Abstract
The autonomic nervous system (ANS) is known to play an important role in the genesis and maintenance of atrial fibrillation (AF). Biomolecular and genetic mechanisms, anatomical knowledges with recent diagnostic techniques acquisitions, both invasive and non‐invasive, have enabled greater therapeutic goals in patients affected by AF related to ANS imbalance. Catheter ablation of ganglionated plexi (GP) in the left and right atrium has been proposed in varied clinical conditions. Moreover interesting results arise from renal sympathetic denervation and vagal nerve stimulation. Despite all this, in the scenario of ANS modulation translational strategies we necessary must consider the treatment or correction of dynamic factors such as obesity, obstructive sleep apnea, lifestyle, food, and stress. Finally, new antiarrhythmic drugs, gene therapy and “ablatogenomic” could be represent exciting future therapeutic perspectives.
Keywords: atrial fibrillation, autonomic nervous system denervation, ganglionated plexi
Cardioneuroablation and cardioneuromodulation for patients affected by AF related to ANS imbalance.

1. INTRODUCTION
Several pathophysiological studies have shown that the genesis and maintenance of atrial fibrillation (AF) is partly influenced by the autonomic nervous system (ANS). 1 , 2 , 3 , 4 , 5 The imbalance of ANS represents one of the most important pathophysiological mechanisms for the AF genesis and maintenance together with the triggers and the substrate. 2 , 3 The vagal hypertonus is more involved in the induction of AF by rapid pulmonary veins (PVs) firing, 6 , 7 , 8 especially in patients without structural heart disease. Moreover the strong interactions between the cholinergic and adrenergic activity represents a significant mechanism for the genesis and recurrences of AF.
Recently, transcatheter biatrial ablation of ganglionated plexi (GP) has been suggested but with heterogeneous results. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 In the same time, several strategies of ANS modulation have been reassessed, considering physiopathological, molecular, genetic mechanisms and the underlying anatomical knowledge. Finally, the correction of dynamic factors capable of influencing ANS imbalance (such as obesity, obstructive sleep apnea (OSA), lifestyle, food, stress, etc.) is, especially today, considered a priority therapeutic strategy.
We reported a review of literature proposing a translational approach to better clarify interplay between ANS and AF and to guide therapeutic goals.
2. ATRIAL FIBRILLATION AND IMBALANCE OF THE AUTOMIC NERVOUS SYSTEM
2.1. Biomolecular mechanisms
Basic and clinical studies regarding the interaction between AF and ANS have highlighted the importance of the extrinsic cardiac ANS, mainly by stimulating the vagosympathetic trunk and by observing electrophysiological changes during AF initiation in animal models and human patients. 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25
The effect of vagal activation 26 on cardiomyocytes mainly consists in changes of ion channels function secondary to muscarinic acetylcholine (ACh) receptors (MAChRs) activation. This pathway is involved in slowing of heart rate, shortening of action potential (AP) duration, a reduction of contractile force in the atrium and, finally, a reduced conduction velocity in the atrio‐ventricular node (AVN). The ACh can influence G‐protein regulated inward‐rectifier K+ (GIRK) channels situated in the sinoatrial node (SAN), atria, AVN and Purkinje fibers. The effect of GIRK activation results in membrane hyperpolarization and a slowing of pacemaker activity in the SAN, and an atrial repolarization. In addition, a significant shortening of AP duration at the level of atrial myocytes, with consequent reentry and tachyarrhythmia inducibility, is one of the most important effect of GIRK activation and L‐type calcium channel (ICa,L) suppression, secondary to muscarinic activation. The interaction between ACh and its cellular receptor can also influence the funny current (If), promoting more negative potential and, consequently, slowing the pacemaker activity of the SAN. Finally, ACh is able to inhibit gap junction communication, with a consequent reduction of conduction velocity in the atrium, causing proarrhythmic reentry‐related effects.
The effects of vagal stimulation are reported in several experiments. 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 Zipes et al, 18 through a selective right and left vagosympathetic trunk and stellate ganglion stimulation in dogs, showed a greater atrial refractory period (ERP) shortening at the SAN level compared to other regions of the left and right atrium and a greater effect on the right atrium (RA) than on the left atrium (LA) after stimulation of the right vagosympathetic trunk. Both ERP and AP duration shortening/heterogeneity are able to facilitate the reentry mechanism and initiation of atrial tachyarrhythmias. The observation that the increased refractoriness heterogeneity plays a significant role in atrial vago‐related proarrhythmic effect is confirmed using flecainide to terminate AF by reducing refractoriness heterogeneity in animal studies. 26 Moreover the increased spatial heterogeneity in refractoriness related to vagal stimulation could be due to inhomogeneous nerve innervation and distribution of the atrial MAChRs and GIRK channel. 26
The sympathetic activation of cardiomyocytes occurs through the stimulation of β1 and β2‐receptor. Consequently, the activation of Gαs, or “stimulatory” subunit, triggers a series of phosphorylation reactions involving calcium channels (ICa,L), the sarcoplasmic‐reticulum Ca2+‐release channel ryanodine‐receptor, phospholamban and troponin I, with an increased calcium influx and augmented contractility, as well as increased calcium reuptake and myofilament relaxation (lusitropic effect). 27 The cascade of vagal e sympathetic activation on cardiomyocyte is summarized in Figure 1. The ANS seems to play an important role in initiating PV firing and paroxysmal AF. Sherlag et al 6 showed that the effects of vagal stimulation at the base of the right superior PV could provide a substrate for the conversion of PV firing into AF in a canine model. Po et al, 7 injecting a parasympathomimetic into the fat pad of 11 dogs, showed an acute autonomic remodeling resulting in spontaneous or easily induced sustained AF with short AF cycle length; the most rapid firing rate was observed in the PV and atria adjacent to the injected fat pad. Furthermore, GP stimulation seems to produce an increase in vagal and adrenergic activity with a consequent shortening of the PVs refractory period and genesis of early after‐depolarization (due to the increasing of intracellular Ca2+ concentrations), respectively.
FIGURE 1.
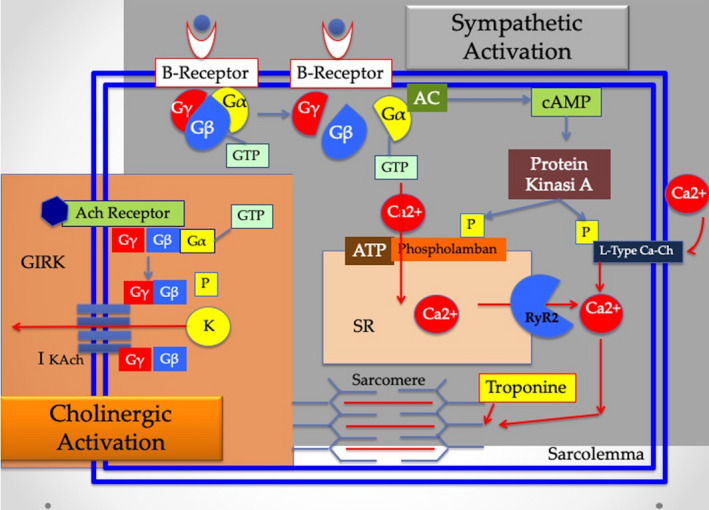
Effects of parasympathetic and sympathetic activation on cardiomyocyte. Vagal activation (indicated in orange) of muscarinic acetylcholine receptors (MAChRs) secondary to the release of the acetylcholine (ACh), influences G‐protein regulated inward‐rectifier K+ (GIRK) and determines GTP‐binding to subunit Gα (releasing Gβγ) and consequent activation of the ACh‐gated potassium currents (Ik,ACh). Sympathetic cascade (showed in orange) starts with β receptor activation followed by GPT‐binding to Gα, dissociation from subunits Gβ and Gγ, conversion‐adenylate cyclase (AC) dependent of ATP to cAMP, Ca2+ phosphorylation and finally activation of L‐Type Ca2+ channel at level of cytoplasmic membrane causing inward Ca2+ currents. In the same time activation of ryanodine receptor (RyR2) promotes outward Ca2 + currents from sarcoplasmic reticulum (SR) to cytoplasm. Finally, phoshorilamban phosphorylation promote SR Ca2+ uptake‐ATP mediated
Patterson et al, 8 demonstrated the important role of both parasympathetic and sympathetic nerve stimulation as triggering firing within canine PVs (calcium transient triggered firing hypothesis). The imbalance between repolarization and Ca2+ transient, initially due to the shortening of action potential duration, becomes arrhythmogenic when myocardial repolarization is accelerated by increased vagal nervous system tone and the Ca2+ transient is elevated by increased sympathetic nervous system tone. The high calcium concentration (Calcium gradient) during and immediately after repolarization drives Na+/Ca2+ exchange with three Na+ entering the cell for each Ca2+ exiting the cell, creating a net inward current. The inward current produces early atrial depolarizations and triggered firing.
