Abstract
Since the World Health Organization launched its commission on the social determinants of health (SDOH) over a decade ago, a large body of research has proven that social determinants—defined as the conditions in which people are born, grow, live, work, and age—are significant drivers of disease risk and susceptibility within clinical care and public health systems. Unfortunately, the term has lost meaning within systems of care because of misuse and lack of context. As many disparate health outcomes remain, including higher risk of maternal mortality among Black women, a deeper understanding of the SDOH—and what forces underlie their distribution—is needed. In this article, we will expand our review of social determinants of maternal health to include the terms “structural determinants of health” and “root causes of inequities” as we assess the literature on this topic. We hypothesize that the addition of structural determinants and root causes will identify racism as a cause of inequities in maternal health outcomes, as many of the social and political structures and policies in the United States were born out of racism, classism, and gender oppression. We will conclude with proposed practice and policy solutions to end inequities in maternal health outcomes.
Keywords: Black maternal health, social determinants of health, structural determinants of health, health equity, maternal mortality, women's health
Introduction
Maternal mortality is a marker of national health and well-being. In the United States, unacceptably high maternal mortality persists, and our dismal ranking relative to other developed nations1 is further marred by vast social inequities in the burden of loss. Black women, in particular, experience maternal morbidity and mortality ratios several times higher than other groups.2 Efforts to understand this inequity have focused on individual behaviors and socioeconomic conditions, typically adopting narratives of personal responsibility and blame.
Meanwhile, the search for biological markers of susceptibility in socially defined groups continues to perpetuate the misconception that race is a risk factor for adverse maternal health outcomes. These misguided approaches have failed to identify and remediate the fundamental causes of maternal mortality and maternal health inequities.
More than a decade ago, the World Health Organization launched its commission on the social determinants of health (SDOH) to foster a global movement to address the conditions in which people are born, grow, live, work, and age.3 Since that time, a large body of research continues to demonstrate the role of SDOH as significant drivers of population health inequities. Unfortunately, however, the term has lost meaning within systems of care because of misuse and lack of context, and large social gradients in health and clinical outcomes persist.
Taking social factors into account is essential to improving both primary and secondary prevention and the treatment of acute and chronic illness because social contexts affect the delivery and outcomes of health care. How health care systems can integrate social care (i.e., services that address health-related social risk factors and social needs) into clinical practice and what types of infrastructure are needed to facilitate such activities are major areas in development.
A recent report from the National Academies of Science, Engineering, and Medicine (NASEM)4 identified five essential activities for the integration of social needs into health care: (1) awareness, (2) adjustment, (3) assistance, (4) alignment, and (5) advocacy. Given the siloing of SDOH from clinical determinants, the NASEM report provides important guidance about how to address social needs in the context of health care service provision. First, awareness indicates the need for screening for SDOH, and adjustment indicates the need to tailor services to resolve the negative determinants and support the positive. Next, assistance and alignment mean both strengthening social supports and redesigning health services to meet the needs of the public. Finally, advocacy includes making use of local, state, and federal governments to support public health efforts in addressing SDOH consistent with clinical care within the context of the communities where the care is provided.
This approach is useful not only for understanding SDOH, but also in moving even farther upstream toward identifying the structural determinants of health: cultural norms, policies, institutions, and practices that define the distribution (or maldistribution) of SDOH. These structures and systems date back to the founding of this nation and its economy on principles of racial, class, and gender hierarchy.5–11 They shape the distribution of power and resources across the population, engendering health inequities along racial, class, and gender lines and intersections.
The purpose of this review is to describe the current state of maternal health in the United States, using Black maternal health as an exemplar to understand the path toward eradication of health inequities. We highlight emergent theoretical frameworks for broader explorations of SDOH and include the terms “structural determinants of health” and “root causes of inequities” as we assess the current understanding of this topic. We conclude by emphasizing existing policy and practice solutions to promote maternal health and advance maternal health equity.
