Abstract
Botulinum toxin has been used to treat persistent erythema and flushing in rosacea for several years. Here, we describe two women and one man, each with rosacea with flushing and permanent erythema refractory to conventional treatment, who achieved satisfactory and lasting results following intradermal application of botulinum toxin. Two different botulinum toxin types were used. Toxin concentrations of 3.75U per 0.1 mL (abobotulinum) and 1.25U per 0.1 mL (incobotulinum) were used for each patient were used for each patient. The outcomes were measured using polarized photography to evaluate the decrease in vascular involvement. In the three cases presented here, botulinum toxin was effective for controlling erythema and flushing associated with rosacea; we also observed a prolonged duration of these improvements without the rebound effect of topical therapies.
Keywords: Botulinum toxin, erythema, flushing, rosacea
Rosacea is a chronic inflammatory cutaneous disease with vascular symptoms, including flushing and facial erythema, which causes frequent discomfort among patients.1 There are several treatments for the management of rosacea, stratified according to the predominant lesions and their severity.2 However, the response of erythematotelangiectatic rosacea to conventional treatment is currently unsatisfactory. The United States Food and Drug Administration has approved oxymetazoline and brimonidine as vasoconstrictors with an effect on the vascular component of rosacea.2,3 Yet, the benefits of these treatments are limited, since they have a temporary efficacy (duration on average of 8–10 hours) and a rebound effect has been reported in some patients.4–6 The application of intradermal botulinum toxin is an alternative treatment for refractory erythema and flushing. This intervention has demonstrated more prolonged effects without a rebound effect.1
Here, we describe two women and one man, each with rosacea with flushing and permanent erythema refractory to conventional treatment, who achieved satisfactory and lasting results following intradermal application of botulinum toxin. The outcomes were measured using polarized photography to evaluate the decrease in vascular involvement.
CASE PRESENTATIONS
Case 1. A 28-year-old female patient presented with facial erythema and pustules on her cheeks persisting for the previous two years and was diagnosed with rosacea (Figure 1). Previously, she received doxycycline (40mg daily for one month), azelaic acid gel 15% once per day, and ivermectin 1% cream at night for three months, with reduction of the pustules count but persistence of erythema. Intradermal botulinum toxin (Dysport®; IPSEN, Paris, France) was applied in areas of erythema on the cheeks. The toxin was diluted to 25% (four times). A total of 30 units distributed in 40 points (0.75U in 0.02mL per injection point) were injected in the affected area, with a 1-cm interval distance, through a 30-gauge 1-mL syringe. An improvement of 75 percent of flushing and 65 percent of permanent erythema were observed one month after treatment.
FIGURE 1.

A, B) Patient with rosacea and persistent erythema on cheeks; C) Same patient four weeks after treatment with botulinum toxin; D) markings for intradermal injections
Case 2. A 39-year-old woman presented with erythema, telangiectasias, and papules on her forehead, cheeks, and chin, persisting for the past year (Figure 2). She had not previously received any medication. Night treatment with 0.75% metronidazole gel, facial moisturizer, and sunscreen were prescribed. The patient discontinued metronidazole due to a local burning sensation. Four months later, she came in with an increased number of papulopustules, telangiectasias, and erythema on her cheeks and chin. She was prescribed doxycycline (40mg daily for two months), ivermectin 1% topical cream at night, and broad-spectrum sunscreen three times per day. After six months, she came back with resolution of all inflammatory lesions. However, despite topical maintenance therapy and general recommendations, the patient showed persistent erythema on the forehead, cheeks, and chin. She received treatment with oral isotretinoin (20mg three times/week) and two sessions of fractional nonablative laser (1,550nm), with no improvement of flushing and erythema. Topical anesthetic cream was applied for 30 minutes before treatment, followed by a fourfold injection of intradermal botulinum toxin (Xeomin; Merz, Frankfurt, Germany) diluted to 25%, in the cheeks, glabella, and chin. A total of 14 units were applied. Injections were applied at 1-cm intervals, with 0.25U per 0.02mL injected at every point (56 points) through a 30-gauge, 1-mL syringe. One month later, she showed a 70-percent improvement of the flushing and erythema.