Finally, fluctuations in autonomic tone could play a significant role in increasing paroxysmal AF recurrences. In fact, interesting studies have demonstrated that the interaction between adrenergic and cholinergic tone could have an important role in initiating and perpetuating AF burden. 28 Simultaneous adrenergic stimulation seems to facilitate the initiation of ACh‐mediated AF. 29 Fluctuations in autonomic tone before AF initiation were also demonstrated by using heart rate variability in human patients. 5 Moreover in AF ablation patients, when the sympathetic tone was prevalent, Lo et al 30 observed a larger LA, a more extensive substrate and the presence of non PVs‐triggers. Finally, the contribution of adrenergic and vagal tone on AF genesis is summarized in Figure 2.
FIGURE 2.
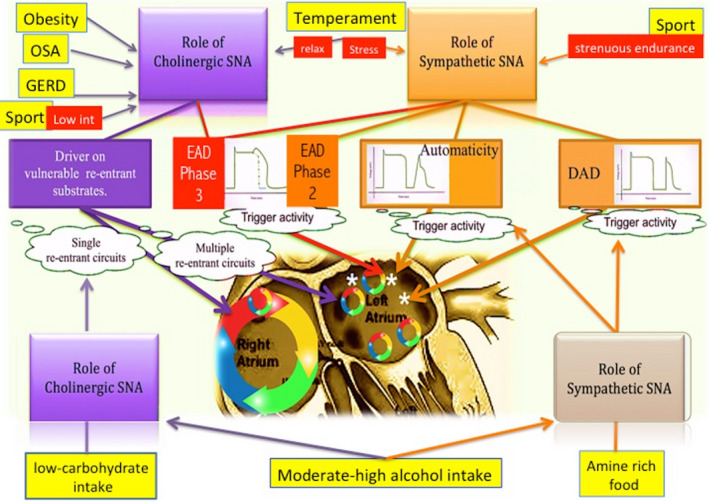
Autonomic Nervous System related‐mechanisms of AF beginning and maintenance The focal (white asterisk) mechanism of AF is mostly due to sympathetic contribution (orange lines and arrows) in order to promote trigger activity via automaticity (due to decreased inward‐rectifier K+ current and increased funny current during diastolic depolarization), genesis of EADs that influence phase 2 of the AP and DADs (due to the calcium overload and abnormal calcium release by the sarcoplasmic reticulum). Another mechanism of focal AF is related to induction of EADs during late phase 3 (red lines and arrows) due to the interaction between parasympathetic system through GIRK channels activation and sympathetic system through the increasing of intracellular calcium transient. Parasympathetic nervous system plays an important role for re‐entrant mechanism (violet lines and arrows). Finally, dynamic factors (yellow) can play an important role in this complex mechanism. (EADs, early after depolarizations; DADs, delayed after depolarization; AP, action potential; GIRK, G‐protein regulated inward‐rectifier K+.)
2.2. Dynamic factors
Several factors and clinical conditions could be implicated in determining of ANS imbalance and AF (Figure 2). The heterogeneous relationship between obesity and AF includes inflammation, lipotoxicity, and autonomic dysregulation determining changes involving both the trigger and the substrate. Epicardial fat is a visceral tissue particularly active in producing several anti and pro‐inflammatory adipocytokines, metabolic and growth factors (TNF‐alpha, IL‐1 beta and IL‐6) considered key mediators of AF. 31 , 32 Moreover epicardial fat pad contains GPs which play an important role in the genesis of AF due to ANS imbalance mainly through ERP shortening and dispersion increasing. Finally, the association between obesity and obstructive sleep apnea (OSA) could be considered particularly interesting in patients with frequent recurrences of AF.
Nevertheless, OSA seems to increase the risk of stroke, independently of other common risk factor, such as hypertension, AF, and diabetes. 33 The pathophysiologic mechanisms of the association between OSA and AF includes several mechanisms such us hypoxic damage, inflammation, oxidative stress, increasing of the cardiac afterload, increasing of left atrial wall stress and finally ANS imbalance. In fact, hypoxic and apneic episodes OSA related cause a hyperactivity of GPs and of the extrinsic ANS (left stellate ganglion) principally shortening ERP and triggering AF. 34 In several case of recurrent OSA episodes, patients could experience persistent AF with an increase in electrical and structural remodeling.
A potential association between gastroesophageal reflux disease and AF development has been proposed. The mechanical irritation subsequent to the anatomical spatial relationship between esophagus and the LA, gastroesophageal acid stimulation and subsequent systemic inflammation and impaired autonomic stimulation can be responsible for the genesis and maintenance of AF. 35
Similarly, AF episodes that occur after rapid ingestion of ice‐cold foods and beverages and after the swallowing are secondary to mechanical irritation and ANS imbalance related to anatomical vicinity of the LA at the esophagus end vagal nerve. 36
Furthermore, it is known that moderate‐high alcohol intake is associated to AF. 37 The most important underlying mechanism is due to ANS imbalance with a variable spectrum of clinical situations which include predominant vagal or hyperadrenergic activity and mixed forms as sometimes showed in ischemic patient. On the other hand, the consumption of red wine in low doses, seems to be associated with a lower risk of AF, thanks to the antiarrhythmic properties of resveratrol (a bioactive polyphenol found in grapes and red wine) that consist in the elimination of calcium overload and in the preservation of cardiomyocytes contractile function. 38
The relationship among food, ANS, and AF is also well known. One of the first examples of association between food and ANS is the protective anti‐inflammatory role of efferent vagal pathway activated by several condition such us electrical, pharmacological and via dietary lipids and proteins/peptides able to trigger release of cholecystokinin. 39 This pathophysiological knowledge is confirmed by the observation that a low‐carbohydrate intake (often recommended for weight control) could be associated to an increased risk of AF independently from the food (animal or plant protein and fat) used to replace the carbohydrate. The most important mechanism is characterized by the activation of inflammatory pathways and stimulation of oxidative stress in which ANS imbalance could play an important role. 40 Several investigations have shown the relationship between the ingestion of histamine‐rich and other amines‐rich foods and risk of AF and other arrhythmias. 41 Histamine is a vasoactive amine, with an arrhythmogenic potential risk in cellular and animal models. In fact, the stimulation of the H2‐ and H1‐receptor in the right atrium the left atrium triggers spontaneous diastolic depolarization, which may be involved in paroxysmal atrial tachycardia and AF. Moreover histamine could increase the risk of ventricular arrhythmias through a mechanism of purkinje‐fibers depolarization. Tryptamine (present in trace in some vegetable such as tomatoes) and tyramine (contained in goat's cheese, sausages, and cocoa) can be considered amines with real sympathomimetic, chronotropic, and vascular effects, determines an increasing risk of AF and other arrhythmias besides to blood pressure modifications due to the vasoconstriction.
Moreover several investigations have shown an association between type of AF and patients temperament. Maryniak A. et al 42 reported that patient affected AF during stress (AF with predominant adrenergic tone) presented higher emotional reactivity and lower endurance then patients with AF occurred during rest and relaxation (AF with predominant vagal tone).
Finally, we cannot leave out the important association between sport and AF related to ANS imbalance. The ANS is differently involved depending on the intensity of physical activity with a dominant parasympathetic activity at rest (example during the night) and during low‐intensity physical work and high sympathetic activity during acute strenuous endurance exercise. 43 Vagally mediated AF is due to shortening of ERP and to the increase of ERP heterogeneity. The mechanism underlying sympathetic‐related AF includes the shortening of the atrial action potential and the sympathetically induction of micro‐reentry, considered one of the most important triggers for the onset of AF in endurance athletes.
