Abstract
Chronic hip pain is distressing to the patient as it not only impairs the daily activities of life but also affects the quality of life. Chronic hip pain is difficult to diagnose as patients often present with associated chronic lumbar spine and/or knee joint pain. Moreover, nonorthopaedic causes may also present as chronic hip pain. The accurate diagnosis of chronic hip pain starts with a detailed history of the patient and thorough knowledge of anatomy of the hip joint. Various physical tests are performed to look for the causes of hip pain and investigations to confirm the diagnosis. Management of chronic hip pain should be mechanistic-based multimodal therapy targeting the pain pathway. This narrative review will describe relevant anatomy, causes, assessment, investigation, and management of chronic hip pain. The focus will be on current evidence-based management of hip osteoarthritis, greater trochanteric pain syndrome, meralgia paresthetica, and piriformis syndrome. Recently, there is emphasis on the role of ultrasound in interventional pain procedures. The use of fluoroscopic-guided radiofrequency in periarticular branches of hip joint has reported to provide pain relief of up to 36 months. However, the current evidence for use of platelet-rich plasma in chronic hip osteoarthritis pain is inconclusive. Further research is required in the management of chronic hip pain regarding comparison of fluoroscopic- and ultrasound-guided procedures, role of platelet-rich plasma, and radiofrequency procedures with long-term follow-up of patients.
Keywords: Chronic pain, greater trochanteric pain syndrome, hip joint, meralgia paresthetica, osteoarthritis, piriformis syndrome, radiofrequency ablation
Introduction
The prevalence of hip pain in the general population is 10%, and it increases with age.[1] In a published study, 14.3% of adults reported significant hip pain on most days over the previous 6 weeks.[2] Hip pain is associated with impairment of simple movements such as sitting and standing which can precipitate chronic pain resulting in impaired functional outcomes and poorer quality of life. The diagnosis of hip pain can be challenging at times due to referred pain from spine or knee, trauma, tumor, abdomen, hernial sites, joint arthropathies, muscular, and neuropathies.[3]
A search of the existing published literature revealed extensive narrative reviews on knee joint osteoarthritis (OA) but not on comprehensive chronic hip pain management.[4] In this narrative review, we searched review articles, randomized controlled trial, and case series from 2000 to 2019 using keywords “hip joint; chronic pain; radiofrequency ablation; osteoarthritis; meralgia paresthetica; piriformis syndrome; greater trochanteric pain syndrome” in PubMed and EMBASE, and relevant articles were included. This narrative review focuses on the pathophysiology, assessment, investigations, and published current evidence-based management of individual conditions causing chronic hip pain, relevant to anesthesiologist and pain physicians.
Relevant anatomy of hip joint
The hip joint is a ball-and-socket synovial joint which transfers the weight between the upper and lower parts of the body and allows movement in the multiaxial plane. This shallow joint is provided depth and stability by the labrum which is a fibrocartilage covering the acetabular rim.[3] The hyaline cartilage covers the articular surfaces and dissipates the shear and compressive forces during hip motion. Hip joint is supported anteriorly by illiofemoral and pubofemoral ligaments and posteriorly by ischiofemoral ligament.[5] The hip joint is surrounded by a large number of muscle groups which help in a wide range of motion [Figure 1].[5] The trochanteric, iliopsoas, gluteus medius, and ischiogluteal bursa act as cushion between the bone and the tendons around the hip joint. Articular branches of nerve to quadratus femoris, obturator, femoral, sciatic, nerves supplying the adjacent muscles, and superior and inferior gluteal supply the hip joint.[5,6] Due to multiple nerves innervating the hip, it is difficult to distinguish between the primary hip and radicular lumbar pain.[3]
Figure 1.
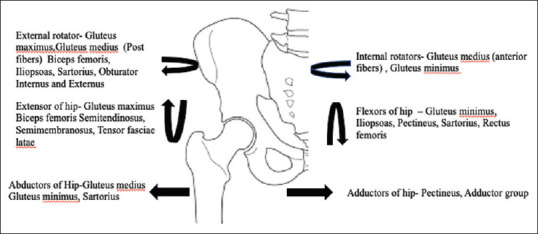
Different movements of the hip joint and the involved muscles
Causes of hip pain
Hip pain can be broadly differentiated into either orthopaedic (intraarticular and extraarticular) and nonorthopaedic causes as mentioned in Table 1.[7,8,9,10] History related to duration, site, severity, characteristic of pain, history of trauma, steroid use, and any referred pain should be asked.[7,8] In prepubescent and adolescent patients, congenital malformations of the femoroacetabular joint, avulsion fractures, and apophyseal or epiphyseal injuries are common.[3] In young skeletally mature patients, hip pain occurs due to musculotendinous strain, ligamentous sprain, contusion, or bursitis. In older adults, degenerative OA and fractures should be considered first.[3] Hip pain can be assessed using different tools such as numeric rating scale, visual analog scale, McGill pain questionnaire, pain quality assessment scale, and Massachusetts general hospital pain center's pain assessment form.[8,9] Red flag signs should always be ruled out which includes sudden onset of severe pain due to hip fracture, infectious arthritis, osteomyelitis, history of malignancy, avascular necrosis, and unexplained chronic pain. Furthermore, a multidisciplinary team approach should be adopted with surgical, physician, pain specialist, psychologist, nursing, and caregivers as major stakeholders.
