Abstract
Background:
A recent trend in the field of primary knee osteoarthritis suggests that elastic tape (e.g., K-tape) relieves pressure on the joint by increasing tension on fascia. Elastic tape (ET) is expected to decrease pain and help patients to recover faster.
Objective:
This systematic review aims to analyze the efficacy of this method on pain in patients with knee osteoarthritis by using The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score.
Data sources:
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standard for reporting systematic reviews of qualitative and quantitative evidence, we used 3 electronic databases, PubMed, Cochrane, and EBSCO, and grey literature was included.
Study eligibility criteria:
Articles were screened for duplicates, screened for inclusion and exclusion criteria, and critically appraised.
Participants and Intervention:
People older than 45 years old with primary osteoarthritis (OA) and application of ET.
Study appraisal and synthesis methods:
2005 Oxford standard.
Results:
Amongst all the papers found, 6 Randomized Control Trials (RCT) for a total of 392 participants met the criteria and were included in our review. Three papers out of the 6 RCT had low risks of bias. When the ET was compared to sham taping, the results show no to moderate decreases of WOMAC scores in patients with primary knee osteoarthritis.
Limitations:
We focused on a single index test (WOMAC) and could not perform meta-analyses.
Conclusion and implications of key findings:
Although ET does not provide strong adverse outcomes, our data do not support the use of ET as a treatment alone because of too slight reductions of the WOMAC score for reaching clinical efficiency. Thus, our systematic review shows no strong evidence regarding the use of elastic taping for pain improvement in patients with primary knee osteoarthritis.
Keywords: elastic tape, elastic taping, k tape, kinesio taping, knee osteoarthritis, pain, sham tape, sham taping, Western Ontario and McMaster Universities Osteoarthritis Index
What is known
A growing number of patients with knee OA seek to be treated with Elastic taping without clear evidence of efficiency.
What is new
Our systematic review shows that elastic taping has a limited effect on the WOMAC score, and studies showing a more substantial effect have important biases. Although ET does not provide strong adverse outcomes, our data do not support the use of ET as a treatment alone because of too slight reductions of the WOMAC score for reaching clinical efficiency
1. Introduction
Knee osteoarthritis (OA) is one of the most common forms of articular degeneration, which causes pain, swelling, and reduced motion.[1,2] It affects 30 million adults in the United States for a cost of US $16.5 billion per year, and it is considered one of the leading causes of disability and pain in older people.[3] Whatever the causes of knee OA,[4,5] several non-operative and chemical interventions exist for reducing the pain associated. For instance, education, weight loss, support devices,[6] modifications of activities of daily living, exercise and physical therapy, and taping[2] have been a part of conservative OA management with efficiency.
Taping has been used for almost 40 years in knee OA management as a method of patellar alignment correction.[7] A new method of taping called elastic taping ([ET] i.e., Kinesio taping, K-tape) gained interest in the Physical Medicine & Rehabilitation community, and a growing number of patients with knee OA seek to be treated with it. ET, popular in sports injuries, has an adhesive material with a high stretch capacity and can be used on various musculoskeletal injuries.[8] This method of taping claims to reduce pain in people suffering from myofascial pain syndrome (i.e., muscle pain due to myofascial trigger points[6]). Furthermore, it is proposed as an inexpensive, safe way to treat OA with few side effects.[8] There are many proposed mechanisms for how elastic tape works to reduce pain, stiffness, and functional limitations. All mechanisms work based on fascia's properties and the ability of the elastic tape to modify its positioning along with the muscle fibers.[9] This positional change might lead to a decrease in the activation of nociceptors, pain receptors within the muscle.[10–12] The first mechanism proposes that the decreased activation is due to a decrease in the stretch of damaged tissue[10] while the other mechanism suggests the decrease of fluid build-up in the surrounding tissue leads to less pressure on the nociceptors.[12] In the case of knee OA, tape is applied by placing 1 medial and 1 lateral “I”-strap with 1 “I”-strap over the patella. “I”-strap means the tape's full width is applied and is not cut into different parts. This is mainly used to limit edema and pain. The strap across the patellar is applied in maximum knee flexion. The base of the tape is applied at the tibial tuberosity at maximum tension over the patella, ending at the lower third of the quadriceps femoris muscle. The medial and lateral straps are applied along the collateral medial and lateral ligaments with the knee in 45° of flexion.[13] Regardless of the technique used, rehabilitation practitioners treat patients with knee OA using ET without clear evidence of efficiency. Although several randomized control trials have been already published, results are scattered and there are no guidelines for integrating ET in a rehabilitation program.
