Abstract
Objectives.
The aim of this study was to explore social engagement and social comparisons as mechanisms to increase physical activity among older adults.
Methods.
Participants (N=60, mean age=65.7) were randomly assigned to one of two conditions. Participants in the treatment condition used the application to track their daily walking steps and interact via text messages with their group members for 4 weeks. Participants in the control group used the application only to track their own walking steps. Outcome variables included mean weekly steps, exercise self-efficacy, and social engagement.
Results.
The results revealed that participants in the experimental condition significantly increased their mean weekly steps and social engagement from the pretest to the posttest whereas the control group did not. These effects were maintained at the one-month follow up.
Discussion.
The study expands our understanding of the motivational role of social engagement and social comparison in increasing physical activity among older adults.
Keywords: Physical Activity, Social Engagement, Walking, Older adults
There is compelling evidence that an active lifestyle has broad benefits for cognitive, physical, and psychological health among older adults (Cockerham, Wolfe, & Bauldry, 2020; Matz-Costa et al., 2016). Physical activity can delay or prevent many chronic diseases, including heart disease, type 2 diabetes, dementia, and some cancers (Booth et al., 2012). Active older adults have a reduced risk of moderate or severe physical limitations, are less likely to suffer from falls and fracturing bones, and are more likely to remain mobile and independent (Kohl et al., 2012; McPhee et al., 2016). Being physically and socially active can also improve mental health and delay dementia and cognitive decline (Holt-Lunstad et al., 2015; Liu & Lachman, 2019). According to the 2016 report from Centers for Disease Control and Prevention (CDC), non-institutionalized adults ages 50 years and older account for $860 billion in health care costs each year, despite the fact that 4 in 5 of the most costly chronic conditions for this age group can be prevented or managed with physical activity (National Center for Health Statistics, 2017).
CDC researchers examined patterns of inactivity using data from the 2014 Behavioral Risk Factor Surveillance System for all 50 states and the District of Columbia (D.C.) and found 31 million Americans (28 percent) age 50 years and older were inactive, defined as no physical activity outside of work during the past month (Watsonet al., 2016). Trends in physical activity consistently show that activity levels progressively decrease with age with the prevalence of inactivity being highest among adults aged 65 or greater. Current estimates indicate that 66% of adults over 75 do not engage in any regular physical activity. Moreover, evidence suggests that 50% of sedentary adults have no plan of starting an exercise program (Watson et al., 2016).
In recent years, a number of researchers have conducted studies to evaluate the potential of using pedometers as health interventions (see Foster et al., 2010; Sullivan & Lachman, 2017). Foster and colleagues (2010) used pedometers and a specifically made app, StepMatron, on Facebook to compare the effects of social and non-social motivation on physical activity within a friend group in the same work place. The ten participants in the social group could see their step counts compared to their friends in a competitive format. The social group could also communicate with each other through the page. The nonsocial group could only see their own step counts and had no communication through the app with other participants. There was a significantly higher number of steps in the social group compared to the non-social group. The conversations of the participants in the social group indicated that the competitive social aspect among the friends influenced the number of steps. In a review of the evidence for increasing physical activity among sedentary adults using fitness technology, Sullivan and Lachman (2017) indicated that fitness technology, including trackers and smartphone applications, have become increasingly popular for measuring and encouraging physical activity. Overall, fitness technology has the potential to significantly impact public health, research, and policies. Behavior change techniques such as goal setting, feedback, rewards, and social factors are often included in fitness technology; however, it is not clear which components are most effective. Sullivan and Lachman (2017) discussed additional cognitive behavioral strategies not typically included in fitness technology devices or apps, such as action planning, restructuring negative attitudes, enhancing environmental conditions, and identifying other barriers to regular physical activity, that were promising for engaging inactive populations. Our study adds to the discussion and considers social engagement as a possible mechanism for increasing physical activity among older adults using fitness technology.
The use of fitness technology services could have beneficial effects on chronic disease management in late life, including positive changes in health perception, social functioning, and mental health (Lindeman et al., 2020). Fitness technology is regarded as a vital means for maintaining and enhancing older people’s quality of life (Khosravi et al., 2016; Mitzner et al., 2018). In addition, previous research also indicated that information communication technologies could provide a link between older adults and their informal and formal networks. Technologies allow older adults to transcend spatial barriers and provide them a greater sense of connection to other people (Clarke et al., 2009; Schlomann et al., 2020). Exploring the role of social factors in increasing physical activity using technology is a promising direction (Zhang et al., 2016).
Social Engagement
Social engagement is an effective strategy for encouraging behavior change (Berkman et al., 2000). When people with similar interests interact to achieve a shared goal, social engagement can reduce the perceived costs of adopting a new exercise routine by providing companionship in the activity (Cavallo et al., 2014). In order to identify what features of online social networks can increase physical activity, Zhang and colleagues (2016) conducted a 4-arm randomized controlled trial. University students (n = 790, mean age = 25.2) were randomly assigned to one of four conditions composed of either supportive or competitive relationships and either with individual or team incentives for attending exercise classes. Their findings indicated that attendance numbers were 90% higher in the social comparison and the combined conditions in contrast to the two conditions without comparisons. Social comparison was more effective for increasing physical activity than social support and its effects did not depend on individual or team incentives. Further, social engagement reduces the uncertainty of exploring new exercises by providing access to relevant sources of peer information (Zhang et al., 2016).
Today, individuals rely more and more on computer-mediated communications to access information, meet people, and make decisions that affect their lives (Wang et al., 2017). Virtual groups, social groups or groups with a common interest that interact in an organized fashion on the Internet, may serve as potential resources for community-engaged health promotion. Schlomann and colleagues (2020) examined technology adoption among the oldest-old cohorts (80+) in private homes and long-term care facilities and analyzed relationships between individual characteristics, the living environment, and different kinds of assistive technologies (AT) and information and communication technologies (ICT). They found that AT and ICT device adoption was related to the living environment and individual characteristics, including functional health, chronological age, education, and technology interest. However, there have been mixed findings through social network sites such as AT and ICT on the relationship between social engagement and subjective well-being. Some studies have demonstrated that social engagement through social network sites can be positively related to peoples’ subjective well-being (e.g., (Appel et al., 2015; Wang et al., 2017); whereas others have reported that social comparison can be associated with depressive symptoms and anxiety (Nehrkorn-Bailey et al., 2019; Shaw et al., 2015). These negative effects may be the result of making upward social comparisons (Wang et al., 2017). The present study extended previous studies by examining whether social engagement through ICT is an effective mechanism for promoting increases in physical activity and well-being (Schlomann et al., 2020).
