Abstract
Background: Lymphedema is a condition characterized by dysfunction of the lymphatic system resulting in chronic, progressive soft tissue edema that can negatively impact individuals' function, self-image, and quality of life. Understanding of the disease process has evolved significantly in the past two decades with advances in diagnostic modalities and surgical techniques revolutionizing prior treatment algorithms.
Methods and Results: We reviewed our current approach at the University of Southern California to improving outcomes in lymphedema treatment. Given the complexity of this medical condition, patients are best served by a multidisciplinary approach. At our institution, this involves a collaborative effort between bench researchers, lymphatic therapists, medical physicians, and lymphedema surgeons. Basic science and translational research provide further understanding into the underlying mechanisms of lymphangiogenesis and the possibility for potential therapeutic interventions. Our surgical algorithms require patients to undergo a thorough diagnostic evaluation and consultation with certified lymphatic therapists prior to undergoing either physiologic or debulking operations. Patients are followed clinically following any interventions. Further community outreach and education is carried out in order to improve upon early diagnosis and symptom recognition.
Conclusions: Optimizing lymphedema care requires a collaborative interplay between researchers, physicians, and therapists. Additionally, patient and provider education on early disease recognition and treatment options is an equally critical aspect of improving patient outcomes.
Keywords: lymphedema, center of excellence, VLNT, LVB
Introduction
Lymphedema is a condition characterized by dysfunction of the lymphatic system resulting in chronic progressive soft tissue edema. Long-standing disease leads to irreversible swelling, fibrosis, and fatty deposition. Advanced lymphedema is both disfiguring and debilitating contributing toward impaired quality of life for afflicted individuals.1–4 In the United States, lymphedema is most commonly a result of iatrogenic causes related to the treatment of oncologic disease. Breast cancer patients, in particular, have been found to have an incidence of as high as 47%5 as the number of lymph nodes removed increases and additional adjunctive therapies such as radiation are applied.
Unfortunately, the management of lymphedema been a long neglected and overlooked area of medicine.6 Much of this is due to the lack of sophisticated diagnostic capabilities and few effective treatment modalities. However, as our understanding of the nature of this disease process has improved for the past two decades, the diagnostic and treatment paradigms have shifted. We now know enough about the intricacies of lymphatic disease processes to make strong evidence-based recommendations on prevention, diagnosis, therapeutic management, and most revolutionarily, incorporate physiologic surgical treatment options to mitigate advanced progression of the disease.
In 2018, the lymphatic education and research network (LE&RN) developed standards for creating centers of excellence (COE) in the diagnosis and treatment of lymphatic disease. Keck Medical Center of USC is one of the eight LE&RN Comprehensive COE in the United States. As a COE, we view it as our obligation to provide comprehensive multidisciplinary clinical care and services to individuals affected by lymphedema while simultaneously contributing toward a better understanding of the disease process through basic, translational, and clinical research. In addition, as the management of lymphedema remains poorly understood by the lay population, we remain committed toward the active promotion of improved education and for lymphatic disease management for patients and providers. The purpose of this article is to review the interplay between research, education, and clinical services in the approach to lymphedema management, while outlining the unique properties of our multidisciplinary system at Keck Medical Center.
Clinical: Recent Updates in Lymphedema Therapy
From the inception of our lymphedema program, we have been dedicated toward a multidisciplinary approach with frequent collaboration between various specialties, including plastic surgery, surgical oncology, breast surgery, vascular surgery, radiology, and certified lymphedema therapists. Each specialty brings their own expertise and holds a unique role in our treatment algorithms aimed producing optimal patient outcomes.
