Abstract
Study Objectives:
Sleep research has grown substantially in recent decades, producing a large amount of data and an increasing number of meta-analyses. This study sought to establish the volume of meta-analyses in this area and assess how this level of material has developed over time.
Methods:
A bibliographic search of the Web of Science database was conducted (1945–2019). The total number of articles and the total number of meta-analyses were extracted for both sleep medicine and a combination of 6 other medical specialties (cardiology, neurology, psychiatry, pulmonology, otorhinolaryngology, and pediatrics).
Results:
A total of 262,384 articles and 1,152 meta-analyses related to sleep medicine were identified. Considering the whole period under analysis, meta-analyses represented 0.44% of the total number of sleep medicine–related articles. Throughout this period, the proportion of meta-analyses published has been increasing in both sleep medicine and the other fields, but it is greater in the other fields. In 2019, meta-analyses in sleep medicine represented 1.10% of the publication output in this area but represented 1.62% of the other areas. However, sleep medicine’s growth rate has been consistently higher than in the other fields. The United States, China, and the United Kingdom have been the top meta-analysis producers.
Conclusions:
Meta-analyses in sleep medicine are underused. As a recent medical field, sleep medicine has more potential to grow and is likely to grow faster than other fields. Researchers should be encouraged to perform and publish meta-analyses on sleep medicine, as long as the analyses are reasonable and feasible from methodological, statistical. and practical perspectives.
Citation:
Pires GN, Niyama A, Andersen ML, Tufik S. Publication of meta-analyses in sleep medicine: a scoping review. J Clin Sleep Med. 2021;17(4):811–817.
Keywords: sleep, systematic review, meta-analysis, epidemiology, scoping review
BRIEF SUMMARY
Current Knowledge: Sleep research has grown substantially in recent decades, producing a large amount of data. Consequently, meta-analyses of sleep-related data are becoming more common.
Study Impact: Meta-analyses in sleep medicine are still not as frequent as in other medical specialties. Researchers should be encouraged to perform and publish meta-analyses on their field of research, as long as the analyses are reasonable and feasible from methodological, statistical, and practical perspectives.
INTRODUCTION
Sleep research output has grown substantially in recent decades. Between 2003 and 2012, both the number of original publications in this area and the number of sleep-related scientific journals more than doubled worldwide.1 Almost 15,000 new sleep-related articles are being published and indexed in PubMed per year. With such a large publication output, valuable research evidence has been piling up for decades. However, considering the complexity and amount of data, it is difficult to summarize all this information and knowledge into a practical form to support clinical advances. In addition, because of methodological heterogeneity and inconsistencies among the results, overall and definitive conclusions are often hard to achieve.
Systematic reviews and meta-analyses would seem to be appropriate tools to use in this case because they are effective in synthesizing data in medicine, usually leading to robust and reliable conclusions. Briefly, a systematic review is a structured and systematic way to comprehensively identify and gather studies addressing a clear question, and meta-analysis refers to a set of techniques allowing different studies to be combined into a single measure of effect.2 From a classical epidemiological perspective, meta-analyses are regarded as the highest possible level of medical evidence3 and have become a popular, powerful, and versatile tool in evidence-based science, with respect to both clinical practice and health policy-making.4,5 In this review we therefore choose to focus on meta-analyses only.
Despite being relatively common and accepted in other medical fields, meta-analyses in sleep medicine seem to be less common. For example, previous data analyzing the number of publications about insomnia showed that only 0.9% of them are meta-analyses.6 In our experience, meta-analyses seem much more common and well-established in other medical specialties than in sleep medicine. Based on this hypothesis, the current study sought to quantify the number of meta-analyses and articles published in the field of sleep medicine (as has been done for other medical fields7–10). We employed scoping review strategies to analyze research trends and the temporal evolution of the publication of meta-analyses in sleep medicine.
