Abstract
Data on the overall epidemiology and temporal trends of end-stage renal disease (ESRD) requiring hemodialysis in Korea are scarce. We aimed to estimate the prevalence and incidence of ESRD requiring hemodialysis in Korea between 2002 and 2017.
Using the National Health Insurance Service database, we analyzed data from the entire Korean population between 2002 and 2017. Hemodialysis patients were identified using rare incurable disease codes (V001) or prescription of medical fee codes of hemodialysis (O7020 and O7021). We only included patients who had been maintained on hemodialysis for more than 90 days from the date of dialysis initiation, to exclude patients who required short-term dialysis for acute kidney injury, conversion to peritoneal dialysis, or kidney transplantation.
During the 16-year follow-up, the number of hemodialysis patients in Korea has steadily increased from 11,215 in 2002 to 67,486 in 2017. The mean age of these patients has gradually increased from 55.57 ± 13.31 years in 2002 to 62.13 ± 13.23 years in 2017. In 2017, the crude prevalence rate of hemodialysis was 1303.4 per million population. Overall, the number of men tended to be somewhat higher than that of women, and the proportion of men increased slightly from 55.56% in 2002 to 58.45% in 2017. The proportion of diabetic patients increased rapidly from 23.84% to 47.84%, and the percentage of dyslipidemic patients rose from 18.9% to 86.7%. The number of incident hemodialysis patients increased significantly from 4406 in 2003 to 12,134 in 2014, and then decreased to 8090 in 2017. In the incident cases of hemodialysis, the observed increase in the proportion of male patients and in diabetes and dyslipidemia were similar to that of prevalent patients. The more recent era of hemodialysis initiation, the better 5-year survival rates were observed.
The prevalence and incidence of hemodialysis in Korea gradually increased between 2002 and 2017. The proportion of men, and patients with diabetes and dyslipidemia requiring hemodialysis also increased continuously. The survival rate of hemodialysis patients was gradually improving. These findings may serve as a reference for future epidemiological studies on hemodialysis in Korea.
Keywords: end-stage renal disease, epidemiology, hemodialysis, incidence, prevalence
1. Introduction
Chronic kidney disease (CKD) is one of the important public health problems worldwide.[1] According to the Global Burden of Disease, Injuries, and Risk Factor Study, 697.5 million individuals worldwide had CKD in 2017, and 1.2 million of them had died.[2] CKD is not only a public health issue, but also an important socio-economic problem. It is known to cause cardiovascular complications and premature death, as well as kidney failure.[1] As a single disease, CKD places a considerable financial burden. Treatment costs for CKD rose rapidly after the 1960s, with availability of renal replacement therapy making the long-term administration of treatment for patients with end-stage renal disease (ESRD) possible.[2] There are three modalities of renal replacement therapy for ESRD: hemodialysis (HD), peritoneal dialysis (PD), and kidney transplantation (KT). The selection of modality is affected by several factors including the socio-economic status, educational status, public health policy, and patient's wishes. Therefore, the selection of RRT modality varies widely from country to country.[3]
Although there are differences among countries, HD is the most predominant RRT modality in many countries, including South Korea.[3] Since home HD is not available in Korea, all patients undergo in-center HD. In the 2000s, the number of patients undergoing HD also increased with the rapid increase in dialysis facilities. Therefore, it is very important to understand the epidemiology at the national level for managing HD patients. To better understand the epidemiologic characteristics of HD patients in the entire Korean population, we analyzed nationally representative data from the Korean National Health Insurance System (NHIS)
2. Methods
2.1. Data source and study population
The Korean NHIS, which includes an eligibility database (age, sex, socioeconomic variables, type of eligibility, income level, etc), a medical treatment database (based on the accounts that were submitted by medical service providers for their medical expenses), a health examination database (results of general health examinations and questionnaires on lifestyle and behavior), and a medical care institution database (types of medical care institutions, location, equipment, and number of physicians), comprises a complete set of health information pertaining to 50 million Koreans. In Korea, the NHIS is the only insurer, is managed by the government, and ∼97% of the Korean population is subscribed to this database. The remaining 3% of the population is covered by the Medical Aid program. In addition, the total claim rate for medical expenses is 100%. Therefore, it can be said that there are few people missing in the NHIS cohort among the Korean population.
2.2. Identification of hemodialysis cases
All medical care expenses for dialysis or kidney transplantation were reimbursed using the Korean Health Insurance Review and Assessment Service database. These participants were also registered in registration program for rare intractable diseases. Therefore, we were able to identify every ESRD patient in the South Korean population and analyze the data for all ESRD patients who had started dialysis. To accurately screen all patients undergoing maintenance HD, we defined ESRD as follows.
-
1.
Patients who have been prescribed a fee code for doing HD (O7020) or fee code of materials used for HD (O7021), for more than 90 days continuously.
-
2.
And, patients who have been prescribed rare intractable diseases code for hemodialysis (V001) for more than 90 days.
By defining patients who meet both of the above criteria as HD patients, we were able to exclude patients with hemodialysis due to acute kidney injury and select only true ESRD patients with maintenance HD. In addition, by limiting the HD cases to patients undergoing HD for more than 90 days, patients who died in the early stage after the HD started or were converted to other RRT modalities could be clearly excluded.
2.3. Estimation of prevalence and incidence
For annual prevalence, the year-specific numerator included subjects with prevalent HD in the specific calendar year, and the denominator included the end-year population from the Korean National Statistical Office of the year. For annual incidence, the year-specific numerator included subjects with incident HD in the specific calendar year, and the denominator included the end-year population from the Korean National Statistical Office of the year. The crude rates that presented as per million population (PMP) were calculated by dividing the year-specific numerator by the end-year population and multiplying it by one million. Incident cases of HD were defined as those without HD in a particular year (e.g., 2005) and the preceding 2 years (e.g., 2003–2004) that met the algorithm in that year (e.g., 2005).
