Abstract
To examine the knowledge level, behaviors, and psychological status of the Chinese population during the COVID-19 pandemic, and to explore the differences between urban and rural areas.
We carried out a cross-sectional survey of the knowledge, behaviors related to COVID-19, and mental health in a probability sample of 3001 community residents in 30 provinces or districts across China from February 16–23, 2020. Convenience sampling and a snowball sampling were adopted. We used General Anxiety Disorder (GAD), the 9-item Patient Health Questionnaire (PHQ-9), and knowledge and behaviors questionnaire of community residents regarding COVID-19 designed by us to investigate the psychological status, disease-related knowledge, and the behavior of Chinese urban and rural residents during the pandemic.
The average score of anxiety and depression among urban residents was 9.15 and 11.25, respectively, while the figures in rural areas were 8.69 and 10.57, respectively. There was a statistically significant difference in the levels of anxiety (P < .01) and depression (P < .01). Urban participants reported significantly higher levels of knowledge regarding COVID-19 in all aspects (transmission, prevention measures, symptoms of infection, treatment, and prognosis) (P < .01), compared to their rural counterparts. While a majority of respondents in urban areas obtained knowledge through WeChat, other apps, and the Internet (P < .01), residents in rural areas accessed information through interactions with the community (P < .01). Urban residents fared well in exchanging knowledge about COVID-19 and advising others to take preventive measures (P < .01), but fared poorly in advising people to visit a hospital if they displayed symptoms of the disease, compared to rural residents (P < .01). Regression analysis with behavior showed that being female (OR = 2.106, 95%CI = 1.259–3.522), aged 18 ≤ age < 65 (OR = 4.059, 95%CI = 2.166–7.607), being satisfied with the precautions taken by the community (OR = 2.594, 95%CI = 1.485–4.530), disinfecting public facilities in the community (OR = 2.342, 95%CI = 1.206–4.547), having knowledge of transmission modes (OR = 3.987, 95%CI: 2.039, 7.798), symptoms (OR = 2.045, 95%CI = 1.054–4.003), and outcomes (OR = 2.740, 95%CI = 1.513–4.962) of COVID-19, and not having anxiety symptoms (OR = 2.578, 95%CI = 1.127–5.901) were positively associated with affirmative behavior in urban areas. Being married (OR = 4.960, 95%CI = 2.608–9.434), being satisfied with the precautions taken by the community (OR = 2.484, 95%CI = 1.315–4.691), screening to ensure face mask wearing before entering the community (OR = 8.809, 95%CI = 2.649–19.294), and having knowledge about precautions (OR = 4.886, 95%CI = 2.604–9.167) and outcomes (OR = 2.657, 95%CI = 1.309–5.391) were positively associated with acceptable conduct in rural areas.
The status of anxiety and depression among urban residents was more severe compared to those living in rural areas. There was a difference in being positively associated with constructive behaviors between rural and urban areas.
Keywords: anxiety, community residents, COVID-19, depression, knowledge and behaviors
1. Introduction
COVID-19, an acute respiratory illness caused by the novel coronavirus SARS-CoV-2, has been spreading extensively across the globe. As of February 3, 2021, the death toll from the ongoing COVID-19 pandemic reached 2,250,000 globally, as confirmed positives cases surpassed 1,044,900,000, with 27,027,347 cases in the United States, 2,570,608 in Italy, and 2,881,793 in Spain.[1] The sharp increase in infections has resulted in a global threat, prompting the World Health Organization (WHO) to declare COVID-19 as a pandemic on March 11.[2]
The pandemic has rapidly evolved and impacted the psychology of the public and social economy in an unprecedented manner, leading to social distancing and travel restrictions, closure of schools and many businesses, and fear of shortages of basic commodities. Previously published research had highlighted the importance of screening mental health and the behavior of people during the SARS and H1N1 epidemics, which would evaluate the effectiveness of disease prevention.[3–7] Newly published studies showed that the knowledge and behavior of the public correlated positively with preventive measures related to COVID-19[8] and better knowledge and constructive behaviors would contribute to the control of the pandemic.[7] Hence, evaluation of knowledge and behavior would help in slowing down the spread of the virus.
While it is clear that the overall knowledge level and behavior among the Chinese have not been ideal,[8] little is known about the disparities between residents in urban and rural areas. In China, there were huge differences between towns and villages in terms of social conditions, economic level, cultural education, and health-care.[9] A forecast study in China indicated that health resources in an urban setting were twice as higher as that of rural areas per 1000 people in 2017, and that the gap is expected to grow further.[10] Considering the difference in the status of health literacy between urban and rural residents,[11] there is a need to clarify the condition and difference of knowledge, behavior, and mental health of community residents in urban and rural settings so as to promote equity in health literacy. Given the importance of knowledge and behavior in controlling COVID-19, it is essential to examine these factors among the Chinese and explore the differences between urban and rural areas, in order to provide a scientific basis for evidence-based public health policies and optimal resource allocation.
