Abstract
Background
Leadless pacemaker (LP) therapy has been proved effective in cases where traditional transvenous right pacing (TRP) failed. TRP through a bioprosthetic tricuspid valve (BTV) has always been considered an unpreferable solution because of possible deleterious effect of permanent pacing leads on BTV function and specifically on tricuspid regurgitation (TR). Very limited data exist about the feasibility and safety of LP implantation in this setting.
Methods
We describe two cases of LP implantation through BTV in patients with failure of epicardial pacemaker implanted after cardiac surgery. The focus is on technical description of the procedure and on electrical and echocardiographic evaluation at implantation and at the follow‐up.
Results
In both cases, skilled and careful handling of the delivery system as well as proper use of X‐ray oblique views was determinant for atraumatic successful valve crossing. Likewise, an accurate selection of the deployment site inside the right ventricle, far enough from the valve to avoid valvular dysfunction, was important for successful implantation. Electrical parameters of LP were satisfying at implantation and at the follow‐up. The echocardiogram after implantation and at the follow‐up showed no mechanical interference of LP with prosthetic valve, no significant TR, and absence of significant changes in the biventricular function.
Conclusion
Our data seem to support feasibility and safety of this type of procedure in skilled hands, allowing efficacious pacing without valvular dysfunction or right ventricular (RV) physiology impairment.
Keywords: bioprosthetic tricuspid valve, leadless pacemaker, Micra Transcatheter pacing system, transvenous pacing failure
Leadless pacemaker (LP) therapy has been proved effective in cases where traditional transvenous right pacing (TRP) failed. TRP through a bioprosthetic tricuspid valve (BTV) has always been considered an unpreferable solution because of possible deleterious effect of permanent pacing leads on BTV function and specifically on tricuspid regurgitation (TR). Very limited data exist about the feasibility and safety of LP implantation in this setting. We describe two cases of LP implantation through BTV in patients with failure of epicardial pacemaker implanted after cardiac surgery. The focus is on technical description of the procedure and on electrical and echocardiographic evaluation at implantation and at the follow‐up. In both cases, skilled and careful handling of the delivery system as well as proper use of X‐ray oblique views was determinant for atraumatic successful valve crossing. Likewise, an accurate selection of the deployment site inside the right ventricle, far enough from the valve to avoid valvular dysfunction, was important for successful implantation. Electrical parameters of LP were satisfying at implantation and at the follow‐up. The echocardiogram after implantation and at the follow‐up showed no mechanical interference of LP with prosthetic valve, no significant TR, and absence of significant changes in the biventricular function. Our data seem to support the feasibility and safety of this type of procedure in skilled hands, allowing efficacious pacing without valvular dysfunction or RV physiology impairment.
![]()
1. INTRODUCTION
The safety and efficacy of the Micra Transcatheter Pacing System (MTPS) seems to be very high both in investigational studies and in the real‐world setting. 1 Leadless pacemaker (LP) therapy was developed to address the limitations of standard lead‐based pacing and it has been proved effective in cases where traditional transvenous right pacing (TRP) failed. 2
TRP through a bioprosthetic tricuspid valve (BTV) has always been considered an unpreferable solution because of possible deleterious effect of permanent pacing leads on BTV function and specifically on tricuspid regurgitation (TR). 3 Epicardial pacing, with all the limits intrinsic to this technology, is still in use and often preferred over transvenous pacemaker implantation in this setting.
Very limited data exist about the feasibility of LP implantation through a BTV and there is some concern about the potential mechanical interference of the large steerable delivery system with BTV structure and about the BTV function over the follow‐up. 4 , 5 , 6
We describe two cases of LP implantation through BTV, with technical description of the procedure and echocardiographic evaluation of BTV and right ventricular (RV) function in the follow‐up.
2. FIRST CASE REPORT
A 75‐year‐old man was referred to our center for epicardial PM malfunction in permanent atrial fibrillation with complete PM dependency. In 1995, the patient had undergone single‐chamber pacemaker implantation and A‐V node ablation inside an “ablate and pace strategy” because of permanent atrial fibrillation with unsatisfying rate control.
In 2003, the patient underwent mitral and tricuspid valve repair because of bivalve prolapse with severe regurgitation. Fifteen years later, because of the worsening of tricuspid and mitral valve regurgitation, the patient underwent mitral and tricuspid valve replacement, respectively, with an Hancock II valve bioprosthesis 29 mm (Medtronic, Inc) and an Hancock II valve bioprosthesis 33 mm (Medtronic, Inc). The RV pacing lead was cut and abandoned and a permanent pacemaker with an epicardial RV lead was implanted. In the follow‐up, the epicardial lead showed a progressive worsening of electrical parameters with a significant increase of the pacing threshold causing a premature device battery end of life (EOL).