METHODS
A bibliographic search was conducted using Web of Science (“all databases” collection) to retrieve meta-analyses published in sleep medicine. Web of Science was chosen because it provides better bibliometric information and covers a longer period compared with other databases.11 The search strategy was limited to articles published between 1945 and 2019, and no additional search filters were applied. Bibliographic searches were performed on July 28, 2020.
First, the total publication output in relation to sleep medicine was identified using a search string containing only “sleep” as the search word. Then the total number of meta-analyses published in sleep medicine was identified by combining meta-analyses-related keywords. The exact search strings used are shown in Table 1.
Table 1.
Search strategies used.
| Areas | Search String |
|---|---|
| Sleep—total publications | TS=(sleep) |
| Sleep—meta-analyses | TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) AND TS=(sleep) |
| Cardiology | SU=(cardiology) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
| Neurology | SU=(neurology) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
| Psychiatry | SU=(psychiatry) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
| Pulmonology | SU=(respiratory system) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
| Otorhinolaryngology | SU=(otorhinolaryngology) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
| Pediatrics | SU=(pediatrics) AND TI=(meta-analysis OR meta-analyses OR metanalysis OR metanalyses) |
SU, TI, and TS refer to the Web of Science research tags for research area (SU = subject), title (TI), and topic (TS). The search words are restricted to words used in the title, in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations.
Because there is no specific sleep medicine category in Web of Science, a single search for the word “sleep” would probably retrieve many false-positive results (ie, articles mentioning “sleep” in the abstract but not directly related to sleep medicine). To increase the specificity of our search, we randomized 200 articles from the original search records and evaluated whether they were actually related to sleep medicine. An article was considered as being sleep medicine–related whenever its population, intervention, or main outcome was related to sleep (based on an abstract-only analysis). The percentage of sleep medicine–related articles in the 200 evaluated articles was used as a correction factor for all the sleep medicine–related data.
After this effort, the overall publication output and the number of meta-analyses published were estimated for the 6 main medical specialties from which sleep medicine originated: cardiology, neurology, psychiatry, pulmonology, otorhinolaryngology, and pediatrics (hereinafter referred to as “other fields”). This assessment was done so that the output of articles and meta-analyses in the field of sleep medicine could be compared with the number of articles and meta-analyses in the specialties from which it evolved. No correction factor was needed for the other specialties because Web of Science already provides search filters for each of these areas. All the search strings are shown in Table 1. For all search strategies, the publication output per year and the source country of the included articles were also extracted. All data were analyzed qualitatively and charted whenever appropriate. Figures and inferential statistics (when appropriated) were made using Prism 5 (GraphPad - San Diego, CA, USA). Overlap analysis using Venn diagrams between meta-analyses pertaining to sleep medicine and meta-analyses in each of the other fields were performed with BioVenn.12 This scoping review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews).13
RESULTS
A total of 130 of the 200 articles from the initial “sleep” search were directly related to sleep medicine, resulting in a correction factor of 0.65, meaning that 65% of all articles using the word “sleep” could be considered to be related to the field of sleep medicine. All sleep-related data hereinafter presented consider this correction factor (unless indicated otherwise).
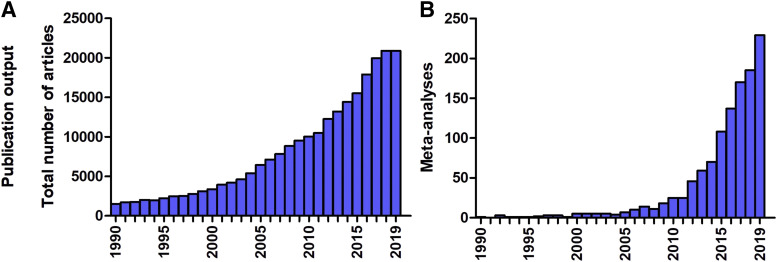
A total of 1,152 meta-analyses in the field of sleep medicine were identified from 1945 to 2019, out of a total publication output of 262,384 articles. The publication of meta-analyses is recent in sleep medicine, with the first one being published in 1989. Since then, while the overall sleep medicine output have had a steady and almost linear growth (Figure 1A), the number of meta-analysis in sleep medicine has grown much rapidly and exponetially, with 229 meta-analysis published in 2019 (Figure 1B).
