Abstract
Introduction:
Persistent misconceptions of frailty and dementia in geriatric patients impact physician-patient communication and leave patients vulnerable to disempowerment. Physicians may inappropriately focus the discussion of treatment options to health care proxies instead of patients. Our study explores the consenting process in a decision-making capable orthogeriatric trauma patient population to determine if there is a relationship between increased patient age and surgical consent by health care proxy.
Methods:
Patients aged 65 and older who underwent operative orthopaedic fracture fixation between 1 of 2 Level 1 Trauma Centers were retrospectively reviewed. Decision-making capable status was defined as an absence of patient history of cognitive impairment and a negative patient pre-surgical Confusion Assessment Method (CAM) and Mini-Cog Assessment screen. Provider of surgical consent was the main outcome and was determined by signature on the consent form.
Results:
510 patients were included, and 276 (54.1%) patients were deemed capable of consent. In 27 (9.8%) of 276 decision-capable patients, physicians obtained consent from health care proxies. 20 of these 27 patients (74.1%) were 80 years of age or older. However, in patients aged 70 to 79, only 7 health care proxies provided consent. (p = 0.07). For every unit increase in age, the log odds of proxy consent increased by .0008 (p < 0.001). Age (p < 0.001), income level (p = 0.03), and physical presence of proxy at consult (p < 0.001) were factors associated with significantly increased utilization of health care proxy provided consent. Language other than English was a significant predictor of proxy-provided consent (p = 0.035). 48 (22%) decision-making incapable patients provided their own surgical consent.
Discussion:
The positive linear association between age and health care proxy provided consent in cognitively intact geriatric orthopaedic patients indicates that increased patient age impacts the consenting process. Increased physician vigilance and adoption of institutional consenting guidelines can reinforce appropriate respect of geriatric patients’ consenting capacity.
Keywords: hip fracture, geriatric, informed consent
Introduction
Patient autonomy in decision making is at the core of modern medical ethics and is foremost captured in the informed consent process.1 Clinicians are charged with ensuring their patients have a comprehensive understanding of treatment options and their right to decide which course is taken.2 This process requires physicians to assess a patient’s capacity to consent. The pervasive nature of cognitive impairment among older patients with fragility fractures renders the assessment of decision making capacity a necessity.3 Studies have reported prevalence of known dementia in adults over the age of 65 suffering from hip fractures at 28% with an additional 8% diagnosed upon presentation.3,4 Prevalence of cognitive impairment in geriatric orthopaedic trauma patients has also been recorded at 35.1%.5 Obtaining a formal assessment in elderly orthopaedic trauma patients not only identifies patients with cognitive impairment but also provides physicians with data to support and uphold patient autonomy.6 Without formal assessment, physicians have displayed an inconsistent ability to accurately judge a patient’s capacity to consent.7
Older patients are vulnerable to ageist assumptions of physical or cognitive impairment, assumptions that may compromise their right to autonomy.6 Persistent misconceptions of frailty and dementia in geriatric patients can gravely impact physician-patient communication and reinforce a paternalistic approach.8 Given that ageism, such as patronizing elderspeak, persists in physician-patient communication it is hypothesized that ageism may also be present during the consenting process.9
Considering the high rate of cognitive impairment in geriatric patients suffering orthopaedic trauma, we were interested in the surgical consenting process.3,5 The Level 1 Trauma centers studied have a 2-step cognitive assessment protocol beginning with a Confusion Assessment Method to rule out delirium followed by a Mini-Cog evaluation. These 2 examinations are validated screening tools for delirium and dementia, respectively.10,11 Negative screening for both Mini-Cog and CAM should reinforce to a physician that the patient retains decision-making capacity. In practice, however, physicians may not be consistently respecting geriatric patients’ autonomy to consent for surgical procedure. If without specific instruction from the patient, physicians may violate patient autonomy by directing the conversation regarding surgical options to the patients’ adult child at the bedside. Many studies have examined the process of informed consent in situations of cognitive impairment; however, none has investigated the specific question of improper consent procedures in decision-making capable geriatric orthopaedic trauma patients. We hypothesized that in a cohort of cognitively intact geriatric orthopaedic trauma patients ages 65 and older, increased age is associated with increased use of health care proxies during the surgical consent process.