3. GANGLIONATED PLEXI ABLATION FOR ATRIAL FIBRILLATION
3.1. Ganglionated plexi anatomy
The significant heterogeneity of this topic can be inferred from the complex anatomy of the ANS, which is the reason why various attempts have been made in the literature to simplify the location of cardiac GP. Anatomy studies 26 have shown that human intrinsic cardiac ganglia are connected with the intrathoracic extracardiac ganglia via cardiopulmonary nerves, which lie adjacent to the superior vena cava, aortic root, and pulmonary artery. Moreover smaller mediastinal nerves run laterally to join the adjacent thoracic vagosympathetic trunks. Armour et al 44 showed that human intrinsic atrial cardiac ganglia and their associated nerves, situated in epicardial fat, form five GP:
(a) the superior right atrial GP (placed on the posterior superior surface of the right atrium adjacent to the junction of the superior vena cava and right atrium); (b) the superior left atrial GP (ganglia identified on the posterior surface of the left atrium between the PVs); (c) the posterior right atrial GP (on the posterior surface of the right atrium adjacent to the interatrial groove); (d) the posteromedial left atrial GP (on the posterior medial surface of the left atrium), (e) posterolateral left atrial GP (on the posterior lateral surface of the left atrial base on the atrial side of the atrioventricular groove). Individual neurons and small ganglia were also found scattered through atrial and ventricular tissues.
3.2. Left and bi‐atrial GP ablation
Several experimental investigations have highlighted a satisfactory effectiveness of GP ablation in order to prevent AF recurrences. 12 , 22 , 23 , 45 Hou et al, 23 evaluated in 28 dogs the effect of vagal stimulation on sinus and ventricular rate before and after sequential ablation of the superior left GP (SLGP, near the junction of the left superior PV and left pulmonary artery), anterior right GP (ARGP, near the SA node), and inferior right GP (IRGP, at the junction of the inferior vena cava and atria). This study confirmed that GPs function as “integration centers” integrating the autonomic innervation between extrinsic and intrinsic cardiac ANS because they affect atrial electrophysiology and pathophysiology as indicated by AF inducibility. The IRGP seems to be the integration center for the extrinsic ANS to innervate the AVN. In fact, in this study, the ablation of IRGP, especially if preceded by ILGP‐ARGP sequence ablation, showed a significant influence on AVN function, slowing the response induced by vagosympathetic stimulation. Moreover the ARGP seems to serve as the integration center for both the right and the left vagosympathetic trunks to modulate SAN function.
The observation by Pappone et al 46 of the best result of VPs isolation when associated to a significant vagal reaction evoked during radiofrequency applications, was the initial clinical confirmation of the potential efficacy of the “cardioneuroblation” for AF due to the ANS imbalance. The first example of a short‐term satisfactory result of GP ablation without VPs isolation came from Platt et al. 47
Many authors adopted a selective GP approach characterized by radiofrequency applications in atrial areas where vagal reaction was elicited during high frequency stimulation (HFS). In several cases, complex fractionated atrial electrograms (CFAEs) were observed near these targeted positive vagal sites. 10 Scanavacca et al 11 during endocardial and epicardial selective GP ablation, observed the absence of AF recurrence in only 29% of patients undergone vagal denervation. Moreover Po et al 16 showed that the combination of GP ablation with PV isolation was effective in more than 80% of patients at a long‐term follow up. The heterogeneous results of selective ANS denervation have outlined some critical attitudes regarding this ablation method. The “octopus theory”, 25 according to which a hyperactive state of the GP/octopus head, may trigger the local release of a gradient of excessive amounts of neurotransmitters and subsequently initiate AF, and that the excitation of assons/tentacles may determine a retrograde activation of GP at a distance, could provide an interesting explanation of the discrepancy between the sites of vagal response (which are also the sites of radiofrequency ablation) and the real location of GP. As a result, the validity of existing methods for the selective location of ganglionated plexi clusters is in question.
The anatomic approach, an alternative method of GP ablation, is characterized by an extended radiofrequency GP ablation based on anatomic knowledge of cardiac ganglia topography. 44 This method, mainly performed in the LA and in patients affected by paroxysmal AF, resulted more effective when compared with selective approach in the investigation published by Pokushalov et al. 15 The same approach was not beneficial when applied to ablate longstanding persistent AF. 17
3.3. Right atrial ganglionated plexi ablation
Our group has previously observed that the anatomic GP ablation in the RA for vagal AF, have a good success in about 70% of patients when compared with selective approach. 48 The rational of the GP ablation in the RA only, proposed by our group, derived from interesting anatomical and pathophysiological assumptions as well as from a better safety profile, considering the potential risk of complication related to standard AF ablation in the LA:
Posterior right atrial GP is made of a series of numerous GPs placed on the posterior surface of the RA adjacent to the interatrial groove, the junction of the superior vena cava (SVC) and between the SVC and the aorta. Ganglionated plexi localized between SVC and aorta is known as “third fat pad” considered the gateway point for the vagal input to the GP before innervating both RA and LA. 49 Lu et al 50 showed that the HFS of this anatomical structure slowed atrioventricular and sino‐atrial conduction, increased the window of vulnerability for AF at the SVC and shortened ERP.
Several experimental investigations have highlighted the physiopathological role of RA GP. 23 , 24 , 25 , 44 First of all, the RA GPs could modulate the function of the LA GPs placed at a distance through anatomical interconnections. In fact, Hou et al 23 showed that AF was no longer inducible only after the ARGP ablation probably because it seems to provide more extended bi‐atrial neural interconnection. Furthermore, the significant role of the ANS can be strongly considered when Lu et al 45 observed that right side GP stimulation was able to promote AF inducibility from PVs focal firing.
Our study showed a significant clinical advantage in patients undergone anatomic RA GP ablation when compared with selective approach. 48 The effectiveness of the anatomic approach could be secondary to the extension of lesions because we do not know for certain “the exact anatomic borders of GP clusters” as assumed by Pokushalov et al. 17 Moreover, IRGP ablation in the right atrium, at level of posteroseptal space (between the inter‐atrial grove and inside the coronary sinus), seems to be crucial to obtain a significant denervation. In fact, IRGP is considered an integration center for extrinsic ANS and a gateway for AVN function.
Several mapping and ablation investigations 51 , 52 identified a prevalence of CFAEs in the same area with the largest prevalence of atrial ganglia and in particular at level of the septum and posterior wall of the RA. Finally, in Figure 3 are schematized ablation bi‐atrial sites, on the basis of anatomical GP localization (IRGP, ARGP; ILGP; SLGP and third fat pad).
FIGURE 3.
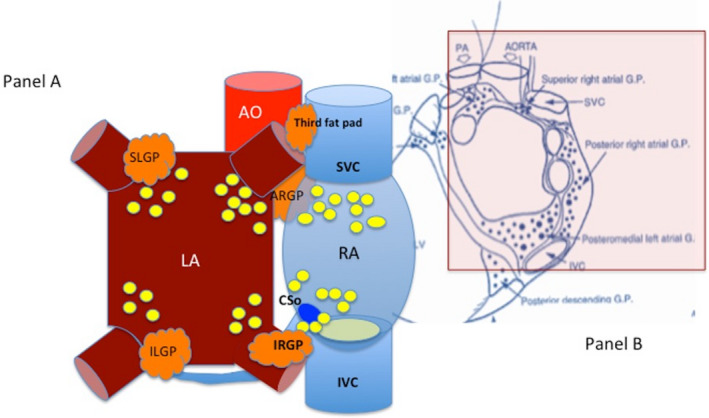
Simplified representation of the anatomical right and left atrial GP ablation in relation to topographic location of ganglion gateways (A) and of the most important GPs in anatomical studies (B). (IRGP, inferior right ganglionated plexi; ARGP, anterior right ganglionated plexi; ILGP, inferior left ganglionated plexi; SLGP, superior left ganglionated plexi; SVC, superior vena cava; IVC, inferior vena cava; CSo, coronary sinus ostium; RA, right atrium; LA, left atrium. (B) Image from Armour JA, Murphy DA, Yuan BX, et al Gross and microscopic anatomy of the human intrinsic cardiac nervous system. Anat Rec 1997; 1997 Feb;247(2):289‐98)
3.4. Surgical cardiac ganglionated plexi ablation
The surgical treatment of AF was reported for the first time in 1981 by Sealy et al. 53 Over the last years, several changes were performed in the surgical ablation procedures of AF. Currently, the Cox‐Maze III procedure has become the gold standard for the surgical treatment of AF, even if it has not been accepted as a standalone treatment because burdened by a high complexity and high incidence of complications. 54 Therefore, a minimally invasive surgery has been proposed to improve outcomes.