Theoretical Considerations Specific to the U.S. Context
When considering maternal health, application of the reproductive justice framework—a framework created by women of color—provides us with some guidance for acknowledging and addressing structural determinants of health inequities.12 Reproductive justice refers to the human right to personal bodily autonomy not to have a child, to have a child, and to raise a child in a safe and sustainable community. This framework calls for program and policy recommendations that dismantle a belief in a hierarchy of human value.11,13 It shifts accountability from individuals to systems by acknowledging that the context of people's lives determines their health and that blaming individuals for having poor health or crediting them for good health is therefore inappropriate.14
Individuals are unlikely to be able to control directly many of the upstream determinants of health: governance, policy, and cultural or societal norms and values that shape who has access to health-promoting resources and opportunities and who does not. Beginning from this vantage point allows an understanding of why social determinants are born from structural determinants and cannot be addressed separately. In other words, no matter how empowered, knowledgeable, or willing someone is to change their behavior, they may not be able to do so because of structural determinants of health inequities.
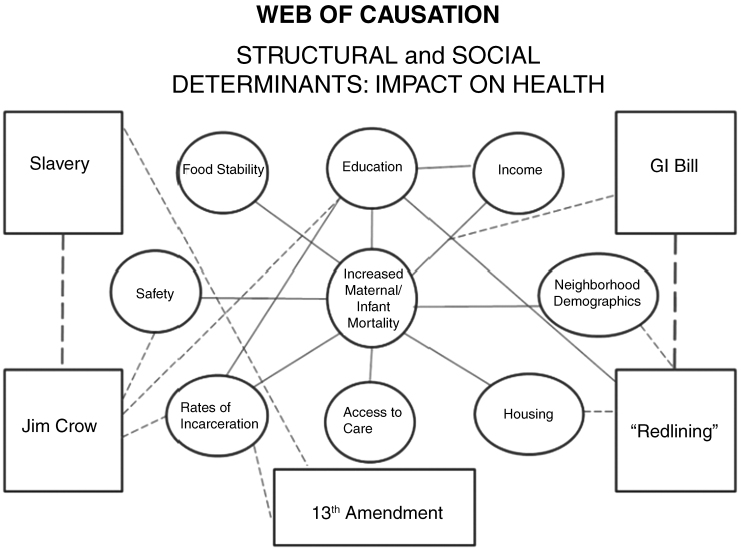
Recent efforts to identify root causes of maternal health inequity have highlighted how a focus on individuals and their experienced risk factors—clinical, behavioral, and even social determinants—reflect actions of the individual rather than the historical, systemic, structural, and political forces that created them. Developed by Roach in 2016, the Restoring Our Own Through Transformation (ROOTT) theoretical framework elucidates the web of causation between structural and SDOH and wellness (Fig. 1).15 This framework identifies the social determinants of Black maternal health—education, income, neighborhood characteristics, housing, access to care, safety, and food stability—and how their availability to Black families has been dictated by the very structure of American society from the time of slavery.
FIG. 1.
ROOTT Theoretical Framework.15 This figure depicts the theoretical framework developed by ROOTT15 used to identify structural and social determinants of maternal and infant mortality in the United States. Structural determinants are those depicted in boxes connected by dashed lines, which in turn shape the distribution of social determinants (those depicted in circles and connected by solid lines). The multiple and interconnected pathways between structural and social determinants lead to increased maternal and infant mortality rates and socially defined inequities in these outcomes. ROOTT, Restoring Our Own Through Transformation.
Structural racism and institutional policies and practices—Jim Crow, the GI Bill, “redlining” (home mortgage denial on the basis of race and government-backed disinvestment in non-White neighborhoods), mass incarceration—are historically based features of an overtly oppressive U.S. society that have endured and adapted over time and continue to shape contemporary access to health-promoting resources and opportunities necessary for optimal Black maternal and infant health outcomes.16–19 Work that seeks to further elucidate the web of causation between the structural and SDOH for Black women and other disenfranchised groups has the potential to facilitate the identification of interventions and policies that can remediate and eliminate inequalities in health across the population.