2.4. Definitions of variables
Enrollees in the Korean NHIS are recommended to undergo a standardized medical examination at least every 2 years. Participants who have received health examination in the year selected as the incident or prevalent case between 2002 and 2017 were included. Descriptions of the variables included in health examinations, such as questionnaires, laboratory data, and disease history, have been documented in our previous study.[4] The above variables were extracted from health examination data provided to health insurance participants by NHIS biennially.[5] Hospitals that performed these health examinations were certified by the NHIS and subjected to regular quality control evaluations. The definition for presence of diabetes mellitus, hypertension and dyslipidemia were described in previous study.[4]
2.5. Statistical analyses
Continuous variables were presented as means ± standard deviation [SD] and categorical variables were presented as n (%). The survival rate according to the era of HD incidence was calculated using Kaplan–Meier curves. Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC), and a P-value < .05 was considered to indicate statistical significance.
2.6. Ethical approval
The requirement for ethical approval of this study was waived by the Institutional Review Board (IRB) of the Chonnam National University Hospital (IRB No. CNUH-EXP-2018–196). The requirement for obtaining informed consent was also waived; hence, consent was not obtained because participants’ records and information were anonymized and de-identified prior to analysis.
3. Results
3.1. Prevalence of hemodialysis
The number of prevalent HD cases in Korea has steadily increased 6-fold, from 11,215 in 2002 to 67,486 in 2017 (Table 1). The crude prevalence rate of HD had also increased continuously from 232.5 PMP in 2014 to 1303.4 PMP in 2017 (Fig. 1). The mean age of prevalent HD cases has consistently increased from 55.57 ± 13.31 years in 2002 to 62.13 ± 13.23 years in 2017 (Table 2). In the number of prevalent HD cases by age group, the proportion of elderly patients aged over 70 years gradually increased. In every year of follow up, the number of men on HD was higher than that of women, and the proportion of men increased slightly from 55.56% in 2002 to 58.45% in 2017 (Table 1). Among prevalent HD cases, the proportion of patients who were eligible for medical aid increased steadily, and more than 22% were medical aid recipients in 2017 (Table 2). The proportion of diabetic patients increased rapidly from 23.84% to 47.84%, and the percentage of dyslipidemic patients rose from 18.9% to 86.7%; however, the percentage of hypertensive patients did not show a considerable increase (Table 2).
Table 1.
Hemodialysis prevalence by year, 2002 to 2017.
| Year | Total population | No. of total prevalent cases | % change from previous year | Total crude rate (per million population) | % change from previous year | Male cases | Male crude rate (per million population) | % change from previous year | Female cases | Female crude rate (per million population) | % change from previous year | % of medical aid | Male:female ratio |
| 2002 | 48,229,948 | 11,215 | N/A | 232.5 | N/A | 6231 | 257.5 | N/A | 4984 | 207.4 | N/A | 0.37 | 1.25 |
| 2003 | 48,386,823 | 15,145 | 35.0 | 313.0 | 34.6 | 8402 | 346.2 | 34.5 | 1940 | 279.6 | 34.8 | 0.03 | 1.25 |
| 2004 | 48,583,805 | 17,789 | 17.5 | 366.2 | 17.0 | 9895 | 406.1 | 17.3 | 1878 | 325.9 | 16.6 | 0.06 | 1.25 |
| 2005 | 48,782,274 | 20,544 | 15.5 | 421.1 | 15.0 | 11,546 | 472.1 | 16.2 | 1914 | 369.9 | 13.5 | 3.86 | 1.28 |
| 2006 | 48,991,779 | 24,256 | 18.1 | 495.1 | 17.6 | 13,670 | 556.7 | 17.9 | 2417 | 433.2 | 17.1 | 11.24 | 1.29 |
| 2007 | 49,268,928 | 28,954 | 19.4 | 587.7 | 18.7 | 16,244 | 657.9 | 18.2 | 2693 | 517.1 | 19.4 | 19.62 | 1.28 |
| 2008 | 49,540,367 | 33,416 | 15.4 | 674.5 | 14.8 | 18,816 | 758.0 | 15.2 | 3012 | 590.7 | 14.2 | 22.12 | 1.29 |
| 2009 | 49,773,145 | 37,207 | 11.3 | 747.5 | 10.8 | 21,030 | 843.6 | 11.3 | 3006 | 651.2 | 10.2 | 15.73 | 1.30 |
| 2010 | 50,515,666 | 40,434 | 8.7 | 800.4 | 7.1 | 23,006 | 909.0 | 7.8 | 2945 | 691.4 | 6.2 | 15.38 | 1.32 |
| 2011 | 50,734,284 | 44,175 | 9.3 | 870.7 | 8.8 | 25,230 | 993.0 | 9.3 | 3227 | 748.0 | 8.2 | 15.86 | 1.33 |
| 2012 | 50,948,272 | 47,452 | 7.4 | 931.4 | 7.0 | 27,169 | 1065.3 | 7.3 | 3260 | 797.2 | 6.6 | 15.5 | 1.34 |
| 2013 | 51,141,463 | 50,794 | 7.0 | 993.2 | 6.6 | 29,221 | 1142.0 | 7.2 | 3407 | 844.2 | 5.9 | 15.55 | 1.35 |
| 2014 | 51,327,916 | 57,673 | 13.5 | 1123.6 | 13.1 | 33,463 | 1303.6 | 14.2 | 4831 | 943.5 | 11.8 | 20.02 | 1.38 |
| 2015 | 51,529,338 | 62,445 | 8.3 | 1211.8 | 7.9 | 36,381 | 1412.4 | 8.3 | 4026 | 1011.4 | 7.2 | 20.6 | 1.40 |
| 2016 | 51,696,216 | 66,457 | 6.4 | 1285.5 | 6.1 | 38,814 | 1502.8 | 6.4 | 4123 | 1068.6 | 5.7 | 21.57 | 1.40 |
| 2017 | 51,778,544 | 67,486 | 1.5 | 1303.4 | 1.4 | 39,446 | 1525.6 | 1.5 | 3224 | 1081.7 | 1.2 | 22.02 | 1.41 |
Figure 1.