The addition of GP ablation to this procedure, seems not to influence the recurrence of AF and the occurrence of postoperative thromboembolic events during minimal invasive surgery. 55
Recently, Driessen et al 56 in the AFACT Study, evaluated the efficacy and safety of additional GP ablation to PV isolation during thoracoscopic surgery. Two hundred‐forty patients with advanced AF were randomized 1:1 to additional epicardial ablation of the 4 major GPs and Marshall's ligament or no extra ablation and followed every 3 months for 1 year. No statistically significant difference was collected on AF recurrence between the two groups; however, the GP group experienced major adverse events, bleeding, sinus node dysfunction, and pacemaker implantation. Moreover GP ablation during thoracoscopic surgery seems not to improve quality of life during follow up. 57
The role of complex fractionated atrial electrograms and the always innovative concept of “cardioneuroablation.”
Although the operative mechanism in the formation of CFAEs remains to be clarified, the blocking of functional conduction due to tissue anisotropy, colliding waveforms, migration rotors, and conduction slowing at critical parts of multiple re‐entrant circuits have been proposed as the underlying mechanisms. 58
Several studies on animal models and human patients have provided evidence that CFAEs can be provoked by ACh‐induced activation of the GP. 9 , 58 Katritsis et al 59 observed a higher representation of CFAEs (68.6%) than the rest of the LA endocardium (34.4%) in patients affected by paroxysmal AF. Oliveira et al 60 showed that atrial conduction times, the duration of the electrograms and fractionated activity are increased in paroxysmal AF, suggesting a role for conduction delays in the arrhythmogenic substrate. Acute vagal stimulation was associated with prolonged interatrial conduction time, and left atrial activation time in patients with inducible sustained AF and ANS modulation influenced the heterogeneity of atrial electrogram duration.
In this study, we found CFAEs at level of the postero‐septal region in the RA and their significant reduction in a large part of patients undergone RA GP ablation. 48 Therefore, GPs plus CFAEs ablation seems to be more effective in vagal AF patients when compared with standard approach represented by PVs isolation proved more advantageous for adrenergic AF patients. 61
Moreover considering the results of several studies based on the use of spectral analysis, the definition of CFAEs seems to be too general if we want to differentiate healthy tissue from fibrotic tissue in the context of atrial myocardium. Pachon et al, 62 , 63 , 64 , 65 from several years, first introduced the concept of “Cardioneuroablation” for treatment of neurocardiogenic syncope, functional AV block, and SA node dysfunction. The localization of postganglionic parasympathetic body neurons over and inside atrial wall, was the anatomical and pathophysiological rationale for the feasibility of this endocardial ablation procedure targeted to eliminate the parasympathetic postganglionic neurons and preserves the sympathetic and sensory systems. The effectiveness of this procedure was also reinforced by a significant reduction of the reinnervation risk, if the endocardial ablation target was represented by the postganglionic neural bodies, unable to regenerate. Furthermore, Pachon et al, analyzing the spectrum of endocardial signals using Fast Fourier Transform, observed the presence of two different pattern: a “compact myocardium” with isotropic conduction, high amplitude and smooth spectrum and a “fibrillar myocardium” characterized by anisotropic conduction, low amplitude and fragmented spectrum and strongly associated to the presence of cardiac nervous fibers. The spectral mapping‐ endocardial identification of fibrillar myocardium areas (AF Nest) and the observation of parasympathetic reflex abolition by using vagal nerve stimulation at level of internal jugular vein represent the main electrophysiological target of cardioneuroablation proposed, by several years, for treatment of patient affected by severe neurocardiogenic syncope and vagal AF. 64 , 65 , 66 , 67
Moreover Lellouche et al 68 showed three different patterns of LA endocardial electrograms in sinus rhythm in paroxysmal AF patients: normal, low amplitude fragmented electrograms (LAFEs), and high amplitude fragmented electrograms (HAFEs). The HAFE pattern was associated with a parasympathetic response during RF ablation especially observed near LA‐PV junctions, the LA posterolateral wall and the interatrial septum. Moreover the HAFE pattern was reproduced experimentally with adenosine and in a mathematical model simulating the effect of ACh. The LAFE pattern could be caused by atrial fibrosis as observed in mathematical simulations of atrial tissue with fibrotic characteristics. Finally, on the basis of these consideration, we could image in the present 69 , 70 and in the future scenario of ANS cardiac denervation an ablation procedure guided by softwares which it will be possible to identify fragmented signal indicative of the presence of nervous tissue in the context of a healthy myocardium (Figure 4).
FIGURE 4.
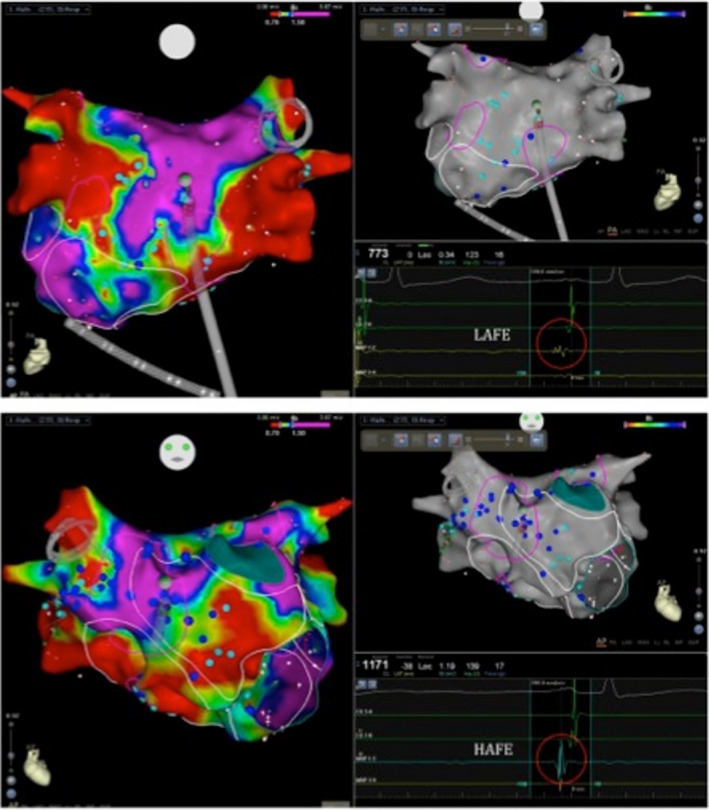
Perspectives future regarding electroanatomic voltage map (CARTO 3) of the left atrial signals with characterization of low amplitude fragmented signals (LAFE; A) and high amplitude fragmented signals (HAFE; B)
3.5. Clinical impact of reinnervation after ganglionated plexi ablation
One of the most interesting topics and issues regarding GP ablation for AF is whether reinnervation can influence middle and long‐term post‐procedural follow up. Some investigations have shown that heart transplantation achieves total sympathetic and parasympathetic denervation. 71
Sympathetic reinnervation is observed frequently after human heart transplantation, while parasympathetic reinnervation has been reported in only a few cases.
There is evidence that the autonomic normal function usually recovers within 6 months after ANS ablation in patients affected by AF 8 . Oh et al 72 observed a recovery of the normal ANS function parameter within 4 months after fat pad radiofrequency ablation and AF returned to be inducible as in the pre‐ablation period. In our experience of RA GP ablation, 48 we observed.
A complete recovery of autonomic function at 12 months in patients undergone anatomical approach and at 6 months in treated with the selective approach.
However, even today, we do not know for certain if there is a temporal relationship between reinnervation and the frequency of AF recurrences 73 .
