Abstract
Background and Aims:
Anesthesia in obese patients is difficult due to associated comorbidities and altered physiology. Desflurane and sevoflurane have a low fat-blood solubility coefficient and are better suited in these patients to achieve a rapid emergence. We studied BIS guided drug titration to compare the postoperative recovery characteristics and cognitive function of desflurane versus sevoflurane in obese patients undergoing laparoscopic abdominal surgeries.
Material and Methods:
After institutional ethics committee approval and written informed consent, sixty obese patients (BMI ≥30 kg/m2) were randomized to receive either BIS guided desflurane or sevoflurane. Recovery was assessed by time taken for eye opening on verbal command, sustained head lift for 5 s, and extubation and orientation to time, place, and person after discontinuation of volatile anesthetic agent. For cognitive function, time taken to complete Mini mental state examination (MMSE) score to baseline was compared in both study groups.
Results:
Difference of time taken for eye opening on verbal command, sustained head lift for 5 s, and extubation and orientation to time, place, and person was not significant between both anesthetic groups. Patients in sevoflurane group took significantly (P-value = 0.001) less time (40.07 ± 13 min) to achieve preoperative MMSE score than desflurane group (51.2 ± 11.7 min).
Conclusion:
Both desflurane and sevoflurane have similar recovery profile in obese patients when anesthetic concentration is carefully titrated. Reversal of cognitive function is significantly earlier in obese patients anesthetized with sevoflurane.
Keywords: Anesthesia for obese, desflurane, inhalational agents, sevoflurane, recovery characteristics
Introduction
A favorable outcome after general anesthesia in obese patients can be achieved once these patients are awake, conscious, pain free, hemodynamically stable and are able to maintain their respiratory functions postoperatively.
All volatile anesthetics accumulate in adipose tissues and skeletal muscles which delays recovery from anesthesia as the anesthetic agent stored in fat returns to blood perfusing the fat or to its adjacent highly perfused tissues (e.g., omental/mesenteric fat to intestine and liver).[1] Desflurane and sevoflurane have significantly lower blood/gas partition coefficients (0.45 and 0.65, respectively) which allows for rapid titration and emergence at the end of surgery.
Desflurane has been associated with faster emergence time when compared to isoflurane in the obese patient,[2] which would be expected based on lower blood-gas and fat-blood solubility coefficient; however, only a little data is available on its comparison with sevoflurane in obese patients. Sevoflurane also has a lower blood-gas solubility and a faster emergence profile compared with isoflurane in the obese patient, despite similar fat-blood solubility.[3,4] These findings lead to speculation that blood-gas solubility, rather than fat solubility, may be the dominant force influencing the speed of recovery in obese patients.
The trend of laparoscopic abdominal surgeries is increasing in today's era as these are associated with improved surgical outcome, reduced postoperative complications like pain, infections, and decreased duration of hospital stay.[5] To have a better outcome of laparoscopic surgeries in obese patients, the importance lies in the choice of more desirable anesthetic agent for induction and emergence. Hence, we conducted this prospective, randomized single-blind study to find out a more desirable inhalational anesthetic agent in regards to recovery profile indices and cognitive function of obese patients undergoing laparoscopic abdominal surgeries.
Material and Methods
After institutional ethics committee approval, CTRI registration (CTRI/2017/10/010268) and written informed patient consent, sixty American Society of Anesthesiologists (ASA) grade II and III obese patients with Body Mass Index (BMI) ≥30 kg/m2 scheduled to undergo laparoscopic abdominal surgeries were enrolled for the study. Patients were randomized by computer-generated random numbers table contained in sealed envelopes into two groups of 30 patients each, to receive either desflurane (group D) or sevoflurane (group S) for maintenance of anesthesia. Volatile anesthetic concentration was titrated to maintain electroencephalographic bispectral index (BIS) value 50 ± 5. Exclusion criteria included ASA III patients with severe obstructive or restrictive pulmonary disease, hepatic disease, end-stage renal disease, history of myocardial infarction, coronary artery disease and stroke, history of allergy to study drugs, susceptible to malignant hyperthermia, disabling disease of CNS or with use of any investigational drug within 30 days before surgery.