Table 1.
| Extraarticular hip causes | Intrarticular hip causes | Other causes |
|---|---|---|
| Nerves Meralgia paresthetica Sciatica Obturator nerve irritation Piriformis syndrome |
Bones Femoroacetabular impingement Osteoarthritis Rheumatoid arthritis Septic arthritis Avascular necrosis Perthes disease Development dysplasia of hip Fracture |
Inguinal hernia Gynecological causes Gonadal tumors Inguinal lymphadenopathy Skin conditions Vascular claudication Fibromyalgia |
| Muscles Gluteus muscle tear Abductor muscle injury |
Soft Tissue Labral tear Chondral defect Ligamentum teres injury |
|
| Tendons Snapping hip Trochanteric bursitis |
||
| Ligaments Inguinal ligament strain Joint capsule |
||
| Referred pain Lumbar spine Knee |
Examination of hip joint
The examination of hip pain is guided by look, feel, range of hip movement, neurovascular evaluation, and physical examination test.[3,8,10] Look for any Trendelenburg gait in which there is excessive drop of the contralateral side of pelvis while walking due to weakness of gluteus medius and minimus muscles.[10] Patients with hip OA and slipped capital femoral epiphysis have demonstrated this type of gait dysfunction.[11] Waddling gait occurs due to congenital hip disorders, spinal muscle dystrophy, or myopathy. Antalgic gait is an adopted limp to avoid pain due to injury in the legs. In spastic gait, a patient walks in a crisscross manner, seen in intoxication, brain injury, stroke, and polyneuropathy. In steppage gait, foot hangs with the toes pointing down and scraping the ground while walking, which is seen in patients suffering from multiple sclerosis, peripheral neuropathy, and spinal cord injury.[12] Patients with an intraarticular source of pain can often show this using the C-sign, deep pointer sign, or coordinate fingers [Figure 2].[8,10]
Figure 2.
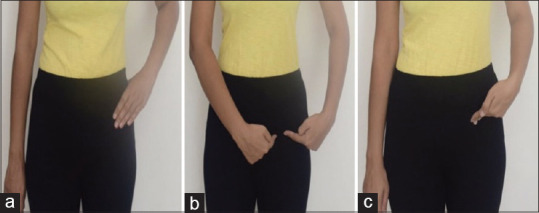
Patient finger pointing indicative of hip joint pain. (a) Trochanteric C sign, (b) triangular sign, and (c) deep pointer sign
The normal range of hip movement is 100° flexion, 30° extension, 40° abduction, and 20°adduction. With hip in flexed position, the internal and external rotation of hip joint is 45°. The range of movement is also restricted in various pathologies of hip joint.
Physical examination of hip can be assessed systematically as starting from leg length difference, contracture of musculature, and intra- and extraarticular hip pathologies as enumerated in Table 2.[13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]
Table 2.
| Anterior pain | Posterior pain | Lateral pain |
|---|---|---|
| Osteoarthritis Iliopsoas bursitis Proximal femur fracture Hip flexor muscle strain Inflammatory arthritis Avascular necrosis of femoral head Acetabular labral tear |
Pyriformis syndrome Sacroiliac joint dysfunction Referred pain from lumbar spine Hip extensor or rotator muscle strain |
Meralgia paraesthetica Greater trochanter bursitis Iliotibial band syndrome Gluteus medius muscle dysfunction |
(a) Leg length difference: Galeazzi test and leg length difference test are commonly performed for leg length difference.[13,14] On measuring the distance from anterior superior iliac spine medial malleolus on each side, if the measured difference is more than 1.5 cm, it is considered abnormal[15]
(b) Contracture of musculature: Noble test and Ober test are done for iliotibial tract. Different tests are done to identify hamstring tightness and adductor contracture test[17,18,19,20] as mentioned in Table 3
(c) For intraarticular hip pain, a patient is made lie flat on the table. One limb is elevated with knee in extension and hip in flexion. A downward resistance is applied at the level of thigh at 30°–45° (Stinchfield test). If there is any intraarticular cause of hip pain, then the patient will complain of pain in the hip[22]
(d) For iliopsoas bursitis, bilateral isometric resisted hip adduction produces groin pain. In trochanteric bursitis, positive resisted abduction release produces pain at the same site. In iliopsoas bursitis pain, a snapping hip manoeuvre produces pain. The patient is made to lie supine with the hip to be examined flexed, then abducted, and externally rotated. The examiner's hand is kept at the inguinal crease. Then the hip is returned to neutral position. A palpable snap during the last phase of the maneuvre is indicative of iliopsoas bursitis. The other tests for hip examination are summarized in Table 3[24,25,26,27]
(e) In piriformis test (FAIR test),[28] The maneuvre elicits pain in hip if pyriformis muscle is tight. If sciatic nerve is pinched in pyriformis muscle, then the patient experiences sciatica-type pain in the hip and leg[29]
(f) The test for hip dislocation is Drehmann sign.[30] The Anvil test is done to differentiate hip pain from spine disorders[31]
(g) Sensory, motor, reflexes, and neurovascular examination should be done of the lower leg. Details will be beyond the scope of this article.