While research had emerged regarding the status of knowledge and behavior among the public in China, the difference between people in urban and rural settings is still unknown. We could not prepare individual measures to prevent COVID-19. Continued research focusing on the comparison of the knowledge level and behavior of residents in urban and rural areas is needed in China, as the COVID-19 pandemic continues to spread. Therefore, using a web-based cross-sectional study, we aimed to survey the knowledge level, behavior, and psychological status of the Chinese population, and explore the differences between urban and rural areas. We hope our findings will provide data support for building a set of easy-to-be-accepted, sustainable, relatively stable, and effective new intervention model for the Chinese population during the pandemic, and discuss how to promote cognition so as to amend public behavior, and develop targeted measures for the prevention of COVID-19.
2. Materials and methods
2.1. Study design and participants
We conducted a cross-sectional survey to examine the knowledge level, behaviors related to COVID-19, and mental health in a probability sample of 3001 community residents in 30 provinces or districts across China from on February16 to 23, 2020. Convenience sampling and a snowball sampling were adopted. The inclusion criteria were:
-
1.
people who have lived in mainland China since January 1, 2020,
-
2.
residents who agreed to participate in the study and signed informed consent,
-
3.
those who could fully understand all the items in the scale,
-
4.
individuals who could use mobile phones and operate the questionnaire filling tool, and
-
5.
people who could complete all the items in the questionnaire.
The exclusion criterion was now time to respond to all questions was >30 or <3 min.
2.2. Instrument
The General Anxiety Disorder (GAD) is a brief self-report scale and an efficient tool for measuring the frequency and severity of generalized anxiety disorder symptoms screening with seven items rated on a 4-point Likert-scale, ranging from 0 (not at all) to 3 (nearly every day).[12,13] The total score ranged from 0 to 21 and can be categorized as minimal (0–4), mild (5–9), moderate (10–14), and severe (15–21). In the present study, the Cronbach's ɑ was 0.92, test–retest reliability was 0.83.[10]
The 9-item Patient Health Questionnaire (PHQ9) was originally designed to measure symptoms of depression and was widely used to screen the occurrence and severity of these symptoms in primary care.[14–16] PHQ-9 offers a sum score for measuring depression severity, with a maximum possible score of 27.[14] Each item is scored from 0 to 3. Score of 5 to 9 indicates mild depression, 10 to 14 moderate depression, 15 to 19 moderately severe depression, and ≥ 20 severe depression.
To assess the knowledge and behaviors of community residents regarding COVID-19, we designed a “knowledge and behaviors regarding COVID-19 questionnaire” under the guidance of two specialist nursing professors. This questionnaire consists of 12 items and participants should respond using “Yes” or “No.” Meanwhile, items 1 to 5 are designed to assess the level of knowledge, and items 6 to 12 concern behaviors related to COVID-19.
2.3. Procedure and data collection
Before commencing the survey, we developed a paper-based questionnaire, and subsequently adopted a networking questionnaire tool (https://www.wjx.cn) to transfer it to a web page edition. The questionnaire was typed and verified to in line with the paper version. Then, three medical staffs and seven community residents were asked to answer this questionnaire to obtain whether there were incomprehensible items or difficulties in completing it. Through the Chinese, the questionnaires were distributed to communities in different provinces and invited eligible residents to participate. An electronic informed consent was obtained from the community members involved before collecting the data. The questionnaire was collected from on February 16 to 23, 2020.
2.4. Statistical analysis
Data analysis was done with SPSS version 21.0, assigning a significance level of 5% (P < .05). Descriptive statistics for social demographic variables, status of community prevention and control, anxiety and depression, knowledge level, and approach toward COVID-19 were presented as count, as well as public behavior which was stratified by urban and rural, Chi-square test and t test were used to compare the differences between groups. Binary logistic regression analysis models were performed to explore potential influence factors for communal behavior. Odds ratio, and 95% confidence intervals was obtained from logistic regression models.
2.5. Ethical considerations
The study was approved by the West China Hospital of Sichuan University Biomedical Research Ethics Committee (No. 2020[273]). All participants voluntarily signed the informed consent after being informed of the purpose of the study. The procedures of this study complied with the provisions of the Declaration of Helsinki, with regard to research on human participants.
3. Results
3.1. Demographic characteristics
The survey was conducted from on February 16 to 23, 2020, and data from all the respondents (1783 in urban and 1218 in rural areas) were analyzed.
