Abstract
An 11-year-old boy was referred to the emergency room (ER) because of a stab wound on the scrotum due to a tree trunk. The external genitalia computed tomography (CT) scan revealed a 5-cm long stick that was stuck in his left hemiscrotum; however, the testis was normal. Scrotal exploration and debridement of non-viable tissue was performed, and no testicular or surrounding structure injury was found. At the postoperative evaluation 1 month later, the surgical wound and the patient's general condition were satisfactory.
Keywords: Scrotal trauma, Penetrating injury, Genitalia, Foreign body
Introduction
Due to the location of the scrotum and its high degree of mobility, penetrating scrotal injury is rare.1 Genitourinary injury occurs in about 10% of abdominal trauma cases, and scrotal and/or testicular injury occurs in about 1% of incidents.2,3 Penetrating scrotal injuries are rare in childhood. We report the case of a pediatric patient with a penetrating scrotal injury.
Case presentation
An 11-year-old boy was referred to the emergency room (ER) for a stab wound to the scrotum due to a stick that had occurred 4 hours previously. The patient complained of severe pain. He had climbed a 2-meter-high tree and then fell onto the tree trunk below. The patient's weight was 37 kg (81.57 lbs) and height was 134 cm. His vital signs and the Glasgow Coma Scale score were within normal limits.
Complete physical examination results were within normal limits. Local examination revealed a penetrating injury due to a stick, with an entry site in the left hemiscrotum and the tip at the upper level of the left pubic bone (Fig. 1). The right testis and hemiscrotum were normal. There was no bloody discharge from the urethral meatus.
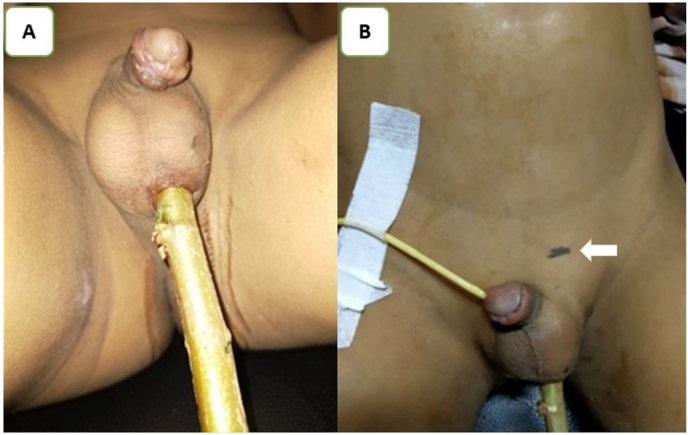
Fig. 1.
Image of the patient's stab wound to the scrotum before surgery.
1A. A stick with an entry site in the left hemiscrotum.
1B. The tip of the stick was at the upper level of the left pubic bone (white arrow).
The focused assessment with sonography in trauma (FAST) result was normal. The abdomen and external genitalia multi-slice computed tomography (MSCT) scan revealed a 5-cm stick that was stuck in his left hemiscrotum from the left caudal hemiscrotum to the cranioanterior pubic bone (Fig. 2A and B). The tip of the foreign body was near the pubic bone, and the testis was normal as revealed by non-contrast computed tomography (CT) (Fig. 2C) and a three-dimensional CT of his external genitalia (Fig. 2D).
Fig. 2.
Non-contrast CT and a three-dimensional CT imaging before the surgery.
2A and 2B. A 5-cm stick (blue arrow) was stuck in the left hemiscrotum.
2C. The foreign body (blue arrow) and the left testis (yellow arrow), which was normal, are shown using non-contrast CT.
2D. A three-dimensional CT of the patient's external genitalia showed the foreign body (blue arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The patient was administered broad-spectrum antibiotics and prophylactic tetanus toxoid, and transferred to the operating theatre for an emergency scrotal exploration. The testis and spermatic cord were normal (Fig. 3A), and we performed a debridement procedure and primary closure. A Penrose drain was left on the side of the wound (Fig. 3B). He was then administered a broad-spectrum antibiotic and intravenous analgesics drugs for 3 days. At the postoperative evaluation 1 month later, the patient's surgical wound and general condition were satisfactory.
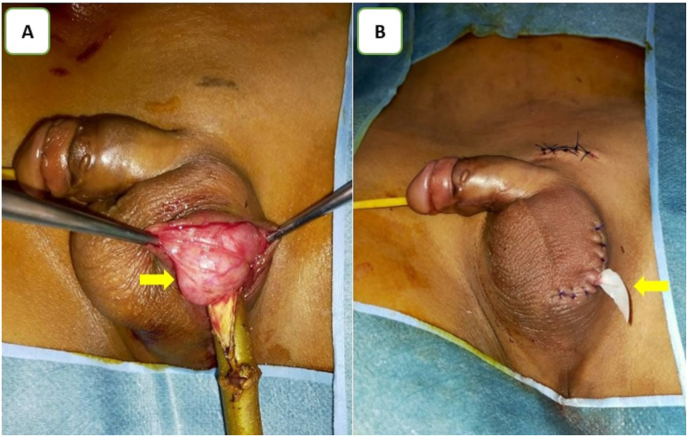
Fig. 3.
Intraoperative image.
3A. The testis (arrow) and spermatic cord was normal upon scrotal exploration and debridement.
