Abstract
Background
the need for social distancing midst the COVID-19 pandemic has forced ophthalmologists to innovate with telemedicine. The novel process of triaging emergency ophthalmology patients via videoconsultations should reduce hospital attendances. However, the safety profile of such services were unknown.
Methods
in this retrospective cohort study, we reviewed case notes of 404 adults who used our videoconsultation service from 20/04/2020 to 03/05/2020. We compared these to 451 patient who attended eye casualty in person at the same time who were deemed not to require same day ophthalmic examination.
Findings
patients seen by videoconsultations tended to be younger (Median = 43 years, Inter-quartile range = 27 vs Median= 49 years, Inter-quartile range = 28)'. More males used the face-to-face triage (55%) while more females used videoconsultation (54%)%. Fewer patients seen by videoconsultations required specialist review compared to face-face triage [X2 (1, N = 854) = 128.02, p<0.001)]. 35.5% of the patients initially seen by videoconsultation had unplanned reattendance within 1 month, compared to 15.7% in the group initially seen in person. X2 (1, N = 234) = 7.31, p = 0.007). The rate of actual harm was no different (at 0% for each method), with perfect inter-grader correlation when graded independently by two senior ophthalmologists. 97% of patients seen on the video platform surveyed were satisfied with their care.
Interpretation
we demonstrate comparable patient safety of videoconsultations at one-month follow-up to in person review. The service is acceptable to patients and reduces the risk of COVID-19 transmission. We propose that videoconsultations are effective and desirable as a tool for triage in ophthalmology.
Funding
the research supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology who fund PT and DS's time to conduct research. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Keywords: Ophthalmology, Telemedicine, Tele-ophthalmology, Triage, Digital health
Research in context.
Evidence before this study
We searched the PubMed database for articles that assess the safety of remote video-based triage systems in emergency ophthalmology before and during the coronavirus pandemic on 1st August 2020 using the search terms (‘telemedicine AND ophthalmology AND safety’ OR ‘emergency AND ophthalmology AND telemedicine’) with no language or time restrictions. However, no published works were found about the safety of remotely triaging emergency ophthalmology patients.
Added value of this study
With the increasing adoption of telemedicine services in healthcare driven simultaneously by increasing digital telecommunications capabilities and the need for social distancing to mitigate COVID-19 transmission, there is an urgent need to assess the safety of these new services. This study assesses the safety of a new video-based remote tele-ophthalmology service adopted at a large eye hospital. It investigates if any patients had come to harm as a result of not having been seen in person within 1 month following the assessment, and compare the outcomes with those who were triaged in person at the emergency service. This pilot shows that no patients came to harm 1 month following their being triaged in either group. This suggests that the safety profile of this remote triage service is comparable to that of in person triage during the COVID-19 pandemic.
Implications of all the available evidence
This study suggests that remote video-based triage systems are safe for more widespread adoption particularly when balanced against the risks of exposure to transmissible diseases during a pandemic. This study is limited in its size, duration of follow-up, and those potentially lost to follow-up and thus further work needs to be done to assess the safety of such services on a larger scale, and to inform how to improve these new services. Additionally, we provide outcomes from patient satisfaction surveys which suggest that patients welcome these new services. There is evidence to suggest some difference in the demographics seeking physical and remote care, and more work is needed in this area to ensure adequate provision to all patients without exclusion.
Alt-text: Unlabelled box
1. Introduction
Coronavirus disease 2019 (COVID-19) swept across the globe in 2020. Social distancing, as a non-pharmaceutical intervention in reducing transmission rates, has been a central strategy in mitigation of the pandemic. Fundamental changes to the delivery of healthcare have had to be implemented at speed. Existing services were reconfigured and digital technologies were adopted in innovative new ways [1]. With the expectation that community transmission of COVID-19 will continue, these new models of care are set to become the new norm.
