Abstract
Despite four decades of resilience research, resilience remains a poor fit for practice as a scientific construct. Using the literature, we explored the concepts attributed to the development of resilience, identifying those that mitigate symptoms of distress caused by adversity and facilitate coping in seven classes of illness: transplants, cancer, mental illness, episodic illness, chronic and painful illness, unexpected events, and illness within a dyadic relationship. We identified protective, compensatory, and challenge-related coping-concept strategies that healthcare workers and patients use during the adversity experience. Healthcare-worker assessment and selection of appropriate coping concepts enable the individual to control their distress, resulting in attainment of equanimity and the state of resilience, permitting the resilient individual to work toward recovery, recalibration, and readjustment. We inductively developed and linked these conceptual components into a dynamic framework, The Resilience Framework for Nursing and Healthcare, making it widely applicable for healthcare across a variety of patients.
Keywords: adversity, resilience, coping concepts, equanimity, recovery, caregivers, transplants, episodic illness, chronic illness, traumatic injury, cancer, mental illness, COVID “Long Haulers”, framework development
Submitting author:
Janice Morse
2151 E 900 S
Salt Lake City Ut 84108
Phone (801) 953 0285
Email: Janice.morse@gmail.com
Adversity, which has been studied through many lenses, is constant throughout life, but the recovery process following these adversities has received significantly less attention in social-sciences research. Resilience is the concept or construct that most frequently addresses this gap. However, the resilience construct has various adversities, mechanisms, and applications in multiple disciplines and cohorts. Here, we have developed a comprehensive framework to synthesize resilience and its application in healthcare: The Resilience Framework for Nursing and Healthcare.
Background Perspective/Theories of Resilience
While resilience is a scientific concept, there is no scientific agreement about its definition. Is it a state or a process? A concept or a construct? Does it originate from a specific adverse event, or is it a general response to adversity? How is the state or process of resilience defined? Is it achieved by “protective factors” available to the individual, or is the state of resilience an inner strength (“stealing it,” “taking it”), a process of adaptation, or a means of learning to reduce the effect of the stressor (Shin et al., 2012)? Resilience is a construct that includes a conglomerate of concepts. But which concepts enable the individual to adapt to or cope with the stressor? If the adversity should return or recur, does the individual return to or reenter the resiliency process? If resilience is indeed a process, as we propose, does it lead to adaptation once achieved? And if so, how can that state be defined? Analysis of the various definitions of resilience used by researchers reflects their perspectives on these questions.
Despite four decades of research, there has been no agreement on these fundamental questions. Resilience originates from the Latin “resilere,” which means to jump back (Kumpfer, 1999). Resilience first developed as a scientific concept in 1867 to describe how metals “bend back again” when placed under stress. (“Resilience,” OED, 2020). This general concept was then used repeatedly throughout many disciplines: theology, entomology, and physics (“Resilience,” OED, 2020). There was no consistent use of a definition or application, however, until approximately the 1980s when the term was adopted in psychology in relation to the study of childhood trauma. Yet even in this literature, there was a lack of agreement about its application as a concept (Olsson et al., 2003), construct (Tusaie & Dyer, 2004), model (Vinson, 2002), framework (Fleming & Ledogar, 2008), or theory (Brown, 2006; Richardson, 2002).
What explains this diversity of perspectives? The conceptualization of the construct differs from the disciplinary focus of the researchers, and this difference is directly associated with its clinical application or use (Markstrom et al., 2001). Our goal was to develop a framework—defined as “an entity between a ‘model’ and a ‘method’ . . . (that) contains an incompletely detailed structure or system for the realization of a defined goal.”1 Therefore, to explore the relevance of resilience to the care and management of disease and illness, we began by defining resilience via our extensive literature review and by identifying the associated concepts.
Description of Resilience in the Literature
Resilience as a state
Resilience is most frequently described as a construct that includes a cluster of concepts. Resilience as a state incorporates concepts of maintenance (Stewart & Yuen, 2011), equilibrium (Bonanno, 2004; Wagnild & Young, 1990), hardiness (Wilks et al., 2011), psychosocial well-being (Bekhet & Avery, 2017; Fletcher & Sarkar, 2013; Gillespie et al., 2007; ; Shaw et al., 2009), and equanimity (Wagnild, 2003). Resilience is seen as a positive and sustaining outcome, often allowing an individual to flourish despite their present life circumstances (Molina et al., 2014). Mancini and Bonanno (2009) further considered resilience as a particular trajectory or mechanism of positive adaptation that changes over time and protects against psychological distress.
Resilience as a process
Resilience as a process reiterates “the action or an act of rebounding or springing back; rebound, recoil” (“Resilience,” OED, 2020, Entry 163619). Securing internal and external resources to flexibly manage illness articulates this process of resilience (Haase et al., 2017). Competency (Greene et al., 2004; Haase et al., 2017; Masten, 1994), adaptation (Kimura et al., 2019), and positive adjustment during adversity outline actions taken during a changed life trajectory (Alizadeh et al., 2018; Black & Dorstyn, 2015).
Most authors agree, however, that resilience commences with adversity (Ungar, 2003). Some recognize that this adversity is an event (e g., acquiring a spinal cord injury, cancer diagnosis); others might consider it the result of a long-term stressor (e.g., mental-health issues or an abusive home environment). Longstanding risk factors include poverty (Garmezy, 1993), being shamed or bullied (Brown, 2006), homelessness (Rew & Horner, 2003), and post-traumatic stress disorder (Zarzaur et al., 2017), all of which are considered adversarial to the individual.
The conseptualization of resilience as strength-based
A strength-based conceptual consideration is inherent in reviewing resilience as both a state and a process. A strength-based perspective is a construct used by social work and psychology to identify internal, positive strengths that the client brings to a situation. These can include past experiences, talents, and skills and are vital components of the person’s ability to “bounce back” after a life-altering diagnosis. An illness, or a new diagnosis of illness in their loved one, poses a unique and uncharted challenge. A strength-based consideration weaves exclusive internal elements and physical deficits that the patient is experiencing, and this, in turn, sustains resilience (Greene et al., 2004). Bonanno et al. (2006) note the many unforged “pathways to resilience” (p. 20) that exemplify the strengths an individual possesses, and they identify practices that can accentuate this internal attribute.
Theoretical perspectives
The following authors have developed major research programs exploring resilience.
Bonanno (2004)
Bonanno’s contribution to the field is the recognition that resilience is the most common, natural reaction to loss or trauma, including post-traumatic stress disorder (Bonanno, 2004). He introduced a rigorous method of research applicable to both bereavement and trauma. Bonanno and his colleagues focused on what goes wrong with people who become chronically symptomatic with poor functioning after adversity while simultaneously seeking to learn which natural mechanisms allow people to cope with adversity (Southwick et al., 2014).
Rutter (2012)
Rutter viewed resilience through the lens of child development. As a child psychologist, his research examined the varied responses to stress experienced by children and the supporting role that the environment, genetics, family, and peers play to influence risk factors (Rutter, 1979, 2012; Rutter & Rutter, 1993). Resilience comprises internal and external supports that act as protective factors (Rutter, 2012). These polarize the effects of stress, accentuating positive responses, and mitigating negative ones as they relate to emotional and cognitive development in children (Rutter & Rutter, 1993).
Greene (2002)
From the field of social work, Greene offered an alternative perspective on resilience, namely, that it is a biopsychosocial and spiritual phenomenon involving a transactional dynamic process of person-environment exchanges. Greene proposed that resilience encompasses an adaptational process of goodness-of-fit and occurs across the life course with individuals, families, and communities experiencing unique paths of development.
Resilience in nursing and health
Stewart and Yuen (2011) explored resilience research and conducted a systematic review comparing psychological factors and coping strategies in adults with children with chronic illness. They concluded that resilience matched with symptoms associated with physical illness, demonstrating that pain is more prominent with a debilitating physical disease like arthritis (Stewart & Yuen, 2011). In their systematic review there was little mention of the role healthcare providers have in maintaining or regaining mental health in their patients who are experiencing adversity.
Many concepts shown to enhance resilience during the management of chronic illness or during the course of a disability have been incorporated independently into nursing theory. While resilience in itself is extremely relevant to nursing care and therapeutic outcomes, nursing has not embraced resilience per se. Some nurse researchers have explored resilience as a concept (Ahern et al., 2006; Olsson et al., 2003), but treating resilience as a concept does not enable the development of a caregiving and supportive framework that might enhance nursing.
One exception is the extensive research program by Haase and her colleagues, which explored resilience as a concept, developed an instrument to measure resilience (Haase et al., 1999), presented a mid-range theory (Haase & Peterson, 2015), and conducted subsequent quantitative testing (Haase et al., 2017). Haase’s research program targeted adolescents with cancer and explored concepts that enabled resilience, such as spirituality (Taylor et al., 2015), family communication and cohesion (Bell et al., 2007), social support (Bell et al., 2007), and information needs (Decker et al., 2004). The Adolescent Resilience Model (Haase, 2004) was developed to guide interventions for adolescents with cancer. From Haase’s work, a consensus statement (Nelson et al., 2004) and interventions were developed and applied using The Adolescent Resilience Model to improve care to adolescents with cancer and their families (Haase, 2004). Haase’s contribution to our understanding of resilience is extraordinary, but it is targeted exclusively to adolescent oncology. A less specific framework for the conceptualization and application of resilience for illness and utilization in nursing has yet to be proposed.
Conceptual Contributions of Interdisciplinary Research
Researchers have noted numerous and varied concepts that the individual uses to assist in achieving resilience. It should be a matter of concern that there is no overall agreement about the components of resilience. Through our literature review, however, we have identified the following concepts most commonly included in resilience theory: acceptance, communication, courage, determination, hardiness, hope, humor, knowledge, locus of control, mindfulness, optimism, perseverance, personal mastery, perspective, reassurance, resourcefulness, self-care, self-compassion, self-efficacy, self-reliance, social support, spirituality, and well-being.
Purpose of the Project
This general lack of agreement regarding what resilience is, and the level of conceptualization, components, mechanisms, and outcomes of resilience have left it “open” for further consideration and application to nursing and health. While researchers from psychology and sociology have examined resilience within topics that are pertinent to health, such applications are tangential to nursing—the profession of those charged with the primary responsibility for the provision of care for the ill.
Thus, the purpose of this project was to explore resilience from the disciplinary perspective of nursing by focusing on the individuals’, caregivers’, and families’ experiences of illness2 and, using modified method for developing theoretical-coalescence frameworks, to develop The Resilience Framework for Nursing and Healthcare.
Methods
We used a hypo-deductive process of theory-building resembling those techniques used in qualitative model- and theory-building. Rather than using raw data obtained from qualitative research (Bradshaw et al., 2017), we used a compendium of diverse literature to identify psychosocial problems associated with sets of illnesses, isolate related concepts, and build and link these to construct the framework.
This method of framework development is a means of creating a pragmatic conceptual infrastructure for higher-level (“parent”) concepts, and it is a basic operation of theory development in qualiaitve research, such as grounded theory and often in ethnography. It is a means of identifying and logically placing relevant concepts, both hierarchically and longitudinally, so that the parent concept becomes comprehensible, attainable, and useful.
This method of framework development is:
-
not concept development, most commonly constructed from data
(data → thematic/content analysis → identification of attributes → concept)
-
not meta-analysis of the label-smoothing type
(search for similar concepts/models/theories → search for commonalities → blend)
-
but is similar to Theoretical Coalescence
(a compilation of manifestations of a concept, derived from different contexts and conditions, netted together to create a stronger, higher-level “meta”-concept. This develops a complementary structure, both temporal and horizontal, thereby increasing the scope of the concept. [See the example of enduring, Morse, 2018].)
In this project, we are using a modification of theoretical coalescence to identify from the literature relevant psychosocial problems inherent in illnesses, and mature scientific concepts representing these problems. The psychological concepts will enable the development and attainment of resilience. We are creating a logical and “developmental” pragmatic structure that enables clinicians to support patients in accessing and attaining a resilience state. The framework will help researchers to explore and further develop this higher-level concept. Psychosocial theorists have created a large pool of independent and sometimes competing scientific concepts, but they have rarely explored their linkages, their complementary applications and their possible communal, complementary contributions to higher-level concepts in order to create frameworks, models and theory. Rather than exploring these concepts internally, one by one, we are using them as the internal structure to understand how resilience develops (through a process) and exists once it is achieved (as a state).
We selected a goal and a definition of primary concepts that fit the appropriate level of description [in this case the individual and related context (family, staff, setting)]. Using resilience as a search term, our search yielded 2,620,000 results in Google Scholar, and we approached the resilience systematically by conducting a series of targeted literature reviews, as classes of illnesses, concepts and other models/conceptualizations of resilience were required.