Our systematic review aims to answer the following question: “What effect does elastic taping (e.g., K-tape) have on pain in patients with primary knee OA compared to the sham taping?” We decided to investigate Randomized Control Trials (RCTs) that tested sham taping vs ET techniques with the gold standard of OA pain evaluation, the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain severity scale.
2. Methods
This review used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines with (Patient [people older than 45 years old with primary OA]; Intervention: application of elastic tape [K-tape, Kinesio Tape], Comparison: sham taping [defined as non-elastic tape or tape applied non-tensioned taping], and Outcome measure [pain level based on the WOMAC scale]). Our study is exempt from ethics approval because we will be collecting and synthesizing data from previous clinical trials in which informed consent has already been obtained by the trial investigators.
2.1. Data sources and searches
From October 2019 to November 2019, we searched 3 databases: PubMed, Cochrane, and EBSCO, with a new search in grey literature. The Mesh terms used were: (knee OA) and ([kinesio taping] or [K tape] or [elastic tape]) and ([sham taping] or [sham tape]), and (pain).
2.2. Study selection
After removing duplicates, we screened the remaining articles with our inclusion and exclusion criteria (Table 1). Twelve articles were removed, leaving 6 articles for critical appraisal. Two separate investigators (SH and GM) conducted critical appraisals for each screened article. All articles and critical appraisals sheets associated were recorded in both a hard and an online drive secured with a password or limited access.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
| Knee osteoarthritis | Post operative |
| Randomized Control Trial Studies | |
| Primary Osteoarthritis | |
| Over 40 Yr Old | |
| WOMAC (The Western Ontario and McMaster Universities Arthritis Index) | |
| English Language | |
| Peer Reviewed Published Paper |
2.3. Data extraction and quality assessment
Regarding the risk of bias assessment, 2 investigators (SH and JM) performed critical appraisals on the selected articles, assessing the articles for internal validity, equal treatment of patients apart from the intervention, and unbiased practices based on the 2005 Oxford standard. In case of conflict in the appraisal between the 2 investigators mentioned previously, a senior investigator (JPhB) performed critical appraisals as a third investigator. Losses to follow-up were further analyzed for quantity and rationale. Reasons for discontinuation included: withdrawing to seek treatment, allergic reaction to the tape, sickness, knee pain, and loss of interest.
2.4. Data synthesis and analysis
Relative risk (RR) reduction was calculated following the 2005 University of Oxford guidelines where a RR >1 indicates that the treatment increased the risk of the outcome according to the following formula:
3. Results
The study selection process (Fig. 1) followed the PRISMA guidelines. A total of 25 articles were retrieved (PubMed = 1, Cochrane = 7, EBSCO = 7, and Grey Literature = 10). Seven duplicate studies were removed, resulting in a total of 18 articles. These articles were subjected to a preliminary screening based on a predetermined inclusion and exclusion criteria (Table 1). Only 6 articles met the criteria and were critically appraised. Thus, our systematic review consists of 6 articles with 392 participants in the 6 studies.[8,13–17]
Figure 1.