Methods
A retrospective cohort study, approved by the institutional review board, was performed at 2 American College of Surgeons (ACS) Level-I trauma centers. The 2 institutions have an orthogeriatric fracture alliance to provide standardized care to all geriatric orthopedic trauma patients. A pilot study was initially conducted with a hypothesis that younger, decision-capable, geriatric patients (aged 65-79) would have higher rates of self-consent than older geriatric patients (aged 80+). This pilot study examined the surgical consent forms of 200 geriatric orthopaedic trauma patients undergoing hip fracture fixation. We witnessed proportions of non-patient consent in younger geriatric patients (aged 65-79) and older geriatric patients (80+) of 0.06 and 0.16, respectively. We utilized the health care proxy provided consent data from the pilot study to generate our sample size for this study. The power analysis design matched the pilot study design, a 2-group comparison between patients aged 65-79 and patients aged 80 and older, and yielded a total sample size of 188 patients. This sample size was calculated to meet a power of 80% and an alpha of 0.05, with a null hypothesis of no difference in the rate of health care proxy provided consent in decision-capable patients. However, as hip fractures in older patients are often fragility fractures, we assumed generalizing the study to all orthopaedic trauma patients 65+ would result in a lower cohort prevalence of fragility fractures.12 We then extrapolated further that considering the likelihood of a lower fragility fracture prevalence, the general orthopaedic trauma patient population aged 65+ would have higher rates of decision-making capable patients who provided consent for their operations. Therefore, we performed the power analysis with estimated cognitively intact non-patient consent proportions of 0.05 and 0.10 for younger (65-79) and older (80+) geriatric patients, respectively. The logistic regression power analysis yielded a sample size of 252 geriatric orthopaedic trauma patients per study arm (total N = 504). In totality; however, 510 geriatric patients undergoing traumatic orthopaedic fracture fixation were included in the study.
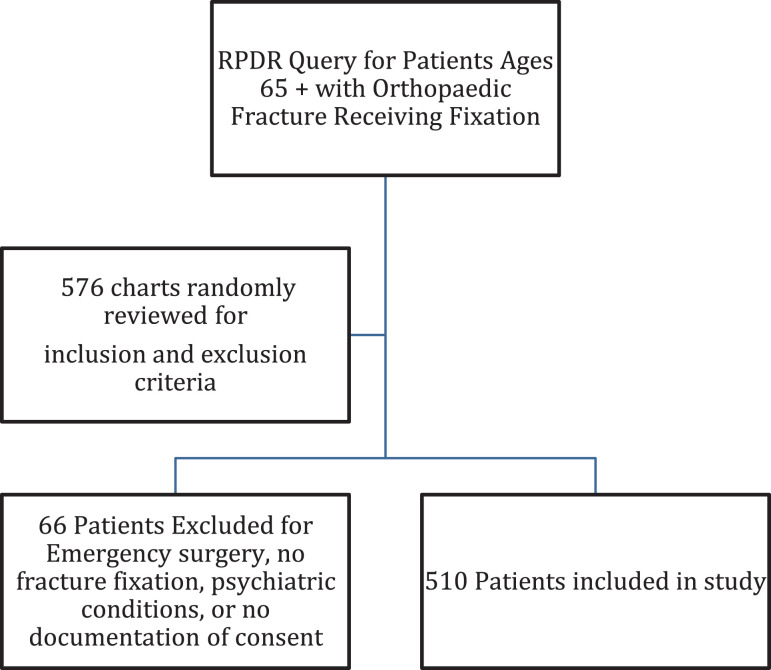
We identified potential cases using our institutions’ Research Patient Data Registry (RPDR), which can identify patients with specific demographics, diagnoses, laboratory tests, medications, molecular medicine, health history, microbiology, procedures, and providers. We used the RPDR Query Tool and queried for patients aged 65 years or older with CPT codes for fracture surgery at any time during the period from 2013 to 2016. From this query, we reviewed the patients’ detailed medical records to confirm whether patients were eligible (Figure 1). The primary outcome measured was party providing consent. This was determined by review of surgical consent form signatures for the appropriate hospital encounter. In situations where 2 signatures were obtained, both patient and health care proxy, we considered it patient self-consent. In cases of illegible signature e.g. upper-extremity trauma or circumstances where only verbal consent was obtained, we deemed patient self-consent. There was only one instance of an illegible signature due to injury and this patient provided consent. Additionally, there was one documentation of patient provided verbal consent for upper extremity injury but the patient had their health care proxy sign the consent form. This was considered a patient self-consent. If the consent form was not found in the patient’s chart, this was recorded. Patients who underwent emergent fixation and had an emergency waiver of consent were excluded from this study.