Finally, as previously mentioned, an extensive endocardial denervation principally targeted to eliminate parasympathetic postganglionic neural bodies placed in the atrial wall and in GP seems to reduce the risk of a significant reinnervation. In fact, only sympathetic efferent and sensorial afferent neuronal fibers regenerate after endocardial ablation because their neural bodies are placed at distance from the heart. Conversely, an epicardial surgical ablation, whose target is represented only by neurons of extra cardiac ganglia, can be associated to a more extensive reinnervation, just for preservation of subepicardial, intramural and subendocardial neurons. 62 , 63 , 64 , 65
4. NON‐DIRECT CARDIAC NEUROMODULATION
4.1. Renal Sympathetic Denervation, stellate ganglion ablation, and vagal nerve stimulation
Several investigations have shown that Renal Sympathetic Denervation (RSD) usually proposed in patient affected by not‐controlled hypertension could play an important role for treatment of AF related to imbalance of sympathetic ANS (Figure 5). Some animal studies provided interesting findings regarding electrophysiological effects of renal modulation in term of prevention of AF inducibility‐atrial pacing guided, of shortening and dispersion of atrial refractoriness as well as of elevated plasma norepinephrine levels. 74 Feyz et al, in the AFFORD study, demonstrate that RSD might be able to decrease AF burden in hypertensive patients, determining a positive effect on quality of life. 75 Finally, same clinical result was recently observed in a metanalysis of six eligible (four randomized and two prospective nonrandomized) studies showing that this combined approach significantly decreased the risk of AF recurrence when compared with PVs isolation alone. 76 Nevertheless, RSD eliminates sympathetic postganglionic axons that can present rapid reinnervation.
FIGURE 5.
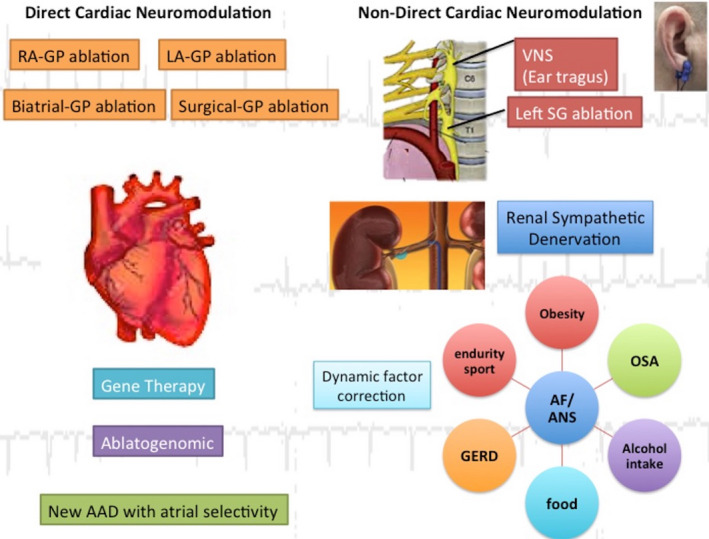
Representation of current and future perspectives regarding direct and non‐direct‐cardiac neuromodulation. (AAD, new antiarrhythmic drugs; VNS, vagal nerve stimulation; SG, stellate ganglion; OSA, obstructive sleep apnea; GERD, gastroesophageal reflux disease)
Other two example of non‐direct cardiac neuromodulation are represented by stellate ganglion ablation and vagal nerve stimulation (Figure 5). Cryoablation of bilateral stellate ganglion and T2 and T4 thoracic ganglia in dogs significantly (1) reduced heart rate response to nerves activity, (2) prolonged the time necessary for sustaining AF during atrial pacing and (3) suppressed premature atrial ectopic beats potentially related to recurrences of paroxysmal AF. This animal model is difficult to apply to human for anatomical barriers (even if today slightly reduced by videoscopy), for influence of cardiac risk factors and pathological conditions that often characterized human AF patients, for high risk of reinnervation and the absence of long‐term results. 77
Transcutaneous low‐level vagal nerve stimulation (through a mechanism of sympathetic activity suppression) showed good results in terms of AF suppression in animal models. One of the most important limits of this procedure is characterized by remodeling of stellate ganglion. In other words, it was observed a switching between adrenergic and cholinergic nerves as effect of vagal nerve stimulation including the activity increase of Ca‐dependent K channel tyrosine hydroxylase–positive ganglion cells. Finally, Stavrakis et al significantly found a reduction of inflammatory cytokines, AF inducibility and duration during ear tragus stimulation. 78 In fact, the “paradoxical” anticholinergic effects of ear tragus stimulation, which require efferent vagal fibers for their actions, are mediated by inhibiting the activity of the major atrial GP. Despite of this, other investigations with a long‐term follow up are necessary to really understand the real efficacy of this promising procedure.
4.2. Dynamic factors treatment
It is common opinion that no treatment of cardioneuromodulation can be definitively effective, if the dynamic factors, contributing to the ANS imbalance, are not simultaneously identified and treated. Therefore, the therapeutic management should inevitably consider the role of dynamic factors and their clinical correction (Figure 5).
As previously said, endurance sport is associated to AF risk because of increase vagal tone secondary to inflammation factors baroreflex responsiveness, inflammatory and sympathetic activity. However, chronic exercise training may be beneficial for the management of permanent AF by improving rate control. 79 Moreover Qureshi et al found an increased cardiorespiratory fitness inversely associated with a lower risk of AF and significantly in obese patients when compared with non obese. 80
In addition to a constant and regular physical activity finalized to weight loss, in obese patient affected by medium‐severe grade of OSA, the optimal treatment is represented by continuous positive airway pressure (C‐PAP). Several investigations showed the positive effects of C‐PAP in reducing AF recurrences even in patients undergone to PV isolation. 81 , 82 , 83
Finally, we cannot underestimate the important role of correct diet in AF patients, especially in those affected by ANS imbalance. It is important to not abuse of arrhythmogenic foods such as chocolate (especially if associated to salbutamol with the increased risk of methylxanthines triggering), cocoa‐rich foods and many other which contains biogenic amines. 41 Moreover a low‐carbohydrate diet, often used for weight loss, and strongly related to the increasing risk of AF should be avoided. 40 On the contrary, there are several evidences regarding Mediterranean diet and lower risk of AF. 84
4.3. Future perspective: from pharmacological to gene therapy
Interesting knowledges are emerging as results of animal studies regarding new antiarrhythmic drugs. In the specific case of autonomic function, the target of new pharmacological therapy is represented by the Ach‐gated potassium currents (Ik,ACh), small‐conductance calcium‐dependent potassium channels (SK channel) and molecular targets involved in intracellular calcium kinetics such us Ca2+/calmodulin–dependent protein kinase. In particular there is an ongoing research regarding selective Ik, ACh inhibitor deprived of neurological effects, toxicity, and capacity of AP prolongation. 85 Moreover other interesting molecules has been developed to modulate and/or to block SK channel particularly implicated in triggered activity of PVs. 86
Furthermore, several studies have contributed to clarify molecular and genetic mechanism underlying AF. The genetic variability is strongly associated to the clinical complexity of AF. Actually, more than 30 AF associated genome loci are investigated. Many of these are implicated in encoding of transcription factors, protein of atrial structure and in transcriptional regulation of ion channel and ion channel‐related proteins. 87 The modification of G protein‐α subunit activity, by using viral or non‐viral gene transfer methods, represent one of the most important target of gene therapy. Donahue et al, 88 using an adenoviral vector overexpressing the Gαi protein determining a reduction of AF heart rate secondary to AV conduction inhibition. Aistrup et al, found a decreasing of vagal related AF after non viral approach characterized by injection of plasmid DNA vector expressing Gαi/o C‐terminal peptide in the posterior left atrium. 89
Finally, future genomic evaluation in patients affected by AF could be used to predict post ablation success and to individualize the different ablation approach. In fact, the RS2200733 genetic variant, present within the 4q25 locus, seems to be associated with an increased risk of AF ablation failure. 90 Therefore, “the “ablatogenomic” is emerging on the scenario of AF therapy as a promising approach to better clarify who will really benefit from ablation procedure (Figure 5).
5. CONCLUSIONS
Data emerging from the experimental and clinical investigations of this review certainly reinforce the important role of the ANS in the pathogenesis of AF. Nevertheless, direct‐cardiac (such as bi‐atrial, RA‐GP ablation and surgical ablation) and non‐direct cardiac (VNS, stellate ganglion ablation, renal sympathetic denervation) neuromodulation procedures have been proposed with conflicting results. In our opinion, an appropriate knowledge of pathophysiological, biomolecular and genetic mechanisms underlying the complex interplay between AF and ANS, is essential to overcame these therapeutic limitations. Moreover this methodological approach must be considered the real neural basis on which to build new translational therapeutics such as gene therapy, ablatogenomic, and new antiarrhythmic drugs. Finally, correction or treatment of dynamic factors should not be underestimated in the context of a translational and individualized approach.