Demographic characteristics of the respondents are presented in Table 1. Of these, 74% of urban and 69.7% of rural residents were female, 9.4% of urban and 21.7% of rural residents were less than 18 years of age, 51.2% of urban and 14.5% of rural residents completed undergraduate education, 38.0% of urban and 38.0% of rural residents waited for work-at-home opportunities, 69.3% of urban and 62.0% of rural residents were married, 9.2% of urban and 8.0% of rural residents reported having chronic diseases, 20.8% of urban and 10.4% of rural residents reported confirmed cases in their community, 35.4% of urban and 4.7% of rural residents were health-care workers, 1.2% of urban and 1.1% of rural residents reported the presence of respiratory symptoms in the past week, and 30.2% of urban and 32.8% of rural residents reported living alone.
Table 1.
Demographic characteristic (n = 3001).
| Group | Urban n (%) | Rural n (%) | x2/t | P |
| Gender | 6.59 | .006 | ||
| Male | 464 (26.0) | 369 (30.3) | ||
| Female | 1319 (74.0) | 849 (69.7) | ||
| Age | 89.25 | <.001 | ||
| < 18 | 167 (9.4) | 264 (21.7) | ||
| 18-64 | 1604 (90.0) | 948 (77.8) | ||
| ≥65 | 12 (0.6) | 6 (0.5) | ||
| Educational level | 597.85 | <.001 | ||
| Elementary school or less | 38 (2.1) | 95 (7.8) | ||
| Middle school and High school | 369 (20.7) | 694 (57.0) | ||
| Professional education | 463 (26.0) | 252 (20.7) | ||
| Undergraduate or more | 913 (51.2) | 177 (14.5) | ||
| Working status | 289.65 | <.001 | ||
| Return to work | 796 (44.6) | 784 (43.1) | ||
| Wait for work at home | 691 (38.8) | 691 (38.0) | ||
| home quarantine | 123 (6.9) | 147 (8.1) | ||
| Others | 173 (9.7) | 196 (10.8) | ||
| Marital status | 17.326 | <.001 | ||
| Unmarried | 482 (27.0) | 411 (33.7) | ||
| Married | 1235 (69.3) | 755 (62.0) | ||
| Divorced/widowed | 66 (3.7) | 52 (4.3) | ||
| Confirmed cases in the community | 56.341 | <.001 | ||
| Yes | 371 (20.8) | 127 (10.4) | ||
| No | 1412 (79.2) | 1091 (89.6) |
Comparing the data gathered from our questionnaires, is impossible to acknowledge some statistically significant differences between urban and rural areas. Analyzing the significant comparisons concerning community control of COVID-19 in the two groups (Table 1), it emerges that: more urban residents compared to those in rural areas wore masks (99.1% and 98.2%, P < .05), and compared to the urban community, there was more educational propaganda in rural areas (97.5% and 94.0%, P < .001).
3.2. Anxiety and depression
Figures 1 and 2 show the anxiety and depression status of respondents during the COVID-19 pandemic. The average score for anxiety and depression among urban residents was 9.15 and 11.25, respectively, while the average score among rural residents was 8.69 and 10.57, respectively. There were statistically significant differences in the status of anxiety (P < .01) and depression (P < .01).
Figure 1.
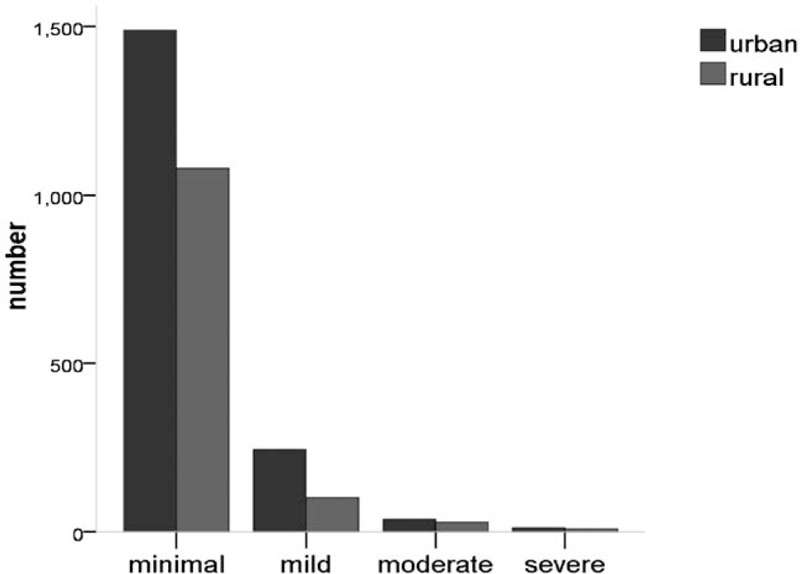
The anxiety status of two groups P < .001.
Figure 2.