The first search was to identify the major research programs in resilience so as to identify the major definitions and scope. Once we had reviewed the major definitions of resilience and the perspectives of the major research programs, we then narrowed our search to explore the scope of resilience research programs in nursing, and the major definitions of resilience used in patient care. We identified illnesses and accidents most commonly encountered in nursing that resulted in a resilience response from the patients, using these as index cases.3 We identified the major characteristics of those illnesses and expanded our search4 to incorporate clusters of illness with similar characteristics, or similar patterns or stages of the illness trajectory (i.e., deteriorating or terminal illness, long-term illness, episodic illness, convalescence, mental illness), forming groups which we called “classes of illness.”
Our next aim in searching the qualitative nursing and health literatures was to identify descriptions of patients displaying resilience, or responses to each class of illness. By searching the qualitative literature, we were seeking inductive descriptions of the patients’ common psychosocial problems, thus identifying the coping concepts5 used for attaining resilience. By this means we determined that resilience was a process-oriented concept, and that resilience as an end result was attained by the individual through the use of both internal and external resources.6
Taking note that resilience was a process-oriented concept attained by the individual through both internal and external resources, we sorted these common psychosocial problems and related coping concepts functionally into protective, compensatory, and challenge-related concepts. The phrase “protective concepts” refers to those resources that ameliorate an adversity event; “compensatory concepts” refers to a person’s active countermeasures against an adversity event; and “challenge-related concepts” refers to the person’s coping efforts to moderate or overcome adversity events. We note that these concepts can be used individually, or as sets of related concepts, or even as mid-range theories. We recognize that, as resilience attainment varies with each of these classes of illness and stages of disease, as well as with internal abilities to become resilient (Rutter & Rutter, 1993), protective, compensatory and challenge-related factors can be incorporated as nursing interventions, and are individualized to each patient, with the nurse responding and adjusting these interventions according to the patient cues. Therefore, in practice, nurses are selecting from a “menu” of protective, compensatory, or challenge-related coping concepts according to patient-assessed needs and stages of illness, in concert with the patient. Finally, we searched the qualitative literature for outcomes—descriptions of the state that indicated the person had become resilient—and for behavioral indicators of equanimity. As some trajectories of illness included recurrence, we recognized that a subsequent episode incorporated experiential learning, which can ease and expedite resilience.
We then placed these descriptions into a table so that they could be compared and contrasted. We were able to identify coping concepts related to the psychosocial problems for each class of illness, grouping similar concepts (for instance, “family cohesion” was categorized under the category of “social support”). Similarly, allied concepts were classified under the parent concept (e.g., “faith” and “religiosity” were incorporated into “spirituality”).
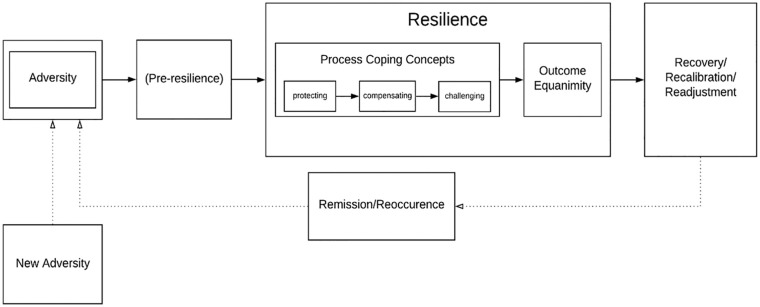
Thus, by identifying the commonalities within each class of illness and the concepts used by individuals to mitigate and cope with these psychosocial problems, we were able to reduce the number of coping-related concepts into those most frequently used and most consistently present throughout their respective illness trajectories. These concept clusters facilitated coping in the individuals’ responses to illness; distress was replaced with equanimity as they achieved resilience. This process is illustrated in Figure 1.
Figure 1.
Process of developing the resilience framework for nursing and healthcare.
Thus, from the literature, we developed a framework of resilience directly applicable to nursing, while considering the adversity experienced.
Results
From a nursing perspective, resilience is both a process that is built within the course of illness and also a state to be achieved. Once resilience is achieved, distress is no longer present, and equanimity enables optimal functioning in the individual (Emlet et al., 2011; Hutchinson, 1993; Janssen et al., 2011; Wagnild & Young, 1990). We conceptualize resilience as both a process that enables the individual’s recovery and as a state. Resilience enables the individual’s recalibration and adjustment to the ramifications of the physical and psychological changes from the illness or accident, thereby moving the individual toward optimal health and the prevention of recurrence. The findings related to each phase will be presented.
In this context, we propose the following definition of resilience: Resilience is a process and state that develops as a response to adversity, resulting in the individual’s dynamic and active use of coping strategies until a state of equanimity is reached. Dynamic and active use of protective, compensatory, and challenge-related concept strategies allows the individual to recover, recalibrate, and readjust so that they can become resilient, and ultimately attain health.7
Overview of the Process
We categorized coping concepts as protective, compensatory, and/or challenge-related (Fleming & Ledogar, 2008) in order to organize the various functions of the concepts of coping according to the trajectory of developing resilience, but we applied these at a different level. Rather than placing these concepts in the context of individual-and-community interaction, we used them to refer to individual-and-caregiving interaction. “Protective factors” (Garmezy, 1985; Rutter, 1979; Spratling & Weaver, 2012) are listed throughout the resilience literature and, in particular, have been adopted by family theories (see, Benzies & Mychasiuk, 2002). We considered this term too passive, however, to represent the necessary work required for attaining resilience in illness, even in the initial stages when the individual was adjusting to the adversity. Moreover, both compensatory and challenge-related concepts are also essential components as the individual is increasingly able to participate in therapy and progresses toward rehabilitation. Additionally, external resources (care providers, family, and support groups) directly link to personal resilience development in an individual, enhancing the work effort of resilience development. The first stage in the development of the framework (Step I) was to search the literature for conditons in which resilience was described as assisting the individual to cope with disease. This process resulted in the identification of our index cases. We then identified the main characteristics of each illness shared by common conditions of the index cases, and sorted them into broader classes of illness (Step II). Next, we identified from the literature the common psychosocial problems commonly associated with these conditions (Step III), and the frequently used coping-concept strategies associated with each class of illness (Step IV). As we identified appropriate concepts that mitigated these psychosocial problems, we sorted them according to the functions they performed in attaining resilience: to protect, compensate, and challenge (Step V). We identified equanimity as an indicator of the attainment of resilience (Step VI), resulting in the development of The Resilience Framework for Nursing and Healthcare (Step VII).
Step I. Identifying Primary Classes of Illness Applicable to Resilience Theory: The Index Case
The first level of analysis was to identify primary illnesses in which resilience was perceived to be significant, and to describe the experience of living with each illness from the perspective of the individuals’ emotional responses to illness. We referred to the conditions as the index case. The seven index cases (i.e., conditions) that were initially identified as requiring a resilience response from the individual were: (a) lung transplant; (b) breast cancer; (c) self-awareness of mental illness; (d) arthritis; (e) asthma; (f) major trauma; and (g) dependent relationships in persons with Alzheimer’s disease. Recognizing that living with these conditions had much in common with related illnesses or conditions, we then referred to these clusters as a class of illness. Each of these index cases and related conditions were seen to share the same characteristics, thereby forming a class of illness, as discussed below.
Step II. Identifying the Class of Related Illnesses for Each Index Case
The characteristics of each of these index cases included the suddenness and/or insidious nature of their onset; the trajectory of the illness; the prognosis and threat to self; the presence of pain; and the degree of disability present and applicable to resilience theory. These were identified so that the original index case represented a class of illness or groupings of allied conditions. For instance, caregivers of persons with Alzheimer’s disease represented a class of individuals responsible for the care of the dependent persons, and transplant survivors represented survivors of all transplant patients who were required to embody and live with a “new” organ. These classes of illness share common emotional responses (primarily the emotional distress of suffering), and these are referred to throughout this article as coping concepts. Our focus on concepts relating to individuals’ emotional experiences led to the exclusion of parallel concepts such as age, socioeconomic status, health systems, and environmental concepts that are also relevant to the attainment of resilience and commonly used to describe patient groupings.
Resilience as a response to surgical transplants
Class of illness: Major solid-organ transplants.
Index case: Patients who experience lung transplants.
Those who require lung transplants have experiences similar to those who undergo any major solid-organ transplant. They usually have a period of illness and physical decline prior to their transplant. The transplant itself is a major surgical event with a long period of recovery, continuous medication and medical surveillance; and it involves uncertainty of success. The waiting period prior to transplant includes significant loss, changes in role identity, attention to the medical system, and introspection (Brown et al., 2006). Continuous medical monitoring for signs of rejection or infection continue postoperatively.
We identified the index case of lung transplant as it includes coping concepts applicable to all solid-organ transplant survivors. Lung transplant recipients, for example, originate from several different processes varying from chronic obstructive pulmonary disease (COPD) to cystic fibrosis. Although improvements to survival increase each year, the peak quality of life post-transplant is noted around 12 months post-surgery (Rosenberger et al., 2012). Concepts enabling resilience concepts post-operatively protect against psychosocial problems of persistent fears of transplant rejection and despair associated with a return of hypoxia (Cohen, 2014; Rosenberger et al., 2012). Resilience enables toleration of activity restrictions, and challenges patients to adopt new stress-reduction techniques and to comply with complex treatment regimens (Barbour et al., 2006; Singer & Singer, 2013).
The patient who experiences living with a lung transplant has commonalties with other solid-organ transplant survivors, expanding this class of illness. Major transplant survivors use strategies represented by protective coping concepts of hopefulness (Molina et al., 2014), mastery and religiosity (Myaskovsky et al., 2006), optimism (Molina et al., 2014), regimental control (Rosenberger et al., 2012), and a pessimism-realism orientation (Brügger et al., 2014). Compensatory coping concepts in transplant survivors include those for the management of fear (Husain et al, 1999), inadequacy (Singer & Singer, 2013), uncertainty (Naef & Bournes, 2009), post-traumatic stress disorder (Cohen, 2014), stigma/guilt (Brügger et al., 2014; Rosenberger et al., 2012), and vulnerability (Husain et al, 1999).
Resilience as a response to living with cancer
Class of illness: Living with uncertain prognosis.
Index case: Breast cancer.
Breast cancer was initially identified as the index case, yet has many commonalities with the class of all cancers, albeit differing in prognosis, trajectory and outcome. The diagnosis of cancer is usually stressful, life-threatening (Morse et al., 2014) and followed by two broad trajectories. Both of these trajectories usually commence with treatment of the cancer, which might include surgery, chemotherapy, and radiation. The first trajectory is when the cancer is malignant and advanced and these treatments are of limited effectiveness, and the patient might decline, entering a time of increasing debility, and potentially palliative care and death. In the event of treatment, the second trajectory is predominantly one of uncertainty and hope over time. With respect to surgery and prolonged therapies, monitoring for possible recurrence and pacing through milestones—most commonly 5 years “cancer-free”—become significant markers. Should the monitoring reveal recurrence of the cancer, or should the cancer metastasize to other sites in the body, the trajectory might move to increasing debility, palliative care and death.
Regardless of the course of the disease, the initial diagnosis causes emotional distress (Breen et al., 2009; Harrison & Maguir, 1994; Morse, 2011; Weisman, 1979). Protective concepts enter at this stage. Self-compassion and social support play an important role during the diagnosis and treatment for the attainment of resilience. The ability of an individual to adjust through both physical and emotional adversity requires the extensive use of strategies represented by compensatory coping concepts, which contribute to building resilience, including hope, motivation (de Moor et al., 2006), optimism (Gardenhire et al., 2019), a sense of coherence (Boscaglia & Clarke, 2007), preexisting and perceived social support, spirituality (Herth, 1992; Lo et al., 2010; Snyder et al., 1991), self-compassion, and a sense of belonging. Challenge-related concepts include knowledge, quality of life, and positive adjustment (Aspinwall & MacNamara, 2005). If the cancer patients are able to cope and develop resilience, they might be less dependent on psychosocial support for the management of their stressful conditions relative to those with low resilience (Brix et al., 2008).
Resilience as response to living with mental illness
Class of illness: Self-awareness of mental illness.
Index case: Anxiety.
Of those mental illnesses of which the persons themselves are aware, a defining feature is the psychological distress that those affected will suffer as a direct result of these illnesses. The specific identification of generalized anxiety disorder (GAD), major depressive disorder (MDD), and post-traumatic stress discorder (PTSD) was derived from the broader category of psychiatric illnesses with self-awareness. Becoming resilient has been noted to act potentially as a buffer that helps to reduce the prevalence of these mental-health conditions (Sheerin et al., 2017; Thompson et al., 2018a).