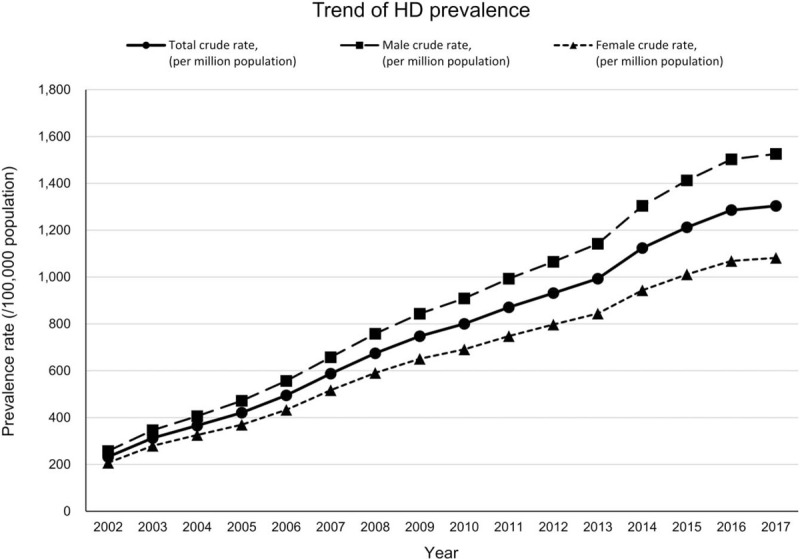
Trend of hemodialysis incidence from 2003 to 2017. HD = hemodialysis.
Table 2.
Hemodialysis prevalence by age, insurance type and comorbidities.
| Year | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| n | 11,215 | 15,145 | 17,789 | 20,544 | 24,256 | 28,954 | 33,416 | 37,207 | 40,434 | 44,175 | 47,452 | 50,794 | 57,673 | 62,445 | 66,457 | 67,486 |
| Age | 55.57 ± 13.31 | 55.53 ± 13.34 | 56.31 ± 13.19 | 56.95 ± 13.17 | 57.37 ± 13.21 | 57.37 ± 13.26 | 57.76 ± 13.29 | 58.31 ± 13.26 | 58.96 ± 13.31 | 59.49 ± 13.33 | 60.04 ± 13.3 | 60.47 ± 13.28 | 60.58 ± 13.27 | 61.03 ± 13.28 | 61.59 ± 13.28 | 62.13 ± 13.23 |
| Age group | ||||||||||||||||
| 0–9 | 5 (0.04) | 7 (0.05) | 5 (0.03) | 7 (0.03) | 3 (0.01) | 7 (0.02) | 3 (0.01) | 3 (0.01) | 9 (0.02) | 5 (0.01) | 5 (0.01) | 8 (0.02) | 8 (0.01) | 11 (0.02) | 11 (0.02) | 5 (0.01) |
| 10–19 | 50 (0.45) | 77 (0.51) | 54 (0.3) | 51 (0.25) | 70 (0.29) | 86 (0.3) | 101 (0.3) | 97 (0.26) | 87 (0.22) | 91 (0.21) | 93 (0.2) | 85 (0.17) | 89 (0.15) | 86 (0.14) | 80 (0.12) | 66 (0.1) |
| 20–29 | 433 (3.86) | 591 (3.9) | 628 (3.53) | 657 (3.2) | 685 (2.82) | 766 (2.65) | 818 (2.45) | 817 (2.2) | 807 (2) | 769 (1.74) | 706 (1.49) | 658 (1.3) | 667 (1.16) | 692 (1.11) | 708 (1.07) | 653 (0.97) |
| 30–39 | 930 (8.29) | 1231 (8.13) | 1384 (7.78) | 1547 (7.53) | 1789 (7.38) | 2176 (7.52) | 2448 (7.33) | 2577 (6.93) | 2645 (6.54) | 2764 (6.26) | 2789 (5.88) | 2841 (5.59) | 3049 (5.29) | 3052 (4.89) | 3055 (4.6) | 2862 (4.24) |
| 40–49 | 1962 (17.49) | 2652 (17.51) | 2979 (16.75) | 3282 (15.98) | 3876 (15.98) | 4695 (16.22) | 5319 (15.92) | 5771 (15.51) | 5914 (14.63) | 6199 (14.03) | 6316 (13.31) | 6586 (12.97) | 7876 (13.66) | 8348 (13.37) | 8446 (12.71) | 8286 (12.28) |
| 50–59 | 2897 (25.83) | 3943 (26.03) | 4523 (25.43) | 5187 (25.25) | 6159 (25.39) | 7447 (25.72) | 8538 (25.55) | 9354 (25.14) | 10,092 (24.96) | 11,068 (25.05) | 12,047 (25.39) | 12,710 (25.02) | 14,609 (25.33) | 15,639 (25.04) | 16,106 (24.24) | 15,967 (23.66) |
| 60–69 | 3457 (30.82) | 4644 (30.66) | 5602 (31.49) | 6483 (31.56) | 7323 (30.19) | 8426 (29.1) | 9513 (28.47) | 10598 (28.48) | 11,378 (28.14) | 12,223 (27.67) | 12,814 (27) | 13,410 (26.4) | 14,816 (25.69) | 16,080 (25.75) | 17,623 (26.52) | 18,144 (26.89) |
| 70–79 | 1300 (11.59) | 1751 (11.56) | 2273 (12.78) | 2881 (14.02) | 3751 (15.46) | 4596 (15.87) | 5684 (17.01) | 6740 (18.11) | 7879 (19.49) | 8947 (20.25) | 10237 (21.57) | 11,593 (22.82) | 13,002 (22.54) | 14,210 (22.76) | 15,217 (22.9) | 15,658 (23.2) |
| 80–89 | 174 (1.55) | 242 (1.6) | 332 (1.87) | 435 (2.12) | 579 (2.39) | 728 (2.51) | 951 (2.85) | 1206 (3.24) | 1557 (3.85) | 2014 (4.56) | 2342 (4.94) | 2779 (5.47) | 3403 (5.9) | 4141 (6.63) | 4970 (7.48) | 5563 (8.24) |
| 90- | 7 (0.06) | 7 (0.05) | 9 (0.05) | 14 (0.07) | 21 (0.09) | 27 (0.09) | 41 (0.12) | 44 (0.12) | 66 (0.16) | 95 (0.22) | 103 (0.22) | 124 (0.24) | 154 (0.27) | 186 (0.3) | 241 (0.36) | 282 (0.42) |
| Insurance type | ||||||||||||||||
| Medical aid | 42 (0.37) | 4 (0.03) | 11 (0.06) | 793 (3.86) | 2727 (11.24) | 5681 (19.62) | 7393 (22.12) | 5853 (15.73) | 6218 (15.38) | 7004 (15.86) | 7356 (15.5) | 7900 (15.55) | 11,546 (20.02) | 12,861 (20.6) | 14,338 (21.57) | 14,863 (22.02) |