Health Systems Considerations as Structural Determinants of Maternal Health
Health policy researchers have identified four key features of the U.S. health care system that result in a health disadvantage for individuals.20 First, the U.S. health system suffers from financial barriers to care, a shortage of primary care providers, and important gaps in quality of care. Second, many Americans live in structured environments that produce a higher prevalence of certain unhealthy behaviors than in other developed countries (consumption of more calories per capita, higher rates of prescription and illicit drug misuse, more traffic accidents involving alcohol). Third, relative to other developed countries, the United States lags in educational attainment, and vast income inequality has resulted in a concentration of resources among a small segment of the population, with adverse implications for population health and health inequities, including maternal and infant mortality.21,22 Fourth, Americans live in a built environment that does not encourage physical activity and live in more racially segregated communities (largely a result of redlining).23
Overlaying these features with the upward trend in maternal mortality and morbidity,2 one may infer that diverse pregnant women may have encountered barriers to well-woman care, which may lead them to delay getting care when they need it the most. The shortage of primary care providers (e.g., nurse midwives, obstetricians, nurses) puts diverse women at risk for the delay or omission of two essential activities during the perinatal period: seeking care at an early stage in pregnancy and building trust with providers. This risk is amplified for women who have preexisting conditions when they become pregnant or who develop comorbidities during the perinatal period. This combination of multilevel factors increases the risk of maternal morbidity and mortality and reflects more fundamental causes and disinvestments, such as (1) public health departments that no longer provide direct medical care24,25; (2) the shortage of obstetricians, nurse midwives, and well-women nurses in low-income communities that are predominantly racially and ethnically diverse26; and (3) data collection efforts that vary across county and states lines.24,25
Overview of Existing Policies and Practices to Address Structural and Social Determinants of Maternal Health
Addressing the deeply rooted causes of maternal health inequities will require multiple and sustained interventions at every level. Passage of evidence-based policies that uphold the tenets of reproductive justice may begin to reduce the disproportionate experience of adverse maternal health outcomes among socially marginalized groups. In this study, we highlight several policy and practice solutions that may help to advance health equity, defined as “assurance of the conditions for optimal health for all people by valuing all populations equally, recognizing and rectifying historical injustices, and providing resources according to need.”27
Paid family leave
A lack of paid family leave is considered a public health crisis in the U.S. context.28 Previous studies have shown that time off after birth to recover and transition without worrying about money is key to maternal and infant health.29 The United States is one of only two countries in the world, along with Papua New Guinea, that does not have a national policy guaranteeing paid leave to new parents.30 The 1993 Family Medical and Leave Act provides for unpaid leave, but almost half of U.S. workers are not eligible, and many cannot afford time off without pay.17
Around the rest of the globe, paid maternity leave is standard practice, averaging 18 weeks and extending beyond 6 months in many developed countries. In addition, a systematic review of the empiric literature on the impact of parental and medical leave policies on socioeconomic and health outcomes in Organization for Economic Cooperation and Development countries concluded that (1) reforms that have increased the duration of job-protected paid parental leave have improved women's economic outcomes; (2) access to paid parental leave around the period of childbirth appears to reduce rates of infant mortality, with breastfeeding representing one possible mechanism; and (3) more generous paid leave entitlement in countries that offer unpaid or short duration of paid leave could help families strike a balance between the competing demands of earning income and focusing on personal and family well-being.29
Health insurance coverage and scope
Ensuring access to affordable and comprehensive health care across a woman's life course is critically important to assuring optimal maternal health outcomes if and when she chooses to reproduce. Substantial new research shows significant improvements in access to health coverage for women of childbearing age achieved through the adoption of the Patient Protection and Affordable Care Act's (ACA) provisions for expanded Medicaid eligibility to adults earning up to 138% of the federal poverty level.31 A review of emergent research found that states that expanded Medicaid eligibility improved the health of women of childbearing age by increasing access to preventive care; reducing adverse health outcomes before, during, and after pregnancies; and reducing incidence of maternal mortality.31 Moreover, expansion states experienced significant reductions in Black–White disparities in adverse birth outcomes shortly after the policy went into effect32 and a 50% reduction in infant mortality, with the greatest declines among Black/African American infants.33
To date, 36 states and the District of Columbia have adopted Medicaid expansion under the ACA and offer low-income women the opportunity to continue their pregnancy-related Medicaid coverage after the 60-day postpartum period.34 In the 14 states that have not adopted Medicaid expansion, women must requalify for Medicaid postpartum to stay in the program. However, many women in these states become uninsured after pregnancy-related coverage ends 60 days postpartum because their income is too high to qualify for Medicaid, even though their infants are eligible for their first year of life. Given the impact and large role of Medicaid in maternal health outcomes, financing coverage for the full year after Medicaid birth may help address the gaps that women suffer in nonexpanded states.
Too often, women struggle in systems of care that are not designed to accommodate their needs through the fourth trimester—the 12 weeks following childbirth, during which women recover from birth and transition to nurture and care for their infants and themselves.35 Since most maternal mortality occurs in the postpartum period,36 it is imperative that women and their supports have the education to recognize and the ability to act on concerning or emergency symptoms following discharge to home.28 Extending Medicaid through at least 12 months would ensure continuous access to services. Currently, fourth trimester care coverage is limited to a single visit for women who delivered vaginally and two visits for those who had a cesarean birth.
