Abstract
Background:
Gallbladder perforation is a known morbid sequela of acute cholecystitis, yet evidence for its optimal management remains conflicting. This study compares outcomes in patients with perforated cholecystitis who underwent cholecystectomy at the time of index hospital admission to those who underwent interval cholecystectomy.
Study Design:
A retrospective analysis was conducted of 654 patients from the ACS NSQIP database who underwent cholecystectomy for perforated cholecystitis (2006–2018). Primary outcomes were 30-day postoperative major and minor morbidity, 30-day mortality, and need for prolonged hospitalization. Patient and procedure characteristics and outcomes were compared using Mann-Whitney rank sum test for continuous variables and Pearson chi square tests for categorical variables. A subset analysis was conducted of patients matched on propensity for receiving interval cholecystectomy.
Results:
The 30-day postoperative mortality rate of matched cohort patients undergoing index cholecystectomy was 7% vs. 0% of patients undergoing interval cholecystectomy (P = .01). The 30-day minor morbidity rates were 2% for Index and 8% for Interval patients (P = .06), while the major morbidity rates were 33% for Index and 14% for Interval patients (P = .003). Of the Index patients, 27% required prolonged hospitalization, compared to 6% of Interval patients (P < .001). Results showed similar trends in the unmatched analysis.
Conclusion:
Patients who underwent index cholecystectomy had significantly longer postoperative hospitalizations and higher 30-day postoperative major morbidity and mortality. There were no differences in 30-day minor morbidity. Selected patients with perforated cholecystitis may benefit from operative management on an interval, rather than urgent, basis.
Keywords: gallbladder perforation, perforated cholecystitis, interval cholecystectomy
Précis
This retrospective study used American College of Surgeons NSQIP data (2006–2018) to analyze patients with perforated cholecystitis and evaluate differences in postoperative outcomes based on timing of cholecystectomy. Patients who underwent index cholecystectomy had significantly longer postoperative hospitalization and higher 30-day postoperative major morbidity and mortality than those who underwent interval cholecystectomy.
Graphical Abstract

INTRODUCTION
Although uncommon, gallbladder perforation (GBP) is a particularly morbid sequela of acute calculous cholecystitis. GBP has an incidence of 2–11% (1, 2), predominantly affecting older males and those with chronic diseases (3, 4). While rare, perforated cholecystitis poses a significant healthcare burden with poorer outcomes compared to non-perforated cholecystitis, including longer operations, increased complications, increased ICU admissions, longer hospital length of stay (LOS), and higher mortality (3–5). Given its morbidity, improving the management of perforated cholecystitis has clear clinical importance.
Perhaps owing to its infrequency, consensus regarding the optimal management of perforated cholecystitis is lacking (2–7). The Tokyo guidelines recommend that patients with severe cholecystitis and associated organ dysfunction (Grade III) undergo early laparoscopic cholecystectomy or elective cholecystectomy after resolution of sepsis with percutaneous cholecystostomy, depending on the patient’s operative candidacy and access to specialists (8, 9). The ideal timing of surgery for patients who are critically ill from perforated cholecystitis is unclear. While some have demonstrated a benefit of early cholecystectomy for perforated cholecystitis (3, 7), others have shown better clinical outcomes with initial percutaneous drainage, suggesting the superiority of delayed surgery (6, 10). Moreover, most existing data on perforated cholecystitis arise from small, single-center studies, and do not explore differences in outcomes in patients undergoing cholecystectomy during index hospital admission versus those undergoing surgery on an interval basis (1, 2, 6, 7). To our knowledge, no large multi-center study to date has investigated differences in outcomes in perforated cholecystitis based specifically on timing of definitive management.
The present study utilizes a large multi-center database to compare outcomes in patients with perforated cholecystitis who underwent an index operation at the time of admission to those who underwent interval cholecystectomy. Primary outcome measures of interest are hospital LOS, morbidity, and mortality. The goal of this study is to evaluate outcomes in patients with perforated cholecystitis following index versus interval cholecystectomy with the aim of identifying the optimal timing of surgery for this rare but clinically significant condition.
METHODS
Patients from the 2006–2018 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Participant Use Files who underwent cholecystectomy (as identified by Current Procedure Terminology codes of 47562, 47563, 47564, 47600, 47605, or 47610) for a principal operative diagnosis of perforated cholecystitis [as identified by an International Classification of Diseases-9th Modification (ICD-9) code of 575.4 or an ICD-10 code of K82.2] were included for this study (11).
