Abstract
Cervical spine (C-spine) fractures in young children are very rare, and little information on treatment modalities and functional, radiographic, and patient-reported outcome exists. In this 2-center, retrospective case series, we assessed subjective and functional mid-term outcomes in children aged ≤5 years whose C-spine fractures were treated nonoperatively.
Between 2000 and 2018, 6 children (median age at injury: 23.5 months; range: 16–31 months) with C1 or C2 injuries were treated with Minerva cast/brace or soft collar brace at 1 of the 2 study centers. Two patients suffered C1 fractures, and 4 patients had lysis of the odontoid synchondrosis. Overall, 3 children had sustained polytrauma. One child died due to the consequences of massive head injury.
For the primary outcome parameter, we recorded subjective symptoms such as pain and functional restrictions due to the sequelae of C-spine injuries at follow-up.
Based on medical records, we also assessed the causes of injury, diagnostic procedures, treatments and complications, and time to fracture consolidation.
Median follow-up of the 5 surviving children was 51 months (range: 36–160 months). At the latest follow-up, 4 of 5 children did not complain of any pain. One child who sustained an open head injury in combination with a subluxation of the odontoid and undisplaced fracture of the massa lateralis reported occasional headache. All patients experienced complete fracture healing and normal range of motion of the cervical spine.
Median duration of cast/brace treatment was 8.5 weeks. Fracture healing was confirmed by computed tomography in all patients.
All C-spine injuries were managed with either Minerva cast/Halo brace or soft collar brace without complications.
In our retrospective case series, nonoperative treatment of atlas fractures and dislocations or subluxations of the odontoid in young children using Minerva casts or prefabricated Halo braces resulted in good subjective and functional outcomes at mid-term. We observed no complications of conservative treatment of C1 and C2 injuries in young children.
Keywords: atlas, children, fracture, Minerva cast, nonoperative treatment, odontoid, outcome, upper cervical spine
1. Introduction
The incidence of cervical spine (C-spine) injuries in children ≤5 years of age is very low with a reported prevalence of 0.4%.[1] Fractures and dislocations of the upper C-spine are usually the result of high-energy trauma and are therefore associated with significant morbidity and mortality rates.[2–4]
Management algorithms used in adults often do not apply to children and diagnosis, adequate treatment, as well as nursing can present a significant challenge.[3]
Treatment of upper C-spine fractures in children is predominantly conservative, but displaced fractures and accompanying neurologic lesions may require surgical stabilization.[5] The goals of treatment are to restore maximum functional ability at a minimum of residual pain, to avoid permanent neurologic deficits, and to achieve stable fracture union with no residual deformity, thus preventing long-term disability.[6,7] Malunion, instability, post-traumatic stenosis of the spinal canal, and neurologic complications may be prevented if such injuries are recognized early and managed appropriately.
Therefore, age-adapted algorithms for evaluating and managing C-spine fractures in children are urgently needed.[8] Most level 1 trauma centers treat only 1 or 2 patients with C-spine fractures per year.[9] For this reason, no large studies are available, and recommendations on diagnosis and therapeutic management are based on case series.[4]
The aim of this study was to evaluate the mid-term subjective and functional outcomes after nonoperative treatment of C1 fractures and lyses of the odontoid synchondrosis with Minerva casts or braces in children ≤5 years of age. In addition, we analyzed the type and duration of immobilization, imaging modalities used for confirmation of consolidation, diagnostic procedures applied to assess C-spine injuries and obtain C-spine clearance, potential complications associated with conservative treatment, and time to consolidation of injuries.
2. Patients and methods
After approval of the study by the responsible Ethics Committee (EKNZ 2017-00112), we performed a retrospective, 2-center case series in children who had suffered a C-spine injury at the level of C1 or C2 and were treated at either of the 2 pediatric trauma centers involved.
The Department of Pediatric Traumatology and Orthopedics, Katowice, Poland, has a catchment area of 5.3 million people (Upper Silesian area), while the Department of Pediatric Surgery, University Children's Hospital Basel, Switzerland, has a catchment area of approx. 0.7 million people. During the 18-year study period (2000–2018), we treated 3 patients at each of the 2 study centers.
Due to the low number of eligible patients for our investigation, we decided against a sample size estimation.
For inclusion, the children with a C1 or C2 injury had to be aged ≤5 years. In accordance with Hale et al, we selected the age range of 0 to 5 years based on the developmental characteristics of the growing spine.[1]
We excluded children with congenital C-spine anomalies, pre-existing musculoskeletal or neurologic disorders, as well as patients with a history of previous C-spine injury.
The primary outcome parameter was patients’ complaints and clinical C-spine function at a minimum follow-up period of 3 years. Within this period, injury-related growth disturbances or functional limitations should be apparent. At follow-up, we elicited the subjective complaints such as pain and/or restrictions in daily activities, evaluated active range of motion (ROM) of the C-spine, and took plain lateral X-ray images of the C-spine.
We recorded the technique and duration of immobilization as well as imaging modalities used for confirmation of consolidation of injuries.
In children with suspected C-spine injury, the C-spine was initially immobilized with a rigid cervical orthosis specifically designed for children. Active ROM of the C-spine was assessed in conscious and cooperative children only. If neurologic alterations were observed on examination, urgent re-assessment was performed by the neuropediatric and pediatric neurosurgeon on call.
