Abstract
Background
Cancer Care Ontario's Systemic Therapy Task Force recently reviewed the medical oncology system in the province. There has been growing concern about anecdotal reports of burnout, high levels of stress and staff leaving or decreasing their work hours. However, no research has systematically determined whether there is evidence to support or refute these reports. To this end, a confidential survey was undertaken.
Methods
A questionnaire was mailed to all 1016 personnel of the major providers of medical oncology services in Ontario. The questionnaire consisted of the Maslach Burnout Inventory, the 12-item General Health Questionnaire, a questionnaire to determine job satisfaction and stress, and questions to obtain demographic characteristics and to measure the staff's consideration of alternative work situations.
Results
The overall response rate was 70.9% (681 of 961 eligible subjects): by group it was 63.3% (131/207) for physicians, 80.9% (314/388) for allied health professionals and 64.5% (236/366) for support staff. The prevalence of emotional exhaustion were significantly higher among the physicians (53.3%) than among the allied health professionals (37.1%) and the support staff (30.5%) (p ≤ 0.003); the same was true for feelings of depersonalization (22.1% v. 4.3% and 5.5% respectively) (p ≤ 0.003). Feelings of low personal accomplishment were significantly higher among physicians (48.4%) and allied health professionals (54.0%) than among support staff (31.4%) (p ≤ 0.002). About one-third of the respondents in each group reported that they have considered leaving for a job outside the cancer care system. Significantly more physicians (42.6%) than allied health professionals (7.6%) or support staff (4.5%) stated that they have considered leaving for a job outside the province.
Interpretation
The findings support the concern that medical oncology personnel are experiencing burnout and high levels of stress and that large numbers are considering leaving or decreasing their work hours. This is an important finding for the cancer care system, where highly trained and experienced health care workers are already in short suppl
Cancer Care Ontario, the provincial cancer control agency for Ontario, recently convened a task force to review the medical oncology system in the province. The task force report points to the many and multifactorial stresses facing the system, from restructuring of the broader health care system to rapid advances in treatment and an increase in the number and complexity of cases.1 For example, from 1994 to 1999 the number of new cancer cases increased by 28% across the province, and the nursing time required to administer chemotherapy increased by 30%. All of these factors have an impact on the day-to-day work environment of the professional and support personnel that make up the system. Although there are many anecdotal reports of burnout, decreased morale, high levels of stress and staff leaving or decreasing their work hours, no research has systematically determined whether there is evidence to support or refute these reports.
Burnout in the life of health care workers is the construct used to describe the psychological state resulting from a prolonged period of high stress levels in their professional lives. It was originally conceptualized as a syndrome resulting from contact with people who are suffering.2,3 It is characterized by physical and emotional exhaustion, depersonalization and low productivity,2,4 and it has been found to be associated with staff intending to leave the stressful work environment.3 Studies to measure the prevalence of burnout and psychological distress among cancer care physicians,2,5,6 cancer care nurses2,6 and other physicians6,7,8 have been reported. Our aim was to measure these factors among cancer care personnel in Ontario.
The specific objectives of our study were to measure the prevalence of burnout, psychological morbidity, job satisfaction and job stress and to understand the relation between consideration of alternative work situations and burnout, psychological morbidity, job satisfaction and job stress among medical oncology personnel.
Methods
Cancer Care Ontario coordinates cancer care through 8 regional cancer centres providing tertiary cancer care. The agency serves a population of over 11 million residents. The medical oncology program of Cancer Care Ontario comprises medical oncologists, clinical associate physicians, allied health professionals (AHPs) and support staff (SS). Cancer Care Ontario, a tertiary care cancer treatment hospital in downtown Toronto and a network of community oncologists in metropolitan Toronto together represent all major providers of medical oncology services in Ontario.
