Abstract
Background
A high prevalence of disability has been previously observed in developed countries. Identifying trends in its prevalence and risk, as well as protective factors of disability, are essential to establish effective prevention strategies.
Objective
The purposes of this study are to outline trends in the prevalence of disability among Australian adults and to analyse the relationship between obesity, and physical activity with disability.
Design
A retrospective longitudinal research design.
Methods
The study utilized the most recent 14 waves (wave 6 through 19) of the nationally-representative Household, Income and Labour Dynamics in Australia (HILDA) survey (2006–2019). The Generalized Estimating Equation (GEE) with the logistic link function model was employed to estimate the relationships between obesity and physical activity with disability. The final study sample consisted of 189,519 person-year observations from 26,208 participants.
Results
The pooled prevalence of disability in adults is 28%. The prevalence of disability among older adults (65 and above years) is more than 50%, irrespective of gender. Further, it identifies obesity and physical activity as risk and protective factors of disability for adults, respectively. The odds of acquisition of a disability was 1.33 times (Odds Ratios [OR]: 1.33, 95% Confidence Interval [CI]: 1.28–1.39) higher among obese adults than healthy weight counterparts. However, adults undertaking recommended level of physical activity (more than thrice a week to everyday) per week have 17% (OR: 0.83, 95% CI: 0.81–0.85) lower chances of disability acquisition.
Conclusions
Obesity imposes a significant toll on adult Australians' health. This risk factor of disability can be reduced through public health interventions.
Keywords: Disability, Obesity, Physical activity, Australia, Generalized estimating equation
Highlights
-
•
The prevalence of self-reported disability among Australian adults is 28%.
-
•
The prevalence of disability among the elderly (aged over 64 years) is more than 50%, irrespective of gender.
-
•
The probability of acquisition of a disability was higher among obese adults compared with healthy weight peers.
-
•
Undertaking the recommended level of physical activity is associated with lower chances of disability acquisition.
1. Introduction
Disability is a crucial health indicator of population health. The term ‘disability’ reters to a condition of the body or mind that affects a person's normal daily activities and participation, such as vision, hearing, thinking, remembering, learning, communicating, and movement (CDC, 2020a, CDC, 2020b). Approximately 15% (over 1 billion) of the global population are living with a disability and is projected to double (2 billion) by 2050 (World Health Organization, 2018). In 2018, over 4.4 million (1 in 5 people) Australians had some form of disability (AIHW, 2019), and around 5.7% have a severe disability (Australian Bureau of Statistics, 2018).
Adults with disabilities experience substantial health disparities. Disabled adults rate their health substantially poorer compared with their non-disabled counterparts in Australia (AIHW, 2019). Disabled adults are more prone to suffer from chronic diseases, such as heart disease, arthritis, back problems, dementia, intellectual disorders, and neurotic disorders (Australian Bureau of Statistics, 2018). Moreover, disabled adults experienced discrimination, violence and difficulties in accessing and utilising health services (AIHW, 2019). Further, disabled people are less likely to be in the workforce and have substantially less personal income compared with adults without disability (Australian Bureau of Statistics, 2018). Additionally, there is evidence that disabled people have lower productivity in the workplace in the form of lower levels of job satisfaction (Keramat, Alam, Gow, & Biddle, 2020a, 2020b, 2020c, 2020d), higher absenteeism (Keramat et al., 2020a, 2020b, 2020c, 2020d) and presenteeism (Keramat et al., 2020a, 2020b, 2020c, 2020d) compared with non-disabled counterparts.
The rising prevalence of disability is, in part, due to the ageing trajectory of the population and higher incidence of chronic diseases (World Health Organization, 2018). Previous research has found that obese, tobacco users, higher levels of alcohol drinkers, and physically inactive people were more likely to be disabled (Mathers & Loncar, 2006; World Health Organization, 2015). A longitudinal study revealed that being obese in mid-life is associated with a higher risk of being physically disabled at an older age (Wong et al., 2015a). A Dutch study identified age, excessive body fat, depression, and joint complaints as the significant risk factors for disability (Taş et al., 2007). Further, a systematic review provides evidence that older age, and poor health condition increased the risk of being disabled (Tas et al., 2007). Furthermore, a prospective cohort study provides evidence that obesity, physical inactivity, and hypertension caused disability in Italian adults (Balzi et al., 2009). Moreover, Korean research identified that people with poor physical health, depression, and obesity had a higher tendency of having a disability (Kim et al., 2005). Additionally, other evidence reported that limited daily activities, low physical functioning, multiple physical and psychological conditions were positively associated with disability (Mehta et al., 2002; Sinclair et al., 2001).
The two main limitations of existing studies on the risk and protective factors of adult disability are small sample sizes and solely focused on disability in elderly (Chen & Guo, 2008; Mehta et al., 2002; Sinclair et al., 2001; Taş et al., 2007). As far as the authors are concerned, this is the first study that report disability trends among Australian adults using longitudinal data. The benefit of utilising such data is that it can capture within and between-person variation in the characteristics of the study population. Moreover, there is little conclusive evidence on the longitudinal relationship between obesity and physical activity with disability in Australian adults. To prevent increasing disability prevalence, it is important to gain a better understanding of the risk and protective factors of adults with disability in Australia. Therefore, this study aims to reveal trends in the national prevalence of disability in Australian adults and assess its association with obesity and physical activity.