Ophthalmology has long adopted telemedicine for image-based screening, most notably with great success for diabetic retinopathy, but has also trialed it for diagnosis and triage [2,3]. Given the particular risk to ophthalmologists and patients of this virus, predominantly transmitted by inhalation of droplets and aerosol, there is an urgent need to reduce in-person ophthalmic examinations which demand close proximity [[4], [5], [6]]. Tele-ophthalmology services have been rapidly upscaled in response to this need [[7], [8], [9], [10], [11]]. Additionally, attendances can be avoided if non-sight-threatening pathologies can be managed remotely with advice and medication. A study prior to the COVID-19 pandemic from our hospital demonstrated around 30% of attendances to accident and emergency were non-acute [12]. Combining effective triage with telemedicine should enable effective identification of patients needing to attend in person, thus allowing those with less acute pathologies to be managed remotely.
The safety of remote triage without supplementary clinical information such as imaging compared to face-to-face triage have not yet been demonstrated to our knowledge. The safety profile of such new services, especially implemented at speed without the usual rigorous quality assessments, must be shown before expansion of services. Importantly, new services should aim to be as equitable as possible in reaching all patients, particularly those who are vulnerable. In this study the primary outcome question is if patients came to harm as a result of being kept away from hospital during the first peak of the COVID-19 pandemic through the use of videoconsultations for triaging in the emergency department.
2. Methods
In this retrospective cohort study, we reviewed electronic notes of adult patients who attended either the videoconsultation platform remotely or face-to-face casualty at Moorfields Eye Hospital NHS Foundation Trust, from 20/04/2020 to 03/05/2020 during the national lockdown imposed in England in response to COVID-19. Within the National Health Service in England, patients seeking emergency eye care during this time were advised to attend their local eye hospital. We confined our study to patients who lived within a 10-mile radius of the hospital.
Patients chose to either attend in person or use the videoconsultation process. The videoconsultation service was only available during normal working hours and therefore the same only patients who attended in person during those hours were included in the study period. Both services were freely available to patients with no limitations on the access of each. The virtual triage was a weblink with access to a virtual waiting room, whence the ophthalmologist was able to connect to the patient by a video call.
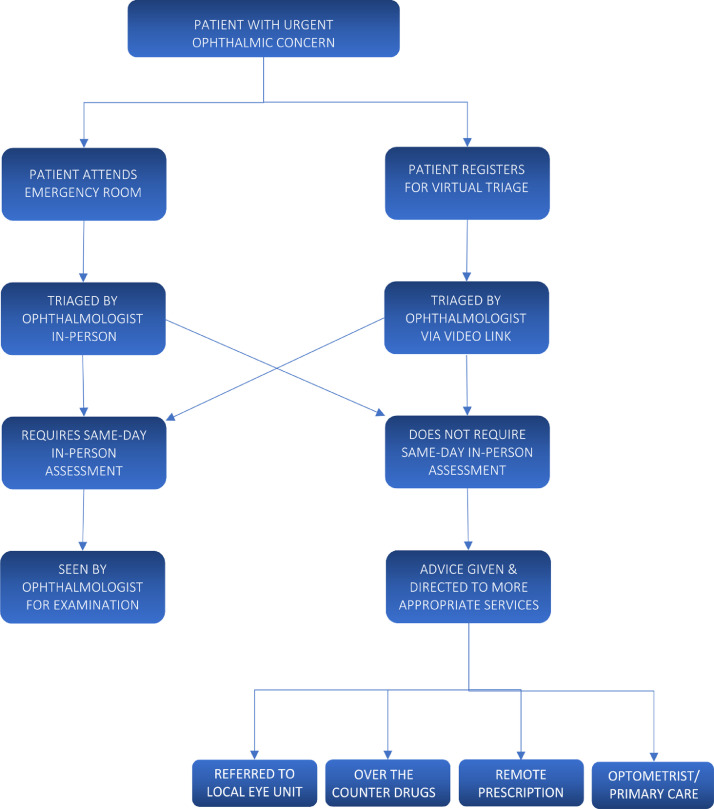
Patients triaged via both methods were managed either in hospital in the emergency service the same day, or managed without same-day in-person review with advice, prescription, direction to primary care provider or pharmacists, or direct onward referral to subspecialty services, referred directly to subspecialty services, or directed to care outside of the hospital, such as their primary care physician, advice on over the counter medication, or a prescription provided without full in person review. Fig. 1 shows virtual triage process. Patients from both pathways have an early assessment by an experienced ophthalmologist immediately after registration, to triage patients to the appropriate clinical services. Patients with presentations requiring further examination or investigation were sent to either the Emergency Room, Urgent Care Centre or Specialist clinics. Those that do not require review were either issued treatment or given verbal advice and discharged directly. Amongst patients who were discharged without further review, we reviewed our database to record any re-attendances within one month following discharge.