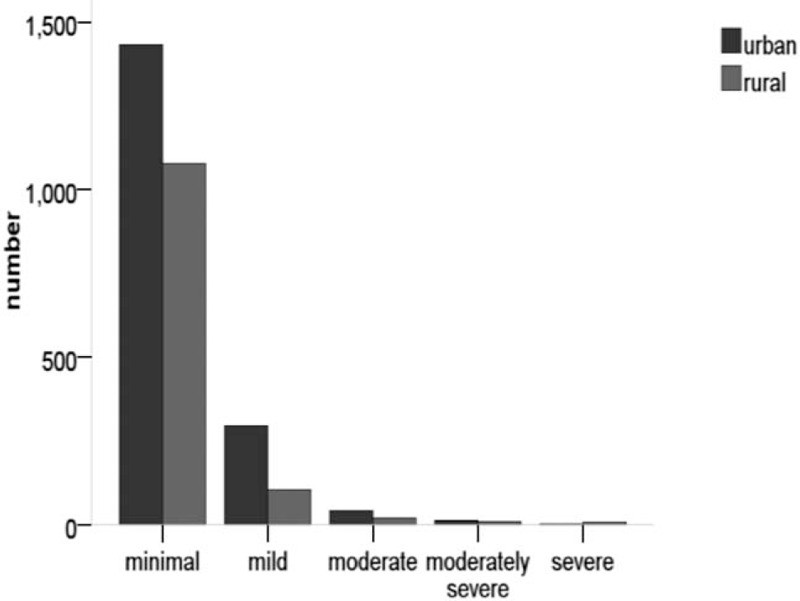
The depression status of two groups P < .001.
3.3. Knowledge and behavioral assessment about COVID-19
Table 2 shows the respondents’ knowledge level and approach toward COVID-19. Urban participants reported significantly higher levels of knowledge about the disease in all aspects (transmission, prevention measures, symptoms of infection, treatments, and prognosis) (P < .01). Most respondents in urban areas acquired knowledge through WeChat, other apps, and the Internet (P < .01), while residents in rural areas gained information through community interactions (P < .01).
Table 2.
Disease-knowledge and approach of knowledge about COVID-19 (n = 3001).
| Urban n (%) | Rural n (%) | |||||
| Group | Yes | No | Yes | No | x2 | P |
| Disease-knowledge | ||||||
| Routes of infection | 1652 (92.7) | 131 (7.3) | 1015 (83.3) | 203 (16.7) | 63.545 | <.001 |
| Prevention measures | 1679 (94.1) | 104 (5.9) | 1082 (88.8) | 136 (11.2) | 27.972 | <.001 |
| Symptoms of infection | 1597 (89.6) | 186 (10.4) | 2697 (87.9) | 371 (12.1) | 20.870 | <.001 |
| Treatments | 1053 (59.1) | 730 (49.1) | 623 (51.1) | 595 (48.9) | 18.355 | .006 |
| Prognosis | 1036 (58.1) | 747 (41.9) | 645 (53.0) | 573 (47.0) | 7.786 | .006 |
| Approach of knowledge | ||||||
| 1620 (90.9) | 163 (9.1) | 1045 (85.8) | 173 (14.2) | 18.65 | <.001 | |
| Other APP | 1393 (78.1) | 390 (21.9) | 829 (68.1) | 389 (31.9) | 38.14 | <.001 |
| Community | 1359 (76.2) | 424 (23.8) | 988 (81.1) | 230 (18.9) | 10.18 | .001 |
| TV news | 1641 (92.0) | 142 (8.0) | 1124 (92.3) | 94 (7.7) | 0.061 | .836 |
| Web page | 1390 (78.0) | 393 (22.0) | 881 (72.3) | 337 (27.7) | 12.447 | <.001 |
Table 3 shows the behaviors of respondents. Urban residents showed positive behavior in exchanging knowledge about COVID-19 with others and counseling them to take preventive measures (P < .01), but failed to advise people to visit a hospital if they had symptoms of COVID-19, compared to rural residents (P < .01).
Table 3.
