ABSTRACT
Introduction:
Little is known whether the duration of opioid use influences the concentrations of pro- and anti-inflammatory cytokines.
Objectives:
This study examined the plasma concentration of pro-inflammatory cytokine, interleukin 6 (IL-6), and anti-inflammatory cytokine, interleukin 10 (IL-10), in short-, and long-term opioid users with noncancer pain.
Materials and Methods:
Adult patients with opioid therapy for noncancer pain were recruited from pain clinics at two tertiary hospital settings in Malaysia between February 2016 and March 2017. They were stratified into short- or long-term users based on opioid prescriptions ≥ 90 days per year. A 10mL blood sample was taken for the analysis of plasma concentrations of IL-6 and IL-10 and were quantified using a highly sensitive multiplex assay.
Results:
Of 38 patients recruited, 24% (n = 9/38) and 76% (n = 29/38) were respectively short- and long-term opioid users. Short-term use of opioid was associated with higher levels of IL-6 (mean ± SD, 173.9 ± 13.7 pg/mL) and IL-10 (50 ± 5.8 pg/mL), whereas long-term use of opioids was associated with lower levels (no significant difference) of both cytokines IL6 (125 ± 16.1 pg/mL) and IL10 (41.3 ± 6.7 pg/mL). There was strong correlation between IL-6 and IL-10 within the same group (r² = 0.72, P < 0.05) and (r² = 0.76, P < 0.05) for short- and long-term users, respectively.
Conclusion:
The duration of opioid use may modulate the level of pro-inflammatory cytokines in which it was higher in short-term use and lower in long-term use, but the effect of pain relief was similar as both cytokines were well correlated.
KEYWORDS: Cytokines, IL-10, IL-6, noncancer pain, opioid
INTRODUCTION
Cytokines released centrally by activated glia or peripherally by macrophages, fibroblasts, and endothelial cells are believed to play a significant role in the establishment of pain conditions, and in modulating the analgesic efficacy of opioid. Duration of opioid therapy is among the factors related to the development of opioid tolerance which is associated with unwanted complications of opioid therapy including overdose death and opioid tolerance in noncancer pain. To date, limited evidence is available about the effect of duration of opioid therapy on the cytokines level. Hence, this research aims to explore the effect of duration of opioid therapy on the pro-inflammatory cytokine, IL-6, and the anti-inflammatory cytokine, IL-10, among noncancer pain patients who were treated with opioids for either long-term or short-term therapy.
MATERIALS AND METHODS
Study design and site
This study was a prospective cross-sectional clinical study, which recruited all the available patients with noncancer pain from pain clinics at two tertiary hospital settings in Malaysia between February 2016 and March 2017. This period was the period required for all the eligible patients to attend the pain clinics for scheduled visits. These patients were treated with any of the five opioids (morphine, oxycodone, dihydrocodeine, fentanyl, and buprenorphine) available at the pain clinics for their pain relief. A 10mL blood samples was taken from each patient for the evaluation of plasma concentrations of pro-inflammatory cytokine interleukin-6 (IL-6) and anti-inflammatory cytokine interleukin-10 (IL-10).
Inclusion and exclusion criteria
Only patients who understood the required study procedures and can communicate in English language and/or Bahasa Malaysia and have given full informed written consent were included. Patients were excluded if they have a history of opioid abuse, received injectable opioids which is used for inpatients only.
Duration of opioid use
Patients were categorized into short-term and long-term opioid users based on the duration of opioid use. The short-term opioid use was defined as using prescribed opioids for less than 90 days per year and if otherwise will be included as long-term opioid use.
Quantification of pro-inflammatory cytokine IL-6 and anti-inflammatory cytokine IL-10 concentrations in plasma using the multiplex assay
Plasma concentrations of cytokines, IL-10, and IL-6 were quantified using a highly sensitive multiplex assay following the procedures provided by the manufacturers (Milliplex, Merck, Germany). The plate was run on Luminex 200, Multiplex Bead-based Fluroanalyzer equipped with xPOTENT software. The analytical method of cytokine quantification was validated over the range of 1.2–5000 pg/mL (IL-10) and 2–10000 pg/mL (IL-6) as instructed by the manufacturers. The lower limit of detection of IL-10 and IL-6 were 0.3 pg/mL and 1.7 pg/mL, respectively. The lower limit of detection was calculated using MILLIPLEX Analyst 5.1 (from the Manufacturer’s specification sheet). Intra-assay %CV and inter-assay %CV, precision was reported as 3 and 11 for IL-10, and 5 and 7 for IL-6. The accuracy of the method was 96% for both cytokines.