In the autumn of 1999 we conducted a confidential cross-sectional mailed survey of all personnel working with the major medical oncology providers in Ontario. Approval for the study was obtained from the Ottawa Hospital Research Ethics Committee. A total of 1015 questionnaires were mailed. Survey subjects were identified from employee lists of the major medical oncology providers. Subjects included physicians (medical oncologists and clinical associates), AHPs (nurses, pharmacists, pharmacy technicians, social workers, dietitians and hematology lab technicians) and SS (unit coordinators, clinic attendants, scheduling clerks, receptionists and medical records staff). To maximize the response rate a reminder notice was sent to nonrespondents 2 weeks after the initial mailing; another copy of the questionnaire was sent after a further 2 weeks, and again 2 weeks after that, to the remaining nonrespondents.9
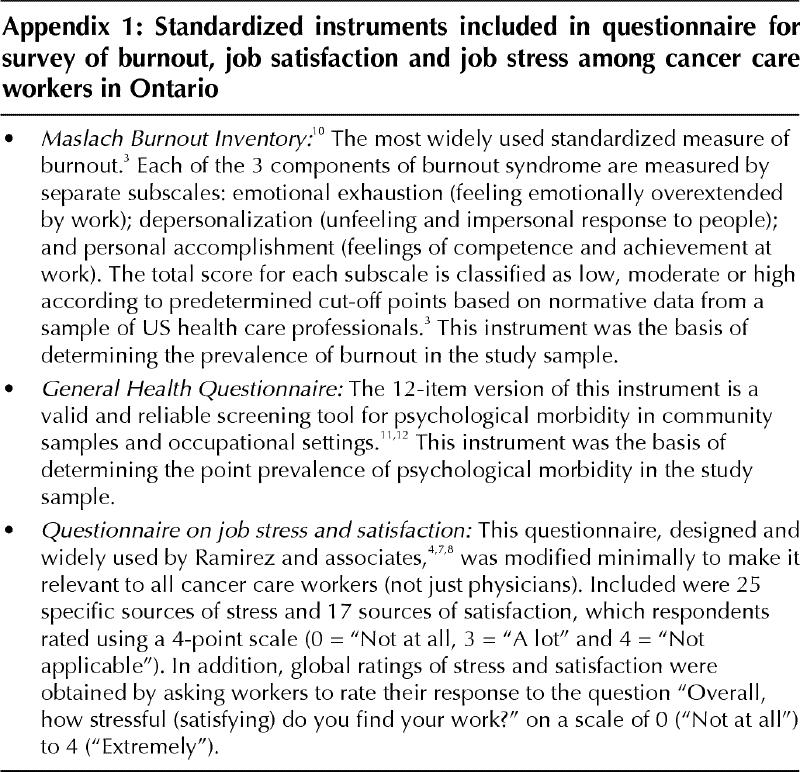
The study questionnaire consisted of the following instruments (Appendix 1):
· The Maslach Burnout Inventory (MBI),10 the most widely used standardized measure of burnout,3 was the basis of determining the prevalence of burnout in the study sample. In the MBI each of the 3 components of burnout — emotional exhaustion, depersonalization and personal accomplishment — are measured by a separate subscale.
· The 12-item version of the General Health Questionnaire (GHQ-12)11,12 was used to assess psychological morbidity.
· A questionnaire designed and widely used by Ramirez and associates4,7,8 was used to measure job stress and satisfaction. It included 25 specific sources of stress and 17 specific sources of satisfaction; in addition, it asked personnel to provide global ratings of stress and satisfaction.
· A questionnaire developed for this study to obtain demographic and job characteristics.
· A section comprising 4 questions to measure personnel's consideration of alternative work situations. Specifically, respondents were asked whether they had seriously considered leaving their current job for a job outside the cancer care system, leaving their job for one outside the province, reducing the number of hours worked or taking early retirement.
MBI scores indicating burnout were classified as high on the basis of cut-off points recommended by the developer of the scale;10 this approach was consistent with that used in other studies.4,7,8 Burnout was defined as high levels of emotional exhaustion, high levels of depersonalization or low levels of personal accomplishment. Psychological morbidity was defined as a score of 4 or more on the GHQ-12; this approach is recommended by the developer of the scale12 and is consistent with other research.4,7,8,13 Differences in the prevalence of burnout and psychological morbidity between the 3 professional groups were assessed using the Fisher's exact test. The Pearson product moment correlation coefficient was used to look at the relation between items on the job satisfaction questionnaire and overall satisfaction, and items on the stress questionnaire and overall stress. High levels of overall satisfaction and overall stress were defined as a score of 3 or more on the respective global satisfaction and stress questions. Logistic regression analysis was used to identify factors associated with consideration of alternative work situations. The level of significance was set at 0.01 for all logistic regression analyses. A 2-sided significance test was used in all cases.