FIGURE 2.

A, B) Patient with rosacea and persistent erythema on the forehead, cheeks, and chin; C) Dramatic improvement of the facial erythema one month after botulinum toxin application; D) Markings for intradermal injections
Case 3. A 35-year-old man presented with telangiectasia, papules, pustules, and persistent erythema on the cheeks and chin, present for eight years prior (Figure 3). During the previous three years, he had been treated with daily applications of 0.75% metronidazole gel with significant improvement. No change was observed concerning the persistent erythema after six months of treatment with tacrolimus ointment 0.03% administered three nights per week.
FIGURE 3.
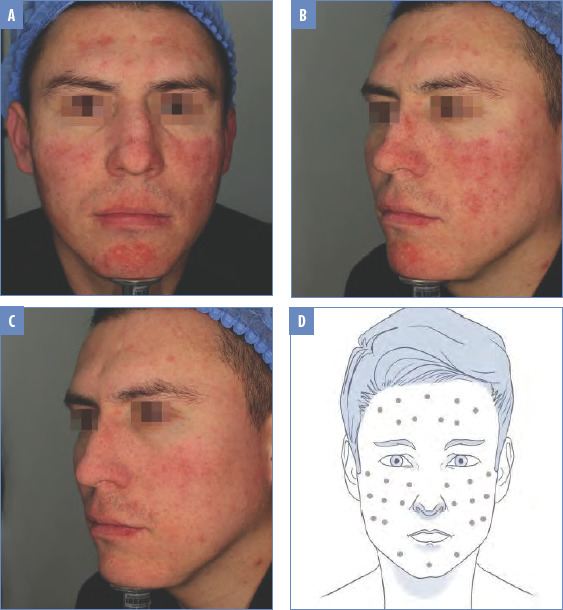
A, B) Male patient with persistent erythema and telangiectasia on the lower cheeks and chin; C) Three weeks after botulinum toxin treatment; D) Markings for intradermal injections
Intradermal botulinum toxin (Dysport®) diluted to 25% was injected in the cheeks and chin. A total of 20 units (0.75U per 0.02mL)were applied at 1-cm intervals at every point (26 points) with a 30-gauge, 1-mL syringe. Three weeks later, a 60-percent reduction in erythema had been achieved.
DISCUSSION
Rosacea is a chronic inflammatory disease whose etiology is not fully understood.7,8 Three pathogenic mechanisms have been postulated; the first is presence of abnormal neurovascular signals, which could be explained by the activation of the vanilloid transient receptor potential and the ankyrin transient receptor potential channel as well as the release of vasoactive peptides that are associated with the vascular changes in rosacea.9,10 The activation of these receptors is triggered by different factors, such as heat, spicy foods, and alcohol.7,8 A second mechanism is dysregulation of the innate immune system, with high abnormal levels of cathelicidin, which has an inflammatory effect through an increased release of metalloproteinases, chemotaxis of leukocytes, and angiogenesis.8 Finally, a microbiome imbalance has been observed in patients with rosacea,7,10,11 with an increased density of demodex mites, which activate the Toll-like receptors and promote an inflammatory response.8,9
The literature reports multiple treatments for rosacea, which act on the etiological pathways previously described. Persistent erythema and flushing are secondary manifestations due to neurovascular alteration and are one of the main and most common symptoms of patients with any grade of rosacea.10 Variable outcomes have been observed with noninvasive therapeutic options, such as intense pulsed light therapy, with topical medications, such as brimonidine, oxymetazoline, azelaic acid, metronidazole, and oral medications, such as clonidine and carvedilol.2,12–14
Intradermal botulinum toxin has been studied to control these neurovascular symptoms.12–15 It blocks acetylcholine release and modulates other neuropeptides, as the expression of vascular endothelial growth factor influences vasodilation and inhibits the release of cathelicidin and inflammatory mediators. In this case, substance P and calcitonin gene-related peptide promote an anti-inflammatory effect that relieves facial flushing.7,12,16,17 There is evidence that botulinum toxin inhibits mast cell degranulation, stimulating an anti-inflammatory effect.7,17