Initial imaging included anteroposterior (AP) and lateral plain X-ray images and further radiographic evaluation with computed tomography (CT) and magnetic resonance imaging (MRI) as described by Platzer et al[9] in case of suspected injury of the upper C-spine.
If an unstable fracture was detected, the Katowice center used prefabricated light-weight synthetic Minerva orthoses (Collar Stark Halo, MDH, Lodz, Poland) whereas the Children's Hospital in Basel favored Minerva plaster casts for conservative treatment.
One child with severe open head injury did not undergo any immobilization to prevent increased intracranial pressure and interference with cerebral blood circulation after bilateral decompressive craniectomy and intracranial pressure monitoring. Lack of immobilization in this patient was not regarded as a problem since we deemed the subluxation of the odontoid synchondrosis stable.
We removed the Minerva braces after confirming fracture consolidation by plain X-ray images or CT scans, and after the child did no longer complain of neck pain or C-spine tenderness. Moreover, active ROM of the neck and spine had to be painless after removal of the Halo brace or Minerva cast; otherwise, the Halo brace or Minerva cast was applied again. After removal, the children had to wear a soft collar brace for additional 2 weeks. Families were advised to increase the number of hours without wearing the brace day by day to ensure the safe build-up of neck muscles. We additionally prescribed physiotherapy to gently increase muscle strength. When the children had regained full and painless ROM of the neck, they could return to physical activities.
We retrospectively recorded patient characteristics, mechanism of injury, concomitant injuries, and complications. Between 2000 and 2018, we treated 6 children (1 boy, 5 girls) with upper C-spine fractures at two level 1 pediatric trauma centers (Table 1).
Table 1.
Patient characteristics, type of cervical spine injury, and diagnostic imaging modalities applied after admission in 6 children who suffered C1/C2 fractures.
| Patient | Age (mo) | Sex | Cause of injury | Type of injury of upper cervical spine; spinal cord injury | Diagnostic imaging modality applied after admission | Concomitant injury |
| 1 | 23 | Female | Bunk bed fall | Fracture of anterior atlas arch, undisplaced (Gehweiler Type I)[27] | CT, MRI | None |
| 2 | 24.5 | Female | MVC, restrained rear seat car passenger | Lysis of odontoid synchondrosis (23° dislocated anteriorly) | X-ray, CT | Liver contusion, skin abrasions |
| 3 | 31 | Female | Roll over injury by MV | Subluxation of odontoid synchondrosis, fracture massa lateralis, undisplaced | CT | Polytrauma, severe open head injury, femur fracture, eye injury, skin abrasions |
| 4 | 18 | Female | MV-pedestrian collision | Dislocation of odontoid synchondrosis (dislocated anteriorly) and quadriplegia | X-ray, CT, MRI | Polytrauma, severe head injury, subarachnoid hematoma, hepatic laceration (on-site resuscitation) |
| 5 | 24 | Female | MVC, restrained rear seat car passenger | Subluxation of odontoid synchondrosis | X-ray, CT, MRI | Polytrauma, head injury, thoracic trauma, pneumothorax forearm fracture |
| 6 | 16 | Male | Fall from a height of 2 m | Fracture of anterior atlas arch (Gehweiler type I)[27] | X-ray, MRI | Thoracic trauma, blunt abdominal trauma |
Due to the very low incidence of C1/C2 injuries in young children and for ethical reasons, we were unable to compare diagnostic and therapeutic procedures applied in our patients to those used in children of a control group. We compared our results to results of other study groups.
The data were analyzed descriptively and presented in tables since no statistical analysis was possible in the small case series.
3. Results
At the final follow-up after a median of 51 months (range: 36–160 months), 1 child of the 5 surviving children complained of occasional headache after severe open head injury and accompanying odontoid fracture. None of the children complained of neck pain or suffered from functional restrictions of cervical spine mobility at follow-up, and all fractures had healed in correct alignment without signs of growth disturbances (Table 2).
Table 2.
Treatment of C1/C2 injuries of the 6 children, and subjective, functional, and radiographic findings at follow-up in the 5 surviving children.
| Patient | Type (and duration) of neck immobilization | Applied imaging modality for confirmation of consolidation | Follow-up interval (mo) | Subjective complaints at follow-up | Functional outcome of cervical spine injury | Radiographic findings at follow-up |
| 1 | Minerva cast (57 d) | CT | 36 | None | No restriction of neck ROM | Healed in correct alignment |
| 2 | Minerva cast (73 d) | X-ray, CT | 44 | None | No restriction of neck ROM | Healed in correct alignment |
| 3 | No immobilization (due to severe open head injury and bilateral decompressive craniectomy) | CT (after 35 d) | 160 | Occasional headache and visual impairment due to severe head injury | No restriction of neck ROM | Healed in correct alignment |
| 4 | Soft collar | – | Died after 5 d from severe head injury | – | – | – |
| 5 | Minerva orthosis (64 d) | X-ray, CT, active flexion and extension radiographs | 134 | None | No restriction of neck ROM | Healed in correct alignment |
| 6 | Minerva orthosis (48 d) | X-ray, CT, active flexion, and extension radiographs | 51 | None | No restriction of neck ROM | Healed in correct alignment |
Table 2 shows the type and duration of C-spine immobilization. We obtained CT scans of the upper C-spine in 2 patients with C1 fractures and 3 patients with C2 injuries after an average of 60 days (range: 48–73 days) to confirm correct fracture healing. In 2 children, the fracture line was still visible on the CT scan performed after 60 days, but there was no instability or tenderness of the neck on clinical examination after removal of the cast or brace in 1 child. In the other child, we re-applied the Minerva brace for 13 additional days.