Results
Of the 1015 potential respondents (216 physicians, 405 AHPs and 394 SS), 54 were ineligible because they had moved or were on extended leave (9 physicians, 17 AHPs and 28 SS). Of the remaining 961 subjects 681 (70.9%) returned a completed questionnaire; the response rates by professional group were 63.3% (131/207) for physicians, 80.9% (314/388) for AHPs and 64.5% (236/366) for SS.
The majority of respondents were married and between the ages of 35 and 55 years. The majority of medical oncologists were male (82.5%), and the majority of AHPs and SS were female (95.7% and 98.2% respectively). Of the nurses and medical oncologists 48.8% and 58.7%, respectively, reported that they have worked over 10 years in the cancer care system in Ontario, and 88.6% and 77.8%, respectively, stated that they spend more than 50% of their work time in direct clinical care.
Burnout and psychological morbidity
The prevalence rates of burnout and psychological morbidity are reported in Table 1. More than one-third of the overall sample, and at least one-third in each professional group, had high levels of emotional exhaustion and low levels of personal accomplishment. About half of the physicians had high levels of emotional exhaustion and low levels of personal accomplishment. Although the physicians and the AHPs had similar rates of low personal accomplishment, significantly more of the physicians than of the AHPs (p = 0.003) or the SS (p < 0.001) had high levels of emotional exhaustion; the same was true for high levels of depersonalization (p < 0.001). The prevalence of psychological morbidity in the overall sample was 12.3%. Physicians had the highest prevalence rate of psychological morbidity (25.4%) (p < 0.001).
Table 1
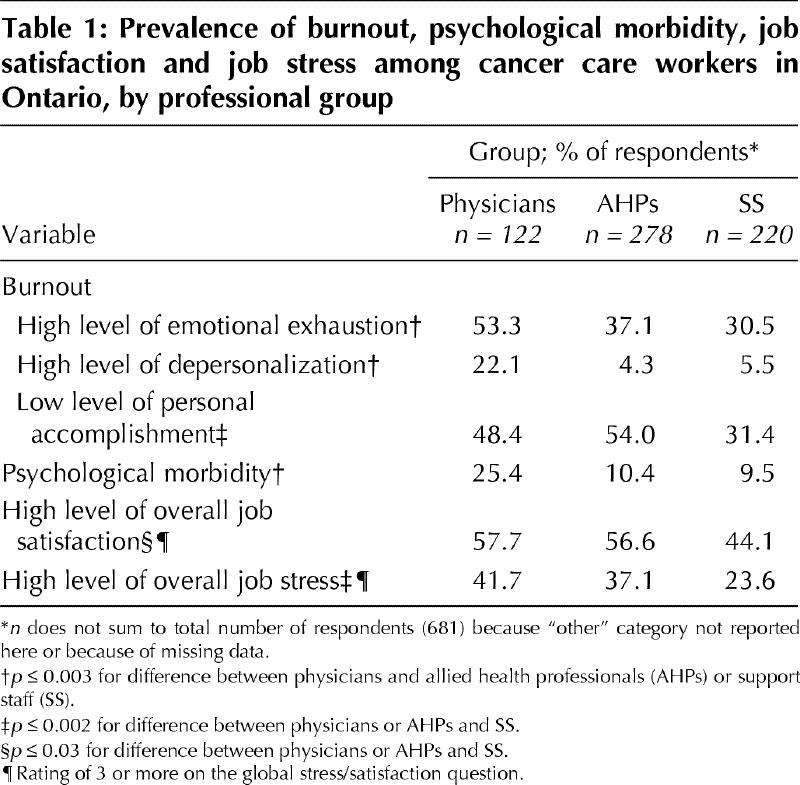
Overall job satisfaction and job stress
The proportions of respondents who indicated high levels of overall job satisfaction and overall job stress are shown in Table 1.
In relation to the various aspects of job satisfaction, in the overall sample a global rating of high job satisfaction was most strongly associated with feeling that professional experience was being used to the fullest (r = 0.46), having variety in the job (r = 0.39) and deriving intellectual stimulation from work (r = 0.42).
In relation to the various aspects of job stress, in the overall sample a global rating of high job stress was most strongly associated with having too great a volume of work (r = 0.61), having inadequate staffing to do the job properly (r = 0.50), feeling under pressure to make deadlines (r = 0.50), having conflicting demands on time (r = 0.46) and having home life disrupted because of long working hours (r = 0.43).