Table 3.
| Test | Performance | Assessment |
|---|---|---|
| Leg length difference test | ||
| Galeazzi test[13,14] | Patient is supine with knees flexed at 90° and the sole of feet lie flat on the examination table. Normally both knees are at the same level. | When one knee is higher than the other, either tibia of the same side is longer or contralateral tibia is shorter. When one knee projects farther forward than the other, either that femur is longer or the contralateral femur is shorter. |
| Actual or functional leg length difference test[13,15] | Patient is standing with shims of varying thickness (0.5, 1, and 2 cm) placed in/under shortened leg until pelvic obliquity is fully compensated. | This will give the estimate of leg length difference. In cases where shims cannot compensate for pelvic obliquity, patient is having a fixed deformity of one or more joints leading to functional leg length difference. This can be a result of flexion or adduction contracture in hip. The pelvic dips towards normal side; the normal leg appears lengthened and effected leg shortened. |
| Contracture of musculature | ||
| Noble compression test[18,19,20] | Patient lies on a flat table with knee at 90° and hips at 50°. The examiner moves the knee back and forth several times from 0° to 90° while palpating the lateral epicondyle of femur on the effected site. | Palpable snapping, rubbing, crepitus or localized pain along the distal iliotibial tract (ITB) suggests a iliotibial tract frictional tendinitis. Pain in the posterior aspect of thigh indicates hamstring contracture. |
| Ober test[13] | Patient is in lateral position, the leg to be examined is up, slightly adducted, and hip is slightly hyperextended. The examiner places hand on distal iliotibial tract and allows leg to move from abduction to adduction. | If the leg fails to touch the floor then Iliotibial band shortening is present. |
| Fingertip test[14] | Patient is asked to sit on a flat table with one leg flexed at hip and knee and the other extended at hip and knee. Patient is asked to touch the toe of the extended leg with hand. | Inability to touch the toes of feet and hand in the general area of foot and complains of “pulling” pain in posterior thigh indicates hamstring contracture. |
| Test for hip osteoarthritis | ||
| Trendelenburg’s sign[15] | Patient in standing position is instructed to lift one leg up by flexing their hip and knee, standing on only one leg. | Positive test is 2 cm drop of the contralateral side of pelvis once the leg is lifted. Sensitivity (SN) 55%, specificity (SP) 70% |
| Test for Impingement/labral tear | ||
| Impingement FADIR test[25,26,27] | Supine, bilateral legs extended. Clinician passively moves the patient’s one leg to 90° hip and knee flexion. The leg is then passively adducted and internally rotated with overpressure to both motions at end range | Positive test is reproduction of concordant pain, locking, clicking and catching pain. |
| Thomas test[27] | Patients hold nontested leg toward their chest with bilateral arms as the clinician passively lowers the tested leg into extension. Holding the other knee to chest allows flatten lumbar lordosis and stabilizes pelvis. | If iliopsoas contracture is present then, the extended leg will not reach a full extension position on the table. |
| Log Roll (Freiberg) test[13,14] | Patient is in supine position with hip in a neutral position, and the leg is passively rolled into full internal and external rotation. | A click reproduced during the test is suggestive of labral tear, while increased external rotation range of movement may indicate iliofemoral ligament laxicity. |
| FABER test (Patrick test)[13,15] | Patient is in supine position, and one leg is extended straight on table. The other leg is flexed, adducted, and externally rotated at the hip joint. The flexed leg is pressed at knee joint. | Pain produced in groin indicates hip pain and if produced in gluteal region indicates sacroiliac pathology. |
| Lumbar spine radiculopathy | ||
| SLR test[11,15] | Patient is in supine, and the examiner passively elevates the leg by holding it at ankle. The hip is flexed to 70°-90° with knee extended. | Positive test is reproduction of pain in from hip to ankle in lumbosacral radiculopathy. Both SLR and cross SLR put strain on lumbosacral nerve roots. Pain restricted to posterior aspect of thigh indicates tension on hamstrings. |
| Miscellaneous | ||
| Piriformis test (FAIR test)[28,29] | Patient lies in lateral position with test leg uppermost.[28] The patient flexes upper hip at 60° with flexed knee. The examiner stabilizes the hip and applies downward pressure on the upper knee with internal rotation. | If sciatic nerve is pinched in pyriformis muscle than patient experiences sciatica type pain in hip and leg.[29] |
FADIR: Flexion-adduction-internal rotation; SLR: Straight Leg Raise
Investigations
Blood investigations such as complete blood counts and erythrocyte sedimentation rate can differentiate infective versus inflammatory cause of hip pain. X-ray of the hip joint should be performed if there is any suspicion of acute fracture, dislocation, or stress fracture. Ultrasonography is a useful technique for evaluating individual tendons, identifying joint effusions, confirming suspected bursitis, and functional causes of hip pain. Conventional magnetic resonance imaging (MRI) of the hip can detect many soft tissue abnormalities and is the preferred imaging modality. Conventional MRI has a sensitivity of 30% and an accuracy of 36% for diagnosing hip labral tears, whereas magnetic resonance arthrography provides added sensitivity of 90% and accuracy of 91% for the detection of labral tears.[32]