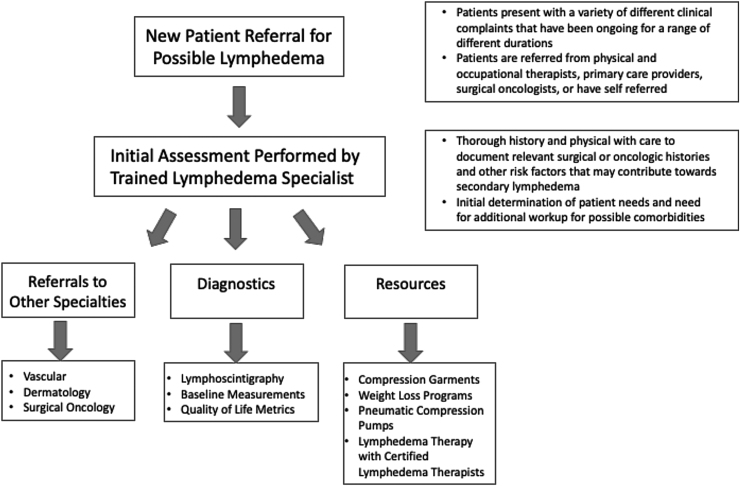
Patients who present to surgical lymphedema clinics are typically referred from a variety of different sources, including outside hospitals, primary care providers, occupational therapists, and other nonphysician health care providers.7 In addition, many patients independently seek out these clinics as a result of their own research. This results in a significant range of presenting symptoms and initial diagnoses, with some patients having incorrectly received a previous diagnosis of lymphedema.7,8 These patients present with great variations in their prior disease workup, history of any previous therapeutic measures, and have significant differences in the knowledge of their underlying disease process and treatment expectations.9
Thus, we follow a standard protocol for all new lymphedema referrals (Fig. 1). During initial consultation, all patients undergo a thorough history and physical, with particular focus on prior oncologic history and treatments, surgical histories, and additional risk factors for the development of lymphedema. Patients are screened for any comorbidities and/or possible alternative diagnoses that may explain their symptoms and referred to other specialists where appropriate. Obesity has been shown to be a major risk factor for developing secondary lymphedema.10,11 As such, weight loss resources and bariatric programs are provided for overweight and obese patients during this initial appointment. Diagnostic imaging and tests are ordered to allow for accurate diagnosis and to aid in treatment of lymphedema.
FIG. 1.
New patient referral for lymphedema.
Lymphoscintigraphy, the current gold standard, is 92% sensitive and 100% specific for the diagnosis of lymphedema.12 This modality provides information regarding both lymphatic anatomy as well as lymphatic function.13 All patients at our institution are referred for lymphoscintigraphy as part of their initial workup.
After this initial assessment and the initiation of conservative measures, patients are seen by our lymphedema surgeons (Fig. 2). Diagnostic tests are reviewed, and an appropriate treatment plan is determined. Treatment plans are tailored to the individual and based on International Society of Lymphology (ISL) classification14 in addition to objective measurements of lymphatic function and subjective quality of life metrics.
FIG. 2.
Determination of treatment plan.
For subclinical lymphedema, we recommend conservative therapies, including compression, and continued close monitoring. Patients are seen in follow-up at our lymphedema clinic and with their lymphedema therapists.
We begin to consider physiologic surgical options such as lymphovenous bypass (LVB) and vascularized lymph node transfers (VLNTs) for ISL Grades 1 and 2. LVBs involve creating a connection between lymphatic vessels to adjacent venules to redirect lymphatic fluid and bypass any areas of lymphatic obstruction. ICG fluorescence allows for the visualization and identification of these channels during the operation.15–18 Several studies have demonstrated the effectiveness in this technique for early-stage lymphedema.19–21 Patients require some degree of functionality and patent lymphatic vessels in their lymphatic system to have success with LVBs.
For patients with more advanced disease, we may consider a VLNT. This involves harvesting vascularized lymph nodes from one area of the body and transferring them to the afflicted extremity. There are two proposed mechanisms through which this achieves improved lymphatic drainage. There is evidence to support that the transferred lymph node induces lymphangiogenesis at the recipient site.22 Alternative hypotheses suggest that the lymph node acts as a “pump” and is able to wick the surrounding interstitial lymph fluid and then dispel it into its efferent venous circulation.23,24
As the disease progresses, the effectiveness of these physiologic options decrease; for those patients, we would consider reductive debulking operations to improve quality of life. Suction-assisted liposuction may be used as an adjunctive debulking method, performed in concert with LVBs and/or VLNTs. More extreme and morbid measures, such as the Charles procedure, are reserved for individuals with significant physical impairment due to their lymphedema. Throughout these surgical procedures, we recommend that patients continue to work closely with their lymphatic therapists.