The primary predictor variable for our study was timing of cholecystectomy (Index Admission versus Interval). We classified procedures as Interval if they met the following three conditions: (1) they were performed in the absence of preoperative systemic inflammatory response syndrome (SIRS), sepsis, or septic shock, (2) they were not classified as an emergency procedure, and (3) they occurred on the initial day of hospitalization. Procedures that were performed in the presence of SIRS or sepsis, those which were classified as emergency, and/or those which occurred beyond the initial day of hospitalization were classified as being performed during the index admission for perforated cholecystitis.
Additional predictor variables included patient age, gender, diabetes mellitus, chronic obstructive pulmonary disease, congestive heart failure, end stage renal disease, chronic steroid use, bleeding disorder (including patients who were on anticoagulation or antiplatelet medications at the time of their procedure), American Society of Anesthesiologists physical status classification, duration of operation, and surgical approach. The outcome variables for our analysis were 30-day postoperative mortality and postoperative morbidity and need for prolonged postoperative hospitalization. Minor complications included superficial and/or deep incisional surgical site infection, urinary tract infection, and deep venous thrombosis. Major complications included organ/deep space surgical site infection, wound dehiscence, pneumonia, pulmonary embolism, renal failure requiring dialysis, stroke, myocardial infarction, bleeding, and septic shock. Prolonged postoperative hospitalization was defined as having a postoperative length of hospital stay greater than or equal to the 75th percentile stratified by surgical approach (≥6 days for laparoscopic procedures, ≥12 days for open procedures) (12).
Patient and procedure characteristics and postoperative outcomes of patients undergoing cholecystectomy for perforated cholecystitis at the time of index admission versus as an interval procedure were compared using Mann-Whitney rank sum test for continuous variables and Pearson chi square tests for categorical variables. In an attempt to adjust for potentially confounding factors that are not captured by ACS NSQIP but which may influence the decision about timing of operation for perforated cholecystitis (such as duration of preoperative symptoms or degree of anticipated acute inflammation), we conducted a separate analysis using a subset of our overall study cohort that was matched on propensity for receiving interval cholecystectomy. For this analysis, a logistic regression model was created to estimate the likelihood of undergoing cholecystectomy on an interval basis (rather than at the time of index admission), with the model including the aforementioned patient- and procedure-related factors as potential predictors of procedure timing. The logit coefficients thus derived were used to calculate a propensity score for interval cholecystectomy for each patient from the overall study cohort. These propensity scores were then used to create an evenly matched of Index Admission and Interval Cholecystectomy patients using a caliper matching algorithm (with a caliper distance of 0.005), with controls being used only once in the matching. Comparisons of the characteristics and outcomes of this matched cohort of patients were then performed using McNemar chi square tests for categorical variables and Wilcoxon signed rank sum tests for continuous variables. All statistical analyses were performed using Stata 16.0 software (StataCorp, College Station, TX).
RESULTS
A total of 654 patients with perforated cholecystitis were included in our analysis, of whom 566 (86.5%) underwent cholecystectomy at index admission and 88 (13.5%) on an interval basis. The preoperative and procedure characteristics of the entire study cohort, stratified by timing of cholecystectomy, are shown in Table 1. As seen in Table 1, of the 566 patients who underwent index cholecystectomy, 189 (33%) were over the age of 75, compared to 15 (17%) of the 88 patients who underwent an interval operation (P = .002). In the Index Admission group, 161 patients (28%) had diabetes mellitus compared to 16 patients (18%) in the Interval group (P = .04), and 93 Index patients (16%) had a bleeding disorder compared to 2 Interval patients (2%) (P < .001). A laparoscopic approach was used in 38% of index and in 49% of interval operations (P = .05), and the median operative time was 100 minutes for both groups.
Table 1.