Figure 1. Publication output over time in sleep medicine.
Data are presented from 1990–2019. All numbers are given using the 0.65 correction factor. (A) Number of meta-analyses published in the field. (B) Number of articles published in the field.
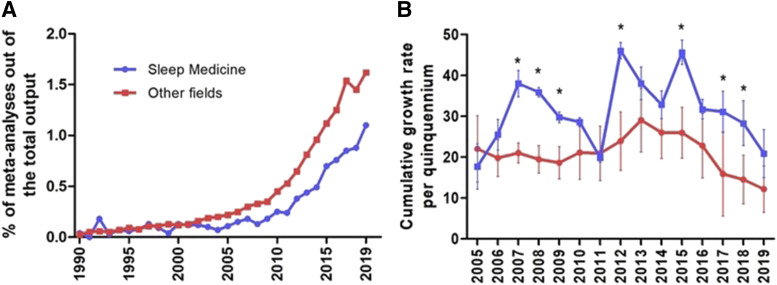
Considering the entire period under analysis, meta-analyses represented 0.44% of the total number of articles in the field of sleep medicine. In comparison, in the other fields combined, meta-analyses represented 0.46% of all articles published (85,718 out of 18,784,820 articles). Throughout this period, the percentage of meta-analyses published has been increasing in both sleep medicine and in the other fields, but it has been substantially greater among the other fields (Figure 2A). In 2019, meta-analyses in sleep medicine represented 1.10% of the publication output in this area but represented 1.62% in the combined medical specialties. Notably, 2019 was the first year when the proportion of meta-analyses in sleep medicine surpassed 1%, whereas in the other fields a proportion of 1% of meta-analyses was reached in 2015.
Figure 2. Comparison of the publication of meta-analyses over time, between sleep medicine and other fields.
(A) Percentage of meta-analyses out of the total number of articles published. Note that although meta-analyses in both sleep medicine and the 6 other fields evaluated are progressively increasing, the proportion of meta-analyses in the other fields is consistently higher than in sleep medicine. (B) Growth rate of meta-analysis publication per 5-year period. Each point represents the average growth rate of that year and the 4 previous years. Data were analyzed with a repeated-measures analysis of variance followed by the Bonferroni posthoc test, using GraphPad Prism 5 and considering a significance level of 5%. Both between-group (sleep medicine vs other fields) and within-group analyses (time) were significant (P < .0001), meaning that sleep medicine growth rate is consistently higher than in the other fields. However, the sleep medicine growth rate curve displays more oscillations, probably reflecting the still limited number of meta-analyses being published. *Significant differences on the Bonferroni posthoc test (P < .05).
Although the proportion of meta-analyses was higher in the combined medical specialties (as shown in Figure 2A), the publication of meta-analyses has grown faster in sleep medicine (Figure 2B). The average growth rate in the number of meta-analyses published was analyzed per quinquennium, from 2005 to 2019. In sleep medicine, the average growth rate for meta-analyses published during this time period was 34.12% (ranging from –22.73% to 83.33%), whereas in the other specialties it was 18.95% (ranging from 7.26%–34.91%). The higher variability in sleep medicine reflects the lower number of meta-analyses in sleep medicine published up to 2010, leading to an erratic pattern. Table 2 presents the number of articles and meta-analyses published and the growth rate per quinquennium since 1990, for both sleep medicine and the combined 6 medical specialties.
Table 2.