Collaboration: Improvements in Care Through Interdisciplinary Partnerships
Studies have proven that early identification and intervention improves outcomes and slows the progression to advanced disease.25 We have directed efforts at identifying individuals who are at high risk for the development of lymphedema. This has led to close collaboration with our breast surgery, pelvic surgery, and occupational therapy (OT) colleagues. When patients are seen in the breast clinic before undergoing their oncologic resection, they are provided with ample resources and educational material on lymphedema. They are measured for baseline measurements and counseled on behavioral actions they can take to mitigate the effects of lymphedema, including eating a healthy diet, engaging in exercise, and avoiding risk factors. They are provided with education on early signs and symptoms that might indicate a lymphedema workup. During their acute care admission, patients are seen promptly postsurgically by an occupational therapist to assess their functional status, initiate an exercise program, provide strategies for safely completing their activities of daily living, and to further address any questions or concerns related to lymphedema. Should a patient begin to develop early signs of lymphedema postoperatively, a referral to our lymphedema clinic is promptly placed to allow for a seamless and timely transition from acute care to outpatient care. There the patient works closely with the occupational therapist and is monitored for progression of disease.
The gold standard for conservative treatment is commonly referred to as complete decongestive therapy (CDT). CDT consists of two phases: the intensive (or decongestive) phase and the management phase. During the intensive phase, a certified lymphedema therapist works closely with the patient to aggressively decongest the affected area through manual lymphatic drainage (MLD), compression therapy, skin care, and tailored remedial exercises. The therapist also provides education on the disease course, lifestyle modifications, strategies for enhancing activities of daily living, functional activities, and mobility. Lymphedema often has significant impacts on quality of life, self-image, intimacy, and psychosocial factors; therefore, these areas may also be addressed by a qualified therapist. Once the affected area is decongested or approaches a plateau, the patient is transitioned into the maintenance phase. In this phase, patients self-manage through use of compression garments, upkeep of skin care, follow-through of remedial exercises, self-MLD and/or use of a pneumatic compression pump. For some patients, a course of CDT may be a means to an end; for others, conservative therapy will be the end of their treatment if they do not pursue surgical options.
If patients choose to pursue lymphatic surgeries, candidates are encouraged to complete a course of preoperative CDT to allow for optimal decongestion of the affected area before surgery. After surgery, patients are then encouraged to follow up with postoperative CDT to further decongest and manage any potential postsurgical edema. This consistent treatment throughout the continuum of care primes patients for optimal surgical outcomes. In addition, constant communication is maintained between our plastic surgery team and OT team to ensure continuity of care.
For our approach to be effective, we rely on frequent collaboration between various specialties. To help facilitate this, we hold monthly meetings where clinical cases are discussed, and knowledge can be shared.
Research: The Main Drive for Better Treatments
Our institution is committed to a multifaceted approach to lymphedema research. Our dedicated basic science laboratories have explored how various signal pathways control lymphatic development and differentiation with the objective of gaining a better understanding of the mechanisms of physiologic and pathologic lymphangiogenesis.26 For example, recent study has shed light into the mechanism by which lymph fluid laminar flow regulates lymphatic vessel regeneration.27 Ultimately, these efforts have laid the groundwork for the development of translational research models that take advantage of transgenic mutant animals, which permit real-time in vivo florescent identification and imaging of lymphatic vasculature during development, postnatal lymphangiogenesis, and in response to lymphatic injury.28 Using these established models, we can more precisely explore the impact of therapeutic lymphatic interventions such as ischemia in the setting of VLNT.29 Finally, research at our institution has successfully identified retinoic acid as an FDA-approved therapeutic agent that may be repurposed for the novel indication of lymphedema prevention.30–33
Beyond the laboratory, our clinical practice has produced several high-impact publications that cover the impact of surgical physiologic treatment modalities. The goal of this research is to produce more streamlined patient care algorithms based on evidence-based objective metrics and patient-reported outcomes to improve overall quality of life for individuals suffering from lymphedema.
Education: Spreading Knowledge Throughout the Medical and Patient Communities
As previously mentioned, one of the challenges with effectively treating lymphedema is the lack of knowledge and understanding about this disease process, its diagnosis, and treatment options by both the lay public and members of the health care community who do not routinely encounter these patients. Studies have demonstrated a direct correlation between improved patient understanding of the disease with improved adherence to therapy and improved outcomes.7
Beyond better educating our patients, we also strive to better educate health care practitioners within the community, as earlier diagnosis and symptom recognition can help direct patients to the appropriate resources in a timelier manner, before disease progression as advanced. To bridge this knowledge gap, Keck hosts an annual multidisciplinary approach to lymphedema symposium. Regional primary care physicians, mid-level providers, and therapists are invited and encouraged to participate. A large focus of the symposium is on improved diagnosis and disease management. Speakers include physicians of different specialties as well as certified lymphedema therapists. This forum brings together all aspects of lymphedema care. This includes basic and translational research updates, where scientists and researchers can discuss the latest innovations and breakthroughs within the field.