Preanesthetic examination comprised of detailed history and systemic examination related to obesity. Cognitive function was assessed by Mini mental state examination (MMSE) [Table 1], with which all patients were familiarized and a baseline value of MMSE was obtained. All the patients were kept nil orally for at least 8 h prior to surgery. The night before surgery, patients were given tab ranitidine hydrochloride 150 mg, tab metoclopramide 10 mg, and tab alprazolam 0.25 mg per oral. Injection enoxaparin 40 mg subcutaneous was given for deep vein thrombosis prophylaxis.
Table 1.
Mini Mental State Examination (MMSE)
| Maximum Score | |
|---|---|
| 5 | Orientation |
| What is the (year) (season) (date) (day) (month)? | |
| 5 | Where are we (state) (country) (town) (hospital) (floor)? |
| 3 | Registration |
| Name 3 objects and asks the patient to repeat the same. Give 1 point for each correct answer. Then repeat until he/she learns all 3. Count trials. | |
| 5 | Attention and Calculation |
| Subtract 100-7=93-7=86-7=79-7=72-7=65 | |
| 3 | Recall |
| Ask the 3 objects repeated above. Give 1 point for each correct answer. | |
| 2 | Language |
| Name a watch and pen. | |
| 1 | Repeat I m a Human Being. |
| 3 | Follow a 3-stage command: “Take the piece of paper with your right hand, fold it in half, and put it on the floor.” |
| 1 | Read and obey: CLOSE YOUR EYES. |
| 1 | Write a sentence. |
| 1 | Copy the design shown. |

|
|
| 30 | Total |
In the operation theater, difficult airway cart was kept ready for all patients. BIS monitor and other standard monitors were applied and patients were positioned on a ramp made up of sheets kept under the shoulders and head so as to bring the tragus in line with sternal notch. After preoxygenation with 100% oxygen for 5 min, anesthesia was induced with 1-2 μg/kg lean body weight (LBW) of fentanyl and 1-2 mg/kg LBW of propofol followed by 0.1 mg/kg total body weight (TBW) of cis-atracurium besylate, to facilitate tracheal intubation with an appropriately sized endotracheal tube. Positive pressure ventilation was initiated and maintained for the duration of surgery with a tidal volume of 6-7 ml/kg. Ventilator rate was adjusted to maintain an end-tidal pCO2 of 30–40 mmHg.
Anesthesia was maintained according to the BIS value between 50 ± 5 with sevoflurane or desflurane in oxygen/air mixture with a fresh gas flow of 1-2 L/min. Neuromuscular block was maintained with 0.02 mg/kg of cis-atracurium besylate to have zero twitch on train of four (TOF) monitoring which was applied post-induction. Additional fentanyl boluses (0.5–0.75 μg/kg) were given to maintain analgesia. Continuous monitoring of HR, BP, SpO2, etCO2, BIS, and TOF was done. Inhalational agent was titrated to BIS value of 60–70 during last 15 min of surgery and injection ondansetron (0.1 mg/kg TBW) was given. Anesthesia was discontinued after the last stitch was done. Neuromuscular block was reversed with neostigmine bromide (0.05 mg/kg TBW) and glycopyrrolate (0.08 mg/kg TBW) when a TOF ratio of 0.7 was reached.[6,7] Trachea was extubated on return of spontaneous breathing with a minimum tidal volume of 6–8 ml/kg.
Recovery was assessed by investigator by recording the time taken for eye opening on verbal command, sustained head lift for 5 s, and extubation and orientation to time, place, and person after discontinuation of volatile anesthetic agent. In post anesthesia care unit (PACU), the MMSE score of the patient was calculated on arrival, and then at 15 min interval till he/she attained the baseline MMSE score.
All statistical analysis was done using SPSS computer software version 21. To summarize the data, we used descriptive analysis. Parametric data were expressed as mean values ± standard deviation (SD). The Chi-square test was used for categorical variables and the Student's t-test for continuous variables. P value <0.05 was considered statistically significant. Post hoc power analysis showed that with a sample size of 60 and effect size of 1.11 with 10% chance of error, the power of the study was 0.97.
Results
All 60 patients recruited for the study successfully completed the required assessments as per the protocol. The two study groups were comparable with respect to age, gender, weight, height, body mass index, lean body weight, and preoperative vital parameters [Table 2].