Correct fracture alignment was confirmed based on lateral X-rays in 3 children. In two of them, we obtained additional active flexion and extension radiographs of the C-spine (Table 2).
To establish initial diagnosis in suspected C-spine injuries, we obtained lateral spine X-ray images in 4 of the 6 children and CT scans in 5 of the 6 children. We obtained lateral spine radiographs with positioning the child's neck and trunk as described by Herzenberg et al.[10] Subsequently, MRI scans of the C-spine were obtained as soon as possible after hospital admission in 4 of the 6 children.
Table 1 shows the radiologic methods applied for diagnostic imaging after admission and results of radiologic imaging. Two patients had suffered C1 fractures, and 4 children had experienced C2 injuries (Figs. 1–10). In 1 child, clinical examination suggested lysis of odontoid synchondrosis, but initial plain X-ray images, CT scan, and MRI alluded to intact basilar odontoid synchondrosis. We applied a Minerva brace and obtained a second opinion from another pediatric radiology department, who confirmed our initial clinical diagnosis of subluxation of the odontoid synchondrosis.
Figure 1.
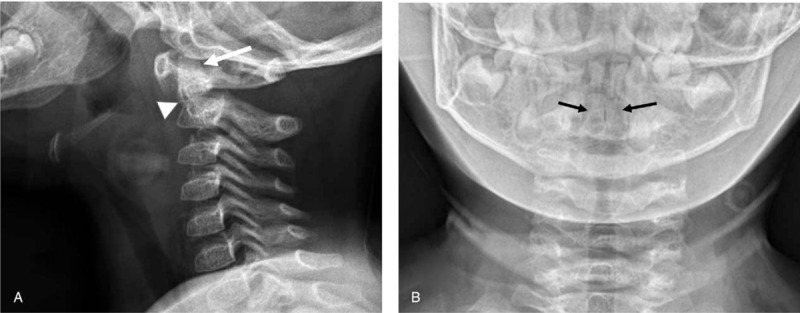
Dislocation of basal synchondrosis of the odontoid process in a girl aged 24.5 mo, who suffered a dislocation of the basal synchondrosis of the odontoid in a car head-onto-head collision. She had been correctly restrained in a safety seat and was conscious at admission. The patient presented without signs of neurologic injury at admission to the A&E unit. (a) Plain lateral X-ray image of the C-spine shows moderate forward angulation of the odontoid process (arrow) and dislocation of the basal synchondrosis of the odontoid (arrowhead). (b) Plain AP X-ray image of the C-spine showing bipartite odontoid process (arrows). The dislocation is not visible in AP view. The neck is immobilized with a rigid cervical collar.
Figure 10.
CT scan of cervical spine obtained more than 6 yr after the first injury. The child was hit in the neck by another child 6.4 yr after the lysis of the synchondrosis of the odontoid. She sustained a painful restriction of neck movements. A&E physicians obtained a CT scan of the C-spine, and no fracture was found. The odontoid synchondrosis had fused at this time point, and there was no residual deformity of the odontoid. The child recovered uneventfully after wearing a soft collar brace for 1 wk.
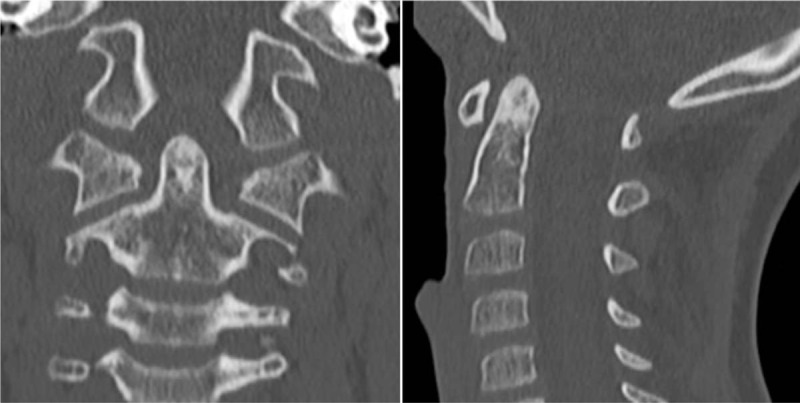
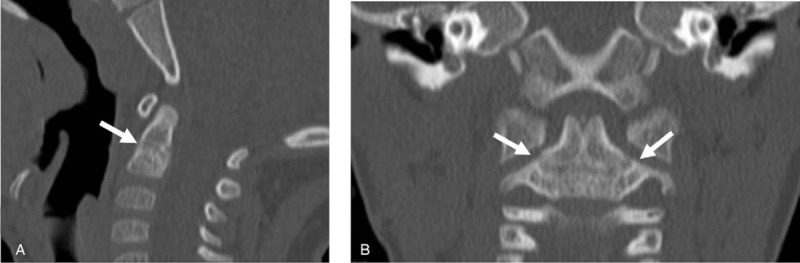
Figure 2.