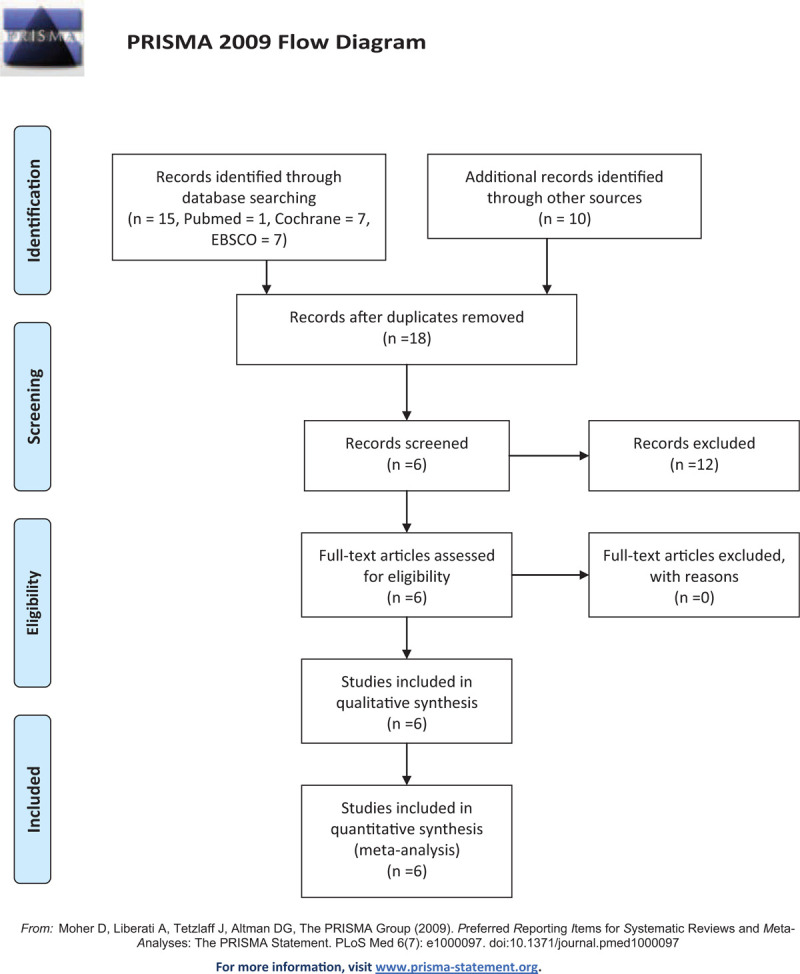
PRISMA 2009 Flow Diagram.
Here, we separated the summary of the findings based on their outcomes. First, a summary of the findings of 5 papers which measured total WOMAC score – Castrogiovanni et al (2016), Wageck et al (2016), Mutlu et al (2017), Aiyegbusi et al (2018), Rahlf et al (2019) – is displayed in Table 2 with the authors, interventions for control and experimental groups, sample sizes, results of total WOMAC mean within-group difference and their RR. Figure 2 is a plot of this RR in function of treatment duration. Second, a summary of the findings of 4 papers which measured component WOMAC scores (with the Pain subscale) – Hinman et al (2003), Castrogiovanni et al (2016), Aiyegbusi et al (2018), Rahlf et al (2019) – is displayed in Table 3 with the RR of pain, stiffness, and function WOMAC scores. Figure 3 is a plot of this RR in function of treatment duration. An RR value <1 indicates that the effect of the treatment compared to the control group results in improved pain, stiffness, and function, thus leading to a decrease in WOMAC scores. An RR value >1 indicates that the effect of the treatment compared to the control group results in more pain, stiffness, and loss of function than the control group thus leading to an increase in WOMAC scores. Here, we present the RR as an indicative comparison between ET and ST by using percentage changes. Finally, we present a summary of risk of bias within studies in Table 4.
Table 2.