2. Data and methods
2.1. Data source and sample selection
The data come from the most recent 14 waves (2006–2019) of the Household, Income and Labour Dynamics in Australia (HILDA) survey. HILDA is an annual nationally representative longitudinal survey of the Australian adult population that collects a wide variety of information on respondents' socio-demographic, economic, and lifestyle characteristics, along with labour market activity and a range of health topics since 2001. HILDA mostly collects information from participating household members aged 15 years or over through face-to-face interviews by trained interviewers and self-completion questionnaire (SCQ). The HILDA survey used multistage sampling technique to select the initial sample of households. More detailed information regarding the HILDA survey design and methodology can be found elsewhere (Freidin et al., 2002). The main reason for using the HILDA data set is that it contains information on self-reported disability, weight status, and physical activity. Other advantages of using the data set is that it includes detailed information on socio-demographic and lifestyle characteristics, including age, gender, education, civil status, labour force status, ethnicity, smoking and alcohol consumption at several time points.
This study pooled waves 6 (2006) through 19 (2019) of the HILDA survey to generate a sample that is sufficiently large to infer the association between overweight, obesity, and physical activity with disability. The main reason for selecting these study waves is that not all variables of interest were available from wave 1 through 19. For example, BMI measure has only been collected from wave 6 onwards. The sample is restricted to adults aged 15 years and over that have valid information on disability, weight status, and physical activity. Application of inclusion and exclusion criteria resulted in a final study sample of 189,519 person-year observations from 26,208 participants for the subsample analyses.
2.2. Outcome variable
The primary outcome of this study is self-reported disability status. The survey collected data on respondents' disability status following the International Classification of Functioning, Disability, and Health (ICF) guidelines under the WHO framework (Keramat et al., 2020a, 2020b, 2020c; LaMontagne et al., 2016; Lopez Silva et al., 2020). The term ‘disability’ has been used as umbrella term covering impairments, functional limitations, and participation restriction in the definition of ICF (World Health Organization, 2001). The HILDA survey participants reported on their disability status in response to the question: ‘do you have any long-term health condition, impairment or disability that restricts your everyday activities, and has lasted, or is likely to last, for 6 months or more?’ The survey presents 17 types of disability, such as sight problems, hearing problems, speech problems, limited use of arms or fingers, difficulty in gripping things, and limited use of feet or legs to the respondents to define their disability status (Cebulla & Zhu, 2016). A binary measurement was used to capture the respondents' disability status. The variable takes the value 1 if the respondent reports that he or she has a disability and 0 for ‘no’ disability.
2.3. Exposure variables
2.3.1. Body mass index (BMI)
The primary exposure variable of interest is BMI which is a continuous variable that measures the participant's weight status. The HILDA survey calculates respondents' BMI using the formula of weight (in kilograms) divided by height (in meters) square. For this study, BMI was converted to categorical variable and collapsed into four categories: ‘underweight’ (<18.50), ‘healthy weight’ (18.50 to <25), ‘overweight’ (25 to <30), and ‘obese’ (≥30) following the World Health Organization (WHO) guidelines and previous studies (Keramat et al., 2020d, 2020e; World Health Organization, 2020).
2.3.2. Physical activity
Information on physical activity was collected by asking the question: ‘In general, how often do you participate in moderate or intensive physical activity for at least 30 min?’ Participants' responses were pre-coded into six categories: ‘not at all’, ‘less than once/week’, ‘1 or 2 times/week’, 3 times/week’, ‘more than 3 times/week but not every day’, and ‘everyday’. This study utilized this information to measure moderate to vigous physical activity (MVPA) undertaken by the respondents following previous study (Perales et al., 2014). Responses were collapsed into two levels: undertaking the recommended level of physical activity (more than 3 times/week but not every day, and everyday) and less than the recommended level of physical activity (not at all, less than once/week, 1 or 2 times/week, and 3 times/week).
2.4. Other covariates
This study included several confounders for their potential relationship with adult disability as based on existing literature (Boyle et al., 2007; Kim et al., 2005; Lee & Park, 2008; Taş et al., 2007; Wong et al., 2015b) and the information available in the HILDA survey. Socio-demographic covariates included in the study were age (15–24, 25–34, 35–44, 45–54, 55–64, and ≥65 years), gender (male, female), education (year 11 and below, year 12, professional courses, undergraduate, postgraduate), civil status (single, married/living together, widow/separated/divorced), household income quintile (quintile 1 to 5), labour force status (employed, unemployed, not in the labour force), indigenous status (not of indigenous origin, Aboriginal or Torres Strait Islander or both), and remoteness (major city, regional city, remote area). Two lifestyle characteristics considered in this study are smoking status (never smoked, ex-smoker, current smoker), and alcohol consumption (never drank, ex-drinker, only rarely to 3 days per week, over three days per week).
2.5. Estimation strategy
This study constructed an unbalanced panel data set consisting of 189,515 person-year observations by linking 26,208 de-identified individuals' records. As there are 14 periods of exposure (2006–2019), most participants are included in the analytic sample more than once. Reports of the pooled characteristics of the study sample are in frequency (n) and percentages (%) with 95% confidence intervals (CIs). Bivariate relationships between disability and main variables of interest (obesity and physical activity) along with other covariates were initially examined through chi-square tests (the test results were not reported here). Only those covariates that had been found statistically significant with a P-value <0.05 in the bivariate analyses were incorporated in the final multivariate regression model as independent variables.