Self-efficacy
Besides social engagement, self-efficacy also plays an important role in increasing physical activity. Self-efficacy is associated with adaptation and regulates human functioning through cognitive, motivational, affective, and selection processes (Bandura, 1990; Lachman et al., 2011). Negative stereotypes about aging and experiences of loss and decline are associated with lowered expectancies for self-efficacy (Bandura, 1997; Lachman et al., 2018). Nehrkorn-Bailey and colleagues (2019) presented findings from an ongoing randomized controlled trial targeting adults’ negative views of aging (NVOA) and low control beliefs to increase their motivation to become physically active. Findings showed changes in NVOA and control beliefs from pretest to immediate posttest were related to changes in physical activity. Previous studies have shown that self-efficacy can be modified in the context of walking interventions (Brothers, & Diehl, 2017; McAuley et al., 2011; Robinson et al., 2018). Our study explored whether a group-based walking intervention could lead to increases in exercise self-efficacy and physical activity.
Theoretical Framework and Mechanisms of Behavior Change for Healthy Aging
The current study was guided by social cognitive theory (SCT), which offers principles on how to predict and change health behavior. SCT considers the unique ways in which individuals acquire and maintain behavior, while also considering the social environment in which individuals perform the behavior (Bandura, 2004). Complex behavior change interventions are often prematurely studied in efficacy and effectiveness trials (Craig et al., 2008; Czajkowski et al., 2015). Both the Medical Research Council (Campbell et al., 2000; Craig et al., 2008) and the National Institutes of Health (Aklin et al., 2020) suggest that behavioral interventions should be designed using a phased approach, similar to the process of drug development. In 2015, the NIH launched the Science of Behavior Change (SOBC) program which aims to address the widespread issue of poor health behaviors (e.g., inactivity, poor diet) by supporting early-phase research to investigate how and why behavioral interventions work (Aklin et al., 2020). SOBC seeks to identify behavior-change targets (i.e., mechanisms or factors associated with the development or maintenance of the behavior of interest) that may be common to multiple clinical conditions (Aklin et al., 2020). An experimental medicine approach involves four steps: 1) identifying an intervention target (i.e., a factor hypothesized to be involved in health behavior); 2) developing valid and reliable assays (i.e., measures) of the target; 3) engaging the target through experimental manipulations or interventions; and 4) testing the degree to which the target is engaged and determining the degree to which this engagement produces the desired behavior change (Aklin et al., 2020).
Attention to active ingredients underlying behavioral interventions may help optimize efficacy and prevent premature abandonment of interventions that fail to impact behavioral and/or biomedical endpoints (Barlow et al, 2013; Czajkowski et al., 2015; Notthoff & Carstensen, 2014). These initiatives advocate for pre-efficacy research to define behavior change interventions through basic science, characterize putative targets through which the intervention will lead to improved outcomes, and assess feasibility and acceptability (Aklin et al., 2020; Rouleau, 2017). In the present study we examined social engagement and social comparisons as mechanisms for changing physical activity behavior.
Current Study
This paper reports on the use of WeChat to improve physical and social activity among community dwelling older adults. WeChat is a free mobile text and voice messaging communication service. This pilot study explored the efficacy of one function of the app WeChat: a group-based pedometer function WeRun. There are previous empirical studies conducted on WeRun with younger adults; for example, Gui and colleagues (2017) conducted a qualitative study of 32 users of WeRun. Their findings indicated that sharing fitness data with pre-existing social networks motivated users to continue self-tracking their steps and enhanced their existing social relationships. However, we are not aware of any empirical studies conducted using WeRun with older adults.
The hypotheses of this study are: a) the participants in the treatment group would show greater increases and higher maintenance of daily steps as well as greater increases in level of social engagement and exercise self-efficacy in comparison to the participants in the control group who were not given the treatment; and b) social engagement would be a significant mediator, that is a mechanism of behavior change.
Methods
Participants
Eligibility.
Inclusion criteria specified that participants must be 60 or older and fit enough to walk for at least 20 minutes at a time. They also needed to have a smartphone, with either an Android or iPhone system with Internet access. A power analysis (using G*Power 3.1) for the study and analysis design indicated that a total of 56 participants (randomly assigned across two groups) would provide adequate power (> 80%) to detect medium-sized effects (ρ = 0.3) at p < .05. We recruited 60 participants in the northeast U.S. by posting recruiting posters in community public posting boards, including public libraries, grocery stores and shopping malls. Participants were given two 25-dollar gift cards (one at the pretest and one after the 4-week intervention) as compensation for their participation.
Sample.
As shown in the consort diagram in Figure S1, of the 241 adults who filled out our eligibility questionnaire online, 38 were not eligible, 15 gave up as they had trouble downloading the app, 4 did not meet the age requirement, 4 indicating participating in a walking intervention would be a potential health risk, and 3 could not participate due to travel. One hundred and forty-three potential participants who were eligible did not respond when we notified them that they were eligible. Recruitment took place from October 2018 to March 2019, with primary data collection completed in February 2019, and follow-up data collection completed in March 2019. Those who were physically active (i.e., who had 7,000 – 10,000 daily steps or above everyday) were not included after the one-week baseline. A total of 60 adults were recruited and randomly assigned to either the control condition (n = 30) or the treatment condition (n = 30). They completed the study in one of three subgroups, with 20 participants randomly assigned into two groups (10 in treatment group, and 10 in control group) for each subgroup.
