Abstract
The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus-2 has affected the health of people across the globe. Cardiovascular diseases (CVDs) have a significant relationship with COVID-19, both as a risk factor and prognostic indicator, and as a complication of the disease itself. In addition to predisposing to CVD complications, the ongoing pandemic has severely affected the delivery of timely and appropriate care for cardiovascular conditions resulting in increased mortality. The etiology behind the cardiac injury associated with severe acute respiratory syndrome coronavirus-2 is likely varied, including coronary artery disease, microvascular thrombosis, myocarditis, and stress cardiomyopathy. Further large-scale investigations are needed to better determine the underlying mechanism of myocardial infarction and other cardiac injury in COVID-19 patients and to determine the incidence of each type of cardiac injury in this patient population. Telemedicine and remote monitoring technologies can play an important role in optimizing outcomes in patients with established CVD. In this article, we summarize the various impacts that COVID-19 has on the cardiovascular system, including myocardial infarction, myocarditis, stress cardiomyopathy, thrombosis, and stroke.
Keywords: COVID-19, cardiovascular, disease, myocardial infarction, thrombosis, myocarditis, Takotsubo cardiomyopathy
In December 2019, a cluster of pneumonia cases caused by a novel coronavirus, now named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), began to spread around the Hubei Provence of China.1 The virus, which causes the clinical condition known as the coronavirus disease 2019 (COVID-19), quickly spreads, and by March 11, 2020, the World Health Organization declared COVID-19 as a pandemic.2 As of January 26, 2021, the SARS-CoV-2 virus has infected 100,243,101 people worldwide and has been responsible for the deaths of 2,156,850.3
Although the initial presentation of COVID-19 was characterized by an unfamiliar viral pneumonia, more investigation has pointed toward a wide range of symptoms and widespread systemic involvement, including various effects on the cardiovascular system.4 Studies have suggested both that preexisting cardiovascular disease (CVD) can increase the risk of severe COVID-19 and that COVID-19 itself can lead to cardiovascular complications.5 Patients at the greatest risk of serious illness sufficient to require intensive care and those at greatest risk of mortality are older individuals, particularly older individuals with underlying comorbid disease, including CVD.6,7 Cardiac injury may occur through either ischemic or nonischemic mechanisms and diffuse microvascular and macrovascular thrombosis is emerging as a recognized complication and possibly important pathology of COVID-19.7 In addition to predisposing to CVD complications, the ongoing pandemic has severely affected the delivery of timely and appropriate care for cardiovascular conditions resulting in increased mortality.8,9 In this review, we aim to explore the relationship between COVID-19 and CVD.
IMPACT OF PREEXISTING CARDIOVASCULAR DISEASE
CVD risk factors and chronic cardiovascular conditions are prevalent among patients affected by COVID-19 and associated with adverse outcomes.7 According to a meta-analysis of six studies looking at the prevalence of preexisting medical conditions in 1527 patients with COVID-19, 16.4% had CVD.10 In an analysis of 72,314 patients with COVID-19 in China, baseline age, hypertension, diabetes mellitus, and known coronary artery disease were associated with adverse outcomes in COVID-19.7 Furthermore, an analysis of 44,672 patients revealed that patients with established CVD had a higher in case fatality rate of 10.5%.5 For comparison, the overall COVID-19 case fatality rate is estimated at around 2–3%.10 In addition, patients with preexisting CVD were more likely to require admission to an intensive care unit (ICU).5 A study of 607 consecutive hospitalized COVID-19 patients in Turkey indicated that 150 presented with concomitant cardiac injury. In addition to the higher mortality rate and increased risk of requiring ICU level care, these patients with cardiac injury were more likely to have longer hospital stays and had a higher risk of developing acute kidney injury and acute respiratory distress syndrome.11
In a study of 132,312 patients with established heart failure and hospitalized between April 1, 2020, to September 30, 2020, 8383 patients (6.4%) were hospitalized with COVID-19, and 100,068 patients (75.6%) were hospitalized with nonacute heart failure reasons.12 Hospitalization with COVID-19 was associated with greater inhospital mortality risk (24.2%) compared with hospitalization with acute heart failure (2.6%). Among patients with heart failure hospitalized with COVID-19, higher age, male sex, and morbid obesity were associated with greater odds of inhospital mortality.12
Data from several studies indicated that age, diabetes mellitus, hypertension, and coronary artery disease history were independent predictors of inhospital mortality; however, it is uncertain due to the lack of more large-scale studies, whether this association between CVD and COVID-19 prognosis is truly due to causation or correlation, since age is the strongest risk factor for CVD and may also be a risk factor for COVID-19 severity due to immune system function decline.7,11 In the same vein, certain CVD risk factors including diabetes and hyperlipidemia have been shown to affect immune system function and therefore may serve as confounding variables to indirectly worsen prognosis and severity of COVID-19.10
ACUTE CARDIAC INJURY AND ELEVATED TROPONIN LEVELS
Several studies have looked at the troponin levels of COVID-19 patients as a marker of acute cardiac injury. Cohort studies from China suggest that 7–17% of hospitalized COVID-19 patients were classified as having acute cardiac injury, which was defined as an elevation of troponin to greater than the 99th percentile of the upper reference limit of normal, along with electrocardiography (ECG) and echocardiography abnormalities. The troponin levels were not only higher in patients with severe disease versus nonsevere disease, but also there was a significantly higher rate of acute cardiac injury in patients who required treatment in an ICU (22.2% vs 2.0%; P < 0.001) and in patients who died (59% vs 1%; P < 0.0001).10 In a cohort study of 416 hospitalized patients with COVID-19 confirmed by reverse transcriptase-polymerase chain reaction, of whom 82 (19.7%) had evidence of myocardial injury had manifested by elevation of high-sensitivity troponin I levels. Patients with myocardial injury had a significantly higher inhospital mortality rate (51.2%) compared with those without myocardial injury (4.5%), and among those with myocardial injury, greater degrees of troponin I elevation were associated with higher mortality rates.6
A meta-analysis of four studies that looked at cardiac troponin I in patients with COVID-19 found that increased levels above the 99th percentile of the upper reference limit was only found in 8–12% of patients but that this correlated with disease severity as well.13 Lippi et al,13 from their meta-analysis of studies including 341 patients, identified increased COVID-19 severity when troponin I levels were elevated, and they deemed a troponin assay as a reasonable initial test in COVID-19 patients, in order to identify those with possible cardiac injury and in turn predict the clinical severity that the patient may experience.