| Health insurance | 11,173 (99.63) | 15,141 (99.97) | 17,778 (99.94) | 19,751 (96.14) | 21,529 (88.76) | 23,273 (80.38) | 26,023 (77.88) | 31,354 (84.27) | 34,216 (84.62) | 37,171 (84.14) | 40,096 (84.5) | 42,894 (84.45) | 46,127 (79.98) | 49,584 (79.4) | 52,119 (78.43) | 52,623 (77.98) |
| Number of individuals undergone health checkups in the year | ||||||||||||||||
| n | 365 | 471 | 659 | 804 | 1206 | 1294 | 2138 | 3000 | 3845 | 4402 | 5382 | 5787 | 7435 | 8493 | 9312 | |
| Diabetes | ||||||||||||||||
| No | 278 (76.16) | 347 (73.67) | 469 (71.17) | 558 (69.4) | 839 (69.57) | 835 (64.53) | 1378 (64.45) | 1915 (63.83) | 2345 (60.99) | 2645 (60.09) | 3203 (59.51) | 3369 (58.22) | 4329 (58.22) | 4816 (56.71) | 4857 (52.16) | |
| Yes | 87 (23.84) | 124 (26.33) | 190 (28.83) | 246 (30.6) | 367 (30.43) | 459 (35.47) | 760 (35.55) | 1085 (36.17) | 1500 (39.01) | 1757 (39.91) | 2179 (40.49) | 2418 (41.78) | 3106 (41.78) | 3677 (43.29) | 4454 (47.84) | |
| Hypertension | ||||||||||||||||
| No | 67 (18.36) | 57 (12.1) | 102 (15.48) | 130 (16.17) | 242 (20.07) | 213 (16.46) | 371 (17.35) | 574 (19.13) | 708 (18.41) | 835 (18.97) | 1066 (19.81) | 1125 (19.44) | 1604 (21.57) | 1821 (21.44) | 1238 (13.3) | |
| Yes | 298 (81.64) | 414 (87.9) | 557 (84.52) | 674 (83.83) | 964 (79.93) | 1081 (83.54) | 1767 (82.65) | 2426 (80.87) | 3137 (81.59) | 3567 (81.03) | 4316 (80.19) | 4662 (80.56) | 5831 (78.43) | 6672 (78.56) | 8073 (86.7) | |
| Dyslipidemia | ||||||||||||||||
| No | 296 (81.1) | 366 (77.71) | 502 (76.18) | 627 (77.99) | 915 (75.87) | 915 (70.71) | 1540 (72.03) | 2109 (70.3) | 2665 (69.31) | 2925 (66.45) | 3596 (66.82) | 3773 (65.2) | 4847 (65.19) | 5339 (62.86) | 4612 (49.53) | |
| Yes | 69 (18.9) | 105 (22.29) | 157 (23.82) | 177 (22.01) | 291 (24.13) | 379 (29.29) | 598 (27.97) | 891 (29.7) | 1180 (30.69) | 1477 (33.55) | 1786 (33.18) | 2014 (34.8) | 2588 (34.81) | 3154 (37.14) | 4699 (50.47) | |
| Smoking status | ||||||||||||||||
| Non-smoker | 252 (69.04) | 331 (70.28) | 472 (71.62) | 607 (75.5) | 944 (78.28) | 983 (75.97) | 1661 (77.69) | 1956 (65.2) | 2489 (64.73) | 2808 (63.79) | 3363 (62.49) | 3632 (62.76) | 4661 (62.69) | 5247 (61.78) | 5728 (61.51) | |
| Ex-smoker | 53 (14.52) | 61 (12.95) | 74 (11.23) | 94 (11.69) | 130 (10.78) | 164 (12.67) | 247 (11.55) | 661 (22.03) | 909 (23.64) | 1089 (24.74) | 1304 (24.23) | 1401 (24.21) | 1792 (24.1) | 2211 (26.03) | 2457 (26.39) | |
| Current smoker | 60 (16.44) | 79 (16.77) | 113 (17.15) | 103 (12.81) | 132 (10.95) | 147 (11.36) | 230 (10.76) | 383 (12.77) | 447 (11.63) | 505 (11.47) | 715 (13.29) | 754 (13.03) | 982 (13.21) | 1035 (12.19) | 1127 (12.1) | |
3.2. Incidence of hemodialysis
During the 16 years’ follow up period, maintenance HD was initiated in 123,502 individuals (Table 3). Figure 2 shows the trends of incidence rate of HD by year. The annual number of incident cases and incidence rates of HD gradually increased and peaked in 2014 (Table 3). The average age of patients starting maintenance HD has increased gradually. In the distribution of HD incident cases by age group, the proportion of cases under the age of 60 to 69 years gradually decreased, while the proportion of the elderly group aged over 70 years gradually increased (Table 4). The number of incident cases of HD was greater in men than in women for all years of follow up (Table 3). In addition, the proportion of incident cases of HD in men tended to increase over the years.
Table 3.
Hemodialysis incidence by year, 2003 to 2017.