Measures
Covariates.
Age, gender, education, race, and self-reported health were used as covariates in the analyses because of their expected relationship with the outcome measures. For physical health, the participants were asked “in general would you say your health is?” The response options ranged from 1 (poor) to 5 (excellent) with a higher score indicating better physical health.
The outcome measures were administered at the pretest, posttest and follow up using self-report questionnaires given before and at the completion of week 4 of the pilot study and at the 1 month follow up through an online platforms-Qualtrics.
Daily step counts.
Participants’ daily steps were recorded by using the WeRun function in WeChat by the end of each day during the 4-week intervention period and at the 1 month follow up. Mean daily steps for pretest week, post-test week and one month follow up week were calculated as the mean number of steps across the 7 days in that week of the study.
Percentage change in mean weekly steps at posttest was calculated as the difference between the mean weekly steps at posttest and pretest divided by the mean weekly steps at pretest. The percentage change in mean weekly steps at the one month follow up was calculated as the difference between the mean weekly steps at one month follow up and pretest divided by the mean weekly steps at pretest.
Social engagement.
We had two measures of social engagement. The 18-item version of the Lubben Social Network Scale (LSNS), was used to examine social contact and support as indicators of social engagement at the pretest and posttests (Lubben & Gironda, 2004). For the treatment group only, the number of participants’ daily text messages exchanged in the group discussion was used to measure social interaction. This version utilizes two subscales for friends and family and has the highest level of internal consistency (α= .82) of the three available versions of the LSNS (Lubben & Gironda, 2004). The scale weighs size, closeness and frequency of social contacts. The sum of the 12 equally weighed items is computed with scores ranging from 0 to 60. Lower scores indicate smaller networks, or lower levels of perceived social support. Items include ‘How many relatives (friends) do you see or hear from at least once a month?’, ‘How many relatives (friends) do you feel you can talk to about private matters?’, and ‘How many relatives (friends) do you feel close to such that you could call on them for help?’
Exercise self-efficacy.
Based on Bandura’s model (Bandura, 1990; Lachman et al., 2011; Resnick & Jenkins, 2000), exercise self-efficacy was measured using the Self-Efficacy for Exercise (SEE) Scale, which was a 9-item instrument that focuses on self-efficacy expectations related to the ability to continue exercising in the face of barriers to exercise. There was sufficient evidence of internal consistency (α = 0.92), and a squared multiple correlation coefficient using structural equation modeling provided further evidence of reliability (R2 ranged from 0.38 to 0.76). The sum of the nine items is computed with scores ranging from 0 to 90. Lower scores indicate lower levels of exercise self-efficacy. Items include ‘the weather was bothering you’, “you were bored by the program or activity” and “you have to exercise alone”.
Procedures and Research Design
The study was approved by the University’s Institutional Review Board. The clinical trial was registered at the US National Institutes of Health (ClinicalTrials.gov) # NCT03803085. After they were deemed eligible to participate in the study, participants were randomly assigned to one of two conditions: treatment or control. During the 4-week study, participants were blinded to condition. Data collection was also blinded to the experimenters, as the survey and physical activity data were collected through online platforms (Qualtrics and WeRun, respectively).
All participants completed a survey with demographic questions and the self-report outcome measures at pretest. They were asked to use WeRun to track their own daily steps for one week, prior to being assigned to groups. This provided pretest physical activity data and helped participants become familiar with WeChat and syncing the data with their phone. After 4 weeks of using the application, all participants completed the same self-report measures to assess changes in the outcomes of interest. They also completed a follow-up assessment 1 month after the post-test for the same measures.
During the intervention, participants’ daily walking steps were recorded by WeRun, and the data were logged by the research assistant every day. The research assistant also recorded each participants’ daily ranking and number of social interactions in the treatment condition. Messages were sent by email and WeChat messages to the participants to remind them to carry their phone with them as often as possible during the day and use the application every day. The trained research assistant explained how to use WeChat, WeRun to all participants.
Participants in both conditions were asked to use the application every day. A message was sent to remind them to use the application if they had not done so for three consecutive days. Participants in both conditions used WeChat for 4 weeks, during which time the steps data were recorded by the WeRun function and downloaded by the research assistants.
Treatment condition:
The participants in the treatment condition could interact with the other group members by sending text messages which were documented by the research assistants. The researchers sent out instructions to check step counts on Monday mornings during the 4-week intervention, for example “Dear all, this is Week 1! please remember to take your phone with you as often as possible during the day and check your step count in WeRun by the end of the day. Please also share your number of steps with your group members. Thank you!” The daily walking steps of the participants in this group were displayed to the group and the participant with the highest daily steps in the group was indicated as the champion each day.
Control condition:
Participants only saw their own daily walking steps using WeRun. They did not see other group members’ daily steps and did not interact or compare walking steps with other group members. The participants received messages on Monday mornings during the 4-week intervention to remind them to take their phones as often as possible during the day.
Data Analysis
Statistical analyses of survey measures were done using SPSS. Descriptive information and correlations were computed for all study variables. Changes in daily steps, social engagement and exercise self-efficacy from the pretest to 4 weeks were examined. Repeated measures ANCOVA was used to test for effects of the treatment on mean daily step counts over the intervention period, exercise self-efficacy, and social engagement and to compare treatment and control groups at pretest, posttest, and follow-up using a two condition by three occasions design. All post hoc analyses were performed using Bonferroni corrections controlling the covariates. We conducted a sensitivity analysis without the covariates and the results were the same.
Conditional process modeling was applied using PROCESS in SPSS to test the predicted mediation model. Mediation analyses was based on 1000 bootstrapped samples using Hayes’ PROCESS Macro v3.3 (Hayes & Preacher, 2014), allowing for formal tests of the total, direct, and indirect effects of intervention on percentage of change of mean weekly steps from pre-test to post test. The predictor variable was condition, the mediator variable was change in social engagement, and the outcome was percent change in mean weekly steps from pre-test to post test.