Table 2.
Patient characteristics
| Mean±SD | P | 95% Confidence Interval of Difference | |||
|---|---|---|---|---|---|
| Sevoflurane | Desflurane | Lower | Upper | ||
| Age (years) | 49.7±13.3 | 50.9±8.8 | 0.689 | -6.975 | 4.641 |
| Gender (M/F) | 9/21 | 10/20 | 0.781 | ||
| Weight (kg) | 95.5±15.8 | 99.4±20.9 | 0.416 | -13.49 | 5.657 |
| Height (m) | 1.6±0.1 | 1.6±0.1 | 0.756 | -0.049 | 0.036 |
| BMI (kg/m2) | 37.5±5.6 | 38.0±6.2 | 0.757 | -3.547 | 2.595 |
| LBW | 53.5±9.7 | 52.6±9.7 | 0.743 | -4.188 | 5.841 |
| SBP (mmHg) | 131.9±16.2 | 130.5±13.5 | 0.898 | 0.867 | 0.973 |
| DBP (mmHg) | 79.9±7.5 | 80.8±8.2 | 0.590 | 0.432 | 0.628 |
| MAP (mmHg) | 97.2±9.3 | 97.4±8.7 | 0.760 | -4.803 | 4.492 |
| Pulse (bpm) | 85.7±8.4 | 82.3±11.1 | 0.189 | -1.707 | 8.440 |
| Respiratory rate (/min) | 20.4±1.9 | 20.4±2.0 | 0.905 | 0.893 | 0.987 |
BMI=Body mass index; LBW=Lean body weight; SBP=Systolic blood pressure; DBP=Diastolic blood pressure; MAP=Mean arterial pressure. Data is expressed as number or mean±SD
After discontinuation of volatile anesthetic agents, the difference of time taken for recovery parameters like eye opening on verbal command, sustained head lift for 5 s, and extubation and orientation to time, place, and person was not significantly different in the two study groups [Figure 1].
Figure 1.
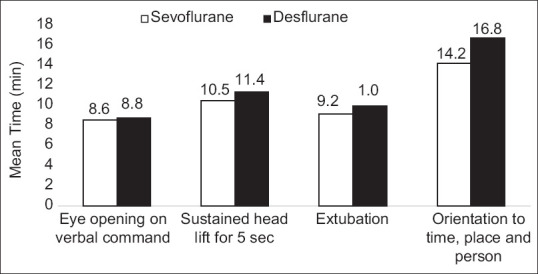
Comparison of mean time taken for various recovery parameters after discontinuation of volatile anesthetics in sevoflurane and desflurane group (P> 0.05)
In sevoflurane group, time taken to attain baseline MMSE score after discontinuation of volatile anesthetic agents was significantly shorter as compared to desflurane group [Table 3].
Table 3.
Time taken to attain baseline MMSE after discontinuation of volatile anesthetics
| Time taken for completion of MMSE to baseline (min) | t | P | 95% Confidence Interval of the Difference | |||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Sevoflurane | Mean | 40.1 | ||||
| SD | 13.0 | -3.484 | 0.001 | -17.529 | -4.737 | |
| Desflurane | Mean | 51.2 | ||||
| SD | 11.7 | |||||
Discussion
Demographic distribution in our study revealed similar mean age and gender distribution in both the groups. Our study population showed a predominance of female patients (68%) indicating that obesity is more prevalent among them which was in accordance with other authors.[8,9] Mean BMI of patients in group S was 37.5 ± 5.6 kg/m2 and in group D it was 38.0 ± 6.2 kg/m2 [Table 1], which was comparable to the study of Arain et al.[10] Both study groups were comparable in terms of BMI and lean body mass.