Guo et al,14 in a study of 187 patients with COVID-19 of whom 28% had myocardial injury, provide additional novel insights that troponin T levels are significantly associated with levels of C-reactive protein and N-terminal pro-B-type natriuretic peptide, thus linking myocardial injury to severity of inflammation and ventricular dysfunction. Their data also show progressive serial increases in both troponin T and N-terminal pro-B-type natriuretic peptide during hospitalization in patients who follow a deteriorating clinical course toward death, whereas those with a more favorable outcome with less severe illness, successful treatment, and hospital discharge show stable low levels of these biomarkers.6
According to Liu et al,15 elevated troponins at presentation or a large increase in the troponin level during hospitalization, are associated with up to five times increased risk of arrhythmias, ventilation requirements, and even mortality. Even low levels of troponin elevation may indicate viral or immune mediated cardiac injury and therefore signify a poor prognosis. Patients with increased troponin and especially those with continued increasing troponin levels should be closely monitored, as they are more likely to have an amplified inflammatory response and worse outcomes.7
MYOCARDIAL INFARCTION
Although an association between cardiac injury and COVID-19 is apparent, both as a risk factor and prognostic factor of disease severity, as well as a complication of the disease itself, the mechanism behind the cardiac injury and the possibility of acute myocardial infarctions (MIs) resulting from SARS-CoV-2 are still under investigation. Associations between the MIs and other viral infections have previously been observed. The risk of MI is around six times higher in the week following confirmed influenza virus infections when compared with MI risk the year preceding or following infection and 3.5 times higher in the week following respiratory syncytial virus infection.16 Furthermore, a prospective study by Musher et al.17 revealed a 7–8% rate of MI in hospitalized patients with pneumococcal pneumonia.
One study analyzed angiogram results of COVID-19 positive patients who had typical symptoms of an MI plus ST segment elevation or new left bundle branch block on ECG. There were 28 patients included across all of the hospitals in the Lombardy region of Italy with cardiac catheterization labs between February 20, 2020, and March 30, 2020. Of these 28 patients, only four were previously diagnosed with COVID-19; for the remaining 24 patients, the ST-segment elevation myocardial infarction (STEMI) was the first clinical presentation of the virus. All 28 of these patients received urgent angiography; however, 39.3% did not have any evidence of obstructive coronary artery disease.18 Although type 1 MI, which is caused by an acute atherothrombotic coronary event, was ruled out in over one-third of the patients, type 2 MI, due to an acute oxygen supply and demand mismatch from a cause other than coronary artery disease, could not be ruled out.19 It is unknown whether these patient presentations were due to SARS-CoV-2 induced myocarditis, endothelial dysfunction, or cytokine storm.18
In another study, 18 patients with confirmed COVID-19 across six New York hospitals presented with ST-segment elevation. Out of the patients who received angiography, 33.3% did not have any obstructive disease, once again ruling out type 1 MI in a large percentage of patients. Similarly, the underlying mechanism behind these presentations is unclear, but may include coronary spasm, microthrombi, endothelial injury, cytokine storm, or plaque rupture, among other hypotheses.20 There are also reports of increased risk for stent thrombosis in patients with COVID-19. A case series described four cases of stent thrombosis, one acute in the setting of an STEMI and three very late, which the authors attributed to infection with SARS-CoV-2.21 In a postmortem pathologic study of 40 hearts of COVID-19 infected patients, 14 (35%) had evidence of myocyte necrosis, predominantly of the left ventricle, of whom three (21%) showed evidence of acute MI.22 Cardiac thrombi were present in 11/14 (78.6%) cases with necrosis, with 2/14 (14.2%) having epicardial coronary artery thrombi, whereas 9/14 (64.3%) had microthrombi in myocardial capillaries, arterioles, and small muscular arteries. The authors noted that the microthrombi from COVID-19 patients had significantly greater fibrin and terminal complement C5b-9 immunostaining as compared with intramyocardial thromboemboli from COVID-19 negative subjects and to aspirated thrombi.23
At Westchester Medical Center in Valhalla, New York, the number of STEMI patients during the local peak of the COVID-19 pandemic was compared with the number of STEMI patients during the same time of the year prior. Between March and May of 2019, 17 patients presented to Westchester Medical Center with STEMI, whereas 23 STEMI patients presented between March and May of 2020. It is uncertain, however, whether this 35% increase in STEMI patients was directly caused by COVID-19. Of the 23 patients who presented with STEMI in March–May of 2020, two patients were confirmed to be positive for COVID-19; both of these patients presented in May. Unfortunately, during the height of the COVID-19 pandemic in New York, especially in March and April, COVID-19 testing was extremality limited; therefore, it is impossible to know how many of those 21 remaining STEMI patients were in fact positive for the disease.
