Abstract
A 59-year-old woman presented to the emergency department with shortness of breath. She had significant oropharyngeal swelling obstructing her upper respiratory tract. A diagnosis of laryngeal myxoedema was made, which was attributed to severe hypothyroidism. She required invasive ventilation and subsequently a tracheostomy. She was treated with levothyroxine and hydrocortisone. She completely recovered with this therapy. In this review, we will discuss similar cases and different therapeutic options. This case also highlights the fact that establishing a diagnosis of laryngeal myxoedema, a condition that can potentially have lethal outcomes and can be challenging.
Keywords: drugs and medicines, endocrine system, ear, nose and throat/otolaryngology, thyroid disease, general practice / family medicine
Background
The prevalence of hypothyroidism in the USA is 4.6%. Hypothyroidism can present with many different symptoms and clinical signs, including lethargy, weight gain, dry skin, constipation and, in severe cases, altered mental status, bradycardia, hypotension and myxoedema coma.1–3 Laryngeal myxoedema is, however, a very rare complication, with a total of 10 reported cases to date. Given the rarity of this presentation, healthcare providers can face a unique diagnostic and management challenge. We present a case of laryngeal myxoedema, where the patient presented with shortness of breath, was correctly diagnosed and had a good clinical outcome.
Case presentation
A 59-year-old woman presented to the emergency department (ED) with shortness of breath. The patient had a medical history significant for hypothyroidism, hypertension, hyperlipidemia, gastro-oesophageal reflux disease, diabetes mellitus, obstructive sleep apnoea and depression. Her surgical history was significant for a tonsillectomy. Family history included asthma and diabetes mellitus in both the parents. She was allergic to clindamycin and penicillin. During her initial evaluation in the ED, the patient had an episode of apnoea and went into cardiac arrest with pulseless electrical activity as the initial cardiac rhythm. She was successfully resuscitated with an advanced cardiac life support protocol and experienced a total downtime of 15 min. Following the placement of an endotracheal tube, and sedation and the initiation of mechanical ventilation, she was transferred to the intensive care unit (ICU). In the ICU, her vitals were stable without vasopressor support. There were no significant abnormalities noted on physical examination. Her family informed the care team that the patient had not been taking her levothyroxine for more than 2 years. Her other home medications included aspirin, lorazepam, omeprazole, metoprolol and hydrochlorothiazide. It was unclear if she was compliant with these medications. Additional investigations were carried out to determine the underlying cause of her shortness of breath and cardiac arrest.
Investigations
Prior to the cardiac arrest, a basic metabolic panel and complete blood count were obtained. Serum sodium was 128 mEq/L, and her white blood cell count was 23×109/L. Lactate was 1.5 mg/dL. Thyroid function tests were done because of the history of non-compliance with recommended thyroid hormone replacement therapy. Thyroid stimulating hormone (TSH) level was 14.3 IU/mL (normal: 0.4–4 IU/mL) and free T4 was <0.25 ng/dL (normal: 0.8–1.8 ng/dL). Further investigations were carried out to evaluate the function of the pituitary gland. Follicle stimulating hormone (FSH) was 9.4 IU/L (normal postmenopausal level: >20 IU/L) and luteinising hormone (LH) was 0.3 IU/L (normal postmenopausal level: >15 IU/L). Plasma adrenocorticotropic hormone (ACTH) level drawn at 08:00 was 5.2 pg/mL (normal: 10–60 pg/mL). Serum prolactin was 15.4 ng/mL (normal: <20 ng/mL). MRI of the brain showed that the size of pituitary gland was much smaller compared with MRI of the brain obtained 12 years prior. CT angiogram (CTA) of the chest was obtained to rule out a pulmonary embolism. It showed parenchymal opacities and enlarged mediastinal lymph nodes without any evidence of pulmonary embolism. A dedicated CT of the neck was also obtained after CTA of the chest suggested soft tissue swelling of the hypopharynx (figure 1). The CT of the neck showed significant soft tissue swelling of the nasopharynx, oropharynx and hypopharynx. A direct laryngoscopy was performed on the fourth day of hospitalisation during which significant oedema of the soft palate, oropharynx and larynx was noted. Biopsies of the left vocal cord, the right arytenoid and the epiglottis were obtained. Subsequent pathological examination of the tissue obtained reported only submucosal oedema (figures 2–4).
Figure 1.
CT scan of the neck showed soft tissue swelling of nasopharynx, oropharynx, hypopharynx (within the circle).
Figure 2.