Management of chronic hip pain
Chronic pain involves nociceptive or/and neuropathic pain. Nociceptive pain originates from the bone, synovium, and other tissues. In nociceptive pain, initially there is only peripheral sensitization and pain can be controlled with systemic or topical drugs as they decrease the release of peripheral inflammatory mediators.[33] Neuropathic pain is due to injury in the path of somatosensory nervous system. For example, in piriformis syndrome, there is stretching of nerves or due to lumbar disc prolapse there is radiculopathy. In chronic conditions such as OA or RA, neural sensitization will not be confined only to the periphery. Due to persistent tissue inflammation around the nerve, pain mediators are released which increase the excitability of pain pathways, and hence lead to neuroplasticity pain.[33] Referred pain and pain away from the original site can be neuroplasticity in origin. The increased excitability of spinal neurons in this condition leads to enhanced pain perception at the site of injury. In chronic pain conditions, the presence and severity of pain is also determined by psychological and social factors. These external factors modulate nociceptive processing at a supra spinal or cortical level enhancing the pain perception, reporting, and behavioral change.[33]
Management of individual chronic hip pain conditions
-
OA hip
OA of the hip is the second most common joint after knee affecting women twice as common as men. The common risk factors are genetic, dysplasia of hip, hip joint laxity, increased body mass index, and manual labour. These factors cause increase in wear and tear, instability, malalignment, microtrauma, and structural damage of hip joint[34]
Patients with hip OA present with groin pain, which is initially intermittent, worse at the end of the day, and activity-related. The most popular score for OA is Kellgren–Lawrence system based on the assessment of the presence of osteophytes, joint space narrowing, subchondral sclerosis, and deformity of femoral head and acetabulum. Computed tomography (CT)-based scoring is accurate and involves assignment of score to osteophytes, subchondral cyst, and joint space narrowing for determining severity of OA. MRI helps in diagnosing cartilage and labrum pathology[35]
In evidence-based medicine, Level A evidence means a strong recommendation and should be followed. Level B evidence is a recommendation, but the clinician should be alert to new information and sensitive to patient preferences. Level C evidence signifies an option and the clinician should be flexible in their decision-making. Level D evidence lacks a sufficient data and its significance is very less[36]
Evidence-based clinical practice guidelines for the management of OA hip are formulated by the American Academy of Orthopedic Surgeons,[37] American College of Rheumatology,[38] National Institute for Health and Care Excellence (NICE),[39] and Royal Australian College of General Practitioners (RACGP).[40]
- (ii) Moderate strength evidence (Level B) does not support the use of glucosamine sulfate because it did not show any added benefits than placebo for improving function, reducing stiffness, and decreasing pain for patients with symptomatic OA hip[37]
- (iii) Strong evidence (Level A) supports the use of intraarticular corticosteroids to improve function and reduce pain in the short-term for patients with symptomatic OA hip.[37] Indications of intraarticular hip joint corticosteroid injection are 1) to determine whether hip pain is secondary to hip versus spine pathology, 2) to determine intraarticular versus extraarticular pathology, 3) likelihood of achieving pain relief with hip arthroplasty, 4) whether surgery is contraindicated, and 5) in young patients in whom there is concern for the longevity of implant. One should be cautious while giving intraarticular steroid injections as rapid destructive OA is one of its complications[41]
- (iv) Ultrasound-guided hip joint injection: The patient lies in supine position with linear transducer placed in longitudinal oblique plane along the axis of the femoral neck to examine the anterior recess. The femoral head is identified and the probe is positioned to obtain an axial view through the head. Then slide the probe distally toward the junction of the femoral neck and head. The needle is inserted from the lateral side along the long axis of the probe [Figure 3]. When the needle as bone contact, it will lie within the joint on the anterolateral aspect of head–neck junction. Under strict asepsis, 4–5 mL of mixture of steroid and local anesthetic is injected at the anterior recess in the axial plane[42]
- (v) Strong evidence (Level A) does not support the use of intraarticular hyaluronic acid because it does not perform better than placebo for function, stiffness, and pain in patients with symptomatic OA hip[37]
- (vi) Strong evidence (Level A) supports the use of physical therapy as a treatment to improve function and reduce pain for patients with OA of the hip with mild to moderate symptoms.[37,38] It is strongly recommended to perform aerobic and stretching exercises, lose weight if obese, and to receive psychosocial interventions[37,38]
- (vii) Duloxetine could be considered for some people with knee and/or hip OA when other forms of pain relief are inadequate.[40] There is a strong recommendation against the use of the oral and transdermal opioids, viscosupplementation injection for hip OA, doxycycline, strontium ranelate, interleukin-1 inhibitors, and stem-cell therapy. Due to a lack of high-quality evidence, no recommendation can be made for the injections of platelet-rich plasma (PRP), NSAIDs cream applied locally, capsaicin, collagen, and methylsulfonylmethane[40]