These diseases are often highly visible to the affected individual and to others, and have the potential to cause devastation to physical health, social, and family relationships, employment, and other critical aspects of life. Shame and stigma can inhibit the individual’s ability to seek care. Common problems encountered in this group are anxiety, behavior disengagement, denial, depression, fatigue, fear, guilt, shame, isolation, numbing, self-blame, stigma, stress, substance use, suicidality, venting, and vulnerability (Mong et al., 2012; Neria et al., 2010; Thompson et al., 2018a; Villaggi et al, 2015). This emotional upheaval serves as a powerful barrier or means to self-protect (or protect), by using self-managing concepts that lead to successful coping (Villaggi et al., 2015). Concepts that have been identified as frequently supporting resilience by compensation include acceptance, hope, humor, self-efficacy, social support, spiritual belief, and physical exercise. Planning, purpose, positive reframing, and mindfulness, (Min et al., 2013; Mong et al., 2012; Thompson et al., 2018a) can be considered challenge-related concepts. One who copes well following adversity or stressors is generally termed resilient in the mental-health community (Sheerin et al., 2017). Yet this prompts the questions, why do some individuals seem to possess more resilience, and how can those deemed to have poor resilience and coping ability develop these skills to aid in recovery and prevent recurrence? Harnessing resilience-focused concepts enable individuals with mental-health disorders to adapt successfully to equanimity and buffer against future hardship.
Resilience as a response to living with chronic pain
Class of illness: Ongoing chronic painful conditions.
Index case: Arthritis.
Arthritis is a chronic painful condition which shares common characteristics with osteoarthritis and rheumatoid arthritis, as well as back pain and fibromyalgia. These ongoing chronic painful conditions are a class of conditions that create unique challenges to those affected. While chronic pain conditions do not present a direct threat to life, they can affect ability, mental outlook, job performance, and mobility for the remainder of the afflicted person’s life (King et al., 2003; Tokish et al., 2017). Osteoarthritis and rheumatoid arthritis present clinically with joint swelling, pain, and immobility (Beeckman et al., 2019; Mangelli et al., 2002). Specific concerns about these chronic painful conditions relating to mobility include preclusion from event attendance, physical vulnerability, and isolation (Beeckman et al., 2019; Liu et al., 2017; Shaw et al., 2019). People living with arthritis also bear worries about future immobility limitations that might require the use of canes, walkers and wheelchairs.
Resilience concepts help improve the pain and procedural outcomes for chronic painful conditions (Hemington et al., 2018; Thompson et al., 2018b; Tokish et al., 2017), and improve adaptability to life changes with arthritis (Hemington et al., 2018). These changes require active “work” throughout the process of seeking resilience. The following concepts have been linked to working toward resilience: acceptance (Shaw et al., 2019), autonomy (Becker & Newson, 2005; Cartwright et al., 2015; Hassani et al., 2017; Mangelli et al., 2002), hope (Xu et al., 2017), optimism (Shaw et al., 2019; Thompson et al., 2018b; Xu et al., 2017), patience (Hassani et al., 2017), perseverance (Shaw et al., 2019), sense of purpose (Hassani et al., 2017; King et al., 2003; Liu et al., 2017; Mangelli et al., 2002; Rojas et al., 2018), self-efficacy (Xu et al., 2017), self-growth (Cartwright et al., 2015; Mangelli et al., 2002), social support (Cartwright et al., 2015; Hassani et al., 2017; King et al., 2003; Mangelli et al., 2002; Musich et al., 2019; Robinson et al., 2019; Shaw et al., 2019; Xu et al., 2017), and well-being (Beeckman et al., 2019; Hassani et al., 2017; Mangelli et al., 2002). Chronic pain researchers also identified these coping concepts as contributors to a resilience outcome (Cartwright et al., 2015; Hassani et al., 2017; Hemington et al., 2018; Rojas et al., 2018; Shaw et al., 2019).
Resilience as a response to incurable episodic illness
Class of illness: Episodic illnesses.
Index case: Asthma.
A class of illnesses that occur as episodes, or repeated “attacks,” such as asthma, provides the person and their family or support system with the opportunity to recognize the onset of the occurrence of the disease and to learn emergency responses in order to intervene, control and even prevent more serious and debilitating consequences of the disease—that is, to learn to become resilient over time. Episodic illness in this category includes such conditions as asthma, migraine, and sickle-cell disease.
For example, asthma is a disease of airways currently without a cure and can only be managed (Asthma Society of Canada, 2020). The condition will not only compromise physical well-being, but will also associate with a range of psychological consequences. Common symptoms like shortness of breath, regular coughing, wheezing, trouble sleeping, and limited physical activities inhibit the patient from leading a “normal” life. In addition to the symptoms, the patient might feel abused, depressed, afraid, lonely, mentally fatigued, shamed, stressed, vulnerable, and inadequate (Barton et al., 2003; Coogan et al., 2013; Lehrer et al., 2002; Metting et al., 2016). In the US, over 24 million people are suffering and coping with this incurable illness (CDC, 2018). Management of symptoms might be the only way for this population to lead a normal life.
For incurable episodic illnesses (i.e., sickle-cell disease, asthma, migraine), therefore, the focus is on control, management, and readjustment after every episode of the syndrome (Bromberg et al., 2012; Vinson, 2002; Williams-Gray & Senreich, 2015). Additionally, over time, such patients might improve their management skills by achieving equanimity. Therefore, concepts of coping are the key to boosting resilience in episodic illnesses. Frequently used protective coping-concept strategies are family cohesion (Fuggle et al., 1996; Koinis Mitchell et al., 2004), hope (Simon et al., 2009; Vinson, 2002; Ziadni et al., 2011), humor (Williams-Gray & Senreich, 2015), knowledge (Fuggle et al., 1996), mutual aid (Ladd et al., 2014), social support (Chen et al., 2011; Montoya et al., 2004; Vinson, 2002), and spiritual belief (Williams-Gray & Senreich, 2015). Frequently used compensatory-concept strategies are empowerment (Vinson, 2002; Williams-Gray & Senreich, 2015), management (Bromberg et al., 2012; Fuggle et al., 1996), and optimism (Chen et al., 2011; Vinson, 2002). Finally, frequently used challenge-concept strategies are empowerment (Vinson, 2002; Williams-Gray & Senreich, 2015), normalization (Protudjer et al., 2009), and self-esteem (Chen et al., 2011; Vinson, 2002). These coping-concept strategies guide patients with episodic illnesses to recalibrate and readjust, thus improving their ability to be resilient.
Resilience as a response to trauma
Class of illness: Unexpected and unanticipated accidents or trauma.
Index case: Spinal-cord injury.
An adverse traumatic event that results in injury is the index case in this class. These injuries can have catastrophic effects on the injured and those close to them. Examples in this category include injuries from major unexpected or unanticipated events, resulting in a major traumatic injury, such as war injuries or motor-vehicle accidents which require extensive intervention.
Consider, for instance, our index case—a major accident resulting in a spinal-cord injury that upends a person’s life, creating a new state of dependence during performance of activities of daily living and causing chronic pain, anxiety, social stressors, and prolonged rehabilitation (Craig et al., 2014, Guest et al., 2015). Distress, depression and altered functioning are frequent outcomes; and the inability to accept the current status makes it difficult to progress toward rehabilitation and overall improved wellness (Bonanno et al., 2012).
Over time, those who consider injury a challenge to be overcome and who use coping skills—both inherent and learned—have a higher likelihood of recovery (Bonanno et al., 2012; Kornhaber et al., 2018; Machida et al., 2013). It has been shown that exhibiting resilience is predictive of psychological, physiological, and sociological wellness among those with a sudden injury or accident such as a spinal-cord injury (McDonald et al., 2019). Some of these learned behaviors include mood management, not just physical recovery (Kilic et al., 2013). One of the most pertinent compensatory coping-concept strategies for those with a sudden illness or injury is optimism (Edward, 2013; McDonald et al., 2019; Stewart & Yuen, 2011; Wagnild, 2003).
Strong social support encompasses protective, compensatory, and challenge-related coping-concept strategies (Ahern et al., 2006; Bhattarai et al., 2018; Edward, 2013; Machida et al., 2013; Monden et al., 2014; Shin et al., 2012; Spratling & Weaver, 2012). The ability to adapt to injury and resultant changes (Ahern et al., 2006; Bhattarai et al., 2018; Edward, 2013; Hunter & Chandler, 1999; Jones et al., 2019; Kornhaber et al., 2018; Machida et al, 2013; McDonald et al., 2019; Monden et al., 2014; Spratling & Weaver, 2012), and the act of serving as a role model or inspiring others (Monden et al., 2014), are key challenge-related coping-concepts strategies. Salient protective coping-concept strategies include spirituality (Bhattarai et al., 2018; Jones et al., 2019; Monden et al., 2014); psychological strength (Monden et al., 2014; Tusaie & Dyer, 2004); and perspective (Garmezy, 1993; Monden et al., 2014). Once obtained, resilience enables the individual to thrive despite the injury (Shin et al., 2012).
Resilience as a response to dyadic dependency
Class of illlness: Caregiving for the frail and ill.
Index case: Caregiving for a person with Alzheimer’s disease.
Caregivers as a group have been selected and included as a class because these individuals, and those they care for, must be considered as a unit, and their dyadic responsibilities to the frail and ill, are important to health and resilience. Additionally, health implications and resulting sequelae (including stress responses) are directly related to caregiving responsibilities for the caregivers themselves.
Informal caregivers, representing nearly 30% of the adult American population, provide essential assistance with activities of daily living and medical care (Hudson et al., 2020). Caregivers help to facilitate resilience in those they care for by buffering the adversity and stress experienced by the ill person; in this way, such caregiving acts as a protective factor.
Studies, however, have documented physical and mental consequences of caregiver burden, including depression, anxiety, social isolation, loneliness, difficulty balancing professional and personal responsibilities, increased occurrence of chronic conditions (Aoun et al., 2018; Brodaty & Donkin, 2009; Deist & Greeff, 2017), difficulty accessing support resources, compassion fatigue (Ferrell et al., 2019), and suicidal ideation (dos Santos Treichel et al., 2018), underlining the importance of developing resilience in the context of caregivers themselves.
Alzheimer’s caregivers have been identified as our index case of caregivers, as they frequently experience both physical and mental psychosocial problems because of the nature and demands of their role. Persons with Alzheimer’s will experience declines in cognitive functions which ultimately impact their ability to carry out activities of daily living (ADLs), resulting in their dependence on formal or, more often, informal caregivers (Plassman et al., 2007). Coping-concept strategies that support resilience in caregiving for persons with Alzheimer’s encompass challenge-related coping-concept strategies such as the finding of meaning in their role as a caregiver. Protective and compensatory coping-concept strategies associated with caregiving for persons with Alzheimer’s include spirituality, optimism, resourcefulness, self-care, knowledge (about the disease), positive communication patterns, family connectedness, and social support (Aoun et al., 2018, Bekhet & Avery, 2017; Deist & Greeff, 2017).
Expanding this class of conditions to caregiving situations in which the person is dependent for most ADLs can also include persons with other types of dementia, parents of disabled children, caregivers of person with cancer, and caregivers of those with mental illness or severe mental deficits. Caregiver stressors might mirror the needs of those for whom they provide care. For example, caregivers of those who have physical deficits will likely provide more assistance with ADLs. Caregivers of persons with mental illness and/or deficits may or may not provide as much help with ADLs, but these caregivers might be at greater risk for experiencing problems with family dynamics. They can have more difficulty securing additional support and resources for such psychosocial issues (Ferrell et al., 2019). These examples illustrate how developing resilience in caregivers subsequently optimizes functioning, both in the dependent person and within the family unit.
These classes of illness discussed above and the psychosocial problems associated with them are summarized on Table 1. Note that these seven index cases and classes of illness are not exclusive—for instance we have not included palliative care and the patients who are dying, infectious diseases, cardiac diseases, and so forth, but those presented here provide a beginning, and a useful taxonomy that addresses the psychosocial aspects of care and associated coping concepts.
Table 1.