Ethics approval
This study was granted ethical approval from the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (Study serial no.: NMRR-14-1837-19898).
Statistical analysis
The plasma concentrations were presented as mean ± SE. The Student’s paired t test was used to compare the mean concentrations within the same group of long- and short-term patients, and the Student’s unpaired t test for comparison between different groups. Correlation between IL-6 and IL-10 concentrations were conducted using linear regression. Data were analyzed using Statistical Package for the Social Sciences (SPSS) software program, version 20.0. A value of P < 0.05 was considered statistically significant.
RESULTS
Patient’s demographics
A total of 38 samples of plasma were obtained from 38 patients (one plasma sample for each patient). Among the 38 patients included in the study, 53% (n = 20/38) were from male patients, and 47% (n = 18/38) were from female patients. The mean age for all patients was 50.2 years old ± SD (14.6). The most common diagnosis for which opioid was prescribed for these patients was mechanical back pain 42% (n = 16/38), followed by autoimmune diseases (osteoarthritis and rheumatoid arthritis) 10% (n = 4/38). The most common prescribed opioid was dihydrocodeine 47% (n = 18/38), followed by oxycodone 31% (n = 12/38), fentanyl 11% (n = 4\38), buprenorphine 8% (n = 3/38) and morphine 3% (n = 1/38).
Of the 38 patients, 24% (n = 9/38) belonged to short-term opioid users, and 76% (n = 29/38) were long-term, opioid users. Three samples (2 long-term and one short-term user) were below the lower limit of quantification for both cytokines. Hence, the results of 35 plasma samples were included in the analysis.
Comparison between IL-6 and IL-10 concentrations in patients with short- and long-term opioid therapy
The mean plasma concentration of IL-6 and IL-10 in the long-term users was 125 ± 16.1 pg/mL and 41.3 ± 6.7 pg/mL, respectively. While in the short-term users, the mean plasma concentration of IL-6 and IL-10 was 173.9 ± 13.7 pg/mL and 50 ± 5.8 pg/mL, respectively. The comparison of IL-6 concentration versus IL-10 concentration within the same group revealed that the mean plasma concentration of IL-6 was significantly higher than the corresponding mean concentration of IL-10 in short- and long-term opioid users (P < 0.05). Similarly, the comparison between short- and long-term opioid users demonstrated that short-term opioid users have higher levels of both IL-6 and IL10 concentration than that of long-term opioid users, but both cytokine levels did not reach a statistical significance (P > 0.05).
Correlation between IL-6 and IL-10 concentrations in patients with short- and long-term opioid therapy
To investigate whether the duration of opioid therapy affects the ratio between IL-6 and IL-10, the correlation between both cytokines’ concentration was explored within the same group of short- and long-term users. Interestingly, both cytokines showed a strong correlation (r² = 0.76, P < 0.05) and (r² = 0.72, P < 0.05) for long- and short-term users, respectively [Figures 1 and 2]. which indicates that the increase in IL-6 was accompanied by an increase in IL-10 in both groups.
Figure 1.
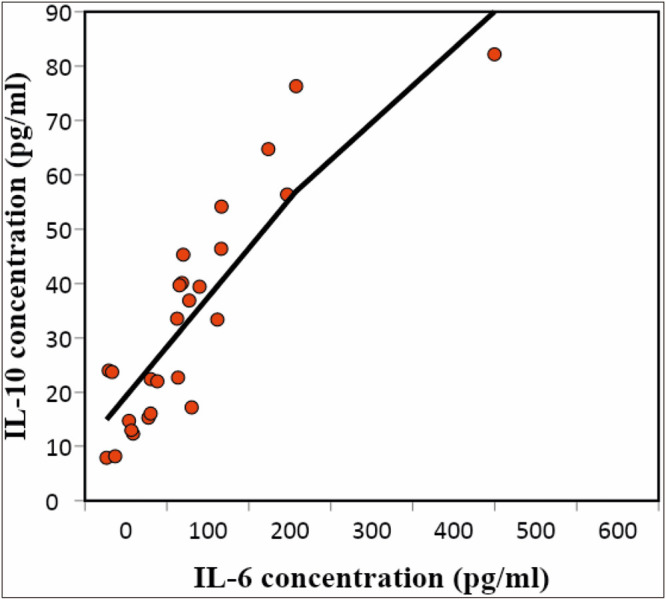
Correlation between IL-6 and IL-10 concentration in long-term patients
Figure 2.