Behaviour of people during the epidemic (n = 3001).
| Urban | Rural | |||||
| Group | Yes | No | Yes | No | x2 | P |
| Popularize knowledge about COVID-19 | 1482 (83.1) | 301 (16.9) | 978 (80.3) | 240 (19.7) | 3.902 | .027 |
| Take preventive measures | 1712 (96.0) | 71 (4.0) | 1154 (94.7) | 64 (5.3) | 2.727 | .060 |
| Advice others taking preventive measures | 1633 (91.6) | 150 (8.4) | 1092 (89.7) | 126 (10.3) | 3.235 | .042 |
| Isolate oneself when necessary | 1749 (98.1) | 34 (1.9) | 1190 (97.7) | 28 (2.3) | 0.549 | .269 |
| Advice others isolating themselves | 1749 (98.1) | 34 (1.9) | 1190 (97.7) | 28 (2.3) | 0.549 | .269 |
| See a doctor after the appearance of symptoms related COVID-19 | 1733 (97.2) | 50 (2.8) | 1190 (97.7) | 28 (2.3) | 0.730 | .231 |
| Advice others going to the hospital after the appearance of symptoms related COVID-19 | 1729 (97.0) | 54 (3.0) | 1197 (98.3) | 21 (1.7) | 5.054 | .015 |
3.4. Regression analysis with behavior
Table 4 shows the regression analysis results for positive behavior (5 or more) during the COVID-19 pandemic. Being female (OR: 2.106, 95%CI: 1.259,3.522), 18 ≤ age < 65 (OR: 4.059, 95%CI: 2.166,7.607), being satisfied with the precautions taken by the community (OR: 2.594, 95%CI: 1.485,4.530), disinfecting public facilities in the community (OR:2.342, 95%CI: 1.206,4.547), having knowledge of transmission (OR: 3.987, 95%CI: 2.039,7.798), symptoms (OR: 2.045, 95%CI: 1.054,4.003) and outcomes (OR: 2.740, 95%CI: 1.513,4.962) of COVID-19, and those without anxiety symptoms (OR: 2.578, 95%CI: 1.127,5.901) were positively associated with affirmative behavior in urban areas. Meanwhile, being married (OR: 4.960, 95%CI: 2.608,9.434), being satisfied with the precautions taken by the community (OR: 2.484, 95%CI: 1.315,4.691), screening for face mask before entering the community (OR: 8.809, 95%CI: 2.649,19.294), having knowledge of precautions (OR: 4.886, 95%CI: 2.604,9.167) and outcomes (OR: 2.657, 95%CI: 1.309,5.391) were positively associated with affirmative behavior in rural areas.
Table 4.
Factors associated with greater behaviour (proxied by 5 or more good behaviours) during COVID-19 pandemic (n = 3001).
| Urban | Rural | |||
| Variables | OR (95% CI) | P | OR (95% CI) | P |
| Woman | 2.106 (1.259,3.522) | .005 | ||
| 18 ≤ age <65 | 4.059 (2.166,7.607) | <.001 | ||
| Age ≥ 65 | 6.064 (0.545, 67.424) | .143 | ||
| Married | 4.960 (2.608,9.434) | <.001 | ||
| Family members or relatives suspected or confirmed | 0.103 (0.008,1.240) | .073 | ||
| Community control | ||||
| Be satisfied with the precautions taken by community | 2.594 (1.485,4.530) | .001 | 2.484 (1.315,4.691) | .005 |
| Screening facemask wearing before entering community | 8.809 (2.649,19.294) | <.001 | ||
| Disinfecting communal facilities in community | 2.342 (1.206,4.547) | .012 | ||
| Knowledge level | ||||
| With knowledge of transmission | 3.987 (2.039,7.798) | <.001 | ||
| With knowledge of symptoms | 2.045 (1.054,4.003) | .0235 | ||
| With knowledge of precautions | 4.886 (2.604,9.167) | <.001 | ||
| With knowledge of outcomes | 2.740 (1.513,4.962) | .001 | 2.657 (1.309,5.391) | .007 |
| Without anxiety | 2.578 (1.127,5.901) | .025 | ||
4. Discussion
4.1. Mental health of rural and urban residents during COVID-19
To the best of our knowledge, this was the first time that a population-based study of psychology, knowledge, and behaviors was conducted in connection with COVID-19 that assessed the association between anxiety and depression among Chinese residents. Our study included a total of 3001 Chinese residents in urban and rural settings. The mental state of urban residents differed from that of their rural counterparts. In terms of anxiety, the mental anxiety of urban residents was significantly greater than that of rural residents, although the overall level was at a minimum. The results were similar with Wang and Ma et al.[17,18] The probable reason is linked to the information obtained. Since residents living in cities and towns could access a great deal of information about COVID-19 from mobile phones, shared media networks, and communities, they were exposed to more negative information than rural residents. Secondly, most of the urban residents lived in residential areas almost without going out, and although their rural counterparts were also home-based in line with disease prevention, the scope of activities was larger than urban residents, and people managed to communicate with their neighbors. Simultaneously, the municipal community management personnel were strict in implementing certain guidelines. Residents had to provide information about their physical condition several times in a day, to ensure that infected people were isolated from the community and prevented from going out. These factors directly aggravated the psychological anxiety of urban residents. Previous studies noted that people often showed anxiety symptoms during crises, which were the normal stress response of the body.[19,20] According to studies by Naragon and Wu,[21,22] anxiety is an acute stress response, and moderate anxiety was beneficial, which would make residents pay more attention toward the prevention of COVID-19. In this study, whether urban or rural, residents were in a perennial state of stress due to the prevailing pandemic situation. However, only 10% of the residents displayed a mild level of psychosomatic anxiety, which comprised the newly diagnosed patients in their private living areas.