- (viii) A moderate quality evidence was reported favoring tramadol alone or in combination with acetaminophen versus placebo but had no important benefit on mean pain or function in people with OA, although slightly more people in the tramadol group report an important improvement (defined as 20% or more)[43]
- (ix) Patients with advanced symptoms and pathology not responding to conventional treatment should be referred for arthroplasty. But total hip arthroplasty is also associated with concerning failure rate (5%–15%),[41,44] significant cost, and persistent postsurgical pain (7%–28%).[45,46] Nerves supplying the hip joint like articular branches of the obturator nerve, articular branches of the femoral nerve, articular branches of the sciatic, and superior gluteal nerve can be ablated with radiofrequency. Ablation of sensory nerves by preserving motor branches can improve the success rate and decrease the complications[7]
- (x) Fluoroscopic-guided ablation of articular branches of hip joint: Initially, a diagnostic block of 0.5–3 mL of local anesthetic is administered under fluoroscopic guidance. For articular branches of the obturator nerve, the target is the point immediately inferior to the “teardrop” silhouette, formed by the junction of the pubic and ischial bones. For articular branches of the femoral nerve, the target point is immediately inferior and medial to the anterior inferior iliac spine [Figure 4]. In narrative review, 14 publications reported high success rate in relieving chronic hip pain at 8 days to 36 months after the procedures, but none of the publications was randomized controlled trials.[7]
-
Greater trochanteric pain syndrome
The term “greater trochanteric pain syndrome” encompasses gluteal medius and minimus tendinopathy/tears, trochanteric bursitis, and external coxa saltans. Bursitis occurs in 4%–46% and gluteal tendinopathy in 18%–50% patients.[47] The trochanteric bursa is located deep to the iliotibial band and superficial to the hip abductors and is a frequent cause of lateral hip pain. A localized tenderness may be elicited on deep palpation of the lateral aspect of greater trochanter. Pain is elicited with resisted hip abduction and hip extension more during gluteal tendinopathy when compared with trochanteric bursitis. Ultrasound will show increased fluid signal with trochanteric bursa[47]
Gluteal tendinopathy presents as chronic activity-related pain and impaired performance of a tendon. X-ray of the hip shows normal study.[48] Patients are advised to avoid cross leg standing and lying on either side as it increases friction of tendon and pain[48]
Conservative treatment is gold standard for 90% success rate. The initial treatment of trochanteric bursitis is conservative with rest, physical therapy, and NSAIDs.[47] In gluteal tendinopathy, therapy is directed toward quadriceps strengthening and ilio tibial band stretching. Hip abduction exercises directed toward strengthening and stretching of gluteus medius and minimus should be initiated. For persistent cases, a corticosteroid injection should be given and repeated in 6 weeks if pain persists.[48] Concern regarding corticosteroid injection is the risk of weakening the tendon structure in long-term. Recently, use of PRP has reported improvement in patients at 3- and 12-month follow up, but lacked high-quality evidence.[49] Surgery may be considered if these measures do not relieve symptoms and pain lasts longer than 1 year[47]
Ultrasound-guided injection of greater trochanteric bursa is best approached with patient in lateral position with effected side up. Under strict asepsis, a linear probe in placed in the longitudinal plane to greater trochanter. Trochanteric bursae lies adjacent to the bone cortex, and a combination of steroid and local anesthetic is injected after aspiration[42]
For iliopsoas tendinopathy, the patient is positioned supine and a linear probe is placed along iliopsoas tendon lateral to the neurovascular bundle. The needle is advanced from the lateral side of the thigh, in plane, and a mixture of steroid and local anaesthetic is injected in the peritendon area.[42]
-
Meralgia paresthetica
Meralgia paresthetica (MP) refers to the entrapment of the lateral femoral cutaneous nerve at the level of the inguinal ligament. The cause is usually idiopathic but can be due to trauma, overuse, leg/trunk discrepancy, prolonged standing, external compression by belts, weight gain, and tight clothing. The symptoms include paresthesia, numbness, burning sensation, dysesthesia, and pain over the lateral aspect of the thigh. Treatment includes removal of source of compression, physical therapy, NSAIDs, tricyclic antidepressants, and anticonvulsants. For patients irresponsive to initial treatment, local anesthetic and/or corticosteroid injection under ultrasound guidance may be therapeutic.[42] Pulsed radiofrequency of the lateral femoral cutaneous nerve (LFCN) provides an effective, low-risk treatment in patients refractory to conservative medical management.[50] In a recently published review article, insufficient data were found to compare the recommendation of neurolysis or neurectomy as the modality of treatment for MP.[51]
Figure 3.
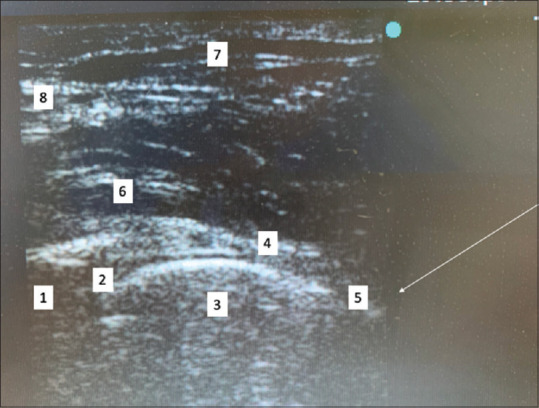
Ultrasound image showing hip joint injection. Longitudinal view high-frequency ultrasound linear probe. 1 acetabulum, 2 hyperechoic labrum, 3 femoral head, 4 iliofemoral ligament, 5 anterior recess, 6 iliopsoas, 7, sartorius. The white line represents the trajectory of the needle for placement in hip joint
Figure 4.