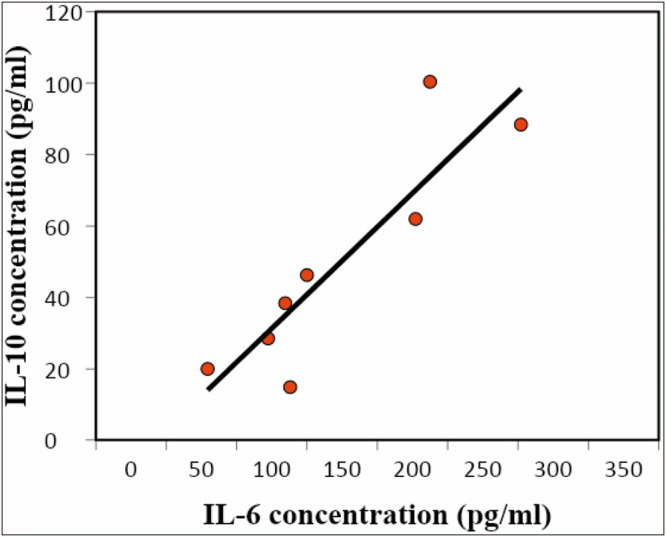
Correlation between IL-6 and IL-10 concentration in short-term patients
DISCUSSION
The main findings from this study showed that there is no statistical difference in the level of the pro-inflammatory cytokine, IL-6, or anti-inflammatory cytokine, IL-10, between short- and long-term opioid users demonstrating that the duration of opioid use was not associated with differences in cytokines level. Moreover, the finding from this study also showed that majority of opioid users tend to use opioid for long terms rather than for short terms as reflected by the majority of patients treated at the pain clinic were belonged to the long-term group.
The IL-6 and IL-10 cytokines analysis showed that both cytokines level were inversely correlated with the duration of opioid use, where short-term users have higher plasma concentration levels of both cytokines than long-term users. Furthermore, the correlation between IL-6 and IL-10 concentrations were explored within each group of short-term and long-term users to study the effect of opioid therapy duration on the cytokines level. This exploration found that both cytokines were similarly correlated in both groups, which indicates that the decrease in IL-6 was accompanied by a correlated decrease in IL-10 when the patients tend to use the opioid therapy for extended periods.
IL-10 is the most potent anti-inflammatory cytokine and it acts to counteract the action of the pro-inflammatory cytokines and hence to ameliorate pain conditions. Our findings showed that extended opioid therapy reduces the concentration of both IL-6 and IL-10 cytokines, and this decrease might be related to opioid tolerance, the pharmacological phenomenon that is characterized by a reduction of opioid analgesic potency over extended periods of exposure.[1,2] Conversely, IL-6 is a pro-inflammatory cytokine, which is linked to various pain conditions and it is reported that IL-6 exacerbate pain when it is upregulated. For example, IL-6 was linked with many pain conditions and was positively correlated with pain intensity in many nociceptive and neuropathic pain conditions. Earlier animal and clinical studies reported that IL-6 and other pro-inflammatory cytokines are upregulated in neuropathic and nociceptive pain conditions. IL-6 was also found significantly increased in neuropathic pain due to herniated intervertebral disc.[3] IL-6 was significantly higher in patients with postherpetic neuralgia compared with herpes zoster patients who did not develop neuropathic pain.[4]
Taken all findings together, it was clear that various chronic pain conditions lead to disturbing the homeostasis of cytokines through upregulation/downregulation of certain cytokines. For this reason, we explored the correlation between IL-6 and IL-10 among short- and long-term opioid users. Interestingly, there was a significant positive correlation between IL-6 and IL-10 within each group, which means that the increase in IL-6 was accompanied by an increase in IL-10, this pattern was observed in short- and long-term groups. Other evidence regarding the balance between different cytokines was noticed as IL-1ß concentration was significantly correlated to IL-6 concentration in healthy controls, whereas no correlation was observed among chronic pain patients.[5]