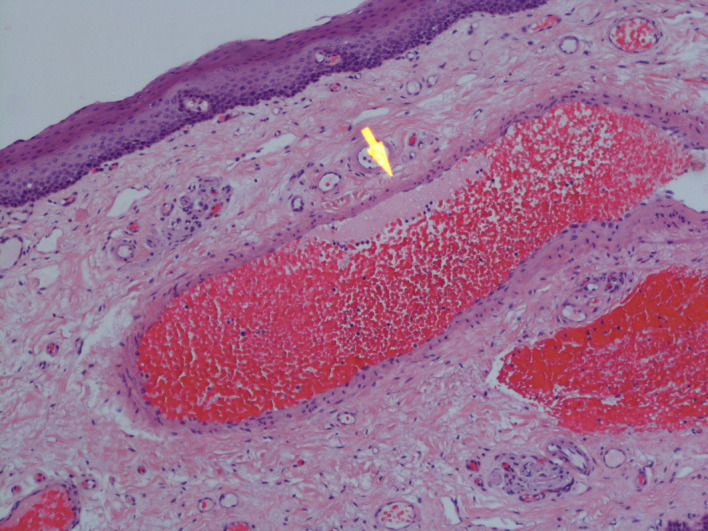
Vocal cord biopsy (arrow) showing venous congestion.
Figure 3.
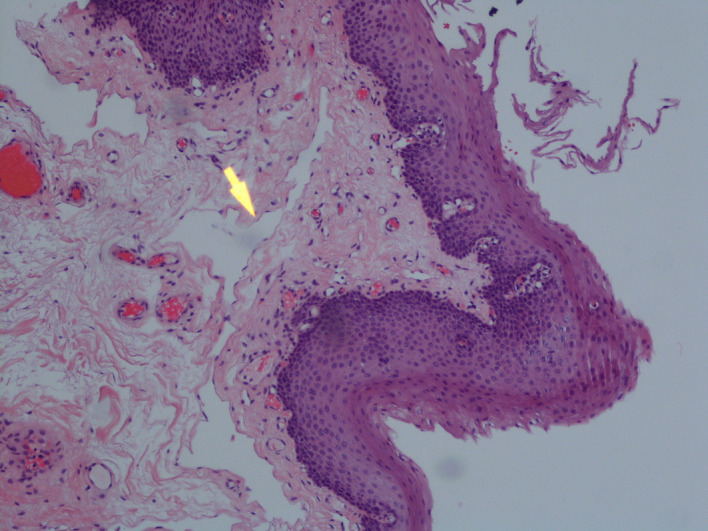
Vocal cord biopsy (arrow) showing dilated lymphatic channels.
Figure 4.
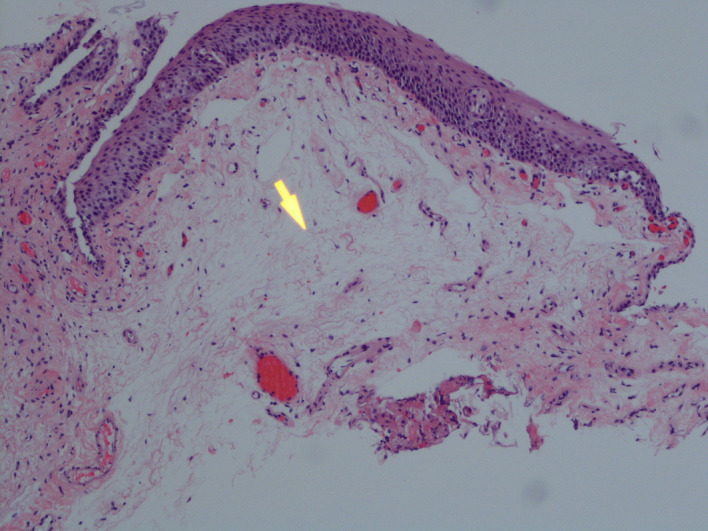
Vocal cord biopsy (arrow) showing interstitial oedema.
Differential diagnosis
Based on the patient’s presentation, the differential diagnosis included pulmonary embolism, respiratory infection with severe sepsis and an allergic reaction to an unidentified allergen. The soft tissue swelling was thought to be related to trauma associated with endotracheal intubation and initially laryngeal myxoedema was not considered. There was no evidence of generalised myxoedema and at this stage of the patient’s care, we were not aware of any changes in her voice preceding the admission. Laryngeal myxoedema only became a consideration when the patient’s upper airway oedema did not subside despite treatment with both steroids and antihistamines.