The first successful case of facial flushing managed with botulinum toxin was reported more than a decade ago,18 with subsequent studies supporting its use.19–21 The evaluation of an improvement in erythema is measured using scales, such as the Clinician Erythema Assessment scale and Global Aesthetic Improvement scale. Although not routinely used by clinicians, these are helpful scales to quantitatively assess the effectiveness of intradermal injections.22 Another option is the use of a digital medical photography system supported by software that uses polarized lighting to analyze redness and objectively measure the vascular component, evaluate outcomes, and improve application points and doses for each patient. Different therapeutic botulinum toxin schemes have been used.16,17,23 The neurotoxin is applied intradermally in the hypervascular areas of the face and the suggested dose interval ranges from 15 to 50IU, diluted in saline solution. Meanwhile, the recommended application intervals vary from 0.5 to 1cm. Intradermal injections follow a grid pattern in the glabella and the cheeks. Areas with prominent erythema are covered using 0.05-mL micro-droplets.16,23 The effect is observed within the first 2 to 6 weeks and persists for between four and six months.
CONCLUSIONS
Botulinum toxin is an alternative treatment that should be considered in patients with refractory erythema and flushing associated with rosacea. In the three patients presented here, satisfactory outcomes were attained without side effects. For long-term use, botulinum toxin might be more cost-effective than topical therapy. Measurement of outcomes with validated scales, such as the Clinician Erythema Assessment scale, the erythema index, or polarized photography devices are important tools to objectively assess treatment effectiveness and results during patient follow-up.
REFERENCES
- Park KY, Hyun MY, Jeong SY et al. Botulinum toxin for the treatment of refractory erythema and flushing of rosacea. Dermatology. 2015;230(4):299–301. doi: 10.1159/000368773. [DOI] [PubMed] [Google Scholar]
- Del Rosso JQ, Tanghetti E, Webster G et al. Update on the management of rosacea from the American Acne & Rosacea Society (AARS). J Clin Aesthet Dermatol. 2019;12(6):17–24. [PMC free article] [PubMed] [Google Scholar]
- Cline A, McGregor SP, Feldman SR. Medical management of facial redness in rosacea. Dermatol Clin. 2018;36(2):151–159. doi: 10.1016/j.det.2017.11.010. [DOI] [PubMed] [Google Scholar]
- Hoover RM, Erramouspe J. Role of topical oxymetazoline for management of erythematotelangiectatic rosacea. Ann Pharmacother. 2018;52(3):263–267. doi: 10.1177/1060028017740139. [DOI] [PubMed] [Google Scholar]
- Routt ET, Levitt JO. Rebound erythema and burning sensation from a new topical brimonidine tartrate gel 0.33%. J Am Acad Dermatol. 2014;70(2):e37–e38. doi: 10.1016/j.jaad.2013.10.054. [DOI] [PubMed] [Google Scholar]
- Gillihan R, Nguyen T, Fischer R et al. Erythema in skin adjacent to area of long-term brimonidine treatment for rosacea: a novel adverse reaction. JAMA Dermatol. 2015;151(10):1136–1137. doi: 10.1001/jamadermatol.2015.1252. [DOI] [PubMed] [Google Scholar]