Fig. 1.
The triage process.
Data was accessed from hospital systems by the authors (AJ, CK, AT, JOL, AL). Details were recorded on the numbers of re-attenders, reasons for review, and potential harm caused by a delay in treatment or misdiagnosis at the point of initial triage. Harm was determined by case review of all re-attenders by two senior ophthalmologists (GH and PT). Inter-rater reliability was also assessed. In order to compare reattendance rates and patient harm with the standard practice of face-to-face triage, we reviewed electronic notes of patients who attended triage in person over the same period, during the same hours as the teleconsultation service, at the times when the videoconsultation service was open.
We separately collected patient feedback from those who used the videoconsultation service at a later date (from 19/5/2020 to 30/6/2020) via an online survey immediately following their assessment. We created and validated a 10-item patient questionnaire which qualitatively and quantitatively assessed numerous domains, including satisfaction and preference of videoconsultations compared to attending casualty. The survey was designed to automatically initiate at the end of each videoconsultations. Data was analyzed by proportion of patients responding with a 5-point (Likert) scoring system, ranging from “strongly agree” to “strongly disagree”. Key themes from free text responses were categorized according to common properties. Subgroup analysis was performed based on whether the patients had used the videoconsultation service before.
The study protocol was reviewed and approved by the Clinical Audit Assessment Committee of Moorfields Eye Hospital NHS Foundation Trust (audit number 646), and consent was not required. It adhered to the principles of the Declaration of Helsinki and the reporting of this study conforms to the STROBE statement [13].
3. Power calculation
There is currently limited data on effect sizes for the detection of harm via telemedicine platforms. A power calculation was conducted using G*Power 3.1.9.4. Given the incidence of harm is likely to be low we used a small effect size of 0•1, a two-sided alpha of 0•05 and a power of 80%. This produced a total sample size requirement of 785.
4. Statistical analysis
Analyses were conducted using SPSS version 24 (IBM Corp., Armonk, New York). Normality of the data was assessed using the Shapiro-Wilk test. Categorical data was analyzed using the Pearson Chi-Squared Test or Fisher's exact Test with adjusted standardized residuals or <−2 or >+2 considered significant. Inter-rater agreement for categorical data was analyzed using a Cohen's Kappa. Non-parametric independent continuous data was analyzed using the Mann-Whitney U test. Graders GH and PT are senior ophthalmologists (each more than 10 years experience). Potential harm was defined as diseases that may have progressed to irreversible loss of vision or other significant irreversible morbidity or death if the patient had not sought further medical input. Harm was defined as irreversible loss of vision or other significant irreversibly morbidity or death.
5. Role of funders
The funders National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology support the research undertaken by PT and DAS. The other authors have no funders to declare.
6. Results
A total number of 451 patients were seen face-to-face while 404 patients were seen via videoconsultation. All were confirmed to be eligible for this study. One patient from the videoconsultation group was excluded due to being abroad and was not able to follow re-attendance advice.