Treatment
After ruling out pulmonary embolism by CTA of the chest, an infectious aetiology was presumed. Vancomycin and piperacillin/tazobactam were given. Given the severity of the upper airway oedema, she was also started on hydrocortisone 50 mg by mouth three times a day. During her stay in the ICU, it was difficult to mechanically ventilate the patient due to excessive airway secretions. A decision was made to insert an extra-long cuffed Shiley tracheostomy tube on the fourth day of admission. Because of her respiratory status, treatment with oral levothyroxine starting with an initial dose of 175 µg/day was initiated.
Outcome and follow-up
Antibiotics were discontinued after 7 days. The patient was transferred to long-term acute care following 10 days of hospitalisation. She was gradually weaned off the ventilator on day 30. The tracheostomy tube was removed on day 34. She was subsequently discharged home after 54 days. The patient subsequently reported by phone that her tracheostomy wound had healed and that she was doing well.
Discussion
Hypothyroidism affects the respiratory system in several different ways. It can cause alveolar hypoventilation and depress both hypoxic and hypercapnic ventilatory drive.4 5 Additionally, it can cause respiratory muscle weakness, a decrease in both forced vital capacity and forced expiratory flow, and also a decrease in carbon monoxide diffusion capacity.6 7 An increased incidence of obstructive sleep apnoea has also been reported.8 Hypothyroidism, depending on the underlying cause can lead to physical obstruction of the airway due to macroglossia and thyromegaly. Thyroid hormone receptors have been identified within the fibrous connective tissue of the lamina propria, the cartilage, and the glandular elements of the human larynx. Although the exact mechanism is not known, hypothyroidism is thought to be due to increased mucin deposition in the subepithelial space.9 10
Following a PubMed and Google Scholar review, we found only four case reports with a total of five patients where laryngeal swelling was presumed to be secondary to laryngeal myxoedema associated with hypothyroidism (table 1).
Table 1.
Summary of the reported cases including our patient
| Reference | Age | Sex | Thyroid function tests | Intubation | Tracheostomy | Decannulation | Levothyroxine (ROA) |
Steroids | Follow-up laryngoscopy |
| Salgado et al 13 | 63 | M | TSH: 53.28 mIU/L (normal, 0.47–4.68 mIU/L) FT4: 0.3 ng/dL (normal, 0.78–2.19 ng/dL) |
Yes | Yes | Not done at discharge | Intravenous | Hydrocortisone | Not done |
| Salgado et al 13 | 70 | M | TSH: 70.6 µIU/mL (normal, 0.35–4.94 µIU/mL) FT4 <0.1 ng/dL (normal, 0.70–1.48 ng/dL) |
Yes | Yes | 6 days | Intravenous + intravenous liothyronine |
Dexamethasone | Oedema resolved by 2 weeks |
| Batniji et al 12 | 69 | M | TSH: elevated FT4: 0.4 ng/dL (normal, 0.7–1.48 ng/dL) |
Yes | Yes | 3 weeks | Intravenous | Not given | Oedema resolved by week 2 |
| Erwin | 48 | M | TSH: 42.4 mIU/L (0–8 mIU/L) T4: 20 mmol/L (normal, 55–140 mmol/L) |
Yes | Yes | 3 weeks | PO | Not given | Persistent oedema after 2 weeks. |
| Uzunpinar | 59 | F | Not available | Yes | Yes | Not available | PO | Hydrocortisone | Oedema resolved by week 4 |
| Case | 59 | F | TSH: 14.3 IU/L (normal, 0.4–4) FT4 <0.25 ng/dL (normal, 0.8–1.8 ng/dL) |
Yes | Yes | 34 days | PO | Hydrocortisone | Not done |
F, female; FT4, free thryoxine; M, male; PO, per oral; ROA, route of administration; T4, total thryoxine; TSH, thyroid stimulating hormone.
Our patient presented with symptoms of shortness of breath. This was a common finding in other reported cases as well.10–13 In one case, the presenting problem was generalised weakness and myalgia.14 Though they were not observed in this case, stridor, myxoedema and macroglossia were common findings in other reported cases.11–14 It is important to note that patients without a prior diagnosis of hypothyroidism can also present with laryngeal myxoedema as noted in cases reported by Erwin and Uzunpinar.11 14
Free T4 level in our patient was comparable to other cases discussed in this review; however, TSH level in our patient was much lower. Hadlow et al evaluated the relationship between TSH and free T4 and found that this is not inverse log-linear, but can be described by two overlapping negative sigmoid curves. At physiological free T4 concentration, TSH is higher in men and elderly; however, TSH response to hypothyroidism was found to be more robust in younger population.15 We did carry out further investigations to evaluate for hypopituitarism. Low FSH and LH levels along with decreased size of pituitary gland on MRI of the brain are suggestive of hypopituitarism; however, the information was insufficient to establish a definitive diagnosis. A low ACTH level can be attributed to hydrocortisone use and serum prolactin level was also normal. Additionally, there were no clinical or lab abnormalities that would indicate an abnormal antidiuretic hormone production.