Meta-analyses published and overall publication output per quinquennium.
| Sleep | Other Fields | |||||||
|---|---|---|---|---|---|---|---|---|
| Overall Publication | Meta-Analyses | Overall Publication | Meta-Analyses | |||||
| n/y | Cumulative | n/y | Cumulative | n/y | Cumulative | n/y | Cumulative | |
| 2015–2019 | 19,032 | 262,384 | 165 | 1,152 | 726,816 | 18,784,820 | 10,151 | 85,718 |
| 2010–2014 | 12,086 | 167,226 | 45 | 325 | 631,198 | 15,150,738 | 4,363 | 34,963 |
| 2005–2009 | 7,955 | 106,794 | 12 | 100 | 502,883 | 11,994,749 | 1,484 | 13,150 |
| 2000–2004 | 4,307 | 67,022 | 5 | 40 | 369,729 | 9,480,336 | 603 | 5,729 |
| 1995–1999 | 2,619 | 45,488 | 2 | 17 | 329,926 | 7,631,689 | 340 | 2,716 |
| 1990–1994 | 1,801 | 32,391 | 1 | 7 | 302,811 | 5,982,031 | 151 | 1,018 |
| 1985–1989 | 1,350 | 23,384 | 0 | 1 | 264,493 | 4,468,007 | 43 | 264 |
| 1980–1984 | 1,141 | 16,635 | 0 | 0 | 211,558 | 3,145,544 | 10 | 51 |
| 1975–1979 | 864 | 10,929 | 0 | 0 | 160,536 | 2,087,752 | 0 | 1 |
| 1970–1974 | 614 | 6,611 | 0 | 0 | 113,978 | 1,285,074 | 0 | 0 |
| 1965–1969 | 405 | 3,541 | 0 | 0 | 68,297 | 715,182 | 0 | 0 |
| 1960–1964 | 152 | 1,515 | 0 | 0 | 31,635 | 373,696 | 0 | 0 |
| 1955–1959 | 65 | 756 | 0 | 0 | 17,594 | 215,521 | 0 | 0 |
| 1950–1954 | 53 | 433 | 0 | 0 | 15,985 | 127,550 | 0 | 0 |
| 1945–1949 | 34 | 168 | 0 | 0 | 9,525 | 47,627 | 0 | 0 |
Data are presented in periods of 5 years (quinquennia) for a more concise presentation. For data presented on an annual basis, see Table S1 (65.7KB, pdf) in the supplemental material. n/y refers to the average number of articles published in a given quinquennia. Cumulative refers to the total number of articles published up to the end of a quinquennia.
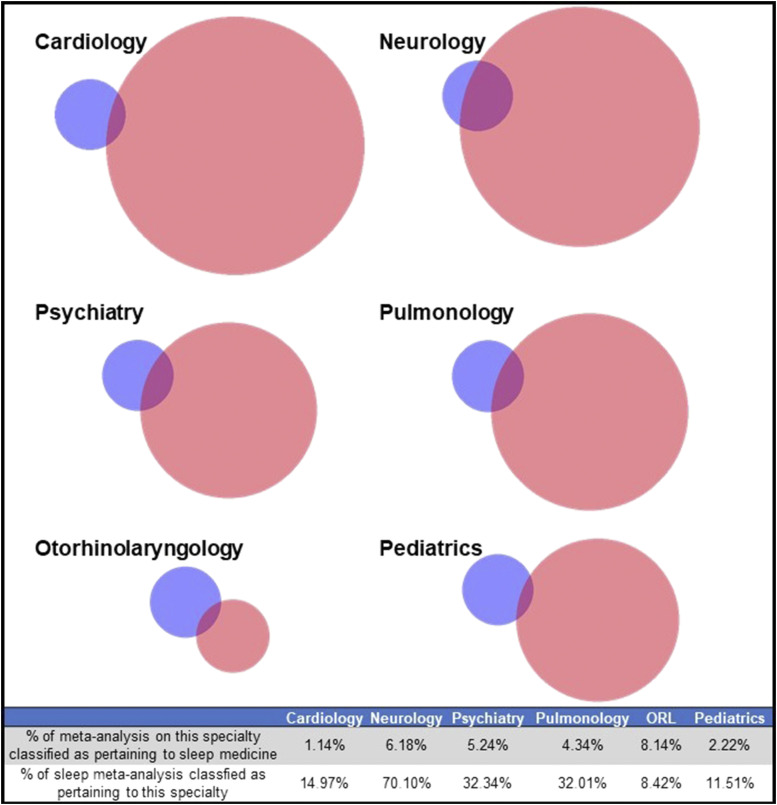
On the overlap analysis, we observed that sleep medicine representation varied among the other fields, ranging from 1.14% (cardiology) to 8.14% (otorhinolaryngology). On the other hand, the percentage of sleep meta-analyses classified as pertaining to each of the other fields was high, ranging from 8.42% (otorhinolaryngology) to 70.10% (neurology; Figure 3). Only 15.72% of all sleep medicine meta-analyses were not classified as pertaining to any of the other fields.