Dislocation of the basal synchondrosis of the odontoid process in a girl aged 24.5 mo. (a) CT scan reconstruction shows the dislocation of the synchondrosis of C2 (arrows). (b) Note forward angulation of the odontoid process by 23° (arrow).
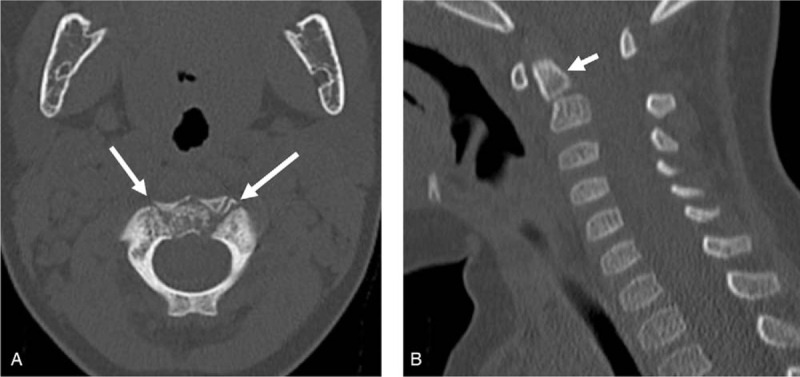
Figure 3.
Dislocation of the basal synchondrosis of the odontoid process in a girl aged 24.5 mo. (a) After shaving her hair and putting on a tricot shirt, padding was applied for the cast. Thereafter we cautiously performed image intensifier-controlled reduction of forward angulation of the odontoid process. (b) Monitoring of manual reduction of dislocation of the odontoid process (arrow) using lateral fluoroscopic imaging.
Figure 4.

Minerva cast application. (a) A synthetic light-weight soft and hard cast (Minerva cast) was applied with hyperextension of the C-spine to stabilize the reduced lysis of the basal synchondrosis of the odontoid. (b) Lateral X-ray image of the C-spine obtained 3 wk after injury confirmed correct position of the odontoid process (arrow). No AP plain X-ray was obtained at this stage.
Figure 5.

Management of the young child treated with Minerva cast. (a) Sufficient padding of the Minerva cast was applied to cover margins of the cast. Note the hyperextension of the C-spine facilitating adequate external retention of lysis of the synchondrosis of the odontoid process. (b) Minerva cast shows an opening at the upper region of the head. (c) Support by parents during ambulation helped to prevent falls due to impaired visibility of the ground when walking.
Figure 6.
Confirmation of bony consolidation by CT scan obtained 2.5 mo after injury. (a and b) Confirmation of stable consolidation of the lysis of the basal synchondrosis of the odontoid (arrowhead) in sagittal plane (a) and frontal plane (b).
Figure 7.

Replacement of Minerva cast by soft cervical collar. The Minerva cast was removed after 2.5 mo, and a soft collar brace (arrowhead) was applied for 2 wk.
Figure 8.

Radiographic confirmation of correct alignment of healed lysis of the synchondrosis of the odontoid. Lateral X-ray image of the C-spine shows correct alignment and normal length of odontoid process at follow-up 44 mo after injury. No AP X-ray image was obtained.
Figure 9.
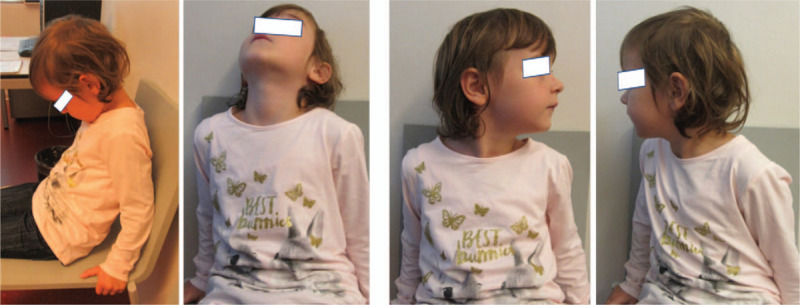
Photographic documentation of unrestricted ROM cervical spine. Documentation of unrestricted ROM of the C-spine at follow-up.
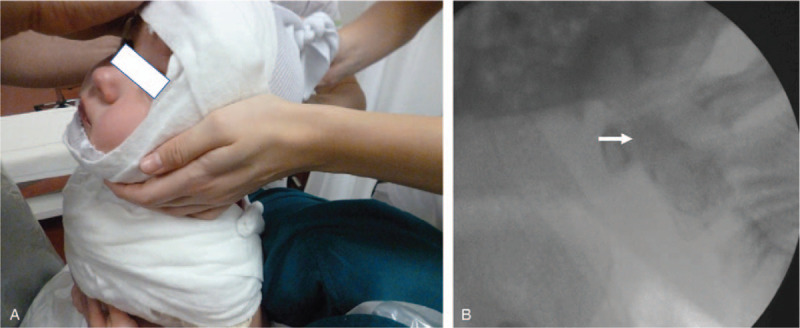
Median age of the 6 children was 23.5 months (range: 16–31 months). One patient with dislocation of odontoid synchondrosis, complete quadriplegia, and severe head injury died from massive head injury 5 days after the incident (Fig. 11).