Of the reported cases, ours is the only case in which tissue biopsies were obtained. Though submucosal oedema was noted, there was not an opportunity to identify mucopolysaccharides because special stains that can identify these (eg, Alcian blue) were not used. The identification of mucopolysaccharides can help healthcare providers make the correct diagnosis and lead to the timely treatment.
All patients, included in prior case reports, required endotracheal intubation and subsequent tracheostomy. The reasons for performing a tracheostomy included self-extubation,11 prolonged intubation,12 13 postextubation stridor,14 and in our patient the inability to ventilate through an endotracheal tube. Other authors do not comment on challenges associated with mechanically ventilating patients with an endotracheal tube. The time before performing a tracheostomy in intubated patients varied from 1 to 3 weeks as shown in the table 1.
Intubation and tracheostomy are merely supportive measures and prompt thyroid hormone replacement is the key to successful treatment of the underlying pathology. Levothyroxine is available in both intravenous and per oral (PO) formulations. Intravenous levothyroxine replacement is recommended due to the possibility of bowel oedema with severe hypothyroidism and an associated impact on the absorption of PO medications.16–19 Among the cases reported intravenous levothyroxine was used in three patients12 13 and PO levothyroxine was used in two other patients.11 14 Given the fact that our patient had a cardiac arrest on admission, we opted for oral levothyroxine due to its better safety profile. Regardless of the route of administration of levothyroxine, all patients had successful outcomes in terms of mortality and discontinuation of mechanical ventilation. Review of the reported cases shows that patients treated with intravenous levothyroxine had mechanical ventilation discontinued sooner than those who received oral treatment. Due to worsening laryngeal oedema, one patient required intravenous liothyronine. For this patient, mechanical ventilation was discontinued after 6 days.13 However, due to unpredictable pharmacodynamics, intravenous liothyronine is used for severe cases of hypothyroidism, including myxoedema coma.1 3 Our case and all of the previously reported cases had mechanical ventilation discontinued within 4 weeks of initiating treatment with levothyroxine.
Steroids are often used to treat laryngeal swelling secondary to allergic reaction, upper airway surgery, periextubation and infection. Dexamethasone, methylprednisolone and nebulised budesonide are all commonly used to prevent postextubation laryngeal oedema.16–18 Because the underlying mechanism is unknown, the role of steroids in the treatment of laryngeal myxoedema remains unclear. Though we decided to continue therapy with hydrocortisone because it appeared to help in some reported cases while other patients were successfully treated without the use of steroids.11–14
Though nebulised epinephrine is often used to treat upper airway oedema by decreasing laryngeal oedema through vasoconstriction, it was not used in any of the reported cases.19–21
Patient’s perspective.
I felt that I was going to die. Thank you to these awesome intensive care unit doctors who saved my life.
Learning points.
Establishing a diagnosis of laryngeal myxoedema can be challenging. History or laboratory tests that are suggestive of hypothyroidism along with upper airway oedema noted on radiological imaging or direct visualisation should raise the suspicion of this uncommon condition.
An important point to consider is that a patient can present with this complication without an established diagnosis of hypothyroidism.
Based on the review of limited literature, patients who received intravenous levothyroxine were liberated from the ventilator quicker and may be a preferred treatment modality.
Practitioners who are caring for a patient with laryngeal oedema should consider laryngeal myxoedema, especially if the patient has a history of hypothyroidism and is not responding to the usual treatments used to manage laryngeal oedema.
Footnotes
Contributors: The case report was written by both Dr FIR and Dr MHI. Editions were made by Dr FIR, Dr MHI, Dr PC and Dr AYD.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer-reviewed.