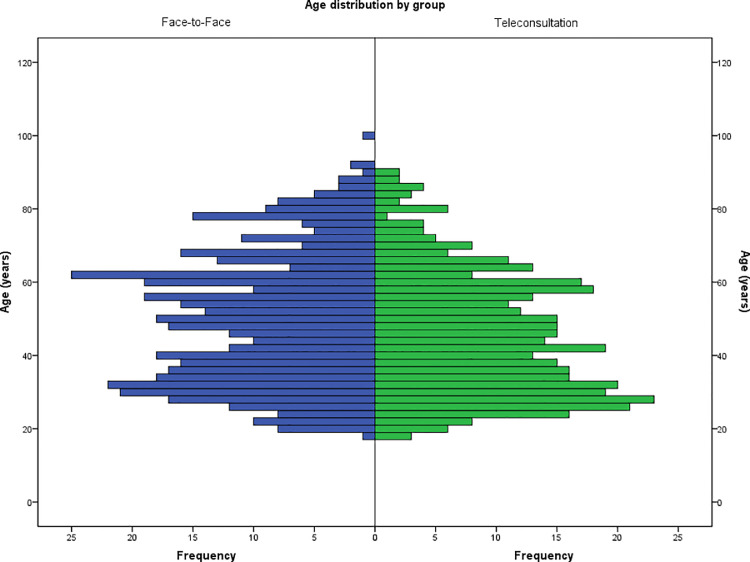
Patients attending face-to-face tended to be older than those using the videoconsultation platform (Median of 49 years versus 43 years). A Mann-Whitney U test indicated this difference was statistically significant U(NAE= 451, NAA= 403) = 96,536, z = −3•10, p = 0•002.
There was a statistically significant difference in the use of face-to-face triage compared to video consultations based on sex. Men were more likely to use face-to-face triage (55%), while women were more likely to use teleconsultation (54%) X2 (1,N = 852) = 6•02, p = 0•014.
Fig. 2.
Comparison of the age distribution between those attending face-to-face versus videoteleconsultation.
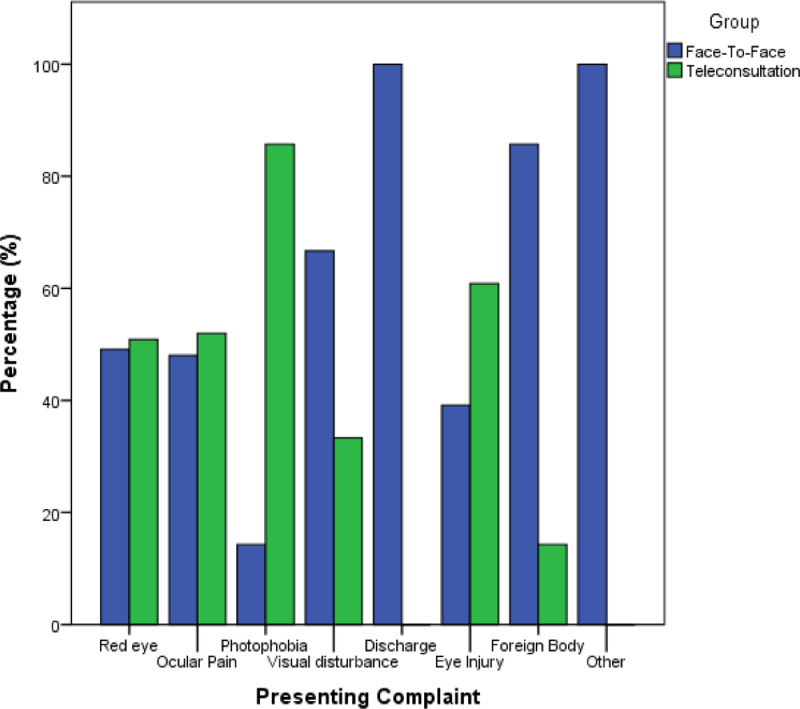
There was a statistically significant difference in the type of presenting complaints seen by face-to-face triage compared to videoconsultation p<0.001. 86% of those with photophobia and 52% of those with ocular pain underwent videoconsultations. 67% of those with visual disturbance and 86% of those with foreign body presented face-to-face. This can be seen in Fig. 3.