Breakout sessions aimed at patient education are a critical part of community outreach and education during the event. Through these meetings we hope to foster an environment of community and collaboration among the researchers, physicians, therapists, and patients themselves.
In addition to the annual lymphedema symposium, the goal of the USC Affiliate Network is to facilitate regional collaboration for those outside of the USC network. Through the USC affiliate Network, we host a biannual dinner meeting with a significant education and networking component. Pertinent topics discussed include best practices in lymphedema diagnosis and management, new ideas and innovations, and review of challenging case reviews. These meetings provide outreach to out-of-network primary care physicians and mid-level providers who may encounter patients with lymphedema in their clinical practice. By promoting improved education regarding early lymphedema diagnosis and management, we hope to elevate the overall level of care individuals suffering from lymphedema will receive.
Conclusion
The management of lymphedema remains challenging and complex, requiring a multidisciplinary approach to optimize care. Collaboration between researchers and practitioners continue to drive forward new and innovative therapies and interventions. Advancements in the field are progressing at a rapid rate. Within the past two decades, improvements in diagnostic and treatment capabilities have shifted the previously accepted disease management paradigms. We now know that early diagnosis and early intervention are correlated with better patient outcomes and improved quality of life. In addition, studies suggest that the application of newer surgical techniques have the potential to slow disease progression. The field of lymphedema is evolving. To improve the overall level of care for lymphedema patients, lymphedema providers are tasked with educating the rest of the medical community on these advances.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received.
References
- 1. Teo I, Novy DM, Chang DW, Cox MG, Fingeret MC. Examining pain, body image, and depressive symptoms in patients with lymphedema secondary to breast cancer. Psychooncology 2015; 24:1377–1383 [DOI] [PubMed] [Google Scholar]
- 2. Stolldorf DP, Dietrich MS, Ridner SH. Symptom frequency, intensity, and distress in patients with lower limb lymphedema. Lymphat Res Biol 2016; 14:78–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dunberger G, Lindquist H, Waldenström AC, Nyberg T, Steineck G, Åvall-Lundqvist E. Lower limb lymphedema in gynecological cancer survivors—Effect on daily life functioning. Support Care Cancer 2013; 21:3063–3070 [DOI] [PubMed] [Google Scholar]
- 4. Fu MR, Kang Y. Psychosocial impact of living with cancer-related lymphedema. Semin Oncol Nurs 2013; 29:50–60 [DOI] [PubMed] [Google Scholar]
- 5. Francis WP, Abghari P, Du W, Rymal C, Suna M, Kosir MA. Improving surgical outcomes: Standardizing the reporting of incidence and severity of acute lymphedema after sentinel lymph node biopsy and axillary lymph node dissection. Am J Surg 2006; 192:636–639 [DOI] [PubMed] [Google Scholar]
- 6. Keast DH, Despatis M, Allen JO, Brassard A. Chronic oedema/lymphoedema: Under-recognised and under-treated. Int Wound J 2015; 12:328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gençay Can A, Ekşioělu E, Çakçl FA. Early detection and treatment of subclinical lymphedema in patients with breast cancer. Lymphat Res Biol 2019; 17:368–373 [DOI] [PubMed] [Google Scholar]
- 8. Maclellan RA, Couto RA, Sullivan JE, Grant FD, Slavin SA, Greene AK. Management of primary and secondary lymphedema. Ann Plast Surg 2015; 75:197–200 [DOI] [PubMed] [Google Scholar]
- 9. Fahradyan A, El-Sabawi B, Patel KM. Understanding patient expectations of lymphedema surgery. Plast Reconstr Surg 2018; 141:1550–1557 [DOI] [PubMed] [Google Scholar]
- 10. Mehrara BJ, Greene AK. Lymphedema and obesity: Is there a link? Plast Reconstr Surg 2014; 134:154e–160e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Helyer LK, Varnic M, Le LW, Leong W, McCready D. Obesity is a risk factor for developing postoperative lymphedema in breast cancer patients. Breast J 2010; 16:48–54 [DOI] [PubMed] [Google Scholar]
- 12. Gloviczki P, Calcagno D, Schirger A, et al. Noninvasive evaluation of the swollen extremity: Experiences with 190 lymphoscintigraphic examinations. J Vasc Surg 1989; 9:683–690 [DOI] [PubMed] [Google Scholar]