Figure 11.
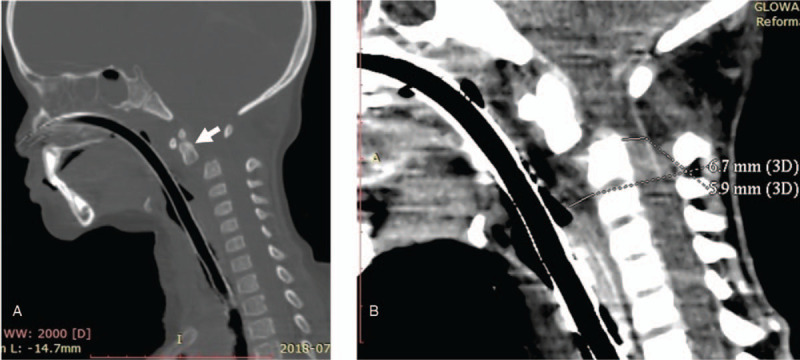
Young child suffering from dislocation of the odontoid synchondrosis, quadriplegia, and severe head injury. (a) Dislocation of synchondrosis of the odontoid process in a girl aged 18 mo (arrow). She was injured in a motor-vehicle pedestrian collision and suffered polytrauma characterized by severe head injury and quadriplegia. (b) Prevertebral soft tissue swelling at the upper C-spine amounted to 6.7 mm, and the diameter of the spinal cord was reduced to 5.9 mm. Note the dislocation of the odontoid process by 1 width of the odontoid.
The injuries were caused by a road-traffic accident in 4 children and a fall from a height of 2 m or a bunk bed in 2 children.
In 3 of the 6 children, C-spine fractures were accompanied by multiple injuries (polytrauma). Three children suffered accompanying head injuries, while 2 children experienced thoracic trauma and 3 children suffered blunt abdominal trauma. In 2 children, we additionally observed long-bone fractures (Table 1).
We did not observe any complications related to conservative treatment of C1/C2 injuries.
4. Discussion
At a median follow-up of 51 months, we observed painless and unrestricted ROM of the C-spine and bony consolidation in all surviving children. These findings are in accordance with the results of other authors reporting on nonoperative treatment of C1/C2 fractures in young children.[4,9,11,12]
In agreement with other authors and according to a Cochrane review,[13] we recommend obtaining cervical X-ray images in lateral projection, rather than open-mouth odontoid X-rays images, in children less than 8 to 10 years of age.[5,14–16] Frequently, the upper C-spine is not visualized clearly in the AP projection, and open-mouth X-ray images are difficult to obtain in young children.[14] We obtained CT or MRI scans in all children as soon as possible after hospital admission.
Herman et al questioned whether CT scans should be used in children younger than 5 years and postulated to use MRI rather than CT.[16] MRI represents the most sensitive and specific imaging modality in acute C-spine trauma in young children.[6,14]
We agree with Hale et al that CT and MRI studies should be conducted in children with clinically suspected C-spine injuries without radiographic abnormalities, and in obtunded or comatose children.[1] Especially in young children, the possibility of a ligamentous spine injury of the upper C-spine must be taken into consideration.[9,14] However, based on the data of Hale et al, the risk of missing a C-spine injury in asymptomatic responsive young children appears to be low.[1]
In accordance with McAllister et al, we observed fractures of the anterior arch of C1 and lyses of the synchondrosis of the odontoid.[14,17]
In 1 child suffering from tenderness of the upper C-spine, we were not able to differentiate between lysis of the basal synchondrosis of the odontoid and a normal ossification pattern despite obtaining a lateral plain X-ray image as well as CT and MRI scans. Lysis of the odontoid synchondrosis was confirmed by obtaining a second opinion by an external pediatric radiology institution.
Especially young children suffering from C-spine injuries usually do not require surgical intervention and can be treated safely with external immobilization after adequate clinical evaluation and diagnostic imaging.[5,9] As far as the indications for conservative treatment of these fractures are concerned, the age of the child and lack of fracture displacement constitute an absolute indication for conservative treatment. However, accompanying severe head injury may be considered an indication for surgery due to the difficulty of immobilizing the head. The rare unstable fractures possibly accompanied by a neurologic deficit may also represent a contraindication for conservative treatment. In 1 of our patients suffering from a stable odontoid fracture and severe open head injury, orthosis application was impossible due to bilateral decompressive craniectomy. If this child would have suffered from an unstable or displaced fracture of the odontoid, we would have considered surgical stabilization of the fracture.
Several authors reported no difference in outcomes after conservative and surgical treatment of C-spine fractures in children.[18] However, the treatment of choice in the management of displaced fractures of the growing C-spine consists of closed reduction and external bracing.