Such approaches as bundling care for mother and child for the first 3 months postpartum and extending parental Medicaid coverage may support integrated care for mothers and infants to address their holistic needs. This could include such resources as doulas, community health workers, and midwives to ensure comprehensive support. In most states where Black women give birth, they do not have access to nurse midwives who are well integrated into the perinatal health care system.26,37 Moreover, to date only two states (Minnesota and Oregon) provide doula services as part of their Medicaid coverage38; a third (California) has proposed a 14-county pilot program.39
Respectful, culturally appropriate care
Although health insurance coverage is an important component of ensuring access to care, health policy experts suggest that health disparities have persisted even when there have been modest improvements in access to health care.25 Coupled with access is the necessity to deliver high-quality maternity care that acknowledges and respects the cultural experiences and contexts in which women live. “Centering at the margins” is an elevated approach to patient-centered care that requires providers to engage with the experience of disenfranchised groups and to acknowledge the role of society and history in influencing both their own understanding of their patient and their patient's understanding of them.40 Infusing a focus on structural determinants of health and health inequities into medical education and clinical training (structural competency) may facilitate cross-cultural understanding of individual patients and shift the way providers recognize the social and economic forces that produce health outcomes.41 Finally, national organizations, such as the Black Mamas Matter Alliance, are advancing perinatal health equity by promoting the uptake of ethical guidelines for perinatal care for Black women.42
Invest in communities
Stepping outside of the acute care setting, it is essential to increase investments in comprehensive community-oriented primary care for diverse women of reproductive age in a variety of settings (e.g., midwifery maternity centers, nurse practitioner practices, maternal and child clinics, and outpatient clinics of hospitals). Also important are tax incentives that build public infrastructure for diverse women of reproductive age and align with the values of taxpayers, including the provision of affordable and quality health care to all Americans.34 This innovative strategy may include tax credits to colocate maternity services and pediatrics clinics within a primary care setting so women may seek medical care for their chronic condition at the same time they are getting their prenatal care.
At the state level, income/wealth inequality may be reduced by supporting higher living wages and asset-generating opportunities to buttress young, low-income families, as well as passing progressive tax systems to fund robust public education, sick leave, family leave, and child care systems. Upholding assurance and availability of comprehensive reproductive health care services for all women at both state and federal levels is important for reversing the upward trend in mortality and broadening of inequities. A recent study of state-level factors linked to maternal mortality found that both fiscal and legislative restrictions on access to family planning and reproductive health services contributed to increased incidence.43 At the national level, a maternity health tracking system that sets national standards for data collection and the development of a unified person-centric electronic health record may help to identify areas of improvement for underperforming maternity care providers in a variety of health care settings.
Conclusion
Identifying the root causes of maternal mortality, remediating factors that may be contributing to its increasing incidence, and eliminating the disproportionate burden of loss among families of color is an imperative for this nation's future. The immense economic costs of maternal morbidity and mortality may justify action among those unmoved by population health promotion and equity alone. Data suggest the economic burden of maternal morbidity and mortality is billions of dollars each year.44 Beyond the 700–900 women who suffer from pregnancy complications that result in death, an additional 60,000 women45 suffer pregnancy-related complications that are near fatal. In particular, the cost of caring for women with preeclampsia is more than $1 billion alone,46 and the prevailing total annual cost of maternity care exceeds $60 billion.47
As the scientific community continues to identify the structural determinants of maternal health inequities and recommend policies to address them, improvements in equitable access to the SDOH and reduction of health inequities are likely to follow. This move to advance upstream structural solutions is critical for families to thrive. By defining the root causes of health inequities, we can move the focus of intervention away from individual blame and misguided theories of the biological basis of race and ethnicity. The shared understanding of how inequities in outcomes based upon race, class, and gender are created by policy and practice is pivotal to ending these inequities. It is an economic, social, and moral imperative that we center the experience of the communities that are the most impacted when we look for solutions, because they hold the answers to improving delivery of respectful care and ensuring reproductive health and well-being for all.
Disclaimer
Any opinions or recommendations expressed in this publication are those of the authors and do not necessarily reflect the views of the National Institutes of Health or the U.S. Department of Health and Human Services.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Dr. Wallace's role in this research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, award numbers R01HD092653 and R01HD096070.