In the present analyses, the outcome variable (self-reported disability) was dichotomous (yes versus no) and data were correlated as observations on an individual in the final analytic sample have been utilized more than once. Therefore, this study deployed Generalized Estimating Equation (GEE) technique with a logistic link to check the association between obesity and physical activity with disability. One of the great advantages of using GEE in the case of correlated data is it provides efficient parameter estimates even in the case of misspecification of correlation structure. Model 1 reports the adjusted association between obesity and physical activity with self-reported disability after adjusting age, gender, education, civil status, household income, labour force status, indigenous status, remoteness, smoking, and alcohol consumption. For ease of interpretation, this study presents the multivariate regression results in the form of odds ratios with 95% confidence intervals and has set the p-value at 5% or lower level for statistical significance. All statistical analyses were performed using the statistical software Stata, version 16.0.
3. Results
Pooled descriptive statistics of the study population are exhibited in Table 1. Of the 189,515 participants, a large number 53,037 (approximately 28%) have some form of disability, 24% were obese, and 66% do not undertake the recommended level of moderate to vigorous physical activity. Among the study participants, 18% were aged over 64 years, 53% were female, 49% were married, 35% have university qualifications (undergraduate and postgraduate combined), 64% were employed, 97% were non-indigenous, and 66% were from major cities. Nearly 18% of respondents currently smoke, and 81% consume alcohol.
Table 1.
Descriptive statistics of the study participants.
| Variables | n | % (95% CI) |
|---|---|---|
| Disability status | ||
| No | 136,482 | 72.01 (71.81–72.22) |
| Yes | 53,037 | 27.99 (27.78–28.19) |
| BMI categories | ||
| Underweight (<18.50) | 4961 | 2.62 (2.55–2.69) |
| Healthy weight (18.50 to <25.00) | 74,928 | 39.54 (39.32–39.76) |
| Overweight (25.00 to <30.00) | 64,656 | 34.12 (33.90–34.33) |
| Obesity (≥30) | 44,974 | 23.73 (23.54–23.92) |
| Moderate to vigorous physical activity (MVPA) | ||
| Less than recommended level | 125,546 | 66.24 (66.03–66.46) |
| Recommended level | 63,973 | 33.76 (33.54–33.97) |
| Socio-demographic characteristics | ||
| Age groups | ||
| 15–24 years | 31,579 | 16.66 (16.50–16.83) |
| 25–34 years | 32,227 | 17.00 (16.84–17.17) |
| 35–44 years | 31,018 | 16.37 (16.20–16.53) |
| 45–54 years | 32,619 | 17.21 (17.04–17.38) |
| 55–64 years | 28,332 | 14.95 (14.79–15.11) |
| 65 and above years | 33,744 | 17.81 (17.63–17.98) |
| Gender | ||
| Male | 89,695 | 47.33 (47.10–47.55) |
| Female | 99,824 | 52.67 (52.45–52.90) |
| Highest educational qualification | ||
| Year 11 or below | 53,825 | 28.40 (28.20–28.60) |
| Year 12 | 28,744 | 15.17 (15.01–15.33) |
| Professional courses | 41,190 | 21.73 (21.55–21.92) |
| Undergraduate | 45,201 | 23.85 (23.66–24.04) |
| Postgraduate | 20,559 | 10.85 (10.71–10.99) |
| Civil Status | ||
| Single | 42,890 | 22.63 (22.44–22.82) |
| Married | 113,822 | 60.06 (59.84–60.28) |
| Widow/separated/divorced | 32,807 | 17.31 (17.14–17.48) |
| Household income quintile | ||
| Quintile 1 (0–20%) | 37,904 | 20.00 (19.82–20.18) |
| Quintile 2 (20–40%) | 37,904 | 20.00 (19.82–20.18) |
| Quintile 3 (40–60%) | 37,905 | 20.00 (19.82–20.18) |
| Quintile 4 (60–80%) | 37,903 | 20.00 (19.82–20.18) |
| Quintile 5 (80–100%) | 37,903 | 20.00 (19.82–20.18) |
| Labour force status | ||
| Employed | 121,790 | 64.26 (64.05–64.48) |
| Unemployed | 6800 | 3.59 (3.51–3.67) |
| Not in the labour force | 60,929 | 32.15 (31.93–32.36) |
| Indigenous status | ||
| Not of indigenous origin | 184,009 | 97.09 (97.02–97.17) |
| Aboriginal/Torres Strait Islander | 5510 | 2.91 (2.83–2.98) |
| Remoteness | ||
| Major city | 125,529 | 66.24 (66.02–66.45) |
| Regional city | 61,293 | 32.34 (32.13–32.55) |
| Remote area | 2697 | 1.42 (1.37–1.48) |
| Lifestyle characteristics | ||
| Smoking status | ||
| Never smoked | 103,051 | 54.38 (54.15–54.60) |
| Ex-smoker | 52,252 | 27.57 (27.37–27.77) |
| Current smoker | 34,216 | 18.05 (17.88–18.23) |
| Alcohol consumption | ||
| Never drank | 20,551 | 10.84 (10.70–10.98) |
| Ex-drinker | 14,914 | 7.87 (7.75–7.99) |
| Only rarely to 3 days/week | 103,147 | 54.43 (54.20–54.65) |
| 3+ days/week | 50,907 | 26.86 (26.66–27.06) |
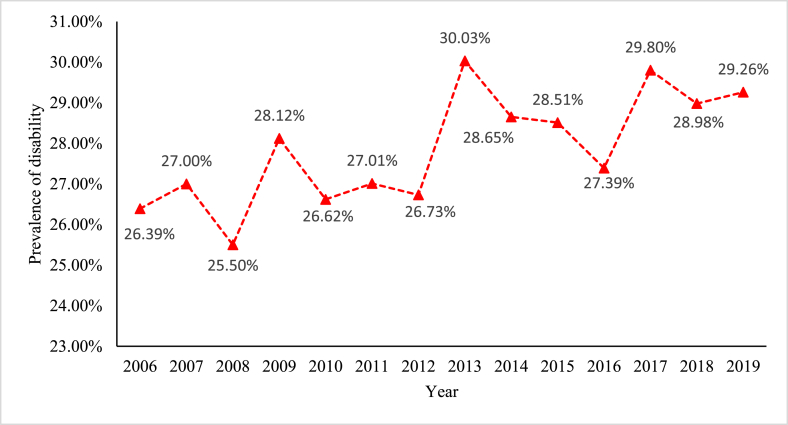
Fig. 1 displays the trends in the prevalence of national adult disability in Australia for the period 2006 to 2019. The percentage of adults with disability in Australia has plateaued during the study period. It has been observed that the rate has been increased by nearly 3 percentage points over the study periods, ranged from 26% (2006) to 29% (2019).