Results
Descriptive Statistics
As shown in Table 1, the mean age of participants was 65.4 years old, with a standard deviation of 5.31. Seventy-five percent of the participants were female, about half of the participants were married and three quarters of the participants identified their race as white. The mean education of participants was 5 (SD=1.633) out of an 8-point scale from “Less than High School” to “Professional Degree”; a score of 5 corresponds to “4-year College Degree. Four dropped out before the end of the study, resulting in a total of 56 participants (control condition, n = 28; treatment condition, n = 28; see additional demographic information in Table S1). Randomization was checked by comparing the two conditions and the three recruitment subgroups with a series of independent t-tests and Chi square tests. Participants in the two conditions did not differ by age, education, gender, race or self-reported health. Participants in the three recruitment subgroups also did not differ by age, education, race, gender or self-reported health. At the pretest, there also were no differences in initial steps, and the other outcomes including level of social engagement and exercise self-efficacy. See Table 1 for more details, including the means and standard deviations for study variables at pre, post-test, and follow-up and Figure S1 for more details on enrollment and retention.
Table 1.
Pretest, Posttest and Follow-up Measures by Condition (n = 56)
| Variables | Treatment Group | Control Group | ||||
|---|---|---|---|---|---|---|
| N | 28 | 28 | ||||
| Pre Post and Follow-up measures | Pre M(SD) | Post M(SD) | Follow up M(SD) | Pre M(SD) | Post M(SD) | Follow up M(SD) |
| Mean weekly steps (range 1054–9,269) | 4,125 (2,693) | 5,872 (3,494) | 5,911 (3,467) | 3,992 (2,388) | 4,171 (3,122) | 4,330 (3,185) |
| % change in mean weekly steps | - | 35.0(39.2) | 36.9(47.7) | - | −3.8(27.4) | −0.05(31.3) |
| Social engagement (range 12–72) | 35.9(11.3) | 45.7(11.5) | 44.1(10.8) | 35.1 (11.5) | 37.1(8.3) | 37.7(8.9) |
| Exercise self-efficacy (range 10–100) | 60.3(22.3) | 67.0(21.6) | 60.3(22.5) | 57.71(22.8) | 55.8(21.8) | 53.2(21.4) |
Note. M: mean; SD: standard deviation.
Effects of Intervention
Mean weekly walking steps.
The results of the repeated measures ANCOVA indicated that there was a significant interaction effect of time and treatment on mean weekly walking steps. Bonferroni corrections were used to make post hoc comparisons for the two condition by three occasion interactions. In line with predictions, the interaction between time and condition was significant for mean weekly steps, F (2, 56), = 4.29, p<0.05. Post hoc comparisons using the Bonferroni corrections indicated that the mean weekly walking steps at pretest for the experimental group was not significantly different than that for the control group (see Figure 1). The mean weekly walking steps at posttest for the experimental group was significantly higher (p<0.05) than that of the control group. And the mean weekly walking steps at follow-up for the experimental group was significantly higher (p<0.05) than that of the control group. In addition, the within group comparisons over time indicated that the mean weekly walking steps at post test for the experimental group was significantly higher (p<0.05) than at the pretest. The mean weekly walking steps at follow-up for the experimental group was also significantly higher (p<0.05) than that of the pretest (M = 4,125, SD = 2,693). There were no significant differences across time for the control group. See Table 1 for more details, including the means and standard deviations for study variables at pretest post-test, and follow-up.
Figure 1.
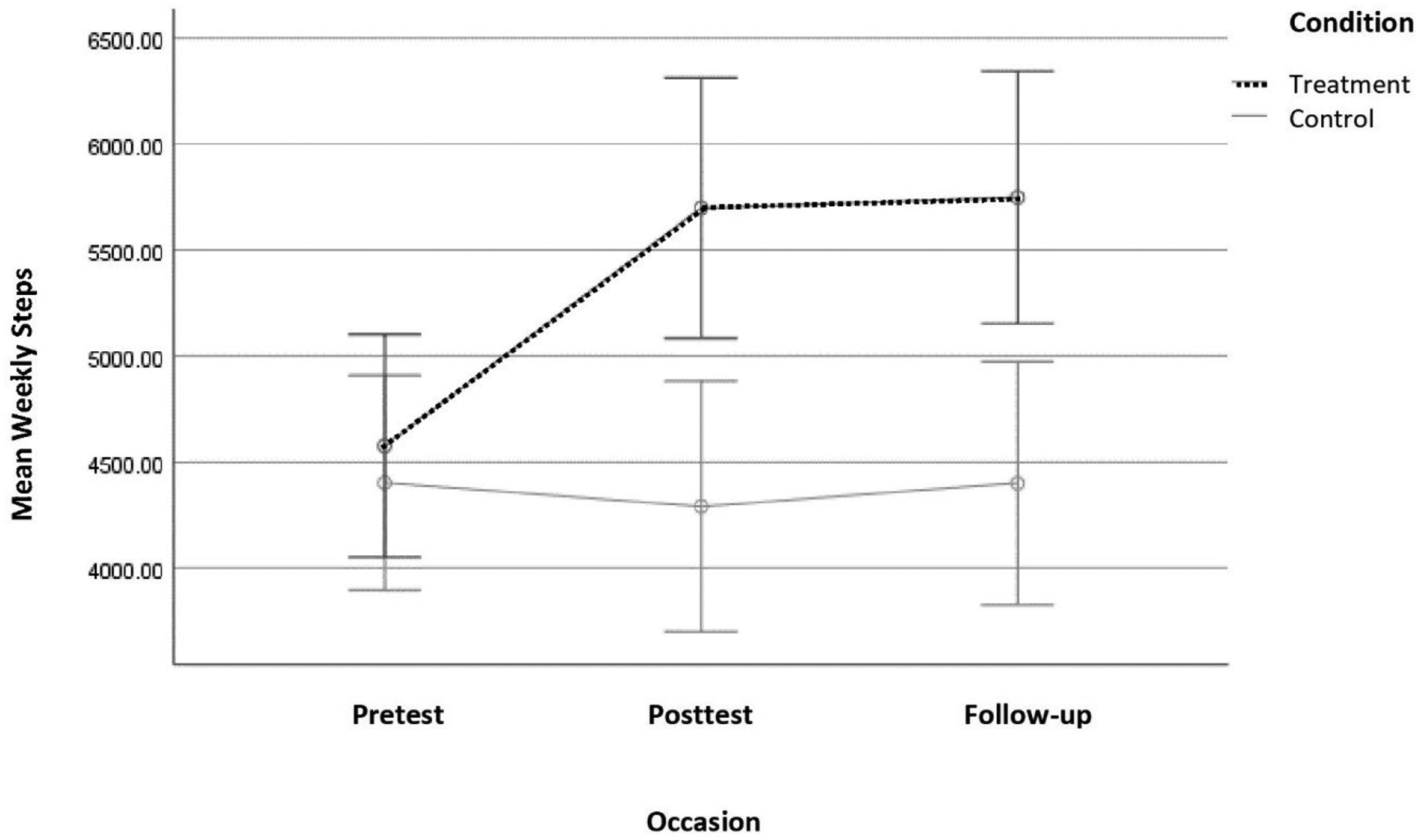
Mean weekly steps by condition and occasion. Note. Covariates include age, gender, self-reported health and education. The Error bars: 95% confidence intervals.
