Abstract
Subtrochanteric (ST) femur fractures are proximal femur fractures, which are often difficult to manage effectively because of their deforming anatomical forces.
Operative management of ST fractures is the mainstay of treatment, with the two primary surgical implant options being intramedullary (IM) nails and extramedullary plates.
Of these, IM nails have a biologic and biomechanical superiority, and have become the gold standard for ST femur fractures.
The orthopaedic surgeon should become familiar and facile with several reduction techniques to create anatomical alignment in all unique ST fracture patterns.
This article presents a comprehensive and current review of the epidemiology, anatomy, biomechanics, clinical presentation, diagnosis, and management of subtrochanteric femur fractures.
Cite this article: EFORT Open Rev 2021;6:145-151. DOI: 10.1302/2058-5241.6.200048
Keywords: femur, intramedullary nail, reduction techniques, subtrochanteric fracture
Introduction
Subtrochanteric (ST) femur fractures are defined as fractures of the proximal femur that occur within 5 cm of the lesser trochanter.1 Overall, the incidence of these fractures has been estimated to be approximately 15–20 per 100,000 individuals.2 The age distribution for these fractures has a bimodal distribution: individuals younger than 40 years old account for approximately 20% of ST fractures, while individuals older than 50 years account for over 2/3 of ST fractures.3 At younger ages, the incidence of these fractures appears to be nearly equal between male and female; however, with increasing age, the incidence among females increases disproportionately to males.3 Additional ST fracture risk factors include patients undergoing treatment of osteoporosis with bisphosphonates, low total bone mineral density, and chronic diseases such as diabetes mellitus.4
Anatomy
To properly diagnose and treat ST fractures, orthopaedic surgeons must have a comprehensive understanding of the relevant anatomy. The ST area comprises the meta-diaphyseal proximal femur within 5 cm distal to the lesser trochanter. The femoral calcar provides significant structural integrity to the proximal femur. It is the dense posteromedial bone that extends from distal to the lesser trochanter to the posteroinferior femoral neck. Biomechanically, the calcar can experience greater than 1000 Newtons of force upon standing and during gait.5 The subtrochanteric region also experiences secondary forces from the numerous muscular attachments found in the area, which increase stress around the proximal femur and hip.6 These muscular attachments include the hip abductors, adductors, short external rotators, and iliopsoas.
Biomechanics
Multiple deforming forces act on both the proximal and distal fragments of these fractures to create a characteristic deformity. On the proximal fragment, the gluteus medius and gluteus minimus cause abduction, the iliopsoas causes flexion, and the short external rotators (piriformis, obturator internus, quadratus femoris, and the superior and inferior gemelli) cause external rotation. On the distal fragment, the gracilis and adductor muscles cause an adduction and shortening force (Fig. 1). The culmination of these forces results in the characteristic deformity seen in ST femur fractures of abduction, external rotation, and flexion of the proximal segment and adduction of the distal segment – overall generating a typical fracture pattern of varus and procurvatum. These anatomical deforming forces can present difficulties when attempting to reduce ST fractures intraoperatively.
Fig. 1.
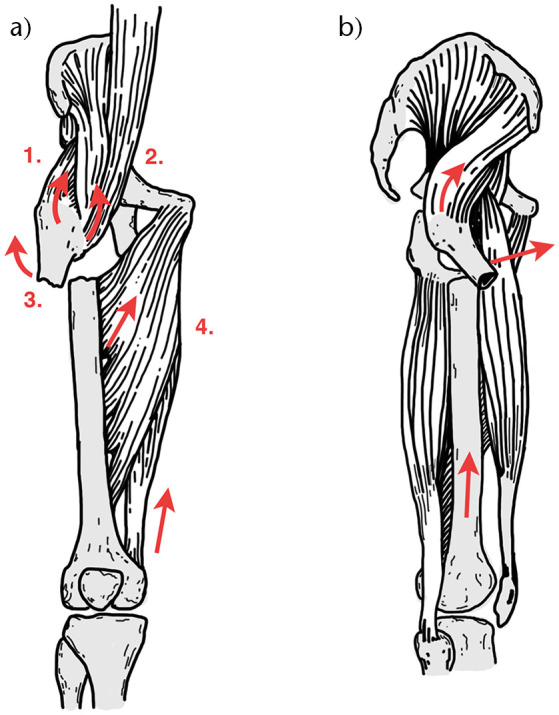
The deforming forces (red arrows) of the proximal and distal fragments in subtrochanteric fractures in the coronal (A) and sagittal (B) planes. The proximal fragment is abducted by the gluteus medius and minimus (1), flexed by the iliopsoas (2), and externally rotated by short external rotators (3). The distal fragment is adducted and shortened by the adductors and gracilis (4).