Under the prevailing situation, depression was considerably greater among urban residents than their rural counterparts, who displayed minor symptoms. The probable causes were the environment in which the residents lived. When they received information about infected persons, urban residents would repeatedly recall whether they had come into contact with that particular person, thus increasing their depression levels. Concurrently, during the Spring Festival season, the residents expressed regret that they could not host the event and had to remain indoors; secondly, since the disease lasted for a long time, most of the residents were at home without returning to work, and they had no income, which led to depression. In a large number of studies, under public emergencies, residents’ depression will rise,[23,24] and the continuous increase of negative emotions was not conducive to physical and mental health.[25,26] Especially in the current global situation, it is imperative to provide timely psychological intervention.
4.2. Knowledge about COVID-19 among rural and urban residents
Based on our results, it can be inferred that knowledge of COVID-19 differed in rural and urban areas. Knowledge of transmission, prevention, infection, treatment, and prognosis of COVID-19 needs to be strengthened. The results were similar with Oh and Yi et al.[27,28] The main factor was that rural residents primarily comprised the elderly, who had a poor ability to access the latest knowledge and obtain information, and hence they did not have adequate knowledge about COVID-19. There is also a need to strengthen knowledge about treatment and prognosis regarding COVID-19. Given that COVID-19 is a nascent respiratory disease, at present, the treatment and prognosis are not evident anywhere in the world, and a corresponding treatment plan has not been announced, so our residents had insufficient knowledge of these two aspects. The principal means for residents to obtain knowledge was through WeChat, the community, the Internet, and TV news. However, there was not any difference between rural and urban residents in acquiring knowledge from TV news. A majority of residents in rural areas accessed knowledge through community interactions. Mohamed's results were different from our study.[29] Urban residents were mainly young people belonging to the contemporary generation. Information acquisition was based primarily on information equipment, the utilization of which was better than that of rural residents in,[30] so it also reflected the corresponding advantages in obtaining information. Individual was a separate entity. Residents conducted themselves differently under the COVID-19 situation. Rural and urban residents had differences in epidemiological history, seeing a doctor after the appearance of clinical symptoms, and suggesting preventive measure to others. The foremost reason was that residents gained knowledge about the disease. The more understanding of disease-related conditions, the better the affirmative behavior of residents.
4.3. Behavior of community residents with regard to COVID-19
The psychological emotions of residents were related to knowledge and behavior. In our study, being female and being urban residents under the age of 18 to 65 resulted in a more positive behavior. The behavior of residents was influenced by many factors.[31] Our research noted that young women's knowledge acceptance and behavioral changes were better than their male counterparts. In addition, most women are more compliant and more willing than men to choose appropriate behavior to protect themselves and their families. Satisfied with the preventive measures being taken by the community such as disinfecting public facilities, urban residents, with their knowledge of disease transmission, clinical symptoms, and prognosis, also have relatively positive behaviors. Under the COVID-19 situation, the positive behavior of residents was the key to prevention.[32] If the residents’ living environment and contact objects were strictly controlled, the lesser they panicked about the infection; secondly, the greater the disease-related knowledge and the deeper the understanding of the disease, the better the residents could use relevant knowledge to conduct positive disease prevention activities. Anxiety symptoms were positively correlated with the behavior of urban residents, that is, urban residents without anxiety symptoms had more positive disease prevention behaviors. A study reported similar trends in patients with breast cancer.[33] Patients without anxiety were calmer when faced with a crisis situation and would not indulge in inappropriate behavior due to panic. Therefore, under the same conditions, patients with better psychological conditions could adhere to appropriate behavior.[34]
Residents who lived in rural areas, who were married, were satisfied with the preventive measures taken by the community, took preventive measures, and had knowledge about COVID-19, demonstrated greater positive behaviors. Research by Taghrir and Geldsetzer showed that the degree of knowledge of the disease influenced the behavior of patients.[35,36] With appropriate knowledge, residents with preventive measures and outcomes of knowledge of COVID-19 could gradually increase their in-depth understanding of the disease, and then choose the right behavior, according to the current development of the disease. In addition, married residents did not consider themselves as just individuals. They often considered family factors and acted accordingly. Meanwhile, if family members chose positive behaviors, under their influence, they would act in accordance with them, which was conducive to the positive behavior of married people. During the period of COVID-19, there were reports of many patients dying and re-infection in patients after treatment, so residents paid close attention to their living environment. Satisfaction with preventive measures taken by the village or community influences the behavior of residents. Due to the surge in the number of confirmed and suspected cases, some patients with clinical symptoms similar to the disease needed to go to the hospital for confirmation, which increased their risk of infection. At this juncture, the disease prevention measures in the village or community were particularly important.