Social engagement.
The results of the repeated measures ANCOVA indicated that there was a significant interaction effect of time and treatment on social engagement. The interaction between time and condition was significant for level of social engagement, F (2, 56) = 6.12, p<0.05. Post hoc comparisons using the Bonferroni correction indicated that the mean level of social engagement at pretest for the experimental group (M = 35.9, SD = 11.3) was not significantly different than that of the control group (M = 35.1, SD = 11.5). The mean level of social engagement for the treatment group at both posttest and follow up were significantly different (p<0.05) than that of the control group. In addition, the within group comparisons over time for the experimental group indicated that the mean level of social engagement at post test (M = 45.7, SD = 11.5) and at follow-up (M=44.1, SD = 10.8) were significantly different (p<0.05) than that of the pretest (M = 35.9, SD = 11.3). There were no within group differences across time for the control group.
Social contact and comparisons.
To index social contact, we used counts of the text messages sent during the study by the experimental group. Across all participants in the experimental group, 10 messages were sent per person on average in week 1, 12 messages on average in week 2, 14 messages on average in week 3, and 15 messages on average in week 4. All the participants sent at least one message weekly during the 4 weeks; the range was 1 to 30 messages per person per week. On all days (during the 4 weeks, 28 days in total), at least one person mentioned their own step counts to the group. 96.4% of the participants sent at least one message that mentioned their own or their group members’ steps each day during the 4 weeks. Only one participant did not send a message related to steps in week 1, but started sending messages related to step counts in week 2. Participants’ comments showed evidence of social engagement. Each day, on average, there were at least four participants congratulating other participants on their activity levels, such as “[name omitted], do you mind if I ask how do you do so many steps, it’s impressive.” We can see from the group chat that participants were engaged in disclosure of information about their own daily steps, commenting on the number of steps and were also open to reciprocity from others. For example, one participant said: “I had over 9,000 steps again yesterday and hope to exceed that number today!” Another participant replied, “Wow, that’s amazing, how did you do that?”.
Exercise self-efficacy.
The results of repeated measures ANCOVA indicated that there were no significant main effects of time, condition or interaction effects of time and treatment on exercise self-efficacy.
Findings from the Mediation Model
The mediation model tested whether condition was related to change in mean of daily steps and whether this relationship was mediated by social engagement. Coefficients and 95% confidence intervals (CIs) are provided (see Table 2 and Figure 3). The total effects model demonstrated that condition was significantly related to change of mean weekly steps (total effect: 1.39, 95% CI: 1.04, 1.43). As shown in Table 2, while controlling for age, sex, race, and education, condition was positively related to change of social engagement (9.14, 95% CI: 3.72, 14.55). Social engagement was also positively related to the change of mean weekly steps, and the direct path between condition and change of mean weekly steps was significant (direct effect: 1.06, 95% CI: 0.97, 1.81). For the mediational effect, kappa squared (κ 2) is provided as a measure of effect size, as recommended by Preacher and Kelley (2011). With the guidelines of Cohen (1988), small, medium, and large effect sizes are stated as 0.01, 0.09, and 0.25 respectively for mediation analysis. The mediation analysis demonstrated that social engagement (indirect effect: 0.22, 95% CI: 0.19, 0.61, κ 2 = 0.03) had a small but significant partial mediation effect on the relationship between condition and change of mean weekly steps.
Table 2.
Coefficients, Standard Errors, and 95% Confidence Intervals for the Mediation Model for Condition Effects on Percentage Change of Mean Weekly Steps from Pretest to Posttest
| Variables | Direct Effects | Path Coefficients | Indirect Effect | |||
|---|---|---|---|---|---|---|
| Social Engagement | ||||||
| b(SE) | CI | b(SE) | CI | b(SE) | CI | |
| Age | 0.02(0.01) | −0.03,0.02 | 0.15(0.02) | −0215, 0.24 | ||
| Gender | 0.15(0.26) | −0.19,0.95 | 0.17(0.04) | −0.29, 0.32 | ||
| Race | 0.04(0.05) | −0.30,0.47 | 0.05(0.06) | −0.18, 0.46 | ||
| Education | 0.06(0.06) | −0.97,0.18 | 0.06(0.08) | −0.05, 0.08 | ||
| Health | 0.11(0.04) | −0.08,0.14 | 0.11 (0.02) | −0.12, 0.20 | ||
| Condition | 1.06***(0.11) | 0.97, 1.81 | 0.77***(0.16) | 0.68, 1.09 | ||
| Social Engagement | 0.18***(0.11) | −1.43, 0.45 | 0.22***(0.01) | 0.19, 0.61 | ||
Notes.
p<0.1,
p<0.05,
p<0.01.
Figure 3.