Fig. 1.
Trend in the prevalence of disability in Australia, 2006–2019
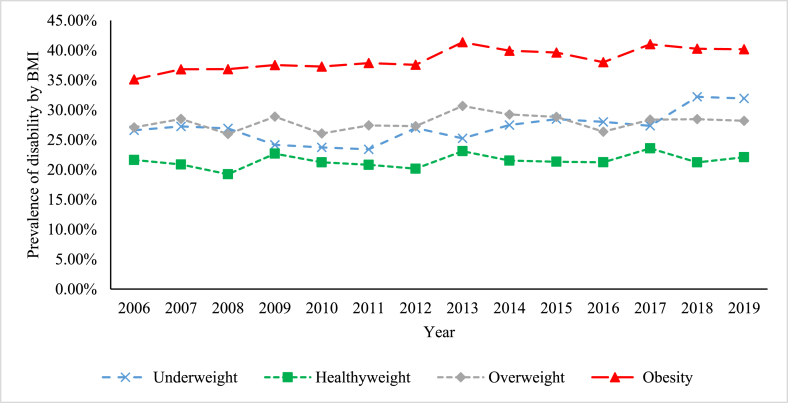
Fig. 2 presents the prevalence of disability stratified by participants' BMI. Disability prevalence varies by weight status, and the prevalence of disability has been found highest among obese adults. Fig. 2 shows that disability rates among obese, overweight, underweight, and healthy weight adults were 40%, 28%, 32%, and 22%, respectively, in 2019. The prevalence of disability among obese adults increased by 5 percentage points during the study periods, from 35% (2006) to 40% (2019).
Fig. 2.
Trends in disability by weight status in Australia, 2006–2019
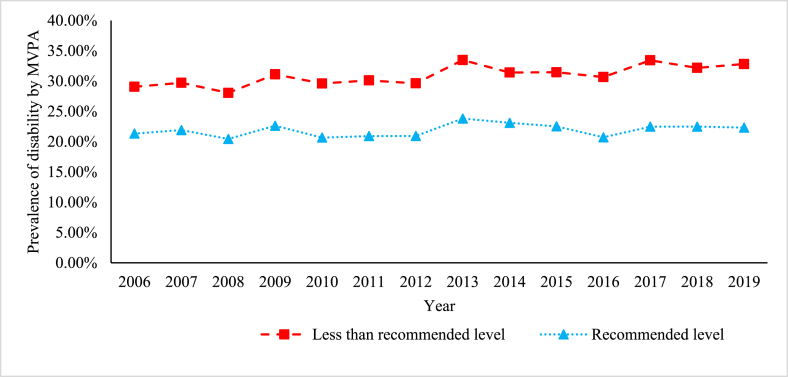
Fig. 3 displays the trend in the prevalence of disability stratified by moderate to vigorous physical activity for the period 2006 to 2019. It is apparent that the prevalence of disability is substantially low among the participants undertaking recommended level of physical activity than peers performing less than the recommended level of physical activity. For example, the prevalence of disability among the particpants performing recommended and less than recommended level of physical activity were 22% and 33%, respectively, in 2019. The prevalence of disability has been found highest among the adults who perform less than recommended level of physical activity, and it ranged from 28% (2008) to 33% (2013). However, the figure shows that disability prevalence among those physically active (undertaking recommenden level) is substantially lower, ranged from 20% (2008) to 24% (2013).
Fig. 3.
Trend in disability by moderate to vigorous physical activity (MVPA) in Australia.
Table 2 reports the pooled prevalence of adults' disability by age and gender at four different time points over the period 2006 to 2019. The results show that the disability rates among the elderly (65 and above years) irrespective of gender were over 50% in all years. The prevalence of disability has been found to be highest among the elderly (65 and above years) followed by middle-aged adults (aged 55–64 years). In 2019, the rate of disability in males aged 15–24, 25–34, 35–44, 45–54, 55–64, and 64+ years were 14, 15, 17, 26, 35, and 55%, respectively.
Table 2.