Common Psychosocial Problems and Coping Concepts for Index Cases and Classes of Illnesses.
| I. Identifying the Index Cases ↓ | ||||||
| Lung Transplant | Breast Cancer | Anxiety | Arthritis | Asthma | Spinal-Cord Injury | Alzheimer’s Caregiver |
| II. Identifying the Classes of Illnesses ↓ | ||||||
| Major Solid-Organ Transplants | Living with Uncertain Prognosis | Self-Awareness of Mental Illness | Ongoing Chronic Painful Conditions | Episodic Illnesses | Unexpected and Unanticipated Accidents or Trauma | Dyadic caregiving for the Frail and Ill |
| III. Identifying Common Psychosocial Problems ↓ | ||||||
| Anger Anxiety Depression Exhaustion Fear Hopelessness Inadequacy Role modification Stigma/guilt Uncertainty Vulnerability |
Anxiety Depression Distress Exhaustion Fatigue Fear Mental adjustment Stress |
Anxiety Depression Fatigue Fear Isolation Stress Vulnerability |
Chronic pain Depression Isolation Social functioning Stress Vulnerability |
Abuse Depression Fear Isolation Mental fatigue Shame Stress Vulnerability Sense of inadequacy |
Anger Anxiety Comorbidities Chronic pain Dependency Fear Grief Hopelessness Isolation Vulnerability |
Altered self-identity Anxiety Comorbidities Depression Isolation Vulnerability |
| IV. Identifying Commonly Used Coping Concepts ↓ | ||||||
| Disability status Hopefulness Mastery Optimism Pessimism/realism Spirituality Regimental control Social support |
Communication Emotional processing Hope Optimism Positive appraisal Social support Spirituality |
Acceptance Hope Humor Mindfulness Planning Reframing Self-efficacy Social support Spirituality |
Acceptance Autonomy Hope Optimism Patience Perseverance Purpose Self-efficacy Self-growth Social support Well-being |
Empowerment Hope Humor Normalization Optimism Social support Spirituality Self-esteem |
Acceptance Adaptation Experience Hope Inspiration Mentorship Optimism Perseverance Self-care Social support Spirituality |
Acceptance Communication Knowledge Mastery Meaning finding Optimism Perspective Resourcefulness Self-care Self-efficacy Social support Spirituality |
| V. Concepts Sorted into Stages in the Illness Trajectory (Table 2) ↓ | ||||||
| VI. Equanimity Identified as an Indicator of Resilience ↓ | ||||||
| VII. Development of The Resilience Framework for Nursing and Healthcare | ||||||
Step III. Identifying Common Psychosocial Problems
As many psychosocial problems commonly occur in all illnesses (Table 1), it is clear from this analysis that these are clustered. Most classes of illness cause profound emotional responses in the individuals. While some of these responses occur in several classes, most differ between classes, forming distinct patterns.
Step IV. Identifying Frequently Used Coping Concepts
Emotional states that frequently interfere with the individual’s ability to cope and that prevent the attainment of resilience include despair, fear, anxiety, depression, hopelessness, loneliness, disabilities, and inabilities (see Table 1). Protective concepts are considered by resilience theorists to shield against those negative states—for instance, optimism, which counters despair. In this framework we have kept the label “protective concepts” but applied this to selected concepts used at the beginning of the resilience work. As individuals realize that they are capable of adopting and utilizing strategies that will enable them to cope with the situation and ease their distress, they move to less passive concepts that imply engagement and work on the part of the individual: compensatory and challenge-related coping concepts (defined below).
Step V. Sorting Concepts According to the Resilience Trajectory
As we further considered the concepts for each class of illness, we were able to sort them into three functions—to protect, to compensate, and to challenge (see Table 2). These three concepts sequentially assist the individual in phases to be more resilient and to work toward a state of resilience. These groups of concepts are:
Table 2.
Concepts Sorted into Classes of Illness by the Stages of Coping.
| Classes of illness® | Major solid-organ transplants | Living with cancer | Self-awareness of mental illness | Ongoing chronic painful conditions | Episodic illness | Unexpected/unanticipated events | Dyadic caregiving for the frail & ill |
|---|---|---|---|---|---|---|---|
| Stages of coping | |||||||
| Protective concepts | Baseline fitness Emotional health Financial resources Pessimism/realism Social support Spirituality |
Acceptance Hope Humor Self-efficacy Self-discipline Social support Survival instinct |
Internal locus Perspective Self-efficacy Spirituality |
Acceptance Autonomy Hope Optimism Patience Perseverance Purpose Social support |
Hope Social support Spirituality Humor |
Acceptance Experience Hope Optimism Social support Spirituality |
Optimism Perspective Resourcefulness Self-care Social support Spirituality Well-being |
| Compensatory concepts | Environment Family support Hopefulness Optimism Spirituality |
Adaptation Personal mastery Optimism |
Acceptance Adaptation Hope Humor Mindfulness Social support Planning Reframing |
Patience Purpose Self-efficacy Self-growth Well-being |
Empowerment Optimism |
Optimism Opportunity Self-car Social support |
Acceptance Communication Knowledge Perspective Self-care Social support |
| Challenge concepts | Ambition Family support Mastery Social support |
Balance Communication Determination Endurance Knowledge |
Compassion Courage Endurance Knowledge |
Autonomy Coping Patience Perseverance Purpose Well-being |
Empowerment Normalization Self-esteem |
Acceptance Adaptation Inspiration Mentor Perseverance Social support |
Knowledge Mastery Meaning finding Perspective Self-efficacy Social support Spirituality |
Protective concepts: These are coping-concept strategies representing assets and resources that the individual can use to protect the self. These protective concepts help the individual to recognize, accept, and cope with their altered condition in particular in the initial phases of the illness.
Compensatory concepts: Once the individual has recognized their illness, coping concept strategies that supplement, replace, and/or support the individual can help them to mitigate and cope with their present condition.
Challenge-related concepts: Later in the illness trajectory, challenge-related concepts are coping-concept strategies that enable the individual to accept and work to overcome physical and psychological challenges and barriers so as to reach equanimity and be resilient (Fleming & Ledogar, 2008, p. 1).
When using strategies represented by these coping concepts, the individuals must have the ability to assess their predicament and envision their future, at least in a limited way. They realize that they are capable of utilizing strategies that will enable them to cope with the situation and ease their distress. Examples are the use of social support, spirituality, and concepts to reduce fear and regain hope. Individuals can visualize what will be reasonably achievable in their current situation, and this provides them with a realistic perspective.
Step VI. Identifying Equanimity as Reaching the State of Resilience
As the individual becomes more adept at coping, equanimity enables the individual to overcome the distress, and hence to attain resilience. Equanimity is characterized by a realistic acceptance of what cannot be changed, and an optimistic appraisal of possibilities for the future (Emlet, et al., 2011). It is an indicator that resilience has been attained. Equanimity is the level-headed acceptance of life’s circumstances with a degree of confidence that is not present in its counterpart, resignation. Equanamity is, therefore, a emotional state that indicates that resilience may now be achieved.
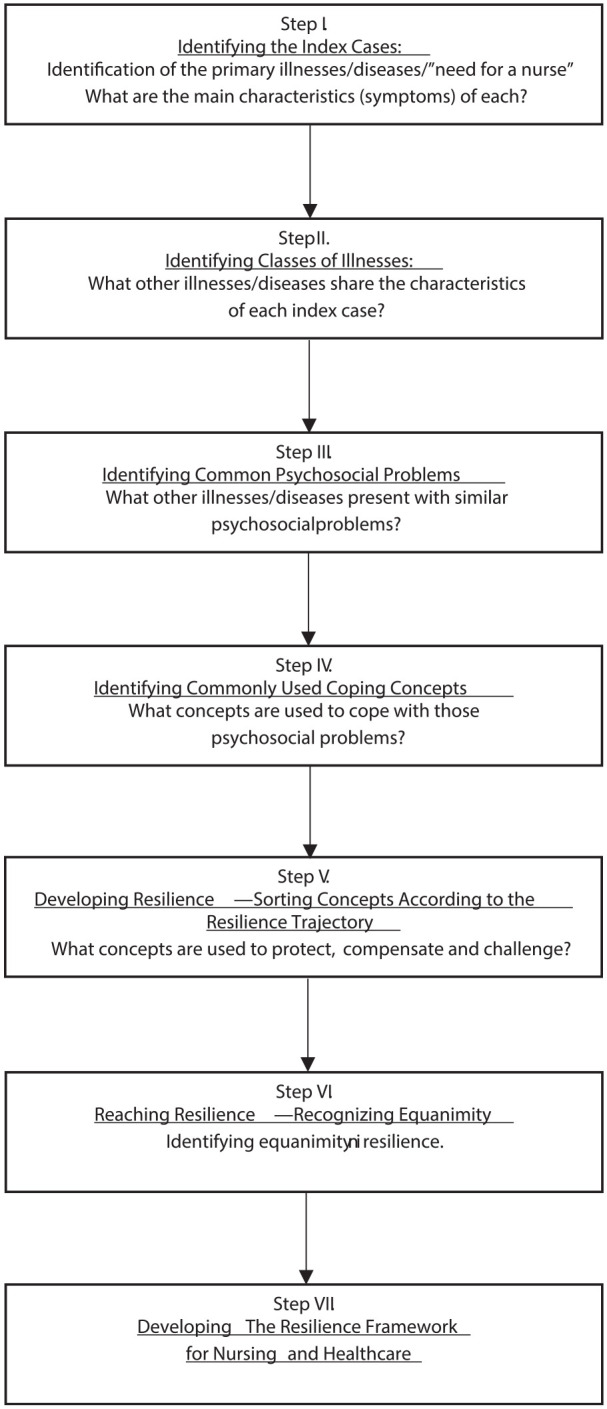
Step VII. Developing the Resilience Framework for Nursing and Healthcare
From the above analysis of the literature we developed a framework of resilience conceptualizing the process that individuals in various classes of illness use to establish resilience. The framework provides possible ways to facilitate patients’ development of resilience in the face of the various adversities they encounter. The process will be reviewed in detail here (see Figure 2).
Figure 2.
The resilience framework for nursing and healthcare.
Working to become resilient requires life readjustments and uses the processes of compensatory, protective, and challenge-related concept strategies previously reviewed (see Figure 2 and Table 2). The framework begins with an event of adversity. Adversity can originate from multiple scenarios that vary from a negative health diagnosis, to a traumatic event or serious illness, or to caregiving of a fragile family member. After a person encounters this devastating and life-altering adversity, they enter a phase of pre-resilience, of shock and enduring (Morse, 2010) that occurs with this sudden life change. The person initially begins to recognize, and then to confront their new limitations and recognize that interventions are necessary to sustain life. The outcome of the adverse event is uncertain, yet the person realizes that their illness or accident has drastically altered their life, and that resources for recovery, recalibration, and readjustment are currently out of reach. For instance, a person might feel that there is no alternative but to endure the pain, with all of their energy focusing on “bearing it” and suppressing emotions (Morse, 2010).8 During this phase the protective strategies are essential.
Once individuals become aware that they are an active participant in their recovery, they begin to recognize the additional resources that are available to help them cope with the work of recovery. In this phase, their capacity for compensatory coping is important and they develop obtainable therapeutic goals. While they recognize that the healthcare team and others in their social network are willing to participate in their recovery, they also recognize that the bulk of this effort must be their own, and move to challenge-related concepts.
These coping mechanisms help get the individual’s perspective and distress under control and provide a state of “self-possession, level-headedness, presence of mind, self-restraint, self-confidence, and equilibrium” (Hutchinson, 1993, p. 217). The person works through these processes and develops a state of equanimity. Equanimity enables hope, to establish realistic goals, to work to achieve these goals, and to be resilient.
Nevertheless, the adversity event might recur through remission (episodic, chronic, or degenerative) or a new experience might occur, such that the person will again move into the process of becoming resilient (see Figure 2). If a new adversity event occurs, the individual who has previously developed resilience can transfer previous experience into becoming resilient more quickly (Hildon et al., 2008). With recurring adversity, learning has occurred, so attaining resilience is abbreviated, the person is more proficient and knows what to expect and how to use the coping strategies.
Connecting the Resilience Framework to Nursing and Healthcare
The Resilience Framework for Nursing and Healthcare has the potential to be a powerful and significant framework that can help experienced nurses and healthcare providers, who are knowledgeable in psychosocial care, establish resilience for those in their care. The framework demands that the nurses have extensive knowledge about classes of illness for patients and their corresponding protective, compensatory, and challenge-related coping needs. These nurses must also possess extensive knowledge of therapeutic mechanisms and the application of coping concepts that can be used to help and support the patient as they navigate the process toward becoming resilient. Through introduction of The Resilience Framework for Nursing and Healthcare, we have provided a significant and versatile framework for improving nursing practice.