Classification
Numerous classification systems have been developed for ST femur fractures. The Russell-Taylor classification is based on involvement of the lesser trochanter and fracture extension into the piriformis fossa.7 Prior to the development of a trochanteric entry nail, this was historically used to differentiate fractures amenable to intramedullary (IM) nailing versus those requiring a lateral fixed-angle device. A Russell-Taylor type I fracture has no piriformis fossa extension and would therefore be amenable to fixation via a piriformis entry IM nail. The AO/OTA classification has utility in its universality and is primarily used in the discussion of research.8 It should be noted that there does not yet appear to be an ideal classification system that guides treatment and establishes prognosis with satisfactory interobserver reproducibility.
It is important to identify two specific ST femur fracture patterns that alter management – reverse obliquity fractures and atypical fractures. Reverse obliquity fractures are intertrochanteric or subtrochanteric (depending on the proximal extent of the fracture) injuries that have a primary fracture line from proximal and medial to distal and lateral. Reverse fractures have a tendency of medial shaft migration and high implant failure when treated operatively with a sliding hip screw, and they are most appropriately treated with an IM nail.9,10 Atypical fracture patterns are associated with bisphosphonate use.4,6,11 For atypical femur fractures, the importance in recognizing the underlying primary risk factor stems from the high incidence of bilateral atypical femur fractures, the need to prevent completion of the fracture in the setting of lateral insufficiency with prophylactic fixation, and the recommendation to discontinue bisphosphonates with transition to another agent.11 Common radiologic features of atypical ST femur fractures have been divided into major and minor criteria by the American Society for Bone and Mineral Research. Four of the five major criteria are required to define a fracture as atypical, while minor criteria may or may not be present based on the individual case. Major criteria include low-impact trauma, minimal comminution, fractures originating at the lateral cortex with transverse orientation, lateral cortical thickening, and a medial spike associated with complete fractures.12
Clinical evaluation/presentation
Patients with ST femur fractures present in a bimodal distribution. Subtrochanteric fractures in young patients are typically the result of high-energy trauma such as a motor vehicle collision or fall from height. This mechanism is often associated with other traumatic injuries and should be comprehensively evaluated by a trauma team through the Advanced Trauma Life Support system. Subtrochanteric fractures in elderly patients are typically the result of low-energy trauma, which often presents as an isolated injury. These individuals should undergo a thorough history to assess for comorbid medical conditions and medication history with specific attention to bisphosphonate usage and duration.
Physical examination of the affected limb will typically reveal a shortened and externally rotated lower extremity. Patients will complain of hip and/or thigh pain, along with an inability to bear weight, and pain with hip motion. While these fractures are normally closed injuries, a skin examination should be performed, as a high degree of flexion of the proximal segment may threaten the overlying skin. Physical examination should include assessment of the competence of surrounding neurovascular structures. A complete skeletal survey should be performed to assess for concomitant orthopaedic injuries. After ruling out other ipsilateral lower extremity injuries, patients may be placed into traction, as this will restore fracture length and improve preoperative pain scores.13
Radiographic evaluation
An appropriate radiographic series allows for proper fracture identification and classification, which aids in preoperative planning. Recommended initial radiographic imaging of a patient with suspected ST fracture should include an anteroposterior pelvis, as well as orthogonal femur and knee radiographs. Contralateral femur films may be useful to estimate femoral version, particularly with comminuted fractures that lack cortical reads to judge anatomical reduction. Computed tomography (CT) scans, although not always necessary, are often obtained as part of the initial trauma evaluation. They should be carefully reviewed, as they allow for a more thorough assessment of fracture morphology, including potential proximal fracture extension, which could influence preoperative planning, fracture reduction methods, and implant choice.1 Typical radiographic findings for ST fractures include abduction, external rotation, and flexion of the proximal segment with adduction of the distal segment.