CORONARY AND EXTRACORONARY THROMBOSIS
Research has shown that COVID-19 infection predisposes to hypercoagulability and a propensity to clot in many patients.24 Excessive inflammation triggered by the cytokine storm, the massive macrophages, and platelet activation and endothelial dysfunction could be associated with the development of coagulopathy.25 Immune-mediated thrombotic mechanisms, complement activation, macrophage activation syndrome, antiphospholipid antibody syndrome, hyperferritinemia, and renin-angiotensin system dysregulation have been postulated to increase thrombotic risk.24 Patients in the ICU with severe COVID-19 have demonstrated a particularly high incidence of thrombotic complications of around 31%.26 Although the mechanism behind this hypercoagulable state is still undetermined at the present time, thrombotic complications have significantly contributed to morbidity and mortality associated with SARS-CoV-2 infection.24
Despite the previously discussed studies that revealed high rates of nonobstructed coronary arteries on angiography, others have found large amounts of thrombosis and multivessel obstructions. One study followed 115 patients admitted with STEMI, who each underwent angiography. Images were then reviewed by three interventional cardiologists who were blinded to the patients’ COVID-19 status.27 The SARS-CoV-2-positive patients were more likely to have additional cardiovascular risk factors including diabetes, hypertension, hyperlipidemia, and previous history of percutaneous coronary intervention (PCI). Furthermore, the SARS-CoV-2-positive patients had higher levels of high sensitivity troponin, D-dimer, and C-reactive protein, as well as lower lymphocyte counts. There was a significantly higher incidence of multivessel disease in this positive patient population (P = 0.0003) and higher incidence of cardiac arrest (28% vs 9%). Not only was multivessel thrombosis significantly higher in the positive group, but also the rate of in-stent thrombosis postintervention was significantly higher as well (P = 0.04), supporting the role of COVID-19 as a risk factor for thrombotic events (Fig. 1). All of the COVID-19-positive patients in this cohort presented with STEMI as their first manifestation of disease. Therefore, the presence of an ST-STEMI may itself be considered a thrombotic complication of SARS-CoV-2 infection.
FIGURE 1.
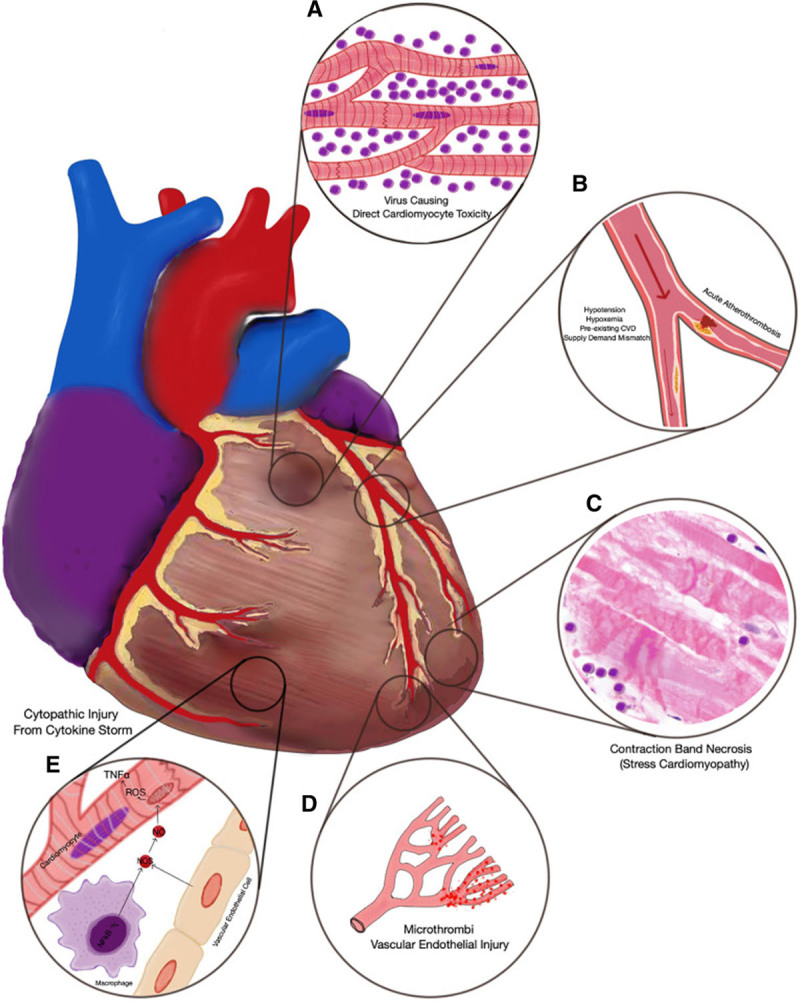
Representation of the possible mechanisms of acute myocardial injury related to COVID-19. A, Myocarditis. B, Type 2 MI (left) and type I MI (right). C, Contraction bands in stress cardiomyopathy. D, Microvascular dysfunction from microthrombi and endothelial injury. E, Cytopathic injury in cytokine storm. Reproduced with permission from Lang JP, Wang X, Moura FA, et al. A current review of COVID-19 for the cardiovascular specialist. Am Heart J. 2020;226:29–44. Copyright Elsevier. COVID-19 indicates coronavirus disease 2019; CVD, cardiovascular disease; MI, myocardial infarction.