References
- 1. Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American association of clinical endocrinologists and the American thyroid association. Thyroid 2012;22:1200–35. 10.1089/thy.2012.0205 [DOI] [PubMed] [Google Scholar]
- 2. Norman AW, Litwack G. Hormones. Academic Press, 1997: 169–91. [Google Scholar]
- 3. Klubo-Gwiezdzinska J, Wartofsky L. Thyroid emergencies. Med Clin North Am 2012;96:385–403. 10.1016/j.mcna.2012.01.015 [DOI] [PubMed] [Google Scholar]
- 4. Wilson WR, Bedell GN. The pulmonary abnormalities in myxedema. J Clin Invest 1960;39:42–55. 10.1172/JCI104025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zwillich CW, Pierson DJ, Hofeldt FD, et al. Ventilatory control in myxedema and hypothyroidism. N Engl J Med 1975;292:662–5. 10.1056/NEJM197503272921302 [DOI] [PubMed] [Google Scholar]
- 6. Khaleeli AA, Griffith DG, Edwards RH. The clinical presentation of hypothyroid myopathy and its relationship to abnormalities in structure and function of skeletal muscle. Clin Endocrinol 1983;19:365–76. 10.1111/j.1365-2265.1983.tb00010.x [DOI] [PubMed] [Google Scholar]
- 7. Sadek SH, Khalifa WA, Azoz AM. Pulmonary consequences of hypothyroidism. Ann Thorac Med 2017;12:204. 10.4103/atm.ATM_364_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rajagopal KR, Abbrecht PH, Derderian SS, et al. Obstructive sleep apnea in hypothyroidism. Ann Intern Med 1984;101:491–4. 10.7326/0003-4819-101-4-491 [DOI] [PubMed] [Google Scholar]
- 9. Altman KW, Haines GK, Vakkalanka SK, et al. Identification of thyroid hormone receptors in the human larynx. Laryngoscope 2003;113:1931–4. 10.1097/00005537-200311000-00014 [DOI] [PubMed] [Google Scholar]
- 10. Bicknell PG. Mild hypothyroidism and its effects on the larynx. J Laryngol Otol 1973;87:123–7. 10.1017/S0022215100076696 [DOI] [PubMed] [Google Scholar]
- 11. Erwin L. Myxoedema presenting with severe laryngeal obstruction. Postgrad Med J 1982;58:169–70. 10.1136/pgmj.58.677.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Batniji RK, Butehorn HF, Cevera JJ, et al. Supraglottic myxedema presenting as acute upper airway obstruction. Otolaryngol Head Neck Surg 2006;134:348–50. 10.1016/j.otohns.2005.03.069 [DOI] [PubMed] [Google Scholar]
- 13. Salgado Nunez Del Prado SR, Steinman RA, Munir KM, et al. Supraglottic myxedema: two cases and a review of the literature. AACE Clinical Case Reports 2017;3:e101–5. 10.4158/EP161378.CR [DOI] [Google Scholar]
- 14. Uzunpinar A. Upper airway obstruction in a patient with severe hypothyroidism presenting as postextubation stridor. Chest 2006;130:315S. 10.1378/chest.130.4_MeetingAbstracts.315S-a [DOI] [Google Scholar]
- 15. Hadlow NC, Rothacker KM, Wardrop R, et al. The relationship between TSH and free T₄ in a large population is complex and nonlinear and differs by age and sex. J Clin Endocrinol Metab 2013;98:2936–43. 10.1210/jc.2012-4223 [DOI] [PubMed] [Google Scholar]
- 16. François B, Bellissant E, Gissot V, et al. 12-h pretreatment with methylprednisolone versus placebo for prevention of postextubation laryngeal oedema: a randomised double-blind trial. Lancet 2007;369:1083–9. 10.1016/S0140-6736(07)60526-1 [DOI] [PubMed] [Google Scholar]
- 17. Darmon JY, Rauss A, Dreyfuss D, et al. Evaluation of risk factors for laryngeal edema after tracheal extubation in adults and its prevention by dexamethasone. A placebo-controlled, double-blind, multicenter study. Anesthesiology 1992;77:245–51. 10.1097/00000542-199208000-00004 [DOI] [PubMed] [Google Scholar]
- 18. Abbasi S, Moradi S, Talakoub R, et al. Effect of nebulized budesonide in preventing postextubation complications in critically patients: a prospective, randomized, double-blind, placebo-controlled study. Adv Biomed Res 2014;3:182. 10.4103/2277-9175.139543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mehta AB, Cooke CR, Wiener RS, et al. Hospital variation in early tracheostomy in the United States: a population-based study. Crit Care Med 2016;44:1506. 10.1097/CCM.0000000000001674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. MacDonnell SP, Timmins AC, Watson JD. Adrenaline administered via a nebulizer in adult patients with upper airway obstruction. Anaesthesia 1995;50:35–6. 10.1111/j.1365-2044.1995.tb04510.x [DOI] [PubMed] [Google Scholar]
- 21. Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American thyroid association Task force on thyroid hormone replacement. Thyroid 2014;24:1670–751. 10.1089/thy.2014.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]