Treatment
Non-operative management of ST fractures is not usually a viable option. Without surgical reduction and fixation, patients have a high risk of symptomatic malunion or nonunion; but more importantly, they are unable to mobilize, resulting in a higher mortality risk.14 The few candidates to consider for non-operative treatment include those who have an unacceptably high mortality risk from anaesthesia, or those who are in hospice care and have minimal hip discomfort. However, due to the benefits of decreased pain and increased mobility, all individuals involved in the medical decision-making process should have a thorough discussion prior to proceeding with non-operative management.15
Operative management of ST fractures can be broadly broken down into two major categories: intramedullary (IM) nailing and extramedullary plating (Fig. 2; Table 1). Of these, the IM nail has become the gold standard of treatment for numerous reasons – decreased hospital length of stay, blood loss, and overall operative time; immediate weight-bearing; and improved functional outcomes.21,22 Recent data from the Swedish registry show that the overwhelming majority (1989/2288, or 87%) of ST fractures are being treated with IM nails.23 Intramedullary nails provide a biomechanical advantage with increased stiffness, rigidity, and a shorter moment arm, which translates to a stronger construct and decreased strain experienced by the implant.24 Nail entry point and construct design can affect fracture reduction and stability; therefore, the surgeon should understand the modifiable variables that can improve surgical outcomes.
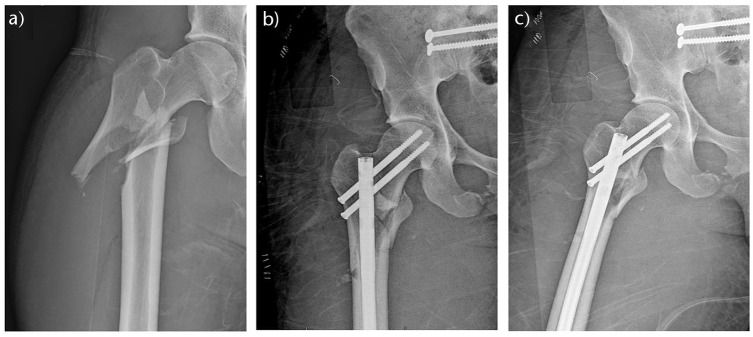
Fig. 2.
Preoperative (A) anteroposterior (AP) and immediate postoperative AP (B) and lateral (C) radiographs of a right subtrochanteric femur fracture with intertrochanteric extension that was treated with a piriformis entry reconstruction nail.
Table 1.
Current evidence on subtrochanteric femur fractures
| Study | Study type | No. of patients | Fracture type and observation | Results |
|---|---|---|---|---|
| Freigang et al16 | Retrospective radio-morphometric case control study | 61 | Subtrochanteric femur fractures; uncomplicated healing within 6 months postoperatively vs. delayed union | At 6 months 29/61 (47.5%) rated healed, 32/61(52.5%) rated delayed union. In total 9/61(14.8%) required revision. At 12 months 48/61 (78.7%) rated healed without further intervention. |
| Xie et al 17 | Meta-analysis | 625 | Subtrochanteric femur fractures; outcomes of intramedullary fixation vs. extramedullary fixation | Intramedullary fixation achieved shorter operation time, less intraoperative blood loss, shorter length of incision, and shorter length of stay. No significant difference for union time, rate of infection, rate of refracture, and rate of nonunion. |
| Horner et al18 | Prospective study | 644 | Subtrochanteric and Intertrochanteric femur fracture; implant-related complications and mortality | Implant-related complication 9.9%. Most common complications included peri-implant fracture (4.2%), proximal thigh pain requiring implant extraction (2.0%), and lag-screw cutout (1.1%). 30-day mortality 9.5%. |
| Zhang et al19 | Randomized controlled trial | 180 | Comminuted subtrochanteric femur fracture; compare the efficacy and safety of the proximal femoral anatomical locking compression plate vs. proximal femoral nail antirotation | Femur intramedullary nail resulted in better recovery of hip function good and excellent Harris hip scores (p < .05). There was no significant difference in complication rate (p > .05). |
| Hoskins et al20 | Retrospective review | 134 | Subtrochanteric fractures; Cerclage wire use improved fracture displacement (3.2 mm vs. 8.8 mm), angulation and quality of reduction (p < 0.05). | Open reduction and the use of cerclage did not produce a negative effect in terms of fracture union. |
Regarding nail entry point, the surgeon has the choice between a piriformis or trochanteric entry point. The incision for both entry portals should be made proximal and in line with the curved axis of the femoral canal to avoid the superior gluteal nerve.25 This posterior incision also allows for passage of the entry wire in a posterior to anterior direction, in line with the anatomical bow of the femur, which reduces the risk of sagittal plane eccentric reaming of the proximal fragment. The piriformis entry portal has an inherent advantage in that it is a straight nail that is in line with the coronal axis of the femoral intramedullary canal.26,27 This collinear advantage results in a decreased risk of varus malreduction and decreased risk of eccentric medial cortex reaming.28,29,30,31 However, the piriformis starting point is more challenging in obese patients, and there is an increased risk for anterior cortical blowout with excessive anterior placement.32 The greater trochanter is the alternative entry portal for treating ST fractures with IM nails. Although the trochanteric portal may minimally decrease soft tissue dissection due to its more superficial location, it does violate the abductor insertion. In addition, the trochanteric entry point carries a greater concern for varus malreduction and presents a high degree of variability based on individual patient trochanteric anatomy.33,34 Overall, the entry point decision should be made on an individualized basis, taking into consideration relevant patient anatomy, surgeon preference, fracture characteristics, and extension of the fracture pattern.