This highlights the importance of recognizing a patient’s COVID-19 status, as it has the potential to change their management and course of treatment. A study spanning four hospitals across Italy, Lithuania, Spain, and Iraq between February 1, 2020, and April 15, 2020, also showed high levels of in-stent thrombosis within SARS-CoV-2 patients. Among this group of patients, those treated with PCI had an in-stent thrombosis rate of 21%—a stark contrast from previous rates of around 1%.28 However, a study in Poland found no significant difference of PCI outcomes in COVID-19-positive and COVID-19-negative patients.29 Although further studies are needed to determine the true impact of COVID-19 on PCI outcomes, the use of anticoagulation may have the ability to decrease COVID-19 complications and improve patient outcomes.28
In addition to the large vessel thrombosis observed in the SARS-CoV-2-positive patient population, there has also been evidence of microvascular thrombotic disease that may be contributing to cardiovascular complications. A case report of a woman with COVID-19 and ST-segment elevations in the inferior and lateral leads revealed histological evidence of microthrombi. Postmortem analysis exposed small vessels with platelet and fibrin thrombi, along with areas of patchy myocardial necrosis, inflammation, and hemorrhage.23 This suggests that the microvascular thrombotic disease served as the underlying mechanism behind the patient’s MI. Microvascular thrombosis may therefore be a source of MI in COVID-19 patients even without the presence of epicardial coronary artery obstruction.23
In addition to coronary thromboses, COVID-19 infection is associated with increased risk for arterial and venous thromboembolism (VTE). Tinelli et al25 reported a case of complete aortic thrombosis in a patients with COVID-19 who presented in cardiogenic shock leading to death. Estimates for VTE varied between studies and pulmonary embolism, and deep vein thrombosis were the most frequently noted thrombotic events in COVID-19, with initial reports noting an incidence of 20–30% in critically ill patients.24 The increased risk was noted despite universal thromboprophylaxis, and the risk of all cause death in that cohort was fivefold higher among patients with a thrombotic event (hazard ratio, 5.4; 95% confidence interval [CI], 2.4–12).24 In another study of 9407 patients with COVID-19 infection, the overall VTE rate was 2.9% (2.4% in the medical ward and 4.9% in the ICU) and a VTE or mortality rate of 26.1%.30 In a recent study of 3239 patients with COVID-19, the overall VTE rate was 6.3%.31
D-dimer, thrombocytopenia, and interleukin-6 are promising markers of COVID-19 severity and could be considered in the laboratory testing to assess thrombotic risk.32 COVID-19-infected patients, whether hospitalized or ambulatory, are at high risk for VTE, and an early and prolonged pharmacological thromboprophylaxis with low-molecular-weight heparin is highly recommended.33 A recent retrospective study in 3239 patients analyzed the role of early therapeutic anticoagulation on mortality and noted that among critically ill adults with COVID-19, early therapeutic anticoagulation did not affect survival.31 Randomized trials are urgently needed to determine the safety of proposed therapeutic anticoagulation with heparin and the role for antiplatelet agents in patient management.32
MYOCARDITIS
Myocarditis is an uncommon diagnosis occurring in 4.5–7.2% of highly selected cases undergoing autopsy or endomyocardial biopsy.34,35 Available data suggest that myocarditis as a cause of myocardial injury in patients with COVID-19 is uncertain and rates of fatal myocarditis are low. Although an inflammatory response to COVID-19 infection could be reported in cases with higher myocardial virus load versus no virus infection, this was not associated with an influx of no inflammatory cell infiltrates or differences in leukocyte numbers.36