Mediation model: The condition effect on percentage change in mean weekly steps is mediated by the hypothesized mechanism, social engagement. Note. The relationship of condition (1=control, 2=treatment) and percentage change in weekly steps averaged over the 4 weeks, mediated by social engagement over 4 weeks. *p < .05. Indirect effect of social engagement: 0.22, 95% CI: 0.19, 0.61, κ2= 0.03
Discussion and Implications
In this study, the WeRun function in WeChat was implemented to test an intervention aimed at increasing steps among older adults. Results showed that those in the treatment condition, which included social contact with other group members via chats as well as information about the number of steps others achieved, increased steps more than those in the control condition, who did not have any information about the other participants. The treatment group also increased their social engagement more than the control group. Moreover, social engagement was found to be a significant mechanism of change for increasing weekly steps. The results suggest that social apps such as WeChat may be able to play a role in increasing physical activity and social engagement among older adults in a fun and enjoyable way. In line with predictions, a group-based walking competition function provided opportunities for social engagement and motivation for physical activity. This highlights the importance of the social environment in increasing physical activity, as suggested by SCT.
As past work had shown, peer groups could be a strong motivator for older adults to be more active, both physically and socially, which can lead to a healthier lifestyle (Brothers, & Diehl, 2017). Therefore, it is promising that the intervention was effective in increasing activity levels which progressively decrease with age and the prevalence of inactivity is highest among adults aged 65 or greater (Watson et al., 2016). Previous research indicated that 66% of adults over 75 do not engage in any regular physical activity and 50% of sedentary adults have no plan of starting an exercise program (Schutzer & Graves, 2004). Recent Pew Research Center surveys (2017) found that older adults are increasingly more digitally engaged and connected. Four-in-ten (42%) adults ages 65 and older report owning smartphones, up from just 18% in 2013. Smartphone ownership among older adults varies substantially by age: 59% of 65 to 69-year-olds own smartphones (Anderson & Perrin, 2017). In fact, some groups of older adults – such as those who are younger and more highly educated – report owning and using various technologies at rates similar to adults under the age of 65. Future interventions using smart phone apps could be expanded to promote physical activity and social engagement and reduce perceived barriers to an active lifestyle in community settings.
Participants in the treatment condition were encouraged to compare their daily steps with the group members and share their thoughts in group text messages. Examination of the messages showed that participants congratulated and encouraged each other. However, in future research, it is important to consider potential negative effects from unmoderated social interactions, which could result from upward social comparisons among participants. Mixed findings have been obtained in previous research on the relationship between social network sites and users’ subjective well-being. Some studies have demonstrated that social comparison through social network sites can be positively related to people’s subjective well-being (e.g., Wang et al., 2017); whereas others have reported that it is associated with depressive symptoms and anxiety (Shaw et al., 2015). The factors associated with positive effects such as support and positive emotions have received significant scholarly attention (Appel et al., 2015). The potential negative effects that might be due to feelings of inadequacy or failure dues to upward social comparisons (Wang et al., 2017) should be considered in future research. We were able to take a preliminary look at possible negative effects by examining results with a measures of happiness in our study: “during the past month, how much time have you been a happy person?” (scale range from 1 to 6, which was reverse coded with 1 represented none of the time, and 6 equaled all of the time). Result of the paired t-test indicated that there was no significant difference between the participants’ pre and posttest ratings in happiness and wellbeing. Further research is needed to understand under what circumstances social comparison in social networks is related to positive or negative outcomes, especially among older adults.
Limitations and Future Directions
This pilot study demonstrated the use of WeChat to increase physical activity in older adults. Several limitations should be noted. Physical activity was only measured by daily walking steps using smart phones, which might vary depending on the devices that participants use and how often they carried their smart phones, even though all participants were encouraged to carry their phone as often as possible through the day during the intervention. Although both groups were asked to use the We Chat and We Run functions, information as to how often and the length of time that the participants actually carried their phones is not available. Thus, the differences in steps between the two groups could be due differences in the amount of time they had their phones with them when walking. In future studies using smart phone apps, it would be ideal to also have participants wear a passive monitor such as a pedometer to supplement the account of steps from the smart phone.
Another consideration is that whereas social networks typically evolve through endogenous social selection based on similar interests or characteristics (Zhang et al., 2016), we artificially constructed the social networks used in this study. While this allowed us to ensure that there were no confounding effects from exogenous social information, it raises the potential that endogenous ties might create networks that were even stronger sources of support with more effective social engagement. The participants in this study interacted with each other virtually instead of with direct social contact or engagement. Therefore, the study may underestimate the effects of social engagement.
The findings also may be technology specific. The effects may generalize to other technologies that are useful and easy to use for older adults, but the same pattern of findings would not be expected with technologies that pose traditional barriers for older adults, for example, technologies that require complex skills (Sullivan & Lachman, 2017; Vaportzis et al., 2017). In addition, the 4-week span of the intervention might not be enough time for the behavior change to become part of the participants’ everyday routines. Future studies should work to develop methods to ensure more enduring behavior changes in physical activity.
Conclusions
In the present study social engagement was found to be a significant mechanism for changing physical activity behavior. Future studies should also test other elements of behavior change that may contribute to longer term maintenance of behavior change. Little is known about how to support community dwelling older adults to sustain positive behavior change. Identifying differences in mediators of behavior change and maintenance is an important area for future research and translation to community settings.
As motivation and social engagement are key factors for sustained healthy behavior (Lachman & Agrigoroaei, 2010; Lachman et al., 2018), the study results suggest that even virtual group-based walking using a smart phone app has the potential to increase physical activity. Exploring a physical activity-encouraging application for community dwelling older adults can contribute to knowledge about effective interventions to improve physical activity participation and overall health and well-being among older adults.
Supplementary Material
Figure 2.

Mean level of social engagement by condition and occasion. Note. Covariates include age, gender, race self-reported health and education. The Error bars: 95% confidence intervals.