Figure 1.
Chart review methodology.
Decision making capacity at time of consent was determined through stepwise retrospective review of patient health records. Patients were considered cognitively intact if they screened negative for the Confusion Assessment Method (CAM) short form, Mini-Cog test, and had no previous diagnosis of cognitive impairment in their chart. The Confusion Assessment Method (CAM) has been validated by multiple studies to assess for delirium with an overall sensitivity of 94% and specificity of 89%.11 Previous research has found patients who are screened with the Mini Mental State Exam and score above 24, signaling normal cognition, have significantly lower likelihood of decision-making incapacity.13 While there is no research directly assessing the use of Mini-Cog as a surrogate marker for decision-making capacity, when Mini-Cog and MMSE were compared for identification of mild cognitive impairment, Mini Cog had a higher sensitivity and specificity than MMSE.14 Therefore, we utilized a negative Mini-Cog screen as a surrogate marker to help determine decision-making capacity in our cohorts. Patients with cognitive impairment have varying degrees of decision-making capacity.15 In cases of cognitive impairment, capacity can be fluid and is decision-specific. To simplify the study design, we established a criterion of no history of cognitive impairment in assessing for decision-making capacity. We acknowledge this limitation in design. Additionally, patients must not have any psychiatric condition that would affect decision-making capacity. Patients were excluded for schizophrenia and those who were declared section 12, or at the hospital against their will for psychiatric instability. This was a total of 3 patients. Traditionally, the delirium screening with the CAM is performed first and, if no delirium, the Mini-Cog (3 object-recall and clock-draw), is performed. Some patients had multiple Mini-Cog and CAM assessments performed during their stay due to the nature of our service’s co-management of patients with geriatrics. If cognitive assessments were completed by both the orthopaedic trauma service and the geriatrician prior to surgical consent and differed in their findings, we deferred to geriatrics. In circumstances where they differed pre and post-operation, the findings pre-fixation, and thus prior to consent being obtained, were recorded. Instances where no Mini-Cog or CAM were obtained were recorded, patients were considered unknown for decision-making capacity.
Other data collected included documentation of official health care proxy, physical presence of proxy, and whether there was a preferred decision maker documented. Health care proxy physically present was determined either by inclusion in initial consult note or health care proxy signature on consent form. We hypothesized that physical presence of a health care proxy might serve as a more convenient provider of consent to physicians. Moreover, preferred decision maker was a datapoint of importance as certain patients were cognitively intact but had documented preference of a proxy as their decision maker.
Additional factors of interest included income, education level, and mechanism of injury. Income was ascertained by utilizing census data for median household income based on patient zip-code. Mechanisms of injury were stratified into low and high energy mechanisms. Finally, patient demographic data such as sex, age, preferred language, race/ethnicity, fracture, and procedure type were analyzed. Chi-square or Fisher’s exact test was used to analyze categorical variables and t-test was used to analyze continuous variables. Linear regression was used to analyze decision making capable patients who weren’t consented against age.
Results
Between 2013 and 2016, 510 geriatric patients with orthopaedic trauma fractures were analyzed for provider of consent for surgical fixation. The mean patient age of the cohort was 83.4 years (range, 72 to 101 years) (Table 1). The most common fracture type was pelvis/lower extremity (79.2%) with 42 patients suffering from upper extremity fractures (8.2%). 426 patients (83.5%) had fragility fractures, or low-energy mechanisms such as falls from standing.16 Table 2 outlines the consent process, including a breakdown of cognitive impairment and delirium in the patient population.
Table 1.