When treating ST femur fractures, the ideal nail is an antegrade, statically and distally locked cephalomedullary nail that allows for added proximal fixation in the femoral neck and head. A large cephalomedullary screw or helical blade can be utilized; however, these provide more utility in intertrochanteric fractures by providing compression at the fracture site. Alternatively, using two smaller diameter reconstruction-style screws decreases the bone removal in the femoral neck and head, while still providing adequate proximal fixation. Additional advantageous nail characteristics are a larger proximal diameter and full-length nails. This strengthens the construct by improving rotational and axial stability and decreases the risk of post-implant fractures when compared to the use of short nails.35 The use of two distal interlocking screws has been demonstrated to provide greater rotational and axial stability than one.36
The second major category of operative fixation for ST fractures is the use of locking or fixed-angle extramedullary plates. Placement of fixed-angle blade plates presents a high degree of technical difficulty. This factor, coupled with decreased rates of union, increased operative time, increased time until weight-bearing, and increased infection rates compared to IM nailing has led to a decreased use of fixed-angle plates.15,37 Using a locking plate compared to a fixed-angle blade plate has demonstrated better biomechanical properties. However, this construct was shown by Collinge et al to result in failed fixation, malalignment/malunion, deep infection, or a combination of these factors in over 40% of patients. Of these patients, over 1/3 underwent a secondary revision surgery.38 There is utility, however, in extramedullary plating, particularly when using a small fragment plate for provision fixation when open reduction is required. Malunion rates have been reported to drop from 27% to 0% when using this provisional plating technique.21
Reduction strategies and techniques
Due to the deforming forces in ST fractures, several techniques can be considered to achieve proper anatomic reduction. These reduction techniques include the use of clamps, a ball spike pusher with a bone hook, percutaneous Schanz pin joysticks, a femoral distractor, a finger reduction tool, blocking wires or screws, and cerclage wiring.39,40,41 Positioning of the patient prior to reduction should be based on the surgeon’s familiarity and preference, as each carries distinct advantages and disadvantages. The lateral decubitus position can allow for easier entry portal access via adduction of the ipsilateral leg in more obese patients, for example. This position also allows for easier reduction of the distal fragment. The supine position is familiar to most surgeons, is superior in the case of polytrauma by providing access to other extremities, and is protective of an injured spine.