CONFLICT OF INTEREST
None of the authors has any conflict of interest.
Rebecchi M, Panattoni G, Edoardo B, et al. Atrial fibrillation and autonomic nervous system: A translational approach to guide therapeutic goals. J Arrhythmia. 2021;37:320–330. 10.1002/joa3.12512
REFERENCES
- 1. Allessie MA, Rensma PL, Brugada J, Smeets JRLM, Penn O, Kirchhof CJHJ. Pathophysiology of atrial fibrillation. In: Zipes DP, Jalife J, editors. Cardiac electrophysiology: from cell to bedside. Philadelphia, PA: WB Saunders Co; 1990; p. 548–58. [Google Scholar]
- 2. Coumel P. Autonomic influences in atrial tachyarrhythmias. J Cardiovasc Electrophysiol. 1996;7(10):999–1007. [DOI] [PubMed] [Google Scholar]
- 3. Coumel P, Thomas O. Cardiac arrhythmias and the autonomic nervous system. J Med Liban. 1997;45(4):212–6. [PubMed] [Google Scholar]
- 4. Schauerte P, Scherlag BJ, Patterson E, Scherlag MA, Matsudaria K, Nakagawa H, et al. Focal atrial fibrillation: experimental evidence for a pathophysiologic role of the autonomic nervous system. J Cardiovasc Electrophysiol. 2001;12(5):592–9. [DOI] [PubMed] [Google Scholar]
- 5. Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation. 2002;105(23):2753–9. [DOI] [PubMed] [Google Scholar]
- 6. Scherlag BJ, Yamanashi W, Patel U, Lazzara R, Jackman WM. Autonomically induced conversion of pulmonary vein focal firing into atrial fibrillation. J Am Coll Cardiol. 2005;45(11):1878–86. [DOI] [PubMed] [Google Scholar]
- 7. Po SS, Scherlag BJ, Yamanashi WS, Edwards J, Zhou J, Richard W, et al. Experimental model for paroxysmal atrial fibrillation arising at the pulmonary vein‐atrial junctions. Heart Rhythm. 2006;3(2):201–8. [DOI] [PubMed] [Google Scholar]
- 8. Patterson E, Po SS, Scherlag BJ, Lazzara R. Triggered firing in pulmonary veins initiated by in vitro autonomic nerve stimulation. Heart Rhythm. 2005;2(6):624–31. [DOI] [PubMed] [Google Scholar]
- 9. Schauerte P, Scherlag BJ, Pitha J, Scherlag MA, Reynolds D, Lazzara R, et al. Catheter ablation of cardiac autonomic nerves for prevention of vagal atrial fibrillation. Circulation. 2000;102(22):2774–80. [DOI] [PubMed] [Google Scholar]
- 10. Lemery R, Birnie D, Tang AS, Green M, Gollob M. Feasibility study of endocardial mapping of ganglionated plexus during catheter ablation of atrial fibrillation. Heart Rhythm. 2006;3(4):387–96. [DOI] [PubMed] [Google Scholar]
- 11. Scanavacca M, Pisani CF, Hachul D,Lara S, Hardy C, Darrieux F,, et al. Selective atrial vagal denervation guided by evoked vagal reflex to treat patients with paroxysmal atrial fibrillation. Circulation. 2006;114(9):876–85. [DOI] [PubMed] [Google Scholar]
- 12. Lemola K, Chartier D, Yeh YH, Dubuc M, Cartier R, Armour A, et al. Pulmonary vein region ablation in experimental vagal atrial fibrillation: role of pulmonary veins versus autonomic ganglia. Circulation. 2008;117(4):470–7. [DOI] [PubMed] [Google Scholar]
- 13. Katritsis D, Giazitzoglou E, Sougiannis D, Goumas N, Paxinos G, Camm AJ. Anatomic approach for ganglionic plexi ablation in patients with paroxysmal atrial fibrillation. Am J Cardiol. 2008;102(3):330–4. [DOI] [PubMed] [Google Scholar]
- 14. Danik S, Neuzil P, d'Avila A, Malchano ZJ, Kralovec S, Ruskin JN, et al. Evaluation of catheter ablation of periatrial ganglionic plexi in patients with atrial fibrillation. Am J Cardiol. 2008;102(5):578–83. [DOI] [PubMed] [Google Scholar]
- 15. Pokushalov E, Romanov A, Shugayev P, et al. Selective ganglionated plexi ablation for paroxysmal atrial fibrillation. Heart Rhythm. 2009;6(9):1257–64. [DOI] [PubMed] [Google Scholar]
- 16. Po SS, Nakagawa H, Jackman WM. Localization of left atrial ganglionated plexi in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2009;20(10):1186–9. [DOI] [PubMed] [Google Scholar]
- 17. Pokushalov E, Romanov A, Artyomenko S, et al. Ganglionated plexi ablation for longstanding persistent atrial fibrillation. Europace. 2010;12(3):342–6. [DOI] [PubMed] [Google Scholar]
- 18. Zipes DP, Mihalick MJ, Robbins GT. Effects of selective vagal and stellate ganglion stimulation on atrial refractoriness. Cardiovasc Res. 1974;8(5):647–55. [DOI] [PubMed] [Google Scholar]
- 19. Ninomiya I. Direct evidence of nonuniform distribution of vagal effects on dog atria. Circ Res. 1966;19(3):576–83. [DOI] [PubMed] [Google Scholar]
- 20. Alessi R, Nusynowitz M, Abildskov JA, Moe GK. Nonuniform distribution of vagal effects on the atrial refractory period. Am J Physiol. 1958;194(2):406–10. [DOI] [PubMed] [Google Scholar]
- 21. Liu L, Nattel S. Differing sympathetic and vagal effects on atrial fibrillation in dogs: role of refractoriness heterogeneity. Am J Physiol. 1997;273(2 Pt 2):H805–H816. [DOI] [PubMed] [Google Scholar]
- 22. Scherlag BJ, Nakagawa H, Jackman WM, Yamanashi WS, Patterson E, Po S, et al. Electrical stimulation to identify neural elements on the heart: their role in atrial fibrillation. J Interv Card Electrophysiol. 2005;13(1):37–42. [DOI] [PubMed] [Google Scholar]
- 23. Hou Y, Scherlag BJ, Lin J, Zhang Y, Lu Z, Truong K, et al. Ganglionated plexi modulate extrinsic cardiac autonomic nerve input: effects on sinus rate, atrioventricular conduction, refractoriness, and inducibility of atrial fibrillation. J Am Coll Cardiol. 2007;50(1):61–8. [DOI] [PubMed] [Google Scholar]
- 24. Hou Y, Scherlag BJ, Lin J, Zhou J, Song J, Zhang Y, et al. Interactive atrial neural network: determining the connections between ganglionated plexi. Heart Rhythm. 2007;4(1):56–63. [DOI] [PubMed] [Google Scholar]
- 25. Zhou J, Scherlag BJ, Edwards J, Jackman WM, Lazzara R, Po SS. Gradients of atrial refractoriness and inducibility of atrial fibrillation due to stimulation of ganglionated plexi. J Cardiovasc Electrophysiol. 2007;18(1):83–90. [DOI] [PubMed] [Google Scholar]
- 26. Yeh YH, Lemola K, Nattel S. Vagal atrial fibrillation. Acta Cardiol Sin. 2007;23(1):1–12. [Google Scholar]
- 27. Arora R. Recent insights into the role of the autonomic nervous system in the creation of substrate for atrial fibrillation: implications for therapies targeting the atrial autonomic nervous system. Circ Arrhythm Electrophysiol. 2012;5(4):850–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sharifov OF, Fedorov VV, Beloshapko GG, Glukhov AV, Yushmanova AV, Rosenshtraukh LV. Roles of adrenergic and cholinergic stimulation in spontaneous atrial fibrillation in dogs. J Am Coll Cardiol. 2004;43(3):483–90. [DOI] [PubMed] [Google Scholar]
- 29. Hashimoto K, Chiba S, Tanaka S, Hirata M, Suzuki Y. Adrenergic mechanism participating in induction of atrial fibrillation by ACh. Am J Physiol. 1968;215(5):1183–91. [DOI] [PubMed] [Google Scholar]
- 30. Lo L‐W, Chiou C‐W, Lin Y‐J, Chang S‐L, Hu Y‐F, Tsao H‐M, et al. Differences in the atrial electrophysiological properties between vagal and sympathetic types of atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24(6):609–16. [DOI] [PubMed] [Google Scholar]