| Year | Total population | No. of total incident cases | % change from previous year | Total crude rate (per million population) | % change from previous year | Male cases | Male crude rate (per million population) | % change from previous year | Female cases | Female crude rate (per million population) | % change from previous year | Male:female ratio |
| 2003 | 48,386,823 | 4406 | N/A | 91.1 | N/A | 2466 | 101.6 | N/A | 1940 | 80.4 | N/A | 1.27 |
| 2004 | 48,583,805 | 4435 | 0.7 | 91.3 | 0.3 | 2557 | 105.0 | 3.3 | 1878 | 77.5 | −3.6 | 1.36 |
| 2005 | 48,782,274 | 4669 | 5.3 | 95.7 | 4.8 | 2755 | 112.7 | 7.3 | 1914 | 78.7 | 1.5 | 1.44 |
| 2006 | 48,991,779 | 5782 | 23.8 | 118.0 | 23.3 | 3365 | 137.0 | 21.6 | 2417 | 98.9 | 25.7 | 1.39 |
| 2007 | 49,268,928 | 6350 | 9.8 | 128.9 | 9.2 | 3657 | 148.1 | 8.1 | 2693 | 109.6 | 10.8 | 1.36 |
| 2008 | 49,540,367 | 7076 | 11.4 | 142.8 | 10.8 | 4064 | 163.7 | 10.5 | 3012 | 121.9 | 11.2 | 1.35 |
| 2009 | 49,773,145 | 7172 | 1.4 | 144.1 | 0.9 | 4166 | 167.1 | 2.1 | 3006 | 121.0 | −0.7 | 1.39 |
| 2010 | 50,515,666 | 7239 | 0.9 | 143.3 | −0.5 | 4294 | 169.7 | 1.5 | 2945 | 116.8 | −3.4 | 1.46 |
| 2011 | 50,734,284 | 7852 | 8.5 | 154.8 | 8.0 | 4625 | 182.0 | 7.3 | 3227 | 127.4 | 9.0 | 1.43 |
| 2012 | 50,948,272 | 7935 | 1.1 | 155.7 | 0.6 | 4675 | 183.3 | 0.7 | 3260 | 128.1 | 0.6 | 1.43 |
| 2013 | 51,141,463 | 8523 | 7.4 | 166.7 | 7.0 | 5116 | 199.9 | 9.1 | 3407 | 133.3 | 4.1 | 1.50 |
| 2014 | 51,327,916 | 12,134 | 42.4 | 236.4 | 41.9 | 7303 | 284.5 | 42.3 | 4831 | 188.3 | 41.2 | 1.51 |
| 2015 | 51,529,338 | 10,171 | −16.2 | 197.4 | −16.5 | 6145 | 238.6 | −16.1 | 4026 | 156.2 | −17.0 | 1.53 |
| 2016 | 51,696,216 | 10,453 | 2.8 | 202.2 | 2.4 | 6330 | 245.1 | 2.7 | 4123 | 159.4 | 2.0 | 1.54 |
| 2017 | 51,778,544 | 8090 | −22.6 | 156.2 | −22.7 | 4866 | 188.2 | −23.2 | 3224 | 124.4 | −22.0 | 1.51 |
Figure 2.
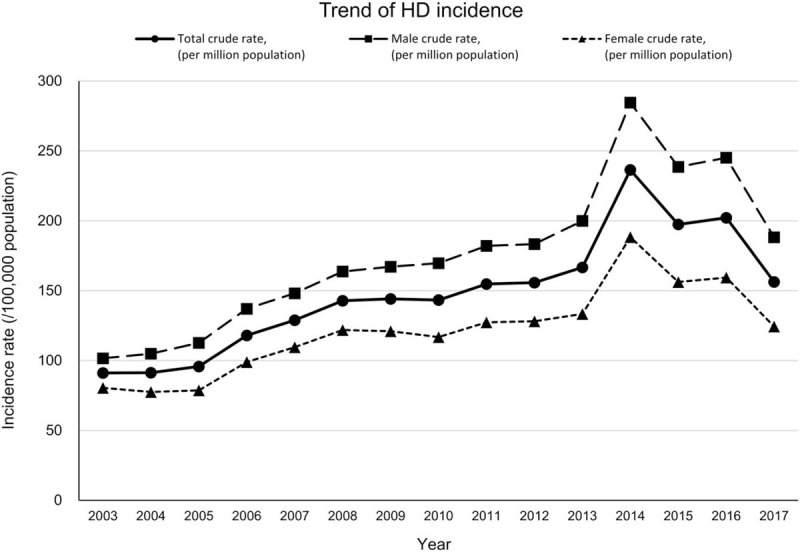
Trend of hemodialysis prevalence from 2002 to 2017. HD = hemodialysis.
Table 4.
Hemodialysis incidence by age, insurance type, and comorbidities.
| Year | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| n | 4406 | 4435 | 4669 | 5782 | 6350 | 7076 | 7172 | 7239 | 7852 | 7935 | 8523 | 12,134 | 10,171 | 10,453 | 8090 |
| Age | 55.29 ± 13.71 | 56.63 ± 13.38 | 57.22 ± 13.53 | 57.24 ± 13.74 | 57.24 ± 13.65 | 57.51 ± 13.81 | 58.89 ± 13.71 | 59.15 ± 14.03 | 59.97 ± 13.98 | 60.86 ± 13.8 | 60.89 ± 14.02 | 59.61 ± 13.84 | 61.7 ± 13.96 | 62.9 ± 14.04 | 63.45 ± 13.92 |
| Age group | |||||||||||||||
| 0–9 | 2 (0.05) | 2 (0.05) | 3 (0.06) | 1 (0.02) | 5 (0.08) | 0 (0) | 2 (0.03) | 6 (0.08) | 1 (0.01) | 3 (0.04) | 4 (0.05) | 2 (0.02) | 5 (0.05) | 4 (0.04) | 1 (0.01) |
| 10–19 | 33 (0.75) | 16 (0.36) | 22 (0.47) | 32 (0.55) | 31 (0.49) | 39 (0.55) | 29 (0.4) | 30 (0.41) | 36 (0.46) | 27 (0.34) | 25 (0.29) | 38 (0.31) | 25 (0.25) | 24 (0.23) | 14 (0.17) |
| 20–29 | 188 (4.27) | 161 (3.63) | 159 (3.41) | 186 (3.22) | 171 (2.69) | 187 (2.64) | 163 (2.27) | 174 (2.4) | 149 (1.9) | 132 (1.66) | 143 (1.68) | 168 (1.38) | 141 (1.39) | 157 (1.5) | 90 (1.11) |
| 30–39 | 355 (8.06) | 329 (7.42) | 331 (7.09) | 413 (7.14) | 472 (7.43) | 529 (7.48) | 468 (6.53) | 466 (6.44) | 476 (6.06) | 433 (5.46) | 471 (5.53) | 684 (5.64) | 494 (4.86) | 467 (4.47) | 341 (4.22) |
| 40–49 | 782 (17.75) | 730 (16.46) | 730 (15.64) | 979 (16.93) | 1078 (16.98) | 1223 (17.28) | 1090 (15.2) | 1059 (14.63) | 1110 (14.14) | 997 (12.56) | 1138 (13.35) | 2020 (16.65) | 1316 (12.94) | 1177 (11.26) | 896 (11.08) |
| 50–59 | 1144 (25.96) | 1059 (23.88) | 1133 (24.27) | 1451 (25.1) | 1602 (25.23) | 1705 (24.1) | 1688 (23.54) | 1719 (23.75) | 1831 (23.32) | 1868 (23.54) | 1928 (22.62) | 3157 (26.02) | 2345 (23.06) | 2199 (21.04) | 1695 (20.95) |
