15( 1), 46. 10.1186/s12954-018-0252-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy MC, Scheim A, Rachlis B, Mitra S, Bardwell G, Rourke S, & Kerr T (2018). Willingness to use drug checking within future supervised injection services among people who inject drugs in a mid-sized Canadian city. Drug and Alcohol Dependence, 185, 248–252. 10.1016/j.drugalcdep.2017.12.026 [DOI] [PubMed] [Google Scholar]
- Kerr T, &Tupper K (2017). Drug Checking as a Harm Reduction Intervention. Retrieved from BC Centre on Substance Use; https://www.bccsu.ca/wp-content/uploads/2017/12/Drug-Checking-Evidence-Review-Report.pdf. [Google Scholar]
- Kerr T, Mitra S, Kennedy MC, & McNeil R (2017). Supervised injection facilities in Canada: Past, present, and future. Harm Reduction Journal, 14(1), 28. 10.1186/s12954-017-0154-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer B, Taylor J, Caulkins JP, Mueller PA, Ober AJ, Pardo B, … Reuter, and P. (2018). Considering Heroin-Assisted Treatment and Supervised Drug Consumption Sites in the United States. Retrieved from https://www.rand.org/pubs/research_reports/RR2693.html.
- Krieger MS, Goedel WC, Buxton JA, Lysyshyn M, Bernstein E, Sherman SG, … Marshall BDL. (2018). Use of rapid fentanyl test strips among young adults who use drugs. International Journal of Drug Policy. 10.1016/j.drugpo.2018.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laing MK, Tupper ΚW, & Fairbairn N (2018). Drug checking as a potential strategic overdose response in the fentanyl era. International Journal of Drug Policy, 62, 59–66. 10.1016/j.drugpo.2018.10.001 [DOI] [PubMed] [Google Scholar]
- Mars SG, Fessel JN, Bourgois P, Montero F, Karandinos G, & Ciccarone D (2015). Heroin-related overdose: The unexplored influences of markets, marketing and source-types in the United States. Social Science & Medicine, 140, 44–53. 10.1016/j.socscimed.2015.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Rosenblum D, & Ciccarone D (2019). Illicit fentanyls in the opioid street market: Desired or imposed? Addiction, 114(5), 774–780. 10.1111/add.14474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae K, Tobias S, & Studen C (2019). Drug Checking: Operational Technician Manual. Retrieved from BC Centre on Substance Use; https://www.bccsu.ca/wp-content/uploads/2017/12/Drug-Checking-Evidence-Review-Report.pdf. [Google Scholar]
- McNeil R, & Small W (2014). ‘Safer environment interventions’: A qualitative synthesis of the experiences and perceptions of people who inject drugs. Social Science & Medicine, 106, 151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Measham FC (2019). Drug safety testing, disposals and dealing in an English field: Exploring the operational and behavioural outcomes of the UK’s first onsite ‘drug checking’ service. International Journal of Drug Policy, 67, 102–107. 10.1016/j.drugpo.2018.11.001 [DOI] [PubMed] [Google Scholar]
- Morelato M, Franscella D, Esseiva P, & Broséus J (2019). When does the cutting of cocaine and heroin occur? The first large-scale study based on the chemical analysis of cocaine and heroin seizures in Switzerland. International Journal of Drug Policy, 73, 7–15. 10.1016/j.drugpo.2019.07.025 [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Acosta P, Sutherland R, Shedlin MG, & Barratt MJ (2019). Adulterants and altruism: A qualitative investigation of “drug checkers” in North America. International Journal of Drug Policy, 74, 160–169. 10.1016/j.drugpo.2019.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardo B, Taylor J, Caulkins JP, Kilmer B, Reuter P, & Stein, and B. D (2019). The Future of Fentanyl and Other Synthetic Opioids. Retrieved from https://www.rand.org/pubs/research_reports/RR3117.html [Google Scholar]
- Peterson M, Rich J, Macmadu A, Truong AQ, Green TC, Beletsky L, … Brinkley-Rubinstein L (2019). “One guy goes to jail, two people are ready to take his spot”: Perspectives on drug-induced homicide laws among incarcerated individuals. International Journal of Drug Policy, 70, 47–53. 10.1016/j.drugpo.2019.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada. (2019). Updated Numbers on Opioid-Related Overdose Deaths in Canada. Retrieved, 2019(4). Retrieved from https://www.canada.ca/en/public-health/news/2019/04/updated-numbers-on-opioid-related-overdose-deaths-in-canada.html [Google Scholar]