Similar findings were reported from other studies, where repeated administration of opioid results in upregulation of proinflammatory cytokines which oppose the analgesic effect of opioid and lead to the development of opioid tolerance,[6,6,8] (which in part; could explain the significant increase in IL-6 concentration compared with IL-10 in the present study). However, blockage of certain cytokines such as IL-6, IL-1ß, TNF, and CX3CL1, were reported to delay or prevent the occurrence of opioid tolerance.[9,9,11] Moreover, upregulation of anti-inflammatory cytokines was linked to opposing opioid tolerance.[12]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Calvo M, Dawes JM, Bennett DL. The role of the immune system in the generation of neuropathic pain. Lancet Neurol. 2012;11:629–42. doi: 10.1016/S1474-4422(12)70134-5. [DOI] [PubMed] [Google Scholar]
- 2.Uçeyler N, Valenza R, Stock M, Schedel R, Sprotte G, Sommer C. Reduced levels of antiinflammatory cytokines in patients with chronic widespread pain. Arthritis Rheum. 2006;54:2656–64. doi: 10.1002/art.22026. [DOI] [PubMed] [Google Scholar]
- 3.Wuertz K, Haglund L. Inflammatory mediators in intervertebral disk degeneration and discogenic pain. Global Spine J. 2013;3:175–84. doi: 10.1055/s-0033-1347299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu S-M, Liu YM, An ED, Chen QL. Influence of systemic immune and cytokine responses during the acute phase of zoster on the development of postherpetic neuralgia. J Zhejiang Univ SCIENCE B. 2009;10:625–30. doi: 10.1631/jzus.B0920049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bäckryd E, Ghafouri B, Larsson B, Gerdle B. Plasma pro-inflammatory markers in chronic neuropathic pain: a multivariate, comparative, cross-sectional pilot study. Scand J Pain. 2016;10:1–5. doi: 10.1016/j.sjpain.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Lundborg C, Hahn-Zoric M, Biber B, Hansson E. Glial cell line-derived neurotrophic factor is increased in cerebrospinal fluid but decreased in blood during long-term pain. J Neuroimmunol. 2010;220:108–13. doi: 10.1016/j.jneuroim.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Mendieta D, De la Cruz-Aguilera DL, Barrera-Villalpando MI, Becerril-Villanueva E, Arreola R, Hernández-Ferreira E, et al. IL-8 and IL-6 primarily mediate the inflammatory response in fibromyalgia patients. J Neuroimmunol. 2016;290: 22–5. doi: 10.1016/j.jneuroim.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Uçeyler N, Häuser W, Sommer C. Systematic review with meta-analysis: cytokines in fibromyalgia syndrome. BMC Musculoskelet Disord. 2011;12:245. doi: 10.1186/1471-2474-12-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramer MS, Murphy PG, Richardson PM, Bisby MA. Spinal nerve lesion-induced mechanoallodynia and adrenergic sprouting in sensory ganglia are attenuated in interleukin-6 knockout mice. Pain. 1998;78:115–21. doi: 10.1016/S0304-3959(98)00121-3. [DOI] [PubMed] [Google Scholar]
- 10.Wolf G, Gabay E, Tal M, Yirmiya R, Shavit Y. Genetic impairment of interleukin-1 signaling attenuates neuropathic pain, autotomy, and spontaneous ectopic neuronal activity, following nerve injury in mice. Pain. 2006;120: 315–24. doi: 10.1016/j.pain.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Coe CL, Muller DA, Schell K. Altered cytokine levels in the blood and cerebrospinal fluid of chronic pain patients. J Neuroimmunol. 2008;195:157–63. doi: 10.1016/j.jneuroim.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Grace PM, Maier SF, Watkins LR. Opioid-induced central immune signaling: implications for opioid analgesia. Headache. 2015;55:475–89. doi: 10.1111/head.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]