Figure 3. Venn diagrams analyzing the overlap between meta-analyses in sleep medicine and in each of the 6 analyzed medical specialties.
Blue circles represent sleep medicine, and red circles represent each of the other fields. Circle sizes are proportional to the number of meta-analyses included. No correction factor applied. Images generated using BioVenn.12
Regarding the number of meta-analyses published by country, the United States, China, and the United Kingdom were the most productive countries when we considered the whole period. When we considered only 2019, China was the most prolific country, followed by the United States and the United Kingdom. Table 3 presents country rankings for the number of meta-analyses published both during the entire period and in 2019.
Table 3.
Country rankings for the number of meta-analyses published in the field of sleep medicine.
| 1945-2019 | 2019 Only | |||||
|---|---|---|---|---|---|---|
| Country | Number | % | Country | Number | % | |
| 1 | United States | 411 | 35.72 | China | 71 | 30.94 |
| 2 | China | 361 | 31.32 | United States | 61 | 26.68 |
| 3 | United Kingdom | 170 | 14.78 | United Kingdom | 31 | 13.62 |
| 4 | Canada | 112 | 9.76 | Australia | 25 | 10.79 |
| 5 | Australia | 105 | 9.14 | Canada | 19 | 8.23 |
| 6 | Germany | 76 | 6.60 | Italy | 16 | 6.81 |
| 7 | Italy | 66 | 5.70 | Germany | 12 | 5.11 |
| 8 | Netherlands | 49 | 4.23 | Brazil | 11 | 4.83 |
| 9 | Brazil | 46 | 3.95 | Netherlands | 8 | 3.69 |
| 10 | Taiwan | 40 | 3.50 | Taiwan | 8 | 3.69 |
| 11 | Spain | 36 | 3.16 | Spain | 8 | 3.41 |
| 12 | Iran | 31 | 2.71 | Switzerland | 8 | 3.41 |
| 13 | Switzerland | 31 | 2.65 | Japan | 7 | 3.12 |
| 14 | France | 29 | 2.48 | South Korea | 7 | 2.84 |
| 15 | Japan | 28 | 2.43 | Iran | 6 | 2.55 |
Values are estimated using the correction factor of 0.65, which may lead to a lack of precision, particularly with respect to countries with reduced publication outputs. The sum of percentages is higher than 100% because each article is attributed to the countries of all listed authors.
DISCUSSION
Sleep medicine is a relatively recent medical field. It began to advance as a research field with the discovery of REM sleep after the observation of eye movements during infant sleep in 1953 by Aserinsky and Kleitman14 but with little description of any clinical implications. In the 1960s, a more formal definition of sleep stages and the standardization of polysomnography took place, which helped sleep medicine develop as a medical field.15 Finally, from the 1980s to the 2000s, sleep medicine became established as an important medical topic because sleep deprivation and sleep disorders were progressively being associated with important health and social outcomes.16,17 Thus, in the past 30–40 years there has been tremendous growth in sleep medicine research, both in terms of numbers and in reputation.18,19
Our results showed that the number of meta-analyses in this area has grown consistently in recent years, with >100 being published per year since 2015. This result is a natural finding because it reflects the growth in overall publications in sleep medicine. Interestingly though, we found that the proportion of meta-analyses in sleep medicine in recent years was consistently smaller than in the other fields. Our results agree with previous studies that have reported that meta-analyses about specific sleep disorders are also less common than expected. For example, meta-analyses about OSA are less common than those regarding other chronic diseases,20 and meta-analyses about insomnia account for only 0.9% of all articles on the subject.6 It is possible to understand that as a recent medical field, sleep medicine has more potential to grow and is likely to grow faster than the other fields, which explains the achieved results. But in general, these results allow us to conclude that meta-analyses are underused and that there is still room for more of them to be performed and published in sleep medicine.