- Ramsay C (2019, July 22). Man charged with manslaughter in fentanyl overdose death pleads guilty to lesser charge. Global News. Retrieved from https://globalnews.ca/news/5667146/edmonton-manslaughter-fentanyl-overdose-jordan-yarmey/ [Google Scholar]
- Race K (2008). The use of pleasure in harm reduction: Perspectives from the history of sexuality. International Journal of Drug Policy, 19(5), 417–423. 10.1016/j.drugpo.2007.08.008 [DOI] [PubMed] [Google Scholar]
- Rhodes T, Wagner K, Strathdee SA, Shannon K, Davidson P, & Bourgois P (2012). Structural violence and structural vulnerability within the risk environment: theoretical and methodological perspectives for a social epidemiology of HIV risk among injection drug users and sex workers. In Rethinking social epidemiology (pp. 205–230). Springer, Dordrecht. [Google Scholar]
- Rose ME (2018). Are Prescription Opioids Driving the Opioid Crisis? Assumptions vs Facts. Pain Medicine, 19(4), 793–807. 10.1093/pm/pnx048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth AM, Krai AH, Mitchell A, Mukherjee R, Davidson P, & Lankenau SE (2019). Overdose Prevention Site Acceptability among Residents and Businesses Surrounding a Proposed Site in Philadelphia, USA. Journal of Urban Health, 96(3), 341–352. 10.1007/s11524-019-00364-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, & Baldwin G (2018). Drug and Opioid-Involved Overdose Deaths—United States, 2013–2017. MMWR. Morbidity and Mortality Weekly Report, 67(5152). 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Park JN, Glick J, Christensen T, Morales K, & and Michelle McKenzie TCG (2018). FORECAST Study Summary Report. In John Hopkins Bloomberg School of Public Health. [Google Scholar]
- Sherman SG, Morales KB, Park JN, McKenzie M, Marshall BDL, & Green TC (2019). Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. International Journal of Drug Policy, 68, 46–53. 10.1016/j.drugpo.2019.03.003 [DOI] [PubMed] [Google Scholar]
- Small W, Maher L, Lawlor J, Wood E, Shannon K, & Kerr T (2013). Injection drug users’ involvement in drug dealing in the downtown eastside of Vancouver: Social organization and systemic violence. International Journal of Drug Policy, 24(5), 479–487. 10.1016/j.drugpo.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit-Rigter L, & van der Gouwe D (2019). The Drug Information Monitoring System (DIMS): Factsheet on Drug Checking in the Netherlands. Trimbos Instituut. Retrieved from https://www.trimbos.nl/docs/cd3e9e11-9555-4f8c-b851-1806dfb47fd7.pdf [Google Scholar]
- TallBear K (2013). Native American DNA: Tribal belonging and the false promise of genetic science. University of Minnesota Press. [Google Scholar]
- Tupper KW, McCrae K, Garber I, Lysyshyn M, & Wood E (2018). Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug and Alcohol Dependence, 190, 242–245. 10.1016/j.drugalcdep.2018.06.020 [DOI] [PubMed] [Google Scholar]
- Tyndall M (2018). An emergency response to the opioid overdose crisis in Canada: A regulated opioid distribution program. Canadian Medical Association Journal, 190(2), E35–E36. 10.1503/cmaj.171060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancouver Coastal Health. (2019). Overdose prevention & response. Vancouver Coastal Health. Retrieved 1 September 2019, from http://www.vch.ca/public-health/harm-reduction/overdose-prevention-response
- Willyard C (2019). Mitigating opioids’ harm. Nature, 573(7773), S17–S19. 10.1038/d41586-019-02689-z [DOI] [PubMed] [Google Scholar]
- York F, Chan K-M, Mugabo L, Taylor E (2019). Displaced: Rents and the Rate of Change in the Downtown Eastside. Carnegie Community Action Reports. http://www.carnegieaction.org/wp-content/uploads/2019/06/FINAL-190611_CCAP-SRO-Hotel-Report-2018-1.pdf [Google Scholar]