The pooled prevalence of disability by age and gender at 4 different time points.
| Year | Age groups |
15–24 years |
25–34 years |
35–44 years |
45–54 years |
55–64 years |
65 and above years |
|---|---|---|---|---|---|---|---|
| Gender | prevalence | prevalence | prevalence | prevalence | prevalence | prevalence | |
| 2006 | Male | 11.36% | 14.20% | 20.55% | 24.51% | 39.42% | 54.74% |
| Female | 11.57% | 15.79% | 18.41% | 25.62% | 36.76% | 53.31% | |
| 2010 | Male | 12.19% | 10.87% | 17.77% | 23.40% | 37.61% | 55.17% |
| Female | 13.99% | 12.85% | 19.48% | 28.27% | 41.00% | 53.73% | |
| 2014 | Male | 14.28% | 13.22% | 18.37% | 25.80% | 36.81% | 58.97% |
| Female | 15.03% | 14.64% | 18.54% | 27.28% | 40.52% | 57.29% | |
| 2019 | Male | 14.35% | 15.32% | 16.73% | 26.46% | 34.66% | 54.83% |
| Female | 19.08% | 17.03% | 18.65% | 26.93% | 37.03% | 56.90% |
Table 3 presents the adjusted association between excess body weight and physical activity with a disability after controlling for age, gender, education, civil status, household income, labour force status, indigenous status, remoteness, smoking and alcohol consumption. The results from the GEE technique showed that the odds of acquisition of a disability was 1.12 (OR: 1.12, 95% CI: 1.09–1.15) and 1.33 (OR: 1.33, 95% CI: 1.28–1.39) times higher among overweight and obese adults, respectively, compared with their healthy-weight counterparts. It is also observed that adults undertaking recommended level of moderate to vigorous physical activity (more than thrice to everyday) have 17% (OR: 0.83, 95% CI: 0.81–0.85) lower chances of suffering from a disability compared with peers performing less than the recommended level of physical activity.
Table 3.
Adjusted relationships between BMI and physical activity with disability among Australian adults.
| Variables | Model 1 disability (yes versus no) OR (95% CI) | P-value |
|---|---|---|
| BMI categories | ||
| Underweight (<18.50) | 1.12 (1.04–1.20) | 0.01 |
| Healthy weight (18.50 to <25.00) (ref) | ||
| Overweight (25.00 to <30.00) | 1.12 (1.09–1.15) | <0.001 |
| Obesity (≥30) | 1.33 (1.28–1.39) | <0.001 |
| Moderate to vigorous physical activity (MVPA) | ||
| Less than recommended level (ref) | ||
| Recommended level | 0.83 (0.81–0.85) | <0.001 |
| Socio-demographic characteristics | ||
| Age groups | ||
| 15–24 years (ref) | ||
| 25–34 years | 1.32 (1.24–1.41) | <0.001 |
| 35–44 years | 1.77 (1.65–1.90) | <0.001 |
| 45–54 years | 2.69 (2.50–2.89) | <0.001 |
| 55–64 years | 3.99 (3.71–4.30) | <0.001 |
| 65 and above years | 5.31 (4.92–5.73) | <0.001 |
| Gender | ||
| Male (ref) | ||
| Female | 0.96 (0.93–1.01) | 0.16 |
| Highest educational qualification | ||
| Year 11 or below (ref) | ||
| Year 12 | 0.91 (0.86–0.97) | <0.001 |
| Professional courses | 0.98 (0.93–1.03) | 0.42 |
| Undergraduate | 0.81 (0.77–0.86) | <0.001 |
| Postgraduate | 0.75 (0.69–0.81) | <0.001 |
| Civil Status | ||
| Single (ref) | ||
| Married/living together | 0.90 (0.85–0.95) | <0.001 |
| Widow/separated/divorced | 1.11 (1.04–1.19) | 0.002 |
| Household income quintile | ||
| Quintile 1 (0–20%) | 1.21 (1.16–1.26) | <0.001 |
| Quintile 2 (20–40%) | 1.13 (1.09–1.17) | <0.001 |
| Quintile 3 (40–60%) | 1.03 (0.99–1.06) | 0.16 |
| Quintile 4 (60–80%) | 1.04 (1.01–1.08) | 0.02 |
| Quintile 5 (80–100%) (ref) | ||
| Labour force status | ||
| Employed (ref) | ||
| Unemployed | 1.36 (1.28–1.44) | <0.001 |
| Not in the labour force | 1.72 (1.66–1.78) | <0.001 |
| Indigenous status | ||
| Not of indigenous origin (ref) | ||
| Aboriginal/Torres Strait Islander | 1.28 (1.14–1.43) | <0.001 |
| Remoteness | ||
| Major city (ref) | ||
| Regional city | 1.13 (1.08–1.18) | <0.001 |
| Remote area | 0.85 (0.74–0.98) | 0.03 |
| Lifestyle characteristics | ||
| Smoking status | ||
| Never smoked (ref) | ||
| Ex-smoker | 1.24 (1.19–1.29) | <0.001 |
| Current smoker | 1.39 (1.33–1.46) | <0.001 |
| Alcohol consumption | ||
| Never drank (ref) | ||
| Ex-drinker | 1.20 (1.13–1.27) | <0.001 |
| Only rarely to 3 days/week | 0.94 (0.90–0.98) | 0.01 |
| 3+ days/week | 0.81 (0.76–0.85) | <0.001 |
Abbreviations: OR, odds ratios; ref, reference.
Values in bold are statistically significant at p < 0.05.