Exploring the Application of Resilience to Nursing-Care Situations
This framework has potentially useful applications in nursing and healthcare. However, using this framework demands that nurses broaden their focus beyond medical diagnoses and immediate presenting symptoms, to encompass patient problems inherent in their care. Moreover, they should consider their patients’ range of dynamic problems as belonging to common classes of illness that present with common psychosocial problems, which override the categorization of medical diagnoses that the patients are primarily living with. Furthermore, these problems can be addressed or mitigated by carefully selecting coping-concept strategies. Identifying concepts is not a matter of prescribing a concept label (such as “social support”) without an understanding of the complexities and intricacies of the dynamic mechanisms and types of support that lie within the concepts and the stage of the illness trajectory. For instance, patients with protective needs require social support that includes comforting and reassurance; patients with compensatory needs require advocacy and assistive social support; and patients with challenge-related needs require mentorship in setting achievable types of support. These separate and varied needs of individuals are required for different classes of illness, with differing concept sets, at different intensities and at different times in the trajectory or course of their illness. This individualization within The Resilience Framework for Nursing and Healthcare is one of the strengths of this approach. Nurses can use their assessment skills, knowledge of nursing concepts and theory and intuition when selecting appropriate coping concepts to incorporate into their care plan and to evaluate the effectiveness of each approach.
One current application that we have identified as Class of Illness: Living with the Uncertain Prognosis is the recently identifed COVID-19 diagnosis known as “long haulers” (Rubin, 2020). To date, approximately 10% of patients who have recovered from Sars-Cov-2 chronically suffer from or relapse into a complex post-viral syndrome with respiratory complaints, dyspnea, fatigue, lingering loss of smell or taste, cardiomyopathy, myalgia, “brain fog,” headaches, and mental illness (Carfì et al., 2020; Greenhalgh et al., 2020). Use of The Resilience Framework for Nursing and Healthcare enables delivery of tailored healthcare by recognizing commonalities with other illness classes. This example illustrates that a knowledge of other illness classes can transfer to compensatory, protective, and challenge-related concepts to this novel condition.
Psychosocial assessment skills are used to identify appropriate coping concepts, to open these concepts, and to determine how the conceptual attributes might match the patient’s needs. For example, should the nurse determine that a patient is hoping unrealistically, the nurse has to understand hope theory thoroughly enough to be able to work with the patient to modify the hoped-for goals, and to establish intermediate steps that can be taken to achieve the overall goal. Exploring the concept of hope and its different mechanisms within hoping in a heart-transplant survivor, in a spinal-cord injury patient, in mothers attempting to breastfeed when returning to work, and in women undergoing recovery from breast cancer, reveals different patterns and modes of obtaining hope for each condition (Morse & Doberneck, 1995).
The usefulness of this framework in practice is likely to depend on the ongoing development of a compendium of coping concepts to the level of mid-range theory, and their translation into practice so that they can contribute to optimal patient care. Coping concepts diminish the untenable aspects of illness by harnessing the strengths of the individual, thereby helping them to develop skills to support the process of building resilience, to achieve and improve outcomes. There is presently a myriad of concepts available within nursing to facilitate the use of this framework, but much urgent work is required to develop these concepts so they can be applied in clinical practice. In addition, this framework is versatile, and can be manipulated to fit the needs of the individual in the selection and pacing of coping concepts.
How should this framework be evaluated? Internally, the framework must be logical, coherent and comprehensive. Externally, evaluation will be determined by the implementation of the framework, as evidenced by its incorporation into nursing texts, curricula, research, and citation rates. The most significant criteria will be the usefulness of the framework, and its fit with nursing practice, and within research demonstrating evidenced-based, patient care outcomes.
Discussion
The Resilience Framework for Nursing and Healthcare provides a versatile and dynamic framework to guide nurses in assisting patients in using coping processes that build their resilience, thereby enabling them to alleviate their distress and to focus on the work of recovery. The utilization of this framework requires nurses to be adept and knowledgeable about assessment and selection of appropriate concepts and their application. Unfortunately, our present level of understanding of concepts, and our research to develop them, have focused narrowly on the meaning of the concept, largely ignoring the interaction of their attributes, their interaction with other concepts, and the versatility of their application in various situations. This work is in its infancy. Without such investigation into the significant concepts for enabling resilience, the selection of appropriate concepts is impotent. As an example, social support, when identified as a concept, will have different attributes and interactions for the stage of protection than it will have for the stage of challenge, and it will assume different roles in enabling social support from nursing and the family.
What Resilience Is and Is Not
Working toward the goal of attainment of resilience requires the nurse to fully comprehend what resilience is and is not. Some authors, taking the perspective of “strength,” have included gender differences in the expression of distress (see, Masood et al., 2016). Concealing distress is a part of enduring (Morse, 2010). It is not an indicator of resilience. Those who are suppressing or blocking emotions as a means of enduring do not have the ability to set future goals, an ability they must have in the process of becoming resilient.
The Versatility of the Framework
As noted earlier, individuals might have multiple psychosocial problems simultaneously. Based on The Framework, these should be assessed so that interventions can be developed that will address the various individual needs of each patient. As such, this should be entered into the patients’ medical record in such a way that all healthcare members are able to analyze and act on this information and thereby ensure coordination in achieving these goals. While some concepts might be prioritized according to immediate needs, this framework does not restrict the caregiver to the use of a single concept, nor only to those listed in Table 2.
Protective factors
In this framework some coping concepts may be categorized as protective in nature, in that they assist in alleviating the initial distress. However, based on the evidence in this analyisis, we dispute the application of the term “protective factors” to all coping concepts, as the term fails to account for the work of resilience and mutes the role of compensatory and challenge-related concepts in contributing to the work of becoming resilient. All coping concepts are not “protective.”
The state of equanimity
Here, we have selected the emotional state of equanimity as the outcome of the process of becoming resilient. Bonanno (2004) is correct when he writes that “resilience is different from recovery” (p. 20). Equanimity enables the channeling of energy from distress to the focus on coping-concept strategies and therapeutic programs, thereby enabling the final stage of recovery, recalibration, and readjustment toward health. Equanimity is the realistic acceptance of the impact of the individual’s current health status and their prognosis (Emlet et al., 2011), and is an indicator that the individual has attained resilience. Acceptance in equanimity is different from acceptance in self-transcendence (Mayan et al., 2006). Equanimity is active. Self-transcendence is the passive peace that occurs with the acceptance of a terminal diagnosis.
The particularity of coping concepts
Some researchers have suggested that there is a set of concepts that occur in all illnesses for the attainment of resilience. For example, optimism, social support, spirituality, and hope are commonly used. In this study, we have found that some concepts are relevant to certain classes of illness, but that only social support was relevant to all illness classes. Our review of the literature and synthesis of coping concepts found that some coping concepts were evident within many of the classes of illness. It must be noted, however, that we were unable to identify a list of universal coping concepts related to obtaining resilience across all classes of illness. By examining Table 2 we can see that specific concept sets relate to particular classes of illness. This is extremely important; extensive work and investigation should be undertaken in order to understand the needs of each class of illness so as to help patients attain the state of resilience.
The state of resilience
Resilience is a patient-centered concept, and the processes of attaining resilience have been described from the perspective of the patient. Yet attaining resilience is an interactive process, involving caregivers and significant others, particularly in the protective set of coping concepts. For instance, social support plays a significant role (in its various types—which, incidentally, have yet to be delineated or described), particularly in caregivers and significant others (when considered in the context of compensatory and challenge-related concepts). It is astonishing that trust is not predominant in this literature [for instance, see Robinson’s (2016) analysis of trust in the caregiver relationship]. Given one’s disabilities, handicaps, and impairments, the state of resilience enables one to achieve relative optimal health.
Does resilience go away? It becomes a part of the individual’s experiential memory (Srivastava & Sinha, 2012). Individuals do not have to be working toward resilience when operating in a state of equanimity. This is a more efficient form of maintaining resilience, one in which the individual can focus on regaining the activities of daily living.
Recurring adveristy
When another adverse event occurs and the person again responds with distress, the person leaves equanimity and reenters the framework at the beginning of pre-resilience (as seen in Figure 2). Prior experience with adversity will make this action more efficient and enable the individual to reach resilience more quickly. Internal and external supports might be needed, however, to buffer the challenge of experiencing so many adverse events in such short succession that their experience could overwhelm pre-established coping mechanisms.
Another aspect to consider in this process would be the duration of time between adverse events and how this timeline might impact an individual’s ability to efficiently reenter the resilience framework. Should too much time pass, will these learned behaviors be forgotten? Will the resources available to the individual have changed radically during this time? And will that change alter, in turn, the individual’s approach and coping concepts employed to navigate through the resilience framework?
Limitations
Rather than collecting targeted “raw” data within a specific project to develop this framework, we constructed the components using qualitative literature. While this means that the framework has the limitation of not been tested “in the real world” or in the clinical setting, the logical application and support of exising literature is a strength.
Conclusion
The framework of resilience proposed in this article is targeted toward the context for which it is intended: that is, the state of the ill who are experiencing profound, devastating, and rapid life-threatening changes. The weakness of our proposed framework lies in the state of the development of the concepts that will be identified and used to attain coping, equanimity, and resilience, and that will, in turn, permit the ill individual to move into the work of recovery, recalibration, and readjustment. The utilization of concepts per se has moved into nursing curricula and mid-range theory. Although these have been a primary interest among nurse researchers, much work into the opening of concepts and development of mid-range theory for nursing praxis remains to be completed. We have briefly mentioned the inadequacies of social support and anxiety, but this list of concepts in need of understanding and development for application is very long. Even the major umbrella concepts in this framework—coping, resilience, and equanimity—demand immediate attention and development in the context of illness. Much inquiry into the strategies of assessment for the selection and utilization of the menu of concepts identified here must be funded, explored, then moved into nursing education and clinical practice. Until nursing itself has developed adequate midrange theory to practice wisely, appropriately, and effectively, as well as the ability to demonstrate and document the changes in patients’ emotional states that result from such practice interventions, nursing will remain incomplete, ineffective, and weighted toward a technical, procedure-driven profession.
Resilience, as an important concept for attaining wellness, has been available to nursing for four decades. As previously stated, Haase’s work focused on developing resilience as a concept per se, identified the attributes, conducted quantitative testing of these variables, and even prepared a program to enhance resilience in adolescents with cancer (Haase, 2004; Haase et al, 2017). Her conception of resilience has application only to adolescents, linked narrowly to adolescent oncology and not to overall practice—a crucial yet missing step for our applied discipline. Her contribution is impactful, but specific. The Framework developed here, however, is different. It is versatile, fluid and adaptable for individual patient needs, available resources, and state-of-the-art concept development. Research into the practical application of midrange theories for developing coping and the coping concepts identified here will move this framework forward.
Acknowledgments
For assistance with pre-submission support, we thank Megan Hebdon, DNP, PhD. We thank the anonymous reviewers for their care and excellent recommendations.
Author Biographies
Janice M. Morse, PhD (Nurs), PhD (Anthro), FAAN is a professor and Presidential Endowed Chair at the University of Utah College of Nursing, and Professor Emeritus, University of Alberta, Canada. She was the founding director of the International Institute for Qualitative Methodology, University of Alberta, founding Editor for the International Journal of Qualitative Methods, and Editor of the Qual Press monograph series. She is the founding editor of Qualitative Health Research. Her research programs are in the areas of suffering and comforting, preventing patient falls, and developing qualitative methods.
Jacqueline Kent-Marvick, BSN, RN, is a PhD student and T32 pre-doctoral fellow at the University of Utah, College of Nursing. Her research focuses on the influences of postpartum social networks on health. She is particularly interested in the nature of social support within these networks, and the role of loneliness during the postpartum period as it relates to maternal and infant health.
Lisa A. Barry, MBA, BSN, RN is a PhD student at the University of Utah, College of Nursing. She has been a Registered Nurse for 24 years, mostly working on pediatric and neonatal intensive care. Her research focuses on nursing workforce and improving documentation for clinicians.
Jennifer Harvey, CPNP-AC, MPH, RN is a pediatric ICU nurse practitioner with Southcentral Foundation working with Alaskan Natives. She is also a PhD student at the University of Utah, College of Nursing with research interests in pediatric resuscitation.
Esther Narkie Okang, MPA, MS, BS, is a PhD student with the University of Utah, College of Nursing. Her research interests are examining cultural beliefs with respect to end-of-life decision-making among sub-Saharan African older adults living in Utah, and understanding the effects of breast cancer screening and education among West African women living in Utah. Miss Okang received prior training in Public Health, Health Promotion, and Public Administration, and currently works with the clinical trials office within the Pediatrics Department at the University of Utah.
Elizabeth A. Rudd, MSN, AGPCNP-BC, is a nurse practitioner and graduate of the Carolinas HealthCare System Advanced Clinical Practitioner Fellowship. She is currently serving as an adjunct clinical faculty member for the University of Utah, College of Nursing where she is also pursuing a PhD in nursing with an emphasis in informatics.