ST-segment elevations, while typically manifested in STEMI, can also be present in myocarditis—an inflammatory disease of the myocardium that is another potential complication of SARS-CoV-2 infection. A meta-summary of COVID-19 patients with suspected myocarditis revealed that 25% of the confirmed myocarditis cases had ST-segment changes including elevation and depression.37 Many symptoms of myocarditis overlap with acute coronary syndrome such as chest pain, fatigue, and dyspnea; however, on angiography, myocarditis does not produce an obstruction of the coronary arteries. There is also significant overlap in symptoms of primary COVID-19 and suspected myocarditis in COVID-19 patients.38
Stable patients with COVID-19 or other recent viral infections, who present with acute chest pain and normal angiography, could undergo further workup including echocardiography and cardiovascular magnetic resonance (CMR) imaging using the Lake Louise criteria, which has a specificity of up to 91% for detecting myocarditis. CMR can aid in differentiating myocarditis from nonobstructive type 2 MI or stress cardiomyopathy.39 When CMR imaging is not feasible, cardiac computed tomographic (CT) angiography with delayed myocardial imaging may serve to exclude significant coronary artery disease and identify myocardial inflammatory patterns.40 An accurate diagnosis is significant, as myocarditis in COVID-19 patients have the potential for rapid clinical deterioration and warrant a multidisciplinary treatment approach.38 CMR analysis of 145 competitive student athletes recovering from mostly mild COVID-19 demonstrated a low prevalence of myocarditis (1.4%) and the authors questioned the utility of CMR as a screening tool for myocarditis in this patient population. However, this is a relatively low risk population with only predominantly mild COVID-19 (50% cases), so these findings might not be generalizable. Recommendations regarding endomyocardial biopsy are not consistent across recommendations.34,40 However, given its extremely low frequency and unclear therapeutic implications, the routine use of endomyocardial biopsy to diagnose myocarditis in the setting of COVID-19 might not be entirely beneficial.34
STRESS CARDIOMYOPATHY
Several case reports have also demonstrated instances of Takotsubo cardiomyopathy in COVID-19-positive patients.41,42 Takotsubo cardiomyopathy is a syndrome that is typically triggered by emotional distress but has also been associated with respiratory failure and infections. It is characterized by acute and transient regional left ventricular systolic dysfunction.43 There was a significant increase in the incidence of stress cardiomyopathy during the COVID-19 period, with an incidence proportion of 7.8% compared with prepandemic incidence proportion range of 1.5–1.8% (rate ratio, 4.58; 95% CI, 4.11–5.11; P < 0.001).44
One case report discussed a woman who presented with acute respiratory failure and ECG changes congruent with STEMI; however, her echocardiogram results were classic for Takotsubo cardiomyopathy with mid-distal left ventricular hypokinesis and apical ballooning. Another reported a woman who had negative T waves and repolarization phase alternations on ECG, but similarly, the echo showed apical ballooning and hypokinesia of the mid-ventricular segments.
An additional study looked at COVID-19 patients at The Mount Sinai Hospital in New York who underwent clinically indicated transthoracic echocardiogram. Out of 118 consecutive patients, five of them (4.2%) had features compatible with Takotsubo cardiomyopathy. On their ECG taken most closely to the echo, two out those five patients had ST-segment elevations as well. These patients were also shown to have higher peak levels of troponin I and creatinine kinase-MB. Takotsubo cardiomyopathy is another form of cardiac injury that should be considered in a differential diagnosis in COVID-19 patients.43
CEREBROVASCULAR DISEASE
Stroke is an important complication of COVID-19. Acute ischemic stroke, particularly of the cryptogenic type, is the predominant form. Ischemic stroke was reported as a complication on certain viral syndromes (0.7%), but the incidence is higher with SARS-CoV-2 infection (1.6%).45 Inflammation both local and systemic, endothelial injury, and hypercoagulability associated thrombosis were implicated in the pathogenesis of ischemic stroke in COVID-19 patients.46 Multicenter studies and meta-analysis reported a 0.5–4.5% incidence of stroke in patients with COVID-19, depending on the patient demographic studied.46–48 The higher the severity of COVID-19, the higher the risk of acute stroke.