- 13. Vaqueiro M, Gloviczki P, Fisher J, Hollier LH, Schirger A, Wahner HW. Lymphoscintigraphy in lymphedema: An aid to microsurgery. J Nucl Med 1986; 27:1125–1130 [PubMed] [Google Scholar]
- 14. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus document of the International Society of Lymphology. Lymphology 2013; 46:1–11 [PubMed] [Google Scholar]
- 15. Landau MJ, Gould DJ, Patel KM. Advances in fluorescent-image guided surgery. Ann Transl Med 2016; 4:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keo HH, Schilling M, Büchel R, et al. Sensitivity and specificity of fluorescence microlymphography for detecting lymphedema of the lower extremity. Vasc Med 2013; 18:117–121 [DOI] [PubMed] [Google Scholar]
- 17. Keo HH, Husmann M, Groechenig E, Willenberg T, Gretener SB. Diagnostic accuracy of fluorescence microlymphography for detecting limb lymphedema. Eur J Vasc Endovasc Surg 2015; 49:474–479 [DOI] [PubMed] [Google Scholar]
- 18. Bollinger A, Amann-Vesti BR. Fluorescence microlymphography: Diagnostic potential in lymphedema and basis for the measurement of lymphatic pressure and flow velocity. Lymphology 2007; 40:52–62 [PubMed] [Google Scholar]
- 19. Scaglioni MF, Fontein DBY, Arvanitakis M, Giovanoli P. Systematic review of lymphovenous anastomosis (LVA) for the treatment of lymphedema. Microsurgery 2017; 37:947–953 [DOI] [PubMed] [Google Scholar]
- 20. Rosian K, Stanak M. Efficacy and safety assessment of lymphovenous anastomosis in patients with primary and secondary lymphoedema: A systematic review of prospective evidence. Microsurgery 2019; 39:763–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chang DW, Suami H, Skoracki R. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast Reconstr Surg 2013; 132:1305–1314 [DOI] [PubMed] [Google Scholar]
- 22. Suami H, Scaglioni MF, Dixon KA, Tailor RC. Interaction between vascularized lymph node transfer and recipient lymphatics after lymph node dissection—A pilot study in a canine model. J Surg Res 2016; 204:418–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cheng MH, Huang JJ, Wu CW, et al. The mechanism of vascularized lymph node transfer for lymphedema: Natural lymphaticovenous drainage. Plast Reconstr Surg 2014; 133:192e–198e [DOI] [PubMed] [Google Scholar]
- 24. Ito R, Zelken J, Yang CY, Lin CY, Cheng MH. Proposed pathway and mechanism of vascularized lymph node flaps. Gynecol Oncol 2016; 141:182–188 [DOI] [PubMed] [Google Scholar]
- 25. Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 2008; 112:2809–2819 [DOI] [PubMed] [Google Scholar]
- 26. Hong M, Jung E, Yang S, et al. Efficient assessment of developmental, surgical and pathological lymphangiogenesis using a lymphatic reporter mouse and its embryonic stem cells. PLoS One 2016; 11:e0157126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Choi D, Park E, Jung E, et al. Laminar flow downregulates Notch activity to promote lymphatic sprouting. J Clin Invest 2017; 127:1225–1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jung E, Gardner D, Choi D, et al. Development and characterization of a novel Prox1-EGFP lymphatic and Schlemm's canal reporter rat. Sci Rep 2017; 7:5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Perrault DP, Lee GK, Bouz A, et al. Ischemia and reperfusion injury in superficial inferior epigastric artery-based vascularized lymph node flaps. PLoS One 2020; 15:e0227599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Choi I, Lee S, Chung HK, et al. 9-Cis retinoic acid promotes lymphangiogenesis and enhances lymphatic vessel regeneration therapeutic implications of 9-Cis retinoic acid for secondary lymphedema. Circulation 2012; 125:872–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perrault DP, Lee GK, Park SY, et al. Small peptide modulation of fibroblast growth factor receptor 3-dependent postnatal lymphangiogenesis. Lymphat Res Biol 2019; 17:19–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Daneshgaran G, Paik CB, Cooper MN, et al. Prevention of postsurgical lymphedema via immediate delivery of sustained-release 9-cis retinoic acid to the lymphedenectomy site. J Surg Oncol 2020; 121:100–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bramos A, Perrault D, Yang S, Jung E, Hong YK, Wong AK. Prevention of postsurgical lymphedema by 9-cis retinoic acid. Ann Surg 2016; 264:353–361 [DOI] [PMC free article] [PubMed] [Google Scholar]