There may be an overlap between the classification of meta-analyses pertaining to sleep medicine and to each of the other fields. We expected some overlap from this study, which we conducted using a bibliometric perspective, because more than 1 Web of Science subject area can be addressed to each article. However, specific to sleep medicine research, this finding of overlap highlights sleep medicine as a multidisciplinary field, in such a way that this overlapping classification can be understood as natural. As an example, whereas meta-analyses about sleep apnea would more probably fall within the scope of pulmonology or otorhinolaryngology, meta-analyses on polysomnographic sleep patterns could easily be classified as pertaining to neurology. From our sample, one can observe that 8 out of each 100 meta-analyses in otorhinolaryngology deal with sleep, probably reflecting the increasing importance of sleep apnea to this specialty practice; meanwhile, only 1 out of each 100 meta-analyses in cardiology is related to sleep medicine. This overlap is unbalanced among sleep medicine and the other fields: Although sleep medicine meta-analyses represents no more than 8.14% of the total number of meta-analyses in the other fields, meta-analyses classified as pertaining to some of the other fields may account for as much as 70.10% of all sleep medicine meta-analyses.
It is hard to estimate how many meta-analyses are needed in any particular field. Previous studies have shown that approximately 1.2% of all articles published are meta-analyses, but this number is increasing as meta-analyses are becoming increasingly popular.4 However, the mass production of meta-analyses has actually been widely criticized.21,22 The main criticism is that many meta-analyses being published are of limited practical value. It is estimated that only approximately 3% of them are actually clinically relevant, whereas many are redundant, conflicting, flawed, or unnecessary.21 Thus, despite meta-analyses being described as the research design associated with the highest level of scientific evidence in evidence-based medicine, this statement cannot be extrapolated to all meta-analyses individually. In fact, flawed or imprecise meta-analyses produce less evidence than a properly performed randomized controlled trial or a rigorous observational study.
Journals possibly feel impelled to publish meta-analyses because they are the most highly cited research design.23 Recent discussion has focused on the need for journals to play a more active role in ensuring the quality of meta-analyses by rejecting those that do not follow rigorous methodological standards (especially related to risk of bias, heterogeneity, eligibility, and conflict of interests).24 Thus, although we encourage more meta-analyses to be published in sleep medicine, this article should not be interpreted as a license for their indiscriminate production.
We cannot be sure whether meta-analyses published in sleep medicine in general lack quality, although some are clearly flawed and redundant. Our experience suggests that it has not yet become a widespread problem. It is important that researchers work to ensure that the number of high-quality meta-analyses in sleep medicine grows in a responsible way and that meta-analyses are only performed when there is a legitimate rationale to do so.