| 60–69 | 1296 (29.41) | 1441 (32.49) | 1464 (31.36) | 1599 (27.65) | 1753 (27.61) | 1896 (26.79) | 1988 (27.72) | 1894 (26.16) | 2025 (25.79) | 2042 (25.73) | 2069 (24.28) | 2670 (22) | 2453 (24.12) | 2592 (24.8) | 1966 (24.3) |
| 70–79 | 521 (11.82) | 609 (13.73) | 709 (15.19) | 946 (16.36) | 1072 (16.88) | 1277 (18.05) | 1446 (20.16) | 1531 (21.15) | 1736 (22.11) | 1917 (24.16) | 2140 (25.11) | 2566 (21.15) | 2503 (24.61) | 2730 (26.12) | 2151 (26.59) |
| 80–89 | 84 (1.91) | 84 (1.89) | 114 (2.44) | 168 (2.91) | 161 (2.54) | 210 (2.97) | 288 (4.02) | 346 (4.78) | 467 (5.95) | 495 (6.24) | 578 (6.78) | 806 (6.64) | 851 (8.37) | 1049 (10.04) | 880 (10.88) |
| 90- | 1 (0.02) | 4 (0.09) | 4 (0.09) | 7 (0.12) | 5 (0.08) | 10 (0.14) | 10 (0.14) | 14 (0.19) | 21 (0.27) | 21 (0.26) | 27 (0.32) | 23 (0.19) | 38 (0.37) | 54 (0.52) | 56 (0.69) |
| Insurance type | |||||||||||||||
| medical aid | 0 (0) | 2 (0.05) | 261 (5.59) | 1102 (19.06) | 1466 (23.09) | 1935 (27.35) | 1267 (17.67) | 940 (12.99) | 1144 (14.57) | 975 (12.29) | 1177 (13.81) | 4094 (33.74) | 1455 (14.31) | 1285 (12.29) | 1033 (12.77) |
| health insurance | 4406 (100) | 4433 (99.95) | 4408 (94.41) | 4680 (80.94) | 4884 (76.91) | 5141 (72.65) | 5905 (82.33) | 6299 (87.01) | 6708 (85.43) | 6960 (87.71) | 7346 (86.19) | 8040 (66.26) | 8716 (85.69) | 9168 (87.71) | 7057 (87.23) |
| Number of individuals undergone health checkups in the year | |||||||||||||||
| n | 170 | 203 | 202 | 304 | 313 | 469 | 650 | 762 | 849 | 957 | 1045 | 1554 | 1524 | 1563 | |
| Diabetes | |||||||||||||||
| No | 110 (64.71) | 131 (64.53) | 116 (57.43) | 161 (52.96) | 146 (46.65) | 240 (51.17) | 338 (52) | 363 (47.64) | 399 (47) | 414 (43.26) | 451 (43.16) | 795 (51.16) | 664 (43.57) | 589 (37.68) | |
| Yes | 60 (35.29) | 72 (35.47) | 86 (42.57) | 143 (47.04) | 167 (53.35) | 229 (48.83) | 312 (48) | 399 (52.36) | 450 (53) | 543 (56.74) | 594 (56.84) | 759 (48.84) | 860 (56.43) | 974 (62.32) | |
| Hypertension | |||||||||||||||
| No | 12 (7.06) | 15 (7.39) | 7 (3.47) | 10 (3.29) | 11 (3.51) | 17 (3.62) | 32 (4.92) | 30 (3.94) | 40 (4.71) | 58 (6.06) | 46 (4.4) | 219 (14.09) | 104 (6.82) | 29 (1.86) | |
| Yes | 158 (92.94) | 188 (92.61) | 195 (96.53) | 294 (96.71) | 302 (96.49) | 452 (96.38) | 618 (95.08) | 732 (96.06) | 809 (95.29) | 899 (93.94) | 999 (95.6) | 1335 (85.91) | 1420 (93.18) | 1534 (98.14) | |
| Dyslipidemia | |||||||||||||||
| No | 119 (70) | 128 (63.05) | 135 (66.83) | 194 (63.82) | 170 (54.31) | 270 (57.57) | 360 (55.38) | 395 (51.84) | 421 (49.59) | 456 (47.65) | 468 (44.78) | 851 (54.76) | 666 (43.7) | 473 (30.26) | |
| Yes | 51 (30) | 75 (36.95) | 67 (33.17) | 110 (36.18) | 143 (45.69) | 199 (42.43) | 290 (44.62) | 367 (48.16) | 428 (50.41) | 501 (52.35) | 577 (55.22) | 703 (45.24) | 858 (56.3) | 1090 (69.74) | |
| Smoking status | |||||||||||||||
| Non-smoker | 110 (64.71) | 144 (70.94) | 146 (72.28) | 233 (76.64) | 229 (73.16) | 334 (71.22) | 421 (64.77) | 468 (61.42) | 502 (59.13) | 534 (55.8) | 628 (60.1) | 917 (59.01) | 855 (56.1) | 861 (55.09) | |
| Ex-smoker | 29 (17.06) | 26 (12.81) | 29 (14.36) | 25 (8.22) | 46 (14.7) | 74 (15.78) | 139 (21.38) | 183 (24.02) | 231 (27.21) | 276 (28.84) | 265 (25.36) | 384 (24.71) | 468 (30.71) | 495 (31.67) | |
| Current smoker | 31 (18.24) | 33 (16.26) | 27 (13.37) | 46 (15.13) | 38 (12.14) | 61 (13.01) | 90 (13.85) | 111 (14.57) | 116 (13.66) | 147 (15.36) | 152 (14.55) | 253 (16.28) | 201 (13.19) | 207 (13.24) | |
When observing the co-morbidities of incident HD cases, the prevalence of hypertension was remarkably high. It was found that more than 90% of patients had hypertension at initiation of HD; this trend was observed in most years (Table 4). The rapid increase in the proportion of patients with diabetes and dyslipidemia at the start of HD was also a very characteristic phenomenon. An increase in the proportion of ex-smokers was also observed among incident HD cases.