Patient Demographics.
| All patients (n = 510) | |
|---|---|
| Age, Mean (range) yrs | 83.4 (72-101) |
| Sex | |
| Female (%) | 376 (73.7%) |
| Male (%) | 134 (26.3%) |
| Hospital | |
| Brigham and Women’s Hospital | 190 (37.3%) |
| Massachusetts General Hospital | 320 (62.7%) |
| Year of Presentation | |
| 2013 | 27 (5.3%) |
| 2014 | 111 (21.8%) |
| 2015 | 185 (36.3%) |
| 2016 | 187 (36.7%) |
| Race | |
| Asian | 8 (1.6%) |
| Black or African-American (%) | 19 (3.7%) |
| White (%) | 461 (90.4%) |
| Other | 9 (1.8%) |
| Not recorded/Refused (%) | 13 (2.5%) |
| Ethnicity | |
| Hispanic/Latino (%) | 11 (2.2%) |
| Non-Hispanic/Latino (%) | 351 (68.8%) |
| Unknown/Declined (%) | 148 (28.6%) |
| Language | |
| English | 486 (95.3%) |
| Non-English | 24 (4.7%) |
| Education | |
| Less than High School | 16 (3.1%) |
| Some High School | 19 (3.7%) |
| High School/GED | 161 (31.6%) |
| Some College | 18 (3.5%) |
| College degree | 113 (22.2%) |
| Graduate degree | 31 (6.1%) |
| Other/Unknown | 152 (29.8%) |
| Median Household Income; Mean (range) | $79,705 ($21,905-$191,744) |
| Mechanism of injury | |
| Fall from standing | 426 (83.5%) |
| Fall from height | 37 (7.3%) |
| MVC | 17 (3.3%) |
| Pedestrian struck | 11 (2.2%) |
| Other | 19 (3.7%) |
| Fracture type | |
| Pelvis/lower extremity | 404 (79.2%) |
| Upper extremity | 42 (8.2%) |
| Multiple fractures | 64 (12.5%) |
Table 2.
Patient Consent Process and Components Contributing to Decision-Making Status.
| Health Care Proxy Present at Consult | |
| Yes | 217 (42.5%) |
| No | 291 (57.1%) |
| Unknown | 2 (0.4%) |
| Documentation of Health Care Proxy in Chart | |
| Yes | 457 (89.6%) |
| Yes (no Health Care Proxy) | 7 (1.4%) |
| Not listed | 46 (9.0%) |
| Preferred Decision Maker listed in Chart | |
| Yes, patient | 112 (22.0%) |
| Yes, patient and proxy | 39 (7.6%) |
| Yes, other | 12 (2.4%) |
| No | 347 (68.0%) |
| Mini-Cog | |
| Positive | 112 (22.0%) |
| Negative | 242 (47.5%) |
| Deferred | 47 (9.2%) |
| Not documented | 109 (21.4%) |
| CAM | |
| Positive | 70 (13.7%) |
| Negative | 381 (74.5%) |
| Not documented | 59 (11.8%) |
| Dementia | |
| None | 313 (61.4%) |
| Dementia Present | 133 (26.1%) |
| Mild Dementia | 47 (9.2%) |
| Moderate Dementia | 10 (2.0%) |
| Severe Dementia | 7 (1.4%) |
| Consent by patient | |
| Yes | 275 (53.9%) |
| Yes and Proxy signed | 55 (10.8%) |
| No | 172 (33.7%) |
| Not in chart | 8 (1.6%) |
There was a significant difference in mean age of patients providing consent for their own surgeries, with mean ages of 86.9 years for health care proxy provided consent and 81.7 years for patient provided consent (p < 0.001) (Table 3). Higher income was also associated with physicians obtaining consent from patients for their own surgery (p = 0.059). Additionally, education level was associated with provider of consent with higher educated patients more likely to provide their own consent. (p = 0.003). Physicians were more likely to obtain consent from proxies in decision-making capable patients who had their proxies physically present (p < .001). Non-English speaking individuals in our cohort were less likely to provide their own surgical consent (p = 0.035). There was no significant difference among fracture type. (p = 0.094).
Table 3.
Demographics of Patients Stratified by Patient Versus Proxy Consent.