Summary of the findings from the 5 RCT with total WOMAC scores analyzed with authors, study name, interventions for control and experimental groups, results of outcome measures, and the relative risk.
| Authors | Interventions | n (group) = sample size | Total WOMAC mean within-group difference | Relative risk reduction between ET and ST |
| Castrogiovanni et al (2016)[8] | Elastic Tape Group (ET) Sham Tape Group (ST) No Tape Group (NT) | N (ET) = 19 N (ST) = 19 N (NT) = 19 | Total WOMAC - 15 Days ET: 6.9 ST: 6.1 NT: 3.5 Total WOMAC- 90 Days ET: 6.8 ST: 6.8 NT: 6.6 | 15 D = 0.974 90 D = 0.936 |
| Wageck et al (2016)[15] | Elastic Tape Group (ET) Sham Tape Group (ST) | N (ET) = 19 N (ST) = 20 | Total WOMAC – 4 Days ET: 9 ST: 12 Total WOMAC – 19 Days ET: 6 ST: 8 | 4 D = 0.969 19 D = 0.949 |
| Mutlu et al (2017)[16] | Elastic Tape Group (ET) Sham Tape Group (ST) | N (ET) = 20 N (ST) = 19 | Total WOMAC (Normalized scale) - 30 Days ET: 4.7 ST: 2.7 | 30 D = 0.84 |
| Aiyegbusi et al (2018) [17] | Elastic Tape Group (ET) Sham Tape Group (ST) | N (ET) = 15 N (ST) = 15 | Total WOMAC – Instantaneous ET: 29.1 ST: 7.6 | Instantaneous = 0.328 |
| Rahlf et al (2019)[13] | Elastic Tape Group (ET) Sham Tape Group (ST) No Tape Group (NT) | N (ET) = 47 N (ST) = 47 N (NT) = 47 | ET: 7.8 ST: 2.5 NT: 1.2 | 3 D = 0.821 |
A relative risk <1 means the effect of the treatment caused a decrease in pain while a relative risk >1 means that the treatment caused pain.
Figure 2.
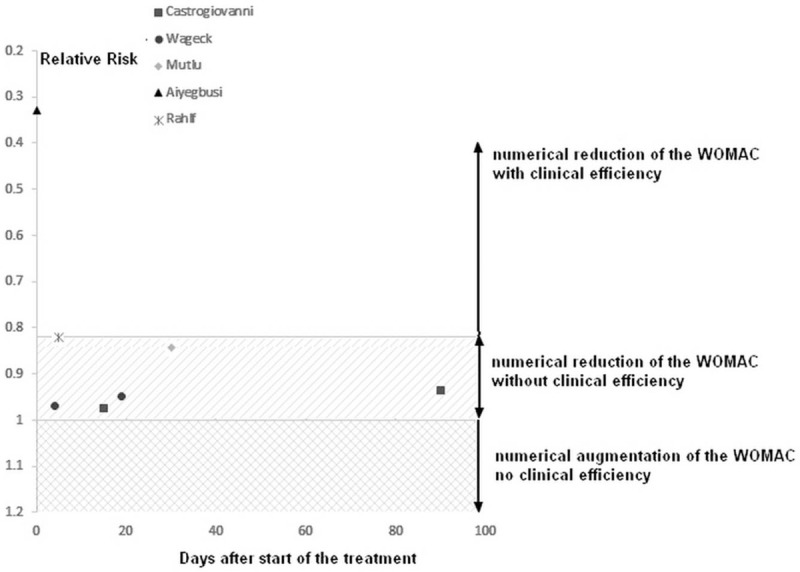
Graphical representation of the relative risk from the 5 studies, Castrogiovanni et al (2016), Wageck et al (2016), Mutlu et al (2017), Rahlf et al (2019), and Aiyegbusi et al (2018) where the total WOMAC score was provided with treatment duration in days.
Table 3.