For many ST fractures, the use of clamps can be considered to assist in maintaining reduction (Fig. 3). The use of this technique has demonstrated excellent reductions and a high union rate.42 For simpler two-segment ST fractures, devices such as percutaneous Schanz pin joysticks or the ball spike pusher and bone hook can be utilized to align the fragments and allow for proper placement of a guide wire.43 Schanz pins can also be coupled with a femoral distractor to establish length and to lock the reduction into place once proper alignment has been achieved. Another tool that can be of significant use for two-segment ST fractures is the finger reduction tool (Fig. 4). While length is typically improved with longitudinal traction, varus malalignment typically persists despite traction due to the proximal insertion of the abductors and the distal insertion of the adductors. In this case, passing a finger reduction tool can be utilized to gain control of the proximal fragment and correct the varus malalignment. Improper starting point or path of the guide wire can result in eccentric reaming, potentially resulting in cortical blowout or malreduction of a previously aligned reduction. For more complex fracture patterns with comminution or those with distal extension, blocking wires or screws can be placed on the concavity of the deformity in the proximal segment to maintain reduction and stiffen the construct (Fig. 5).24 Although there is concern for disruption of the femoral blood supply, the use of percutaneous cerclage wiring has also been shown to be an effective and safe reduction method.40,41
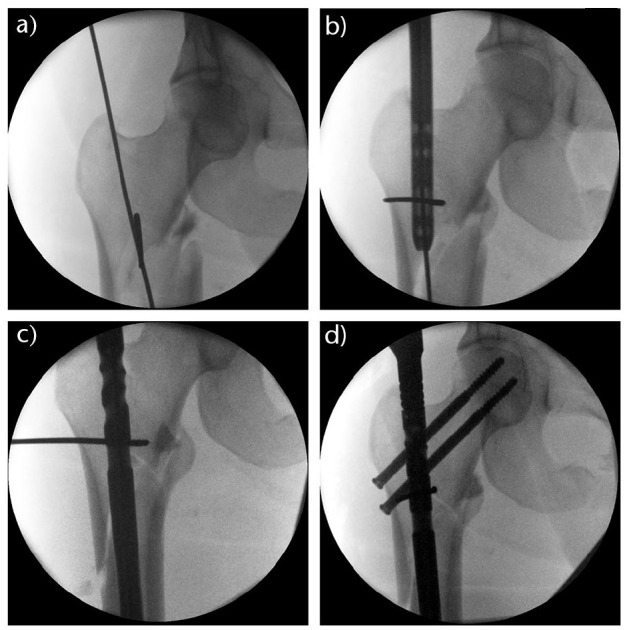
Fig. 3.
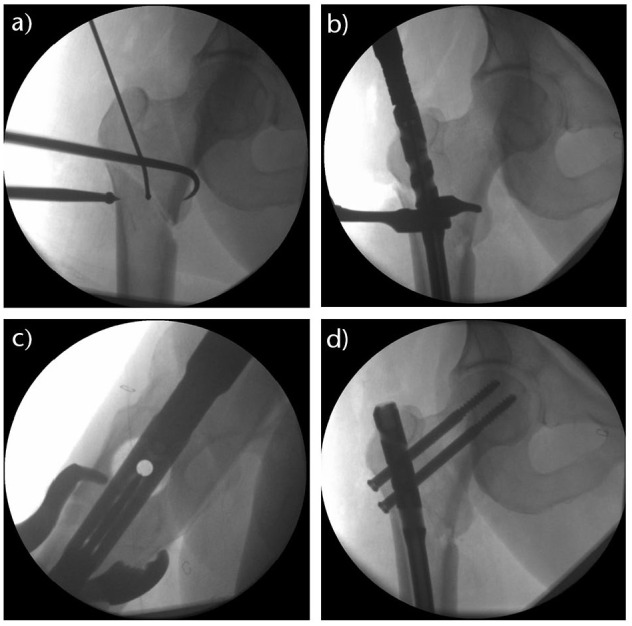
Use of a ball spike pusher to medialize the distal fracture fragment while simultaneously pulling the proximal fragment with a bone hook to address the varus fracture deformity (A). After the guidewire was placed, a clamp was utilized to maintain the reduction in the coronal (B) and sagittal (C) planes. Anatomical reduction was achieved and the subtrochanteric femur fracture was fixed with a trochanteric entry reconstruction nail (D).
Fig. 4.
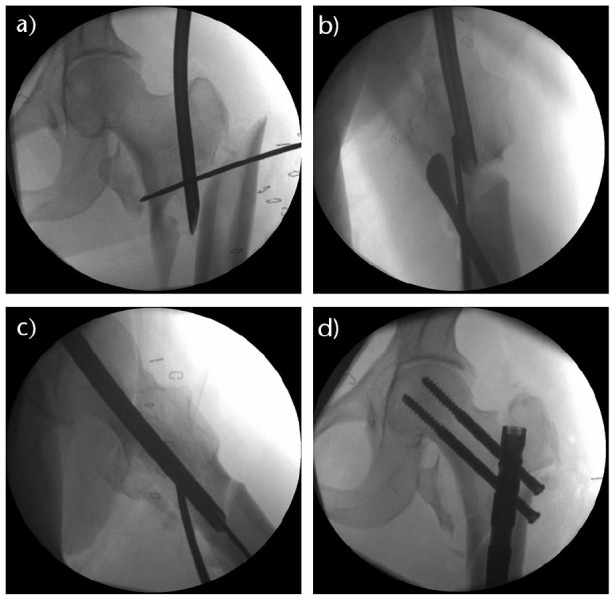
Multiple reduction techniques were used to address this complex subtrochanteric femur fracture with intertrochanteric extension. The finger reduction tool was placed into the piriformis fossa entry portal to gain control of the proximal fragment (A). A Cobb periosteal elevator and a posterior blocking wire were utilized to correct the sagittal plane deformity (B). The finger reduction tool was then passed to the level of the distal fragment to allow for passage of the guidewire (C). Anatomical reduction was achieved and maintained with a piriformis entry reconstruction nail (D).