We found that both volatile agents were similar in term of time taken for eye opening which was in accordance with previous reports.[10,11] In contrast, De Baerdemaeker et al.[12] had shown that eye opening occurred earlier in obese patients anesthetized with desflurane as compared to sevoflurane. This difference was because in their technique of emergence, mechanical ventilation was continued for 2 min after the end of surgery and cessation of volatile anesthetic agent. If the patient was not spontaneously breathing, then 1 rescue breath would be administered every 30 s. If a patient did not quickly resume spontaneous breathing, emergence would have been delayed by a decreased minute ventilation and alveolar washout of the anesthetic gas. In their study, no patient in the sevoflurane group was spontaneously breathing after 2 min, whereas approximately 20% of the desflurane group were spontaneously breathing. Although the average time until spontaneous respiration between desflurane and sevoflurane groups was not significantly different, the small early difference in minute ventilation may have been important in generating a 2 min difference of time taken for eye opening. In our technique, we continued mechanical ventilation until spontaneous respiration began and, thus, patients maintained comparable minute ventilations in the early anesthetic elimination period.
In our study population, sustained head lift for 5 s after discontinuation of volatile anesthetic agent occurred at similar times. None of the previous studies had compared the time taken for sustained head lift in obese patients; hence, more studies are required to assess the effect of different volatile agents on this recovery parameter.
Another recovery parameter, time taken for extubation after discontinuation of volatile anesthetic agent was similar in the two group which was in line with a previous study,[10] whereas Strum et al.[8] advocate the use of desflurane for early extubation in obese patients. But unlike our study, they used MAC equivalents of the two inhalational agents. The use of MAC as a guide to titrate volatile anesthetics can result in either under or over dosing.[13] Multiple confounding factors can also affect the MAC in individual patients. Instead of using MAC equivalent doses of sevoflurane or desflurane, we used BIS, which is a quantifiable measure of sedative and hypnotic effects of inhaled anesthetics, and an indicator of adequate anesthesia. BIS values between 40 and 60 correlate well with clinical endpoints of sedation and loss of consciousness and are relatively agent independent.[14]
Difference of time taken for orientation to time, place, and person after discontinuation of volatile anesthetic agent in both groups was not different (P-value = 0.072) which was similar to findings of Arain et al.[10] indicating that none of the two inhalational agents was superior to other for early orientation. However, a meta-analysis including five trials showed that use of desflurane in morbidly obese patients allows attaining faster verbal contact as compared to sevoflurane.[15]
We assessed the post anesthesia recovery of cognitive function by time taken to attain baseline MMSE score after discontinuation of volatile anesthetic agent. Our study revealed that patients in sevoflurane group took much less time (40.1 ± 13 min) to complete MMSE score than desflurane group (51.2 ± 11.7 min; P-value = 0.001) [Table 3]. Hence, in our study, recovery of cognitive function occurred early in obese patients when sevoflurane was used; however, none of the previous studies had such finding. In contrast Bilotta et al.[16] showed that in obese patients undergoing craniotomy, desflurane-based anesthesia allowed earlier postoperative cognitive recovery; however, they used Short Orientation Memory Concentration Test and Rancho Los Amigos Scale instead of MMSE to assess cognitive function and their study population consists of patients undergoing craniotomy for supratentorial expanding lesions. In another study, Arain et al.[10] found no difference in recovery of cognitive function assessed by MMSE after desflurane and sevoflurane anesthesia in morbidly obese patients, but they conducted this study in patients undergoing a variety of surgical procedures including orthopedic surgery of extremities, hip arthroplasty, and spine surgery. Mean age of patients in their study was more than that of ours and consisted of 92% (36/39) males, while our study had female predominance. Although the findings of different studies are conflicting and we could not find any study on recovery of cognitive function in obese patients undergoing laparoscopic abdominal surgery, we suggest that sevoflurane is better for early cognitive recovery in obese patients undergoing laparoscopic abdominal surgery.