Summary of the findings from the 4 RCT with component WOMAC scores (pain, stiffness, and function) analyzed with authors, study name, interventions for control and experimental groups, results of outcome measures, and the relative risk.
| Authors | Interventions | N (group) = sample size | RR of Pain WOMAC Score between ET and ST | RR of Stiffness WOMAC Score between ET and ST | RR of Function WOMAC Score between ET and ST |
| Hinman et al (2003)[14] | Elastic Tape Group (ET) Sham Tape Group (ST) No Tape Group (NT) | N (ET) = 29 N (ST) = 29 N (NT) = 28 | 21 D = 1.006 42 D = 1.091 | 21 D = 0.972 42 D = 1.128 | |
| Castrogiovanni et al (2016)[8] | Elastic Tape Group (ET) Sham Tape Group (ST) No Tape Group (NT) | N (ET) = 19 N (ST) = 19 N (NT) = 19 | 15 D = 1.005 90 D = 0.892 | 15 D = 0.975 90 D = 0.894 | 15 D = 0.967 90 D = 0.954 |
| Aiyegbusi et al (2018)[17] | Elastic Tape Group (ET) Sham Tape Group (ST) | N (ET) = 15 N (ST) = 15 | Instantaneous = 0.346 | Instantaneous = 0.124 | Instantaneous = 0.349 |
| Rahlf et al (2019)[13] | Elastic Tape Group (ET) Sham Tape Group (ST) No Tape Group (NT) | N (ET) = 47 N (ST) = 47 N (NT) = 47 | 3 D = 0.819 | 3 D = 0.752 | 3 D = 0.832 |
A relative risk <1 means the effect of the treatment caused a decrease in pain while a relative risk >1 means that the treatment caused pain.
Figure 3.
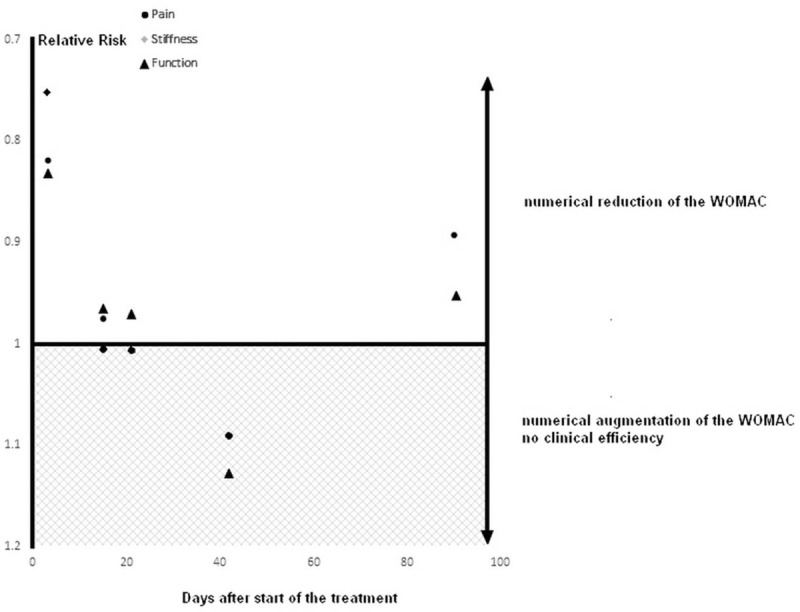
Graphical representation of the relative risk from the 3 studies Hinman et al (2003), Castrogiovanni et al (2016), Rahlf et al (2019), where subscales (pain, stiffness, and function) of the WOMAC score were provided with treatment duration in days.
Table 4.
Summary of risk of bias within studies.
| Authors | Was the assignment of patients to treatments randomized | Were the groups similar at the start of the trial? | Aside from the allocated treatment, were groups treated equally? | Were all patients who entered the trial accounted for? | Were measures objective or were the patients and clinicians kept “blind” to which treatment was being received? |
| Hinman et al (2003)[14] | Yes | Yes | Yes | Yes | Yes |
| Castrogiovanni et al (2016)[8] | Yes | Yes | Yes | Yes | Yes |
| Wageck et al (2016)[15] | Yes | Unclear | Yes | No | No |
| Mutlu et al (2017)[16] | Yes | Yes | Yes | Yes | Yes |
| Aiyegbusi et al (2018)[17] | No | Unclear | Yes | Unclear | No |
| Rahlf et al (2019)[13] | Yes | Yes | Yes | Yes | No |
4. Discussion
Our systematic review provides new references pertaining to ET efficiency for patients suffering from knee OA, in relation to WOMAC score items and timeline. Although, ET does not provide strong adverse outcomes regarding the items evaluated in the WOMAC scale, there is no strong evidence suggesting that ET is efficient by itself at reducing the WOMAC scale.