Acknowledgements:
Y. Liu and M. E. Lachman planned the study and wrote the article. Y. Liu collected the data and conducted the data analysis and was supervised by M. Lachman. Both authors interpreted the research findings. The authors would like to thank Victoria Sorrentino, the Lifespan Lab manager and the student research assistants Becca Feenstra and Alexis Sverdlik at Brandeis University for their help with recruiting participants and data collection. The authors also would like to thank Executive Committee Members of the Boston Roybal Center for Active Lifestyle Interventions, Drs. Lewis Lipsitz, James Lubben, and Carmen Castaneda Sceppa, for their valuable comments.
Funding:
This work was supported by a National Institute on Aging grant [P30 AG048785] for the Boston Roybal Center for Active Lifestyle Interventions (RALI).
Biographical statement for all authors:
Y. Liu is an assistant professor at the College of Health and Human Sciences in Northern Illinois University. She completed a two-year postdoctoral fellowship in the Department of Psychology at Brandeis University. Yujun received her PhD in Human Development with a simultaneous degree in Public Health from Virginia Tech.
M. E. Lachman, PhD is Minnie and Harold L. Fierman Professor of Psychology and Director of the Lifespan Developmental Psychology Lab at Brandeis University and the Boston Roybal Center for Active Lifestyle Interventions.
Footnotes
Conflict of Interest:
The authors declare that they have no conflict of interest.
ClinicalTrials.gov Identifier: NCT03803085
References
- Aklin WM, Stoeckel L, Green P, Keller C, King JW, Nielsen L, & Hunter C (2020). Commentary: National Institutes of Health (NIH) Science of Behavior Change (SOBC). Health Psychology Review, 1(14), 1–10. doi: 10.1080/17437199.2020.1716383 [DOI] [PubMed] [Google Scholar]
- Anderson M & Perrin A (2017). Tech adoption climbs among older adults. Pew Research Center. Retrieve from http://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/ [Google Scholar]
- Appel H, Crusius J, & Gerlach AL (2015). Social comparison, envy, and depression on Facebook: A study looking at the effects of high comparison standards on depressed individuals. Journal of Social and Clinical Psychology, 34(4), 277–289. doi: 10.1521/jscp.2015.34.4.277 [DOI] [Google Scholar]
- Bandura A (1990). Perceived self efficacy in the exercise of personal agency. Journal of Applied Sport Psychology, 2, 128–163. [Google Scholar]
- Bandura A (2004). Health promotion by social cognitive means. Health education & behavior, 31(2), 143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Barlow DH, Bullis JR, Comer JS, & Ametaj AA (2013). Evidence-based psychological treatments: An update and a way forward. Annual Review of Clinical Psychology, 9, 1–27. doi: 10.1146/annurev-clinpsy-050212-185629 [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE, (2000). From social integration to health: Durkheim in the new millennium. Soc. Sci. Med 51, 843–857. doi: 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Booth FW, Roberts CK, & Laye MJ (2012). Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology, 2(2), 1143–1211. doi: 10.1002/cphy.c110025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brothers AF, & Diehl M (2017). Feasibility and efficacy of the AgingPLUS program: Changing views on aging to increase engagement in physical activity. Journal of Aging and Physical Activity, 25, 402–411. 10.1123/japa.2016-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, & Tyrer P (2000). Framework for design and evaluation of complex interventions to improve health. British Medical Journal, 321, 694–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo DN, Tate DF, Ries AV, Brown JD, DeVellis RF, & Ammerman AS (2012). A social media–based physical activity intervention: a randomized controlled trial. American journal of preventive medicine, 43(5), 527–532.doi: 10.1016/j.amepre.2012.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, Chan P, Santaguida P, & Colantonio A (2009). The use of mobility devices among institutionalized older adults. Journal of Aging and Health, 21(4), 611–626. doi: 10.1177/0898264309333313 [DOI] [PubMed] [Google Scholar]
- Cockerham WC, Wolfe DJ, & Bauldry S (2020). Health lifestyles in late middle age. Research on Aging, 42(1), 34–46. doi: 10.1177/0164027519884760 [DOI] [PubMed] [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, & Petticrew M (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ, 337, 979–983. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, … Obesity Related Behavioral Intervention Trials (ORBIT) Consortium. (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971–982. https://doi.org/2015-03938-001 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Wahl H-W, Brothers A, & Miche M (2015). Subjective aging and awareness of aging: Toward a new understanding of the aging self. In Diehl M & Wahl H-W (Eds.), Annual review of gerontology and geriatrics: Vol. 35. Annual review of gerontology and geriatrics, Vol. 35, 2015: Subjective aging: New developments and future directions (p. 1–28). Springer Publishing Co. [Google Scholar]
- Foster D, Linehan C, Kirman B, Lawson S, & James G (2010, October). Motivating physical activity at work: using persuasive social media for competitive step counting. In Proceedings of the 14th International Academic Mind Trek Conference: Envisioning Future Media Environments. 111–116. ACM. [Google Scholar]
- Gui X, Chen Y, Caldeira C, Xiao D, & Chen Y (2017, May). When fitness meets social networks: Investigating fitness tracking and social practices on WeRun. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (pp. 1647–1659). [Google Scholar]
- Hayes AF, & Preacher KJ (2014). Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical and Statistical Psychology, 67, 451–470. doi: 10.1111/bmsp.12028 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. [DOI] [PubMed] [Google Scholar]
- Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, & Kahlmeier S (2012). The pandemic of physical inactivity: Global action for public health. The Lancet, 380, 294–305. doi: 10.1016/S0140-6736(12)60898-8 [DOI] [PubMed] [Google Scholar]
- Khosravi P, Rezvani A, & Wiewiora A (2016). The impact of technology on older adults’ social isolation. Computers in Human Behavior, 63, 594–603. [Google Scholar]