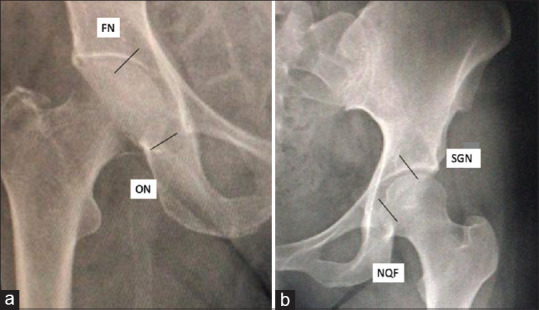
Suggested site of needle placement for radiofrequency ablation of articular nerves under fluoroscopic guidance. (a) Site for articular branches of FN – femoral nerve, OV – obturator nerve on anterior surface of hip joint. (b) Site for articular branches of SGN – superior gluteal nerve, NQF – nerve to quadratus femoris on posterior surface of hip joint
4) Piriformis syndrome
Treatment of piriformis syndrome is mainly conservative methods, such as stretching exercises, injections, NSAIDs, muscle relaxants, ice, and activity modifications.[52] Corticosteroid injections may provide temporary analgesia to allow patients to participate in physical therapy, but it does not correct the underlying pathophysiology and may need to be repeated. Injections with neurotoxins such as botulinum toxin are also being investigated.[53,54] Surgical decompression can be considered as the last option to reduce any tension in the piriformis muscle by releasing fibrous bands or constrictions compressing the sciatic nerve.[52]
Clinical points for management of chronic hip pain
Correct diagnosis is most important in management of chronic hip pain. Taking detailed history, clinical examination, investigations, and clinical judgement allow one to reach the cause of pain
Mechanistic-based management of chronic pain relies on the type of pain, somatic, neuropathic, or mixed type of chronic pain
Strong evidence in support for use of NSAIDS and use of physical therapy as a treatment to improve function and reduce pain for patients with OA hip with mild to moderate symptoms
For OA hip, intra-articular hip joint once very popular is not being slowly replaced with extra-articular ablation of articular branches of hip joint
Treatment of trochanteric bursitis is conservative and NSAIDS. Local anesthetic with steroid may be injected in refractory cases
Gluteal tendinopathy therapy is directed toward quadriceps strengthening and iliotibial band stretching. Recently, use of PRP has reported improvement in patients at 3- and 12-month follow up, but lacked high-quality evidence
For MP and pyriformis syndrome, removal of source of compression, physical therapy, NSAIDs, tricyclic antidepressants, and anticonvulsants. Pulsed radiofrequency of the LFCN provides an effective, low-risk treatment in patients refractory to MP. For pyriformis syndrome, corticosteroid injections may provide temporary analgesia and may need to be repeated.
Conclusion
Management of chronic hip pain requires accurate diagnosis, multimodal approach with nonpharmacological, pharmacological, and pain-relieving procedures for therapeutic success. Further research is required in comparison of fluoroscopic- and ultrasound-guided procedures, role of PRP, and radiofrequency procedures with long-term follow-up of chronic hip pain patients.
Financial support and sponsorship
Institutional funding only.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands: Prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003;102:167–78. doi: 10.1016/s0304-3959(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 2.Christmas C, Crespo CJ, Franckowiak SC, Bathon JM, Bartlett SJ, Andersen RE. How common is hip pain among older adults. Results from the Third National Health and Nutrition Examination Survey? J Fam Pract. 2002;51:345–48. [PubMed] [Google Scholar]
- 3.Wilson JJ, Furukawa M. Evaluation of the patient with hip pain. Am Fam Physician. 2014;89:27–34. [PubMed] [Google Scholar]
- 4.Timmins KA, Leech RD, Batt ME, Edwards KL. Running and knee osteoarthritis: A systematic review and meta-analysis. Am J Sports Med. 2017;45:1447–57. doi: 10.1177/0363546516657531. [DOI] [PubMed] [Google Scholar]
- 5.Chang A, Hubbard JB. Anatomy, Bony Pelvis and Lower Limb, Femur.StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2019-2018. [PubMed] [Google Scholar]
- 6.Alzaharani A, Bali K, Gudena R, Railton P, Ponjevic D, Matyas JR, et al. The innervation of the human acetabular labrum and hip joint: An anatomic study. BMC Musculoskelet Disord. 2014;15:41. doi: 10.1186/1471-2474-15-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatia A, Hoydonckx Y, Cohen SP. Radiofrequency procedures to relieve chronic hip pain, an evidence-based narrative review. Reg Anesth Pain Med. 2018;43:1–12. doi: 10.1097/AAP.0000000000000694. [DOI] [PubMed] [Google Scholar]
- 8.Margo K, Drezner J, Motzkin D. Evaluation and management of hip pain: An algorithmic approach. J Fam Pract. 2003;52:607–17. [PubMed] [Google Scholar]