The total WOMAC incorporates 3 dimensions of the scale: pain, stiffness, and physical function. The total score is given by the sum of the three-dimensional scores of the questionnaire and varies from 0 to 96, with high scores indicating a more inferior health status. Here, 5 studies Castrogiovanni et al (2016), Wageck et al (2016), Mutlu et al (2017), Aiyegbusi et al (2018), Rahlf et al (2019) examined the effects of ET using a total WOMAC score rather than just the pain portion of the scale. Castrogiovanni et al (2016), Wageck et al (2016), Mutlu et al (2017), and Rahlf et al (2019), showed a decrease between 3% to 16% on the total WOMAC score, indicating that pain, stiffness, and functional limitations may have decreased due to the correct application of elastic tape. To evaluate whether these results were clinically relevant or not, recent evidence has shown that the minimum important change for the total WOMAC score is 17% (i.e., the change is not due to uncertainty in the score after this threshold) for people with Total Knee Arthroplasty.[18] Minimum important change is the smallest change in score that a patient will be able to perceive in their clinical state which in this case is the smallest WOMAC score change needed to have a perceivable effect to quality of life. If we translate this information to our population and our system of quantification, it means that clinical efficiency starts from 17% decrease of the total WOMAC score (i.e., RR under 0.83). Out of these 5 studies, only Aiyegbusi et al (2018) and Rahlf et al (2017) are under the 0.83 threshold. Regarding Aiyegbusi et al (2018), the authors investigated the instantaneous effect of ET on the knee (Day 1) but did not evaluate the effect thereafter. Furthermore, this study had a higher risk of bias due to lack of
-
1.
randomization,
-
2.
blinding,
-
3.
similar groups at the start and
-
4.
reporting subject dropout rate in their experiment (Table 4).
Rahlf et al (2017) only evaluated the effect of ET in the short term (3 days post tape) while using a non-double blinded protocol which makes it more susceptible to bias.
When looking at studies which provided quantitative evaluation for the 3 dimensions of the WOMAC scale: pain, stiffness, and physical function (Table 3), minimum important change was also used to evaluate clinical efficiency. For pain a 21% (i.e., RR under 0.79) change was needed and which only Aiyegbusi et al (2018) presented with a threshold below 0.79. For stiffness a 13% (i.e., RR under 0.87) change was needed both Aiyegbusi et al (2018) and Rahlf et al (2017) presented with a threshold below 0.87. For stiffness a 16% (i.e., RR under 0.84) change was needed both Aiyegbusi et al (2018) and Rahlf et al (2017) presented with a threshold below 0.84. Thus, our results do not show strong evidence in support of the clinical efficiency of ET because the reductions of the WOMAC score are too small to meet minimum important change. On the contrary, Hinman et al (2003) showed ET had a negative effect[14] with decreased effectiveness compared to sham tape 21 days post application on the WOMAC component for pain and 42 days post application on the WOMAC component both for pain and function.
Similarly to our review, a meta-analysis on elastic taping and its effects on pain function in patients with knee OA by Lu et al (2018) made claims that WOMAC scores improved with Kinesio tape when compared to Sham tape.[19] However, it seems that this meta-analysis was partially flawed. According to our critical appraisal of this review, the authors plotted and analyzed WOMAC scores from 2 studies Cho et al (2015), Aydoğdu et al (2017),[20,21] whereas both these studies did not measure WOMAC scores. Furthermore, Lu et al (2018) claimed that Aydoğdu et al (2017) used sham tape as their control group. However, Aydoğdu et al (2017) used no tape as their control group. These misleading claims serve as our reasoning for rejecting findings from this recently published systematic review. Regarding the limitations of our systematic review, we acknowledge that
-
1.
we focused on a single index test (WOMAC) and
-
2.
it will be of interest to perform analyses like sensitivity or subgroup analyses.