Some limitations of this study needed to be considered, given the fact that information on specific aspects of the residents’ way of knowledge and depression should have been added to the regression analysis. This was a cross-sectional studied by the residents. This study used a self-report questionnaire which might have the risk of overestimating the persons with anxiety or depression. Contrarily, there is a possibility of underestimating the number by using common diagnostic criteria. Since cognitive distortion can be present in persons with depression and anxiety, the assessment of psychology, knowledge and behaviors regarding COVID-19, and environmental factors could be biased. Furthermore, the data were accessed from only one country (China), which limits the applicability of the results. Data from additional countries are needed to confirm our results. Despite these limitations, our study also had considerable strength. First, this was a relatively large sample size study of Chinese residents on COVID-19, where we created a dichotomous residents variable (“urban” vs “rural”). Second, we were able to identify determinants of mild, moderate, or severe problems among urban and rural residents.
5. Conclusion
The status of anxiety and depression among urban residents was more severe compared to those living in rural areas. There was a difference in being positively associated with constructive behaviors between rural and urban areas. Urban participants reported significantly higher levels of knowledge regarding COVID-19 in all aspects (transmission, prevention measures, symptoms of infection, treatment, and prognosis), compared to their rural counterparts. While a majority of respondents in urban areas obtained knowledge through WeChat, other apps, and the Internet, residents in rural areas accessed information through interactions with the community. Urban residents fared well in exchanging knowledge about COVID-19 and advising others to take preventive measures, but fared poorly in advising people to visit a hospital if they displayed symptoms of the disease, compared to rural residents.
Acknowledgments
We are grateful to the residents who participated in the study. Members of the participators and researchers, Jianmei Zhang, Liang Zhu, Simin Li, Jing Huang, Zhiyu Ye, Quan Wei, Chunping Du.
Author contributions
Formal analysis: Jing Huang.
Investigation: Zhiyu Ye.
Methodology: Simin Li.
Writing – original draft: Jianmei Zhang, Liang Zhu.
Writing – review & editing: Quan Wei, Chunping Du.
Footnotes
Abbreviations: COVID-19 = The novel coronavirus SARS-CoV-2, GAD = General Anxiety Disorder, PHQ-9 = The 9-item Patient Health Questionnaire.
How to cite this article: Zhang J, Zhu L, Li S, Huang J, Ye Z, Wei Q, Du C. Rural–urban disparities in knowledge, behaviors, and mental health during COVID-19 pandemic: A community-based cross-sectional survey. Medicine. 2021;100:13(e25207).
There was no applicable funding.
The authors have no potential conflict of interests to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 90. World Health Organization; 2020. https://apps.who.int/iris/handle/10665/331859. [Google Scholar]
- [2].WHO. WHO Director-General's opening remarks at the media briefing on COVID-19. 2020. http://www.un.org.cn/info/7/1044.html. [Google Scholar]
- [3].Lau JT, Yang X, Tsui H, et al. Monitoring community responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J Epidemiol Community Health 2003;57:864–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lau JT, Tsui H, Lau M, et al. SARS transmission, risk factors, and prevention in Hong Kong. Emerg Infect Dis 2004;10:587–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Balkhy HH, Abolfotouh MA, Al-Hathlool RH, et al. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis 2010;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Leung GM, Lam TH, Ho LM, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health 2003;57:857–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Brodin P. Why is COVID-19 so mild in children? Acta Paediatr 2020;109:1082–3. [DOI] [PubMed] [Google Scholar]
- [8].Luo L, Zeng XJ, Yang YQ. Disease cognition, coping style and exercise behavior among the public during novel coronavirus epidemic: an online survey. Chin J Public Health 2020;36:156–9. [Google Scholar]
- [9].Zhang JH, Yan LX, Yuan Y. Comparing the mental health of rural-to-urban migrant children and their counterparts in china: Protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Xu Y, Wang CQ, Zhu Y. Forecast of the gap between urban and rural health resources in China from the perspective of healthy China Action. Chin Hosp Manage 2019;39:17–9. [Google Scholar]
- [11].Wang P, Mao QA, Tao MX, et al. Survey on the status of health literacy of Chinese residents in 2008. Chin J Health Educ 2010;doi:10.16168/j.cnki.issn.1002-9982.2010.04.021. [Google Scholar]