Fig. 5.
A blocking wire was placed in the concavity of the deformity in the proximal fracture fragment just medial to the guidewire and was left in place during reaming to guide the reaming of the proximal fragment (A). As the nail was passed (B), the blocking wire effectively lateralized the distal segment (C) and created an anatomical reduction that was maintained with a piriformis entry reconstruction nail (D).
Complications
Operative complications for ST fractures are similar to the complications found in other proximal femur fractures, and include malunion, nonunion, infection, implant breakage, and mortality.44 Mortality rates for ST fractures have been shown at 30 days, one year, and four years to be approximately 9.5%, 27%, and 60%, respectively.18 One of the most common complications of ST fracture fixation is that of a varus and procurvatum malunion or nonunion.45 This risk is primarily linked to improper intraoperative anatomical reduction, so the effective use of reduction techniques should improve alignment and minimize union complications. Malunion, in particular, can be associated with rotational errors which may result in gait abnormalities and hip pain.1 Rotational malalignment is particularly prevalent with the use of a traction table, as excessive internal rotation is often used for attempted fracture reduction. This is especially concerning in severely comminuted fractures.1,7 When healed in the typical ST malreduction pattern, excessive varus angulation and flexion of the proximal fragment can negatively alter the patient’s gait mechanics. Symptomatic malunion may require a corrective osteotomy with instrumentation, and nonunion can be effectively managed with exchange of the implants with or without use of bone grafting.15 As with all surgical procedures, infection is a potential risk. Superficial infections can typically be managed with antibiotics alone. However, deep infections require surgical irrigation and debridement and possible implant removal. In the setting of an infected nonunion, the implants are removed and replaced with an antibiotic intramedullary implant, along with long-term intravenous (IV) or oral antibiotics.15
Conclusion
Subtrochanteric femur fractures are challenging orthopaedic injuries due to their complex and powerful deforming forces, which create significant difficulty in fracture reduction and implant fixation. As operative management remains the definitive treatment of choice for ST femur fractures, it is imperative to understand these forces and the techniques to properly reduce these fractures in order to improve alignment, stability, and patient outcomes.
Footnotes
ICMJE Conflict of interest statement: The other authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Joglekar SB, Lindvall EM, Martirosian A. Contemporary management of subtrochanteric fractures. Orthop Clin North Am 2015;46:21–35. [DOI] [PubMed] [Google Scholar]
- 2. Dell RM, Adams AL, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012;27:2544–2550. [DOI] [PubMed] [Google Scholar]
- 3. Ng AC, Drake MT, Clarke BL, et al. Trends in subtrochanteric, diaphyseal, and distal femur fractures, 1984–2007. Osteoporos Int 2012;23:1721–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Napoli N, Schwartz AV, Palermo L, et al. Risk factors for subtrochanteric and diaphyseal fractures: the study of osteoporotic fractures. J Clin Endocrinol Metab 2013;98:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koch JC. The laws of bone architecture. Am J Anat 1917;21:177–211. [Google Scholar]
- 6. Nordin M, Frankel VH. Basic biomechanics of the musculoskeletal system. Baltimore, MD: Lippincott Williams & Wilkins, 2012. [Google Scholar]
- 7. Bedi A, Toan Le T. Subtrochanteric femur fractures. Orthop Clin North Am 2004;35:473–483. [DOI] [PubMed] [Google Scholar]
- 8. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32:S1–S170. [DOI] [PubMed] [Google Scholar]