4. Discussion
The results showed that the adult disability rate in Australia is approximately 28%. It is also revealed that the prevalence of disability among older adults (65 and above years) is more than 50% irrespective of gender. This finding corroborates previous survey findings that the rate of disability is higher among older adults (AIHW, 2019).
The GEE population-averaged model identified obesity and physical activity as the risk and protective risk factors of adults with disability, respectively, after adjusting for confounders. The results reveal a positive association between obesity and disability, that is obese people reported higher disability compared with their healthy-weight peers. This finding confirms existing evidence (Alley & Chang, 2007; Chen & Guo, 2008; Zoico et al., 2004). A longitudinal study also supports the result of the present study, as it found that obesity was significantly positively associated with disability (Wong et al., 2015b). That study showed that obese adults experienced a 3% higher risk of having some form of disability for each additional year they lived (Wong et al., 2015b). A possible explanation is that obesity is closely associated with chronic diseases that result in health complexities (Al Snih et al., 2010). Further, metabolic irregularities due to obesity is another unanticipated explanation for developing a disability (Donini et al., 2016).
The study results also revealed a negative association between physical activity and disability. Adults undertaking recommended level of moderate to vigorous physical activity were less prone to be disabled compared with peers performed less than recommended level of physical activity per week. This finding corroborates previous study results (Boyle et al., 2007; Lee & Park, 2008). The mechanism through which physical activity negatively affects disability is complex. Existing evidence shows that physical inactivity is responsible for the progression of chronic disease (Penedo & Dahn, 2005). Besides, physical inactivity may decrease learning power, increase ischemia, and cause neurotoxic damage (Kramer et al., 2005). The possible reason behind physical activity being a protective factor against disability acquisition is that regular physical activity has several beneficial effects on health. The benefits include improved aerobic capacity, bone and muscle strength, maintaining a healthy weight, and lower risk of having cardiovascular disease, type 2 diabetes and metabolic syndrome, and some cancers (Boyle et al., 2007; CDC, 2020a, CDC, 2020b).
This study found that excess body weight and cigarette/tobacco smoking are significant risk factors of adults disability. There is evidence that the elimination of five modifiable risk factors (smoking, obesity, high blood pressure, high cholesterol, and diabetes) could reduce disability by 53% (Mehta et al., 2017). Therefore, the present study suggests that public health intervention should target weight management, reduce cigarette smoking to the lowest observed levels, and promote physical activity to prevent disability. These suggestions align with the existing evidence. Promotion of physical activity may reduce the level of obesity, and harsh tobacco control law discourages smoking, which in turn postpones the progression of disability (Lee & Park, 2008).
This study has several strengths that include the longitudinal nature of the data, the large sample size, and incorporation of a wide range of confounders. To the best of the authors' knowledge, this is the first Australian study that has used a nationally representative sample along with a longitudinal follow-up to check the association between obesity and physical activity with disability. The present study has used a nationally representative sample of 189,519 person-year observations from 26,2018 respondents that help to find out precise estimates and draw a valid inference. Besides, this study adjusted the potential confounding effects of smoking, alcohol consumption, labour force status, and ethnicity.
There are some limitations that should be considered when interpreting the study results. Disability status, BMI, smoking, alcohol consumption, and physical activity were all assessed using self-report. Therefore, self-reported bias may arise since overweight and obese adults tend to overestimate height and underestimate weight (Gorber et al., 2007; Maukonen et al., 2018). Also, justification bias may arise in case of self-reported disability, as respondents reported worse disability levels than probably exists in the general Australian population to obtain financial benefits through government transfer payments (Black et al., 2017). The present study is a retrospective longitudinal study that reveals the long-term association between obesity and physical activity with disability. However, causality cannot be drawn as the current study performed analyses on an unbalanced panel data set. Therefore, further investigation is required to draw causal inferences to explore the association between obesity and physical activity with disability using a prospective longitudinal cohort study design.
5. Conclusion
This study used de-identified data from the most recent 14 waves of the nationally-representative HILDA survey covering the period 2006 to 2019 to show the trend in the prevalence of adult disability and to check the relationship between obesity and physical activity with disability in Australia. The study results showed that the prevalence of adult disability is nearly 28% and that the rate is over 50% among older adults (65 and above years) irrespective of gender. Using the GEE technique, this study found that obesity is a significant risk, and physical activity a protective factor of adult disability in Australia. These findings have significant implications as Australia is currently experiencing sharp increases in adult disability and obesity. The population of adults with some form of disability should be a target group for public health interventions. Improved risk factor prevention and health promotion may assist in reducing the disability level. Therefore, health policymakers should target obesity for interventions to prevent adult disability. Another effective strategy to avoid disability should be encouraging physical activity in all Australians.
Ethics approval
This study did not require ethical approval as the analysis used only de-identified existing unit record data from the HILDA survey. However, the authors completed and signed the Confidentiality Deed Poll and sent it to NCLD (ncldresearch@dss.gov.au) and ADA (ada@anu.edu.au) before the data applications' approval. Therefore, datasets analysed and/or generated during the current study are subject to the signed confidentiality deed.
Author's contributions
SAK and NJS initiated the study, conducted the data analysis, and drafted the manuscript. KA, JG, and SB offered advice, critical comments, and edited the draft manuscript. All the authors read and approved the final manuscript.