3B. A Penrose drain (arrow) was left on the side of the wound.
Discussion
Penetrating scrotal injury by foreign bodies in childhood are rare due to the location and degree of mobility, and surrounding structures such as spermatic cord, testes, penis, urethra, femoral vessels, and rectum could be involved. Thus, a systematic evaluation of all children with these injuries is required to prevent complications including testicular tissue loss or urethral strictures.1
Our patient's testicles were normal, which could be because: 1) in the scrotum, the testicles move inherently; 2) the elastic scrotal skin allowed the internal structure to avoid the point of contact during trauma; 3) the cremaster reflex provides a protective reflex mechanism; and 4) the tensile strength of the tunica albuginea was a physical defense.
Pediatric patients with penetrating scrotal injury are managed the same as adult patients, including controlling active bleeding and stabilizing vital signs.1,4 Once hemodynamically stable, the patient should immediately receive a tetanus booster and broad-spectrum antibiotics.1,3,4 Laboratory tests such as fecal guaiac and urinalysis, which may show rectal or urethral injury, should be performed. The injured area such as the urethra, penis, testes, perineal area, rectum, and femoral arteries in both lower extremities should be examined.1,4 Anoscopy examination is usually performed if there is suspicion of trauma to the anus or rectum, but in this patient, we did not do so because we saw that the direction of the puncture was from the left caudal hemiscrotum to the cranioanterior pubic bone.
The European Association of Urology recommends immediate debridement for penetrating scrotal injury if the patient is stable and if physical examination and abdominal CT shows no concomitant injuries.1 Immediate surgical exploration of penetrating scrotal injury is required to accurately assess the level of damage to the genitourinary and reproductive organs and to prevent severe complications.5
Scrotal hematoma is a sign of trauma to the dartos muscle and testicular rupture, whereas hematuria, bloody discharge from urethra, dysuria, or urinary retention are signs of possible urethral injury. A penile hematoma is a sign of a possible rupture of the corpus cavernosa, although injury to the penis is rare. A decreased or missing lower extremity pulse, decreased or missing lower limb pulse, and blood per rectum can be a sign of non-genitourinary injury.1
Both careful physical examination and radiographic examination are required to determine the surgical approach, accurate injury rates, and the need for caution regarding foreign body containment. If a physical examination shows or does not rule out urethral injury, a retrograde urethral examination may be performed. A urethral catheter can be inserted if there is no urethral injury, but if there is urethral injury, a suprapubic urine diversion, or less frequently, primary repair is required [1,5]. Our patient was stable, so we performed abdominal and external genitalia non-contrast CT scans, which showed that the abdominal organs and testis were normal.
Most patients who require surgery have multiple injuries, with associated organ injury reported to be as high as 83%. Surgical exploration aims to prevent complications such as infection, secondary bleeding, chronic pain, erectile dysfunction, curvature, and unrecognized urethral injury, and to save the gonads as much as possible if they are injured. If the vas deferens is injured, ligation with the plan to repair it electively is the most appropriate plan for multiple injuries. If the spermatic cord is injured, the damaged vessel must be ligated.5
Our young patient had no further symptoms on the external genitalia at a follow-up outpatient visit 1 month after discharge.
Conclusion
Penetrating scrotal injury in childhood requires prompt surgical exploration to prevent delayed complications.
Consent
Written informed consent was obtained from the child's parents or guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
No funding or sponsorship was received for this study or publication of this article.
Declaration of competing interest
The authors declare that they have no conflict of interests.
Contributor Information
Muhammad Asykar Palinrungi, Email: apalinrungi@yahoo.com.
Syarif, Email: syarifbakri@hotmail.com.
Khoirul Kholis, Email: khoirulkholis@yahoo.com.
Syakri Syahrir, Email: drsyakrisyahrir@gmail.com.
Herman Syah Putra Nasution, Email: drputranstok@yahoo.com.
Muhammad Faruk, Email: faroex8283@gmail.com.
References
- 1.Ferlise V.J., Haranto V.H., Ankem M.K., Barone J.G. Management of penetrating scrotal injury. Pediatr Emerg Care. 2002;18 doi: 10.1097/00006565-200204000-00009. https://journals.lww.com/pec-online/Fulltext/2002/04000/Management_of_penetrating_scrotal_injury.9.aspx [DOI] [PubMed] [Google Scholar]
- 2.Randhawa H., Blankstein U., Davies T. Scrotal trauma: a case report and review of the literature. Can Urol Assoc J. 2019;13 doi: 10.5489/cuaj.5981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owusu Ofori E., Bin Alhassan B.A., Essoun S., Asante-Asamani A., Maison P. Penetrating scrotal injury: two unusual case reports in children and brief review of literature. J Adv Med Med Res. 2020:39–44. doi: 10.9734/jammr/2020/v32i930480. [DOI] [Google Scholar]
- 4.Lynch T., Martinez-Pineiro L., Plas E. EAU guidelines on urological trauma. Eur Urol. 2005;47:1–15. doi: 10.1016/j.eururo.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Morey A.F., Metro M.J., Carney K.J., Miller K.S., McAninch J.W. Consensus on genitourinary trauma: external genitalia. BJU Int. 2004;94:507–515. doi: 10.1111/j.1464-410X.2004.04993.x. [DOI] [PubMed] [Google Scholar]