Ching-Yu Wang, MSN, RN is a clinical informaticist and PhD student at the University of Utah, College of Nursing. His research focuses on social-determinants data and implementing health information technology to support patient-centered emergency department care.
Marcia R. Williams MSN, FNP, is a PhD student at the University of Utah, College of Nursing. She is a Nurse Educator, Family Nurse Practitioner, and Health Systems Scientist with research interests in preventive rural healthcare.
Best Practice, Model, Framework, Method, Guidance, Standard: toward a consistent use of terminology—revised (Dec 18, 2019). https://www.vanharen.net/blog/best-practice-model-framework-method-guidance-standard-towards-consistent-use-terminology/
Here we are also including the role of prevention and the role of advanced practice.
We borrowed this term from epidemiology, where index case refers “the first identifiable” case. It is used in this instance to refer to the most typical example in which resilience is perceived to place a significant role.
Rather that adding a static list of uncited references for each index case, an inclass “exercise” may be using Google Scholar, the Index case and “resilience” as key words, as a means of “testing” and expanding the framework.
In 1962 Lois Murphy introduced the notion of “coping skills” in children learning to cope with new situations (Murphy, 1962)].
As previously mentioned we adapted constructs from earlier theorist, “Protective” introduced by Rutter (1979), and the application of Fleming & Ledogar’s, 2008) individual-community framework to patient care: “compensatory” and “challenge.”
This definition was synthesized from the literature within this project.
According to the Praxis Theory of Suffering (Morse, 2010), this phase concludes once the person begins to comprehend that they cannot change what has happened, then moves into emotional suffering, and finally, accepts whatever has happened.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: (Jacqueline Kent-Marvick, T32NR013456; m-PIs: Ellington & Mooney) National Institute of Nursing Research of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ORCID iD: Jacqueline Kent-Marvick  https://orcid.org/0000-0001-8850-2539
https://orcid.org/0000-0001-8850-2539
References
- Ahern N. R., Kiehl E. M., Sole M. L., Byers J. (2006). A review of instruments measuring resilience. Issues in Comprehensive Pediatric Nursing, 29(2), 103–125. 10.1080/01460860600677643 [DOI] [PubMed] [Google Scholar]
- Alizadeh S., Khanahmadi S., Vedadhir A., Barjasteh S. (2018). The relationship between resilience with self-compassion, social support and sense of belonging in women with breast cancer. Asian Pacific Journal of Cancer Prevention, 19(9), 2469–2474. 10.22034/APJCP.2018.19.9.2469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoun S. M., Toye C., Slatyer S., Robinson A., Beattie E. (2018). A person-centred approach to family carer needs assessment and support in dementia community care in Western Australia. Health & Social Care in the Community, 26(4), e578–e586. 10.1111/hsc.12575. [DOI] [PubMed] [Google Scholar]
- Aspinwall L. G., MacNamara A. (2005). Taking positive changes seriously. Cancer, 104(S11), 2549–2556. 10.1002/cncr.21244 [DOI] [PubMed] [Google Scholar]
- Asthma Society of Canada. (2020). Understanding asthma. Retrieved October 17, 2020, from https://asthma.ca/get-help/understanding-asthma/
- Barbour K. A., Blumenthal J. A., Palmer S. M. (2006). Psychosocial issues in the assessment and management of patients undergoing lung transplantation. Chest, 129(5), 1367–1374. 10.1378/chest.129.5.1367 [DOI] [PubMed] [Google Scholar]
- Barton C., Clarke D., Sulaiman N., Abramson M. (2003). Coping as a mediator of psychosocial impediments to optimal management and control of asthma. Respiratory Medicine, 97(7), 747–761. [DOI] [PubMed] [Google Scholar]
- Becker G., Newsom E. (2005). Resilience in the face of serious illness among chronically ill African Americans in later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(4), S214–S223. [DOI] [PubMed] [Google Scholar]
- Beeckman M., Hughes S., Van Ryckeghem D., Van Hoecke E., Dehoorne J., Joos R., Goubert L. (2019). Resilience factors in children with juvenile idiopathic arthritis and their parents: The role of child and parent psychological flexibility. Pain Medicine, 20(6), 1120–1131. [DOI] [PubMed] [Google Scholar]
- Bekhet A. K., Avery J. S. (2017). Resilience from the perspective of caregivers of persons with dementia. Archives of Psychiatric Nursing, 32(1), 19–23. 10.1116/j.apnu.2017.09.008. [DOI] [PubMed] [Google Scholar]
- Bell C. J., Phillips C. R., Haase J. E., Monahan P. O. (2007). 24: Relationship of communication to family adaptability and cohesion in adolescents diagnosed with cancer. Journal of Adolescent Health, 40(2), S29. 10.1016/j.jadohealth.2006.11.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzies K., Mychasiuk R. (2002). Fostering family resiliency: A review of the key protective factors. Child & Family Social Work, 14, 103–114. 10.1111/j.1365-2206.2008.00586.x [DOI] [Google Scholar]
- Bhattarai M., Maneewat K., Sae-Sia W. (2018). Determinants of resilience among people who sustained spinal cord injury from the 2015 earthquake in Nepal. Spinal Cord, 56, 78–83. 10.1038/sc.2017.93 [DOI] [PubMed] [Google Scholar]
- Black R., Dorstyn D. (2015). A biopsychosocial model of resilience for multiple sclerosis. Journal of Health Psychology, 20(11), 1434–1444. 10.1177/1359105313512879 [DOI] [PubMed] [Google Scholar]
- Bonanno G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20. 10.1037/0003-066X.59.1.20/ [DOI] [PubMed] [Google Scholar]
- Bonanno G. A., Galea S., Bucciarelli A., Vlahov D. (2006). Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychological Science, 17(3), 181–186. 10.1111/j.1467-9280.2006.01682.x [DOI] [PubMed] [Google Scholar]
- Bonanno G. A., Kennedy P., Galatzer-Levy I. R., Lude P., Elfström M. L. (2012). Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabilitation Psychology, 57(3), 236. 10.1037/a0029256 [DOI] [PubMed] [Google Scholar]
- Boscaglia N., Clarke D. (2007). Sense of coherence as a protective factor for demoralization in women with a recent diagnosis of gynecological cancer. Psycho-Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 16(3), 189–195. [DOI] [PubMed] [Google Scholar]
- Bradshaw C., Atkinson S., Doody O. (2017). Employing a qualitative description approach in health care research. Global Qualitative Nursing Research, 4, 2333393617742282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen S. J., Baravelli C. M., Schofield P. E., Jefford M., Yates P. M., Aranda S. K. (2009) Is symptom burden a predictor of anxiety and depression in patients with cancer about to commence chemotherapy? The Medical Journal of Australia, 190(S7), S99–S104. [DOI] [PubMed] [Google Scholar]
- Brix C., Schleussner C., Füller J., Roehrig B., Wendt T. G., Strauss B. (2008). The need for psychosocial support and its determinants in a sample of patients undergoing radioecological treatment of cancer. Journal of Psychosomatic Research, 65(6), 541–548. [DOI] [PubMed] [Google Scholar]
- Brodaty H., Donkin M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217–228. https://doi:10.1111/j.1447-0349.2012.00877.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberg J., Wood M. E., Black R. A., Surette D. A., Zacharoff K. L., Chiauzzi E. J. (2012). A randomized trial of a web-based intervention to improve migraine self-management and coping. Headache: The Journal of Head and Face Pain, 52(2), 244–261. 10.1111/j.1526-4610.2011.02031.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B. (2006). Shame resilience theory: A grounded theory study on women and shame. Families in Society, 87(1), 43–52. 10.1606/1044-3894.3483 [DOI] [Google Scholar]
- Brown J., Sorrell J. H., McClaren J., Creswell J. W. (2006). Waiting for a liver transplant. Qualitative Health Research, 16(1), 119–136. 10.1177/1049732305284011 [DOI] [PubMed] [Google Scholar]
- Brügger A., Aubert J. D., Piot-Ziegler C. (2014). Emotions while awaiting lung transplantation: A comprehensive qualitative analysis. Health Psychology Open, 1(1), 2055102914561272. 10.1177/2055102914561272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carfì A., Bernabei R., Landi F. (2020). Persistent symptoms in patients after acute COVID-19. JAMA, 324(6), 603–605. 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright T., Fraser E., Edmunds S., Wilkinson N., Jacobs K. (2015). Journeys of adjustment: The experiences of adolescents living with juvenile idiopathic arthritis. Child: Care, Health and Development, 41(5), 734–743. 10.1111/cch.12206 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). National current asthma prevalence. Retrieved October 17, 2020, from https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
- Chen E., Strunk R. C., Trethewey A., Schreier H. M., Maharaj N., Miller G. E. (2011). Resilience in low-socioeconomic-status children with asthma: adaptations to stress. Journal of Allergy and Clinical Immunology, 128(5), 970–976. 10.1016/j.jaci.2011.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D. G. (2014). Cognitive function, mental health, and health-related quality of life after lung transplantation. Annals of the American Thoracic Society, 11(4), 522–530. 10.1513/AnnalsATS.201311-388OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coogan P. F., Wise L. A., O’Connor G. T., Brown T. A., Palmer J. R., Rosenberg L. (2013). Abuse during childhood and adolescence and risk of adult-onset asthma in African American women. Journal of Allergy and Clinical Immunology, 131(4), 1058–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig A., Rodrigues D., Tran Y., Guest R., Bartrop R., Middleton J. (2014). Developing an algorithm capable of discriminating depressed mood in people with spinal cord injury. Spinal Cord, 52, 413–416. 10.1038/sc.2014.25 [DOI] [PubMed] [Google Scholar]
- de Moor J. S., de Moor C. A., Basen-Engquist K., Kudelka A., Bevers M. W., Cohen L. (2006). Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosomatic Medicine, 68(4), 555–562. 10.1097/01.psy.0000222379.71389.91 [DOI] [PubMed] [Google Scholar]
- Decker C., Phillips C. R., Haase J. E. (2004). Information Needs of Adolescents with Cancer. Journal of Pediatric Oncology Nursing, 21(6), 327–334. 10.1177/1043454204269606 [DOI] [PubMed] [Google Scholar]
- Deist M., Greeff A. P. (2017). Living with a parent with dementia: A family resilience study. Dementia, 16(1), 126–141. 10.1177/1471391215621853 [DOI] [PubMed] [Google Scholar]
- dos Santos Treichel C. A., da Rosa Jardim V. M., Prado Kantorski L., Guimarães Lima M. (2018). Prevalence and factors associated with suicidal ideation among family caregivers of people with mental disorders. Journal of Clinical Nursing, 28, 3470–3477. 10.1111/jocn.14938 [DOI] [PubMed] [Google Scholar]
- Edward S-L. (2013). Chronic illness and well-being: Using nursing practice to foster resilience as resistance. British Journal Nursing, 22, 741–742, 744, 746. 10.12968/bjon.2013.22.13.741 [DOI] [PubMed] [Google Scholar]
- Emlet C. A., Shakima T., Raveis V. H. (2011). “I’m not going to die from the AIDS”: Resilience in aging with HIV disease. The Gerontologist, 51(1), 101–111. 10.1093/geront/gnq060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrell E. L., Russin S. E., Hardy R. M. (2019). Informal caregiving experiences in post-traumatic stress disorder: A content analysis of an online community. Journal of Community Psychology, 47, 757–771. 10.1002/jcop.22151 [DOI] [PubMed] [Google Scholar]
- Flemming J., Ledogar R. J. (2008) Resilience, an evolving concept: A review of literature relevant to Aboriginal research. Pimatisiwin, 6(2), 25–46. [PMC free article] [PubMed] [Google Scholar]
- Fletcher D., Sarkar M. (2013). Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist, 18(1), 12–23. 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- Fuggle P., Shand P., Gill L., Davies S. (1996). Pain, quality of life, and coping in sickle cell disease. Archives of Disease in Childhood, 75(3), 199–203. 10.1348/135910702760213715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardenhire J., Mullet N., Fife S. (2019). Living with Parkinson’s: The process of finding optimism. Qualitative Health Research, 29(12), 1781–1793. [DOI] [PubMed] [Google Scholar]