- 9. Hiragami K, Ishii J. Embedding the lateral end of the lag screw within the lateral wall in the repair of reverse obliquity intertrochanteric femur fracture. J Int Med Res 2018;46:1103–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am 2001;83:643–650. [DOI] [PubMed] [Google Scholar]
- 11. Shah A, Shah M. Functional outcomes of subtrochanteric femur fractures treated by intramedullary proximal femur nail. Int J Orthop Sci 2017;3:876–881. [Google Scholar]
- 12. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1–23. [DOI] [PubMed] [Google Scholar]
- 13. Bumpass DB, Ricci WM, McAndrew CM, Gardner MJ. A prospective study of pain reduction and knee dysfunction comparing femoral skeletal traction and splinting in adult trauma patients. J Orthop Trauma 2015;29:112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chlebeck JD, Birch CE, Blankstein M, Kristiansen T, Bartlett CS, Schottel PC. Nonoperative geriatric hip fracture treatment is associated with increased mortality: a matched cohort study. J Orthop Trauma 2019;33:346–350. [DOI] [PubMed] [Google Scholar]
- 15. Koval KJ, Rezaie N, Yoon RS. Subtrochanteric femur fractures. In: Egol KA, Leucht P, eds. Proximal femur fractures. Cham: Springer, 2018:101–112. [Google Scholar]
- 16. Freigang V, Gschrei F, Bhayana H, et al. Risk factor analysis for delayed union after subtrochanteric femur fracture: quality of reduction and valgization are the key to success. BMC Musculoskelet Disord 2019;20:391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xie H, Xie L, Wang J, Chen C, Zhang C, Zheng W. Intramedullary versus extramedullary fixation for the treatment of subtrochanteric fracture: a systematic review and meta-analysis. Int J Surg 2019;63:43–57. [DOI] [PubMed] [Google Scholar]
- 18. Horner NS, Samuelsson K, Solyom J, Bjørgul K, Ayeni OR, Östman B. Implant-related complications and mortality after use of short or long Gamma nail for intertrochanteric and subtrochanteric fractures: a prospective study with minimum 13-year follow-up. JB JS Open Access 2017;2:e0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang JR, Xiong SX, Tian XL, Gao FM, Lin C, Yang LX. Efficacy and safety of proximal femoral anatomical locking compression plate and proximal femoral nail antirotation for long-segment comminuted subtrochanteric fractures of the femur: a non-randomized controlled trial. Clin Trials Orthop Disord 2019;4:8–16. [Google Scholar]
- 20. Hoskins W, Bingham R, Joseph S, et al. Subtrochanteric fracture: the effect of cerclage wire on fracture reduction and outcome. Injury 2015;46:1992–1995. [DOI] [PubMed] [Google Scholar]
- 21. Robertson R, Tucker M, Jones T. Provisional plating of subtrochanteric femur fractures before intramedullary nailing in the lateral decubitus position. J Orthop Trauma 2018;32:e151–e156. [DOI] [PubMed] [Google Scholar]
- 22. Brumback RJ, Toal TR, Jr, Murphy-Zane MS, Novak VP, Belkoff SM. Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J Bone Joint Surg Am 1999;81:1538–1544. [DOI] [PubMed] [Google Scholar]
- 23. Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord 2018;19:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang J, Ma XL, Ma JX, et al. Biomechanical analysis of four types of internal fixation in subtrochanteric fracture models. Orthop Surg 2014;6:128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lowe JA, Min W, Lee MA, Wolinsky PR. Risk of injury to the superior gluteal nerve when using a proximal incision for insertion of a piriformis-entry reamed femoral intramedullary nail: a cadaveric study. J Bone Joint Surg Am 2012;94:1416–1419. [DOI] [PubMed] [Google Scholar]
- 26. Gausepohl T, Pennig D, Koebke J, Harnoss S. Antegrade femoral nailing: an anatomical determination of the correct entry point. Injury 2002;33:701–705. [DOI] [PubMed] [Google Scholar]
- 27. Harper MC, Carson WL. Curvature of the femur and the proximal entry point for an intramedullary rod. Clin Orthop Relat Res 1987;220:155–161. [PubMed] [Google Scholar]