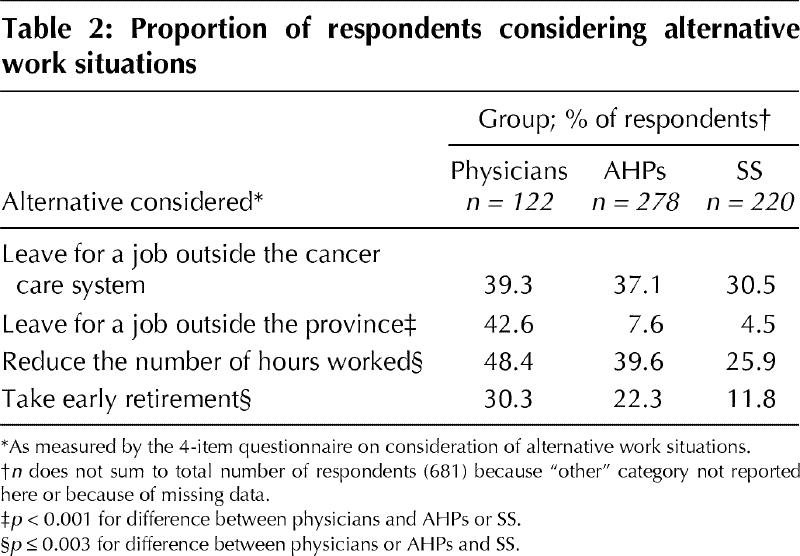
Consideration of alternative work situations
Respondents were asked a series of questions regarding possible alternative work situations. The responses to these questions and differences between the 3 groups are provided in Table 2. Similar proportions of subjects in all 3 groups reported having seriously considered leaving the cancer care system. However, significantly more physicians and AHPs than SS reported having seriously considered reducing the number of work hours (p < 0.002) or taking early retirement (p ≤ 0.003). Significantly more physicians than either of the other 2 groups reported having considered leaving for a job outside the province (p < 0.001).
Table 2
Logistic regression analysis was performed, with consideration of alternative work situations (defined as Yes to any of the 4 specific questions) as the dependent variable. Independent variables tested in the model were psychological morbidity, the 3 components of burnout, demographic characteristics (e.g., sex, age and marital status), overall job stress and overall job satisfaction. Only 4 variables were independent predictors of consideration of alternative work situations. The odds of considering alternative work were increased by high levels of emotional exhaustion (odds ratio [OR] 2.38, 95% confidence interval [CI] 1.46-3.86; p < 0.001), high levels of overall job stress (OR 1.57, 95% CI 1.22-2.03; p < 0.001) and number of years worked at the cancer centre (OR 1.07, 95% CI 1.03-1.10; p < 0.001). High levels of overall job satisfaction reduced the odds of considering leaving (OR 0.55, 95% CI 0.37-0.82; p < 0.002).
Interpretation
Our findings support the concern that medical oncology personnel in Ontario are experiencing burnout and high levels of stress and that large numbers of staff are considering leaving or decreasing their work hours.
Burnout is understood to be a pattern of responses to stressors at work. Work overload has been shown to be one of the important antecedents of burnout.3 The Ontario Systemic Therapy Task Force Report1 documents an increase in the number and complexity of cases managed within the formal cancer care system without a commensurate increase in human resources.
In our study we found that the physician group had the highest prevalence of psychological morbidity and 2 components of burnout. Mindful of the problems associated with temporally and culturally distinct studies, we compared our findings with those from 2 other studies of physician burnout (as measured by the MBI): one involving Canadian emergency physicians13 and the other medical oncologists in the United Kingdom.4 More physicians in our study than in the other 2 had low levels of personal accomplishment and high levels of emotional exhaustion.
Emotional exhaustion is considered to be the first stage in the burnout syndrome and central to the experience of burnout. It has been consistently shown to be directly related to high levels of work demand.3,14 A relation between emotional exhaustion, depression and anxiety was reported in an acute care hospital in Ontario over a 3-year period of hospital restructuring.15 In the present study we found that about half of the physicians and one-third of the respondents in the 2 other professional groups experienced high levels of emotional exhaustion.
We also found that emotional exhaustion was associated with an increased likelihood of personnel considering an alternative work situation, either by changing jobs or by reducing work hours. A relation between burnout and an intention to leave the job has been reported in surveys of emergency physicians,13 nurses16 and workers not in the health care field.3,14 This is an important finding for the cancer care system, where highly trained and experienced health care workers are already in short supply.1 Because of the relation between burnout and work overload, burnout of health care workers may be an important indicator of health care system overload.