- Garmezy N. (1985). Stress-resistant children: The search for protective factors. In Stevenson J. E. (Ed.), Recent research in developmental psychopathology: Journal of child psychology and psychiatry book supplement (pp. 213–233). Pergamon. [Google Scholar]
- Garmezy N. (1993). Children in poverty: Resilience despite risk. Psychiatry, 56(1), 127–136. 10.1080/00332747.1993.11024627 [DOI] [PubMed] [Google Scholar]
- Gillespie B. M., Chaboyer W., Wallis M. (2007). Development of a theoretically derived model of resilience through concept analysis. Contemporary Nurse, 25(1–2), 124–135. 10.5172/conu.2007.25.1-2.124 [DOI] [PubMed] [Google Scholar]
- Greene R. R. (2002). Holocaust survivors: A study in resilience. Journal of Gerontological Social Work, 37(1), 3–18. 10.1300/J083v37n01_02 [DOI] [Google Scholar]
- Greene R. R., Galambos C., Lee Y. (2004). Resilience theory: Theoretical and professional conceptualizations. Journal of Human Behavior in the Social Environment, 8(4), 75–91. 10.1300/J137v08n04_05 [DOI] [Google Scholar]
- Greenhalgh T., et al. (2020). Management of post-acute covid-19 in primary care. BMJ, 370, m3026. 10.1136/bmj.m3026 [DOI] [PubMed] [Google Scholar]
- Guest R., Craig A., Tran Y., Middleton J. (2015). Factors predicting resilience in people with spinal cord injury during transition from inpatient rehabilitation to the community. Spinal Cord, 53(9), 682–686. 10.1038/sc.2015.32 [DOI] [PubMed] [Google Scholar]
- Haase J. E. (2004). The adolescent resilience model as a guide to interventions. Journal of Pediatric Oncology Nursing, 21(5), 289–299. https://doi.org/ 10.1177/1043454204267922 [DOI] [PubMed] [Google Scholar]
- Haase J. E., Heiney S. P., Ruccione K. S., Stutzer C. (1999). Research triangulation to derive meaning-based quality-of-life theory: Adolescent Resilience Model and instrument development. International Journal of Cancer, 83(S12), 125–131. [DOI] [PubMed] [Google Scholar]
- Haase J. E., Kintner E. K., Robb S. L., Stump T. E., Monahan P. O., Phillips C., Stegenga K. A., Burns D. S. (2017). The resilience in illness model part 2: Confirmatory evaluation in adolescents and young adults with cancer. Cancer Nursing, 40(6), 454–463. 10.1097/NCC.0000000000000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haase J. E., Peterson S. J. (2015). Resilience. In Peterson S. J., Bredow T. S. (Eds.), Middle range theories: Application to nursing research and practice (4th ed, pp. 256–284). Walters Kluwer. [Google Scholar]
- Harrison J., Maguire P. (1994). Predictors of psychiatric morbidity in cancer patients. British Journal of Psychiatry, 165(5), 593–598. 10.1192/bjp.165.593 [DOI] [PubMed] [Google Scholar]
- Hassani P., Izadi-Avanji F., Rakhsan M., Majd H. (2017). A phenomenological study on resilience of the elderly suffering from chronic disease: A qualitative study. Psychology Research and Behavior Management, 10, 59–67. 10.2147/PRBM.S121336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemington K., Rogachov A., Cheng J., Bosma R., Kim J., Osborne N., Inman R., Davis K. (2018). Patients with chronic pain exhibit a complex relationship triad between pain, resilience, and within- and cross-network functional connectivity of the default mode network. Pain, 159(8), 1621–1630. 10.1097/j.pain.0000000000001252 [DOI] [PubMed] [Google Scholar]
- Herth K. (1992). Abbreviated instrument to measure hope: Development and psychometric evaluation. Journal of Advanced Nursing, 17(10), 1251–1259. 10.1111/j.13652648.1992.tb01843.x [DOI] [PubMed] [Google Scholar]
- Hildon Z., Smith G., Netuveli G., Blane D. (2008). Understanding adversity and resilience at older ages. Sociology of Health & Illness, 30(5), 726–740. [DOI] [PubMed] [Google Scholar]
- Hudson P., Morrison R. S., Schulz R., Brody A. A., Dahlin C., Kelly K., Meier D. E. (2020). Improving support for family caregivers of people with a serious illness in the United States: Strategic agenda and call to action. Palliative Medicine Reports, 1(1), 6–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter A. J., Chandler G. E. (1999). Adolescent resilience. Image: Journal of Nursing Scholarship, 31, 243–247. 10.1111/j.1547-5069.1999.tb00488.x [DOI] [PubMed] [Google Scholar]
- Husain A. N., Siddiqui M. T., Holmes E. W., Chandrasekhar A. J., McCabe M., Radvany R., Garrity E. R., Jr. (1999). Analysis of risk factors for the development of bronchiolitis obliterans syndrome. American Journal of Respiratory and Critical Care Medicine, 159(3), 829–833. 10.1164/ajrccm.159.3.9607099 [DOI] [PubMed] [Google Scholar]
- Hutchinson S. A. (1993). People with bipolar disorders quest for equanimity: Doing grounded theory. National League for Nursing, 19(2535), 213–236. [PubMed] [Google Scholar]
- Janssen B. M., Regenmortel T. V., Abma T. A. (2011). Identifying sources of strength: Resilience from the perspective of older people receiving long-term community care. European Journal of Ageing, 8, 145–156. 10.1007/s10433-011-0190-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones K.F., Simpson G., Briggs L., Dorsett P., Anderson M. (2019). A study of whether individual and dyadic relations between spirituality and resilience contribute to psychological adjustment among individuals with spinal cord injuries and their family members. Clinical Rehabilitation, 33(9), 1503–1514. 10.1177/0269215519845034 [DOI] [PubMed] [Google Scholar]
- Kilic S., Dorstyn D., Guiver N. (2013). Examining factors that contribute to the process of resilience following spinal cord injury. Spinal Cord, 51(7), 553–557. 10.1038/sc.2013.25 [DOI] [PubMed] [Google Scholar]
- Kimura N., Aso Y., Yabuuchi K., Ishibashi M., Hori D., Sasaki Y., Nakamichi A., Uesugi S., Fujioka H., Iwao S., Jikumaru M., Katayama T., Sumi K., Eguchi A., Nonaka S., Kakumu M., Matsubara E. (2019). Modifiable lifestyle factors and cognitive function in older people: A Cross-Sectional Observational Study. Frontiers in Neurology, 10, 401. 10.3389/fneur.2019.00401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G., Cathers T., Brown E., Specht J., Willoughby C., Polgar J., Mackinnon E., Smith L., Havens L. (2003). Turning points and protective processes in the lives of people with chronic disabilities. Qualitative Health Research, 13(2), 184–206. 10.1177/1049732302239598 [DOI] [PubMed] [Google Scholar]
- Koinis Mitchell D., Klein Murdock K., McQuaid E. L. (2004). Risk and resilience in urban children with asthma: A conceptual model and exploratory study. Children’s Health Care, 33(4), 275–297. 10.1207/s15326888chc3304_3 [DOI] [Google Scholar]
- Kornhaber R., Mclean L., Betihavas V., Cleary M. (2018). Resilience and the rehabilitation of adult spinal cord injury survivors: A qualitative systematic review. Journal of Advanced Nursing, 74(1), 23–33. 10.1111/jan.13396 [DOI] [PubMed] [Google Scholar]
- Kumpfer K. L. (1999). Factors and processes contributing to resilience: The resilience framework. In Glantz M. D., Johnson J. L. (Eds.), Longitudinal research in the social and behavioral sciences. Resilience and development: Positive life adaptations (pp. 179–224). Kluwer Academic. [Google Scholar]
- Ladd R. J., Valrie C. R., Walcott C. M. (2014). Risk and resilience factors for grade retention in youth with sickle cell disease. Pediatric Blood & Cancer, 61(7), 1252–1256. 10.1002/pbc.24974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer P., Feldman J., Giardino N., Song H. S., Schmaling K. (2002). Psychological aspects of asthma. Journal of Consulting and Clinical Psychology, 70(3), 691–711. 10.1037/0022-006X.70.3.691 [DOI] [PubMed] [Google Scholar]
- Liu L., Xu X., Xu N., Wang L. (2017). Disease activity, resilience and health-related quality of life in Chinese patients with rheumatoid arthritis: a multi-center, cross-sectional study. Health and Quality of Life Outcomes, 15(1), 149. 10.1186/s12955-017-0725-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo C., Zimmermann C., Rydall A., Walsh A., Jones J. M., Moore M. J., Shepherd F. A., Gagliese L., Rodin G. (2010). Longitudinal study of depressive symptoms in patients with metastatic gastrointestinal and lung cancer. Journal of Clinical Oncology, 28(18), 3084–3089. 10.1200/JCO.2009.26.9712 [DOI] [PubMed] [Google Scholar]
- Machida M., Irwin B., Feltz D. (2013). Resilience in competitive athletes with spinal cord injury: The role of sport participation. Qualitative Health Research, 23(8), 1054–1065. 10.1177/1049732313493673 [DOI] [PubMed] [Google Scholar]
- Mancini A. D., Bonanno G.A. (2009), Predictors and parameters of resilience to loss: Toward an individual differences model. Journal of Personality, 77, 1805–1832. 10.1111/j.1467-6494.2009.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangelli L., Gribbin N., Büchi S., Allard S., Sensky T. (2002). Psychological well-being in rheumatoid arthritis: Relationship to ‘disease’ variables and affective disturbance. Psychotherapy and Psychosomatics, 71(2), 112–116. 10.1159/000049354 [DOI] [PubMed] [Google Scholar]
- Markstrom C. A., Marshall S. K., Tryon R. J. (2001). Resiliency, social support, and coping in rural low-income Appalachian adolescents from two racial groups. Journal of Adolescence, 23(6), 693–703. 10.1006/jado.2000.0353 [DOI] [PubMed] [Google Scholar]
- Masood A., Masud Y., Mazahir S. (2016). Gender differences in resilience and psychological distress of patients with burns. Burns, 42(2), 300–306. 10.1016/j.burns.2015.10.006 [DOI] [PubMed] [Google Scholar]
- Masten A. S. (1994). Resilience in individual development: Successful adaptation despite risk and adversity. In Wang M. C., Gordon E. W. (Eds.), Educational resilience in inner-city America: Challenges and prospects (pp. 3–25). Lawrence Erlbaum. [Google Scholar]
- Mayan M., Morse J. M., Eldershaw L. P. (2006). Developing the concept of self-reformulation. QHW: International Journal of Qualitative Studies on Health and Well-being, 1(1), 20–26. [Google Scholar]
- McDonald S., Pugh M., Mickens M. (2019). Resilience after spinal cord injury: A scoping review. American Journal of Physical Medicine & Rehabilitation. Advance online publication. 10.1097/PHM.0000000000001371 [DOI] [PubMed]
- Metting E., van der Molen T., Kocks J. (2016). Loneliness and lack of social support severely influences patients’ quality of life. Secondary findings from our focus group study in asthma and COPD patients. European Respiratory Journal, 48(Suppl 60), PA729. 10.1183/13993003.congress-2016.PA729 [DOI] [Google Scholar]
- Min J., Jung Y., Kim D., Yim H., Kim J., Kim T., Lee C., Lee C., Chae J. (2013). Characteristics associated with low resilience in patients with depression and/or anxiety disorders. Quality of Life Research, 22, 231–241. 10.1007/s11136-012-0153-3 [DOI] [PubMed] [Google Scholar]
- Molina Y., Yi J. C., Martinez-Gutierrez J., Reding K. W., Yi-Frazier J. P., Rosenberg A. R. (2014). Resilience among patients across the cancer continuum: diverse perspectives. Clinical Journal of Oncology Nursing, 18(1), 93–101. 10.1188/14.CJON.93-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monden K., Trost Z., Catalano D., Garner A. N., Simcox J., Driver S., Hamilton R. G., Warren A. M. (2014). Resilience following spinal cord injury: A phenomenological view. Spinal Cord, 52(3), 197–201. 10.1038/sc.2013.159 [DOI] [PubMed] [Google Scholar]
- Mong M. D., Noguchi K., Ladner B. (2012). Immediate psychological impact of the deepwater horizon oil spill: symptoms of PTSD and coping skills. Journal of Aggression, Maltreatment & Trauma, 21(6), 691–704 10.1080/10926771.2012.694402 [DOI] [Google Scholar]
- Montoya P., Larbig W., Braun C., Preissl H., Birbaumer N. (2004). Influence of social support and emotional context on pain processing and magnetic brain responses in fibromyalgia. Arthritis & Rheumatism, 50(12), 4035–4044. [DOI] [PubMed] [Google Scholar]