| Health care proxy consent (n = 172) | Patient consent (n = 330) | p-value | |
|---|---|---|---|
| Age (mean) | 86.9 | 81.7 | p < 0.001 |
| Median Income | $76,210 | $82,418 | p = 0.059 |
| Education | p = .003 | ||
| College/Graduate degree | 32 (18.6%) | 110 (33.3%) | |
| Some College | 5 (2.9%) | 12 (3.6%) | |
| High School/GED/Trade | 56 (32.6%) | 103 (31.2%) | |
| Some High School | 11 (6.4%) | 8 (2.4%) | |
| Less than High School | 8 (4.7%) | 8 (2.4%) | |
| Other/Unknown | 60 (34.9%) | 89 (27.0%) | |
| Health Care Proxy Present at Consult | p < 0.001 | ||
| No | 67 (39.0%) | 220 (66.7%) | |
| Yes | 105 (61.0%) | 110 (33.3%) | |
| Language | p = 0.035 | ||
| English | 159 (92.4%) | 319 (92.4%) | |
| Non-English | 13 (7.6%) | 11 (3.3%) | |
| Fracture type | p = 0.094 | ||
| Pelvis/lower extremity | 142 (82.6%) | 255 (75.3%) | |
| Upper extremity | 8 (5.3%) | 34 (10.9%) | |
| Multiple fractures | 22 (11/0%) | 41 (13.8%) |
Of the 510 patients included in the study, 276 (54.1%) were deemed capable of decision-making consent (Table 4). In total, consent was obtained from health care proxies in 27 patients (9.8%) who were of sound decision making capacity. Among the cohort of younger geriatric patients who were deemed decision-making capable, 7 (6.1%) had surgical consent forms signed by their health care proxies. Meanwhile, 20 (12.7%) of decision-making capable patients who were 80 years or older, had health care proxy surgical consent (p = 0.07) (Table 4). Although there was not a significant difference for provider of consent between the 65-79 years old and 80 years and older groups, for each year increase in patient age, the odds ratio of proxy consent increased by 1.00 (p < .001).
Table 4.
Provider of Consent Stratified by Consent Capacity.
| Patients’ Ability to Consent | |||
|---|---|---|---|
| Consent by patient | Capable of consent (n = 276) | Incapable of consent (n = 218) | |
| Yes | 227 (82.2%) | 48 (22.0%) | |
| Yes and Health Care Proxy signed | 18 (6.5%) | 34 (15.6%) | |
| No | 27 (9.8%) | 136 (62.4%) | |
| Not in chart | 4 (1.4%) | ||
| Patients Capable of Consent | |||
| Patient Consent (n = 245) | Proxy Consent (n = 27) | ||
| Age | |||
| 65 - 79 | 108 (44.1%) | 7 (25.9%) | p = 0.07 |
| 80+ | 137 (55.9%) | 20 (74.1%) | |
By our decision-making criteria, 48 (22%) of 218 patients deemed incapable of consent were the sole provider of consent for their surgical fixation. For each year increase in patient age, the odds ratio of proxy consent in the cohort of decision-incapable geriatric patients increased by 1.00 (p < 0.001). An additional 34 patients (15.6%) were decision-incapable but dually consented for surgery with their health care proxies. This group of patients who dually consented for surgery alongside their health care proxy was difficult to separate as to whether the patient provided assent with proxy consent or if consent was a obtained via a co-decision model. Additionally difficult to interpret was the group of 18 (6.5%) of decision making capable patients who were consented alongside their health care proxies. It was a challenge to distinguish patient assent from a co-decision model, but considering the lack of cognitive impairment, we considered these patients providers of consent. Only 4 patients (1.4%) did not have a consent form uploaded into their electronic health records.
Discussion
Increasing age is a known, non-modifiable risk factor for cognitive impairment that places older patients at risk for misconceptions of incapacity. An appropriate consent process engages patients and culminates with a signature to document the informed decision. Without question, patients who are cognitively intact and capable of making executive decisions should serve as provider of consent. It is concerning that decision making capable geriatric orthopaedic trauma patients are not always consented for their own surgical procedures. The association between age and health care proxy consent in this cohort indicates an age-impacted consenting process. It is not unreasonable that physicians may hesitate to consent patients in efforts to protect their safety; however, studies have shown poor reliability of unstructured physician assessment of capacity.7
Without formal tools, physicians have inconsistent accuracy in their assessment of patient decision-making capacity.7 There is an opportunity and a need for standardization of cognitive assessment in geriatric orthopaedic trauma patients. Studies have shown that providing clinicians with a specific set of questions to assess patient capacity increases accuracy in assigning decision-making capability.7 While our study’s systematic evaluation of decision-making capacity involved screening with the Mini-Cog and CAM, we observed that physicians still failed to consent these patients for surgery. The formal standard of assessing capacity includes the abilities to understand relevant information, appreciate the situation and consequences of a decision, and to communicate that decision.17 An argument can be made for a more robust capacity assessment, such as utilization of the Aid to Capacity Evaluation (ACE) tool, to ensure main competencies are assessed for decision-making capacity.18 Some research has shown; however, that a high Mini-Mental Status Examination (MMSE) score has a high sensitivity in detecting decision-making capable patients (96-100%).19 Our centers do not routinely employ MMSE in initial pre-surgical evaluation, but the Mini-Cog has demonstrated higher sensitivity and specificity than the MMSE in detecting mild cognitive impairment as a screening tool.14
Physical presence of a health care proxy at the time of orthopaedic consult was significant for use of health care proxy as provider of consent (p < .001). Potential factors that contribute to why physicians seek consent from health care proxies include ease of communication, proxy pressure, or patient preference. Sensory deficits, such as hearing or visual impairments, have the potential to augment insufficient physician-patient communication if physicians fail to devote additional time for their geriatric patients to adequately understand their options.8 Thus, physicians may view health care proxies as a time-saving option for consent in situations where patients have sensory deficits. Given the emotional and physical burden of a traumatic fracture, family members may attempt to relieve the patient of any additional onus—including difficult decision-making or paperwork. In a circumstance where a decision-making capable patient prefers that their proxy make care decisions, a health care proxy signed consent form is an exemplary following of the ethical principle of autonomy.