Availability of data and materials
The data used for the study were collected from the Melbourne Institute of Applied Economic and Social Research. There are some restrictions on this data, and it is not available to the public. Those interested in accessing this data should contact the Melbourne Institute of Applied Economic and Social Research, The University of Melbourne, VIC 3010, Australia.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgements
The authors would like to thank the Melbourne Institute of Applied Economic and Social Research for providing the HILDA data set. This paper uses unit record data from the Household, Income and Labour Dynamics in Australia Survey (HILDA) conducted by the Australian Government Department of Social Services (DSS). The findings and views reported in this paper, however, are those of the authors and should not be attributed to the Australian Government, DSS, or any of DSS contractors or partners. DOI: 10.26193/OFRKRH, ADA Dataverse, V2."
Abbreviations
- ATSI
Aboriginal or Torres Strait Islander
- BMI
Body Mass Index
- GEE
Generalized Estimating Equation
- HILDA
Household, Income and Labour Dynamics in Australia Survey
- OR
Odds Ratios
- WHO
World Health Organization
References
- Al Snih S., Graham J.E., Kuo Y.F., Goodwin J.S., Markides K.S., Ottenbacher K.J. Obesity and disability: Relation among older adults living in Latin america and the caribbean. American Journal of Epidemiology. 2010;171:1282–1288. doi: 10.1093/aje/kwq087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alley D.E., Chang V.W. The changing relationship of obesity and disability, 1988-2004. Journal of the American Medical Association. 2007;298:2020–2027. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . 2018. Disability, ageing and carers, Australia: Summary of findings [Internet]https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summary-findings/latest-release#data-download [cited 3 Nov 2020]. Available: [Google Scholar]
- Australian Institute of Health and Welfare . AIHW; Canberra: 2019. People with disability in Australia 2019: In brief [Internet]. Canberra: AIHW. Cat. No. DIS 74.https://www.aihw.gov.au/reports/disability/people-with-disability-in-australia/summary Available. [Google Scholar]
- Balzi D., Lauretani F., Barchielli A., Ferrucci L., Bandinelli S., Buiatti E. Risk factors for disability in older persons over 3-year follow-up. Age and Ageing. 2009;39:92–98. doi: 10.1093/ageing/afp209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black N., Johnston D.W., Suziedelyte A. Justification bias in self-reported disability: New evidence from panel data. Journal of Health Economics. 2017;54:124–134. doi: 10.1016/j.jhealeco.2017.05.001. [DOI] [PubMed] [Google Scholar]
- Boyle P.A., Buchman A.S., Wilson R.S., Bienias J.L., Bennett D.A. Physical activity is associated with incident disability in community-based older persons. Journal of the American Geriatrics Society. 2007;55:195–201. doi: 10.1111/j.1532-5415.2007.01038.x. [DOI] [PubMed] [Google Scholar]
- Cebulla A., Zhu R. Disability, and social and economic inclusion: Who is in and out of the Australian national disability insurance scheme? Scandinavian Journal of Disability Research. 2016;18:256–268. doi: 10.1080/15017419.2015.1064026. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Disability and health overview [Internet]https://www.cdc.gov/ncbddd/disabilityandhealth/disability.html [cited 3 Nov 2020]. Available: [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Benefits of physical activity [Internet]https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm [cited 4 Nov 2020]. Available: [Google Scholar]
- Chen H., Guo X. Obesity and functional disability in elderly Americans. Journal of the American Geriatrics Society. 2008;56:689–694. doi: 10.1111/j.1532-5415.2007.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donini L.M., Merola G., Poggiogalle E., Lubrano C., Gnessi L., Mariani S. Disability, physical inactivity, and impaired health-related quality of life are not different in metabolically healthy vs. Unhealthy obese subjects. Nutrients. 2016;8:1–10. doi: 10.3390/nu8120759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freidin S., Watson N., Household W.M. Vol. 1. 2002. (Income and labour Dynamics in Australia (HILDA) survey: Wave). Melbourne. [DOI] [PubMed] [Google Scholar]
- Gorber S.C., Tremblay M., Moher D., Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obesity Reviews. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- Keramat S.A., Alam K., Gow J., Biddle S.J.H. Obesity, long-term health problems, and workplace satisfaction: A longitudinal study of Australian workers. Journal of Community Health. 2020;45:288–300. doi: 10.1007/s10900-019-00735-5. Springer US. [DOI] [PubMed] [Google Scholar]
- Keramat S.A., Alam K., Gow J., Biddle S.J.H. Gender differences in the longitudinal association between obesity, and disability with workplace absenteeism in the Australian working population. PLoS ONE15. 2020;(5):1–14. doi: 10.1371/journal.pone.0233512. e0233512, Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keramat S.A., Alam K., Gow J., Biddle S.J.H. A longitudinal exploration of the relationship between obesity , and long term health condition with presenteeism in Australian workplaces , 2006-2018. PloS One. 2020;15(8):1–17. doi: 10.1371/journal.pone.0238260. e0238260, Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keramat S.A., Alam K., Gow J., Biddle S.J.H. Impact of disadvantaged neighborhoods and lifestyle factors on adult obesity: Evidence from a 5-year cohort study in Australia. American Journal of Health Promotion. 2020 doi: 10.1177/0890117120928790. [DOI] [PubMed] [Google Scholar]