3.3. Trends in survival rate of incident hemodialysis cases
To examine the changes in the survival rate of incident HD cases, we analyzed age and sex adjusted 5-year survival stratified by the era of HD initiation. As shown in Figure 3, the more recent era of HD initiation, the better survival rates were observed. The 5-year survival rate of cases who started HD in 2013 to 2017 was about 64%, an improvement of about 7% compared to those who started HD in 2003 to 2007.
Figure 3.
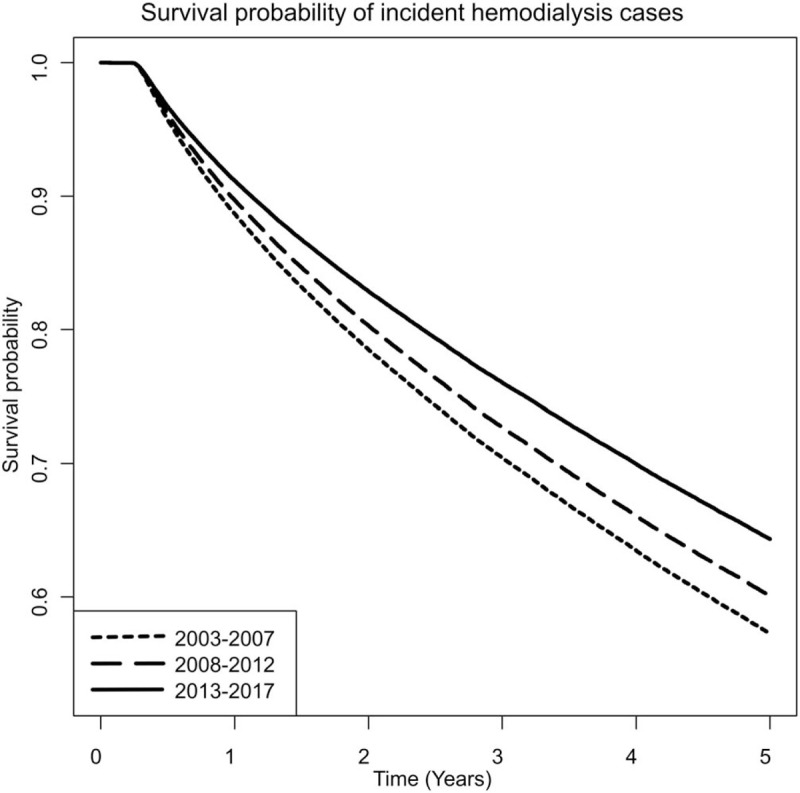
Trends in survival rate of incident hemodialysis cases.
4. Discussion
In this study, we determined the nationwide prevalence and incidence of HD in South Korea using the NHIS data that covered almost all of the Korean population. Our main finding was that the prevalence and incidence of hemodialysis in South Korea has been continuously increasing in the past 16 years.
According to the 2018 USRDS report, the prevalence rate of ESRD in South Korea was 1816 PMP, that ranked sixth in the world in 2016.[3] The incidence rate of ESRD in South Korea was 311 PMP, that also ranked sixth in the world in 2016. The prevalence and incidence of ESRD has been steadily increasing in South Korea; this has been attributed to an increase in lifestyle diseases such as diabetes, hypertension, and dyslipidemia due to dietary changes and an increase in life expectancy. The findings of the present study agree with this notion. The prevalence of diabetes and dyslipidemia showed a tendency to increase rapidly during the years in incident or prevalent HD cases (Tables 2 and 4). The increase in the prevalence of dyslipidemia is considered to be affected by the KDIGO guidelines for management of dyslipidemia released in November 2013.[6] After the new KDIGO guideline for dyslipidemia was released, the prevalence of dyslipidemia has increased sharply from 2015, and it is observed to exceed 50% in 2016.
With an increase in ESRD, the prevalence and incidence of HD, which accounts for the largest proportion of RRT cases in South Korea, has also increased.[7] Compared to PD or KT, HD demonstrated the most prominent increase. This has been attributed to certain factors; first, the profit generated with HD is higher than that of PD. As a result, HD facilities have increased in South Korea; being easily accessible to patients, it appears to be more prevalent than PD. Conversely, PD is mostly limited to tertiary hospitals. Secondly, the increase in ESRD in South Korea is strongly associated with the aging of the population. In our study, we also observed a gradual increase in the average age of HD patients (Tables 1 and 3). Hemodialysis is preferred over peritoneal dialysis in older patients, as they have difficulties in performing the fine movements required to perform PD. In this context, an increase in geriatric nursing hospitals in South Korea has also contributed to an increase in HD. As HD was used as a means of life support in the elderly, it has led to an increase in geriatric nursing hospitals equipped with HD facilities.
According to 2019 USRDS data, 62.9% of prevalent RRT patients were receiving HD (PD 7.1% and KT 30.0%), and 86.9% of incident RRT patients opted for HD (PD 10.1%, KT 2.9%) in 2017.[8] Estimates from 2018 USRDS data showed the crude incidence rate of HD in 2016 to be 334 PMP, and the crude prevalence rate to be ∼1412 PMP.[3] This shows that the prevalence and incidence rates were higher than those of South Korea in the same period. HD is more preferred in the neighboring country, Japan, than in South Korea.[9] In 2017, 97.3% of prevalent dialysis patients (except KT patients) in Japan were on maintenance HD, and 94.8% of incident dialysis patients selected HD. The reasons include concerns regarding encapsulating peritonitis, longer dialysis vintage, and easy access to hemodialysis facilities.[9] Estimates of the 2017 Japanese Society for Dialysis Therapy Renal Data Registry (JRDR) showed the crude incidence rate of HD to be 307 PMP in 2017, and the crude prevalence rate to be ∼2569 PMP.[9] The Korean ESRD registry is Korea's representative ESRD patient registration program, organized by the Korean Society of Nephrology (KSN).[10] According to the Korean ESRD registry, the crude incidence rate of HD was 285.2 PMP in 2017, and the crude prevalence rate was approximately 1497.6 PMP.[10] This shows some differences from our research. In general, the number of prevalent or incident cases and the prevalence or incidence rates calculated in our study are smaller than those of the Korea ESRD registry. In addition, the number of incident cases or incidence rate continued to increase in the KSN registry, while our study showed a decrease after peaking in 2014. The reason for this discrepancy is thought to be related to differences between the methods of patient screening in the two studies. The Korean ESRD registry collects data through voluntary input from dialysis facilities via an online registry program on the KSN web site. However, national health insurance is mandatory in Korea; it is therefore possible to obtain data regarding all the medical services received by the entire Korean population. Since dialysis patients can receive medical expenses reduction under the rare intractable diseases registration program, data on all dialysis patients exist in the NHIS database, without any missing data.