- Morse J. M. (2010). The Praxis Theory of Suffering. In Philosophies and theories in advanced nursing practice. (Chapter 28). Ed by Butts J.B., Rich K.L. Sudbury, MA.: Jones & Bartlett. [Google Scholar]
- Morse J. M. (2011). Hearing bad news. Journal of Medical Humanities, 32:187–211. [DOI] [PubMed] [Google Scholar]
- Morse J. M. (2018). Theoretical coalescence: A method to develop qualitative concepts and theory. The example of enduring. Nursing Research, 67(2), 177–187. 10.1097/NNR.0000000000000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse J. M., Doberneck B. M. (1995). Delineating the concept of hope. Image: Journal of Nursing Scholarship, 27(4), 277–285. [DOI] [PubMed] [Google Scholar]
- Morse J. M., Pooler C., van Ward T., Maddox L., Olausson J.M., Roche-Dean M., Colorafi K., Madden C., Rogers B., Martz K. (2014). Awaiting the diagnosis of breast cancer: Strategies of enduring for preserving self. Oncology Nursing Research, 41(4), 350–359. 10.1188/14.ONF.350-359 [DOI] [PubMed] [Google Scholar]
- Murphy L. B. (1962). The widening world of childhood: Paths toward mystery. New York: Basic Books. [Google Scholar]
- Musich S., Wang S., Slindee L., Kraemer S., Yeh C. (2019). Association of resilience and social networks with pain outcomes among older adults. Population Health Management, 22(6), 511–521. 10.1089/pop.2018.0199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myaskovsky L., Dew M. A., McNulty M. L., Switzer G. E., DiMartini A. F., Kormos R. L., McCurry K. R. (2006). Trajectories of change in quality of life in 12-month survivors of lung or heart transplant. American Journal of Transplantation, 6(8), 1939–1947. [DOI] [PubMed] [Google Scholar]
- Naef R., Bournes D. A. (2009). The lived experience of waiting: A parse method study. Nursing Science Quarterly, 22(2), 141–153. 10.1177/0894318409331932 [DOI] [PubMed] [Google Scholar]
- Nelson A. E., Haase J., Kupst M. J., Clarke-Steffen L., Brace-O’Neill J. (2004). Consensus statements: Interventions to enhance resilience and quality of life in adolescents with cancer. Journal of Pediatric Oncology Nursing, 21(5), 305–307. [DOI] [PubMed] [Google Scholar]
- Neria Y., Besser A., Kiper D., Westphal M. (2010). A longitudinal study of post-traumatic stress disorder, depression, and generalized anxiety disorder in Israeli civilians exposed to war trauma. Journal of Traumatic Stress, 23(3), 322–330. 10.1002/jts.20522 [DOI] [PubMed] [Google Scholar]
- Olsson C. A., Bond L., Burns J. M., Vella-Brodrick D. A., Sawyer S. M. (2003). Adolescent resilience: A concept analysis. Journal of Adolescence, 26, 1–11. 10.1016/S0140-1971(02)00118-5 [DOI] [PubMed] [Google Scholar]
- Plassman B. L., Langa K. M., Fisher G. G., Heeringa S. G., Weir D. R., Ofstedal M. B., Burke J. R., Hurd M. D., Potter G. G., Rodgers W. L., Steffens D. C., Willis J. R., Wallace R. B. (2007). Prevalence of dementia in the United States: The aging demographics, and memory study. Neuroepidemiology, 29(1–2), 125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protudjer J. L., Kozyrskyj A. L., Becker A. B., Marchessault G. (2009). Normalization strategies of children with asthma. Qualitative Health Research, 19(1), 94–104. [DOI] [PubMed] [Google Scholar]
- Resilience. (2020). In Oxford English dictionary. https://www-oed-com.ezproxy.lib.utah.edu/view/Entry/163619
- Rew L., Horner S. D. (2003). Youth resilience framework for reducing health-risk behaviors in adolescents. Journal of Pediatric Nursing, 18(6), 379–388. 10.1016/S0882-5963(03)00162-3 [DOI] [PubMed] [Google Scholar]
- Richardson G. E. (2002). The metatheory of resilience and resiliency. Journal of Clinical Psychology, 58, 307–321. 10.1002/jclp.10020 [DOI] [PubMed] [Google Scholar]
- Robinson C. A. (2016). Trust, health care relationships, and chronic illness: A theoretical coalescence. Global Qualitative Nursing Research, 3, 2333393616664823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M., Hanna E., Raine G., Robertson S. (2019). Extending the comfort zone: Building resilience in older people with long-term conditions. Journal of Applied Gerontology, 38(6), 825–848. 10.1177/0733464817724042 [DOI] [PubMed] [Google Scholar]
- Rojas M., Rodriguez Y., Pacheco Y., Zapata El, Monsalve D., Mantilla R., Rodriguez Jimenez M., Ramirez-Santana C., Molano-Gonzalez N., Anaya J. (2018). Resilience in women with autoimmune rheumatic diseases. Joint, Bone, Spine, 85(6), 715–720. 10.1016/j.jbspin.2017.12.012 [DOI] [PubMed] [Google Scholar]
- Rosenberger E. M., Dew M. A., DiMartini A. F., DeVito Dabbs A. J., Yusen R. D. (2012). Psychosocial issues facing lung transplant candidates, recipients and family caregivers. Thoracic Surgery Clinics, 22(4), 517–529. 10.1016/j.thorsurg.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R. (2020). As their numbers grow, COVID-19 “Long Haulers” stump experts. JAMA, 324(14), 1381–1383. 10.1001/jama.2020.17709\ [DOI] [PubMed] [Google Scholar]
- Rutter M. (1979). Fifteen thousand hours: Secondary schools and their effects on children. Harvard University Press. [Google Scholar]
- Rutter M. (2012). Resilience as a dynamic concept. Development and Psychopathology, 24(2), 335–344. 10.1017/S0954579412000028 [DOI] [PubMed] [Google Scholar]
- Rutter M., Rutter M. (1993). Developing minds: Challenge and continuity across the life span. Basic books. [Google Scholar]
- Shaw L. M., Vanderstichele H., Knapik-Czajka M., Clark C. M., Aisen P. S., Petersen R. C., Blennow K., Soares H., Simon A., Lewczuk P., Dean R., Siemers E., Potter W., Lee V. M., Trojanowski J. Q., & Alzheimer’s Disease Neuroimaging Initiative (2009). Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Annals of Neurology, 65(4), 403–413. 10.1002/ana.21610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw Y., Bradley M., Zhang C., Dominique A., Michaud K., McDonald D., Simon T. (2019). The development of resilience among rheumatoid arthritis patients: A qualitative study. Arthritis Care & Research, 72, 1257–1265. 10.1002/acr.24024 [DOI] [PubMed] [Google Scholar]
- Sheerin C. M., Lind M. J., Brown E. A., Gardner C. O., Kendler K. S., Amstadter A.B. (2017). The impact of resilience and subsequent stressful life events on MDD and GAD. Depression & Anxiety, 35(2), 140–147. 10.1002/da.22700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. I., Chae J. H., Min J. A., Lee C. U., Hwang S. I., Lee B. S., Han S. H., Ju H. I., Lee C. Y. (2012). Resilience as a possible predictor for psychological distress in chronic spinal cord injured patients living in the community. Annals of Rehabilitation Medicine, 36(6), 815–820. 10.5535/arm.2012.36.6.815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon K., Barakat L. P., Patterson C. A., Dampier C. (2009). Symptoms of depression and anxiety in adolescents with sickle cell disease: The role of intrapersonal characteristics and stress processing variables. Child Psychiatry and Human Development, 40(2), 317. 10.1007/s10578-009-0129-x [DOI] [PubMed] [Google Scholar]
- Singer J. P., Singer L. G. (2013). Quality of life in lung transplantation. Seminars in Respiratory and Critical Care Medicine, 34(3), 421–430. 10.1055/s-0033-1348470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder C. R., Harris C., Anderson J. R., Holleran S. A., Irving L. M., Sigmon S. T., Harney P. (1991). The will and the ways: Development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology, 60(4), 570–585. 10.1037/0022-3514.60.4.570 [DOI] [PubMed] [Google Scholar]
- Southwick S. M., Bonanno G. A., Masten A. S., Panter-Brick C., Yehuda R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5, 25338. 10.3402/ejpt.v5.25338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spratling R., Weaver S. R. (2012). Theoretical perspective: Resilience in medically fragile adolescents. Research and Theory for Nursing Practice, 26(1), 54–68. 10.1891/1541-6577.26.1.54 [DOI] [PubMed] [Google Scholar]
- Srivastava S., Sinha A. (2012). Resilience for well-being: The role of experiential learning. In Dalel A. K., Misra G. (Eds.), New directions in health psychology (pp. 329–349). SAGE. [Google Scholar]
- Stewart D. E., Yuen T. (2011). A systematic review of resilience in the physically ill. Psychosomatics, 52(3), 199–209. 10.1016/j.psym.2011.01.036 [DOI] [PubMed] [Google Scholar]
- Taylor E. J., Petersen C., Oyedele O., Haase J. (2015). Spirituality and spiritual care of adolescents and young adults with cancer. Seminars in Oncology Nursing, 31(3), 227–241. 10.1016/j.soncn.2015.06.002 [DOI] [PubMed] [Google Scholar]
- Thompson K., Bulls H., Sibille K., Bartley E., Glover T., Terry E., Vaughn I., Cardoso J., Sotolongo A., Staud R., Hughes L., Edberg J., Redden D., Bradley L., Goodin B., Fillingim R. (2018. b). Optimism and psychological resilience are beneficially associated with measures of clinical and experimental pain in adults with or at risk for knee osteoarthritis. The Clinical Journal of Pain, 34(12), 1164–1172. 10.1097/AJP.0000000000000642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson N. J., Fiorillo D., Rothbaum B. O., Ressler K. J., Michopoulos V. (2018. a). Coping strategies as mediators in relation to resilience and post-traumatic stress disorder. Journal of Affective Disorders, 225, 153–159. 10.1016/j.jad.2017.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokish J., Kissenberth M., Tolan S., Salim T., Tadlock J., Kellam T., Long C., Crawford A., Shanley E. (2017.). Resilience correlates with outcomes after total shoulder arthroplasty. Journal of Shoulder and Elbow Surgery: JSES, 26(5), 752–756. 10.1016/j.jse.2016.12.070 [DOI] [PubMed] [Google Scholar]
- Tusaie K., Dyer J. (2004). Resilience: A historical review of the construct. Holistic Nursing Practice, 18, 3–8. [DOI] [PubMed] [Google Scholar]
- Ungar M. (2003). Qualitative contributions to resilience research. Qualitative Social Work, 2(1), 85–102. https://doi.org/10:1177/1473325003002001123 [Google Scholar]
- Villaggi B., Provencher H., Coulombe S., Meunier S., Radziszewski S., Hudon C., Roberge P., Provencher M.D., Houle J. (2015). Self-management strategies in recovery from mood and anxiety disorders. Global Qualitative Nursing Research, 2, 2333393615606092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinson J. A. (2002). Children with asthma: Initial development of the Child Resilience Model: Practice applications of research. Pediatric Nursing, 28, 149–158. [PubMed] [Google Scholar]
- Wagnild G. (2003). Resilience and successful aging: Comparison among low and high income older adults. Journal of Geron-tological Nursing, 29(12), 42–49. 10.3928/0098-9134-20031201-09 [DOI] [PubMed] [Google Scholar]
- Wagnild G., Young H. M. (1990). Resilience among older women. The Journal of Nursing Scholarship, 22(4), 252–255. 10.1016/j.gerinurse.2016.02.014 [DOI] [PubMed] [Google Scholar]
- Weisman A. D. (1979) A model for psychosocial phasing in cancer. General Hospital. [DOI] [PubMed] [Google Scholar]
- Wilks S. E., Little K. G., Gough H. R., Spurlock W. J. (2011). Alzheimer’s aggression: Influences on caregiver coping and resilience. Journal of Gerontological Social Work, 54(3), 260–275. 10.1080/01634372.2010.544531 [DOI] [PubMed] [Google Scholar]
- Williams-Gray B., Senreich E. (2015). Challenges and resilience in the lives of adults with sickle cell disease. Social Work in Public Health, 30(1), 88–105. 10.1080/19371918.2014.938396 [DOI] [PubMed] [Google Scholar]
- Xu N., Zhao S., Xue H., Fu W., Liu L., Zhang T., Huang R., Zhang N. (2017). Associations of perceived social support and positive psychological resources with fatigue symptom in patients with rheumatoid arthritis. PLoS One, 12(3), e0173293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarzaur B., Bell T. M., Zanskas S. A. (2017). Resiliency and quality of life trajectories after injury. Journal of Trauma and Acute Care Surgery, 82, 939–945. 10.1097/TA.0000000000001415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziadni M. S., Patterson C. A., Pulgarón E. R., Robinson M. R., Barakat L. P. (2011). Health-related quality of life and adaptive behaviors of adolescents with sickle cell disease: Stress processing moderators. Journal of Clinical Psychology in Medical Settings, 18(4), 335–344. [DOI] [PubMed] [Google Scholar]