Special attention to patients with additional risk for marginalization, such as non-English speaking patients, is necessary to ensure that autonomy is not substituted with provider convenience.20 In our study, patients with lower socioeconomic status and education levels were less likely to provide surgical consent. Health literacy is an area of concern for older adults, with one study citing 22.7% of patients with normal cognitive function and 40.8% of patients with mild cognitive impairment having inadequate health literacy.21 Moreover, considering education is a predictor of health literacy, these findings of increased proxy-provided surgical consent correspond to patients with lower health literacy.22 While health literacy may impact capacity for some patients, it is critical that physicians serve as advocates for marginalized groups to ensure they retain agency in decision-making.
An equally concerning finding is the subset of decision-making incapable patients who provided consent for their surgical procedures. It is important to acknowledge that decision-making capacity is fluid and patients with cognitive impairment may retain varying levels of decision capacity.13 Patients who are identified to have cognitive impairment require further evaluation with specific assessment tools as previous research indicates an indeterminate zone between patients with mild cognitive impairment and their decision-making status.19 Moreover, there is high specificity for decision-making incapacity in patients with MMSE scores indicating moderate or severe cognitive impairment (MMSE < 17).19 Interestingly, however, the association between increased age and proxy consent in this sub-cohort of patients also indicates an age-impacted consenting process. We seek a balance between autonomy and protection of safety in the older adult when cognitive impairment impacts decision-making capacity.
A significant limitation in our study design was the established criteria assessing patients with cognitive impairment as incapable of consent. Certain patients in this cohort may have retained decision-making capacity. We also acknowledge the limitation that patients have different preferences in who makes health decisions. The principle of autonomy reflects the understanding that patients retain agency in how decisions around their care are made, including who makes them. Consent can be a nuanced process with many players involved. The goal of this study is to review the state of consent procedures involving our older patients to illuminate any discrepancy in their engagement in the process. We acknowledge that a signature fails to fully represent the process of consent. While our study design utilized the patient’s signature as the primary data point, the signature on a form may not accurately display the extent to which the signee was involved. The discrepancy between written consent and documentation of the robust process leading up to it is an issue that is out of the scope of this study. Though, this serves as a reminder that physicians should reconcile form signatures with their personal attestation of the process.
Furthermore, there were often situations where the signatures of both the patient and proxy were present on the consent form. Retrospective studies are inherently limited as the design requires data review in the absence of its full context. The presence of both signatures made us question the primary provider of consent; however, as mentioned previously, consent is a process that may involve many individuals. These patients may have preferred to make a joint decision with their proxies and the presence of both signatures represents this choice.
Finally, another limitation of our study was the lack of diversity in our patient population. Our population was majority female (73.7%). Moreover, 461 (90.4%) of our patients were white. A key point of analysis was consent in non-English speaking patients and only 24 (4.7%) of our patients were of limited English proficiency. Although we included all patients 65 and older in our query, our patient population ranged from 72 to 101. As we did observe an age-related increase in health care proxy provided consent, we do not think an analysis of patients between 65 and 71 years would have changed these findings. We expect that this younger cohort of patients would have a higher prevalence of patient provided consent, similar to what we witnessed in our study.