In order to avoid the risk of iatrogenic BTV dysfunction with a traditional TRP, we decided to implant a LP (Micra, Medtronic Inc). The procedure was performed according to the standard technique. Skilled use of X‐ray oblique views was fundamental for a correct engagement of the tricuspid ring without injuries to the bioprosthetic valve. Left anterior oblique (LAO) view (40°) was helpful to visualize the tricuspid annulus as a clock to be crossed exactly in the center. Right anterior oblique (RAO) view (40°) was used to establish the correct advancement of the delivery system across the tricuspid valve and to evaluate the proper distance of deployment site from the valve (Figure 1). The pacing threshold was 0.75 V at 0.24 ms, the R‐wave sensing amplitude was 12.7 mV, and the pacing impedance was 430 Ohm. The chest X‐ray confirmed the correct position of the device.
FIGURE 1.
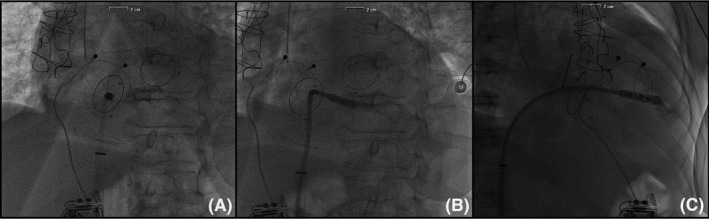
(A) LAO view before Micra deployment, (B) LAO view with iodate contrast medium before Micra deployment, (C) RAO view with iodate contrast medium before Micra deployment
The exhausted pacemaker was then removed after the maturation period of LP and the epicardial lead abandoned.
The echocardiogram, just after implantation and at 6 months follow‐up, showed no mechanical interference of the LP with the BTV, no worsening of TR, and good parameters of RV function (Table 1).
TABLE 1.
Micra Transcatheter Pacing System implantation through bioprosthetic tricuspid valve: Echocardiographic and device related electrical parameters at implantation and at 6 month follow‐up
| Variables | Case 1 | Case 2 | ||
|---|---|---|---|---|
| At implantation | 6 mo FU | At implantation | 6 mo FU | |
| LVSV (mL/mq) | 50 | 50 | 132 | 130 |
| LVDV (mL/mq) | 117 | 119 | 190 | 201 |
| LVEF (%) | 57 | 57 | 30 | 35 |
| TAPSE (mm) | 8 | 8 | 12 | 12 |
| TR (x/++++) | + | + | + | + |
| Sensing (mV) | 12.7 | 12.1 | 6.5 | 7 |
| Pacing (mV at 0.24 ms) | 0.75 | 0.63 | 0.88 | 0.63 |
| Impedance (Ohm) | 430 | 440 | 470 | 400 |
Abbreviations: LVDV, left ventricular diastolic volume; LVEF, left ventricular ejection fraction; LVSV, left ventricular systolic volume; TAPSE, tricuspid annular plane systolic excursion; TR, tricuspid regurgitation.
3. SECOND CASE REPORT
A 75‐year‐old male with a permanent atrial fibrillation and a BTV was referred to our center for early failure of epicardial PM. In 1998, he had undergone mitral valve replacement with a Carbomedics mechanical valve 31 mm (Carbomedics) and in 2019, he underwent tricuspid valve replacement with a 33 mm Hancock bioprosthetic valve because of massive regurgitation. He developed permanent heart block as a complication of cardiac surgery that required permanent pacing accomplished by epicardial PM implantation with lead positioning through a left mini‐thoracotomy. Because of recurrent malignant ventricular arrhythmias persisting in the follow‐up, the patient also underwent subcutaneous implantable cardioverter defibrillator (EMBLEM MRI S‐ICD system Boston Scientific) implantation.
After 1 month follow‐up, the electrical parameters of the epicardial pacing system showed a rapid worsening with progressive increase of RV pacing threshold reaching 5 V at 1.5 ms, disabling automatic pacing threshold algorithm, and raising serious concern about the reliability of pacing function.
The patient, after collegial discussion of the case, underwent LP implantation (Micra, Medtronic Inc) by the means of standard technique just after 40 days following tricuspid valve replacement.
Because of the very recent placement of BTV, particular caution was because of the engagement of the annulus to avoid any mechanical contact of the delivery system with the stent of the BTV. Also, just before LP deployment, while shaping the goose neck with the Micra delivery system to ensure adequate pressure of the tip against the wall, particular caution was because of avoid pushing of the bend of the loop against the valve ring (Figure 2). The LP implantation was successfully accomplished without any complication.