- 9.Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 10.Dick AG, Houghton JM, Bankes MJK. An approach to hip pain in a young adult. BMJ. 2018;361:k1086. doi: 10.1136/bmj.k1086. [DOI] [PubMed] [Google Scholar]
- 11.Song KM, Halliday S, Reilly C, Keezel W. Gait abnormalities following slipped capital femoral epiphysis. J Pediatr Orthop. 2004;24:148–55. doi: 10.1097/00004694-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Hurwitz DE, Foucher KC, Andriacchi TP. A new parametric approach for modeling hip forces during gait. J Biomech. 2003;36:113–9. doi: 10.1016/s0021-9290(02)00328-7. [DOI] [PubMed] [Google Scholar]
- 13.Hip, Buckup K. Clinical Tests for the Musculoskeletal System: Examinations, Signs, Phenomena. 2nd ed. Thieme Publishing Group, Georg Thieme, Rüdigerstrasse, Germany; 2008. pp. 167–95. [Google Scholar]
- 14.Reiman MP, Thorborg K. Clinical examination and physical assessment of hip joint-related pain in athletes. Int J Sports Phys Ther. 2014;9:737–55. [PMC free article] [PubMed] [Google Scholar]
- 15.Reiman MP, Mather RC, III, Cook CE. Physical examination tests for hip dysfunction and injury. Br J Sports Med. 2015;49:357–61. doi: 10.1136/bjsports-2012-091929. [DOI] [PubMed] [Google Scholar]
- 16.Beals C, Flanigan D. A review of treatments for iliotibial band syndrome in the athletic population. J Sports Med. 2013;2013:367169. doi: 10.1155/2013/367169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ellis R, Hing W, Reid D. Iliotibial band friction syndrome—A systematic review. Man Ther. 2007;12:200–8. doi: 10.1016/j.math.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 18.Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. Is iliotibial band syndrome really a friction syndrome? J Sci Med Sport. 2007;10:74–6. doi: 10.1016/j.jsams.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: Implications for understanding iliotibial band syndrome. J Anat. 2006;208:309–16. doi: 10.1111/j.1469-7580.2006.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Falvey EC, Clark RA, Franklyn-Miller A, Bryant AL, Briggs C, McCrory PR. Iliotibial band syndrome: An examination of the evidence behind a number of treatment options. Scand J Med Sci Sports. 2010;20:580–7. doi: 10.1111/j.1600-0838.2009.00968.x. [DOI] [PubMed] [Google Scholar]
- 21.Youdas JW, Madson TJ, Hollman JH. Usefulness of the Trendelenburg test for identification of patients with hip joint osteoarthritis. Physiother Theory Pract. 2010;26:184–94. doi: 10.3109/09593980902750857. [DOI] [PubMed] [Google Scholar]
- 22.Willett GM, Keim SA, Shostrom VK, Lomneth CS. An anatomic investigation of the ober test. Am J Sports Med. 2016;44:696–701. doi: 10.1177/0363546515621762. [DOI] [PubMed] [Google Scholar]
- 23.Delahunt E, McEntee BL, Kennelly C, Green BS, Coughlan GF. Intrarater reliability of the adductor squeeze test in gaelic games athletes. J Athl Train. 2011;46:241–5. doi: 10.4085/1062-6050-46.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lequesne M, Mathieu P, Vuillemin-Bodaghi V, Bard H, Djian P. Gluteal tendinopathy in refractory greater trochanter pain syndrome: Diagnostic value of two clinical tests. Arthritis Rheum. 2008;59:241–6. doi: 10.1002/art.23354. [DOI] [PubMed] [Google Scholar]
- 25.Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop. 2009;80:314–8. doi: 10.3109/17453670902988402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sink EL, Gralla J, Ryba A, Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop. 2008;28:806–11. doi: 10.1097/BPO.0b013e31818e194f. [DOI] [PubMed] [Google Scholar]
- 27.Petersilge CA, Haque MA, Petersilge WJ, Lewin JS, Lieberman JM, Buly R. Acetabular labral tears: Evaluation with MR arthrography. Radiology. 1996;200:231–5. doi: 10.1148/radiology.200.1.8657917. [DOI] [PubMed] [Google Scholar]
- 28.Foster MR. Piriformis syndrome. Orthopedics. 2002;25:821–5. doi: 10.3928/0147-7447-20020801-12. [DOI] [PubMed] [Google Scholar]
- 29.Beatty RA. The piriformis muscle syndrome: A simple diagnostic maneuver. Neurosurgery. 1994;34:512–4. doi: 10.1227/00006123-199403000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Kamegaya M, Saisu T, Nakamura J, Murakami R, Segawa Y, Wakou M. Drehmann sign and femoro-acetabular impingement in SCFE. J Pediatr Orthop. 2011;31:853–7. doi: 10.1097/BPO.0b013e31822ed320. [DOI] [PubMed] [Google Scholar]
- 31.Pasic N, Bryant D, Naudie D, Willits K. Diagnostic validity of the physical examination maneuvers for hip pathology: A systematic review. Orthopedic Muscul Syst. 2014;3:157. [Google Scholar]