Most authors opt for operative stabilization only in C-spine fractures caused by penetrating wounds, in case of severe deformities of the spine, or if closed reduction cannot be achieved.[19] Secondary surgical stabilization is required in children suffering from malunion, nonunion, or chronic instability.[19] Surgical stabilization also allows minimization of external fixation, early mobilization, and simplified nursing.[20] The youngest patient reported in the literature who underwent surgery for C-spine fracture was 2 weeks old.[21]
To confirm consolidation of fractures and stability of the upper C-spine, we obtained plain lateral and AP X-ray images in 3 of the 5 surviving children. In 2 of these children, we additionally obtained X-ray images with active flexion and extension of the C-spine according to the recommendation of McAllister et al.[14] In addition, we obtained CT scans of the C-spine in all surviving children. This corroborates the notion that confirming stable fracture consolidation and excluding any residual C-spine instability in children is as challenging as establishing the correct diagnosis in the accident and emergency (A&E) setting.
Use of Minerva-type orthoses has been recommended for a treatment period of 2 to 3 months.[22] It should be noted that some authors used a soft cervical collar only,[10,21] while others used a Philadelphia collar[23] or halo vest[24–26] to stabilize C-spine fractures in young children. We used prefabricated, light-weight synthetic Minerva brace orthoses (Collar Stark Halo, MDH, Lodz, Poland) at the Katowice center and Minerva plaster casts at the Basel center for a median duration of 8.5 weeks (range: 7–10 weeks). The use of different orthoses did not translate into divergent handling problems or differences in outcome. The Minerva cast seems to provide more stability, whereas the prefabricated Collar Stark Halo is technically easier and more comfortable.
Overall, we treated 2 children suffering from anterior atlas arch fractures (Gehweiler type I)[27] (Table 1). Atlas ring injuries in children are unique because of the open synchondrosis which may remain non-ossified until late in the first decade of life. Non-ossified synchondrosis does not provide sufficient protection during massive tension, allowing the ring to widen.[8,24,28]
Because the immature spine ossifies progressively throughout childhood, injuries in younger children tend to be avulsions or epiphyseal separations rather than typical fractures. In our series of patients; in most children, separation of the synchondrosis at the base of the odontoid process was present.[11,19,28–30] In 2 of the 6 children in our study, dislocation of the odontoid process occurred. This was complicated by quadriplegia in 1 child.
Our study did not bring to light any complications associated with conservative treatment of C1/C2 injuries involving Minerva cast or braces. However, occurrence of pressure sores, redness of the skin, and itching sensations related to the use of braces or casts may occur.
C-spine injures in young children are usually caused by motor-vehicle incidents, falls from height, or child abuse.[3,4,6,11,28,31] In our group of patients, road-traffic incidents predominated as the cause of injury.
In total, 3 of the 6 children suffered from multiple injuries and were admitted to the intensive care unit. One child with polytrauma died from severe head injury and complete quadriplegia (ASIA A).[4,32] Mortality associated with severe head injury in children suffering from C-spine injuries has been described by other authors.[4,9]
4.1. Study limitations and strengths
The results of our case series should be interpreted with caution due to the small number of children included and bias related to the retrospective design of our investigation.
In terms of the study strengths, we collected data from 2 busy level 1 pediatric trauma centers in Europe. Children underwent nonoperative treatment by closed reduction if required, followed by Minerva cast or brace immobilization. We followed up surviving children for at least 36 months to obtain mid-term subjective, functional, and radiographic results.
4.2. Recommendations and future directions
Due to the severity of these injuries, we recommend implementation and reinforcement of active and passive injury prevention guidelines for children involved in motor-vehicle incidents, as either car occupants or pedestrians. Further prospective, adequately powered multicenter studies are required to investigate causes and consequences of C-spine injuries in young children.
Figure 12 shows our proposed management algorithm for young children with suspected upper C-spine injury based on our findings and the cited literature.[1,4,8–21,24,25,27–38]
Figure 12.
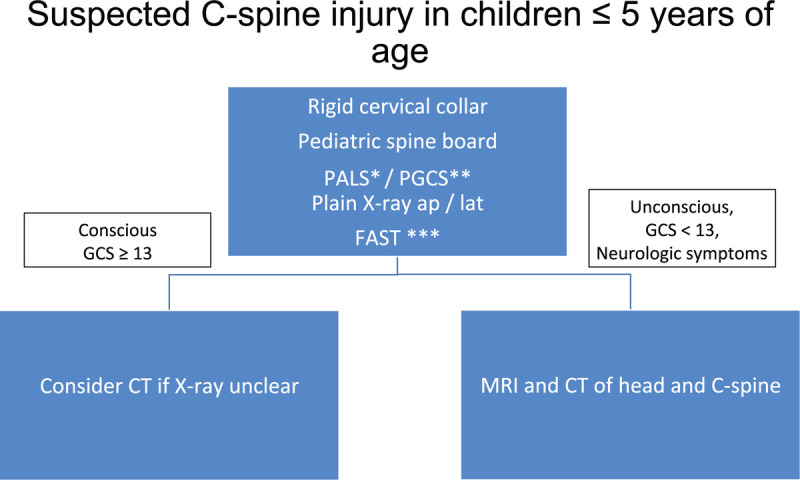
Management algorithm for young children with suspected upper C-spine injury. Algorithm applied for injured children presenting to the A&E room (∗PALS: Pediatric Advanced Live Support[34,36]; ∗∗PGCS: Pediatric Glasgow Coma Scale[37]; ∗∗∗FAST: Focused Assessment Sonography for Trauma[38]).