In a recently published large cohort analysis of 67,845 patients with SARS-CoV-2, 1.3% were hospitalized for cerebrovascular events, 1.1% for ischemic stroke, and 0.2 for hemorrhagic stroke. Compared with noninfected contemporary or historical controls, patients with SARS-CoV-2 infection had increased odds of ischemic stroke (odds ratio [OR] = 3.58; 95% CI = 1.43–8.92) and cryptogenic stroke (OR = 3.98; 95% CI = 1.62–9.77).49 SARS-CoV-2 infection status was not associated with the likelihood of receiving intravenous thrombolysis among hospitalized ischemic stroke patients during the COVID-19 pandemic. Odds of inhospital mortality were higher among SARS-CoV-2 stroke patients than noninfected contemporary or historical stroke patients (OR = 5.60, 95% CI = 3.19–9.80). In a review of neuroimaging findings from 954 patients with COVID-19 and associated neurological manifestations, ischemia with large vessel occlusion event was revealed in 59.9% of ischemic stroke patients, whereas 69.2% of patients with intracerebral hemorrhage exhibited bleeding in a location that was not associated with hypertension. Callosal and/or juxtacortical location was identified in 58.7% of cerebral microbleed positive images.50 In another study, the authors suggested a possibly higher proportion of microangiopathic involvement or undetected distal large-vessel occlusion with COVID-19-related strokes.51
In an analysis of 277 patients with stroke of whom 105 (38%) had COVID-19, COVID-19-positive patients were more likely to have a cryptogenic (51.8% vs 22.3%, P < 0.0001) stroke cause and were more likely to suffer ischemic stroke in the temporal (P = 0.02), parietal (P = 0.002), occipital (P = 0.002), and cerebellar (P = 0.028) regions. Outcomes were worse among COVID-19-positive patients, including longer length of stay (P < 0.0001), greater percentage requiring ICU care (P = 0.017), and greater rate of neurological worsening during admission (P < 0.0001); additionally, more COVID-19-positive patients suffered inhospital death (33% vs 12.9%, P < 0.0001).52 In a study of 550 acute stroke patients from seven centers in Spain, 124 (22.6%) had COVID-19. There were no differences found in the rates of reperfusion therapies in ischemic strokes (45.5% non-COVID-19, 35.7% confirmed COVID-19, and 40% suspected COVID-19; P = 0.265). However, the COVID-19 group had longer median door-to-puncture time (110 vs 80 minutes) due to performance of chest CT imaging. Multivariate analysis confirmed poorer outcomes for confirmed or suspected COVID-19 (adjusted ORs, 2.05 [95% CI, 1.12–3.76] and 3.56 [95% CI, 1.15–11.05], respectively). COVID-19 has more severe strokes and poorer outcomes despite similar acute management.53
In addition to increasing stroke risk, the COVID-19 pandemic has also caused disruptions in optimal stroke care delivery and decreased stroke hospitalizations resulting in poor outcomes.54,55 A “hospital avoidance” nature was noted among stroke patients due to the pandemic restrictions and the fear of being exposed to infected individuals at medical centers.56 A meta-analysis on nine studies with 59,233 subjects showed that the number of stroke alerts, reperfusions, and mechanical thrombectomies was reduced by 36%, 31%, and 22%, respectively, during the pandemic. However, the number of patients receiving mechanical thrombectomy per stroke increased by 23%, which could probably result from a higher admission threshold for stroke during the pandemic and decreased admission rates for milder strokes.57,58 These findings were confirmed in other larger studies in which the authors reported that reperfusion treatments declined by 31% and specifically thrombolysis by 33% during the pandemic.59
Data from several large stroke centers have demonstrated that compared with patients in the prepandemic, patients with acute ischemic stroke during the pandemic had three times the discharge mortality despite having statistically similar rates of door to head CT time door to groin puncture times, time to alteplase administration, door to reperfusion times, and successful recanalization.60 These findings are concerning, and while we investigate the optimal strategies to identify and manage acute stroke in patients with COVID-19, we should have pathways to maintain availability of stroke care during the COVID-19 outbreak as these are crucial to prevent indirect mortality and disability due to suboptimal care, while decreasing potential COVID-19 exposure to patients and healthcare providers.61,62 Telemedicine and telestroke assessments have an important role to play in these pathways.63 A well-established stroke care network helps to diminish the impact of such an outbreak in stroke care, reducing secondary transfers and allowing maintenance of reperfusion therapies, with a minor impact on door-to-puncture times, which were longer in patients who underwent chest computed tomography.64
SUMMARY AND FUTURE DIRECTIONS
CVD is common in severe COVID-19 presentations both as a predisposing risk factor and as complications. Patients with preexisting CVD have worse outcomes with COVID-19 and patients with heart failure hospitalized with COVID-19 are at high risk for complications, with nearly one in four dying during the hospitalization. In addition to predisposing to CVD complications, the ongoing pandemic has severely affected the delivery of timely and appropriate care for cardiovascular conditions resulting in increased mortality.8,9 Cardiac injury and specifically increased troponin levels have been shown to lead to worse clinical outcomes and higher mortality rates. Children with multisystem inflammatory syndrome from SARS-CoV-2 infection have several cardiac manifestations common, including ventricular dysfunction, coronary artery dilation and aneurysms, arrhythmia, and conduction abnormalities.65 The etiology behind the cardiac injury associated with SARS-CoV-2 is likely varied, including coronary artery disease, microvascular thrombosis, myocarditis, and even stress cardiomyopathy. Furthermore, large-scale investigations are needed to better determine the underlying mechanism of MI and other cardiac injury in COVID-19 patients, and to determine the incidence of each type of cardiac injury in this patient population. Determining the etiology of cardiac injury is imperative, as it can change the clinical management of the patient and also potentially provide further information about how to prevent these cardiac injuries in future COVID-19 patients and improve outcomes. Telemedicine and remote monitoring technologies can play an important role in optimizing outcomes in patients with established CVD.
Footnotes
Disclosure: The authors have no conflicts of interest to report.