Conclusions
There were no differences in emergence and recovery profiles of obese patients undergoing laparoscopic abdominal surgeries receiving desflurane or sevoflurane. However, cognitive recovery assessed by MMSE was significantly earlier with sevoflurane. Thus, we recommend the use of sevoflurane for early cognitive recovery in obese patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Carpenter RL, Eger EI, 2nd, Johnson BH, Unadkat JD, Sheiner LB. Pharmacokinetics of inhaled anesthetics in humans: Measurements during and after the simultaneous administration of enflurane, halothane, isoflurane, methoxyflurane, and nitrous oxide. Anesth Analg. 1986;65:575–82. [PubMed] [Google Scholar]
- 2.Juvin P, Vadam C, Malek L, Dupont H, Marmuse JP, Desmonts JM. Postoperative recovery after desflurane, propofol, or isoflurane anesthesia among morbidly obese patients: A prospective, randomized study. Anesth Analg. 2000;91:714–9. doi: 10.1097/00000539-200009000-00041. [DOI] [PubMed] [Google Scholar]
- 3.Sollazzi L, Perilli V, Modesti C, Annetta MG, Ranieri R, Tacchino RM, et al. Volatile anesthesia in bariatric surgery. Obes Surg. 2001;11:623–6. doi: 10.1381/09608920160557138. [DOI] [PubMed] [Google Scholar]
- 4.Torri G, Casati A, Albertin A, Comotti L, Bignami E, Scarioni M, et al. Randomized comparison of isoflurane and sevoflurane for laparoscopic gastric banding in morbidly obese patients. J Clin Anesth. 2001;13:565–70. doi: 10.1016/s0952-8180(01)00330-0. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham AJ, Dowd N. Intra-abdominal laparoscopic surgery: Anesthetic implications. In: Healy T, Knight PR, editors. Wyeli and Churchill Davidson: A Practice of Anesthesia. 7th ed. London: CRC Press; 2003. pp. 893–904. [Google Scholar]
- 6.Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R. Handbook of Clinical Anesthesia. 7th ed. Philadelphia: Wolters Kluwer Health; Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 7.De Baerdemaeker LE, Mortier EP, Struys MM. Pharmacokinetics in obese patients. Cont Educ Anaesth Crit Care Pain. 2004;4:152–5. [Google Scholar]
- 8.Strum EM, Szenohradszki J, Kaufman WA, Anthone GJ, Manz IL, Lumb PD. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients: A prospective, randomized study. Anesth Analg. 2004;99:1848–53. doi: 10.1213/01.ANE.0000136472.01079.95. [DOI] [PubMed] [Google Scholar]
- 9.Kaur A, Jain AK, Sehgal R, Sood J. Hemodynamics and early recovery characteristics of desflurane versus sevoflurane in bariatric surgery. J Anaesthesiol Clin Pharmacol. 2013;29:36–40. doi: 10.4103/0970-9185.105792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arain SR, Barth CD, Shankar H, Ebert TJ. Choice of volatile anesthetic for the morbidly obese patient: Sevoflurane or desflurane. J Clin Anesth. 2005;17:413–9. doi: 10.1016/j.jclinane.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Vallejo MC, Sah N, Phelps AL, O'Donnell J, Romeo RC. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth. 2007;19:3–8. doi: 10.1016/j.jclinane.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 12.De Baerdemaeker LE, Struys MM, Jacobs S, Den Blauwen NM, Bossuyt GR, Pattyn P, et al. Optimization of desflurane administration in morbidly obese patients: A comparison with sevoflurane using an 'inhalation bolus' technique. Br J Anaesth. 2003;91:638–50. doi: 10.1093/bja/aeg236. [DOI] [PubMed] [Google Scholar]
- 13.Song D, Joshi GP, White PF. Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology. 1997;87:842–8. doi: 10.1097/00000542-199710000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Sandlr NA. The use bispectral analysis to monitor outpatient sedation. Anesth Prog. 2000;47:72–83. [PMC free article] [PubMed] [Google Scholar]
- 15.Singh PM, Borle A, McGavin J, Trikha A, Sinha A. Comparison of the recovery profile between desflurane and sevoflurane in patients undergoing bariatric surgery-A meta-analysis of randomized controlled trials. Obes Surg. 2017;27:3031–9. doi: 10.1007/s11695-017-2929-6. [DOI] [PubMed] [Google Scholar]
- 16.Bilotta F, Doronzio A, Cuzzone V, Caramia R, Rosa G PINOCCHIO Study Group. Early postoperative cognitive recovery and gas exchange patterns after balanced anesthesia with sevoflurane or desflurane in overweight and obese patients undergoing craniotomy: A prospective randomized trial. J Neurosurg Anesthesiol. 2009;21:207–13. doi: 10.1097/ANA.0b013e3181a19c52. [DOI] [PubMed] [Google Scholar]