However, most of the study lack of supplementary dataset that will help to perform meta-analysis.
To summarize, the initial approach for patients with signs of knee OA are non-operative treatments (e.g., exercise, electrical stimulation and tapping) that aim at relieving pain, improving function, and limiting disabilities.[22] However, when pain persists for more than 21 to 42 days, there is an indication of the use of advance imaging (e.g., Magnetic Resonance Imagery) to predict the need for added treatment.[23] In our systematic review, none of the studies reached the minimum important change to provide clinically efficient results in pain reduction evaluated through the WOMAC score for more than 21 to 42 days after starting ET. Thus, other interventions, besides conservative exercise, could be considered, such as electrical stimulation, pain relievers, anti-inflammatories, and corticosteroids when deciding to reduce knee pain.[2,3,6]
5. Conclusion
Our systematic review provides new references pertaining to ET efficiency for patients suffering from knee OA, in relation to WOMAC score items and timeline. We show no evidence regarding the use of ET for pain improvement for more than 21 to 42 days in patients with primary knee osteoarthritis. Although ET does not provide strong adverse outcomes, our data do not support the use of ET as a treatment alone because of too slight reductions of the WOMAC score for reaching clinical efficiency.
Acknowledgments
We want to express our gratitude to the City University of New York College of Staten Island Physical Therapy program staff and students for making this systematic review possible.
Author contributions
Conceptualization: Jean-Philippe Berteau.
Formal analysis: Stephan Heddon, Nicole Saulnier, Jorge Mercado, Michelle Shalmiyev.
Investigation: Stephan Heddon.
Supervision: Jean-Philippe Berteau.
Writing – original draft: Stephan Heddon.
Writing – review & editing: Jean-Philippe Berteau.
Footnotes
Abbreviations: OA = osteoarthritis, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCT = Randomized Control Trials, RR = relative risk, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
How to cite this article: Heddon S, Saulnier N, Mercado J, Shalmiyev M, Berteau JP. Systematic review shows no strong evidence regarding the use of elastic taping for pain improvement in patients with primary knee osteoarthritis. Medicine. 2021;100:13(e25382).
SH, NS, JM, MS were responsible of the research, SH and JPhB were responsible of the writing, JPhB is the guarantor of the review. No Amendments to our review protocol occurred and the review protocol was not registered.
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Thomas A, Eichenberger G, Kempton C, et al. Recommendations for the treatment of knee osteoarthritis, using various therapy techniques. J Geriatr Phys Ther 2009;32:33–8. [DOI] [PubMed] [Google Scholar]
- [2].Kocyigit F, Turkmen MB, Acar M, et al. Kinesio taping or sham taping in knee osteoarthritis? A randomized, double-blind, sham-controlled trial. Complement Ther Clin Pract 2015;21:262–7. [DOI] [PubMed] [Google Scholar]
- [3].Novak S, Guerron G, Zou Z, et al. New guidelines for electrical stimulation parameters in adult patients with knee osteoarthritis based on a systematic review of the current literature. Am J Phys Med Rehabil 2020;1.doi:10.1097/PHM.0000000000001409. [DOI] [PubMed] [Google Scholar]
- [4].Deshpande BR, Katz JN, Solomon DH, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity: symptomatic knee OA in the US. Arthritis Care Res 2016;68:1743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Samson DJ, Grant MD, Ratko TA, et al. Treatment of primary and secondary osteoarthritis of the knee. Evid Report Technol Assess 2007;157:1–57. [PMC free article] [PubMed] [Google Scholar]