REFERENCES
- 1.Fauci AS, Lane HC, Redfield RR. Covid-19 - navigating the uncharted. N Engl J Med. 2020; 382:1268–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Timeline: WHO’s COVID-19 Response. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline. Accessed January 26, 2021.
- 3.COVID-19 Map. Johns Hopkins Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/map.html. Accessed April 10, 2020
- 4.Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) [published online ahead of print March 27, 2020]. JAMA Cardiol. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golemi Minga I, Golemi L, Tafur A, et al. The novel coronavirus disease (COVID-19) and its impact on cardiovascular disease. Cardiol Rev. 2020; 28:163–176 [DOI] [PubMed] [Google Scholar]
- 6.Bonow RO, Fonarow GC, O’Gara PT, et al. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020; 5:751–753 [DOI] [PubMed] [Google Scholar]
- 7.Lang JP, Wang X, Moura FA, et al. A current review of COVID-19 for the cardiovascular specialist. Am Heart J. 2020; 226:29–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadhera RK, Shen C, Gondi S, et al. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021; 77:159–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu J, Mamas MA, Mohamed MO, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021; 107:113–119 [DOI] [PubMed] [Google Scholar]
- 10.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020; 75:2352–2371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barman HA, Atici A, Sahin I, et al. Prognostic significance of cardiac injury in COVID-19 patients with and without coronary artery disease [published online ahead of print June 19, 2020]. Coron Artery Dis. doi: 10.1097/MCA.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatt AS, Jering KS, Vaduganathan M, et al. Clinical outcomes in patients with heart failure hospitalized with COVID-19. JACC Heart Fail. 2021; 9:65–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020; 63:390–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5:811–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu PP, Blet A, Smyth D, et al. The science underlying COVID-19: implications for the cardiovascular system. Circulation. 2020; 142:68–78 [DOI] [PubMed] [Google Scholar]
- 16.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018; 378:345–353 [DOI] [PubMed] [Google Scholar]
- 17.Musher DM, Rueda AM, Kaka AS, et al. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis. 2007; 45:158–165 [DOI] [PubMed] [Google Scholar]
- 18.Stefanini GG, Montorfano M, Trabattoni D, et al. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020; 141:2113–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.López-Cuenca A, Gómez-Molina M, Flores-Blanco PJ, et al. Comparison between type-2 and type-1 myocardial infarction: clinical features, treatment strategies and outcomes. J Geriatr Cardiol JGC. 2016; 13:15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020; 382:2478–2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prieto-Lobato A, Ramos-Martínez R, Vallejo-Calcerrada N, et al. A case series of stent thrombosis during the COVID-19 pandemic. JACC Case Rep. 2020; 2:1291–1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pellegrini D, Kawakami R, Guagliumi G, et al. Microthrombi as a major cause of cardiac injury in COVID-19: a pathologic study [published online ahead of print January 22, 2021]. Circulation. doi: 10.1161/CIRCULATIONAHA.120.051828. [DOI] [PubMed] [Google Scholar]
- 23.Guagliumi G, Sonzogni A, Pescetelli I, et al. Microthrombi and ST-segment-elevation myocardial infarction in COVID-19. Circulation. 2020; 142:804–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanff TC, Mohareb AM, Giri J, et al. Thrombosis in COVID-19. Am J Hematol. 2020; 95:1578–1589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tinelli G, Minelli F, Sica S, et al. Complete aortic thrombosis in SARS-CoV-2 infection [published online ahead of print January 26, 2021]. Eur Heart J. doi: 10.1093/eurheartj/ehab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klok FA, Kruip MJHA, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020; 191:148–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choudry FA, Hamshere SM, Rathod KS, et al. High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2020; 76:1168–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamadeh A, Aldujeli A, Briedis K, et al. Characteristics and outcomes in patients presenting with COVID-19 and ST-segment elevation myocardial infarction. Am J Cardiol. 2020; 131:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siudak Z, Grygier M, Wojakowski W, et al. Clinical and procedural characteristics of COVID-19 patients treated with percutaneous coronary interventions. Catheter Cardiovasc Interv. 2020; 96:E568–E575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen SL, Gianos E, Barish MA, et al. Prevalence and predictors of venous thromboembolism or mortality in hospitalized COVID-19 patients [published online ahead of print January 20, 2021]. Thromb Haemost. doi: 10.1055/a-1366-9656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Samkari H, Gupta S, Leaf RK, et al. Thrombosis, bleeding, and the observational effect of early therapeutic anticoagulation on survival in critically ill patients with COVID-19 [published online ahead of print January 26, 2021]. Ann Intern Med. doi: 10.7326/M20-6739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Page EM, Ariëns RAS. Mechanisms of thrombosis and cardiovascular complications in COVID-19. Thromb Res. 2021; 200:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020; 95:834–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kawakami R, Sakamoto A, Kawai K, et al. Pathological evidence for SARS-CoV-2 as a cause of myocarditis: JACC review topic of the week. J Am Coll Cardiol. 2021; 77:314–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Halushka MK, Vander Heide RS. Myocarditis is rare in COVID-19 autopsies: cardiovascular findings across 277 postmortem examinations. Cardiovasc Pathol. 