- [12].Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- [13].Plummer F, Manea L, Trepel D, et al. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- [14].Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 1999;282:1737–44. [DOI] [PubMed] [Google Scholar]
- [15].Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wittkampf KA, Naeije L, Schene AH, et al. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: a systematic review. Gen Hosp Psychiatry 2007;29:388–95. [DOI] [PubMed] [Google Scholar]
- [17].Wang HJ, Tan G, Deng Y, et al. Prevalence and risk factors of depression and anxiety among patients with convulsive epilepsy in rural West China. Acta Neurol Scand 2018;138:541–7. [DOI] [PubMed] [Google Scholar]
- [18].Ma X, Xiang YT, Cai ZJ, et al. Generalized anxiety disorder in China: prevalence, sociodemographic correlates, comorbidity, and suicide attempts. Perspect Psychiatr Care 2009;45:119–27. [DOI] [PubMed] [Google Scholar]
- [19].Beesley SJ, Hopkins RO, Holt-Lunstad J, et al. Acute physiologic stress and subsequent anxiety among family members of ICU patients. Crit Care Med 2018;46:229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sangenstedt S, Jaljuli I, Sachser N, et al. Stress responsiveness and anxiety-like behavior: The early social environment differentially shapes stability over time in a small rodent. Horm Behav 2017;90:90–7. [DOI] [PubMed] [Google Scholar]
- [21].Naragon-Gainey K, McMahon TP, Chacko TP. The structure of common emotion regulation strategies: a meta-analytic examination. Psychol Bull 2017;143:384–427. [DOI] [PubMed] [Google Scholar]
- [22].Wu DY, Guo M, Gao YS, et al. Clinical effects of comprehensive therapy of early psychological intervention and rehabilitation training on neurological rehabilitation of patients with acute stroke. Asian Pac J Trop Med 2012;5:914–6. [DOI] [PubMed] [Google Scholar]
- [23].Kinner SA, Alati R, Watt K, et al. Substance misuse, anxiety and depression and urgency of presentation to a public emergency department in Australia. Emerg Med Australas 2005;17:363–70. [DOI] [PubMed] [Google Scholar]
- [24].Kirsch KR, Feldt BA, Zane DF, et al. Longitudinal community assessment for public health emergency response to Wildfire, Bastrop County, Texas. Health Secur 2016;14:93–104. [DOI] [PubMed] [Google Scholar]
- [25].Shields MC, Matt LM, Coifman KG. Physical activity and negative emotion during peer-rejection: Evidence for emotion context sensitivity. J Health Psychol 2016;21:2851–62. [DOI] [PubMed] [Google Scholar]
- [26].Oh VYS, Tong EMW. Negative emotion differentiation and long-term physical health—the moderating role of neuroticism. Health Psychol 2020;39:127–36. [DOI] [PubMed] [Google Scholar]
- [27].Fritzell C, Raude J, Adde A, et al. Knowledge, attitude and practices of vector-borne disease prevention during the emergence of a new arbovirus: implications for the control of Chikungunya Virus in French Guiana. PLoS Negl Trop Dis 2016;10:e0005081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yi L, Xu X, Ge W, et al. The impact of climate variability on infectious disease transmission in China: current knowledge and further directions. Environ Res 2019;173:255–61. [DOI] [PubMed] [Google Scholar]
- [29].Mohamed MMG, Shwaib HM, Fahim MM, et al. Ebola hemorrhagic fever under scope, view of knowledge, attitude and practice from rural Sudan in 2015. J Infect Public Health 2017;10:287–94. [DOI] [PubMed] [Google Scholar]
- [30].Zhu T, Xu H. Status and influencing factors of diabetes information acquisition among rural elderly with pre-diabetes in Yiyang City, China: a cross-sectional study. BMJ Open 2019;9:e029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Grysman A, Merrill N, Fivush R. Emotion, gender, and gender typical identity in autobiographical memory. Memory 2017;25:289–97. [DOI] [PubMed] [Google Scholar]
- [32].Richards P, Amara J, Ferme MC, et al. Social pathways for Ebola virus disease in rural Sierra Leone, and some implications for containment. PLoS Negl Trop Dis 2015;9:e0003567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Tsaras K, Papathanasiou IV, Mitsi D, et al. Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pac J Cancer Prev 2018;19:1661–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Li S, Wang Y, Xue J, et al. The Impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo Users. Int J Environ Res Public Health 2020;17:2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Taghrir MH, Borazjani R, Shiraly R. COVID-19 and Iranian Medical Students; a survey on their related-knowledge, preventive behaviors and risk perception. Arch Iran Med 2020;23:249–54. [DOI] [PubMed] [Google Scholar]
- [36].Geldsetzer P. Use of rapid online surveys to assess people's perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res 2020;22:e18790. [DOI] [PMC free article] [PubMed] [Google Scholar]