Fig. 3.
Comparison of the presenting complaints between those attending face-to-face versus videoconsultation.
Fewer patients triaged via videoconsultation were deemed to require in-person ophthalmic review compared to those seen via face-to-face triage platform X2 (1, N = 854) = 128•02, p<0•001).
Patients who initially attended for videoconsultation and discharged without onward in-person examination were more likely to reattend to the emergency service within 1 month compared to those who initially attended in-person. X2 (1, N = 234) = 7.31, p = 0•007).
There were statistically significantly differences in the nature of presenting complaints between those triaged via videoconsultations and those presenting via face to face triage (p<0•001). This was due to higher rates of visual disturbance and foreign body presentations via face-to-face triage, and photophobia presentations via videoconsultation.
When we look at potential harm, there was poor inter-rater reliability (κ=0•10, p = 0•324) between graders. However, higher rates of potential harm were found amongst patients seen on the video triage service. This was found to be statistically significant for both Grader A (p<0•001) and Grader B (p = 0•006). When looking at actual harm, there was perfect inter-rater reliability (100% rater agreement). No difference in rates of actual harm were found between both triage methods. Both graders found a 0% rate of actual harm.
We performed 2022 videoconsultations over the 6 weeks between 19th May and 30th June 2020. Of these, 603 online survey responses (30%) were captured. 568 (28%) complete entries were included for analysis. 97% agreed or strongly agreed that they were satisfied with their overall care, and 55% preferred using video consultations to coming into eye casualty. 403 patients (71%) had never used the videoconsultation service before, compared to 165 who had previously used the service (29%). There was no statistically significant difference in the overall satisfaction (p = 0.89) or the proportion of patients who preferred using videoconsultations to coming into eye casualty (p = 0.12) between the two subgroups.
Most free text responses expressed appreciation and praise praise for the service. Negative comments related to suboptimal video quality. Several patients with disabilities or medical conditions were keen to point out that the availability of videoconsultations circumvented the need for cumbersome and risky (considering the pandemic) travel. Some elderly patients required help to use the videoconsultations platform. Useful suggestions included introduction of audio cues so that the visually impaired could know what is happening while waiting for their consultation.
7. Discussion
In 854 patients over a two-week period, we observed that no patients came to harm after videoconsultation triage and without an in-person review during a 1 month follow-up period. However, when a retrospective review of case notes comparing videoconsultation and face-to-face triage, there were significantly more cases of potential harm for videoconsultation triage.
Several reasons may account for this. Firstly, videoconsultation triage may be inferior to a face-to-face encounter for identifying clinical signs that require further examination; for example assessing pupil size or facial asymmetry, and may be further degraded by poor internet connection. The underlying disease and severity in the two groups will likely differ, with different risk profiles. Finding no actual harm in either group could be due to the need for a bigger sample size, but others have also demonstrated only small numbers of patients experience delay in treatment as a result of misdiagnosis when triaged remotely [14]. Additionally because the risks of virtual triage was unknown at the time of the study, we gave comprehensive patient education encouraging them to return in case of any concern.
This study is limited by its retrospective design, and relied on patients to re-attend when their symptoms changed or worsened. However, the collaborative network of eye units across the Greater London region proactively shares information if and when a patient attends another eye department in the region, particularly where a patient has come to harm. Additionally, the exclusion of patients living more than 10-miles from the hospital reduced the likelihood of their attending anther emergency unit during the national lockdown. Our hospital was the single ophthalmology service within Greater London offering a 24h a day, 7 days a week emergency care during the study period, and offered the first remote triage service locally that was directly accessible to patients without referrals. Most private providers were not offering outpatient care during this time, and the private outpatient clinic of our unit, one of the largest in the region, was closed. Therefore any patients seeking care elsewhere would have likely attended another emergency unit within the public system within our collaborative network. We actively sought other local units to inform us of any patients who came to harm as a result of an unsatisfactory face-to-face person or virtual consultation. There were none that we and they were aware of during the study period. Thus this bias, and the limited sample size, is likely to have resulted in only a limited underestimation of patients who have come to harm.