Characteristics of Overall Cohort Patients Undergoing Cholecystectomy for Perforated Cholecystitis, Stratified by Timing of Operation
| Characteristic | Procedure timing | p Value | |
|---|---|---|---|
| Index admission (n = 566) | Interval (n = 88) | ||
| Age ≥75 y, n (%) | 189 (33) | 15 (17) | 0.002 |
| Sex, female, n (%) | 196 (35) | 37 (42) | 0.18 |
| Diabetes mellitus, n (%) | 161 (28) | 16 (18) | 0.04 |
| COPD, n (%) | 52 (9) | 7 (8) | 0.71 |
| Congestive heart failure, n (%) | 25 (4) | 1 (1) | 0.14 |
| End stage renal disease, n (%) | 18 (3) | 1 (1) | 0.29 |
| Chronic steroid use, n (%) | 36 (6) | 4 (5) | 0.51 |
| Bleeding disorder, n (%) | 93 (16) | 2 (2) | <0.001 |
| Operative time, mins, median (IQR) | 100 (75–133) | 100 (61.5,139.5) | 0.48 |
| Laparoscopic approach, n (%) | 215 (38) | 43 (49) | 0.05 |
IQR, interquartile range
The 30-day postoperative mortality rate of patients undergoing cholecystectomy at index admission was 7% compared to 0% for patients undergoing interval cholecystectomy (P = .004). The 30-day minor postoperative morbidity rates were 6% for Index Admission patients and 8% for Interval patients (P = .48), while the 30-day major postoperative morbidity rates were 32% for Index Admission patients and 15% for Interval patients (P = .001). A total of 169 (30%) of Index Admission patients required prolonged postoperative hospitalization, compared to 6 (7%) of Interval patients (P < .05).
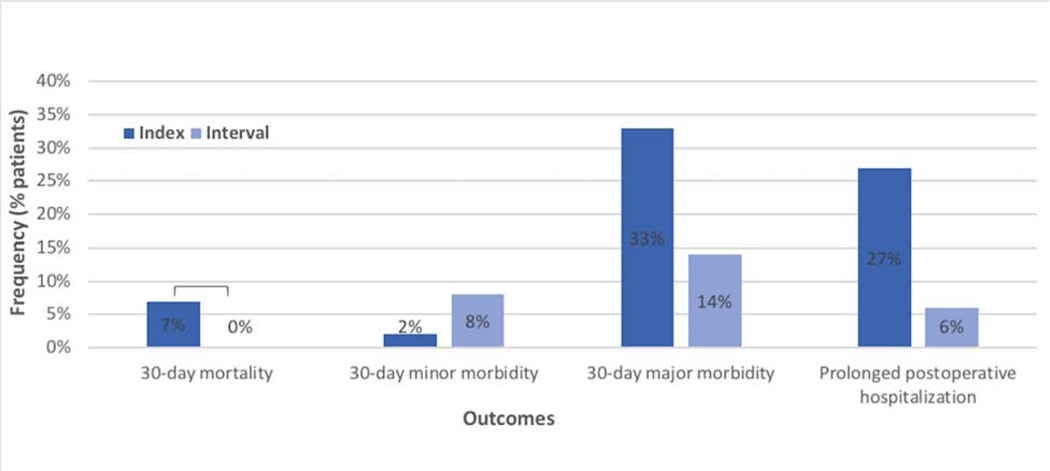
Propensity score matching techniques yielded a cohort of 85 Index Admission and 85 Interval Cholecystectomy patients that were well-matched for all known patient and procedure characteristics, as evidenced by the lack of statistical or clinical differences in these characteristics between the two groups of the matched cohort (see Table 2). The postoperative outcomes of this matched cohort are shown in Figure 1.
Table 2.
Characteristics of Propensity Score-Matched Cohort of Patients Undergoing Cholecystectomy for Perforated Cholecystitis, Stratified by Timing of Operation
| Characteristic | Procedure timing | p Value | |
|---|---|---|---|
| Index admission (n = 85) | Interval (n = 85) | ||
| Age ≥75 y, n (%) | 15 (18%) | 15 (18%) | 1.0 |
| Sex, female, n (%) | 35 (41%) | 36 (42%) | 0.16 |
| Diabetes mellitus, n (%) | 17 (20%) | 16 (19%) | 0.32 |
| COPD, n (%) | 7 (8%) | 4 (5%) | 0.08 |
| Congestive heart failure, n (%) | 0 (0%) | 1 (1%) | 0.32 |
| End stage renal disease, n (%) | 0 (0%) | 1 (1%) | 0.32 |
| Chronic steroid use, n (%) | 2 (2%) | 4 (5%) | 0.32 |
| Bleeding disorder, n (%) | 2 (2%) | 2 (2%) | 1.0 |
| Operative time, mins, median (IQR) | 100 (74–134) | 101 (62–139) | 0.10 |
| Laparoscopic approach, n (%) | 41 (48%) | 41 (48%) | 0.08 |
IQR, interquartile range
Figure 1.
Comparison of postoperative outcomes of matched cohort of patients undergoing interval vs index cholecystectomy.