5. Conclusion
In our retrospective case series, nonoperative treatment of dislocation or subluxation of the odontoid synchondrosis or C1 fractures in young children using Minerva braces or casts resulted in stable consolidation of injuries with good mid-term subjective and functional outcomes. Nonoperative treatment did not result in any complications.
Because radiographic findings of the growing C-spine are complex and variable, care must be taken to correctly interpret fracture lines, synchondroses, and signs of instability.
Acknowledgments
We thank Dr. Silvia M. Rogers, MEDIWRITE GmbH, Basel, Switzerland, for her editorial assistance.
Author contributions
Conceptualization: Ryszard Tomaszewski, Johannes M Mayr, Sergio B Sesia.
Data curation: Ryszard Tomaszewski, Sergio B Sesia.
Formal analysis: Sergio B Sesia, Ryszard Tomaszewski.
Methodology: Sergio B Sesia.
Project administration: Johannes M Mayr.
Supervision: Johannes M Mayr, Daniel Studer, Erich Rutz.
Validation: Erich Rutz.
Writing – original draft: Ryszard Tomaszewski.
Writing – review & editing: Johannes M Mayr, Daniel Studer, Erich Rutz.
Footnotes
Abbreviations: A&E = accident and emergency, AP = anteroposterior, C1, C2 = vertebral body C1, C2, C-spine = cervical spine, CT = computed tomography, FAST = focused assessment sonography for trauma, MRI = magnetic resonance imaging, PALS = pediatric advanced life support, PGCS = Pediatric Glasgow Coma Scale, ROM = range of motion, SCIWORA = spinal cord injury without radiographic abnormality.
How to cite this article: Tomaszewski R, Sesia SB, Studer D, Rutz E, Mayr JM. Conservative treatment and outcome of upper cervical spine fractures in young children: A STROBE-compliant case series. Medicine. 2021;100:13(e25334).
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Hale DF, Fitzpatrick CM, Doski JJ, et al. Absence of clinical findings reliably excludes unstable cervical spine injuries in children 5 years or younger. J Trauma Acute Care Surg 2015;78:943–8. [DOI] [PubMed] [Google Scholar]
- [2].Mohseni S, Talving P, Branco BC, et al. Effect of age on cervical spine injury in pediatric population: a National Trauma Data Bank review. J Pediatr Surg 2011;46:1771–6. [DOI] [PubMed] [Google Scholar]
- [3].Polk-Williams A, Carr BG, Blinman TA, et al. Cervical spine injury in young children: a National Trauma Data Bank review. J Pediatr Surg 2008;43:1718–21. [DOI] [PubMed] [Google Scholar]
- [4].Knox JB, Schneider JE, Cage JM, et al. Spine trauma in very young children: a retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J Pediatr Orthop 2014;34:698–702. [DOI] [PubMed] [Google Scholar]
- [5].Goldstein HE, Anderson RC. Classification and management of pediatric craniocervical injuries. Neurosurg Clin N Am 2017;28:73–90. [DOI] [PubMed] [Google Scholar]
- [6].Kapapa T, Tschan CA, König K, et al. Fracture of the occipital condyle caused by minor trauma in child. J Pediatr Surg 2006;41:1774–6. [DOI] [PubMed] [Google Scholar]
- [7].Badman BL, Rechtine GR. Spinal injury considerations in the competitive diver: a case report and review of the literature. Spine J 2004;4:584–90. [DOI] [PubMed] [Google Scholar]
- [8].Reilly CW. Pediatric spine trauma. J Bone Joint Surg Am 2007;89: Suppl 1: 98–107. [DOI] [PubMed] [Google Scholar]
- [9].Platzer P, Jaindl M, Thalhammer G, et al. Cervical spine injuries in pediatric patients. J Trauma 2007;62:389–96. [DOI] [PubMed] [Google Scholar]
- [10].Herzenberg JE, Hensinger RN, Dedrick DK, et al. Emergency transport and positioning of young children who have an injury of the cervical spine. The standard backboard may be hazardous. J Bone Joint Surg Am 1989;71:15–22. [PubMed] [Google Scholar]
- [11].Odent T, Langlais J, Glorion C, et al. Fractures of the odontoid process: a report of 15 cases in children younger than 6 years. J Pediatr Orthop 1999;19:51–4. [PubMed] [Google Scholar]
- [12].Hosalkar HS, Greenbaum JN, Flynn JM, et al. Fractures of the odontoid in children with an open basilar synchondrosis. J Bone Joint Surg Br 2009;91:789–96. [DOI] [PubMed] [Google Scholar]
- [13].Slaar A, Fockens MM, Wang J, et al. Triage tools for detecting cervical spine injury in pediatric trauma patients. Cochrane Database Syst Rev 2017;12:CD011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].McAllister AS, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Radiographics 2019;39:1126–42. [DOI] [PubMed] [Google Scholar]
- [15].Easter JS, Barkin R, Rosen CL, et al. Cervical spine injuries in children, part I: mechanism of injury, clinical presentation, and imaging. J Emerg Med 2011;41:142–50. [DOI] [PubMed] [Google Scholar]