2021; 50:107300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lindner D, Fitzek A, Bräuninger H, et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020; 5:1281–1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ho JS, Sia CH, Chan MY, et al. Coronavirus-induced myocarditis: a meta-summary of cases. Heart Lung. 2020; 49:681–685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pirzada A, Mokhtar AT, Moeller AD. COVID-19 and myocarditis: what do we know so far? CJC Open. 2020; 2:278–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cosyns B, Lochy S, Luchian ML, et al. The role of cardiovascular imaging for myocardial injury in hospitalized COVID-19 patients. Eur Heart J Cardiovasc Imaging. 2020; 21:709–714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020; 17:1463–1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Minhas AS, Scheel P, Garibaldi B, et al. Takotsubo syndrome in the setting of COVID-19. JACC Case Rep. 2020; 2:1321–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roca E, Lombardi C, Campana M, et al. Takotsubo syndrome associated with COVID-19. Eur J Case Rep Intern Med. 2020; 7:001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giustino G, Croft LB, Oates CP, et al. Takotsubo cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020; 76:628–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jabri A, Kalra A, Kumar A, et al. Incidence of stress cardiomyopathy during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020; 3:e2014780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smilowitz NR, Subashchandran V, Yuriditsky E, et al. Thrombosis in hospitalized patients with viral respiratory infections versus COVID-19. Am Heart J. 2021; 231:93–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19) [published online ahead of print January 23, 2021]. J Neurol. doi: 10.1007/s00415-021-10406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siepmann T, Sedghi A, Simon E, et al. Increased risk of acute stroke among patients with severe COVID-19: a multicenter study and meta-analysis. Eur J Neurol. 2021; 28:238–247 [DOI] [PubMed] [Google Scholar]
- 48.Mendes A, Herrmann FR, Genton L, et al. Incidence, characteristics and clinical relevance of acute stroke in old patients hospitalized with COVID-19. BMC Geriatr. 2021; 21:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Katsanos AH, Palaiodimou L, Zand R, et al. The impact of SARS-CoV-2 on stroke epidemiology and care: a meta-analysis. Ann Neurol. 2021; 89:380–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ladopoulos T, Zand R, Shahjouei S, et al. COVID-19: neuroimaging features of a pandemic [published online ahead of print January 9, 2021]. J Neuroimaging. doi: 10.1111/jon.12819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Naval-Baudin P, Rodriguez Caamaño I, Rubio-Maicas C, et al. COVID-19 and ischemic stroke: clinical and neuroimaging findings. J Neuroimaging. 2021; 31:62–66 [DOI] [PubMed] [Google Scholar]
- 52.Dhamoon MS, Thaler A, Gururangan K, et al. ; Mount Sinai Stroke Investigators*. Acute cerebrovascular events with COVID-19 infection. Stroke. 2021; 52:48–56 [DOI] [PubMed] [Google Scholar]
- 53.Ntaios G, Michel P, Georgiopoulos G, et al. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke. 2020; 51:e254–e258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Esenwa C, Parides MK, Labovitz DL. The effect of COVID-19 on stroke hospitalizations in New York City. J Stroke Cerebrovasc Dis. 2020; 29:105114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hoyer C, Ebert A, Huttner HB, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 2020; 51:2224–2227 [DOI] [PubMed] [Google Scholar]
- 56.Paolucci M, Biguzzi S, Cordici F, et al. Impact of COVID-19 pandemic on acute stroke care: facing an epidemiological paradox with a paradigm shift [published online ahead of print November 21, 2020]. Neurol Sci. doi: 10.1007/s10072-020-04914-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.July J, Pranata R. Impact of the coronavirus disease pandemic on the number of strokes and mechanical thrombectomies: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2020; 29:105185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 2020; 51:2315–2321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hsiao J, Sayles E, Antzoulatos E, et al. Effect of COVID-19 on emergent stroke care: a regional experience. Stroke. 2020; 51:e2111–e2114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Agarwal S, Scher E, Rossan-Raghunath N, et al. Acute stroke care in a New York City comprehensive stroke center during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2020; 29:105068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aguiar de Sousa D, van der Worp HB, Caso V, et al. Maintaining stroke care in Europe during the COVID-19 pandemic: results from an international survey of stroke professionals and practice recommendations from the European Stroke Organisation. Eur Stroke J. 2020; 5:230–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leira EC, Russman AN, Biller J, et al. Preserving stroke care during the COVID-19 pandemic: potential issues and solutions. Neurology. 2020; 95:124–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meyer D, Meyer BC, Rapp KS, et al. A stroke care model at an academic, comprehensive stroke center during the 2020 COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2020; 29:104927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fuentes B, Alonso de Leciñana M, García-Madrona S, et al. Stroke acute management and outcomes during the COVID-19 outbreak: a cohort study from the Madrid stroke network. Stroke. 2021; 52:552–562 [DOI] [PubMed] [Google Scholar]
- 65.Alsaied T, Tremoulet AH, Burns JC, et al. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation. 2021; 143:78–88 [DOI] [PubMed] [Google Scholar]