We will use the findings from this early pilot to inform a second study to assess patient safety as the service is more established, and behaviors and policies adapt to COVID-19. Potential harm can be more usefully quantified when we move to a larger group of graders with consensus on each case where there is disagreement between graders. As the digital maturity of our network grows, we will be able to better follow-up patients who seek care elsewhere via the new regional integrated care system where we will gain access to patient records across the region from other providers. Additional analysis into the details of the presenting complaints in the two groups and their severity will also aid future risk stratification and service planning.
Further studies to characterize the case-mix of those electing for virtual review compared to in-person attendance will help to define the risk of harm for each group. The 1 month follow-up period of this study limits the longer-term outcomes of patients, and this should be addressed in future studies.
Interestingly we note women are more likely to use the videoconsultation service, which echoes the findings from the United States Centre for Medicare and Medicaid (CMS) with 30% of female and 25% of male beneficiaries receiving telemedicine consultations during this pandemic period [15].
We note significantly higher proportion of patients from videoconsultation triage did not require in-person review compared to those who attended in person. That is to say, patients who attended in person were more likely to be referred onwards for same day emergency review. This is likely to be fairly independent of the clinicians, as the same team of ophthalmologists work in both services. The cause is likely multifactorial. Patients with severe eye disorders are more likely to attend for a face-to-face review, as shown by more physical attendances where the chief complaint is blurred vision. We did not have sufficient data to comment further on this as no detailed analysis of the clinical presentations were undertaken.
The COVID-19 pandemic has forced the widespread adoption of telemedicine [16,17]. Being able to demonstrate the safety of a virtual service compared to its physical counterpart is powerful, particularly given the obvious public health advantages midst a pandemic. Further studies need to be carried out to evaluate its safety outside of a pandemic setting, though studies such as this will be valuable for the continued service planning during the COVID-19 pandemic, and future pandemics. Given though that these services were established for the first time during the pandemic, and are set to stay with us in some format for the foreseeable future, we believe our findings offer a useful contribution generalizable to other providers of emergency eye services planning in the current and future climate, in spite of its weaknesses. Furthermore, this pandemic has highlighted the needed for healthcare providers and governments to be prepared for future pandemics [5], and a record of health seeking behavior from this time may still be valuable despite the shortcomings already discussed.
Table 1.
Comparison between face-to-face vs videoconsultation triage: referred to in-person evaluation with an ophthalmologist.
| Method of Triage |
Total | ||||
|---|---|---|---|---|---|
| Videoconsultation | Face-to-face | ||||
| Patients triaged to in-person evaluation | No | Total | 183 | 51 | 234 |
| % within Method | 45•4% | 11•3% | 27•4% | ||
| Adjusted Residual | 11.2 | −11•2 | |||
| Yes | Total | 220 | 400 | 620 | |
| % within Method | 54•6% | 88•7% | 72•6% | ||
| Adjusted Residual | −11•2 | 11•2 | |||
| Total | Total | 403 | 451 | 854 | |
| % within Method | 100•0% | 100•0% | 100•0% | ||
Table 2.