Nevertheless, the HD incidence and prevalence confirmed by our study were observed to be lower than those of Korean ESRD registry data. This may be attributed to the criteria used for selecting HD patients in our study. We only selected patients who had been on HD for more than 90 days after initiation. This was performed for two reasons; the first was to exclude patients who discontinued HD after a short period of time, such as those with acute kidney injury, or those who initially undergo HD and switch to another RRT modality. The second reason was that patients who died within 90 days of starting HD were more likely to die from underlying disease than from complications of dialysis. In future studies on the HD population using this database, these two reasons will be extremely important for the accurate selection of patients on maintenance HD. Owing to these stringent criteria, the incidence and prevalence of HD in our study was lower than those of the Korean ESRD registry. The incidence of HD appears to be continuously increasing in the Korean ESRD registry, whereas in our study, the HD incidence has been found to be decreasing since 2014. This phenomenon is presumed to be due to an increase in the number of incident HD patients, who begin hemodialysis and die prematurely; this is a possibility in patients who undergo hemodialysis as life support treatment, and die within 90 days. The incident cases of KT were steadily rising, but not enough to affect the decline in HD cases (see Supplemental Digital Content 1, Table, which demonstrates the incidence of HD and KT).
This study also showed that the proportion of patients who were eligible for medical aid increased continuously. In 2017, more than 22% of prevalent HD cases were medical aid recipients. Patients undergoing HD in South Korea receive a significant reduction in treatment costs due to the benefits of rare and intractable diseases. Nevertheless, HD places socioeconomic constraints, leading to further financial difficulties. As the poor receive medical aid, they are entitled to a reduction in medical expenses; however, policy support will be needed to prevent HD patients from becoming a socially disadvantaged class.
Despite providing certain important findings regarding HD in South Korea, this study had a few limitations. First, due to the limitations in the information registered in the NHIS database that we used for the study, the detailed history or laboratory data of patients was not available for analysis. Therefore, it was difficult to compare ESRD by cause of CKD, and the accurate estimation of other comorbidities was not possible. In addition, modalities such as HD or hemodiafiltration could not be distinguished. Second, since most of the existing studies provide data on the prevalence and incidence of ESRD, it was difficult to compare the prevalence and incidence of HD only with those of other studies. Third, it was not possible to distinguish whether dialysis catheter or arteriovenous fistula was actually used at the start of dialysis.
In summary, this study showed that the incidence and prevalence of HD has increased over recent years. The mean age of HD patients and the proportion of men have gradually increased; diabetes and dyslipidemia have also increased continuously among patients receiving HD. The survival rate of hemodialysis patients was gradually improving. These findings may serve as a reference for epidemiological studies on HD in South Korea.
Author contributions
Conceptualization: Hong Sang Choi, Tae Ryom Oh, Sang Heon Suh, Minah Kim, Chang Seong Kim, Eun Hui Bae, Seong Kwon Ma, Soo Wan Kim.
Data curation: Kyung-Do Han.
Formal analysis: Kyung-Do Han.
Funding acquisition: Hong Sang Choi, Soo Wan Kim.
Supervision: Soo Wan Kim.
Writing – original draft: Hong Sang Choi.
Supplementary Material
Footnotes
Abbreviations: CKD = chronic kidney disease, ESRD = end-stage renal disease, HD = hemodialysis, IRB = Institutional Review Board, JRDR = Japanese Society for Dialysis Therapy Renal Data Registry, KSN = Korean Society of Nephrology, KT = kidney transplantation, NHIS = National Health Insurance System, PD = peritoneal dialysis, PMP = per million population, USRDS = United States Renal Data System.
How to cite this article: Choi HS, Han KD, Oh TR, Suh SH, Kim M, Kim CS, Bae EH, Ma SK, Kim SW. Trends in the incidence and prevalence of end-stage renal disease with hemodialysis in entire Korean population: a nationwide population-based study. Medicine. 2021;100:13(e25293).
This study was supported by the Bio and Medical Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (2017M3A9E8023001 and 2017M3A9E8023016), grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI18C0331, HR20C0021), and grant (BCRI20041, BCRI20076) of Chonnam National University Hospital Biomedical Research Institute.
The authors have no conflict of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental digital content is available for this article.
References
- [1].Levey AS, Atkins R, Coresh J, et al. Chronic kidney disease as a global public health problem: approaches and initiatives—a position statement from kidney disease improving global outcomes. Kidney Int 2007;72:247–59. [DOI] [PubMed] [Google Scholar]
- [2].GBD, Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2020;395:709–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Saran R, Robinson B, Abbott KC, et al. Us renal data system 2018 annual data report: Epidemiology of kidney disease in the united states. Am J Kidney Dis 2019;73:A7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Choi HS, Han KD, Oh TR, et al. Smoking and risk of incident end-stage kidney disease in general population: a nationwide population-based cohort study from Korea. Sci Rep 2019;9:19511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Seong SC, Kim YY, Park SK, et al. Cohort profile: the national health insurance service-national health screening cohort (nhis-heals) in Korea. BMJ Open 2017;7:e016640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group. KDIGO clinical practice guideline for lipid management in chronic kidney disease. Kidney Int Suppl 2013;3:259–305. [Google Scholar]
- [7].Jin DC, Yun SR, Lee SW, et al. Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res Clin Pract 2018;37:20–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2019 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2020;75:A6–7. [DOI] [PubMed] [Google Scholar]
- [9].Nitta K, Masakane I, Hanafusa N, et al. Annual dialysis data report 2017, JSDT Renal Data Registry. Renal Replacement Ther 2019;5:53. [Google Scholar]
- [10].ESRD Registry Committee Korean Society of Nephrology. Current renal replacement therapy in Korea, 2019; Available at: http://www.ksn.or.kr/rang_board/list.html?code5sinchart_eng. Accessed December 28, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