What are the implications of these findings? Research has shown that burnout has important consequences both for the workers involved and for the organizations that employ them.3 At the individual level, literature on burnout of health care personnel has linked the components of burnout with mental and physical health problems.3,14,15,17 At the organizational level, burnout is associated with negative organizational outcomes such as absenteeism, high staff turnover rates and diminished productivity.3 All are important factors for the overall efficient functioning of the cancer care system.3,14 Perhaps even more important, however, is the relation between burnout and quality of care.18 The potential for burnout to affect quality of care negatively has been raised in the literature.5,8,15 For example, burnout may make it more difficult to work with people who are dying.6 At a time when stresses in the health care system are becoming more acute, the impact of burnout on either process or outcome measures of quality of care may be an important new area of research.
Appendix 1.
Footnotes
This article has been peer reviewed.
Dr. Grunfeld is supported in part by a Career Scientist Award from the Ontario Ministry of Health. The views expressed in this article are those of the authors, and no official endorsement by the ministry is intended or should be inferred.
Competing interests: None declared.
Reprint requests to: Dr. Eva Grunfeld, Ottawa Regional Cancer Centre, Ottawa Hospital — Civic Campus, 190 Melrose Ave., Ottawa ON K1Y 4K7; eva.grunfeld@orcc.on.ca
References
- 1.Systemic Therapy Task Force. Systemic Therapy Task Force Report. Toronto: Cancer Care Ontario; 2000.
- 2.Barni S, Mondin R, Nazzani R, Archili C. Oncostress: evaluation of burnout in Lombardy. Tumori 1996;82:85-92. [DOI] [PubMed]
- 3.Cordes CL, Dougherty TM. A review and an integration of research on job burnout. Acad Manage Rev 1993;18:621-56.
- 4.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM, Snashall DC, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer 1995;71:1263-9. [DOI] [PMC free article] [PubMed]
- 5.Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: results of a random survey of 1000 oncologists. J Clin Oncol 1991;9:1916-21. [DOI] [PubMed]
- 6.Catalan J, Burgess A, Pergami A, Hulme N, Gazzard B, Phillips R. The psychological impact on staff of caring for people with serious diseases: the case of HIV infection and oncology. J Psychosom Res 1996;40:425-35. [DOI] [PubMed]
- 7.Graham J, Ramirez AJ, Cull A, Finlay I, Hoy A, Richards MA. Job stress and satisfaction among palliative physicians. Palliat Med 1996;10:185-94. [DOI] [PubMed]
- 8.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 1996;347:724-7. [DOI] [PubMed]
- 9.Dillman DA. Mail and telephone surveys: the total design method. New York: John Wiley and Sons; 1978.
- 10.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. Palo Alto (CA): Consulting Psychologists Press; 1996.
- 11.McDowell I, Newell C. Measuring health: a guide to rating scales and questionnaires. Oxford (UK): Oxford University Press; 1996. p. 225-34.
- 12.Goldberg D, Williams P. A user's guide to the General Health Questionnaire. Windsor (UK): Nfer-Nelson Publishing; 1988.
- 13.Lloyd S, Streiner D, Shannon S. Burnout, depression, life and job satisfaction among Canadian emergency physicians. J Emerg Med 1994;12:539-65. [DOI] [PubMed]
- 14.Felton JS. Burnout as a clinical entity — its importance in health care workers. Occup Med 1998;48:237-50. [DOI] [PubMed]
- 15.Woodward CA, Shannon H, Cunningham C, McIntosh J, Lendum B, Rosenbloom D, et al. The impact of re-engineering and other cost reduction strategies on the staff of a large teaching hospital. Med Care 1999;37:556-69. [DOI] [PubMed]
- 16.Leiter MP, Harvie P, Frizzell C. The correspondence of patient satisfaction and nurse burnout. Soc Sci Med 1998;47:1611-7. [DOI] [PubMed]
- 17.Aasland OG, Olff M, Falkum E, Schweder T, Ursin H. Health complaints and job stress in Norwegian physicians: The use of an overlapping questionnaire design. Soc Sci Med 1997;45:1615-29. [DOI] [PubMed]
- 18.Brook RH, McGlynn EA. Quality of health care: Part 2: Measuring quality of care. N Engl J Med 1996;335:966-70. [DOI] [PubMed]