- 28. Nicolaou D, Watson JT. Nailing proximal femur fractures: how to choose starting point and proximal screw configuration. J Orthop Trauma 2015;29:S22–S27. [DOI] [PubMed] [Google Scholar]
- 29. Ostrum RF, Marcantonio A, Marburger R. A critical analysis of the eccentric starting point for trochanteric intramedullary femoral nailing. J Orthop Trauma 2005;19:681–686. [DOI] [PubMed] [Google Scholar]
- 30. Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures: a report of five hundred and twenty cases. J Bone Joint Surg Am 1984;66:529–539. [PubMed] [Google Scholar]
- 31. Honeycutt MW, Cox K, Cox WT, Delgado G, Brewer J. The effect of intramedullary nail entry point on postoperative femoral shaft fracture alignment [abstract]. In: Orthopaedic Trauma Association 35th Annual Meeting, 2019. September 25–28, Denver, CO. OTA Final Program, 2019. Abstract nr 100. [Google Scholar]
- 32. Johnson KD, Tencer AF, Sherman MC. Biomechanical factors affecting fracture stability and femoral bursting in closed intramedullary nailing of femoral shaft fractures, with illustrative case presentations. J Orthop Trauma 1987;1:1–11. [DOI] [PubMed] [Google Scholar]
- 33. Streubel PN, Wong AH, Ricci WM, Gardner MJ. Is there a standard trochanteric entry site for nailing of subtrochanteric femur fractures? J Orthop Trauma 2011;25:202–207. [DOI] [PubMed] [Google Scholar]
- 34. Antonelli L. Closed intramedullary nailing of diaphyseal fractures of the femur: problems related to anatomical variations of the greater trochanter. Ital J Orthop Traumatol 1989;15:67–74. [PubMed] [Google Scholar]
- 35. Russell TA. Intramedullary nailing: evolutions of femoral intramedullary nailing: first to fourth generations. J Orthop Trauma 2011;25:S135–S138. [DOI] [PubMed] [Google Scholar]
- 36. Lundy DW. Subtrochanteric femoral fractures. J Am Acad Orthop Surg 2007;15:663–671. [DOI] [PubMed] [Google Scholar]
- 37. Brien WW, Wiss DA, Becker V, Jr, Lehman T. Subtrochanteric femur fractures: a comparison of the Zickel nail, 95 degrees blade plate, and interlocking nail. J Orthop Trauma 1991;5:458–464. [PubMed] [Google Scholar]
- 38. Collinge CA, Hymes R, Archdeacon M, et al. ; Members of the Proximal Femur Working Group of the Southeast Trauma Consortium. Unstable proximal femur fractures treated with proximal femoral locking plates: a retrospective, multicenter study of 111 cases. J Orthop Trauma 2016;30:489–495. [DOI] [PubMed] [Google Scholar]
- 39. Yoon RS, Donegan DJ, Liporace FA. Reducing subtrochanteric femur fractures: tips and tricks, do’s and don’ts. J Orthop Trauma 2015;29:S28–S33. [DOI] [PubMed] [Google Scholar]
- 40. Kim JW, Park KC, Oh JK, Oh CW, Yoon YC, Chang HW. Percutaneous cerclage wiring followed by intramedullary nailing for subtrochanteric femoral fractures: a technical note with clinical results. Arch Orthop Trauma Surg 2014;134:1227–1235. [DOI] [PubMed] [Google Scholar]
- 41. Tomás J, Teixidor J, Batalla L, Pacha D, Cortina J. Subtrochanteric fractures: treatment with cerclage wire and long intramedullary nail. J Orthop Trauma 2013;27:e157–e160. [DOI] [PubMed] [Google Scholar]
- 42. Afsari A, Liporace F, Lindvall E, Infante A, Jr, Sagi HC, Haidukewych GJ. Clamp-assisted reduction of high subtrochanteric fractures of the femur: surgical technique. J Bone Joint Surg Am 2010;92:217–225. [DOI] [PubMed] [Google Scholar]
- 43. Kim KC, Lee JK, Hwang DS, Yang JY, Kim YM. Stabilizing subtrochanteric femoral fractures with an interlocked intramedullary nail using the ‘Joystick’ technique. Orthopedics 2007;30:705–708. [DOI] [PubMed] [Google Scholar]
- 44. Damany D, Parker M, Gurusamy K, Upadhyay P. Complications of subtrochanteric fractures: a meta-analysis of 39 studies involving 1835 Fractures. Orthop Proc 2018;88-B:168. [Google Scholar]
- 45. Lo YC, Su YP, Hsieh CP, Huang CH. Augmentation plate fixation for treating subtrochanteric fracture nonunion. Indian J Orthop 2019;53:246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]