- 31. Lavie CJ, Pandey A, Lau DH, Alpert MA, Sanders P. Obesity and atrial fibrillation prevalence, pathogenesis, and prognosis: effects of weight loss and exercise. J Am Coll Cardiol. 2017;70(16):2022–35. [DOI] [PubMed] [Google Scholar]
- 32. Mazurek T, Zhang L, Zalewski A, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–6. [DOI] [PubMed] [Google Scholar]
- 33. Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea‐hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182(2):269–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yu L, Li X, Huang B, et al. Atrial fibrillation in acute obstructive sleep apnea: autonomic nervous mechanism and modulation. J Am Heart Assoc. 2017;6(9):e006264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Linz D, Hohl M, Vollmar J, Ukena C, Mahfoud F, Böhm M. Atrial fibrillation and gastroesophageal reflux disease: the cardiogastric interaction. Europace. 2017;19(1):16–20. [DOI] [PubMed] [Google Scholar]
- 36. Lugovskaya N, Vinson DR. Paroxysmal atrial fibrillation and brain freeze: a case of recurrent co‐incident precipitation from a frozen beverage. Am J Case Rep. 2016;17:23–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Liang Y, Mente A, Yusuf S, et al.; ONTARGET and TRANSCEND Investigators . Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ. 2012;184(16):E857–E866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zhang Y, Zhang S, Liu Z, Zhao X, Yuan Y, Sheng L, et al. Resveratrol prevents atrial fibrillation by inhibiting atrial structural and metabolic remodeling in collagen‐induced arthritis rats. Naunyn Schmiedebergs Arch Pharmacol. 2018;391(11):1179–90. [DOI] [PubMed] [Google Scholar]
- 39. Luyer MD, Habes Q, van Hak R, Buurman W. Nutritional stimulation of the autonomic nervous system. World J Gastroenterol. 2011;17(34):3859–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang S, Zhuang X, Lin X, et al. Low‐carbohydrate diets and risk of incident atrial fibrillation: a prospective cohort study. J Am Heart Assoc. 2019;8(9):e011955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gammone MA, Vicentini A, Riccioni G, Girolamo DEM, D'Aurelio A, D'Orazio N. Food‐related atrial fibrillation? The potential role of biogenic amines in “nutri‐arrhythmias” genesis. Reports. 2019;2(1):1–11. [Google Scholar]
- 42. Maryniak A, Hasiec A, Duda B, Orczykowski M, Szumowski L. Temperament, stress, and atrial fibrillation. Polish Psychological Bull. 2015;46(2):223–7. [Google Scholar]
- 43. Sanchis‐Gomar F, Perez‐Quilis C, Lippi G, Cervellin G, Leischik R, Löllgen H, et al. Atrial fibrillation in highly trained endurance athletes – description of a syndrome. Int J Cardiol. 2017;226:11–20. [DOI] [PubMed] [Google Scholar]
- 44. Armour JA, Murphy DA, Yuan BX, Macdonald S, Hopkins DA. Gross and microscopic anatomy of the human intrinsic cardiac nervous system. Anat Rec. 1997;247(2):289–98. [DOI] [PubMed] [Google Scholar]
- 45. Lu Z, Scherlag BJ, Lin J, Yu L, Guo J‐H, Niu G, et al. Autonomic mechanism for initiation of rapid firing from atria and pulmonary veins: evidence by ablation of ganglionated plexi. Cardiovasc Res. 2009;84(2):245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pappone C, Santinelli V, Manguso F, Vicedomini G, Gugliotta F, Augello G, et al. Pulmonary vein denervation enhances long‐term benefit after circumferential ablation for paroxysmal atrial fibrillation. Circulation. 2004;109(3):327–34. [DOI] [PubMed] [Google Scholar]
- 47. Platt M, Mandapati R, Scherlag BJ, et al. Limiting the number and extent of radiofrequency applications to terminate atrial fibrillation and subsequently prevent its inducibility. Heart Rhythm. 2004;1(Suppl 1):S11. [Google Scholar]
- 48. Calò L, Rebecchi M, Sciarra L, De Luca L, Fagagnini A, Zuccaro LM, et al. Catheter ablation of right atrial ganglionated plexi in patients with vagal paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2012;5(1):22–31. [DOI] [PubMed] [Google Scholar]
- 49. Chiou C, Eble JN, Zipes DP. Efferent vagal innervation of the canine atria and sinus and atrioventricular nodes: the third fat pad. Circulation. 1997;95(11):2573–84. [DOI] [PubMed] [Google Scholar]
- 50. Lu Z, Scherlag BJ, Niu G, Lin J, Fung K‐M, Zhao L, et al. Functional properties of the superior vena cava (SVC)‐aorta ganglionated plexus: evidence suggesting an autonomic basis for rapid SVC firing. J Cardiovasc Electrophysiol. 2010;21(12):1392–9. [DOI] [PubMed] [Google Scholar]
- 51. Calò L, Lamberti F, Loricchio ML, Castro A, Shpun S, Boggi A, et al. Long‐term follow‐up of right atrial ablation in patients with atrial fibrillation: efficacy and impact of a hybrid approach on quality of life. J Cardiovasc Electrophysiol. 2004;15(1):37–43. [DOI] [PubMed] [Google Scholar]
- 52. Calò L, Lamberti F, Loricchio ML, De Ruvo E, Colivicchi F, Bianconi L, et al. Left atrial ablation versus biatrial ablation for persistent and permanent atrial fibrillation: a prospective and randomized study. J Am Coll Cardiol. 2006;47(12):2504–12. [DOI] [PubMed] [Google Scholar]
- 53. Sealy WC, Gallagher JJ, Kasell J. His bundle interruption for control of inappropriate ventricular responses to atrial arrhythmias. Ann Thorac Surg. 1981;32(5):429–38. [DOI] [PubMed] [Google Scholar]
- 54. Prasad SM, Maniar HS, Camillo CJ, Schuessler RB, Boineau JP, Sundt TM 3rd, et al. The Cox maze III procedure for atrial fibrillation: long‐term efficacy in patients undergoing lone versus concomitant procedures. J Thorac Cardiovasc Surg. 2003;126(6):1822–8. [DOI] [PubMed] [Google Scholar]
- 55. La Meir M, Gelsomino S, Luca F, Pison L, Colella A, Lorusso R, et al. Minimal invasive surgery for atrial fibrillation: an updated review. Europace. 2013;15(2):170–82. [DOI] [PubMed] [Google Scholar]
- 56. Driessen AHG, Berger WR, Krul SPJ, et al. Ganglion plexus ablation in advanced atrial fibrillation: the AFACT study. J Am Coll Cardiol. 2016;68(11):1155–65. [DOI] [PubMed] [Google Scholar]
- 57. Driessen AHG, Berger WR, Bierhuizen MFA, et al. Quality of life improves after thoracoscopic surgical ablation of advanced atrial fibrillation: results of the Atrial Fibrillation Ablation and Autonomic Modulation via Thoracoscopic Surgery (AFACT) study. J Thorac Cardiovasc Surg. 2018;155(3):972–80. [DOI] [PubMed] [Google Scholar]
- 58. Lin J, Scherlag BJ, Zhou J, Lu Z, Patterson E, Jackman WM, et al. Autonomic mechanism to explain complex fractionated atrial electrograms (CFAE). J Cardiovasc Electrophysiol. 2007;18(11):1197–205. [DOI] [PubMed] [Google Scholar]
- 59. Katritsis D, Giazitzoglou E, Sougiannis D, Voridis E, Po SS. Complex fractionated atrial electrograms at anatomic sites of ganglionated plexi in atrial fibrillation. Europace. 2009;11(3):308–15. [DOI] [PubMed] [Google Scholar]
- 60. Oliveira M, da Silva N, Cunha P, Ramos R, Marques F, Santos S, et al. Effects of acute autonomic modulation on atrial conduction delay and local electrograms duration in paroxysmal atrial fibrillation. Int J Cardiol. 2011;149(3):290–5. [DOI] [PubMed] [Google Scholar]