References
- 1. Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:980–1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoyert DL, Miniño AM. Maternal mortality in the United States: Changes in coding, publication, and data release, 2018. Natl Vital Stat Rep 2020;69:1–18 [PubMed] [Google Scholar]
- 3. World Health Organization. Social determinants of health. Available at: https://www.who.int/social_determinants/sdh_definition/en Accessed March10, 2020
- 4. National Academies of Sciences, Engineering, and Medicine. Integrating social care into the delivery of health care: Moving upstream to improve the nation's health. Washington, DC: The National Academies Press. 2019 [PubMed] [Google Scholar]
- 5. Roberts DE. Killing the Black body: Race, reproduction, and the meaning of liberty, 1st ed. New York: Pantheon Books, 1997 [Google Scholar]
- 6. Black Women Scholars, Research Working Group for Black Mamas Matter Alliance. Black maternal health research re-envisioned: Best practices for the conduct of research with, for, and by Black mamas. Harvard Policy and Law Review 2020;14,2
- 7. Williams DR, Lawrence JA, Davis BA. Racism and health: Evidence and needed research. Annu Rev Public Health 2019;40:105–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Washington HA. Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present, 1st ed. New York, NY: Doubleday, 2006 [Google Scholar]
- 9. Francis MM. The price of civil rights: Black lives, white funding, and movement capture. Law Soc Rev 2019;53:275–309 [Google Scholar]
- 10. Smith SL. Sick and tired of being sick and tired: Black women's health activism in America, 1890–1950. Philadelphia, PA: University of Pennsylvania Press, 1995 [Google Scholar]
- 11. Kendi IX. Stamped from the beginning: The definitive history of racist ideas in America. New York, NY: Nation Books, 2016 [Google Scholar]
- 12. Ross L, Solinger R. Reproductive justice: An introduction. Oakland, CA: University of California Press, 2017 [Google Scholar]
- 13. Crear-Perry J. You can't have quality without equity, 2020. Available at: www.ihi.org/communities/blogs/you-can-t-have-quality-without-equity Accessed March23, 2020
- 14. Scott KA, Britton L, McLemore MR. The ethics of perinatal care for Black women: Dismantling the structural racism in “mother blame” narratives. J Perinat Neonatal Nurs 2019;33:108–115 [DOI] [PubMed] [Google Scholar]
- 15. Roach J. ROOTT's theoretical framework of the web of causation between structural and social determinants of health and wellness—2016. Restoring Our Own Through Transformation (ROOTT), 2016. Available at: https://www.roottrj.org/policy-advocacy Accessed March10, 2020
- 16. Dawson MC, Francis MM. Black politics and the neoliberal racial order. Public Cult 2016;78:23–62 [Google Scholar]
- 17. Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017;389:1453–1463 [DOI] [PubMed] [Google Scholar]
- 18. Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small-for-gestational-age birth. Am J Public Health 2015;105:1681–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wallace M, Crear-Perry J, Richardson L, Tarver M, Theall K. Separate and unequal: Structural racism and infant mortality in the US. Health Place 2017;45:140–144 [DOI] [PubMed] [Google Scholar]
- 20. National Research Council. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press, 2013 [PubMed] [Google Scholar]
- 21. Vilda D, Wallace M, Dyer L, Harville E, Theall K. Income inequality and racial disparities in pregnancy-related mortality in the U.S. SSM Popul Health 2019;9:100477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Siddiqi A, Jones MK, Bruce DJ, Erwin PC. Do racial inequities in infant mortality correspond to variations in societal conditions? A study of state-level income inequality in the U.S., 1992–2007. Soc Sci Med 2016;164:49–58 [DOI] [PubMed] [Google Scholar]
- 23. Massey D, Denton N. American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press, 1993 [Google Scholar]
- 24. Howell EA, Ahmed ZN. Eight steps for narrowing the maternal health disparity gap: Step-by-step plan to reduce racial and ethnic disparities in care. Contemp Ob Gyn 2019;64:30–36 [PMC free article] [PubMed] [Google Scholar]
- 25. Woolf SH, Braveman P. Where health disparities begin: The role of social and economic determinants—And why current policies may make matters worse. Health Aff (Millwood) 2011;30:1852–1859 [DOI] [PubMed] [Google Scholar]