- Keramat S.A., Alam K., Gow J., Biddle S.J.H. Job-Related characteristics and obesity in Australian employees: Evidence from a longitudinal nationally representative sample. American Journal of Health Promotion. 2020 doi: 10.1177/0890117119901093. [DOI] [PubMed] [Google Scholar]
- Kim J.M., Stewart R., Glozier N., Prince M., Kim S.W., Yang S.J. Physical health, depression and cognitive function as correlates of disability in an older Korean population. International Journal of Geriatric Psychiatry. 2005;20:160–167. doi: 10.1002/gps.1266. [DOI] [PubMed] [Google Scholar]
- Kramer A.F., Colcombe S.J., McAuley E., Scalf P.E., Erickson K.I. Fitness, aging and neurocognitive function. Neurobiology of Aging. 2005;26:124–127. doi: 10.1016/j.neurobiolaging.2005.09.009. [DOI] [PubMed] [Google Scholar]
- LaMontagne A.D., Krnjacki L., Milner A., Butterworth P., Kavanagh A. Psychosocial job quality in a national sample of working Australians: A comparison of persons working with versus without disability. SSM - Popul Heal. 2016;2:175–181. doi: 10.1016/j.ssmph.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y., Park K. Does physical activity moderate the association between depressive symptoms and disability in older adults? International Journal of Geriatric Psychiatry. 2008;23:249–256. doi: 10.1002/gps.1870. [DOI] [PubMed] [Google Scholar]
- Lopez Silva C.P., Singh A., Calache H., Derbi H.A., Borromeo G.L. Association between disability status and dental attendance in Australia—a population‐based study. Community Dentistry and Oral Epidemiology. 2020 doi: 10.1111/cdoe.12571. [DOI] [PubMed] [Google Scholar]
- Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006;3:2011–2030. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maukonen M., Männistö S., Tolonen H. A comparison of measured versus self-reported anthropometrics for assessing obesity in adults: A literature review. Scandinavian Journal of Public Health. 2018;46:565–579. doi: 10.1177/1403494818761971. [DOI] [PubMed] [Google Scholar]
- Mehta N.K., Patel S.A., Ali M.K., Narayan K.M.V. Preventing disability: The influence of modifiable risk factors on state and national disability prevalence. Health Affairs. 2017;36:626–635. doi: 10.1377/hlthaff.2016.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta K.M., Yaffe K., Covinsky K.E. Cognitive impairment, depressive symptoms, and functional decline in older people. Journal of the American Geriatrics Society. 2002;50:1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penedo F.J., Dahn J.R. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Perales F., del Pozo-Cruz J., del Pozo-Cruz J., del Pozo-Cruz B. On the associations between physical activity and quality of life: Findings from an Australian nationally representative panel survey. Quality of Life Research. 2014;23:1921–1933. doi: 10.1007/s11136-014-0645-4. [DOI] [PubMed] [Google Scholar]
- Sinclair P.A., Lyness J.M., King D.A., Cox C., Caine E.D. Depression and self-reported functional status in older primary care patients. American Journal of Psychiatry. 2001;158:416–419. doi: 10.1176/appi.ajp.158.3.416. [DOI] [PubMed] [Google Scholar]
- Taş Ü., Verhagen A.P., Bierma-Zeinstra S.M.A., Hofman A., Odding E., Pols H.A.P. Incidence and risk factors of disability in the elderly: The Rotterdam Study. Preventive Medicine. 2007;44:272–278. doi: 10.1016/j.ypmed.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Tas Ü., Verhagen A.P., Bierma-Zeinstra S.M.A., Odding E., Koes B.W. Prognostic factors of disability in older people: A systematic review. British Journal of General Practice. 2007;57:319–323. [PMC free article] [PubMed] [Google Scholar]
- Wong E., Stevenson C., Backholer K., Woodward M., Shaw J.E., Peeters A. Predicting the risk of physical disability in old age using modifiable mid-life risk factors. Journal of Epidemiology & Community Health. 2015;69:70–76. doi: 10.1136/jech-2014-204456. [DOI] [PubMed] [Google Scholar]
- Wong E., Tanamas S.K., Wolfe R., Backholer K., Stevenson C., Abdullah A. The role of obesity duration on the association between obesity and risk of physical disability. Obesity. 2015;23:443–447. doi: 10.1002/oby.20936. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva, Switzerland: 2001. International classification of functionning, disability, and health (ICF) [Internet]http://www.who.int/classifications/icf/en/ [cited 5 Jan 2021]. Available: [Google Scholar]
- World Health Organization . 2015. WHO global disability action plan 2014-2021. Better health for all people with disability. [Internet]https://apps.who.int/iris/bitstream/handle/10665/199544/9789241509619_eng.pdf;jsessionid=568A630974C5747097E7E3BDB69B2B69?sequence=1 Geneva, Switzerland. Available: [Google Scholar]
- World Health Organization . 2018. Disability and health [Internet]https://www.who.int/news-room/fact-sheets/detail/disability-and-health [cited 3 Nov 2020]. Available: [Google Scholar]
- World Health Organization (WHO) 2020. Obesity and overweight [Internet]https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [cited 19 Aug 2020]. Available: [Google Scholar]
- Zoico E., Di Francesco V., Guralnik J.M., Mazzali G., Bortolani A., Guariento S. Physical disability and muscular strength in relation to obesity and different body composition indexes in a sample of healthy elderly women. International Journal of Obesity. 2004;28:234–241. doi: 10.1038/sj.ijo.0802552. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for the study were collected from the Melbourne Institute of Applied Economic and Social Research. There are some restrictions on this data, and it is not available to the public. Those interested in accessing this data should contact the Melbourne Institute of Applied Economic and Social Research, The University of Melbourne, VIC 3010, Australia.