Comparison between face-to-face vs videoconsultation triage reattendance rate within 1 month.
| Method of Triage |
Total | ||||
|---|---|---|---|---|---|
| Videoconsultation | Face-to-face | ||||
| Did the patient re-attend ? | No | Count | 118 | 43 | 161 |
| % within Method | 64•5% | 84•3% | 68•8% | ||
| Adjusted Residual | −2•7 | 2•7 | |||
| Yes | Count | 65 | 8 | 73 | |
| % within Method | 35•5% | 15•7% | 31•2% | ||
| Adjusted Residual | 2.7 | −2.7 | |||
| Total | Count | 183 | 51 | 234 | |
| % within Method | 100•0% | 100•0% | 100•0% | ||
We note telemedicine might appear to be a solution to connect the more vulnerable and less mobile to healthcare providers, patients may be excluded by the infrastructure of available telecommunications networks at sufficient speeds, or by lack of digital literacy or access to equipment. Those who could see the greatest benefit through this shift towards telehealth offerings, such as the elderly and disabled, paradoxically could be less likely to be able to access these services [18].
Our finding that younger patients tended to use the videoconsultation service is also consistent with the CMS reported data [15]. This may be due to greater digital literacy. However, the findings do not demonstrate true preference, as not all patients were aware of the options of care available. Given the major burden of disease in ophthalmology affects the elderly, it is important that such fundamental changes in care access and delivery should consider the impact on all service users, and existing services should continue in parallel while new pathways are trialed. Our study did exclude the paediatric population therefore cannot be used to apply to those under the age of 18. Given we did not find any actual harm in this study, we are unable to conclude if videoconsultations are safer for any particular population. Larger studies, perhaps with stratification by presenting complaint, will offer greater insight into which specific groups can more safely undergo video-based triaged in ophthalmology. There also needs to be urgent work to ensure equitable access to care, recognizing that the causes of inequitable access for telemedicine are multi-faceted and can differ from traditional healthcare access, such as individual skill, current health status, access to infrastructure, as well as training and support [19].
Medicolegal implications should be considered as the profession, legislation and regulatory bodies, respond. There is also evidence suggesting over-prescribing in telemedicine [20], which could have significant consequences such as in antimicrobial resistance. Economic implications must be studied, and the implications for state and private providers considered.
We have demonstrated that video-based remote triaging for patients with urgent ophthalmic conditions is comparable to face-to-face triage in terms of demonstrable harm to patients. Whilst efforts to find the right balance between accessibility and quality of care must continue, we recognize that this balance may shift midst a pandemic of significant mortality and morbidity. We propose that virtual triage using videoconsultation for emergency eye conditions during the COVID-19 pandemic is a safe adjunct to traditional emergency care provision, with ongoing safety evaluation.
Contributors
All listed authors meet the criteria for authorship agreed upon by the International Committee of Medical Journal Editors and are in agreement with the content of the manuscript.
Li: design, literature review, data collection, data analysis, draft manuscript, critical revisions, final approval
A Thomas: literature review, data collection, critical revisions, final approval
Kilduff: data collection, figures, critical revisions, final approval
Logeswaran: data analysis, figures, literature review, writing, critical revisions, final approval
Ramessur: data collection, data analysis, writing, critical revisions, final approval
Jaselsky: data collection, data analysis, final approval
Sim: design, critical revisions, final approval
Hay: design, critical revisions, final approval
P Thomas: design, critical revisions, final approval
Data sharing statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, therefore supporting data is not available.
Funding
The research supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology who fund PT and DS's time to conduct research. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Declaration of Competing Interest
Li: The author declares no competing interests., A Thomas: The author declares no competing interests., Kilduff: The author declares no competing interests., Logeswaran: The author declares no competing interests., Ramessur: The author declares no competing interests., Jaselsky: The author declares no competing interests., Sim: Dr. Sim reports other from Bayer, Allergan, Novartis, Roche, grants from Health Education England, grants from Moorfields Eye Charity, personal fees from Big Picture Medical Ltd, grants from Oculocare Ltd, outside the submitted work., Hay: The author declares no competing interests., P Thomas: Dr. Thomas reports personal fees from Novartis, personal fees from Abbvie, personal fees from Go Visibly, personal fees from Santen, outside the submitted work.
Acknowledgments
None.
Contributor Information
Gordon R. Hay, Email: gordon.hay3@nhs.net.
Peter B.M. Thomas, Email: peterthomas2@nhs.net.