- Lachman ME, & Agrigoroaei S (2010). Promoting functional health in midlife and old age: Long-term protective effects of control beliefs, social support, and physical exercise. PLoS ONE, 5, e13297. doi: 10.1371/journal.pone.0013297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Neupert SD, & Agrigoroaei S (2011). The relevance of control beliefs for health and aging. In Schaie KW & Willis SL (Eds.), Handbook of the psychology of aging (7th ed., pp. 175–190). New York, NY: Elsevier. [Google Scholar]
- Lachman ME, Lipsitz L, Lubben J, Castaneda-Sceppa C, & Jette AM (2018). When adults don’t exercise: Behavioral strategies to increase physical activity in sedentary middle-aged and older Adults. Innovation in Aging, 2(1), igy007. doi: 10.1093/geroni/igy007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, & Lachman ME (2019). Education and cognition in middle age and later life: The mediating role of physical and cognitive activity. The Journals of Gerontology: Psychological Sciences, gbz020. 1–12. doi: 10.1093/geronb/gbz020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindeman DA, Kim KK, Gladstone C, & Apesoa-Varano EC (2020). Technology and caregiving: Emerging interventions and directions for research. The Gerontologist, 60(Supplement_1), S41–S49. doi: 10.1093/geront/gnz178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubben J, & Gironda M (2004). Measuring Social Networks and Assessing their Benefits. Social Networks and Social Exclusion: Sociological and Policy Perspectives. Burlington, VT: Ashgate Publishing Company. [Google Scholar]
- Marello MM, Patrick JH, & Nehrkorn-Bailey AM (2019). (Older) people remember how you make them feel: age differences in the effects of social exchanges. Innovation in Aging, 3(Suppl 1), S178. [Google Scholar]
- Matz-Costa C, Carr DC, McNamara TK, & James JB (2016). Physical, cognitive, social, and emotional mediators of activity involvement and health in later life. Research on Aging, 38(7), 791–815. doi: 10.1177/0164027515606182 [DOI] [PubMed] [Google Scholar]
- McAuley E, Mailey EL, Mullen SP, Szabo AN, Wójcicki TR, White SM, … Kramer AF (2011). Growth trajectories of exercise self-efficacy in older adults: influence of measures and initial status. Health psychology: official journal of the Division of Health Psychology, American Psychological Association, 30(1), 75–83. doi: 10.1037/a0021567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, & Degens H (2016). Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology, 17(3), 567–580. doi: 10.1007/s10522-016-9641-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2017). Health, United States, 2016: With Chartbook on Long-term Trends in Health. Hyattsville, MD. [PubMed] [Google Scholar]
- Mitzner TL, Savla J, Boot WR, Sharit J, Charness N, Czaja SJ, & Rogers WA (2018). Technology adoption by older adults: findings from the PRISM trial. The Gerontologist, 59(1), 34–44. doi: 10.1093/geront/gny113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nehrkorn-Bailey AM, Patrick JH, & Marello MM (2019). The impact of negative social exchanges on adult physical and mental health. Innovation in Aging, 3(Suppl 1), S144. 10.1093/geroni/igz038.519 [DOI] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports Exercise, 39, 1435–1445. [DOI] [PubMed] [Google Scholar]
- Notthoff N, & Carstensen LL (2014). Positive messaging promotes walking in older adults. Psychology and Aging, 29(2), 329–341.doi: 10.1037/a0036748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell KE, Paluch AM, & Blair SN (2011). Physical activity for health: What kind? How much? How intense? On top of what? Annual Review of Health, 32, 349–365. doi: 10.1146/annurev-publhealth-031210-101151 [DOI] [PubMed] [Google Scholar]
- Pun R (2015). WeChat in the library: promoting a new virtual reference service using a mobile app. Library High Tech News, 32, 6, 9–11, 10.1108/LHTN-03-2015-0017 [DOI] [Google Scholar]
- Resnick B, & Jenkins LS (2000). Testing the reliability and validity of the self-efficacy for exercise scale. Nursing Research, 49(3), 154–159. [DOI] [PubMed] [Google Scholar]
- Robinson SA, Bisson AN, Hughes ML, Ebert J & Lachman ME (2018). Time for change: Using implementation intentions to promote physical activity in a randomised pilot trial. Psychology & Health, 34 (2), 232–254. doi: 10.1080/08870446.2018.1539487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlomann A, Seifert A, Zank S, & Rietz C (2020). Assistive technology and mobile ICT usage among oldest-old cohorts: Comparison of the oldest-old in private homes and in Long-Term Care facilities. Research on Aging. doi: 10.1177/0164027520911286 [DOI] [PubMed] [Google Scholar]
- Shaw AM, Timpano KR, Tran TB, & Joormann J (2015). Correlates of Facebook usage patterns: The relationship between passive Facebook use, social anxiety symptoms, and brooding. Computers in Human Behavior, 48, 575–580. doi: 10.1016/j.chb.2015.02.003 [DOI] [Google Scholar]
- Sullivan AN, & Lachman ME (2017). Behavior change with fitness technology in sedentary adults: A review of the evidence for increasing physical activity. Frontiers in public health, 4, (289), 1–16. doi: 10.3389/fpubh.2016.00289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JL, Wang HZ, Gaskin J, & Hawk S (2017). The mediating roles of upward social comparison and self-esteem and the moderating role of social comparison orientation in the association between social networking site usage and subjective well-being. Frontiers in psychology, 8, 771. doi: 10.3389/fpsyg.2017.00771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson KB, Carlson SA, & Gunn JP et al. (2016). Physical inactivity among adults aged 50 years and older — United States, 2014. Morbility and Mortality Weekly Report. 65, 954–958. doi: 10.15585/mmwr.mm6536a3externalicon. [DOI] [PubMed] [Google Scholar]
- Vaportzis E, Clausen MG, & Gow AJ (2017). Older adults perceptions of technology and barriers to interacting with tablet computers: A focus group study. Frontiers in psychology, 8, 1687–1698. doi: 10.3389/fpsyg.2017.01687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Brackbill D, Yang S, Becker J, Herbert N, & Centola D (2016). Support or competition? How online social networks increase physical activity: A randomized controlled trial. Preventive Medicine Reports, 4, 453–458. doi: 10.1016/j.pmedr.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