- 32.Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Description of pain provocation tests used for the diagnosis of sports-related chronic groin pain: Relationship of tests to defined clinical (pain and tenderness) and MRI (pubic bone marrow oedema) criteria. Scand J Med Sci Sports. 2005;15:36–42. doi: 10.1111/j.1600-0838.2004.00380.x. [DOI] [PubMed] [Google Scholar]
- 33.Kidd BL, Langford RM, Wodehouse T. Arthritis and Pain. Current approaches in the treatment of arthritic pain. Arthritis Res Ther. 2007;9:214. doi: 10.1186/ar2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aresti N, Kassam J, Nicholas N, Achan P. Hip osteoarthritis. BMJ. 2016;354:i3405. doi: 10.1136/bmj.i3405. [DOI] [PubMed] [Google Scholar]
- 35.Lewinska A, Palczewski P, Rongies W, Szczesny G, Tomaszewski W. Advances in Imaging of Hip Osteoarthritis. Ortop Traumatol Rehabil. 2019;21:1–14. doi: 10.5604/01.3001.0013.0384. [DOI] [PubMed] [Google Scholar]
- 36.Burns PB, Rohrich RJ, Chung KC. The Levels of Evidence and their role in Evidence-Based Medicine. Plast Reconstr Surg. 2011;128:305–10. doi: 10.1097/PRS.0b013e318219c171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jevsevar DS. Treatment of osteoarthritis of the knee: Evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21:571–6. doi: 10.5435/JAAOS-21-09-571. [DOI] [PubMed] [Google Scholar]
- 38.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64:465–74. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 39.National Institute for Health and Care Excellence. Osteoarthritis: Care and Management in Adults. London: NICE; 2014. [PubMed] [Google Scholar]
- 40.Fernandez M, Wall P, O'Donnell J, Griffin D. Hip pain in young adults. Aust Fam Physician. 2014;43:205–9. [PubMed] [Google Scholar]
- 41.Tiwari A, Karkhur Y, Keeney JA, Aggarwal A. Rapid destructive osteoarthritis of the hip after intra-articular steroid injection. Arthroplast Today. 2018;4:184–6. doi: 10.1016/j.artd.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rowbotham EL, Grainger AJ. Ultrasound - Guided intervention around the hip joint. AJR Am J Roentgenol. 2011;197:W122–7. doi: 10.2214/AJR.10.6344. [DOI] [PubMed] [Google Scholar]
- 43.Toupin April K, Bisaillon J, Welch V, Maxwell LJ, Jüni P, Rutjes AW, et al. Tramadol for osteoarthritis. Cochrane Database Syst Rev. 2019;5:CD005522. doi: 10.1002/14651858.CD005522.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grayson CW, Decker RC. Total joint arthroplasty for persons with osteoarthritis. PM R. 2012;4:S97–103. doi: 10.1016/j.pmrj.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 45.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis. A systematic review of prospective studies in unselected patients? BMJ Open. 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: A nationwide questionnaire study. Acta Anaesthesiol Scand. 2006;50:495–500. doi: 10.1111/j.1399-6576.2006.00976.x. [DOI] [PubMed] [Google Scholar]
- 47.Rowand M, Mackler L. How should you treat trochanteric bursitis? J Fam Pract. 2009;58:494–500. [PubMed] [Google Scholar]
- 48.Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, et al. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: Prospective, single blinded, randomised clinical trial. BMJ. 2018;361:k1662. doi: 10.1136/bmj.k1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ali M, Oderuth E, Atchia I, Malviya A. The use of platelet-rich plasma in the treatment of greater trochanteric pain syndrome: A systematic literature review. J Hip Preserv Surg. 2018;5:209–19. doi: 10.1093/jhps/hny027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Onat SS, Ata AM, Ozcakaar Ultrasound-guided diagnosis and treatment of meralgia paresthetica. Pain Physician. 2016;19:667–9. [PubMed] [Google Scholar]
- 51.Payne R, Seaman S, Sieg E, Langan S, Harbaugh K, Rizk E. Evaluating the evidence: Is neurolysis or neurectomy a better treatment for meralgia paresthetica? Acta Neurochirurgica. 2017;159:931–6. doi: 10.1007/s00701-017-3136-x. [DOI] [PubMed] [Google Scholar]
- 52.Philip CN, Candido KD, Joseph NJ, Crystal GJ. Successful treatment of meralgia paresthetica with pulsed radiofrequency of the lateral femoral cutaneous nerve. Pain Physician. 2009;12:881–5. [PubMed] [Google Scholar]
- 53.Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009;40:10–8. doi: 10.1002/mus.21318. [DOI] [PubMed] [Google Scholar]
- 54.Fishman LM, Konnoth C, Rozner B. Botulinum neurotoxin type B and physical therapy in the treatment of piriformis syndrome: A dose-finding study. Am J Phys Med Rehabil. 2004;83:42–5. doi: 10.1097/01.PHM.0000104669.86076.30. [DOI] [PubMed] [Google Scholar]