- 61. Oral H, Chugh A, Scharf C, et al. Pulmonary vein isolation for vagotonic, adrenergic, and random episodes of paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15(4):402–6. [DOI] [PubMed] [Google Scholar]
- 62. Pachon JC, Pachon EI, Pachon JC, et al. "Cardioneuroablation" – new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF‐ablation. Europace. 2005;7(1):1–13. [DOI] [PubMed] [Google Scholar]
- 63. Pachon JC, Pachon EI, Cunha Pachon MZ, Lobo TJ, Pachon JC, Santillana TG. Catheter ablation of severe neurally meditated reflex (neurocardiogenic or vasovagal) syncope: cardioneuroablation long‐term results. Europace. 2011;13(9):1231–42. [DOI] [PubMed] [Google Scholar]
- 64. Pachon MJC, Pachon MEI, Santillana PTG. Simplied method for vagal effect evaluation in cardiac ablation and electrophysiological procedures. JACC Clin Electrophysiol. 2015;1(5):451–60. [DOI] [PubMed] [Google Scholar]
- 65. Pachon MJC, Pachon MEI, Pachon MJC, et al. A new treatment for atrial fibrillation based on spectral analysis to guide the catheter RF‐ablation. Europace. 2004;6(6):590–601. [DOI] [PubMed] [Google Scholar]
- 66. Hu F, Zheng L, Liang E, et al. Right anterior ganglionated plexus: the primary target of cardioneuroablation? Heart Rhythm. 2019;16(10):1545–51. [DOI] [PubMed] [Google Scholar]
- 67. Aksu T, Guler TE, Bozyel S, Yalin K. Vagal responses during cardioneuroablation on different ganglionated plexi: is there any role of ablation strategy? Int J Cardiol. 2020;304:50–5. [DOI] [PubMed] [Google Scholar]
- 68. Lellouche N, Buch E, Celigoj A, et al. Functional characterization of atrial electrograms in sinus rhythm delineates sites of parasympathetic innervation in patients with paroxysmal atrial fibrillation. J Am Coll Cardiol. 2007;50(14):1324–31. [DOI] [PubMed] [Google Scholar]
- 69. Rebecchi M, de Ruvo E, Strano S, et al. Ganglionated plexi ablation in right atrium to treat cardioinhibitory neurocardiogenic syncope. J Interv Card Electrophysiol. 2012;34(3):231–5. [DOI] [PubMed] [Google Scholar]
- 70. Calò L, Rebecchi M, Sette A, et al. Catheter ablation of right atrial ganglionated plexi to treat cardioinhibitory neurocardiogenic syncope: a long‐term follow‐up prospective study. J Interv Card Electrophysiol. 2020. [DOI] [PubMed] [Google Scholar]
- 71. Kaye DM, Esler M, Kingwell B, McPherson G, Esmore D, Jennings G. Functional and neurochemical evidence for partial cardiac sympathetic reinnervation after cardiac transplantation in humans. Circulation. 1993;88(3):1110–8. [DOI] [PubMed] [Google Scholar]
- 72. Oh S, Zhang Y, Bibevski S, Marrouche NF, Natale A, Mazgalev TN. Vagal denervation and atrial fibrillation inducibility: epicardial fat pad ablation does not have long‐term effects. Heart Rhythm. 2006;3(6):701–8. [DOI] [PubMed] [Google Scholar]
- 73. Bauer A, Deisenhofer I, Schneider R, Zrenner B, Barthel P, Karch M, et al. Effects of circumferential or segmental pulmonary vein ablation for paroxysmal atrial fibrillation on cardiac autonomic function. Heart Rhythm. 2006;3(12):1428–35. [DOI] [PubMed] [Google Scholar]
- 74. Hou Y, Hu J, Po SS, Wang H, Zhang L, Zhang F, et al. Catheter‐based renal sympathetic denervation significantly inhibits atrial fibrillation induced by electrical stimulation of the left stellate ganglion and rapid atrial pacing. PLoS One. 2013;8(11):e78218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Feyz L, Theuns DA, Bhagwandien R, Strachinaru M, Kardys I, Van Mieghem NM, et al. Atrial fibrillation reduction by renal sympathetic denervation: 12 months' results of the AFFORD study. Clin Res Cardiol. 2019;108(6):634–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Atti V, Turagam MK, Garg J, Lakkireddy D. Renal sympathetic denervation improves clinical outcomes in patients undergoing catheter ablation for atrial fibrillation and history of hypertension: a meta‐analysis. J Cardiovasc Electrophysiol. 2019;30(5):702–8. [DOI] [PubMed] [Google Scholar]
- 77. Chen PS, Chen LS, Fishbein MC, Lin SF, Nattel S. Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res. 2014;114(9):1500–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Stavrakis S, Humphrey MB, Scherlag BJ, Hu Y, Jackman WM, Nakagawa H, et al. Low‐level transcutaneous electrical vagus nerve stimulation suppresses atrial fibrillation. J Am Coll Cardiol. 2015;65(9):867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Reed JL, Mark AE, Reid RD, Pipe AL. The effects of chronic exercise training in individuals with permanent atrial fibrillation: a systematic review. Can J Cardiol. 2013;29(12):1721–8. [DOI] [PubMed] [Google Scholar]
- 80. Qureshi WT, Alirhayim Z, Blaha MJ, Juraschek SP, Keteyian SJ, Brawner CA, et al. Cardiorespiratory fitness and risk of incident atrial fibrillation: results from the Henry Ford Exercise Testing (FIT) Project. Circulation. 2015;131(21):1827–34. [DOI] [PubMed] [Google Scholar]
- 81. Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62(4):300–5. [DOI] [PubMed] [Google Scholar]
- 82. Wilcox I, Chan KH, Dimitri H. Diagnosis and treatment of obstructive sleep apnea is key to achieving optimal results after catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2014;63(6):607–8. [DOI] [PubMed] [Google Scholar]
- 83. Deng F, Raza A, Guo J. Treating obstructive sleep apnea with continuous positive airway pressure reduces risk of recurrent atrial fibrillation after catheter ablation: a meta‐analysis. Sleep Med. 2018;46:5–11. [DOI] [PubMed] [Google Scholar]
- 84. Mattioli AV, Miloro C, Pennella S, Pedrazzi P, Farinetti A. Adherence to Mediterranean diet and intake of antioxidants influence spontaneous conversion of atrial fibrillation. Nutr Metab Cardiovasc Dis. 2013;23(2):115–21. [DOI] [PubMed] [Google Scholar]
- 85. Ravens U, Odening KE. Atrial fibrillation: therapeutic potential of atrial K+channel blockers. Pharmacol Ther. 2017;176:13–21. [DOI] [PubMed] [Google Scholar]
- 86. Skibsbye L, Poulet C, Diness JG, et al. Small‐conductance calcium‐activated potassium (SK) channels contribute to action potential repolarization in human atria. Cardiovasc Res. 2014;103(1):156–67. [DOI] [PubMed] [Google Scholar]
- 87. Fatkin D, Santiago CF, Huttner IG, Lubitz SA, Ellinor PT. Genetics of atrial fibrillation: state of the art in 2017. Heart Lung Circ. 2017;26(9):894–901. [DOI] [PubMed] [Google Scholar]
- 88. Kevin Donahue J, Heldman AW, Fraser H, McDonald AD, Miller JM, Rade JJ, et al. Focal modification of electrical conduction in the heart by viral gene transfer. Nat Med. 2000;6(12):1395–8. [DOI] [PubMed] [Google Scholar]
- 89. Aistrup GL, Cokic I, Ng J, et al. Targeted non‐viral gene‐based inhibition of Gαi/o‐mediated vagal signaling in the posterior left atrium decreases vagal induced atrial fibrillation. Heart Rhythm. 2011;8(11):1722–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Roberts JD, Marcus GM. Ablatogenomics: can genotype guide catheter ablation for cardiac arrhythmias? Pharmacogenomics. 2016;17(17):1931–40. [DOI] [PubMed] [Google Scholar]