As seen in Figure 1, the 30-day postoperative mortality rate of matched cohort patients undergoing cholecystectomy at index admission was 7% compared to 0% of patients undergoing interval cholecystectomy (P = .01). The 30-day minor postoperative morbidity rates were 2% for Index Admission patients and 8% for Interval patients (P = .06), while the 30-day major morbidity rates were 33% for Index patients and 14% for Interval patients (P = .003). Of the Index Admission patients, 27% required prolonged postoperative hospitalization, compared to 6% of Interval patients (P < .001).
DISCUSSION
This study demonstrated no significant differences in operative time and surgical approach between index and interval operations for perforated cholecystitis. In both unmatched and propensity matched cohorts, patients undergoing index cholecystectomy had significantly higher 30-day postoperative mortality, higher 30-day postoperative major morbidity, and more frequent need for prolonged postoperative hospitalizations than patients undergoing interval cholecystectomy. There were no significant differences in 30-day postoperative minor morbidity between the index and interval groups. Our results suggest that selected patients with perforated cholecystitis may benefit from operative management on an interval, rather than urgent, basis.
Several groups have evaluated outcomes in perforated cholecystitis based on timing of management with variable results. Stefanidis et al. (3) demonstrated increased morbidity, mortality, ICU admissions, and hospital LOS with late operative intervention for perforated cholecystitis, and advocated for early cholecystectomy within 24 hours. Similarly, Lo et al. (7) found that urgent laparoscopic cholecystectomy (LC) had comparable outcomes with shorter LOS compared to delayed LC for GBP. In contrast, Huang et al. (6) showed higher survival rates in patients with GBP who underwent PC compared to those who underwent initial open cholecystectomy. More broadly, Kim et al. (10) found that delayed LC after PC decreased complication rates in complicated acute cholecystitis, and Melloul et al. (13) showed increased perioperative morbidity following emergency cholecystectomy compared to PC for septic patients with cholecystitis; however, neither of these studies was specific to perforated cholecystitis.
These studies provide conflicting results and have a number of limitations. First, the study by Stefanidis et al. (3) was single-institution with a small number of patients with GBP (n=30). Next, Huang et al. (6) only compared PC to open cholecystectomy, and did not evaluate LC. While Lo et al. (7) did compare urgent and delayed LC, their small single-center study (n=74) excluded patients with critical illness and had significantly younger patients in their early LC group. Finally, the studies by Kim et al. (10) and Melloul et al. (13) included patients with complicated acute cholecystitis and sepsis from cholecystitis, respectively, and their results therefore may not be applicable more narrowly to perforated cholecystitis. Furthermore, Melloul et al. (13) compared early surgery to PC rather than to delayed surgery.
Our study is therefore the first to our knowledge to utilize a large, multi-center database to specifically investigate patients with perforated cholecystitis and evaluate outcomes based on timing of operative management. Compared to the aforementioned studies, ours has a larger sample size, only includes patients with a principal operative diagnosis of perforated cholecystitis, and specifically evaluates outcomes based on timing of definitive management. The differences noted between our two groups remain significant in our subset analysis of an evenly matched cohort of patients undergoing index and interval cholecystectomy, despite no significant differences between the groups in age, gender, operative time, comorbidities such as COPD and diabetes mellitus, and use of laparoscopy.
We postulate that the improved postoperative outcomes in patients who underwent interval cholecystectomy may be attributed both to patients’ increased clinical stability at the time of operation, as well as to decreased acute inflammation and improved operative ease in the delayed setting. These results have important implications, as existing protocols for the treatment of acute cholecystitis such as the Tokyo guidelines do not provide algorithms specifically for perforated cholecystitis (8, 9). Findings such as ours may shift the operative paradigm for perforated cholecystitis toward interval cholecystectomy and thereby decrease morbidity, mortality, and costs associated with prolonged inpatient hospitalizations following index cholecystectomy.
This study has several limitations. First, it retrospectively utilizes data from the NSQIP database which was not created for the purpose of this study, and is therefore inherently subject to selection bias. We assumed that the ICD codes for GBP were related to perforated cholecystitis, as we were unable to make a distinction between acute cholecystitis and other causes of GBP. Another limitation was our inability to delineate if the patients who underwent interval cholecystectomy were treated in the interim with PC. We were also unable to explicitly determine the timing of operation relative to hospital admission, thus performance of interval cholecystectomy was inferred based on three criteria: (1) absence of preoperative sepsis, (2) lack of classification as an emergency procedure, and (3) occurrence on the initial day of hospitalization. There is therefore the possibility that interval cholecystectomies that did not meet these criteria were not captured by our study, and/or that cholecystectomies that were not in fact performed on an interval basis (i.e., performed during index admission) were unintentionally included in the interval group. Given that interval cholecystectomies are not typically performed until sepsis has resolved and patients have returned to near baseline health status, it seems unlikely that this would have excluded a significant number of critically ill patients from the interval group; however, there remains the possibility that this inference altered our group composition and results in other ways. Finally, we lacked information about re-admissions and interventions performed between initial presentation and time of definitive surgical management in the interval group, and we were therefore unable to draw conclusions about differences in health care resource utilization between groups.