FIGURE 2.
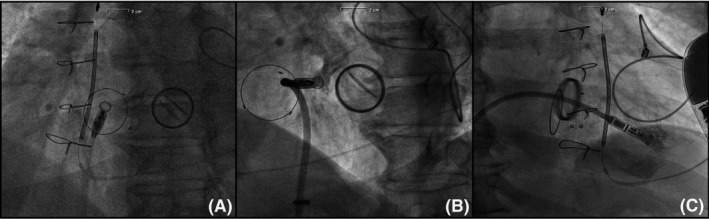
(A) LAO view before Micra deployment, (B) LAO view with iodate contrast medium before Micra deployment, (C) RAO view with iodate contrast medium before Micra deployment
Electrical parameters were satisfying at implantation and at the follow‐up. The echocardiogram after implantation showed no mechanical interference of LP with prosthetic valve and no significant regurgitation (Table 1).
4. DISCUSSION
For many years, BTV have traditionally represented a relative contraindication to transvenous RV pacing for possible BTV damage and dysfunction. Crossing the valve with a traditional lead may cause damaging of the leaflets, may worsen valvular regurgitation, and finally, the silicon‐coated lead represents an ideal substrate for the infectious colonization of pathogenic microorganisms potentially involving the valve. The contraindication for RV lead implantation is generally absolute in case of mechanical valve.
LP implantation is an emerging technology validated in clinical studies and real‐world setting with the potential advantage of overcoming some of the limits of the traditional lead‐based pacing.
LP implantation after tricuspid valve replacement (TVR) might represent a new frontier of this new technology by eliminating the risks connected with the presence of the lead across the bioprosthetic valve. Specifically, besides the reduction of risk of iatrogenic TR of the prosthetic valve because of the absence of pacing lead, LP technology could bring the further advantage of reducing the infectious risk and the occurrence of valvular endocarditis linked to silicon‐coated pacing leads.
Some concern is related to the procedural risk for the possible mechanical contact between the large steerable delivery system and the valve structure. The risk may be higher if the LP implantation is performed just after TVR, for a possible damage of sewing ring. Skilled and careful handling of the delivery system as well as proper use of X‐ray oblique views is determinant for atraumatic successful valve crossing. Likewise, an accurate selection of the deployment site inside the right ventricle, far enough from the valve to avoid valvular dysfunction, is important for successful implantation.
Taking in account all the limitations intrinsic to this limited experience, our data seem to support the feasibility and safety of this type of procedure in skilled hands, allowing efficacious pacing without valvular dysfunction or RV physiology impairment.
Further experience is needed to evaluate long‐term safety of this new frontier of application of LP technology.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
Morani G, Bolzan B, Pepe A, Ribichini FL. Leadless pacemaker through tricuspid bioprosthetic valve: Early experience. J Arrhythmia. 2021;37:414–417. 10.1002/joa3.12478
REFERENCES
- 1. Reddy VY, Exner DV, Cantillon DJ, Doshi R, Bunch TJ, Tomassoni GF, et al; LEADLESS II Study Investigators . Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med. 2015;373:1125–35. [DOI] [PubMed] [Google Scholar]
- 2. Morani G, Bolzan B, Borio G, Tomasi L, Ribichini FL. Leadless pacemaker implantation in achondroplastic dwarfism and recurrent cardiac implantable electronic device infections: a case report. Europace. 2018;20(7):1160. [DOI] [PubMed] [Google Scholar]
- 3. Eleid MF, Blauwet LA, Cha YM, Connolly HM, Brady PA, Dearani JA, et al. Bioprosthetic tricuspid valve regurgitation associated with pacemaker or defibrillator lead implantation. J Am Coll Cardiol. 2012;59(9):813–8. [DOI] [PubMed] [Google Scholar]
- 4. Kerwin SA, Mayotte MJ, Gornick CC. Transcatheter pacemaker implantation in a patient with a bioprosthetic tricuspid valve. J Interv Card Electrophysiol. 2015;44(1):89–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boveda S, Durand P, Combes S, Mariottini CJ. Leadless pacemaker surrounded by three valvular prostheses. Heart Rhythm. 2017;14(9):1421. [DOI] [PubMed] [Google Scholar]
- 6. Tang G, Kaple R, Cohen M, Dutta T, Undemir C, Ahmad H, et al. First percutaneous Micra leadless pacemaker implantation and tricuspid valve repair with MitraClip NT for lead‐associated severe tricuspid regurgitation. EuroIntervention. 2017;12(15):e1845–e1848. [DOI] [PubMed] [Google Scholar]