A few considerations about our methods and some limitations are needed to make a proper appraisal of our data. First, this article should be interpreted under the concept of a scoping review. This is a type of knowledge-synthesis approach that aims at providing a broad overview about what has been published in a field, is frequently used to map the literature, and analyzes publication trends and knowledge gaps.25,26 It frequently relies more on an exploratory and descriptive mapping of the findings than on quantitative analysis and inferential statistics.27 Second, our search strategy may have low sensitivity because it included only 1 database. However, unlike in meta-analyses in which any missing record influences the results, we were not intending to synthesize all results but rather to draw a picture of the research landscape. In this case, using a single database is suitable and is common in purely bibliometric analysis.28,29 Third, only studies using “meta-analysis” in the title were included. This factor may have excluded some studies from our sample, although the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement and checklist are clear in advising that “meta-analysis” should be mentioned in the title.30 It is reasonable to assume that the majority of articles would follow Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations and that restricting the search to articles mentioning “meta-analysis” in the title had little effect on our bibliometric results. Fourth, the search focused on the word “sleep” but was not specific to several sleep medicine–related terms that do not encompass “sleep” (such as insomnia, narcolepsy, and parasomnia). However, articles about any of these topics are very likely to mention “sleep” at least once in their abstract or keywords. Adding these terms to our search would have increased our sample by 5%–10%, which would probably not change the overall behavior of our data. Fifth, the comparator for this article (a combination of meta-analyses from 6 medical fields) was used based on the historical bond they have with sleep medicine. Other types of comparators may be possible (such as calculating the average number of meta-analyses in the parent fields or pooling nonsleep meta-analyses regardless of the source field) but with minimal advantage over the current one. Finally, our results exist only with respect to meta-analyses and are not applicable to narrative or systematic reviews. Because our study is based on the need to synthesize data, focusing only on meta-analyses seemed to be the best approach.
In conclusion, this study provides an overview of the use of meta-analyses in sleep medicine that can help structure and design future research plans in the field. Despite being relatively common in other medical fields, meta-analyses in sleep medicine are less common, making sleep-related meta-analysis an area with a broad potential for growth. Sleep researchers should be encouraged to perform and publish meta-analyses on their field of research, as long as the analyses are reasonable and feasible from methodological, statistical, and practical perspectives. Such concerns are needed to avoid mass production of meta-analyses and to assure analyses relevant to policy-making, research, or clinical areas.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Preliminary data related to the current study were presented as a poster at the 2019 World Sleep Congress (September 20–25, 2019; Vancouver, Canada). GNP, ST, and MLA are supported by grants from the Associação Fundo de Incentivo à Pesquisa (AFIP), the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES - Financial code 001), and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). This article has not been submitted elsewhere for publication. The authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
REFERENCES
- 1.Dinges DF. The growth of sleep science and the role of SLEEP. Sleep. 2014;37(1):7–8. 10.5665/sleep.3296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brusselaers N. How to teach the fundamentals of meta-analyses. Ann Epidemiol. 2015;25(12):948–954. 10.1016/j.annepidem.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 3.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nordmann AJ, Kasenda B, Briel M. Meta-analyses: what they can and cannot do. Swiss Med Wkly. 2012;142:w13518. 10.4414/smw.2012.13518 [DOI] [PubMed] [Google Scholar]
- 5.Møller MH, Ioannidis JPA, Darmon M. Are systematic reviews and meta-analyses still useful research? We are not sure. Intensive Care Med. 2018;44(4):518–520. 10.1007/s00134-017-5039-y [DOI] [PubMed] [Google Scholar]