- [16].Herman MJ, Brown KO, Sponseller PD, et al. Pediatric cervical spine clearance: a consensus statement and algorithm from the pediatric cervical spine clearance working group. J Bone Joint Surg Am 2019;101:e1. [DOI] [PubMed] [Google Scholar]
- [17].Shah K, Tikoo A, Kothari MK, et al. Current concepts in pediatric cervical spine trauma. Open Orthop J 2017;11:346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Aebi M. Surgical treatment of upper, middle, and lower cervical injuries and non-unions by anterior procedures. Eur Spine J 2010;19: Suppl 1: S33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hill SA, Miller CA, Kosnik EJ, et al. Pediatric neck injuries. A clinical study. J Neurosurg 1984;60:700–6. [DOI] [PubMed] [Google Scholar]
- [20].Saleh S, Swanson KI, Bragg T. Successful surgical repair, and recovery in a 2-week-old infant after birth-related cervical fracture dislocation. J Neurosurg Pediatr 2018;21:16–20. [DOI] [PubMed] [Google Scholar]
- [21].Kakarla UK, Chang SW, Theodore N, et al. Atlas fractures. Neurosurgery 2010;66: Suppl: 60–7. [DOI] [PubMed] [Google Scholar]
- [22].Gaskill SJ, Marlin AE. Custom fitted thermoplastic Minerva jackets in the treatment of cervical spine instability in preschool age children. Pediatr Neurosurg 1990;16:35–9. [DOI] [PubMed] [Google Scholar]
- [23].Alcelik I, Manik KS, Sian PS, et al. Occipital condylar fractures. Review of the literature and case report. J Bone Joint Surg Br 2006;88:665–9. [DOI] [PubMed] [Google Scholar]
- [24].Vilela MD, Peterson EC. Atlantal fracture with transverse ligament disruption in a child. Case report. J Neurosurg Pediatr 2009;4:196–8. [DOI] [PubMed] [Google Scholar]
- [25].Lowry DW, Pollack IF, Clyde B, et al. Upper cervical spine fusion in the pediatric population. J Neurosurg 1997;87:671–6. [DOI] [PubMed] [Google Scholar]
- [26].Caird MS, Hensinger RN, Weiss N, et al. Complications and problems in halo treatment of toddlers: limited ambulation is recommended. J Pediatr Orthop 2006;26:750–2. [DOI] [PubMed] [Google Scholar]
- [27].Gehweiler JA, Duff DE, Martinez S, et al. Fractures of the atlas vertebra. Skelet Radiol 1976;1:97–102. [Google Scholar]
- [28].Bisson E, Schiffern A, Daubs MD, et al. Combined occipital-cervical and atlantoaxial disassociation without neurologic injury: case report and review of the literature. Spine 2010;35:E316–21. [DOI] [PubMed] [Google Scholar]
- [29].Huber H, Ramseier LE, Boos N. Open mouth digital reduction of an odontoid synchondrosis fracture: a case report. J Pediatr Orthop 2010;30:115–8. [DOI] [PubMed] [Google Scholar]
- [30].Kinkpé CV, Dansokho AV, Coulibaly NF, et al. Fracture of the odontoid process in children: a case report. Orthop Traumatol Surg Res 2009;95:234–6. [DOI] [PubMed] [Google Scholar]
- [31].Dormans JP. Evaluation of children with suspected cervical spine injury. J Bone Joint Surg Am 2002;84:124–32. [DOI] [PubMed] [Google Scholar]
- [32].Aarabi B, Sansur CA, Ibrahimi DM, et al. Intramedullary lesion length on postoperative magnetic resonance imaging is a strong predictor of ASIA impairment scale grade conversion following decompressive surgery in cervical spinal cord injury. Neurosurgery 2017;80:610–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ahmed OZ, Yang S, Farneth RA, et al. Association between prearrival notification time and advanced trauma life support protocol adherence. J Surg Res 2019;242:231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].OʼConnell KJ, Carter EA, Fritzeen JL, et al. Effect of family presence on advanced trauma life support task performance during pediatric trauma team evaluation [published online ahead of print]. Pediatr Emerg Care 2017;DOI 10.1097/PEC.0000000000001164. [DOI] [PubMed] [Google Scholar]
- [35].Ahmed OZ, Webman RB, Sheth PD, et al. Errors in cervical spine immobilization during pediatric trauma evaluation. J Surg Res 2018;228:135–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sperka J, Hanson SJ, Hoffmann RG, et al. The effects of pediatric advanced life support guidelines on pediatric trauma airway management. Pediatr Emerg Care 2016;32:499–503. [DOI] [PubMed] [Google Scholar]
- [37].Borgialli DA, Mahajan P, Hoyle JD, Jr, et al. Pediatric emergency care applied research network (PECARN). Performance of the Pediatric Glasgow Coma Scale Score in the evaluation of children with blunt head trauma. Acad Emerg Med 2016;23:878–84. [DOI] [PubMed] [Google Scholar]
- [38].Faruque AV, Qazi SH, Khan MA, et al. Focused abdominal sonography for trauma (FAST) in blunt paediatric abdominal trauma. J Pak Med Assoc 2013;63:361–4. [PubMed] [Google Scholar]