- [6].Wu W-T, Hong C-Z, Chou L-W. The Kinesio taping method for myofascial pain control. Evid Based Complement Alternat Med 2015;2015:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother 1986;32:215–23. [DOI] [PubMed] [Google Scholar]
- [8].Castrogiovanni P, Di Giunta A, Guglielmino C, et al. The effects of exercise and Kinesio tape on physical limitations in patients with knee osteoarthritis. J Funct Morphol Kinesiol 2016;1:355–68. [Google Scholar]
- [9].Parreira P, do CS, Costa L, et al. Kinesio taping to generate skin convolutions is not better than sham taping for people with chronic non-specific low back pain: a randomised trial. J Physiother 2014;60:90–6. [DOI] [PubMed] [Google Scholar]
- [10].Williams & Wilkins, Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed.1998;1056. [Google Scholar]
- [11].Gusella A, Bettuolo M, Contiero F, et al. Kinesiologic taping and muscular activity: a myofascial hypothesis and a randomised, blinded trial on healthy individuals. J Bodyw Mov Ther 2014;18:405–11. [DOI] [PubMed] [Google Scholar]
- [12].Reynard F, Vuistiner P, Léger B, et al. Immediate and short-term effects of Kinesio taping on muscular activity, mobility, strength and pain after rotator cuff surgery: a crossover clinical trial. BMC Musculoskelet Disord 2018;19:305.doi:10.1186/s12891-018-2169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rahlf AL, Braumann K-M, Zech A. Kinesio taping improves perceptions of pain and function of patients with knee osteoarthritis: a randomized, controlled trial. J Sport Rehabil 2019;28:481–7. [DOI] [PubMed] [Google Scholar]
- [14].Hinman RS, Crossley KM, McConnell J, et al. Efficacy of knee tape in the management of osteoarthritis of the knee: blinded randomised controlled trial. BMJ 2003;327:135.doi:10.1136/bmj.327.7407.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Wageck B, Nunes GS, Bohlen NB, et al. Kinesio taping does not improve the symptoms or function of older people with knee osteoarthritis: a randomised trial. J Physiother 2016;62:153–8. [DOI] [PubMed] [Google Scholar]
- [16].Kaya Mutlu E, Mustafaoglu R, Birinci T, et al. Does Kinesio taping of the kknee improve pain and functionality in patients with knee osteoarthritis?: a randomized controlled clinical trial. Am J Phys Med Rehabil 2017;96:25–33. [DOI] [PubMed] [Google Scholar]
- [17].Aiyegbusi A, Ogunfowodu O, Akinbo S. Kinesio taping is an effective stop-gap measure in alleviating the symptoms of osteoarthritis of the knee. J Clin Sci 2018;15:102.doi:10.4103/jcls.jcls_43_17. [Google Scholar]
- [18].Clement ND, Bardgett M, Weir D, et al. What is the minimum clinically important difference for the WOMAC Index after TKA? Clin Orthop 2018;476:2005–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lu Z, Li X, Chen R, et al. Kinesio taping improves pain and function in patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg 2018;59:27–35. [DOI] [PubMed] [Google Scholar]
- [20].Cho H, Kim E-H, Kim J, et al. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: a randomized controlled trial. Am J Phys Med Rehabil 2015;94:192–200. [DOI] [PubMed] [Google Scholar]
- [21].Aydoğdu O, Sari Z, Yurdalan SU, et al. Clinical outcomes of Kinesio taping applied in patients with knee osteoarthritis: a randomized controlled trial. J Back Musculoskelet Rehabil 2017;30:1045–51. [DOI] [PubMed] [Google Scholar]
- [22].Lespasio MJ, Piuzzi NS, Husni ME, et al. Knee Osteoarthritis: A Primer. Perm J 2017;21:16–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Oei EHG, Nikken JJ, Ginai AZ, et al. Acute knee trauma: value of a short dedicated extremity MR imaging examination for prediction of subsequent treatment. Radiology 2005;234:125–33. [DOI] [PubMed] [Google Scholar]