- 6.Ma Y, Dong M, Mita C, Sun S, Peng CK, Yang AC. Publication analysis on insomnia: how much has been done in the past two decades? Sleep Med. 2015;16(7):820–826. 10.1016/j.sleep.2014.12.028 [DOI] [PubMed] [Google Scholar]
- 7.Cote MP, Apostolakos JM, Voss A, DiVenere J, Arciero RA, Mazzocca AD. A systematic review of meta-analyses published in Arthroscopy: The Journal of Arthroscopic and Related Surgery. Arthroscopy. 2016;32(3):528–537. 10.1016/j.arthro.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 8.Chen H, Jhanji V. Survey of systematic reviews and meta-analyses published in ophthalmology. Br J Ophthalmol. 2012;96(6):896–899. 10.1136/bjophthalmol-2012-301589 [DOI] [PubMed] [Google Scholar]
- 9.Häuser W, Tölle TR. Meta-analyses of pain studies: what we have learned. Best Pract Res Clin Rheumatol. 2015;29(1):131–146. 10.1016/j.berh.2015.04.021 [DOI] [PubMed] [Google Scholar]
- 10.Ioannidis JPA. Meta-analyses in environmental and occupational health. Occup Environ Med. 2018;75(6):443–445. 10.1136/oemed-2016-104128 [DOI] [PubMed] [Google Scholar]
- 11.Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22(2):338–342. 10.1096/fj.07-9492LSF [DOI] [PubMed] [Google Scholar]
- 12.Hulsen T, de Vlieg J, Alkema W. BioVenn—a web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics. 2008;9:488. 10.1186/1471-2164-9-488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 14.Aserinsky E, Kleitman N. Regularly occurring periods of eye motility, and concomitant phenomena, during sleep. Science. 1953;118(3062):273–274. 10.1126/science.118.3062.273 [DOI] [PubMed] [Google Scholar]
- 15.Rechtschaffen A, Kales A, eds. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. Los Angeles, CA: University of California, Brain Information Service/Brain Research Institute; 1968. [Google Scholar]
- 16.Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimäki M. Sleep epidemiology—a rapidly growing field. Int J Epidemiol. 2011;40(6):1431–1437. 10.1093/ije/dyr203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huon LA, Guilleminault C. Future perspectives in sleep medicine. Adv Otorhinolaryngol. 2017;80:145–147. 10.1159/000470886 [DOI] [PubMed] [Google Scholar]
- 18.Chokroverty S. Current status of sleep medicine today and future trends: an editorial. Sleep Med. 2019;61:2–5. 10.1016/j.sleep.2019.06.013 [DOI] [PubMed] [Google Scholar]
- 19.Schulz H, Salzarulo P. The development of sleep medicine: a historical sketch. J Clin Sleep Med. 2016;12(7):1041–1052. 10.5664/jcsm.5946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Araslanova R, Paradis J, Rotenberg BW. Publication trends in obstructive sleep apnea: evidence of need for more evidence. World J Otorhinolaryngol Head Neck Surg. 2017;3(2):72–78. 10.1016/j.wjorl.2017.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ioannidis JP. The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q. 2016;94(3):485–514. 10.1111/1468-0009.12210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chevret S, Ferguson ND, Bellomo R. Are systematic reviews and meta-analyses still useful research? No. Intensive Care Med. 2018;44(4):515–517. 10.1007/s00134-018-5066-3 [DOI] [PubMed] [Google Scholar]
- 23.Patsopoulos NA, Analatos AA, Ioannidis JP. Relative citation impact of various study designs in the health sciences. JAMA. 2005;293(19):2362–2366. 10.1001/jama.293.19.2362 [DOI] [PubMed] [Google Scholar]
- 24.Annane D, Jaeschke R, Guyatt G. Are systematic reviews and meta-analyses still useful research? Yes. Intensive Care Med. 2018;44(4):512–514. 10.1007/s00134-018-5102-3 [DOI] [PubMed] [Google Scholar]
- 25.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–1294. 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 26.Lockwood C, Tricco AC. Preparing scoping reviews for publication using methodological guides and reporting standards. Nurs Health Sci. 2020;22(1):1–4. 10.1111/nhs.12673 [DOI] [PubMed] [Google Scholar]
- 27.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. 10.11124/JBIES-20-00167 [DOI] [PubMed] [Google Scholar]
- 28.Ioannidis JP, Chang CQ, Lam TK, Schully SD, Khoury MJ. The geometric increase in meta-analyses from China in the genomic era. PLoS One. 2013;8(6):e65602. 10.1371/journal.pone.0065602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huamaní C, Rey de Castro J, González-Alcaide G, Polesel DN, Tufik S, Andersen ML. Scientific research in obstructive sleep apnea syndrome: bibliometric analysis in SCOPUS, 1991-2012. Sleep Breath. 2015;19(1):109–114. 10.1007/s11325-014-0969-x [DOI] [PubMed] [Google Scholar]
- 30.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.