References
- 1.Ting D.S.W., Carin L., Dzau V., Wong T.Y. Digital technology and COVID-19. Nat Med. 2020;26(4):459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caffery L.J., Taylor M., Gole G., Smith A.C. Models of care in tele-ophthalmology: a scoping review. J Telemed Telecare. 2019;25(2):106–122. doi: 10.1177/1357633X17742182. [DOI] [PubMed] [Google Scholar]
- 3.Tang R.A., Morales M., Ricur G., Schiffman J.S. Telemedicine for eye care. J Telemed Telecare. 2005;11(8):391–396. doi: 10.1177/1357633X0501100803. [DOI] [PubMed] [Google Scholar]
- 4.Li J.O., Lam D.S.C., Chen Y., Ting D.S.W. Novel Coronavirus disease 2019 (COVID-19): the importance of recognizing possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104(3):297–298. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 5.Li J.O., Shantha J., Wong T.Y. Preparedness among ophthalmologists: during and beyond the COVID-19 Pandemic. Ophthalmology. 2020;127(5):569–572. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saleem S.M., Pasquale L.R., Sidoti P.A., Tsai J.C. Virtual ophthalmology: telemedicine in a Covid-19 era. Am J Ophthalmol. 2020;216:237–242. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sim D.A., Thomas P., Canning C. Tackling COVID-19 with telemedicine. 2020. https://theophthalmologist.com/subspecialties/tackling-covid-19-with-telemedicine.
- 8.Kang S., Thomas P.B.M., Sim D.A., Parker R.T., Daniel C., Uddin J.M. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye (Lond) 2020;34(7):1193–1195. doi: 10.1038/s41433-020-0953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wickham L., Hay G., Hamilton R. The impact of COVID policies on acute ophthalmology services-experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye (Lond) 2020;34(7):1189–1192. doi: 10.1038/s41433-020-0957-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams A.M., Kalra G., Commiskey P.W. Ophthalmology practice during the coronavirus disease 2019 pandemic: the University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. 2020:1–9. doi: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS Forth Valley. Pioneering virtual eye project extended to help respond to Covid-19. 2020. https://nhsforthvalley.com/virtual-emergency-eye-consultations-extended-to-help-respond-to-covid-19/.
- 12.Hau S., Ioannidis A., Masaoutis P., Verma S. Patterns of ophthalmological complaints presenting to a dedicated ophthalmic accident and emergency department: inappropriate use and patients' perspective. Emerg Med J. 2008;25(11):740–744. doi: 10.1136/emj.2007.057604. [DOI] [PubMed] [Google Scholar]
- 13.Vandenbroucke J.P., von Elm E., Altman D.G. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. doi: 10.1097/EDE.0b013e3181577511. [DOI] [PubMed] [Google Scholar]
- 14.Bourdon H., Jaillant R., Ballino A. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: experience with 500 patients in March and April 2020. J Fr Ophtalmol. 2020;43(7):577–585. doi: 10.1016/j.jfo.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verma S. Early impact of CMS expansion of medicare telehealth during COVID-19. 2020. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/.
- 16.Cohen E., Cohen M.I. COVID-19 will forever change the landscape of telemedicine. Curr Opin Cardiol. 2020;36(1):110–115. doi: 10.1097/HCO.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 17.Sommer A.C., Blumenthal E.Z. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol. 2020;258(11):2341–2352. doi: 10.1007/s00417-020-04879-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noel K., Ellison B. Inclusive innovation in telehealth. NPJ Digit Med. 2020;3(89) doi: 10.1038/s41746-020-0296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levin-Zamir D., Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018;15(8) doi: 10.3390/ijerph15081643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffman L.C. Shedding light on telemedicine and online prescribing: the need to balance access to health care and quality of care. Am J Law Med. 2020;46(2–3):237–251. doi: 10.1177/0098858820933497. [DOI] [PubMed] [Google Scholar]