- Choi JE, Werbel T, Wang Z et al. Botulinum toxin blocks mast cells and prevents rosacea like inflammation. J Dermatol Sci. 2019;93(1):58–64. doi: 10.1016/j.jdermsci.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buddenkotte J, Steinhoff M. Recent advances in understanding and managing rosacea. F1000Res. 2018;7:F1000. doi: 10.12688/f1000research.16537.1. Faculty Rev-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addor FA. Skin barrier in rosacea. An Bras Dermatol. 2016;91(1):59–63. doi: 10.1590/abd1806-4841.20163541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn CS, Huang WW. Rosacea pathogenesis. Dermatol Clin. 2018;36(2):81–86. doi: 10.1016/j.det.2017.11.001. [DOI] [PubMed] [Google Scholar]
- Two AM, Wu W, Gallo RL et al. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015;72(5):749–758. doi: 10.1016/j.jaad.2014.08.028. [DOI] [PubMed] [Google Scholar]
- Bloom BS, Payongayong L, Mourin A, Goldberg DJ. Impact of intradermal Abobotulinumtoxin A on facial erythema of rosacea. Dermatol Surg. 2015;41(1):9–16. doi: 10.1097/DSS.0000000000000277. [DOI] [PubMed] [Google Scholar]
- Del Rosso JQ. Topical a-Agonist therapy for persistent facial erythema of rosacea and the addition of oximetazoline to the treatment armamentarium: where are we now?. J Clin Aesthet Dermatol. 2017;10(7):28–32. [PMC free article] [PubMed] [Google Scholar]
- Steinhoff M, Schmelz M, Schauber J. Facial erythema of rosacea - aetiology, different pathophysiologies and treatment options. Acta Derm Venereol. 2016;15;96(5):579–586. doi: 10.2340/00015555-2335. [DOI] [PubMed] [Google Scholar]
- Schlessinger J, Gilbert E, Cohen JL, Kaufman J. New uses of abobotulinumtoxinA in aesthetics. Aesthet Surg J. 2017;37(1):45–58. doi: 10.1093/asj/sjx005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Hong ES, Kim HS. Botulinum toxin in the field of dermatology: novel indications. Toxins. 2017;9(12):403. doi: 10.3390/toxins9120403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharti J, Sonthalia S, Jakhar D. Mesotherapy with botulinum toxin for the treatment of refractory vascular and papulopustular rosacea. J Am Acad Dermatol. 2018. pp. S0190–9622(18)30808-9. [DOI] [PubMed]
- Yuraitis M, Jacob C. Botulinum toxin for the treatment of facial flushing. Dermatol Surg. 2004;30(1):102–104. doi: 10.1111/j.1524-4725.2004.30017.x. [DOI] [PubMed] [Google Scholar]
- Alexandroff AB, Sinclair SA, Langtry JA. Successful use of botulinum toxin a for the treatment of neck and anterior chest wall flushing. Dermatol Surg. 2006;32(12):1536. doi: 10.1111/j.1524-4725.2006.32372.x. [DOI] [PubMed] [Google Scholar]
- Oh YJ, Lee NY, Suh DH et al. A split-face study using botulinum toxin type B to decrease facial erythema index. J Cosmet Laser Ther. 2011;13(5):243–248. doi: 10.3109/14764172.2011.613479. [DOI] [PubMed] [Google Scholar]
- Dayan SH, Pritzker RN, Arkins JP. A new treatment regimen for rosacea: onabotulinumtoxin A. J Drugs Dermatol. 2012;11(12):76–79. [PubMed] [Google Scholar]
- Kim MJ, Kim JH, Cheon HI. Assessment of skin physiology change and safety after intradermal injections with botulinum toxin: a randomized, double-blind, placebo-controlled, split-face pilot study in rosacea patients with facial erythema. Dermatol Surg. 2019;45(9):1155–1162. doi: 10.1097/DSS.0000000000001819. [DOI] [PubMed] [Google Scholar]
- Guida S, Farnetani F, Nisticò SP, Mariarosaria CG. New trends in botulinum toxin use in dermatology. Dermatol Pract Concept. 2018;8(4):277–282. doi: 10.5826/dpc.0804a05. [DOI] [PMC free article] [PubMed] [Google Scholar]