Preferential utilization of health care proxies to provide consent over decision-making capable older orthopaedic trauma patients occurred in 10% of patients. Risk factors associated with proxy provided consent include increased age, low socioeconomic status, level of education, limited English proficiency, and presence of health care proxy at time of consult. To aid in physician awareness of potential consenting biases such as age and frailty, as well as facilitate the balance between respect for patient autonomy and protection of patient safety, physicians should utilize standardized assessment and consenting protocols.
Footnotes
Author’s Note: Dr. Heng serves as a consultant for Zimmer-Biomet, Inc. No funds were received or utilized for the research reported in this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Madeline M. McGovern, BSc  https://orcid.org/0000-0001-7618-6073
https://orcid.org/0000-0001-7618-6073
References
- 1. Faden RR, Beauchamp TL. A History and Theory of Informed Consent. Oxford University Press; 1986. [PubMed] [Google Scholar]
- 2. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 5th ed. Oxford University Press; 2001. [Google Scholar]
- 3. Bernstein J, LeBrun D, MacCourt D, Ahn J. Presumed consent: licenses and limits inferred from the case of geriatric hip fractures. BMC Med Ethics. 2017;18(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daniels AH, Daiello LA, Lareau CR, et al. Preoperative cognitive impairment and psychological distress in hospitalized elderly hip fracture patients. AM J Orthop (Belle Mead NJ). 2014;43(7):E146–152. [PubMed] [Google Scholar]
- 5. Heng M, Eagen CE, Javedan H, Kodela J, Weaver MJ, Harris MB. Abnormal mini-cog is associated with higher risk of complications and delirium in geriatric patients with fracture. J Bone Joint Surg Am. 2016;98(9):742–750. [DOI] [PubMed] [Google Scholar]
- 6. Messer NG. Professional-patient relationships and informed consent. Postgrad Med J. 2004;80(943):277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840. [DOI] [PubMed] [Google Scholar]
- 8. Ouchida KM, Lachs MS. Not for doctors only: ageism in healthcare. Generations. 2015;39(3):46–57. [Google Scholar]
- 9. Williams KN, Herman R, Gajweski B, Wilson K. Elderspeak communication: impact on dementia care. Am J Alzheimers Dis Other Demen.2009;24(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451–1454. [DOI] [PubMed] [Google Scholar]
- 11. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method (CAM): a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tsuda T. Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature. Curr Orthop Pract. 2017;28(6):580–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427. doi:10.1001/jama.2011.1023 [DOI] [PubMed] [Google Scholar]
- 14. Li X, Dai J, Zhao S, Liu W, Li H. Comparison of the value of Mini-Cog and MMSE screening in the rapid identification of Chinese outpatients with mild cognitive impairment. Medicine (Baltimore). 2018;97(22):e10966. doi:10.1097/MD.0000000000010966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Okonkwo O, Griffith HR, Belue K, et al. Medical decision-making capacity in patients with mild cognitive impairment. Neurology. 2007;69(15):1528–1535. [DOI] [PubMed] [Google Scholar]
- 16. Ravindrarajah R, Hazra NC, Charlton J, et al. Incidence and mortality of fractures by frailty level over 80 years of age: cohort study using UK electronic health records. BMJ Open. 2018;8(1):e018836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment [published correction appears in N Engl J Med. 1989:16;320(11):748]. N Engl J Med. 1988;319(25):1635–1638. [DOI] [PubMed] [Google Scholar]
- 18. Etchells E, Darzins P, Silberfeld M, et al. Assessment of patient capacity to consent to treatment. J Gen Intern Med. 1999;14(1):27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gilbert T, Bosquet A, Thomas-Antérion C, Bonnefoy M, Le Saux O. Assessing capacity to consent for research in cognitively impaired older patients. Clin Interv Aging. 2017;12:1553–1563. Published 2017 Sep 26. doi:10.2147/CIA.S141905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel DN, Wakeam E, Genoff M, Mujawar I, Ashley SW, Diamond LC. Preoperative consent for patients with limited English proficiency. J Surg Res. 2016;200(2):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu YB, Chen YL, Xue HP, Hou P. Health literacy risk in older adults with and without mild cognitive impairment. Nurs Res. 2019;68(6):433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patel PJ, Joel S, Rovena G, et al. Testing the utility of the newest vital sign (NVS) health literacy assessment tool in older African-American patients. Patient Edu Couns. 2011;85(3):505–507. [DOI] [PubMed] [Google Scholar]