- 26. Vedam S, Stoll K, Taiwo TK, et al. The Giving Voice to Mothers study: Inequity and mistreatment during pregnancy and childbirth in the United States. Reprod Health 2019;16:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jones CP. Systems of power, axes of inequity: Parallels, intersections, braiding the strands. Med Care 2014;52(Suppl 3):S71–S75 [DOI] [PubMed] [Google Scholar]
- 28. Tully KP, Stuebe AM, Verbiest SB. The fourth trimester: A critical transition period with unmet maternal health needs. Am J Obstet Gynecol 2017;217:37–41 [DOI] [PubMed] [Google Scholar]
- 29. Nandi A, Jahagirdar D, Dimitris MC, et al. The impact of parental and medical leave policies on socioeconomic and health outcomes in OECD Countries: A systematic review of the empirical literature. Milbank Q 2018;96:434–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Organization for Economic Co-operation and Development. SIGI 2019 Global report: Transforming challenges into opportunities; social institutions and gender index. Paris, France: OECD Publishing, 2019 [Google Scholar]
- 31. Searing A, Ross DC. Medicaid expansion fills gaps in maternal health coverage leading to healthier mothers and babies. Washington, DC: Georgetown University Health Policy Institute, Center for Children and Families, 2019. Available at: https://ccf.georgetown.edu/2019/05/09/medicaid-expansion-fills-gaps-in-maternal-health-coverage-leading-to-healthier-mothers-and-babies Accessed March10, 2020
- 32. Brown CC, Moore JE, Felix HC, et al. Association of state Medicaid expansion status with low birth weight and preterm birth. JAMA 2019;321:1598–1609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bhatt CB, Beck-Sague CM. Medicaid expansion and infant mortality in the United States. Am J Public Health 2018;108:565–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ranji U, Gomez I, Salganicoff A. Expanding postpartum Medicaid coverage. Women's Health Policy Issue Brief, 2019. Available at: https://www.kff.org/womens-health-policy/issue-brief/expanding-postpartum-medicaid-coverage Accessed May14, 2020
- 35. Stuebe A, Moore JE, Mittal P, Reddy L, Low LK, Brown H. Extending Medicaid coverage for postpartum moms. Health Affairs Blog, 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190501.254675/full Accessed May14, 2020
- 36. Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011–2013. Obstet Gynecol 2017;130:366–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vedam S, Stoll K, MacDorman M, et al. Mapping integration of midwives across the United States: Impact on access, equity, and outcomes. PLoS One 2018;13:e0192523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Association of State and Territorial Health Officials. State policy approaches to incorporating doula services into maternal care, 2018. Available at: https://www.astho.org/StatePublicHealth/State-Policy-Approaches-to-Incorporating-Doula-Services-into-Maternal-Care/08-09-18 Accessed March23, 2020
- 39. National Health Law Program. Doula Medicaid project, 2020. Available at: https://healthlaw.org/doulamedicaidproject Accessed March23, 2020
- 40. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting Black lives—The role of health professionals. N Engl J Med 2016;375:2113–2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014;103:126–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Black Mamas Matter Alliance. Setting the standard for holistic care of and for Black women, 2018. Available at: http://blackmamasmatter.org/wp-content/uploads/2018/04/BMMA_BlackPaper_April-2018.pdf Accessed March23, 2020
- 43. Hawkins SS, Ghiani M, Harper S, Baum CF, Kaufman JS. Impact of state-level changes on maternal mortality: A population-based, quasi-experimental study. Am J Prev Med 2020;58:165–174 [DOI] [PubMed] [Google Scholar]
- 44. Moran PS, Wuytack F, Turner M, et al. Economic burden of maternal morbidity—A systematic review of cost-of-illness studies. PLoS One 2020;15:e0227377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ellison K, Martin N. Lost mothers: Maternal mortality in the U.S.—Nearly dying in childbirth: Why preventable complication are growing in U.S., 2017. Available at: https://www.npr.org/2017/12/22/572298802/nearly-dying-in-childbirth-why-preventable-complications-are-growing-in-u-s Accessed March23, 2020
- 46. Howell EA, Zeitlin J. Quality of care and disparities in obstetrics. Obstet Gynecol Clin North Am 2017;44:13–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Agrawl P. Maternal mortality and morbidity in the United States of America. Bull World Health Organ 2015;93:135. [DOI] [PMC free article] [PubMed] [Google Scholar]