CONCLUSIONS
Our study found that patients with perforated cholecystitis who underwent index cholecystectomy had significantly higher 30-day postoperative major morbidity and mortality, as well as longer postoperative hospitalizations, compared to patients who underwent interval cholecystectomy. These findings suggest that patients with perforated cholecystitis who are selected to undergo operative management may benefit from doing so on an interval, rather than urgent, basis. Future studies should prospectively investigate the optimal interval between diagnosis of perforated cholecystitis and definitive operative management, as well as differences in hospital resource utilization and costs between index and interval surgery, to further standardize the treatment of this rare but clinically significant condition.
Acknowledgments
Support: This work was supported by the National Cancer Institute of the NIH, Grant #T32CA090217.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Selected for the 2020 Southern Surgical Association Program
Footnotes
Disclosure Information: Nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Derici H, Kara C, Bozdag AD, et al. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol 2006;12:7832–7836. 10.3748/wjg.v12.i48.7832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ausania F, Guzman Suarez S, Alvarez Garcia H, et al. Gallbladder perforation: morbidity, mortality and preoperative risk prediction. Surg Endosc 2015;29:955–960. 10.1007/s00464014-3765-6 [DOI] [PubMed] [Google Scholar]
- 3.Stefanidis D, Sirinek KR, Bingener J. Gallbladder perforation: Risk factors and outcome. J Surg Res 2006;131:204–208. 10.1016/j.jss.2005.11.580 [DOI] [PubMed] [Google Scholar]
- 4.Jansen S, Doerner J, Macher-Heidrich S, et al. Outcome of acute perforated cholecystitis: a register study of over 5000 cases from a quality control database in Germany. Surg Endosc 2017;31:1896–1900. 10.1007/s00464-016-5190-5 [DOI] [PubMed] [Google Scholar]
- 5.Jansen S, Stodolski M, Zirngibl H, et al. Advanced gallbladder inflammation is a risk factor for gallbladder perforation in patients with acute cholecystitis. World J Emerg Surg 2018;13. 10.1186/s13017-018-0169-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang CC, Lo HC, Tzeng YM, et al. Percutaneous transhepatic gall bladder drainage: A better initial therapeutic choice for patients with gall bladder perforation in the emergency department. Emerg Med J 2007;24:836–840. 10.1136/emj.2007.052175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo HC, Wang YC, Su LT, Hsieh CH. Can early laparoscopic cholecystectomy be the optimal management of cholecystitis with gallbladder perforation? A single institute experience of 74 cases. Surg Endosc 2012;26:3301–3306. 10.1007/s00464-012-2344-y [DOI] [PubMed] [Google Scholar]
- 8.Miura F, Takada T, Strasberg SM, et al. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2013;20:47–54. 10.1007/s00534012-0563-1 [DOI] [PubMed] [Google Scholar]
- 9.Okamoto K, Suzuki K, Takada T, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci John Wiley & Sons, Ltd 2018;25:55–72. 10.1002/jhbp.516 [DOI] [PubMed] [Google Scholar]
- 10.Kim HO, Ho Son B, Yoo CH, Ho Shin J. Impact of delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Surg Laparosc Endosc Percutaneous Tech 2009;19:20–24. 10.1097/SLE.0b013e318188e2fe [DOI] [PubMed] [Google Scholar]
- 11.Anon. User guide for the 2018 ACS NSQIP Participant Use Data File (PUF). American College of Surgeons National Surgical Quality Improvement Program. 2019. Available at: https://www.facs.org/-/media/files/quality-programs/nsqip/nsqip_puf_userguide_2018.ashx. Accessed March 19, 2020.
- 12.Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg 1999;230:251–259. 10.1097/00000658-19990800000016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melloul E, Denys A, Demartines N, et al. Percutaneous Drainage versus Emergency Cholecystectomy for the Treatment of Acute Cholecystitis in Critically Ill Patients: Does it Matter? World J Surg 2011;35:826–833. 10.1007/s00268-011-0985-y [DOI] [PubMed] [Google Scholar]